Abstract
Purpose
Horses are used for many recreational and occupational activities. They are large, strong, temperamental, and unpredictable animals and people involved with them are at risk for injuries, from minor abrasions to severe injuries that may lead to death. This review reports on horse trauma in relation to the characteristics of injured equestrians, characteristics of horse trauma, and clinical outcomes.
Methods
A literature search was conducted from health-related electronic databases to identify studies from 2018 to 2023. The search returned 115 relevant full-text articles but after screening and assessment for eligibility, 39 were included in this review for a detailed examination of horse trauma epidemiology. Most studies were undertaken in the USA and the most used method was a retrospective review of hospital or trauma registry data.
Results
There have only been very slight changes in horse trauma numbers and outcomes over the past 5 years. Most injuries often follow falls and kicks. Females in their late-20 s to mid-30 s who are recreational equestrians are the group most represented in the data. The commonest injuries include fractures, and head, thoracic, and abdominal trauma. Most individuals with horse trauma were treated in the Emergency Department and discharged. For the equestrians who were admitted to hospital, around one-third required surgery. Mortality rates are very low.
Conclusion
The popularity of occupational and recreational horse activities does not seem to wane and horse trauma continues to represent a significant concern for the health system. Health care workers need to be cognizant of the scope of trauma presentations as the mechanisms of injury can be complicated putting the equestrian at a high risk of associated injuries that may be life-threatening.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Horses are large, heavy, and unpredictable animals that run at high speeds and can kick, strike, and bite. Despite these inherent risks, horses and humans have close ties in occupational and recreational activities with all age and gender groups involved. In the United States of America (USA), it is estimated that each year 20 million people aged 16 years and older participate in horse-related activities [1]. British Equestrian reported 1.8 million regular equestrians and approximately 1% (283,000) of the Australian population are horse enthusiasts [2, 3]. Most horse trauma occurs during recreational activities, with a greater representation of adult females, children, and teenagers. Injuries occur in both mounted and unmounted situations with many injuries considered as serious. While fractures are the predominant injury sustained, it is abdominal trauma and head injuries, ranging from concussion through to severe structural brain injury, that are usually responsible for longer hospitalization and death.
Horse trauma incurs significant costs at several levels. In a Swedish study (1997–2014), Meredith et al. [4] gave a conservative calculation of 3.2 million Euro annually of 1800 Euro per injury event. A USA study which analyzed thoroughbred horse farm workers’ compensation insurance claims (2008–2015) found that the total amount paid on claims were USD $11,181,268 and the total number of lost-time days was 18,412 [5]. When analyzing the costs for treatment at a USA Level 1 Trauma Centre for the period of 2010–2013, Adler et al. [6] calculated the mean expenditure per injured patient at USD $29,737 with the total expenditure for all the patients (N = 222) more than USD $6.5 million. Jones et al. [7] estimated the cost for 332 patients in New Zealand (2012–2016) at NZ $2.6 million with the costliest 10% of patients accounting for 36.9% of the overall cost (NZ $929,285). The average cost per patient was NZ $7805 with males costing more (NZ $8901) than females (NZ $7391). Adults were more expensive to treat than children (0–14 years of age) and over 76.3% of the total cost was for recreational equestrians.
Four previous literature reviews on horse trauma were sourced [8,9,10,11]. The focus of Zuckerman et al. [10] was specifically on traumatic brain injury and Gates and Lin [11] on head and spinal injuries. Havlik [9] and Meredith et al. [8] took a broader review of injuries with Havlik [9] reviewing literature from 2007 to 2009 and Meredith et al. [8] reviewing literature from 1973 to 2017. Therefore, it is timely to provide an updated review of the literature. The epidemiology of horse trauma is difficult to specifically characterize with some studies analyzing large national databases through to small, single institutions from a variety of countries and geographical areas. Taking this diversity into account, this review was designed to critically appraise and summarize reports on horse trauma as well as examine the characteristics of injured equestrians, characteristics of horse trauma, and clinical outcomes.
Methods
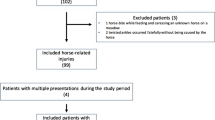
Search terms used were “horse/hors* or equine or equestrian and trauma or injury/injur*or accident/accident* or fall” to identify English language studies in academic journals from 1 Jan 2018 to 30 June 2023. See Fig. 1 for details of the study selection process.
