Abstract
The objective of the present study was to characterize the molecular features of endometrial carcinomas with ambiguous histology. Eighteen carcinomas that could not be conclusively typed based on morphology and immunohistochemistry underwent analysis of mismatch repair (MMR) status, microsatellite status, and whole-exome sequencing. None of the tumors had pathogenic POLE mutation. Twelve tumors (67%) were microsatellite stable, and 6 (33%) had microsatellite instability. Fourteen tumors (78%) harbored TP53 mutations, and 2 (11%) had mutations in MMR genes. Eleven carcinomas (61%) were classified as copy number high and 7 (39%) as MSI-hypermutated, the latter including 3 tumors with TP53 mutation who concomitantly had MSI or mutation in a MMR gene. Other mutations that were found in > 1 tumor affected MUC16 (7 tumors), PIK3CA (6 tumors), PPP2R1A (6 tumors), ARID1A (5 tumors), PTEN (5 tumors), FAT1 (4 tumors), FAT4 (3 tumors), BRCA2 (2 tumors), ERBB2 (2 tumors), FBXW7 (2 tumors), MET (2 tumors), MTOR (2 tumors), JAK1 (2 tumors), and CSMD3 (2 tumors). At the last follow-up (median = 68.6 months), 8 patients had no evidence of disease, 1 patient was alive with disease, 8 patients were dead of disease, and 1 patient died of other cause. In conclusion, based on this series, the molecular landscape of endometrial carcinomas with ambiguous histology is dominated by TP53 mutations and the absence of POLE mutations, with heterogeneous molecular profile with respect to other genes. A high proportion of these tumors is clinically aggressive.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endometrial cancer, consisting predominantly of endometrial carcinoma (EC), is the 6th most common cancer in women globally. In 2020, it accounted for 417,367 new cancer diagnoses and 97,370 deaths [1]. In developed countries, it is the 4th common cancer in women, and its incidence is on the rise, primarily due to an increase in obesity [2].
EC histotypes include endometrial endometrioid carcinoma (EEC), serous carcinoma (SC), clear cell carcinoma (CCC), mucinous carcinoma (MC), mesonephric-like carcinoma, neuroendocrine carcinoma, dedifferentiated and undifferentiated carcinoma, and mixed tumors and tumors with hybrid phenotype and genetic profile. Additionally, carcinosarcomas (CS) are now regarded as biphasic malignancies derived from EC, most commonly SC [3].
The TCGA study identified 4 molecularly and clinically distinct EC groups, consisting of POLE ultramutated, microsatellite instability hypermutated, copy-number low, and copy-number high tumors [4]. Follow-up studies have demonstrated that a surrogate panel consisting of immunohistochemistry (IHC) for p53 and mismatch repair (MMR) proteins, combined with POLE mutations analysis, can reliably assign the majority of EC into one of the 4 abovementioned groups [reviewed in 5].
While the majority of EC can be reliably classified based on morphology and IHC, some cases with ambiguous features remain challenging. The latter include tumors harboring POLE mutation and tumors with deficient MMR (dMMR) from patients with Lynch syndrome, but tumors that do not belong to either of these groups are not rare.
Studies that have specifically focused on EC with ambiguous features have been few to date. Analysis of 13 cases by Espinosa et a. showed heterogenous IHC and molecular features in this group [6].
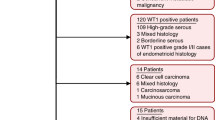
In the process of reviewing a large series of high-grade EC from our archives, with the objective of identifying grade 3 EEC (G3EEC) and SC, we identified 18 carcinomas that could not unequivocally be assigned to a histologic entity. The present study focuses on the genetic analysis of these tumors.
