Abstract
Objectives
This study aims to investigate the changes in alveolar bone following the simultaneous performance of labial and lingual augmented corticotomy (LLAC) in patients with insufficient alveolar bone thickness on both the labial and lingual sides of the mandibular anterior teeth during presurgical orthodontic treatment.
Materials and methods
Thirth-five surgical patients with skeletal Class III malocclusion were included: 19 (LLAC group) accepted LLAC surgery during presurgical orthodontic treatment, and 16 (non-surgery group, NS) accepted traditional presurgical orthodontic treatment. Cone-beam computed tomography (CBCT) scans were obtained before treatment (T0) and at the completion of presurgical orthodontic treatment (T1). The amount of vertical alveolar bone and contour area of the alveolar bone in the labial and lingual sides of mandibular incisors were measured.
Results
After presurgical orthodontic treatment, the contour area of the alveolar bone at each level on the lingual side and alveolar bone level on both sides decreased significantly in the NS group (P < 0.001). However, the labial and lingual bone contour area at each level and bone level increased significantly in the LLAC group (P < 0.001). The bone formation rate in the lingual apical region was the highest, significantly different from other sites (P < 0.001).
Conclusions
During presurgical orthodontic treatment, LLAC can significantly increase the contour area of the labio-lingual alveolar bone in the mandibular anterior teeth to facilitate safe and effective orthodontic decompensation in skeletal Class III patients.
Clinical relevance
: This surgery has positive clinical significance in patients lacking bone thickness (< 0.5 mm) in the labial and lingual sides of the lower incisors.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
During orthodontic treatment, maintaining the integrity of the root and surrounding alveolar bone is crucial for ensuring the safety, function, speed, aesthetics, and long-term health of the treatment [1]. Patients with skeletal Class III malocclusion have high aesthetic requirements and often require orthodontic-orthognathic treatment to improve both function and appearance [2]. However, these patients frequently encounter challenges such as insufficient soft and hard tissue around the anterior teeth, a high incidence of bone fenestration and dehiscence, thin alveolar bone and gingiva, and a narrow width of keratinized gingiva, particularly in the lower anterior teeth [3,4,5]. Those with inadequate basal bone, especially on the labial and lingual sides, are at a high risk of gingival recession, root resorption, tooth loosening, and dental relapse after extensive anterior tooth movement during the orthodontic decompensation process [6,7,8].
Recently, augmented corticotomy (AC)-assisted orthodontic treatment, developed from periodontally accelerated osteogenic orthodontics (PAOO), has gained wider acceptance. Existing studies have shown that the labial alveolar bone thickness of the lower anterior teeth can increase by approximately 0.19–1.56 mm after AC [9,10,11]. AC surgery can improve the periodontal condition of anterior teeth with fenestration and dehiscence, prevent the secondary occurrence of alveolar bone fenestration and dehiscence during presurgical orthodontic treatment (POT) [12, 13], and avert gingival recession on the labial side. However, in some skeletal Class III patients with inadequate basal bone, the height and thickness of the lingual alveolar bone are significantly reduced after POT [14, 15]. Currently, research on simultaneous labial and lingual augmented corticotomy (LLAC) of the lower anterior teeth during orthodontic treatment is limited to individual case reports [16, 17], and no systematic studies have confirmed the safety and long-term efficacy of the postoperative bone increment following LLAC in lower anterior teeth.
This study performed LLAC on skeletal Class III patients with alveolar bone thickness < 0.5 mm in the lingual and labial sides of the lower anterior teeth before POT. Clinical examination and cone-beam computed tomography (CBCT) were used to evaluate the changes in the labio-lingual alveolar bone before orthognathic surgery to verify the effectiveness and safety of LLAC. The clinical indications of the operation were also discussed.
Materials and methods
This study was approved by the Research Ethics Committee of Peking University Health Science Center (approval no PKUSSIRB-202,277,090) and conducted following the Helsinki Declaration of 1975, as revised in 2013. The study was registered in the National Health Security Information Platform / Medical Research Registration and Filing System (www.medicalresearch.org.cn) [Medical Research Filing Number MR-11-22-007414]. Notably, all protocols were performed following the approved guidelines and regulations, and written informed consent was obtained from all participants.
Sample size
Appropriate sample size is required to distinguish changes in the alveolar bone area between the non-surgery group (NS) and the LLAC group. Our previous study [18] showed that the labial alveolar bone area changes during presurgical orthodontic treatment in NS and AC were 0 ± 3.54mm2 and 8.32 ± 5.91 mm2, respectively. Based on this data, we used the PASS 15.0 (Power Analysis and Sample Size Software 15.0, NCSS, USA) software to determine that at least seven subjects were required for this study under the conditions α = 0.05 and β = 0.2.
