Abstract
Background
Physiological patterns of coronary artery disease (CAD) have emerged as potential determinants of functional results of percutaneous coronary interventions (PCI) and of vessel-oriented clinical outcomes (VOCE).
Objectives
In this study, we evaluated the impact of angiography-derived physiological patterns of CAD on post-PCI functional results and long-term clinical outcomes.
Methods
Pre-PCI angiography-derived fractional flow reserve (FFR) virtual pullbacks were quantitatively interpreted and used to determine the physiological patterns of CAD. Suboptimal post-PCI physiology was defined as an angiography-derived FFR value ≤ 0.91. The primary endpoint was the occurrence of VOCE at the longest available follow-up.
Results
Six hundred fifteen lesions from 516 patients were stratified into predominantly focal (n = 322, 52.3%) and predominantly diffuse (n = 293, 47.7%). Diffuse pattern of CAD was associated with lower post-PCI angiography-derived FFR values (0.91 ± 0.05 vs. 0.94 ± 0.05; p = 0.001) and larger rate of suboptimal post-PCI physiology (43.0 vs. 22.7%; p = 0.001), as compared to focal CAD. At the median follow-up time of 37 months (33–58), post-PCI suboptimal physiology was related to a higher risk of VOCE (16.2% vs. 7.6%; HR: 2.311; 95% CI 1.410–3.794; p = 0.0009), while no significant difference was noted according to baseline physiological pattern. In diffuse disease, the use of intracoronary imaging was associated with a lower incidence of long-term VOCE (5.1% vs 14.8%; HR: 0.313, 95% CI 0.167–0.614, p = 0.030).
Conclusions
Suboptimal post-PCI physiology is observed more often in diffusely diseased arteries and it is associated with higher risk of VOCE at follow-up. The use of intravascular imaging might improve clinical outcomes in the setting of diffuse CAD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Post-PCI suboptimal physiology is associated with reduced quality-of-life improvement and worse clinical outcomes. Despite being very common, it is seldom investigated and poorly recognized [3,4,5]. Physiological patterns of CAD (i.e., focal, diffuse, mixed, and serial) have recently been shown to potentially impact on PCI outcomes. Pressure wire (PW)-pullback has the potential to qualitatively interpret the physiological pattern of CAD. However, this method lacks of standardization and reproducibility, especially when dealing with ambiguous lesions, on top of requiring a dedicated pressure-wire. To overcome such limitations, the pullback pressure gradient index (PPGi) and the instantaneous fractional flow reserve (FFR) gradient per unit time (dFFR[t]/dt) have been introduced, both calculated based on PW-pullback performed during continuous hyperaemia. PPGi is a continuous metric that serves as a quantitative measure of the physiological distribution of coronary plaques along the vessel and is capable of distinguishing between focal and diffuse disease, while dFFR[t]/dt reflects the local physiological disease severity [6,7,8,9,10].
Despite the extensive evidence in support of physiological assessment as a gate-keeper for coronary revascularization, and the growing one in support of physiology guidance for PCI optimization, its use remains hampered by economic and logistic reasons (i.e., need for a PW and for hyperaemic agents, increased costs and procedural time). To overcome such limitations, angiography-derived physiological indices, such as the quantitative flow ratio (QFR), have been recently developed and validated [11,12,13,14]. However, the prognostic value of the functional angiography-based longitudinal analysis, including the QFR-based virtual pullback index (QVPi) and the dQFR/ds, is not fully understood [15, 16].
Therefore, this study aimed at defining the interaction of pre-PCI physiological pattern of CAD, defined according to the QVPi, and local disease severity, defined according to the dQFR/ds, with post-PCI physiological result. Moreover, we sought to assess the association between functional angiography-derived metrics and the incidence of VOCE at long-term follow-up.
Methods
Study population
This is a patient-level pooled analysis of four prospective cohorts of patients with de-novo CAD that underwent clinically indicated PCI, enrolled in three European centers (Verona University Hospital, Verona, Italy [185 CESC]; Policlinico Gemelli, Rome, Italy [PROPHET-FFR NCT05056662 and FORZA NCT01824030]; Hippokration Hospital, Athens) between December 2012 and September 2020. Coronary angiograms were anonymized, transferred, and analyzed in two independent laboratories (University of Verona, Italy; The Lambe Institute of Translational Research, University of Galway, Ireland) in a blinded fashion, by experienced and certified analyzers.
Patients younger than 18 years old, with known contraindication to dual anti-platelet therapy, a concomitant indication to open-heart surgery, presenting with resuscitated cardiac arrest and women with childbearing potential were excluded from the study. Furthermore, patients with unavailable pre-PCI and post-PCI coronary angiograms and those with angiographic features limiting either pre-PCI or post-PCI angiography-derived FFR computation (ostial left main or ostial right coronary artery, ongoing ventricular arrhythmias or significant and persistent tachycardia, poor angiography image quality, and severe tortuosity) were excluded from the analysis.
The study was conducted in accordance with the ethical principles of the Declaration of Helsinki, and it was approved by the institutional ethical board of each referring hospital. All the patients had provided their written consent for the anonymous data collection.