Material and methods
Patients and specimens
The study material consisted of a series of 18 hysterectomy specimens, submitted to the Departments of Pathology at the Norwegian Radium Hospital and Ullevål University Hospital (currently both part of Oslo University Hospital) for routine diagnostic purposes during the period 2007–2019. Tumors from recent years were diagnosed by experienced gyn-pathologists, whereas some of the earlier cases were signed out also by pathologists with less specialized training. Overall, 10 tumors were diagnosed as adenocarcinomas, NOS, 2 as SC, 2 as G3EEC, 2 as mixed SC-EEC, 1 as CS, and 1 as undifferentiated carcinoma.
The number of slides containing tumor in the hysterectomy specimens ranged from 1 to 10, with 3–4 tumor slides available in the majority of cases (12/18; 67%). In the 3 specimens for which < 3 slides were available, the reason was either the presence of a small tumor in a polyp (1 case, 2 slides containing tumor) or removal of most tumor tissue in the pre-operative curettage (1 case with 1 slide, 1 with 2 slides).
Specimens were independently reviewed by two experienced pathologists with sub-specialty in gynecologic pathology (BD and AJN) as part of a larger review of high-grade carcinomas focusing on grade 3 EEC (G3EEC) and SC. Cases were subsequently discussed in a consensus meeting. All cases underwent staining for p53 and MMR proteins, and additional IHC was performed as regarded necessary, using various combinations of the antibodies listed in Table 1. Lack of agreement with the original diagnosis or between the two observers after re-evaluation of morphology and IHC staining led to inclusion in the present study.
One of the pathologists (BD) selected the paraffin blocks and tumor area to be analyzed by whole-exome sequencing (WES). Minimum tumor cell content was set at 30%, and the majority of specimens contained > 50% tumor cells.
Clinicopathologic data are presented in Table 2. Study approval was given by the South-Eastern Norway Committee for Medical Research Ethics.
Whole-exome sequencing (WES)
DNA isolation
Tissue sections (two to five 10–20-µm-thick sections per patient) from formalin-fixed paraffin-embedded (FFPE) tumor and normal tissue were incubated overnight at 45 °C before deparaffinization in limonene and rehydration in a series of graded alcohol solutions. Areas of tumor cells were carefully scraped off the tumor tissue slides with a scalpel using adjacent H&E-stained sections as guides and transferred to lysis buffer in Eppendorf Safe-Lock tubes. From the normal tissue slides, the entire area was included. DNA and RNA were then extracted on a Qiacube (Qiagen, Hilden, Germany), using the Qiagen AllPrep DNA/RNA FFPE protocol, with buffer EB replacing buffer ATE as elution buffer. The isolated DNA was quantified using the Qubit dsDNA HS Assay Kit (Thermo Fisher, Waltham MA, USA).
Genomic analysis
Tumor and normal DNA were sequenced at the OUH Genomics Core Facility using Twist Human Core Exome enrichment (Twist Bioscience, South San Francisco CA, USA). Libraries were sequenced paired-end 2 × 150 bp on the NovaSeq6000 System (Illumina, San Diego CA, USA). The average coverage was 369.9 for the tumor samples and 157.2 for the normal samples.
Variant calling
Variant calling and analysis were performed with Illumina Dragen Bio-IT v. 3.9. The normal samples were first separately analyzed with the germline pipeline to identify potential single nucleotide (SNVs) and structural (SVs) variants. Tumor and normal samples were then analyzed with the tumor-normal analysis pipeline to identify somatic SNVs and SVs. The human reference genome GRCh38 (patch p12) (obtained from the UCSC database) was used for mapping and alignment. SNV and SV calling was performed with Twist Exome BED target file (target BED padding 250).
Variant annotation and filtration
The open-source software package Personal Cancer Genome Reporter (PCGR) [7] was used for somatic variant annotation. For each individual sample, a report summarizing the detected SNVs and SVs, in addition to computed tumor mutational burden (TMB), microsatellite instability (MSI) status, and mutational signatures, was generated.
