Abstract
Purpose
Previous studies have examined the optimal mode of breech delivery extensively, but there is a scarcity of publications focusing on the birth injuries of neonates born in breech presentation. This study aimed to examine birth injury in breech deliveries.
Methods
In this retrospective register-based nationwide cohort study, data on birth injuries in vaginal breech deliveries with singleton live births were compared to cesarean section with breech presentation and cephalic vaginal delivery between 2004 and 2017 in Finland. The data were retrieved from the National Medical Birth Register. Primary outcome variables were severe and mild birth injury. Incidences of birth injuries in different gestational ages and birthweights were calculated in different modes of delivery. Crude odds ratios of risk factors for severe birth injury were analyzed.
Results
In vaginal breech delivery (n = 4344), there were 0.8% of neonates with severe birth injury and 1.5% of neonates with mild birth injury compared to 0.06% and 0.2% in breech cesarean section (n = 16,979) and 0.3% and 1.9% in cephalic vaginal delivery (n = 629,182). Brachial plexus palsy was the most common type of injury in vaginal breech delivery. Increasing gestational age and birthweight had a stronger effect on the risk for injury among cephalic vaginal deliveries than among vaginal breech deliveries.
Conclusion
Birth injuries were rare in vaginal breech deliveries. The incidence of severe birth injury was two times higher in vaginal breech delivery compared to cephalic vaginal delivery. Brachial plexus palsy was the most common type of injury in vaginal breech delivery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
In vaginal breech delivery, birth injuries are rare, but brachial plexus palsy is more common than in cephalic vaginal delivery. |
Introduction
Approximately two to three percent of neonates diagnosed with birth injury [1, 2] are also at increased risk for other morbidities, such as hypoxic-ischemic encephalopathy, seizures, and death [1]. Concern has been raised about the risks for neonates in breech presentation, especially in vaginal delivery (VD), and the risks for the mother and subsequent pregnancies associated with cesarean section (CS) in term [3] and preterm delivery [4,5,6].
The risk for birth injury in breech presentation is considered comparable to that of cephalic vaginal delivery (cephalic VD) [7, 8], as the reported incidence of birth injury in singleton vaginal breech delivery at term varies from 0.3% to 7.4% [7,8,9,10,11]. In addition, the incidence of birth injury in breech CS has been reported to be between 0.2% and 0.9% [7, 8, 10, 11].
The incidence of morbidity and mortality of neonates after 37+0 weeks of gestation with breech presentation was higher after an attempt of VD than after planned CS in two large population-based studies [8, 10] and a randomized multicenter trial (the Term Breech Trial) [11]. Similarly, a systematic review and meta-analysis of non-randomized studies of preterm neonates concluded, and a retrospective cohort study of extremely preterm neonates observed that CS was associated with reduced neonatal mortality [4, 12]. Nevertheless, there is observational evidence showing that VD can be safe with the proper selection of women for both term [13, 14] and preterm neonates with breech presentation [15,16,17].
A considerable amount of literature has been published on morbidity and mortality rates, whereas only a few studies have focused on birth injuries among neonates born in breech presentation. Since the incidence of birth injuries has been described to be relatively low, a large nationwide register was chosen as a study cohort. This study aims to examine the type and rate of birth injuries in vaginal breech deliveries (breech VD) compared to CS with breech presentation (breech CS) and cephalic vaginal deliveries (cephalic VD) in Finland, where breech VD in selected women is still a common practice. We also aim to describe the incidence of birth injuries in different gestational weeks and explore the risk factors involved, especially those associated with severe birth injury in different types of delivery.
Materials and methods
This nationwide population-based cohort study was conducted using data from the Finnish Medical Birth Register (MBR) and the Care Register for Health Care. Both registers are maintained by the Finnish Institute for Health and Welfare. All Finnish hospitals are required to report clinical data to these national registries. The MBR includes data on pregnancies, deliveries, and information on the health of neonates. The data are completed by information obtained from the Central Population Register and the Cause-of-Death Register. The Care Register for Health Care contains information on patient diagnoses and operations performed during the hospital stay. The coverage and accuracy of these registers have been shown to be excellent [18, 19].