Percutaneous coronary intervention
Invasive coronary angiography and PCI were performed according to the best local practice and to standardized technical recommendations. Particularly, intracoronary nitrates (100–300 mcg) were administered in all cases. Standard radial or femoral access with 5 or 6F catheters were used. Intravascular imaging pre- and post-PCI, such as intravascular ultrasound (IVUS) and optical coherence tomography (OCT), was left to operator discretion. Patients enrolled in the FORZA trial were randomly assigned to either FFR- or OCT-guidance during PCI.
All the patients received dual anti-platelet therapy based on aspirin combined with either clopidogrel, ticagrelor, or prasugrel for at least 12 months in case of acute coronary syndrome or 6 months in case of chronic coronary syndrome, according to the international recommendations. In patients requiring anticoagulation, a direct oral anticoagulant combined with aspirin and clopidogrel for 7–28 days and clopidogrel for 12 months was recommended.
Quantitative flow ratio and Murray law-based quantitative flow ratio analysis
Quantitative coronary angiography was performed and minimum lumen diameter, reference vessel size, percent diameter stenosis, and lesion length were measured. Estimation of angiography-derived FFR was based on single-view Murray law-based quantitative flow ratio analysis (μFR) and on 3D quantitative flow ratio (QFR). Computational analysis of μFR was performed with the AngioPlus Core, version V3 software (Pulse Medical, Shanghai, China), while of 3D-QFR with the Medis Medical Imaging Systems software (Leiden, The Netherlands), respectively. Analyzers were blinded to any clinical data. Methodologies for 2D-μFR and 3D-QFR were adopted as previously reported [12, 17] and are reported in the Supplementary material. Post-PCI assessment was performed on the angiographic projection acquired at the end of the procedure. Conventional validated cut-off values for ischemia pre-PCI (QFR ≤ 0.80 and μFR ≤ 0.80) and suboptimal physiology post-PCI (QFR ≤ 0.91 and μFR ≤ 0.91) were adopted [18, 19].
Physiological pattern characterization
Physiological patterns of CAD were classified, based on QFR or μFR virtual pullback trace. More specifically, physiological distribution was assessed through the QFR-virtual pullback pressure gradient index (QVPi) which discriminates predominantly focal from predominantly diffuse disease, providing a continuous metric based on the magnitude of maximum pressure drop over 20 mm and on the extent of functional disease over the entire interrogated vessel.
QVPi was calculated as follows:
As previously reported, high QVPi values (close to 1) suggest predominantly focal disease, whereas low values (close to 0) predominantly diffuse disease. The median QVPi value (0.68) was used to dichotomize CAD into focal (QVPi ≥ 0.68) and diffuse (QVPi < 0.68) disease [17].
Next, the local physiological severity was calculated by the instantaneous QFR gradient per unit length (dQFR/ds), using a cut-off value of 0.025/mm to identify the presence (≥ 0.025/mm) or the absence (< 0.025/mm) of major gradients, as previously validated [17].
Follow-up and outcomes
The occurrence of any procedural-related clinical complication was prospectively evaluated. After discharge, follow-up was prospectively conducted during outpatients’ clinic visits or with telephonic interviews and clinical controls and confirmed with medical records’ consultation. Clinical endpoints were assessed at the longest follow-up available.
The target vessel was defined as the entire major coronary vessel proximal and distal to the target lesion, including upstream and downstream branches and the target lesion itself. All clinical outcomes were defined according to the Academic Research Consortium [20]. Vessel-oriented composite endpoint (VOCE) was defined as a composite of cardiac death, target vessel-related myocardial infarction, clinically driven target vessel revascularization (TVR). All deaths were considered cardiac unless an undisputed non-cardiac cause could be demonstrated.
Statistical analysis
Continuous variables are presented as mean and standard deviation if normally distributed and compared with unpaired t test. Categorical data are reported as a percentage and compared with the χ2 test or Fisher exact test as appropriate. Correlation coefficients were calculated to assess the relationships of QVPi and dQFR/ds with post-PCI angiography-derived FFR and percentage of angiography-derived FFR increase (Pearson or Spearman according to normality). Mean values and percentage increase of post-PCI angiography-derived FFR were compared between predominant focal and diffuse disease groups, as well as major gradient and no major gradient groups using Student’s t tests. Logistic regression was performed to assess predictors of suboptimal functional PCI results. Survival analysis was performed using Kaplan–Meier methods and groups were compared with log-rank test. Cox regression analysis was performed to assess significant predictors of VOCE. Hazard ratio with 95% confidence interval were provided. Shared frailty Cox regression multivariable analysis, with patient identification introduced in a multilevel model, was performed to take into account the nonindependence of lesions. All analyses were performed with IBM® SPSS® Statistics (Version 26, SPSS Inc., Chicago, IL). Graphics were realized with GraphPad Prism 7.0.