Vcf files were used as input using settings “tumor-control, uterus samples.” Tumor reading depth (tdb) was set as > 1, and tumor allele frequency (taf) was set as > 0. SNVs with known relevance to endometrial carcinoma were extracted and filtered first for coding mutations, then for tumor reading depth ≥ 30 and tumor allele frequency ≥ 0.05. Occasional mutations with allele frequencies close to 0.5 or 1 were ignored, assuming these represent germline variations.
Mutational signatures
COSMIC single base substitution (SBS) mutational signatures [8] were generated for each tumor sample by the PCGR workflow [7], given that the total number of SNVs in the exome data exceeded 200. The mutational signature reconstruction was limited to the subset of SBS signatures relevant to the uterus category. An accuracy of fitting was calculated that reflects how well the mutation profile can be reconstructed based on the available signatures.
Mutational signatures were reported as the most dominant signature for a given tumor. Of note, contributions and fitting of the signatures varied among the samples (37–82%, 75–96%), and the contribution of the most dominant signature and second most dominant signature may be similar.
Results
Two representative cases (#8 and #16 in Table 2) of this series of 18 EC are shown in Figs. 1 and 2. Tumors tended to be morphologically homogenous, with the exception of one specimen in which part of the tumor had endometrioid features and the other part was serous-like, though IHC failed to highlight this difference.
Case # 8. A–D Morphology, H&E staining: invasive adenocarcinoma with high-grade nuclear features growing predominantly with a solid pattern, with a minor component showing glandular/acinar pattern. The tumor is infiltrated by a large number of mature lymphocytes. E–J Immunostaining. The tumor is only focally positive for ER (E) and PR (F). ARID1A is retained (G), PTEN is lost (H). p16 stains with block-positivity (I), p53 is aberrant/mutation-type (diffusely positive; J)
Case # 16. A–D Morphology, H&E staining: invasive adenocarcinoma growing with confluent glandular/acinar and trabecular pattern. The tumor consists of high columnar cells with high-grade nuclear features and strongly eosinophilic cytoplasm, with brisk mitotic activity. The tumor is infiltrated by some mature lymphocytes, though less densely than the case in Fig. 1. E–L Immunostaining. The tumor is partly positive for ER (E), but only focally positive for PR (F). ARID1A is retained (G), PTEN is lost (H). p16 stains with block-positivity (I), p53 is aberrant/mutation-type (diffusely positive; J). The tumor is negative for WT1 (K) and vimentin (L)
Fourteen tumors (78%) had aberrant (mutation-type) p53 staining patterns by IHC, and 4 (22%) had wild-type patterns. Loss of PMS2 or MSH6 occurred in 2 tumors (11%) each, with no overlap. Twelve tumors (67%) were microsatellite stable (MS), and 6 (33%) had microsatellite instability (MSI). Results are summarized in Table 3.
In exome sequencing, none of the tumors had pathogenic POLE mutation. Fourteen tumors (78%) harbored TP53 mutations, and 2 (11%) had mutations in MMR genes. Eleven carcinomas (61%) were classified as copy number high and 7 (39%) as MSI-hypermutated.
Other mutations that were found in > 1 tumor affected MUC16 (7 tumors), PIK3CA (6 tumors), PPP2R1A (6 tumors), ARID1A (5 tumors), PTEN (5 tumors), FAT1 (4 tumors), FAT4 (3 tumors), BRCA2 (2 tumors), ERBB2 (2 tumors), FBXW7 (2 tumors), MET (2 tumors), MTOR (2 tumors), JAK1 (2 tumors), and CSMD3 (2 tumors). Data are summarized in Supplementary Table 1.
Median follow-up was 69 months (range 25–169 months). Three patients did not receive any adjuvant therapy, while the remaining ones all received Platinol-based chemotherapy regimens.
At the last follow-up, 8 patients had no evidence of disease, 1 patient was alive with disease, 8 patients were dead of disease, and 1 patient died of other cause.
The 3 patients who did not receive chemotherapy (# 3, 14, and 16 in Table 2) did not have disease recurrence. Of note, all 3 tumors carried TP53 mutation (Supplementary Table 1).