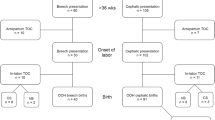
The study period was from 2004 to 2017, and it focused on singleton breech deliveries that resulted in a live birth. Breech VD and breech CS were studied separately. Planned and unplanned CS were analyzed together (breech CS) since birth injuries were infrequent after CS. Neonates with cephalic presentation born by spontaneous vaginal delivery or vacuum-assisted delivery formed a cephalic VD group, which was used for comparison. Forceps deliveries were excluded as they were rare (254/650,528 neonates), and the presentation of the neonate could not be reliably defined in all cases. Figure 1 presents a flowchart of the study population.
In Finland, five universities with medical faculties offer the education of medical doctors and trainees in gynecology and obstetrics. The management of breech delivery is included in the curriculum of gynecology and obstetrics. There are no national guidelines for term breech pregnancies. However, according to an inquiry addressed to the tertiary level obstetrics centers in Finland, there are common well-established clinical practices for managing breech pregnancies and deliveries after 37+0 weeks of gestation: Breech VD is an option if the mother is motivated to vaginal delivery, the estimated fetal weight is < 4000 g, and the fetus is in a frank, complete, or incomplete breech position with the head in a flexed position during the delivery. Often, adequate measurements of the maternal pelvis are confirmed by magnetic resonance pelvimetry. CS is preferred if intrauterine growth restriction is suspected, or the fetus is otherwise at high risk for distress during delivery. According to national guidelines for preterm deliveries, CS may lower the risk for morbidity in primiparas before 32 gestational weeks [20]. However, the mode of preterm delivery is individually selected based on obstetric indications. All breech deliveries are guided by experienced gynecologists, and CS is performed if distress of the fetus is suspected or when difficulties occur during delivery.
The two primary outcome variables were severe and mild birth injury. Birth injuries detected during the early neonatal period (0 to 6 days) were coded with the Finnish implementation of the 10th Revision of International Statistical Classification of Diseases and Related Health Problems (ICD-10) codes and retrieved from the MBR. In addition, hospital visits linked to any birth injury diagnosis recorded in the Care Register for Health Care during the first year after birth were included to increase the coverage. Severe birth injury was defined according to Muraca et al. [21] and included intracranial hemorrhage and laceration, severe injury to the central nervous system, subaponeurotic hemorrhage, skull fracture, long bone injury other than clavicle fracture, brachial plexus palsy (BPP), and injury to the liver or spleen. Mild birth injury included all birth injuries other than severe birth injuries. Outcomes were defined as one or more of the injuries described above. Neonates with both severe and mild birth injuries were included in the severe birth injury group. Outcomes for mild and severe birth injuries with ICD-10 codes are listed in Supplementary information, Table S1.
Tables 2 and 3 present the variables included in the final analysis. Diagnosis of type 1 and type 2 diabetes was based on ICD-10 codes retrieved from the MBR (O24.0, E10*, and O24.1, E11*), and gestational diabetes was defined as pathologic 2 h 75 g oral glucose tolerance test (also O24.4, O24.9). Data concerning prepregnancy body mass index (kg/m2) were included after 2006, as values from several hospitals were missing for the years 2004 and 2005. Birthweight above + 2 standard deviations (SD) or below − 2 SDs were defined as large for gestational age and small for gestational age standardized for parity, sex, and gestational age in a Finnish population [22]. The use of oxytocin was registered if it was used to induce and/or augment labor.
Statistical analyses
The incidences of severe and mild birth injury were calculated and stratified by gestational age. Variables were described as frequencies and proportions for categorical variables, and as means and standard deviations or medians and interquartile ranges for continuous variables. Welch two sample t-test and Mann–Whitney U-test were used for comparisons of continuous variables.
The risk factors for severe birth injury were calculated. The results are presented as odds ratios and risk differences with 95% confidence intervals (CI). Poisson regression model was used to assess the incidences of birthweight and gestational age using the number of cases per gestational weeks/birthweight as an offset term. The model was used separately for mild and severe birth injuries and in different modes of delivery. Regression analysis was limited to birthweight < 4000 g, as the clinical practice in Finland mainly recommend breech VD when the estimated fetal weight is < 4000 g. Statistical analysis was performed using R Statistical Software version 4.0.3.
Results
In total, 650,528 neonates were included. Of these, 4344 neonates (0.7%) had breech VD, 16,979 neonates (2.6%) had breech CS, and 629,182 neonates (96.7%) had cephalic VD, either spontaneous (90%) or vacuum-assisted (10%) (Fig. 1).