Patient selection
This study was performed as a historical controlled trial. A series of patients who had completed POT between June 2022 and June 2024 were selected. These patients had not yet undergone orthognathic surgery. Thirty-five patients with skeletal Class III malocclusion requiring surgical orthodontic treatment participated in the study at the Peking University School and Hospital of Stomatology. Nineteen patients who met the inclusion criteria were collected into LLAC group. Another 16 patients who met 1 ~ 5 inclusion criteria and received traditional presurgical orthodontic treatment therapy were matched as control group (NS group). The same exclusion criteria were applied to LLAC and NS group (Fig. 1; Table 1).
Inclusion criteria were as follows: (1) age 14˗30 years old with good systemic health; (2) skeletal class III malocclusion requiring orthodontic and orthognathic treatment (ANB < 0°, overjet < 0 mm); (3) mild crowding in the lower anterior arch (< 4 mm); (4) good periodontal health, with probing depth ≤ 3 mm and bleeding on probing ≤ 15%; (5) no smoking history. (6) CBCT revealed the thickness of the labial and lingual cortical bone of < 0.5 mm at 4 mm and 8 mm apical to the cementoenamel junction (CEJ) before or during treatment in the LLAC group; (7) during the presurgical orthodontic treatment process, the orthodontist predicts that the tooth root will protrudes beyond the boundaries of the existing lingual alveolar bone.
Exclusion criteria were as follows: (1) pregnancy or lactation; (2) uncontrolled periodontal infection; (3) history of periodontal surgical treatment on the anterior teeth; (4) systemic disease or use of medication known to affect periodontal status; and (5) cleft lip/palate or maxillofacial abnormality.
The medical records of these patients were reviewed, including clinical examination, intraoral photographs, and imaging examinations.
Treatment procedures
All recruited patients were referred to one periodontal specialist for periodontal examination and treatment, including oral hygiene instruction, scaling, and root planning if indicated. Regular professional care was performed every 3˗6 months to ensure each subject met and maintained clinical periodontal health status.
For the patients in the LLAC group, periodontal surgeries were performed by the same experienced periodontist (Li Yi). The surgical procedure took place between 3 and 6 months after the orthodontic treatment, during which time the crowding of the teeth was largely alleviated, but the primary orthodontic decompensation process had not yet commenced. The orthodontic movement of the lower front teeth was halted during the surgical procedure and resumed four weeks after the operation.
The surgical procedure is shown in Fig. 2. Following local anesthesia administration, a modified papilla preservation incision was made at the base of the labial papilla. Full-thickness flaps on the labial and lingual sides were carefully elevated, and the flap range stopped at the apical level of the roots, not exceeding 15 mm apical to CEJ on both sides. A Piezo-Surgical knife (OT7S-4; PiezoSurgery, Mectron, Italy) was used to create a vertical interproximal alveolar decortication below the alveolar crest to a depth of 2–3 mm. The vertical decortication length is approximately 5 mm, and the depth is approximately 1.5 mm. Decortication on the labial and lingual sides was not located on the same sagittal plane to avoid bone penetration. Bone derivative material (Bio-Oss, 1 g; Geistlich, Switzerland) was grafted onto the labial and lingual aspects of the decorticated anterior cortical bone and into dehiscence and fenestrations, in the coronal-apical direction. Bioabsorbable collagen membrane (Bio-Gide, 25 mm × 25 mm; Geistlich, Switzerland) was adapted to completely cover the graft site. The membrane reflexed inward toward the root to avoid displacing the bone graft material towards the root. Flaps were coronally repositioned with double-sling sutures and interrupted interdental sutures using non-absorbable 6 − 0 Prolene (Ethicon US, CA). Amoxicillin capsules (500 mg thrice daily for 5 days) and 0.12% chlorhexidine (10 mL twice daily for 14 days) were recommended postoperatively. Ibuprofen was used at 0.3 g every 12 h within 3 days postoperatively when the patient felt intense pain. Sutures were removed 2 weeks postoperatively. Orthodontic forces were applied 4 weeks after the periodontal surgery. Presurgical and postsurgical orthodontic treatments were performed by specialist orthodontists using a straight-wire fixed appliance.