Results
Baseline characteristics
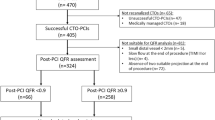
Overall, 615 coronary vessels (n = 516 patients) underwent PCI with implantation of at least one drug eluting stent (DES; n = 427) or a bio-resorbable scaffold (BRS; n = 188) and were included in this analysis (Supplementary Fig. 1). The mean age was 65.2 ± 12.6 years, and the majority of the patients were males (416 patients; 67.7%) and presented with chronic coronary syndromes (441 patients; 71.7%). Multivessel CAD was present in 282 patients (45.9%).
Complete baseline characteristics of all patients are displayed in Table 1.
Lesion and procedural characteristic
The average QVPi value was 0.69 ± 0.12 and the physiological pattern was interpreted as predominantly diffuse in 293 vessels (47.7%). The average dQFR/ds value was 0.04 ± 0.04 and a major gradient was detected in 351 vessels (57.1%).
Diffuse CAD pattern was more likely to be observed in the left anterior descending artery (54.9 vs. 39.4%; p = 0.013). Diffuse CAD had on average longer lesion length (26.32 ± 10.39 vs. 22.65 ± 9.24 mm; p = 0.001) and were more frequently either moderately or severely calcified, according to the angiographic evaluation (19.4 vs. 9.4%; p = 0.003) compared with focal CAD. Consistently, pre-dilatation was performed more frequently in the group with diffuse CAD (97.9 vs. 86.9%; p = 0.042). Intravascular imaging was used more frequently in case of diffuse disease compared to focal CAD (26.6 vs. 20.5%; p = 0.047). Vessels with diffuse pattern showed a higher MLD (1.34 ± 0.41 vs. 1.19 ± 0.33 mm; p = 0.001) and lower DS (49.8 ± 11.2 vs. 55.2 ± 11.0%; p = 0.001). Vessels presenting a focal pattern showed a higher rate of major gradients (70.4 vs. 42.7%; p = 0.001).
Overall, the length of implanted stents/scaffold was significantly higher in patients with predominantly diffuse disease (34.21 ± 17.74 vs. 20.76 ± 5.83 mm; p < 0.001).
Complete procedural characteristics are displayed in Table 1.
Quantitative flow ratio assessment
Pre-PCI mean angiography-derived FFR was 0.73 ± 0.12 with 430 vessels (69.9%) deemed as flow-limiting. Post-PCI mean angiography-derived FFR was 0.94 ± 0.04, with 199 vessels (32.4%) deemed as having suboptimal post-PCI physiology.
Pre-PCI QVPi showed a modest but significant correlation with post-PCI angiography-derived FFR (R = 0.272; p < 0.001), and weak correlation with the %FFR increase (R = 0.117; p = 0.004), while pre-PCI dQFR/ds showed no correlation with post-PCI angiography-derived FFR (R = 0.086; p = 0.033), and strong correlation with the %FFR increase (R = 0.680; p = 0.001), as displayed in Fig. 1.
A Correlation between pre-PCI QVPi and post-PCI angiography-derived FFR (left) and between pre-PCI dQFR/ds and post-PCI angiography-derived FFR (right). B Correlation between pre-PCI QVPi and % μFR/QFR increase after PCI (left) and between pre-PCI dQFR/ds and % μFR/QFR increase after PCI (right). PCI percutaneous coronary intervention; μFR Murray law quantitative flow ratio; QFR quantitative flow ratio; dQFR/ds instantaneous QFR gradient per unit length; QVPi virtual pullback pressure gradient index
Importantly, at completion of PCI, diffuse CAD showed worse post-PCI angiography-derived FFR values (0.91 ± 0.05 vs. 0.94 ± 0.05; p = 0.001) and percentage increase (28.7 ± 28.2 vs. 36.5 ± 44.0; p = 0.010) compared to focal with a higher rate of suboptimal physiological result (43.0 vs. 22.7%, p = 0.001), as shown in Fig. 2. Pre-PCI QVPi was inversely associated with the incidence of post-PCI angiography-derived FFR ≤ 0.91 (for 0.10 QVPi increase: OR 0.666; 95% CI 0.576–0.771; p = 0.001; supplementary Fig. 2). Angiography-derived FFR analysis data are reported in Table 2.
A Post-PCI μFR/QFR (left) and % μFR/QFR increase after PCI (right) according to physiological pattern of disease. B Post-PCI μFR/QFR (left) and % μFR/QFR increase after PCI (right) according to the presence of major drops at the dQFR/ds. PCI percutaneous coronary intervention; μFR Murray law quantitative flow ratio; QFR quantitative flow ratio; dQFR/ds instantaneous QFR gradient per unit length; QVPi virtual pullback pressure gradient index
Intravascular imaging-guided PCI
Intravascular imaging was performed in 144 vessels (23.4%): 66 were classified as focal and 78 as diffuse (p = 0.047). IVUS was used in 49 (34.0%) vessels (20 focal vs. 29 diffuse; 40.8% vs. 49.2%, respectively; p = 0.127) and OCT in the remaining 97 (66.0%) vessels (41 focal vs. 56 diffuse; 42.3% vs. 57.7% respectively; p = 0.031). Clinical and procedural characteristics of vessel treated with intravascular imaging use are displayed in Supplementary Table 1.