The incidences and frequencies of injured neonates with different birth injuries are presented in Table 1. The incidence of severe birth injury was highest in the breech VD group, whereas mild birth injury was more common in the cephalic VD group. BPP and clavicle fracture were the most frequent injuries after breech VD. In the breech VD group, 28% of injured neonates had BPP (0.6% of live births) and 24% had clavicle fracture (0.5% of live births). After cephalic VD, clavicle fracture (47% of injured neonates, 1.0% of live births) and cephalhematoma (35% of injured neonates, 0.8% of live births) were the most frequent injuries, followed by BPP (12% of injured neonates, 0.3% of live births). BPP accounted for 82% of the severe birth injuries in the breech VD group and 86% of the severe birth injuries in the cephalic VD group. None of the neonates with breech presentation had both clavicle fracture and BPP, whereas 323 neonates in the cephalic VD group had both. There were no intracranial hemorrhage or central nervous system injuries in the breech VD group and very few in the cephalic VD group. Both severe and mild birth injuries were infrequent in breech CS.
The birthweight of neonates with severe birth injury was 3320 g (SD 483) in the breech VD group and 4071 g (SD 518) in the cephalic VD group. Gestational ages were similar in both groups, 40+0 (interquartile range 38+5–40+4) and 40+2 (interquartile range 39+2–41+1), respectively (Table 2). We found no statistically significant risk factors for severe birth injury in breech VD (Table 3). For neonates in the cephalic VD group, the most important risk factors for severe birth injury were pregestational diabetes and large for gestational age. In the breech VD group, 3% of neonates with severe birth injury were large for gestational age compared with 19% in the cephalic VD group. Conversely, 3% of injured neonates in the breech VD group were small for gestational age in contrast to 0.6% in the cephalic VD group. The use of oxytocin was the only risk factor found for severe birth injury in the breech CS group.
Between gestational weeks 24+0 and 27+6 41% (51/124), 28+0 and 31+6 29% (55/187), 32+0 and 36+6 30% (500/1654), 37+0 and 40+6 19% (3336/18,014), and 41+0 and 42+6 30% (402/1344) of fetuses with breech presentation had VD. There were no severe birth injuries, and three neonates (at 31 weeks of gestation) in the breech VD group had a mild birth injury between 24+0 and 31+6 weeks of gestation. In the cephalic VD group, there was a similar finding of single injuries. After 32 weeks of gestation, the incidence of injury remained stable with some sporadic fluctuation up to 42 weeks of gestation among the breech VD group (Fig. 2). Between gestational weeks 32+0 and 36+6 8 mild and 4 severe birth injuries, 37+0 and 40+6 48 mild and 24 severe, and 41+0 and 42+6 4 mild and 5 severe birth injuries were diagnosed among the breech VD group. Also, in the breech VD group, no association was found in Poisson regression analysis between the incidence of mild birth injury and gestational weeks (estimated increase to incidence of injury for 1 gestational week was 0.96, 95% CI 0.88–1.05) or the incidence of severe birth injury and gestational weeks (1.12, 95% CI 0.93–1.35). In contrast, the incidence of birth injury showed an increasing trend with higher gestational age in the cephalic VD group (mild birth injury: 1.13, 95% CI 1.11–1.14, severe birth injury: 1.07, 95% CI 1.04–1.11), Fig. 2. There was no association between gestational age and incidence of birth injury in breech CS.
The incidence of mild birth injury (%) and severe birth injury (%) in different gestational weeks in vaginal breech delivery (n = 4344), cephalic vaginal delivery (n = 629,182), and cesarean section with breech presentation (n = 16,979) between 2004 and 2017 in Finland. Incidence presented as square root variant
Furthermore, no association was found in Poisson regression between birthweight (500 g to 4000 g) and incidence of mild birth injury (the estimated increase in incidence of injury for an increase of 100 g in birthweight was 1.01, 95% CI 0.97–1.06) or between birthweight and severe birth injury (1.06, 95% CI 0.98–1.14) in breech VD. In the cephalic VD group, the incidence of mild birth injury (1.09, 95% CI 1.09–1.10) and the incidence of severe birth injury (1.20, 95% CI 1.17–1.22) showed an increasing trend along with higher birthweight. In the breech CS group, however, the incidence of mild birth injury seemed to show a decreasing trend with increasing birthweight (0.94, 95% CI 0.90–1.0) (Fig. 3). There were only three neonates with severe birth injury (incidence 1.63%) and no neonates with mild birth injury and birthweight over 4000 g in the breech VD group (total of 184 neonates) (Fig. 4).