Discussion
Extensive research in recent years has compellingly shown that EC is a highly heterogenous disease with complex genetic make-up, in which molecular features are informative of the clinical behavior and thereby patient outcome. Consequently, analysis of some of these features at the protein or gene level, mainly those derived from the TCGA study, has become a diagnostic standard in many institutions in developed countries, with the potential to affect patient management [5, 9,10,11]. Many tumors may be thus assessed, but some defy classification. This often pertains to tumors in which morphology and IHC are equivocal. While some of these tumors, including those carrying POLE mutations, may have indolent behavior, it is likely that others do not.
In the present series, 7 patients died of the disease, and 1 was diagnosed with recurrence at the last follow-up, data which denote a patient group with worse outcome than the entire population diagnosed with EC. In agreement with this, TP53 mutations, as well as aberrant p53 protein expression by IHC, were commonly found. Furthermore, while MSI and mutations in MMR genes were present in 6 and 2 cases, respectively, loss of MMR proteins by IHC was infrequent, and POLE pathogenic mutations were universally absent.
While the number of cases analyzed in the present study is insufficient for survival analysis, a closer look at the tumors which resulted in fatalities (# 1–2, 4–6, 15, and 17–18) does not suggest that p53 and MMR status by IHC or MS status are able to differentiate these patients from the remaining ones. The same is true for the sequencing analysis. This is particularly exemplified in the 3 patients who received no chemotherapy and experienced no disease recurrence, despite the presence of TP53 mutation in their tumors. The latter had otherwise different genetic features.
Other mutations detected in WES analysis affected several genes known to be mutated in EC, including those more common in EEC and/or CCC (PTEN, PIK3CA, ARID1A), and those more commonly observed in SC or other high-risk EC, as well as CS (PPP2R1A, ERBB2, FBXW7, MTOR, MET). The latter are considered to be diagnostic in the differentiation between SC and EC, as well as potential therapeutic targets in high-risk EC [12,13,14].
BRCA2 mutations were found in 2 tumors, of which 1 also had a TP53 mutation. In the series by Jamieson et al., BRCA2 mutations were found in 3% of EC with aberrant p53 expression [13]. In a recent analysis of 1625 EC of all histological types, 11 tumors carried pathogenic germline mutation in BRCA2 [15]. In another large study, the presence of BRCA2 mutations was more common in early-onset (< 50 years) compared to late-onset EC [16]. Treatment of these patients with poly (ADP-ribose) polymerase (PARP) inhibitors has obvious rationale.
Mutations in FAT1 and FAT4 were found in 4 and 3 tumors, respectively, and were not mutually exclusive. FAT genes encode FAT atypical cadherins, one of the 6 subfamilies of cadherins. Four FAT members (FAT1-4) have been identified in vertebrates. FAT proteins are transmembrane proteins involved in adhesion, migration, and proliferation, and modulate intracellular signaling via the WNT and MAPK pathways, additionally affecting epithelial-to-mesenchymal transition (EMT) [17]. Mutations in FAT1 have been described in various cancers, including leukemias and hepatocellular carcinoma, and altered, predominantly reduced, expression of FAT1 protein has been reported in these and other cancers, the latter including head and neck, esophageal, cervical, and breast carcinoma [reviewed in 17]. Similarly, mutations in FAT4 have been reported in various malignancies, including melanoma [18], colorectal carcinoma [19], and esophageal carcinoma [20]. Our data are in agreement with a recent study in which frequent FAT4 mutations were found in the analysis of 9 high-risk EC, consisting of 6 SC, 1 CCC, 1 G3EEC, and 1 dedifferentiated carcinoma [21].