Results
There were 39 articles which detailed the injury epidemiology of horse trauma. Most studies (30.8%) were published in 2019. Over 30% (n = 13) of the studies were conducted in the USA, followed by Australia (n = 5), Ireland (n = 4), and then various other countries including the UK, Israel, and New Zealand. There was one international study, 12 that analyzed national databases, eight that analyzed data from multiple centers, and 18 that reported on single centers. Retrospective analysis of medical records was the most common method (87.2%; n = 34), then cross-sectional (7.7%; n = 3) with two prospective studies (5.1%). Three studies specifically examined pediatric samples. Most studies (26/39) reported on trauma in all horse-related activities, whereas five investigated injuries in horse racing, three looked at injuries on farms, three examined injuries from horse sport competitions, and there were individual studies for amateur, collegiate, and riding school equestrians. The majority (29/39) of studies reported on the overall injury pattern to the entire body, while four detailed maxillofacial injuries, three specifically examined head and neck trauma, two concentrated on pelvic injuries, and one looked a radial neck in children. More summary details are provided in table format (see Table 1).
Incidence of injury
It needs to be noted that incidence rates of injury vary geographically and is dependent on the type of horse activity being undertaken. The type of data available and the methods of data collection also influence consistent reporting. Despite this, four studies reported a decrease in horse trauma over their study periods [19, 21, 22, 36], one reported no change [39], and Jones et al. [7] reported a slight non-significant annual increase. A recent assessment of fatal incidents on Australian farms involving children (2001–2019) found that horses were the agent of injury in 5.4% of cases [47]. A retrospective analysis of data from the USA’s Nationwide Emergency Department Sample identifying horse trauma-related visits revealed 21,899 visits but when weighted these represented 100,964 visits or 0.64 per 10,000 persons (95% CI, 0.60–0.68) [1].
Characteristics of injured equestrians
Gender
Of the 39 studies included in the review, 20 reported that horse-related trauma most frequently involved females with the disparity ranging between 52 [42] and 93.7% [29]. This skewing is usually explained by the fact that many recreational and amateur horse-related activities are predominantly undertaken by females [9] with British Equestrian recently reporting a female participation rate of 74% [2]. However, Gross et al. [39] found males outnumbered females in a pediatric population. In a study by Samuels et al. [14] that undertook subgroup analyses, it was found occupational injuries affected predominantly males between the ages of 18 and 49 years, while non-occupational injuries predominantly affected females less than 18 years old and greater than 60 years old (p < 0.001). Where the type of horse- activity is specified such as in a competition it was found that the frequency of injury did not differ significantly in male and female participants [23, 41].
Age
In respect to age, some studies reported mean age whereas others reported median. The years of age between 22 and 49 is the most common with females generally in their late-20 s to mid-30 s and males in their early 40 s. However, two large national epidemiological studies in the USA found younger populations were more predominant. Asa et al. [1] who analyzed horse trauma from the Nationwide Emergency Department Sample (2010–2014; N = 21,899) found the proportion of visits were highest in females aged 15–19 years. Similarly, Acton et al. [19] using the National Electronic Injury Surveillance System (1990 – 2017; N = 1,836,536) found the injury rate per 100,000 population was highest among 5–18-year-olds (gender not specified). Studies that concentrated on pediatrics have a mean age of 11 years with male children tending to be younger [30, 35, 39].
Occupational or non-occupational
Abdulkarim et al. [44] reported that 82% of those injured were recreational horse equestrians. Whereas Samuels et al. [14] established that 6.1% of injuries were occupation-related and furthermore, of the non-occupational injuries, 43.7% occurred on a farm, 8.6% occurred in sporting locations, 21.7% occurred in recreational locations, and 20% occurred in residential locations.
Characteristics of horse trauma
Mechanism of injury
The most common mechanism of injury was a fall from a horse, with the proportion ranging from 45.1 to 86.4% of all mechanisms [36, 41]. Equestrians who had fallen had the highest injury scores, were most likely to be admitted to hospital, had the most diagnostic imaging performed, and tied with horse kick injuries for the longest mean hospital stay [6]. Kicks, usually while unmounted, accounted for around 23% of injuries [29] and often caused facial fractures [33, 40]. Other important mechanisms included trampling (10%) as well as strikes, bites, and being squashed [32]. Injuries also occur in relation to being caught up in equipment such reins, leads, and stirrups or landing on saddle horns [29, 35, 43]. Two studies reported that approximately 20% of injured equestrians had a combined mechanism such as being trampled or knocked following a fall [7, 28].
Injured body regions and types of injury
With horse trauma, the musculoskeletal system is commonly affected. Although dependent on specific study categorizations, generally in order, the most frequently injured body parts were the thorax, upper extremities and lower extremities, spinal column, head, face, and abdomen [14, 16, 28]. Table 2 summarizes the injury patterns by body part reported in the four largest epidemiological studies identified for this review. It is important to point out that in over 28% of the injured cases, the equestrian suffered multiple injuries resulting from the same injury event [4].