No significant differences were noted in terms of post-PCI angiography-derived FFR values according to use of intravascular imaging both in diffuse and focal lesions. Pre-PCI QVPi showed a significant correlation with post-PCI angiography-derived FFR, regardless of the use of intravascular imaging (imaging: R = 0.196; p = 0.001; non-imaging: R = 0.341; p < 0.001), as displayed in Supplementary Fig. 3.
Long-term outcomes
At the median follow-up time of 37 months (35–60) VOCE occurred in 77 (12.7%) vessels, mainly driven by TVR (n = 66, 10.9%). Notably, patients with post-PCI suboptimal physiological result demonstrated a significantly higher risk of VOCE compared with patients with optimal physiological result in the shared frailty Cox regression model (16.2 vs. 7.6%; HR:2.311; 95% CI: 1.410–3.794; p = 0.0009), as displayed in Fig. 3A. Conversely, no significant difference in terms of VOCE incidence was reported according to the disease pattern (focal 8.8% vs. diffuse 12.2% HR: 1.54; 95% CI 0.939–2.547; p = 0.087; Fig. 3B1. Patients with predominantly diffuse disease who underwent intravascular imaging-guided PCI experienced a significantly lower incidence of VOCE at long term compared with patients without intravascular imaging (5.1% vs 15.8%; HR: 0.313, 95% CI 0.167–0.614, p = 0.030; Fig. 3B2. Long-term outcomes according to disease pattern and immediate post-PCI functional results are displayed in Table 3. Kaplan–Meier curves are displayed in Fig. 3.
A Kaplan–Meier survival curves for 4 years VOCE according to sub-optimal post-PCI functional results (μFR/QFR ≤ 0.91). B1 Kaplan–Meier survival curves for 4 years VOCE according to the physiological pattern of CAD. B2 Kaplan–Meier survival curves for 4 years VOCE according to the physiological pattern of CAD stratified by the use of intravascular imaging. PCI percutaneous coronary intervention; μFR Murray law quantitative flow ratio; QFR quantitative flow ratio; VOCE vessel-oriented composite endpoint
Presence of major gradients (dQFR/ds ≥ 0.025/mm) was shown to have no impact on VOCE incidence at long term (7.9% vs. 12.1%; HR: 1.501; 95% CI: 0.879–2.562; p = 0.157) regardless from the use of intravascular imaging.
The type of prosthesis implanted (either BRS or DES) had no significant impact on both immediate post-PCI suboptimal physiology (10.8% vs. 10.2%; p = 0.885) and long-term VOCE occurrence (30.1% vs. 33.6% p = 0.452). Kaplan–Meier analysis for implanted stent and disease pattern are shown in Supplementary Fig. 4.
Discussion
In this large, multicenter, international cohort of patients with CAD undergoing PCI, we observed that the physiological pattern of disease, defined by functional angiography-derived quantitative measures, was associated with the functional outcome of the intervention. In particular, patients with predominantly diffuse disease showed a significantly worse post-PCI angiography-derived FFR and percentage of FFR increase compared with patients with predominantly focal disease.
Moreover, suboptimal post-PCI physiology was associated with worse vessel-oriented clinical outcomes and diffuse disease showed a numerically but not significantly higher rate of adverse events. Notably, the use of intracoronary imaging mitigated the risk of VOCE in patients with diffuse coronary disease, yielding a significantly improved clinical outcome compared to interventions guided by angiography alone.
Longitudinal physiological vessel analysis is a powerful tool to enhance precision medicine in terms of accurate diagnosis, procedural planning, and tailored treatment. Diffuse longitudinal distribution of atherosclerosis may impair the effectiveness of PCI. Indeed, stenting is a segmental treatment which may produce suboptimal functional outcomes in case of long lesions.
Discrimination between focal and diffuse disease is based mostly on coronary angiography, which is, however, characterized by low accuracy [25]. μFR/QFR-virtual pullback curve can be derived from standard angiographic images without further instrumentation of the coronary artery allowing identification of the lesions responsible for pressure loss along the vessel and quantifying the functional gain achievable with PCI [27, 28]. Results from AQVA and AQVA-2 trials already confirmed superiority of QFR-based virtual PCI over angiography-based PCI with regard to post-PCI optimal physiological results [29, 30].
Shin et al. suggested angiography-derived physiological pattern of disease to be a major determinant of optimal PCI result. Moreover, diffuse coronary atherosclerosis showed a correlation with higher rate of target vessel failure at follow-up despite optimal functional post-PCI results [31]. A third study from Dai et al. confirmed the prognostic value of pre-PCI QFR-PPGi regardless the post-PCI results [32]. Of note, in a sub-analysis of the TARGET-FFR (Trial of Angiography vs. pressure-Ratio-Guided Enhancement Techniques-Fractional Flow Reserve) study, diffuse CAD defined based on PW-pullback PPGi was seen to be associated with a higher rate of residual angina after successful PCI, as compared to focal disease (51.9% vs. 27.5%; p = 0.020) [5]. Our findings confirmed the impact of baseline QVPi on immediate functional PCI results. However, pre-PCI QVPi was not significantly associated with the risk of VOCE. Beside the longer follow-up, a possible reason for this divergence compared with the previously available evidence may be related to use of intravascular imaging that was performed in roughly a quarter of cases in our cohort.