JAK1 mutation was found in 2 tumors in the present study, of which one had MSI (frameshift mutation in JAK1) and one MSS (splice donor variant in JAK1). JAK1 is part of the JAK-STAT signaling pathway, which regulates the transcription of proteins involved in proliferation and cell survival. JAK family members, consisting of JAK1, JAK2, JAK3, and TYK2, are deregulated in immune response disorders, such as systemic lupus erythematosus, and in hematological cancers, and JAK inhibitors are used in the treatment of these diseases [22]. JAK1 frameshift mutations mediate immune response evasion via inhibition of antigen presentation in microsatellite unstable EC. In a large series published by Stelloo et al., 62/181 (34%) of EC has MSI, of which 35 (22%) harbored JAK1 mutation, though no prognostic role was found for this alteration [23]. Activation of the interferon-γ pathway is downregulated in EC carrying JAK1 mutation [24]. JAK1 mutations were additionally found to be significantly more common (45% vs. 4%) in EC with MLH1 methylation compared to tumors lacking this methylation [25]. Nevertheless, in a recent phase 2 study of EC patients treated with pembrolizumab, JAK1 mutations were not associated with resistance to this drug, as evidenced by the response in 7/10 patients with mutated tumors compared to 7/14 of patients with tumors lacking this mutation [26].
Finally, we report the finding of CSMD3 mutation in 2 carcinomas. CUB and sushi multiple domains 1 gene (CSMD1), the first gene cloned from this family, was described as a postulated adhesion molecule or transmembrane protein with a role as tumor suppressor in head and neck squamous cell carcinoma. Two other members, CSMD2 and CSMD3, were subsequently identified [27]. Reduced expression of CSMD1-3 proteins was reported in colorectal carcinoma compared to patient-matched normal tissue [28]. CSMD3 mutations were recently found in lung adenocarcinomas, with more frequent mutations in invasive compared to in situ tumors (8% vs. 3%) [29]. A previous report of CSMD3 mutations in EC has suggested that this finding likely reflects an elevated background mutation rate rather than the accumulation of pathogenic driver mutations [30].
Given the results of the molecular analysis, we reassessed the morphology and the IHC features of the tumors and attempted to assign them to one of the TCGA tumor groups. Applying this combined knowledge, and regarding, in the absence of POLE mutations, TP53 mutation as the determining molecular event, 14 of the carcinomas would be placed in the TP53-mutated category, whereas 4 would be classified as NSMP.
One obvious limitation of this study is the fact that molecular analysis was limited to a single paraffin block from each tumor. Despite the fact that tumors tended to have homogeneous morphology, the possibility that some were more heterogeneous at the genomic level cannot be entirely ruled out. Thus, for example, carcinomas initially belonging to the dMMR group may develop a clone carrying a TP53 mutation, an event which would result in a more aggressive clinical course. Studies of intra-tumoral heterogeneity may shed more light on this issue.
In conclusion, genomic analysis of the mutation profile of EC with ambiguous pathology reveals frequent TP53 mutations, as well as mutations in other genes related to aggressive clinical behavior, with universal absence of POLE pathogenic mutations. This suggests a need to regard these tumors as potentially aggressive, despite their heterogeneous clinical course. Several of the genes mutated in these tumors are relevant therapeutic targets.