Most diagnosed conditions were contusions (41.8%), followed by one or more fractures (39%), traumatic brain injury (13%), and visceral organ injury (3.1%) [1, 4, 17, 28, 44]. Most thoracic injuries were caused by fall from horse (78.9%) [7]. Dick et al. [36] found that there was an associated flail segment in 16% of patients with a rib fracture. Of patients with a pneumothorax, 40% were complicated by a hemothorax and 8.33% by tension. Injury to the upper limbs (27%) occurred primarily to the shoulder, scapula, clavicle, and hand [7, 17]. For the lower limbs (20.3%), tibia and fibula fractures were most common [1, 35].
Head injuries accounted for about 22% of the injuries [19], with about half of these injuries being traumatic brain injuries (TBI) [1]. According to Jones et al. [7], nearly 14% of all TBIs had a serious or severe Abbreviated Injury Scale (AIS) [48] score of 3–4. TBI events by mechanism were as follows: fall from horse (79.5%), kicked (10.2%), and knocked (4.5%). When skull and jaw fractures were diagnosed, these were found to occur at the vault of the skull, base of the skull, mandible, orbit and zygoma, and maxilla and nose [36]. The commonest head injury sustained was concussion with complex head injuries represented by subarachnoid (2.5%) and subdural hematomas and temporal lobe contusion (0.62%) [36].
Puolakkainen et al. [37] in a study of craniofacial fractures (n = 39) reported that over 90% of the patients sustained a facial fracture. Furthermore, Singleton et al. [40] found that out of a total of 61 facial fractures (those that did and did not require operative treatment), 54 were treated operatively. Of them, 44 were managed with internal fixation, nine with closed reduction, and one with a combination of both. When dentoalveolar and soft-tissue lacerations were included, there were 83 injuries in total with the most common fractures being naso-orbitoethmoidal and orbital fractures. Of note was that over a quarter of injuries to the face (26.9%), resulting from kicks [7]. Kicks or crushing were also responsible for abdominal visceral injuries seen in around 14% of reported cases, often resulting in liver, splenic, kidney laceration, and/or pancreatic contusion [7, 16, 36].
With the pediatric population, head trauma (30%) was the most common injury, followed by injuries of the upper and lower extremities (28%). Other injuries included the face (23%), chest (13%), abdomen (8%), and spine (4%) [4, 35, 39, 45]. The higher rate of head trauma was put down to children having a greater head-to-body size ratio and thinner skull bones [49, 50]. Of note, Wolyncewicz et al. [45] found that unmounted children suffered more severe injuries than mounted children.
Injury patterns also vary with the type of horse activity. For example, in vaulting which is a combination of dancing and gymnastics on horseback [41], the most frequently injured body part was the lower extremity (45.6%), followed by the upper extremity (27.2%), torso (21.6%), and head (5.6%) and rather than fractures and dislocations, the most common injury types were contusions (46.3%) followed by ligament injuries (28.9%) [4]. In the horse racing industry, jockeys mostly experience bruises and abrasions followed by fractures and dislocations of the upper and lower limbs; however, fracture and concussion incidences were higher in amateur than professional jockeys [21, 38]. Whereas in grooms, when working unmounted, the most common injuries reported were bruises (23.47%), lower back pain (14.5%), muscle strain (13.5%), upper back/neck pain (8.7%), lacerations (5.97%), tendon/ligament damage (5.2%), and suspected concussion (5.1%) [15]. In horse activities such as rodeos, an equestrian may be bucked into the air and subsequently land with their perineum striking a rigid saddle horn with consequential lower genitourinary injuries particularly in those individuals who fractured their pelvis due to saddle horn injury [43].
Hospital admission, length of stay, and rehabilitation
Most individuals with horse trauma (85.7–87.3%) were treated in the Emergency Department (ED) and discharged with the rest admitted [1, 19]. Of patients admitted, reports of those requiring surgery varied between 29.1 [28] and 55.6% [29]. Examples of the various surgical procedures carried out in a pediatric population included closed reduction of limb fractures (28.5%), closed reductions requiring percutaneous stabilization (31.5%), open limb fractures requiring reduction and fixation (18.5%), and spinal fixations, craniotomies, facial repairs, laparotomy, wound explorations and sutures (13.9%) [35]. Other reports indicated that between 18 and 27% of patients required Intensive Care Unit (ICU) admission [18, 28, 30] and furthermore Buchanan et al. [18] reported that 276 (5%) of patients in their study had mechanical ventilation. Of note, Acton et al. [19] found that mounted injuries were 2.10 (95% CI, 1.59–2.77) times more likely to be admitted than unmounted. Older patients, < 60 years of age (RR, 2.41; 95% CI, 2.01–2.90), were more likely to be hospitalized than younger patients. Patients with a fracture (RR, 3.22; 95% CI, 2.89–3.60) or a concussion/closed head injury (RR, 2.00; 95% CI, 1.79–2.23) were more likely to be admitted than patients with other injuries. Patients injured from a horse bucking, rearing, or spooking were 1.55 (95% CI, 1.36–1.78) times more likely to be admitted than patients injured from other mechanisms [19].