The incidence of mild birth injury (%) and severe birth injury (%) in different birthweight (500–4000 g) in vaginal breech delivery (n = 4344), cephalic vaginal delivery (n = 629,182), and cesarean section with breech presentation (n = 16,979) between 2004 and 2017 in Finland. Incidence presented as square root variant
Discussion
In this population-based study, the incidence of severe birth injury was higher in the vaginal breech delivery group than in the cesarean section with breech presentation group and the cephalic vaginal delivery group. However, the incidence remained low in all groups. A brachial plexus palsy was the most frequent injury in vaginal breech delivery. Perhaps because of the more rigorous selection of women for vaginal delivery, high birthweight did not seem to be as important a risk factor for birth injury in vaginal breech delivery as in cephalic vaginal delivery.
The total incidence of birth injury in breech VD was similar to that previously reported [8, 9, 11]. Surprisingly, there were no intracranial hemorrhage or central nervous system injuries after breech VD. In breech VD, a BPP was the most common injury followed by clavicle fractures. Although breech presentation is a risk factor for BPP [23], few studies have exclusively focused on BPP among neonates in breech presentation [24]. Moreover, it has been suggested that neonates born in breech presentation with BPP have a worse prognosis, a higher rate of bilateral plexus injuries, and a higher rate of concurrent phrenic nerve palsies than neonates born with an injury in cephalic presentation [24]. In our study, no concurrent clavicle fractures were found, and the birthweight of the injured neonates was lower in the breech VD group than in the cephalic VD group. These findings may suggest that BPP in breech VD may be due to unnecessary traction of the shoulders during delivery or difficulties in delivering an entrapped head. However, based on the findings of this study, we are unable to draw a definitive conclusion on this. In addition, we do not know whether the BPP identified in our study population were bilateral or persistent. Spinal cord injuries, of which none were found in our data, have been reported after a difficult head delivery [25]. In Finland, Løvset and Mauriceau maneuvers are most often used to deliver shoulders and head. However, due to the retrospective study design, we do not know which maneuvers if any, were used. International clinical practice guidelines recommend avoiding traction in the active second stage of vaginal delivery, but any specific maneuver is not favored [26]. In future studies, BPP in breech deliveries and difficulties with delivering the head should be specifically assessed.
Risk factors for severe birth injury, mostly representing the risk factors for BPP, found in cephalic VD were comparable to the risk factors reported for BPP in previous studies that mainly concerned neonates in cephalic presentation (fetal macrosomia, maternal diabetes, instrumental vaginal delivery, and shoulder dystocia) [23]. In the present study, we found no risk factors for severe birth injuries in breech VD. This finding may be due to the low number of injuries in the breech VD group. Another possible explanation might be the stricter selection of women for vaginal delivery and the lower threshold for antepartum and intrapartum CS when the fetus is in the breech presentation compared to pregnancies with the fetus in the cephalic presentation. The observed increase in the risk for severe birth injury with the use of oxytocin in the breech CS group is probably attributed to the attempted vaginal delivery.
The incidence of birth injury was low in all gestational ages in neonates with breech presentation, and no evidence was found of an association between gestational age and birth injury. It has been suggested that CS reduces perinatal morbidity and mortality in preterm breech neonates [4, 12, 27], but the improvement in neonatal outcomes is not supported by all researchers [15,16,17]. The Finnish guideline for preterm deliveries concludes that CS may reduce morbidity and mortality for neonates in breech presentation at < 32 weeks of gestation [20]. Although the low number of injuries in breech deliveries reduces the predictability and accuracy of the regression analysis results, our results suggest that the current clinical policy in Finland to manage preterm vaginal breech deliveries in selected women is acceptable, considering the low risk for birth injuries. Unfortunately, head entrapments are not registered in the MBR, and therefore the number of this rare and feared complication that is associated with preterm breech VD is unknown [15, 16].
Furthermore, the significance of high birthweight remains unclear. The guidelines recommend preferring CS when the estimated birthweight is > 3800 to 4000 g [28,29,30], but high birthweight has not been clearly shown to be associated with adverse outcomes [14, 31]. In Finland, there are no national guidelines for managing breech deliveries, although an estimated fetal weight of < 4000 g is a widely used criterion for attempted vaginal delivery. In the present study, we could not find an association between increasing birthweight or large for gestational age and birth injury in breech VD; however, they were risk factors for severe birth injury in cephalic VD. As previously mentioned, these results regarding breech VD and birthweight may have been affected by the rigorous selection of women and the surveillance of labor in addition to a low number of cases. To summarize, our results suggest that the current Finnish policy of managing breech pregnancies and breech VD up to a birthweight of 4000 g is acceptable, especially concerning birth injuries.