Data availability
Sequencing data are available upon reasonable request.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
Torre LA, Islami F, Siegel RL, Ward EM, Jemal A (2017) Global cancer in women: burden and trends. Cancer Epidemiol Biomarkers Prev 26(4):444–457. https://doi.org/10.1158/1055-9965.EPI-16-0858
WHO Classification of Tumours Editorial Board. Female genital tumours (2020) WHO classification of tumours, 5th edn, vol 4. IARC, Lyon
Cancer Genome Atlas Research Network; Kandoth C, Schultz N, Cherniack AD, Akbani R, Liu Y, Shen H, Robertson AG, Pashtan I, Shen R, Benz CC, Yau C, Laird PW, Ding L, Zhang W, Mills GB, Kucherlapati R, Mardis ER, Levine DA (2013) Integrated genomic characterization of endometrial carcinoma. Nature 497(7447):67–73.https://doi.org/10.1038/nature12113
Gatius S, MatiasGuiu X, Davidson B (2024) Molecular features for timely cancer diagnosis and treatment - tumors of the ovary, fallopian tube and endometrium. Virchows Arch 484(2):339–351. https://doi.org/10.1007/s00428-023-03710-7
Espinosa I, D’Angelo E, Palacios J, Prat J (2016) Mixed and ambiguous endometrial carcinomas: a heterogenous group of tumors with different clinicopathologic and molecular genetic features. Am J Surg Pathol 40(7):972–981. https://doi.org/10.1097/PAS.0000000000000640
Nakken S, Fournous G, Vodák D, Aasheim LB, Myklebost O, Hovig E (2018) Personal cancer genome reporter: variant interpretation report for precision oncology. Bioinformatics 34(10):1778–1780. https://doi.org/10.1093/bioinformatics/btx817
Alexandrov LB, Kim J, Haradhvala NJ, Huang MN, Tian Ng AW, Wu Y, Boot A, Covington KR, Gordenin DA, Bergstrom EN, Islam SMA, Lopez-Bigas N, Klimczak LJ, McPherson JR, Morganella S, Sabarinathan R, Wheeler DA, Mustonen V; PCAWG Mutational Signatures Working Group; Getz G, Rozen SG, Stratton MR; PCAWG Consortium (2020) The repertoire of mutational signatures in human cancer. Nature 578(7793):94–101. https://doi.org/10.1038/s41586-020-1943-3
Talhouk A, McConechy MK, Leung S, Li-Chang HH, Kwon JS, Melnyk N, Yang W, Senz J, Boyd N, Karnezis AN, Huntsman DG, Gilks CB, McAlpine JN (2015) A clinically applicable molecular-based classification for endometrial cancers. Br J Cancer 113(2):299–310. https://doi.org/10.1038/bjc.2015.190
Concin N, Creutzberg CL, Vergote I, Cibula D, Mirza MR, Marnitz S, Ledermann JA, Bosse T, Chargari C, Fagotti A, Fotopoulou C, González-Martín A, Lax SF, Lorusso D, Marth C, Morice P, Nout RA, O’Donnell DE, Querleu D, Raspollini MR, Sehouli J, Sturdza AE, Taylor A, Westermann AM, Wimberger P, Colombo N, Planchamp F, Matias-Guiu X (2021) ESGO/ESTRO/ESP guidelines for the management of patients with endometrial carcinoma. Virchows Arch 478(2):153–190. https://doi.org/10.1007/s00428-020-03007-z
Santoro A, Angelico G, Travaglino A, Inzani F, Arciuolo D, Valente M, D’Alessandris N, Scaglione G, Fiorentino V, Raffone A, Zannoni GF (2021) New pathological and clinical insights in endometrial cancer in view of the updated ESGO/ESTRO/ESP guidelines. Cancers (Basel) 13(11):2623. https://doi.org/10.3390/cancers13112623
Ferriss JS, Erickson BK, Shih IM, Fader AN (2021) Uterine serous carcinoma: key advances and novel treatment approaches. Int J Gynecol Cancer 31(8):1165–1174. https://doi.org/10.1136/ijgc-2021-002753