Regarding length of stay (LOS) in hospital, most studies placed in the 3- to 4-day band (range 0–15) [14, 16, 17, 31, 35, 39, 40] with more severe injuries (ISS equal/greater than 4) requiring 8.56 (± 10.84, range 1–64) days [30]. Older patients had longer LOS although not recording any worse injuries, the explanation being perhaps the case of more cautious monitoring [33, 42].
Almost 50% of all cases required professional rehabilitation [13] with O'Connor et al. [17] reporting that 39.13% of jockeys self-rehabilitated and 8.70% completed no rehabilitation. Aref-Ali Gharooni et al. [30] administered the Glasgow Outcome Scale [51] to patients on discharge from a major trauma center in the UK with nearly 75% with no disability, 22.3% with moderate disability (i.e., minor deficits that do not affect function), 1.3% with severe disability, and 0.7% in a persistent vegetative state. Given the importance of mental health, one study [12] conducted a cross-sectional survey (N = 511) to evaluate concussion history, depression symptoms, resilience, and well-being in equestrian athletes. Almost a third of the sample had depression, and there were significant relationships between a history of concussion, depression, and a sense of low well-being.
Severity of injury
GCS
In studies that reported on the Glasgow Coma Scale (GCS) [52], around 88% of individuals presented with scores between 13 and 15 [16, 18, 30, 31, 44]. Furthermore, Mutore et al. [16] found severe neurological impairment classified as a GCS score of 3–8 on presentation was observed in 3.58% patients. Within the severe impairment group, head and neck injuries were the most likely cause. Puolakkainen et al. [37] found that patients with GCS score < 12 were more likely to have cranial fractures (p = 0.002).
ISS/SBP
Reports regarding Injury Severity Score (ISS) [46] have shown varying results and are most likely due to such factors as different mechanisms, cohorts, and types of riding. For example, the mean ISS ranges from 5 [7] to 11 (SD 6.4) [31], median 4 (IQR = 1) [7] to 12 (range 4–45) [30] with similar fluctuations for the pediatric studies [35, 39, 45]. Both Van Balen, Barten [28] and Gross, Hadar [39] reported on cases with an ISS greater than 15. Two studies noted systolic blood pressure (SBP) as a measure for hemodynamic shock [16, 18]. Approximately 95% of Emergency Department (ED) presentations (N = 23619) had a SBP of ≥ 90 mm Hg with 1.40% of patients meeting the threshold of an SBP < 90 mm Hg whereas Buchanan et al. [18] reported a mean (SD) SBP of 132 (22) in 5731 patients with 1.2% SBP < 90.
Mortality
Mortality rates are noted as between 0.6 and 1.0% [30, 36]. The most common critical injuries were traumatic brain injuries (74.83%), thoracic injuries (18.44%), abdominal injuries (5.31%), and 2.19% patients dying to extremity injuries [16]. Lethal head injuries often follow falls and kicks [26]. Higher ISS scores resulted in the more likelihood of death [16]. Meredith et al. [4] found that there was an increase of 5.1% in the odds of fatality for every year increase in age of the patient with Byard [26] noting an age range of 8–73 years (mean 47 years) and as with Meredith et al. [4] a male–female ratio of approximately 5:3. Helmets and other protective equipment such as vests, boots, and safety stirrups have been shown to decrease traumatic injury with many horse-riding associations promoting the use of such items [18].
Use and effects of protective equipment
Helmets and other protective equipment such as vests, boots, and safety stirrups have been shown to decrease traumatic injury with many horse-riding associations promoting the use of such items [13]. In relation to the use and effects of protective equipment, Samuels and Bettis [14] (n = 3911) reported the use of helmets as low (19.8% helmet worn; 80.2% no helmet worn) and showed that the use of helmets significantly reduced the incidence of a head injury (AIS > 2) among equestrians (p = 0.003). Similarly, an examination of head injuries in children (n = 505) [45] found that equestrians not wearing a helmet were 12 times more likely to sustain a major head injury (AIS 4–5) than those who were wearing a helmet (OR 11.6: 95% CI 3.8, 36.9). Stier and Tavassol [33] in a study of maxillofacial fractures (n = 71) found that helmets were worn by 67% of beginner equestrians, but only by 44% of advanced equestrians and 33% of professional equestrians despite most injuries occurring in the latter two groups. The findings of these recent studies are consistent with previous ones that the wearing of helmets is associated with a reduction in head injuries, but the rates of use remain low [26].
Discussion
The purpose of this review was to critically appraise and summarize reports on horse trauma and to examine the characteristics of injured equestrians, characteristics of trauma, and clinical outcomes since 2018. Previous reviews were before this time frame. Meredith et al. [8] examined equestrian accidents from 1973 to 2017, and Havlik [9] reviewed equestrian sport-related injuries (2007–2009) while Gates and Lin [11] examined head and spinal injuries specifically (2009–2019) and Zuckerman et al. [10] focused on functional and structural traumatic brain injury in equestrian sports which included studies from 1993 to 2013. Therefore, a comprehensive review of this topic is timely.