Indeed, upfront characterization of the vessel may predict the risk of unsuccessful intervention and the need for additional tools such as intracoronary imaging.
The potential advantage of intracoronary imaging-guided PCI in case long coronary lesions has been already supported in several studies. A meta-analysis involving seven randomized trials (3,192 participants) demonstrated the superiority of IVUS-guided PCI compared to angiography alone in cases of long lesions, leading to a reduction in the risk of intra-stent restenosis and TLR by 79% [21]. Similarly, findings from the IVUS-XPL (Impact of Intravascular Ultrasound Guidance on the Outcomes of Xience Prime Stents in Long Lesions) and ULTIMATE (Intravascular Ultrasound-Guided Drug-Eluting Stents Implantation in “All-Comers” Coronary Lesions) trial revealed a decreased risk of major adverse cardiovascular events (5.6 vs. 10.7%; HR: 0.50; 95% CI 0.34–0.75; p < 0.001) and target lesion failure (6.6 vs. 10.7%; p = 0.01), respectively, in patients with long coronary lesions who underwent IVUS—compared to angiography-guided PCI [22, 23]. Also, in the RENOVATE-COMPLEX PCI (Randomized Controlled Trial of Intravascular Imaging Guidance versus Angiography-Guidance on Clinical Outcomes after Complex Percutaneous Coronary Intervention) trial, angiography-defined diffuse disease (lesion length > 38 mm) acknowledged for the 54% of the cases included [24]. In this trial, the use of intracoronary imaging led to a reduction of MACE (7.7 vs. 12.3%; HR: 0.64; 95% CI 0.45 to 0.89; p = 0.008), as compared to angiography alone. To the best of our knowledge, our study is the first to investigate the role of intravascular imaging according to the specific endotype of physiological pattern of disease. Notably, the use of either IVUS or OCT to optimize PCI seems to be associated with a better functional result and improved clinical outcomes, especially in patients with predominantly diffuse disease.
Limitations
Our findings must be interpreted considering some limitations. First, this was a retrospective analysis of a multicenter international pooled cohort of patients. Moreover, the event adjudication was not performed by a dedicated independent event adjudication committee. Therefore, even though all the data collection was performed prospectively, reporting bias could not be excluded.
Second, variability in baseline clinical and procedural characteristics of the study sub-populations must be acknowledged. In particular, PCI was performed with BRS in a subgroup of patients enrolled in Verona. Furthermore, patients enrolled in the FORZA trial were randomized to OCT-guided vs FFR-guided PCI.
Third, cut-off values of the QVP index to define CAD patterns are not established and, in this study, we used the QVP median value to discriminate between predominantly focal vs predominantly diffuse pattern of disease. Moreover, it must be acknowledged that QVP index and dQFR/ds provide quantitative metrics to describe the pattern of disease and the local severity of CAD, but these indices do not inform on the presence of serial lesions or mixed patterns of disease.
Fourth, suboptimal angiographic quality may have impacted on the accuracy of angiography-derived coronary physiology measures. However, all the coronary imaging has been reviewed by expert QFR-certified operators blinded to the clinical data who have excluded low-quality angiograms.
In view of these limitations, our findings should be considered hypothesis-generating and they should be confirmed in a larger cohort of patients undergoing prospective assessment of the disease pattern.