Jamieson A, Sobral de Barros J, Cochrane DR, Douglas JM, Shankar S, Lynch BJ, Leung S, Martin S, Senz J, Lum A, Drew Y, Gilks CB, Huntsman DG, McAlpine JN (2024) Targeted and shallow whole-genome sequencing identifies therapeutic opportunities in p53abn endometrial cancers. Clin Cancer Res 30(11):2461–2474. https://doi.org/10.1158/1078-0432.CCR-23-3689
Cuevas D, Valls J, Gatius S, Roman-Canal B, Estaran E, Dorca E, Santacana M, Vaquero M, Eritja N, Velasco A, Matias-Guiu X (2019) Targeted sequencing with a customized panel to assess histological typing in endometrial carcinoma. Virchows Arch 474(5):585–598. https://doi.org/10.1007/s00428-018-02516-2
Gordhandas S, Rios-Doria E, Cadoo KA, Catchings A, Maio A, Kemel Y, Sheehan M, Ranganathan M, Green D, Aryamvally A, Arnold AG, Salo-Mullen E, Manning-Geist B, Sia T, Selenica P, Da Cruz PA, Vanderbilt C, Misyura M, Leitao MM, Mueller JJ, Makker V, Rubinstein M, Friedman CF, Zhou Q, Iasonos A, Latham A, Carlo MI, Murciano-Goroff YR, Will M, Walsh MF, IssaBhaloo S, Ellenson LH, Ceyhan-Birsoy O, Berger MF, Robson ME, Abu-Rustum N, Aghajanian C, Offit K, Stadler Z, Weigelt B, Mandelker DL, Liu YL (2023) Comprehensive analysis of germline drivers in endometrial cancer. J Natl Cancer Inst 115(5):560–569. https://doi.org/10.1093/jnci/djad016
Choi J, Holowatyj AN, Du M, Chen Z, Wen W, Schultz N, Lipworth L, Guo X (2022) Distinct genomic landscapes in early-onset and late-onset endometrial cancer. JCO Precis Oncol 6:e2100401. https://doi.org/10.1200/PO.21.00401
Peng Z, Gong Y, Liang X (2021) Role of FAT1 in health and disease. Oncol Lett 21(5):398. https://doi.org/10.3892/ol.2021.12659
Nikolaev SI, Rimoldi D, Iseli C, Valsesia A, Robyr D, Gehrig C, Harshman K, Guipponi M, Bukach O, Zoete V, Michielin O, Muehlethaler K, Speiser D, Beckmann JS, Xenarios I, Halazonetis TD, Jongeneel CV, Stevenson BJ, Antonarakis SE (2011) Exome sequencing identifies recurrent somatic MAP2K1 and MAP2K2 mutations in melanoma. Nat Genet 44(2):133–139. https://doi.org/10.1038/ng.1026
Yu J, Wu WK, Li X, He J, Li XX, Ng SS, Yu C, Gao Z, Yang J, Li M, Wang Q, Liang Q, Pan Y, Tong JH, To KF, Wong N, Zhang N, Chen J, Lu Y, Lai PB, Chan FK, Li Y, Kung HF, Yang H, Wang J, Sung JJ (2015) Novel recurrently mutated genes and a prognostic mutation signature in colorectal cancer. Gut 64(4):636–645. https://doi.org/10.1136/gutjnl-2013-306620
Gao YB, Chen ZL, Li JG, Hu XD, Shi XJ, Sun ZM, Zhang F, Zhao ZR, Li ZT, Liu ZY, Zhao YD, Sun J, Zhou CC, Yao R, Wang SY, Wang P, Sun N, Zhang BH, Dong JS, Yu Y, Luo M, Feng XL, Shi SS, Zhou F, Tan FW, Qiu B, Li N, Shao K, Zhang LJ, Zhang LJ, Xue Q, Gao SG, He J (2014) Genetic landscape of esophageal squamous cell carcinoma. Nat Genet 46(10):1097–1102. https://doi.org/10.1038/ng.3076
Feng W, Jia N, Jiao H, Chen J, Chen Y, Zhang Y, Zhu M, Zhu C, Shen L, Long W (2021) Circulating tumor DNA as a prognostic marker in high-risk endometrial cancer. J Transl Med 19(1):51. https://doi.org/10.1186/s12967-021-02722-8
Agashe RP, Lippman SM, Kurzrock R (2022) JAK: not just another kinase. Mol Cancer Ther 21(12):1757–1764. https://doi.org/10.1158/1535-7163.MCT-22-0323
Stelloo E, Versluis MA, Nijman HW, de Bruyn M, Plat A, Osse EM, van Dijk RH, Nout RA, Creutzberg CL, de Bock GH, Smit VT, Bosse T, Hollema H (2016) Microsatellite instability derived JAK1 frameshift mutations are associated with tumor immune evasion in endometrioid endometrial cancer. Oncotarget 7(26):39885–39893. https://doi.org/10.18632/oncotarget.9414