Surgical procedure for labial and lingual augmented corticotomy in a subject with severe skeletal Class III malocclusion, (A-B): Presurgical view of labial and lingual side; (C): Papilla preservation incision was made on labial side. Multiple bone fenestration and dehiscence were found on the labial after flap; (D): Multiple dehiscences on the lingual side; (E-F): Bone derivative material was placed in the exposed mandibular area, and bioabsorbable collagen membrane covered the graft site. The membrane on the labial and lingual side reflexed inward toward the root to avoid displacement of the bone graft material toward the root. (G): Flaps were coronally repositioned and sutured in place; (H-I): 2 weeks postoperatively, early wound healing index = 1; (J-K): Intraoral photos before orthognathic operation, there was no gingival recession; (L): Sagittal view before orthodontic treatment by CBCT; (M): Sagittal view before orthognathic by CBCT. CBCT: Cone-beam computed tomography
Patients in the NS group did not undergo the LLAC operation because the periodontal condition was acceptable or the patients refused. The two orthodontists performed the presurgical and postsurgical orthodontic treatments.
Thereafter, all patients underwent bimaxillary jaw surgery (Le-Fort I maxillary advancement and mandibular setback sagittal split ramus osteotomy) with rigid internal fixation by one orthognathic surgeon.
Radiographic measurements
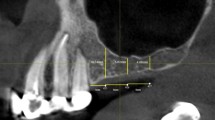
Cephalometric radiographs were collected at T0. For LLAC group, CBCT scans were performed before orthodontic treatment (T0), before LLAC (TS0), immediately after LLAC (TS1), and after presurgical orthodontic treatment (T1) using a NewTom VG device (Aperio Services, Italy) to evaluate changes produced by the surgical and orthodontic procedure. For NS group, CBCT scans were performed at T0 and T1. The NS group underwent 2 CBCT scans, while LLAC group underwent 4 CBCT scans. The overall radiation dose for one patient ranges from 80 to 200 µSv, which met the principle of radiological protection recommended by International Commission on Radiological Protection (ICRP).) Radiographic data collected in this study were as follows: cephalometric measurements including ANB, SN-GoGn, L1-MP; sagittal root position (SRP) to its osseous housing (Table 2), classified as Class I (root positioned against the labial cortical plate), Class II (root centered in the middle of the osseous housing without engaging the labial or the palatal cortical plates at the apical third of the root), Class III (root positioned against the palatal cortical plate), or Class IV (at least two-thirds of the root engages the labial and palatal cortical plates) [19]; alveolar bone contour area was measured by importing DICOM files into the Mimics software (versus 21.0; Materialise Mimics Medical, Belgium). Bone contour area was recorded perpendicular to the long axis of each mandibular incisor at four levels (4 mm, 6 mm, and 8 mm levels apical to CEJ and at the root apex level). The alveolar bone level was defined as the distance from the CEJ to alveolar crest (CEJ-AC) parallel to the root long axis, which was also recorded (Fig. 3). Notably, all variables were measured on the sagittal slices where the incisors were the widest labiolingual in the axial view. Bone formation rate (BFR) is the ratio of final bone formation to initial bone grafting calculated in the LLAC group. BFR was calculated using the formula: (T1- TS0) / (TS1 - TS0 ).
Illustration of measurements and reference points used in this study. Reference points and lines: 1 and 2, cemento-enamel junction (CEJ) points; 3, midpoint of the CEJ; 4 and 5, alveolar crest points; 6, root apex; 7, root long axis, a line from points 3 to 6; 8, 9 and 10, intersecting line perpendicular to the root long axis at 4, 6 and 8 mm apical to the midpoint of the CEJ; 11, intersecting line perpendicular to the root long axis at the root apex. Measurement variables: B-CEJ-AC and L-CEJ-AC, buccal and lingual bone level, distance from the CEJ to the alveolar crest parallel to the root long axis; BA-4 and LA-4, labial and lingual bone area at 4 mm apical to the CEJ; BA-6 and LA-6, labial and lingual bone area at 6 mm apical to the CEJ; BA-8 and LA-8, labial and lingual bone area at 8 mm apical to the CEJ; BA-A and LA-A, labial and lingual bone area at the apex level
Statistical analysis
All measurements of radiographic examinations were conducted twice at an interval of 2 weeks. The investigator for orthodontic radiographic examination (Fu Y), the investigator for periodontal radiographic examination (Liu J), and the investigator for clinical periodontal examination (Li Y) had undergone the intraclass correlation check. The intraclass correlation coefficient (ICC) values for all parameters were > 0.9, indicating that the measurements had excellent reliability. The mean of the two measurements was used in the statistical analysis. Variables are presented as mean ± standard deviation (SD; normal distribution). Statistical analyses were performed using Statistical Package for the Social Sciences Statistics version 25 software (IBM Corp., Armonk, NY, USA). The distributional normality of each variable was evaluated through the application of the Shapiro-Wilk test. SRP changes from T0 to T1 were analyzed with the Fisher’s exact test. A paired t-test was used to compare changes in all the measurements before and after presurgical orthodontic treatment in the two groups. Differences between the LLAC and NS groups were analyzed using the independent-sample t-test. Dunnett-t3 multiple comparison test was used to compare the BFR at different levels.