In relation to characteristics of injured equestrians, much of the injured population were females with some reports up to 90%, and most equestrians were teenagers to younger adults up to around 40 years of age. This is like that reported in previous reviews [8,9,10,11]. Therefore, the demographics of the population under study has not changed over this period and this result is put down to the fact that there continues to be a high participation rate of females in equestrian-related activities [2, 3]. As with others, recreational horse activities mostly involve females [9], whereas men get injured while working [11]. Interestingly, in high-level competitions, there is no difference in gender which may indicate that the levels of skill and experience of the equestrian and the training of the horse are risk factors for horse trauma and support the need for more comprehensive and standardized data collection regarding equestrian and horse characteristics and mechanism of injury [23, 41].
In regard to characteristics of horse trauma, little has changed over the decades with most common mechanism of injury while mounted being a fall from the horse whereas in unmounted situations it was a kick from the horse [8,9,10,11]. There is also a reasonable possibility that an equestrian will have a combined mechanism such as being trampled following a fall. As with the review by Havlik [9], we found the most frequently injured body regions were the thorax and upper extremities, followed by the head and then lower extremities. However, Meredith et al. [8] found a greater predominance of head injuries and particularly noted higher occurrences with pediatric populations which is also supported by Gross et al. [39] who examined characteristics of horse-related injuries in Israeli children (n = 53). These findings infer again that the level of skill and experience of the equestrian are potential risk factors for horse trauma. While difficult to quantify, it is postulated that awareness of the horse and the surroundings, which comes with knowledge and experience, may reduce the incidence of injury [13, 44]. It is not evident from this review whether a horse safety awareness program for equestrians would reduce the incidence of mounted and unmounted injury.
In line with the most common mechanism of fall which can occur from a height of 9 feet/2.7 m/18 hands and at times at speeds of 40 miles/64 km/h, the most frequently diagnosed injuries were skin and/or bone contusion, fractures, head and neck injury, and visceral organ injury which in general correspond to previous reviews but with the proviso that data collection and analysis remain inconsistent [9]. Horses also weigh up to 1200 pounds/545 kg and can deliver 1000 newtons of force from a single kick [9] making injuries, even if the individual is unmounted, significant and common to the face, lower extremity, and abdomen. Given the variable size, speed, height, training, and temperament of different breeds of horse and the obvious impact this can have on severity and pattern of injury, it is important to gather this information at the time of presentation to hospital. The less frequent injury to the perineum and lower genitourinary tract sustained due to saddle horn strike is an injury that can have significant effect on morbidity in terms of fertility, sexual function, and cosmesis and is something that has not been commented on in the literature. As some of the mishaps occur because of the unpredictable nature of this large animal, it does not matter if the environment is recreational or a workplace [14, 44]; it is recommended that protective equipment, such as helmets and protective vests, be used across the board to control the incidence and severity of injury [8, 10]. It has been established that the incidence of severe head injury is lower in groups that wear helmets [14, 31, 33].
Other reviews have not reported on severity of injuries [8, 9, 11] and although there were reports of serious injuries across our reviewed studies, the average patient with horse trauma was not severely injured with medians of ISS reported as 4 (IQR = 1) [7] to 12 (range 4–45) [30]. Additionally, Mutore et al. [16] recorded systolic blood pressure (SBP) as a measure for hemodynamic shock with 1.40% of individuals meeting its threshold of < 90 mm Hg. GCS scores in most studies were noted as between 13 and 15 but if head and neck injuries were involved these usually dropped below 12 [16, 37]. Given the potential for severe injury resulting in significant morbidity and mortality, horse trauma should not be underestimated and should be treated as seriously as other mechanisms such as fall from height, motor vehicle, or motorbike accident. Inclusion of vital signs and GCS should be a part of a standardized horse trauma protocol.
Considering the data in relation to severity of injury, it is no surprise that well over 80% of individuals are treated in the ED and then released [19]. However, if admission is required, surgery for fractures and organ damage may be part of the course, through to ICU admission. Length of stays, and if required, rehabilitation, varies according to the injury with the resultant health system costs and if the case, cost for workplaces, and insurance companies. The rate of hospitalization has not changed, and this should be the driver for more injury prevention strategies to be put in place. Most of the research concentrated on physical injuries but mental health concerns particularly depression following concussion need greater attention for equestrians particularly in relation to getting treatment and being involved in health promotion programs [12]. Fortunately, death continues to occur at minimal rate with Meredith et al. [8] citing it as 0.17 per 100,000 people in a 1993 New Zealand study.