Glaire MA, Ryan NA, Ijsselsteijn ME, Kedzierska K, Obolenski S, Ali R, Crosbie EJ, Bosse T, de Miranda NF, Church DN (2022) Discordant prognosis of mismatch repair deficiency in colorectal and endometrial cancer reflects variation in antitumour immune response and immune escape. J Pathol 257(3):340–351. https://doi.org/10.1002/path.5894
Manning-Geist BL, Liu YL, Devereaux KA, Paula ADC, Zhou QC, Ma W, Selenica P, Ceyhan-Birsoy O, Moukarzel LA, Hoang T, Gordhandas S, Rubinstein MM, Friedman CF, Aghajanian C, Abu-Rustum NR, Stadler ZK, Reis-Filho JS, Iasonos A, Zamarin D, Ellenson LH, Lakhman Y, Mandelker DL, Weigelt B (2022) Microsatellite instability-high endometrial cancers with MLH1 promoter hypermethylation have distinct molecular and clinical profiles. Clin Cancer Res 28(19):4302–4311. https://doi.org/10.1158/1078-0432.CCR-22-0713
Chow RD, Michaels T, Bellone S, Hartwich TMP, Bonazzoli E, Iwasaki A, Song E, Santin AD (2023) Distinct mechanisms of mismatch-repair deficiency delineate two modes of response to Anti-PD-1 immunotherapy in endometrial carcinoma. Cancer Discov 13(2):312–331. https://doi.org/10.1158/2159-8290.CD-22-0686
Lau WL, Scholnick SB (2003) Identification of two new members of the CSMD gene family. Genomics 82(3):412–415. https://doi.org/10.1016/s0888-7543(03)00149-6
Zhang R, Song C (2014) Loss of CSMD1 or 2 may contribute to the poor prognosis of colorectal cancer patients. Tumour Biol 35(5):4419–4423. https://doi.org/10.1007/s13277-013-1581-6
Lin Y, Li D, Hui H, Miao H, Luo M, Roy B, Chen B, Zhang W, Shao D, Ma D, Jie Y, Qiu F, Li H, Jiang B (2024) Genomic landscape and tumor mutational features of resected preinvasive to invasive lung adenocarcinoma. Front Oncol 14:1389618. https://doi.org/10.3389/fonc.2024.1389618
Bianco B, Barbosa CP, Trevisan CM, Laganà AS, Montagna E (2020) Endometrial cancer: a genetic point of view. Transl Cancer Res 9(12):7706–7715. https://doi.org/10.21037/tcr-20-2334
Funding
Open access funding provided by University of Oslo (incl Oslo University Hospital). This study was supported by a grant from the Cancer Foundation at the Norwegian Radium Hospital (Radiumhospitalets Legater).
Author information
Authors and Affiliations
Contributions
BD designed the study, reviewed the tumors and IHC staining, selected specimens for molecular analysis, and wrote the manuscript; KTL performed the molecular analysis, interpreted the results, and critically read the manuscript; AH performed the IHC analysis and critically read the manuscript; KL and AGZE provided clinical data and critically read the manuscript; TS supervised the molecular analysis, interpreted the results, and critically read the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Informed consent was obtained according to national and institutional guidelines. Study approval was given by the South-Eastern Norway Committee for Medical Research Ethics.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Davidson, B., Teien Lande, K., Nebdal, D. et al. Endometrial carcinomas with ambiguous histology often harbor TP53 mutations. Virchows Arch (2024). https://doi.org/10.1007/s00428-024-03912-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00428-024-03912-7