Results
There were 19 patients (5 males and 14 females, mean age of 22.16 ± 2.95 years) in LLAC and 16 patients (4 males and 12 females, mean age of 20.68 ± 2.60 years) in NS. The two groups matched well in terms of age, sex, ANB, SN-GoGn, L1-MP, PD and BI. (Table 2).
Sixty-three mandibular incisors were allocated to the NS group and 74 to the LLAC group. In total, 137 mandibular incisors (two mandibular lateral incisors and one central incisor were congenitally missing) were included.
Regarding SRP in the NS group, 30 teeth (55.56%) had roots positioned against the labial cortical plate (SRP I), and 28 teeth (44.45%) had at least two-thirds of the root engaging the labial and palatal cortical plates (SRP IV) at T0. After POT, 5 (7.94%) had roots positioned against SRP I,16 (25.40%) teeth had roots positioned against the palatal cortical plate (SRP III), and 42 teeth (66.67%) had roots positioned against SRP IV at T1. The change in SRP was significantly different in the NS group (P < 0.001). The number of teeth belonging to SRP IV increased significantly. In the LLAC group, 63 teeth (85.14%) had roots positioned against SRP IV and other teeth positioned SRP I (9, 9.46%) or SRP III (2, 2.70%) at T0. However, after LLAC and presurgical orthodontic treatment, 64 teeth (86.49%) had roots centered in the middle of the osseous housing (SRP II) at T1. The number of teeth belonging to SRP II increased significantly (P < 0.001). After LLAC surgery, the root could be kept in the center of the alveolar bone, even with extensive decompensation (Table 3).
The amount of labiolingual bone was extremely deficient in the LLAC group at T0 (Table 4). The height of the labiolingual alveolar bone and the area of the lingual alveolar bone in the LLAC group were significantly lower than those in the NS group. However, after POT, the alveolar bone height and alveolar bone area in the LLAC group were significantly higher than those in the NS group at T1.
In the NS group, there is a decreasing trend in the labial bone contour area at 4 mm and 6 mm apical to CEJ after T1, but the difference was not statistically significant. Hower, lingual alveolar bone contour area decreased significantly at each level in the NS group after POT. Before orthodontic treatment, LA-4 mm, LA-6 mm, LA-8 mm and LA-A in NS group were 0.24 ± 0.33 mm2, 0.72 ± 0.93 mm2, 1.39 ± 1.53 mm2, 5.04 ± 3.84 mm2 respectively. LA-4 mm, LA-6 mm, LA-8 mm and LA-A decreased to an average of 0.06 ± 0.08 mm2, 0.16 ± 0.35 mm2, 0.29 ± 0.62 mm2, 0.74 ± 1.13 mm2.
In contrast, the labial and lingual bone contour area increased significantly in the LLAC group at each level. The comparisons revealed the following changes: at BA-4 mm and LA-4 mm, the average bone area rose from 0.28 ± 0.46 mm2, 0.12 ± 0.22 mm2 to 1.18 ± 1.25 mm2 and 1.22 ± 1.94 mm2. At BA-6 mm and LA-6 mm, there was an increase from an initial average of 0.46 ± 0.66 mm2, 0.43 ± 0.55 mm2 to 3.22 ± 1.76 mm2 and 3.41 ± 2.13 mm2. Progressing to BA-8 mm and LA-8 mm, the bone measurement saw a growth from 0.56 ± 0.78 mm2, 0.89 ± 1.08 mm2 to 6.24 ± 2.28 mm2 and 6.59 ± 3.52 mm2. Finally, at BA-A and LA-A, the bone measurement expanded from a starting average of 1.89 ± 1.09 mm2, 3.06 ± 2.32 mm2 to 10.95 ± 4.55 mm2 and 11.23 ± 5.84 mm2 (Table 4). There was a statistically significant difference in the changes of labial and lingual bone contour area between the two groups (Table 5; Fig. 4). The labial alveolar bone area increased approximately 1.81 ± 2.90 mm2 while the lingual side showed a decrease of about 4.62 ± 3.69 mm2 in NS group. However, in LLAC group, the bone contour area of the labial and lingual sides increased by 9.06 ± 4.47mm2 and 8.17 ± 6.34mm2, respectively.