This study provides valuable information on the risks associated with breech deliveries. The strength of this study was the nationwide study population and the long study period that enabled us to study rare incidents such as birth injuries. In Finland, reporting to the registers is mandatory, the medical treatment of pregnancies is homogenous even without national guidelines for breech pregnancies, and the rate of breech VD has remained stable during the twenty-first century [32]. Thus, register data have good national coverage, and the reporting and selection biases are low [18, 19]. Our results were, however, restricted by the retrospective study design in which we are unable to study the intended mode of delivery, and rule out the possibility of variation among coding practices. Some of the most difficult deliveries, with failure to deliver head by traditional maneuvers, may have been excluded due to exclusion of forceps deliveries. Furthermore, even with a large sample size, the number of birth injuries remained modest, and thus limited the statistical power of the results. The simulation-based training of breech deliveries started at the end of the study period in delivery units, and a specific program of simulation training was launched in 2021 [33]. Hopefully, the implementation of the simulation training program improves the training and safety of breech deliveries in the future.
Conclusion
Our study confirmed that risk for birth injury is low in breech VD and breech CS. Nevertheless, the risk for severe birth injury, specifically BPP, was higher among breech VD than breech CS or cephalic VD. Birth injuries in neonates with breech presentation were sporadic, and no clinically relevant risk factors were found. These findings suggest that careful selection of women is required to ensure safe vaginal breech delivery.
References
Gupta R, Cabacungan ET (2021) Neonatal birth trauma: analysis of yearly trends, risk factors, and outcomes. J Pediatr 238:174-180.e3. https://doi.org/10.1016/j.jpeds.2021.06.080
Kekki M, Salonen A, Tihtonen K, Mattila VM, Gissler M, Huttunen TT (2020) The incidence of birth injuries decreased in Finland between 1997 and 2017: a nationwide register study. Acta Paediatr 109(12):2562–2569. https://doi.org/10.1111/apa.15267
Keag OE, Norman JE, Stock SJ (2018) Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: systematic review and meta-analysis. PLoS Med 15(1):e1002494–e1002494. https://doi.org/10.1371/journal.pmed.1002494
Hills F, Way M, Sekar R (2018) Mode of delivery for singleton extreme preterm breech fetuses: a 10 year retrospective review from a single tertiary obstetric centre. Aust N Z J Obstet Gynaecol 58(2):178–184. https://doi.org/10.1111/ajo.12681
Reddy UM, Rice MM, Grobman WA et al (2015) Serious maternal complications after early preterm delivery (24–33 weeks’ gestation). Am J Obstet Gynecol 213(4):538.e1-538.e9. https://doi.org/10.1016/j.ajog.2015.06.064
Toijonen A, Hinnenberg P, Gissler M, Heinonen S, Macharey G (2022) Maternal and neonatal outcomes in the following delivery after previous preterm caesarean breech birth: a national cohort study. J Obstet Gynaecol 42(1):49–54. https://doi.org/10.1080/01443615.2021.1871888
Berhan Y, Haileamlak A (2016) The risks of planned vaginal breech delivery versus planned caesarean section for term breech birth: a meta-analysis including observational studies. BJOG 123(1):49–57. https://doi.org/10.1111/1471-0528.13524
Lyons J, Pressey T, Bartholomew S, Liu S, Liston RM, Joseph K, Canadian perinatal surveillance system (public health agency of Canada) (2015) Delivery of breech presentation at term gestation in Canada, 2003–2011. Obstet Gynecol 125(5):1153–1161. https://doi.org/10.1097/AOG.0000000000000794
Azria E, Le Meaux J-P, Khoshnood B, Alexander S, Subtil D, Goffinet F, PREMODA study group (2012) Factors associated with adverse perinatal outcomes for term breech fetuses with planned vaginal delivery. Am J Obstet Gynecol 207(4):285.e1-285.e9. https://doi.org/10.1016/j.ajog.2012.08.027