Since there has been little change in how data is collected for horse trauma over the last few decades, we would recommend a standardized approach for data collection with the intention of prospective design to ensure complete data collection, for example, to include if the equestrian was using protective equipment, the level of experience of the equestrian, environmental conditions, and importantly the characteristics of the horse [53]. More work could also take place on the long-term effects of horse trauma, for example, head injury given the recent focus of other sports on chronic traumatic encephalopathy or fertility given the seriousness of lower genitourinary tract injury sustained from saddle horn injury.
Conclusion
Horse trauma remains an ongoing presentation for health services. Since 2018, little has changed in relation to outcomes except for a continued decline in head injuries due to the use of protective equipment. A high risk of significant injury remains so there is a continuing need for more work to be done in this space. This review demonstrated that this is a global issue and there is potential to standardize data collection across these jurisdictions and work with the different types of horse-related industries at the recreational and occupational level to achieve better outcomes for equestrians and health services.
References
Asa N, Newton A, Sullivan L, Shi J, Wheeler K, Smith GA, et al. Horseback riding-related injuries treated in emergency departments: risk factors and prevention strategies. J Safety Res. 2019;71:251–7. https://doi.org/10.1016/j.jsr.2019.09.004.
British Equestrian. British Equestrian Annual Report 2022. Britian: British Equestrian; 2022.
Australian Sports Commission. Ausplay: Equestrian Report. Canberra: Clearinghouse for Sport; 2023.
Meredith L, Thomson R, Ekman R, Kovaceva J, Ekbrand H, Bálint A. Equestrian-related injuries, predictors of fatalities, and the impact on the public health system in Sweden. Public Health. 2019;168:67–75. https://doi.org/10.1016/j.puhe.2018.11.023.
Flunker JC, Clouser JM, Swanberg JE. Analysis of Thoroughbred horse farm workers’ compensation insurance claims in Kentucky: injury frequency, cost, lost time, and associated occupational factors. Am J Ind Med. 2020;63(10):936–48. https://doi.org/10.1002/ajim.23159.
Adler CR, Hopp A, Hrelic D, Patrie JT, Fox MG. Retrospective analysis of equestrian-related injuries presenting to a level 1 trauma center. Emerg Radiol. 2019;26(6):639–45. https://doi.org/10.1007/s10140-019-01718-8.
Jones AR, Smith A, Christey G. Equine-related injuries requiring hospitalisation in the Midland Region of New Zealand: a continuous five-year review. NZMJ. 2018;131(1483):50–8 (http://www.nzma.org.nz/journal/read-the-journal/all-issues/2010-2019/2018/vol-131-no-14835-october-2018/7711).
Meredith L, Ekman R, Brolin K. Epidemiology of equestrian accidents: a literature review. Internet J Allied Health Sci Pract. 2019;17(1):1–15 (https://nsuworks.nova.edu/ijahsp/vol17/iss1/9).
Havlik HS. Equestrian sport-related injuries: a review of current literature. Curr Sports Med Rep. 2010;9(5):299–302. https://doi.org/10.1249/JSR.0b013e3181f32056.
Zuckerman SL, Morgan CD, Burks S, Forbes JA, Chambless LB, Solomon GS, et al. Functional and structural traumatic brain injury in equestrian sports: a review of the literature. World Neurosurg. 2015;83(6):1098–113. https://doi.org/10.1016/j.wneu.2014.12.030.
Gates JK, Lin CY. Head and spinal injuries in equestrian sports: update on epidemiology, clinical outcomes, and injury prevention. Curr Sports Med Rep. 2020;19(1):17–23. https://doi.org/10.1249/JSR.0000000000000674.
McGivern A, Shannon S, Breslin G. Resilience, well-being, depression symptoms and concussion levels in equestrian athletes. J Public Mental Health. 2021;20(3):172–81. https://doi.org/10.1108/JPMH-08-2020-0110.
Pinto LV, Gouveia FC, Ramalho JF, Silva SR, Silva JR. Horseback riding-related injuries in portugal and prevention strategies. J Sport Rehab. 2023;32(4):409–14. https://doi.org/10.1123/jsr.2022-0101.
Samuels K, Bettis A, Davenport DL, Bernard AC. Occupational vs. non-occupational equestrians: differences in demographics and injury patterns. Injury. 2022;53(1):171–5. https://doi.org/10.1016/j.injury.2021.10.033.
Davies E, McConn-Palfreyman W, Parker JK, Cameron LJ, Williams JM. Is injury an occupational hazard for horseracing staff? Int J Environ Res Public Health. 2022;19(4):2054. https://doi.org/10.3390/ijerph19042054.
Mutore K, Lim J, Fofana D, Torres-Reveron A, Skubic JJ. Hearing hoofbeats? Think head and neck trauma: a 10-year NTDB analysis of equestrian-related trauma in the USA. Trauma Surg Acute Care Open. 2021;6(1): e000728. https://doi.org/10.1136/tsaco-2021-000728.