Conclusions
Functional angiography-derived longitudinal vessel analysis is a major determinant of post-PCI functional result. Suboptimal post-PCI coronary physiology is observed more often in coronary arteries with diffuse disease (low QVP) and no major gradient (low dQFR/ds), and it is associated with higher risk of vessel-oriented adverse events at long-term follow-up. In patients with diffuse disease intracoronary imaging may lower the risk of adverse events reducing the risk of unscheduled target vessel revascularization.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP, Douglas PS, Foody JM, Gerber TC, Hinderliter AL, King SB 3rd, Kligfield PD, Krumholz HM, Kwong RY, Lim MJ, Linderbaum JA, Mack MJ, Munger MA, Prager RL, Sabik JF, Shaw LJ, Sikkema JD, Smith CR Jr, Smith SC Jr, Spertus JA, Williams SV, Anderson JL, American College of Cardiology Foundation/American Heart Association Task Force (2012) ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation 126:354–471
Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Jüni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferović PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO (2018) ESC/EACTS guidelines on myocardial revascularization. EuroIntervention 2019(14):1435–1534
Johnson NP, Tóth GG, Lai D, Zhu H, Açar G, Agostoni P, Appelman Y, Arslan F, Barbato E, Chen SL, Di Serafino L, Domínguez-Franco AJ, Dupouy P, Esen AM, Esen OB, Hamilos M, Iwasaki K, Jensen LO, Jiménez-Navarro MF, Katritsis DG, Kocaman SA, Koo BK, López-Palop R, Lorin JD, Miller LH, Muller O, Nam CW, Oud N, Puymirat E, Rieber J, Rioufol G, Rodés-Cabau J, Sedlis SP, Takeishi Y, Tonino PA, Van Belle E, Verna E, Werner GS, Fearon WF, Pijls NH, De Bruyne B, Gould KL (2014) Prognostic value of fractional flow reserve: linking physiologic severity to clinical outcomes. J Am Coll Cardiol 64:1641–1654
Rimac G, Fearon WF, De Bruyne B, Ikeno F, Matsuo H, Piroth Z, Costerousse O, Bertrand OF (2017) Clinical value of post-percutaneous coronary intervention fractional flow reserve value: a systematic review and meta-analysis. Am Heart J 183:1–9
Collet C, Collison D, Mizukami T, McCartney P, Sonck J, Ford T, Munhoz D, Berry C, De Bruyne B, Oldroyd K (2022) Differential Improvement in Angina and health-related quality of life after PCI in focal and diffuse coronary artery disease JACC. Cardiovasc Interv 15:2506–2518
Collet C, Sonck J, Vandeloo B, Mizukami T, Roosens B, Lochy S, Argacha JF, Schoors D, Colaiori I, Di Gioia G, Kodeboina M, Suzuki H, Van’t Veer M, Bartunek J, Barbato E, Cosyns B, De Bruyne B (2019) Measurement of hyperemic pullback pressure gradients to characterize patterns of coronary atherosclerosis. J Am Coll Cardiol 74:1772–1784
Mizukami T, Sonck J, Sakai K, Ko B, Maeng M, Otake H, Koo BK, Nagumo S, Nørgaard BL, Leipsic J, Shinke T, Munhoz D, Mileva N, Belmonte M, Ohashi H, Barbato E, Johnson NP, De Bruyne B, Collet C (2022) Procedural outcomes after percutaneous coronary interventions in focal and diffuse coronary artery disease. J Am Heart Assoc 11:e026960
Lee SH, Kim J, Lefieux A, Molony D, Shin D, Hwang D, Choi KH, Chang HS, Jeon KH, Lee HJ, Jang HJ, Kim HK, Ha SJ, Park TK, Yang JH, Song YB, Hahn JY, Choi SH, Doh JH, Shin ES, Nam CW, Koo BK, Gwon HC, Lee JM (2021) Clinical and prognostic impact from objective analysis of post-angioplasty fractional flow reserve pullback. JACC Cardiovasc Interv 14:1888–1900
Lee SH, Shin D, Lee JM, Lefieux A, Molony D, Choi KH, Hwang D, Lee HJ, Jang HJ, Kim HK, Ha SJ, Kwak JJ, Park TK, Yang JH, Song YB, Hahn JY, Doh JH, Shin ES, Nam CW, Koo BK, Choi SH, Gwon HC (2020) Automated algorithm using pre-intervention fractional flow reserve pullback curve to predict post-intervention physiological results. JACC Cardiovasc Interv 13:2670–2684
Fezzi S, Huang J, Lunardi M, Ding D, Ribichini FL, Tu S, Wijns W (2022) Coronary physiology in the catheterisation laboratory: an A to Z practical guide. AsiaIntervention 8:86–109
Xu B et al (2017) Diagnostic accuracy of angiography-based quantitative Flow†Ratio measurements for online Assessment†of coronary stenosis. J Am Coll Cardiol 70:3077–3087
Xu B, Tu S, Qiao S, Qu X, Chen Y, Yang J, Guo L, Sun Z, Li Z, Tian F, Fang W, Chen J, Li W, Guan C, Holm NR, Wijns W, Hu S (2016) Diagnostic accuracy of fast computational approaches to Derive†Fractional flow reserve from diagnostic coronary angiography: the international multicenter FAVOR pilot study. JACC Cardiovasc Interv 9:2024–2035