Bin YS, Roberts CL, Ford JB, Nicholl MC (2016) Outcomes of breech birth by mode of delivery: a population linkage study. Aust N Z J Obstet Gynaecol 56(5):453–459. https://doi.org/10.1111/ajo.12488
Hannah ME, Hannah WJ, Hewson SA, Hodnett ED, Saigal S, Willan AR, Term breech trial collaborative (2000) Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Lancet 356(9239):1375–1383. https://doi.org/10.1016/S0140-6736(00)02840-3
Bergenhenegouwen LA, Meertens LJE, Schaaf J, Nijhuis JG, Mol BW, Kok M, Scheepers HC (2014) Vaginal delivery versus caesarean section in preterm breech delivery: a systematic review. Eur J Obstet Gynecol Reprod Biol 172:1–6. https://doi.org/10.1016/j.ejogrb.2013.10.017
Goffinet F, Carayol M, Foidart J-M, Alexander S, Uzan S, Subtil D, Bréart G, PREMODA study group (2006) Is planned vaginal delivery for breech presentation at term still an option? Results of an observational prospective survey in France and Belgium. Am J Obstet Gynecol 194(4):1002–1011. https://doi.org/10.1016/j.ajog.2005.10.817
Macharey G, Ulander V-M, Heinonen S, Kostev K, Nuutila M, Väisänen-Tommiska M (2017) Risk factors and outcomes in “well-selected” vaginal breech deliveries: a retrospective observational study. J Perinat Med 45(3):291–297. https://doi.org/10.1515/jpm-2015-0342
Kayem G, Combaud V, Lorthe E, Haddad B, Descamps P, Marpeau L, Goffinet F, Sentilhes L (2015) Mortality and morbidity in early preterm breech singletons: impact of a policy of planned vaginal delivery. Eur J Obstet Gynecol Reprod Biol 192:61–65. https://doi.org/10.1016/j.ejogrb.2015.06.019
Lorthe E, Sentilhes L, Quere M, Lebeaux C, Winer N, Torchin H, Goffinet F, Delorme P, Kayem G, EPIPAGE-2 obstetric writing group (2019) Planned delivery route of preterm breech singletons, and neonatal and 2 year outcomes: a population-based cohort study. BJOG 126(1):73–82. https://doi.org/10.1111/1471-0528.15466
Toivonen E, Palomaki O, Korhonen P, Huhtala H, Uotila J (2018) Impact of the mode of delivery on maternal and neonatal outcome in spontaneous—onset breech labor at 32+0–36+6 weeks of gestation: a retrospective cohort study. Eur J Obstet Gynecol Reprod Biol 225:13–18. https://doi.org/10.1016/j.ejogrb.2018.03.054
Gissler M, Teperi J, Hemminki E, Merilainen J (1995) Data quality after restructuring a national medical registry. Scand J Soc Med 23(1):75–80. https://doi.org/10.1177/140349489502300113
Sund R (2012) Quality of the Finnish hospital discharge register: a systematic review. Scand J Public Health 40(6):505–515. https://doi.org/10.1177/1403494812456637
Preterm birth. Current care guidelines (2018) Working group set up by the Finnish medical society duodecim and the Finnish gynaecological association. Helsinki: the Finnish Medical Society duodecim. www.kaypahoito.fi. Accessed 11 November 2021
Muraca GM, Lisonkova S, Skoll A, Brant R, Cundiff GW, Sabr Y, Joseph KS (2018) Ecological association between operative vaginal delivery and obstetric and birth trauma. CMAJ 190(24):E734–E741. https://doi.org/10.1503/cmaj.171076
Sankilampi U, Hannila M-L, Saari A, Gissler M, Dunkel L (2013) New population-based references for birth weight, length, and head circumference in singletons and twins from 23 to 43 gestation weeks. Ann Med 45(5–6):446–454. https://doi.org/10.3109/07853890.2013.803739
Van der Looven R, Le Roy L, Tanghe E, Samijn B, Roets E, Pauwels N, Deschepper E, De Muynck M, Vingerhoets G, Van den Broeck C (2020) Risk factors for neonatal brachial plexus palsy: a systematic review and meta-analysis. Dev Med Child Neurol 62(6):673–683. https://doi.org/10.1111/dmcn.14381
Al-Qattan M, El-Sayed AA, Al-Zahrani A, Al-Mutairi SA, Al-Harbi MS, Al-Mutairi AM, Al-Kahtani FS (2010) Obstetric brachial plexus palsy: a comparison of affected infants delivered vaginally by breech or cephalic presentation. J Hand Surg Eur 35(5):366–369. https://doi.org/10.1177/1753193409355895
Vialle R, Piétin-Vialle C, Vinchon M, Dauger S, Ilharreborde B, Glorion C (2008) Birth-related spinal cord injuries: a multicentric review of nine cases. Childs Nerv Syst 24(1):79–85. https://doi.org/10.1007/s00381-007-0437-z