O’Connor S, Warrington G, O’Brien S, McDermott E, McGoldrick A, Pugh J, et al. Injuries outside of horseracing: is it time to focus on injury prevention of jockeys outside of races? Phys Sportsmed. 2021;49(1):45–50. https://doi.org/10.1080/00913847.2020.1760693.
Buchanan FR, Cardenas TC, Leede E, Riley CJ, Brown LH, Teixeira PG, et al. A national trauma data bank analysis of large animal-related injuries. Injury. 2021;52(9):2677–81. https://doi.org/10.1016/j.injury.2021.03.020.
Acton AS, Gaw CE, Chounthirath T, Smith GA. Nonfatal horse-related injuries treated in emergency departments in the United States, 1990–2017. Am J Emerg Med. 2020;38(6):1062–8. https://doi.org/10.1016/j.ajem.2019.158366.
Amey J, Christey G. Farm injury resulting in hospital admission: a review of farm work and non-farm work-related injury. J Prim Health Care. 2019;11(4):342. https://doi.org/10.1071/hc19049.
O’Connor S, Warrington G, McGoldrick A, Cullen S. A 9-year epidemiologic study (2007–2015) on race-day jockey fall and injury incidence in amateur Irish horse racing. J Athl Train. 2018;53(10):950–5. https://doi.org/10.4085/1062-6050-339-17.
Stanbouly D, Besmer AV, Chuang SK. Exploring the severity of craniomaxillofacial injuries from horseback riding. J Craniofac Surg. 2022;33(1):62–5. https://doi.org/10.1097/scs.0000000000008004.
Haines C, Jensen HK, Karim SA, McGhee L. Analysis of injuries in competitive equestrian events. Clin J Sport Med. 2022;32(5):e508–12. https://doi.org/10.1097/JSM.0000000000001004.
Bastard C, Le Hanneur M, Pannier S, Fitoussi F. Radial neck fractures in children secondary to horse-riding accidents: a comparative study. Orthop Traumatol Surg Res. 2020;106(7):1293–7. https://doi.org/10.1016/j.otsr.2020.04.021.
Pilato ML, Zaihra T, Henry T. Concussion in the collegiate equestrian athlete. Sport J. 2020: http://ezproxy.usq.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=cul&AN=141698082&site=ehost-live. Accessed 10 July 2023.
Byard RW. Lethal recreational activities involving horses – a forensic study. Leg Med. 2020;46: 101728. https://doi.org/10.1016/j.legalmed.2020.101728.
Pinidiyapathirage J, Kitchener S, McNamee S, Wynter S, Langford J, Doyle A, et al. Analysis of agriculture-related life-threatening injuries presenting to emergency departments of rural generalist hospitals in Southern Queensland. Emerg Med Australas. 2019;31(4):587–92. https://doi.org/10.1111/1742-6723.13215.
Van Balen PJ, Barten DG, Janssen L, Fiddelers AAA, Brink PR, Janzing HMJ. Beware of the force of the horse: mechanisms and severity of equestrian-related injuries. Eur J Emerg Med. 2019;26(2):133–8. https://doi.org/10.1097/mej.0000000000000511.
Hoffmann MF, Bernstorff M, Kreitz N, Roetman B, Schildhauer TA, Wenning KE. Horse-related injury patterns: a single center report. J Orthop Surg Res. 2023;18(1). https://doi.org/10.1186/s13018-023-03549-3.
Gharooni Aref-Ali, Anwar Fahim, Ramdeep Romann, Mee H. Severe equestrian injuries: a seven-year review of admissions to a UK major trauma centre. Trauma. 2023;25(1):41–7. https://doi.org/10.1177/14604086211041271.
Bhade P, Parsons A, Smiley A, Shreffler J, Nash N, Baker J, et al. Fall, crush, kick: mechanisms and outcomes in a cohort of equine-related injuries. Am Surg. 2023;89(4):875–80. https://doi.org/10.1177/00031348211048836.
Savage G, Liesegang A, Campbell J, Lyon M, Fry D. Horse and cattle-related trauma: a retrospective review of injuries and management in a Regional Queensland Hospital. Cureus. 2023. https://doi.org/10.7759/cureus.35746.
Stier R, Tavassol F, Dupke C, Rüter M, Jehn P, Gellrich N-C, et al. Retrospective analysis of 15 years of horse-related maxillofacial fracture data at a major German trauma center. Eur J Trauma Emerg Surg. 2022;48(4):2539–46. https://doi.org/10.1007/s00068-020-01450-w.
Francis AO, McCabe F, McCabe P, O’Daly BJ, Leonard M. Pelvic and acetabular trauma in amateur equestrian enthusiasts - a retrospective review. Surg. 2022;20(3):164–8. https://doi.org/10.1016/j.surge.2021.04.001.