Fan Y, Fezzi S, Sun P, Ding N, Li X, Hu X, Wang S, Wijns W, Lu Z, Tu S (2022) In vivo validation of a novel computational approach to assess microcirculatory resistance based on a single angiographic view. J Pers Med 12:1798
Fezzi S, Ding D, Scarsini R, Huang J, Del Sole PA, Zhao Q, Pesarini G, Simpkin A, Wijns W, Ribichini F, Tu S (2023) Integrated assessment of computational coronary physiology from a single angiographic view in patients undergoing TAVI. Circ Cardiovasc Interv 16:e013185
Dai N, Hwang D, Lee JM, Zhang J, Jeon KH, Paeng JC, Cheon GJ, Koo BK, Ge J (2021) Feasibility of quantitative flow ratio-derived pullback pressure gradient index and its impact on diagnostic performance. JACC Cardiovasc Interv 14:353–355
Sonck J, Mizukami T, Johnson NP, Nagumo S, Gallinoro E, Candreva A, Mileva N, Munhoz D, Shinke T, Svanerud J, Barbato E, De Bruyne B, Collet C (2022) Development, validation, and reproducibility of the pullback pressure gradient (PPG) derived from manual fractional flow reserve pullbacks. Catheter Cardiovasc Interv 99:1518–1525
Westra J, Andersen BK, Campo G, Matsuo H, Koltowski L, Eftekhari A, Liu T, Di Serafino L, Di Girolamo D, Escaned J, Nef H, Naber C, Barbierato M, Tu S, Neghabat O, Madsen M, Tebaldi M, Tanigaki T, Kochman J, Somi S, Esposito G, Mercone G, Mejia-Renteria H, Ronco F, Bøtker HE, Wijns W, Christiansen EH, Holm NR (2018) Diagnostic performance of in-procedure angiography-derived quantitative flow reserve compared to pressure-derived fractional flow reserve: the FAVOR II Europe-Japan Study. J Am Heart Assoc 7:e009603
Kogame N, Takahashi K, Tomaniak M, Chichareon P, Modolo R, Chang CC, Komiyama H, Katagiri Y, Asano T, Stables R, Fath-Ordoubadi F, Walsh S, Sabaté M, Davies JE, Piek JJ, van Geuns RJ, Reiber JHC, Banning AP, Escaned J, Farooq V, Serruys PW, Onuma Y (2019) Clinical implication of quantitative flow ratio after percutaneous coronary intervention for 3-vessel disease. JACC Cardiovasc Interv 12:2064–2075
Koo BK, Lee JM, Hwang D, Park S, Shiono Y, Yonetsu T, Lee SH, Kawase Y, Ahn JM, Matsuo H, Shin ES, Hu X, Ding D, Fezzi S, Tu S, Low AF, Kubo T, Nam CW, Yong ASC, Harding SA, Xu B, Hur SH, Choo GH, Tan HC, Mullasari A, Hsieh IC, Kakuta T, Akasaka T, Wang J, Tahk SJ, Fearon WF, Escaned J, Park SJ (2023) Practical application of coronary physiologic assessment: Asia-Pacific expert consensus document: part 1. JACC Asia 3:689–706
Ybarra LF, Rinfret S, Brilakis ES, Karmpaliotis D, Azzalini L, Grantham JA, Kandzari DE, Mashayekhi K, Spratt JC, Wijeysundera HC, Ali ZA, Buller CE, Carlino M, Cohen DJ, Cutlip DE, De Martini T, Di Mario C, Farb A, Finn AV, Galassi AR, Gibson CM, Hanratty C, Hill JM, Jaffer FA, Krucoff MW, Lombardi WL, Maehara A, Magee PFA, Mehran R, Moses JW, Nicholson WJ, Onuma Y, Sianos G, Sumitsuji S, Tsuchikane E, Virmani R, Walsh SJ, Werner GS, Yamane M, Stone GW, Rinfret S, Stone GW (2021) Chronic total occlusion academic research consortium. Definitions and clinical trial design principles for coronary artery chronic total occlusion therapies: CTO-ARC consensus recommendations. Circulation 143:479–500
Elgendy IY, Mahmoud AN, Elgendy AY, Bavry AA (2016) Outcomes with intravascular ultrasound-guided stent implantation: a meta-analysis of randomized trials in the era of drug-eluting stents. Circ Cardiovasc Interv 9:e003700
Hong SJ, Mintz GS, Ahn CM, Kim JS, Kim BK, Ko YG, Kang TS, Kang WC, Kim YH, Hur SH, Hong BK, Choi D, Kwon H, Jang Y, Hong MK (2020) IVUS-XPL investigators effect of intravascular ultrasound-guided drug-eluting stent implantation: 5-year follow-up of the IVUS-XPL randomized trial. JACC Cardiovasc Interv 13:62–71
Gao XF, Ge Z, Kong XQ, Kan J, Han L, Lu S, Tian NL, Lin S, Lu QH, Wang XY, Li QH, Liu ZZ, Chen Y, Qian XS, Wang J, Chai DY, Chen CH, Pan T, Ye F, Zhang JJ, Chen SL (2021) ULTIMATE investigators. 3-year outcomes of the ULTIMATE trial comparing intravascular ultrasound versus angiography-guided drug-eluting stent implantation. JACC Cardiovasc Interv 14:247–257
Lee JM, Choi KH, Song YB, Lee JY, Lee SJ, Lee SY, Kim SM, Yun KH, Cho JY, Kim CJ, Ahn HS, Nam CW, Yoon HJ, Park YH, Lee WS, Jeong JO, Song PS, Doh JH, Jo SH, Yoon CH, Kang MG, Koh JS, Lee KY, Lim YH, Cho YH, Cho JM, Jang WJ, Chun KJ, Hong D, Park TK, Yang JH, Choi SH, Gwon HC, Hahn JY (2023) RENOVATE-COMPLEX-PCI investigators intravascular. Imaging-guided or angiography-guided complex PCI. N Engl J Med 388:1668–1679