NS, non-surgery treatment group; LLAC, labial and lingual augmented corticotomy; △=T1-T0; B-CEJ-AC and L-CEJ-AC, distance between Cemento-Enamel Junction and Alveolar Crest on buccal and lingual sides; P, student t-test for comparison between groups.
CBCT images of 19 skeletal Class III patients who accepted labial and lingual augmented corticotomy (LLAC). The same tooth position (right mandibular lateral incisor) of 19 patients were selected. (A): before LLAC; (B): immediately after LLAC; (C): after presurgical orthodontic treatment; CBCT: Cone-beam computed tomography
The 2 groups showed a significant difference in the labial and lingual vertical bone levels (B-CEJ-AC and L-CEJ-AC) (Table 5). In NS group, bone levels (CEJ-AC) on the labial and lingual sides after POT decreased by 0.84 ± 0.96 mm and 1.81 ± 1.69 mm, respectively, and the difference is statistically significant. However, in the LLAC group, bone levels(CEJ-AC) on the labial and lingual sides increased significantly by 2.93 ± 2.83 mm and 2.83 ± 2.32 mm, respectively after POT (Table 5).
The BFR of above CEJ-4 mm (coronal region), CEJ-4 mm to CEJ-8 mm (midroot region), and CEJ-8 mm to apical (apical region) was 41.94 ± 26.41%, 65.20 ± 44.93%, and 76.62 ± 75.18%, respectively. The further the distance to the apical root, the higher the BFR. The BFR in the lingual apical region was the highest, significantly different from those of the other regions(Table 6).
Discussion
Skeletal Class III patients who require orthodontic-orthognathic treatment often have proclined upper incisors and retroclined lower incisors in various sagittal directions. Orthodontic decompensation should be applied during the presurgical orthodontic stage to correct these compensated tooth positions and achieve the best surgical results [2]. In individuals with skeletal Class III malocclusion and long-face syndrome, a common occurrence is the narrowing mandibular symphysis. This is perhaps attributed to the increased facial height characteristic of these patients [20]. Consequently, this problem limits the range of orthodontic tooth movement of lower anterior teeth. When the tooth exceeds the limit of alveolar bone remodeling, periodontal complications, such as attachment loss and gingival recession, may occur [6,7,8].
Presently, labial AC has been widely used in the orthodontic-orthognathic treatment of Class III patients, and its effects on soft and hard tissues have been extensively confirmed [9,10,11,12,13]. However, the risk of alveolar bone height reduction, dehiscence, gingival recession, and apical root exposure on the lingual side remains unmitigated [21]. Previous studies have shown that the height of alveolar bone on labial and lingual sides of lower incisors decreased during labially inclined movement. Guo et al. [18] conducted a meta-analysis on the changes of alveolar in maxillary and mandibular anterior teeth during orthodontic treatment. The results showed that in non-extraction cases, when mandibular incisors moved to labial direction, vertical alveolar bone loss was significant on the labial side (0.97 mm) and lingual side (0.86 mm). Ma et al. [15] found that during the process of labial inclination of lower anterior teeth in skeletal Class III patients, the height of labial and lingual sides significantly decreased, with an average decrease of 2.78 ± 2.29 mm and 3.09 ± 2.52 mm, respectively. Bone thickness and bone area on both sides decreased, too.
Consistent with previous studies [15, 21, 22], the alveolar bone height and bone contour area on the lingual side significantly decreased in the NS group before the orthognathic operation in this study. Similarly, during LLAC process in 19 patients, we observed varying degrees of bone fenestration and dehiscence on the labio-lingual sides of the lower anterior teeth. This finding underscores the necessity for lingual AC in these patients. This study demonstrated that after LLAC, the lower anterior teeth with thin alveolar bone in the labial and lingual sides or two-thirds of the root engage the labial and palatal cortical plates (Kan, Class IV), and the bone level and contour area of labial-lingual alveolar bone were significantly increased. The lingual bone formation was similar to that of the labial side.