Naef S, Steiger CN, Tabard-Fougère A, Dayer R, Ceroni D. Epidemiological study of equestrian trauma in Geneva. J Pediatric Orthop. 2022;42(2):e126–31. https://doi.org/10.1097/BPO.0000000000002025.
Dick L, Yule M, Green J, Young J. Patterns of injury following equine trauma: a non-trauma centre experience. Scott Med J. 2021;66(2):73–6. https://doi.org/10.1177/0036933021994264.
Puolakkainen T, Marttila E, Thorén H, Snäll J. Craniofacial fractures in equine-related injuries: what should a maxillofacial surgeon expect? J Craniofac Surg. 2021;32(4):1409–12. https://doi.org/10.1097/scs.0000000000007545.
Fortina M, Maniscalco P, Carulli C, Meccariello L, Colasanti GB, Carta S. Jockey injuries during the Siena “Palio”. A 72-year analysis of the oldest horse race in Italy. Injury. 2019;50:S56–9. https://doi.org/10.1016/j.injury.2019.03.015.
Gross I, Hadar A, Bala M, Hashavya S. The epidemiology, injury patterns and outcomes of horse-related injuries in Israeli children. Isr Med Assoc J. 2019;21(4):279–82.
Singleton C, Manchella S, Nastri A. Operative management of equine-related maxillofacial trauma presenting to a Melbourne level-one trauma centre over a six-year period. Br J Oral Maxillofac Surg. 2019;57(10):1126–30. https://doi.org/10.1016/j.bjoms.2019.10.301.
Zarghooni K, Hub L, Bredow J, Yagdiran A, Hackenberg RK, Scheyerer M, et al. Injuries in equestrian vaulting: results of a prospective study. J Sports Med Phys Fitness. 2019;59(3):476–80. https://doi.org/10.23736/S0022-4707.18.08250-6.
Serio F, Fujii Q, Shah K, Andrew McCague A. Horsing around: a retrospective review of horse-related trauma. J Emerg, Trauma, & Shock. 2019;12(1):69 (http://journals.lww.com/onlinejets).
Service CA, Moses RA, Majercik SD, Hotaling JM, Keihani S, Rothberg D, et al. Urethral trauma following pelvic fracture from horseback saddle horn injury versus other mechanisms of pelvic trauma. Urology. 2019;124:260–3. https://doi.org/10.1016/j.urology.2018.11.003.
Abdulkarim A, Juhdi A, Coffey P, Edelson L. Equestrian injury presentations to a regional trauma centre in Ireland. Emerg Med Int. 2018: 1–5. https://doi.org/10.1155/2018/7394390.
Wolyncewicz GEL, Palmer CS, Jowett HE, Hutson JM, King SK, Teague WJ. Horse-related injuries in children - unmounted injuries are more severe: a retrospective review. Injury. 2018;49(5):933–8. https://doi.org/10.1016/j.injury.2017.12.003.
Baker SP, O’Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–96.
Peachey KL, Lower T, Rolfe M. Protecting the future: fatal incidents on Australian farms involving children (2001–2019). Aust J Rural Health. 2020;28(4):385–93. https://doi.org/10.1111/ajr.12650.
Gennarelli TA, Wodzin E. Abbreviated Injury Scale 2005-update 2008. Des Plaines: Association for the Advancement of Automotive Medicine; 2008.
Gross I, Weiss DJ, Eliasi E, Bala M, Hashavya S. E-Bike-related trauma in children and adults. J Emerg Med. 2018;54(6):793–8. https://doi.org/10.1016/j.jemermed.2017.12.012.
Kannan N, Ramaiah R, Vavilala MS. Pediatric neurotrauma. Int J Crit Illn Inj Sci. 2014;4(2):131–7. https://doi.org/10.4103/2229-5151.134152.
Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1(7905):480–4. https://doi.org/10.1016/s0140-6736(75)92830-5.
Teasdale G, Jennett B. Assessment of coma and impaired consciousness, a practical scale. Lancet. 1974;2(7872):81–4. https://doi.org/10.1016/s0140-6736(74)91639-0.
Kaim A, Bodas M, Bieler D, Radomislensky I, Matthes G, Givon A, et al. Severe trauma in Germany and Israel: are we speaking the same language? A trauma registry comparison. Front Public Health. 2023;11:1136159. https://doi.org/10.3389/fpubh.2023.1136159.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. There are no funding, or financial or non-financial interests, and approval by an ethics committee was not required for a literature review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Neville, E.K., Hicks, H. & Neville, C.C. Epidemiology of horse trauma: a literature review. Eur J Trauma Emerg Surg 50, 741–754 (2024). https://doi.org/10.1007/s00068-023-02436-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-023-02436-0