Morris S, Geraghty S, Sundin D (2022) Breech presentation management: a critical review of leading clinical practice guidelines. Women Birth 35(3):e233–e242. https://doi.org/10.1016/j.wombi.2021.06.011
Toijonen A, Heinonen S, Gissler M, Macharey G (2020) Risk factors for adverse outcomes in vaginal preterm breech labor. Arch Obstet Gynaecol 303(1):93–101. https://doi.org/10.1007/s00404-020-05731-y
Azria E (2020) Breech presentation: CNGOF guidelines for clinical practice—case selection for trial of labour. Gynecol Obstet Fertil Senol 48(1):120–131. https://doi.org/10.1016/j.gofs.2019.10.026
Impey LWM, Murphy DJ, Griffiths M, Penna LK (2017) Management of breech presentation. BJOG 124(7):e151–e177. https://doi.org/10.1111/1471-0528.14465
Kotaska A, Menticoglou S, Gagnon R et al (2009) SOGC clinical practice guideline: vaginal delivery of breech presentation no. 226, June 2009. Int J Gynaecol Obstet 107(2):169–176. https://doi.org/10.1016/j.ijgo.2009.07.002
Jennewein L, Kielland-Kaisen U, Paul B, Möllmann CJ, Klemt A-S, Schulze S, Bock N, Schaarschmidt W, Brüggmann D, Louwen F (2018) Maternal and neonatal outcome after vaginal breech delivery at term of children weighing more or less than 3.8 kg: a frabat prospective cohort study. PLoS ONE 13(8):e0202760. https://doi.org/10.1371/journal.pone.0202760
Perinatal statistics—parturients, delivers and newborns 2019. Statistical report 48/2020. 20.11.2020. Finnish institute for health and welfare. https://www.julkari.fi/bitstream/handle/10024/140702/Tr48_20.pdf?sequence=1&isAllowed=y. Accessed 21 September 2021
Working group set up by the Finnish association of perinatology (2021). Raskaana olevien ja synnyttäjien hätätilanteiden hoito—Suomen synnytyssairaaloiden yhtenäinen koulutusohjelma. (training program for obstetric emergencies in Finnish delivery units) https://www.perinatologinenseura.fi/simulaatiojaos/raskaana-olevien-ja-synnyttajien/. Accessed 8 June 2022
Acknowledgements
We would like to thank the following individuals for their expertise and assistance in reviewing the management of breech deliveries in Finland: Leena Rahkonen (Helsinki University Hospital), Maija-Riitta Orden (Kuopio University Hospital), and Kristiina Tertti (Turku University Hospital).
Funding
The competitive State Research Financing of the Expert Responsibility area of Tampere University Hospital partly supported this study financially.
Author information
Authors and Affiliations
Contributions
MK: project development, data management and analysis, manuscript writing. TK: data management and analysis, manuscript editing. AS: project development, data management and analysis, manuscript editing. MG: data management and analysis, manuscript editing. HL: project development, data analysis, manuscript editing. TTH: project development, data management and analysis, manuscript editing. KT: project development, data management and analysis, manuscript writing. All authors contributed to the design of the study. TH, AS, and MG contributed to the acquisition of the data. MK, TK, KT, and TH were responsible for data analysis. All authors contributed to the interpretation of the data. MK was a major contributor in the writing of the manuscript. All authors participated in the drafting and revising of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Ethics committee of Tampere University Hospital (reference number R17069). Institutional approval was also obtained from the Finnish Institute for Health and Welfare (reference number THL/1659/5.05.00/2017).
Consent to participate
In accordance with Finnish regulations, and due to the retrospective register-based study design, no informed written consent was required. Only pseudonymized data were used.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kekki, M., Koukkula, T., Salonen, A. et al. Birth injury in breech delivery: a nationwide population-based cohort study in Finland. Arch Gynecol Obstet 308, 1139–1150 (2023). https://doi.org/10.1007/s00404-022-06772-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06772-1