Scarsini R, Fezzi S, Leone AM, De Maria GL, Pighi M, Marcoli M, Tavella D, Pesarini G, Banning AP, Barbato E, Wijns W, Ribichini FL (2022) Functional patterns of coronary disease: diffuse, focal, and serial lesions. JACC Cardiovasc Interv 15:2174–2191
Warisawa T, Howard JP, Cook CM, Ahmad Y, Doi S, Nakayama M, Goto S, Yakuta Y, Karube K, Seike F, Uetani T, Murai T, Kikuta Y, Shiono Y, Kawase Y, Shun-Shin MJ, Kaihara T, Higuma T, Ishibashi Y, Matsuda H, Nishina H, Matsuo H, Escaned J, Akashi YJ, Davies JE (2021) Inter-observer differences in interpretation of coronary pressure-wire pullback data by non-expert interventional cardiologists. Cardiovasc Interv Ther 36:289–297
Nijjer SS, Sen S, Petraco R, Escaned J, Echavarria-Pinto M, Broyd C, Al-Lamee R, Foin N, Foale RA, Malik IS, Mikhail GW, Sethi AS, Al-Bustami M, Kaprielian RR, Khan MA, Baker CS, Bellamy MF, Hughes AD, Mayet J, Francis DP, Di Mario C, Davies JE (2014) Pre-angioplasty instantaneous wave-free ratio pullback provides virtual intervention and predicts hemodynamic outcome for serial lesions and diffuse coronary artery disease. JACC Cardiovasc Interv 7:1386–1396
Nijjer SS, Sen S, Petraco R, Mayet J, Francis DP, Davies JE (2015) The Instantaneous wave-Free Ratio (iFR) pullback: a novel innovation using baseline physiology to optimize coronary angioplasty in tandem lesions. Cardiovasc Revasc Med 16:167–171
Biscaglia S, Verardi FM, Tebaldi M, Guiducci V, Caglioni S, Campana R, Scala A, Marrone A, Pompei G, Marchini F, Scancarello D, Pignatelli G, D’Amore SM, Colaiori I, Demola P, Di Serafino L, Tumscitz C, Penzo C, Erriquez A, Manfrini M, Campo G (2023) QFR-based virtual PCI or conventional angiography to guide PCI: the AQVA trial. QFR-based virtual PCI or conventional angiography to guide PCI: the AQVA trial. JACC Cardiovasc Interv 16:783–794
Biscaglia S, Verardi FM, Erriquez A, Colaiori I, Cocco M, Cantone A, Pompei G, Marrone A, Caglioni S, Tumscitz C, Penzo C, Manfrini M, Leone AM, Versaci F, Campo G (2024) Coronary physiology guidance vs conventional angiography for optimization of percutaneous coronary intervention: the AQVA-II trial. JACC Cardiovasc Interv 17:277–287
Shin D, Dai N, Lee SH, Choi KH, Lefieux A, Molony D, Hwang D, Kim HK, Jeon KH, Lee HJ, Jang HJ, Ha SJ, Park TK, Yang JH, Song YB, Hahn JY, Choi SH, Doh JH, Shin ES, Nam CW, Koo BK, Gwon HC, Ge J, Lee JM (2021) Physiological distribution and local severity of coronary artery disease and outcomes after percutaneous coronary intervention. JACC Cardiovasc Interv 14:1771–1785
Shin D, Dai N, Lee SH, Choi KH, Lefieux A, Molony D, Hwang D, Kim HK, Jeon KH, Lee HJ, Jang HJ, Ha SJ, Park TK, Yang JH, Song YB, Hahn JY, Choi SH, Doh JH, Shin ES, Nam CW, Koo BK, Gwon HC, Ge J, Lee JM (2022) Physiological distribution and local severity of coronary artery disease andoutcomes after percutaneous coronary intervention. J Am Heart Assoc 11:e024903
Acknowledgements
The authors thank Medis Medical Imaging Systems (Leiden, The Netherlands) for providing the QAngio XA 3D software and Pulse Medical (Shanghai, China) for providing the AngioPlus Core version V3 software free of charge for research purposes.
Funding
Open access funding provided by Università degli Studi di Verona within the CRUI-CARE Agreement. This work was supported in part by Science Foundation Ireland Research Professorship Award (15/RP/2765) to W. Wijns, which supports S. Fezzi, D. Ding and J. Huang.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
ST is the co-founder of Pulse Medical, reports research grants and consultancy from Pulse Medical. WW reports grants and consulting fees from MicroPort, outside the submitted work, and medical advisor of Corrib Core Laboratory and Rede Optimus, co-founder of Argonauts, an innovation facilitator. RS reports speaker fees from Abbott Vascular and research grant from Philips and Abbott. FR reports research grant from Philips and Abbott. All other authors report no competing interests.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fezzi, S., Del Sole, P.A., Burzotta, F. et al. Angiography-derived physiological patterns of coronary artery disease: implications with post-stenting physiology and long-term clinical outcomes. Clin Res Cardiol (2024). https://doi.org/10.1007/s00392-024-02500-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00392-024-02500-8