The difference of patient selection in two groups and study results in this study suggested that in skeletal Class III patients, the decision to undergo AC should depends on the condition of the basal bone in the mandibular anterior teeth. To avoid unnecessary trauma, LLAC is only indicated when both labial and lingual alveolar bones are insufficient, dehiscenced or fenestrated. In this study, only patients with the distance of CEJ-AC more than 4 mm or labio-lingual alveolar bone thickness less than 0.5 mm, and a specific range of sagittal movement is required during the orthodontic process were considered to have LLAC.
Labial alveolar bone area can be significantly increased by AC after presurgical orthodontic treatment. Ma et al. [21] found that before orthognathic surgery, the labial alveolar bone area in the AC group increased by 8.32 ± 5.91 mm², whereas on the lingual side, the alveolar bone area decreased by 6.14 ± 5.31 mm². In this study, after performing LLAC on the lower anterior teeth, the labial alveolar bone area increased by 8.48 ± 4.59 mm². Simultaneously, the lingual alveolar bone area also increased by 8.00 ± 6.10 mm², indicating that this surgical method effectively increases hard tissue on both sides of the lower anterior teeth. The result showed that after LLAC, the augmented bone area allows for more predictable presurgical decompensation and favorable orthognathic surgical outcomes. This increased alveolar bone volume clearly enhances post-treatment stability and the overall quality of the orthodontic results, supporting additional tooth movements without periodontal side effects.
There have been no previous literature reports on the osteogenic efficiency of AC. This study’s results show that the further the distance to the apical root, the higher the BFR. Specifically, the lingual coronal region has the lowest BFR at 35.20 ± 21.79%, while the lingual apical region has the highest BFR at 86.62 ± 98.83%. Possible reasons for these results are as follows: (1) during the decompensation of mandibular anterior teeth, the teeth tilt to the labial side. The angle between the root and the base of the labial alveolar bone is less than 180°, which is conducive to the stability of the bone graft material. Conversely, the angle between the root and the base of the lingual alveolar bone is greater than 180°, which is not conducive to the stability of the bone graft material and may affect the regeneration efficiency of the coronal hard tissue; (2) during the surgical process, the soft tissue on the lingual side is looser and more mobile than on the labial side, potentially influencing the stability and integration of the bone graft material; (3) The traction force generated by tongue movement during the healing process may also affect the surgical area, compromising the stability of the bone graft material and ultimately affecting the BFR. In this study, the method of folding the barrier membrane inward in the root direction was used to prevent root displacement of bone graft materials. However, it may not completely eliminate this process. This finding suggests that sufficient thickness of bone graft material should be ensured at a location closer to the CEJ during surgery to achieve ideal hard tissue regeneration postoperatively. Finally, the average BFR on the labial side was 59.51%, which may be lower than the true value due to the apical root moving towards the lingual side. The average BFR on the lingual side was 61.89%, and due to the sagittal movement of the lower anterior teeth, the true value may be higher than this estimate.
Labial AC significantly increased the soft and hard tissue on the labial side without causing loss of periodontal attachment, gingival recession, or open gingival embrasures [23, 24]. Its safety has been preliminarily verified. However, lingual AC for the lower anterior teeth is difficult and high-risk, and there is currently a lack of systematic clinical research to prove its efficacy. Due to the presence of vital blood vessels and glandular tissues, such as the sublingual gland ducts, submental artery branches, and sublingual artery branches, the lingual side of the lower anterior teeth is often considered a restricted area for periodontal surgery. Tomljenovic et al. [25] reviewed 27 cases of fatal bleeding after oral implant surgery. Among them, 21 cases occurred on the lingual side of the mandibular anterior teeth area. The bleeding was caused by damage to the central or lateral lingual canal of the lingual bone plate in the lower anterior teeth area during the preparation process of the mandibular implant cavity, resulting in damage to the submental artery or the branch of the lingual artery that runs through it. The anatomy of 100 adult cadavers by Loukas et al. [26] showed that the central mandibular lingual canal was mostly located between the central incisors (98%). In this study, all patients who underwent LLAC surgery had CBCT scans performed presurgically to determine the depth of the central and lateral lingual canals. During the intraoperative flap-flipping process, the lingual periosteum was kept intact, and the flap depth did not exceed 5 mm from the natural apical root to avoid damaging the blood vessels in the central lingual canal of the mandible. To reduce the tension of the lingual soft tissue, the tip of a blade was used to finely cut the lingual periosteum, followed by a blunt detacher to avoid damaging the blood vessels, nerves, and glandular ducts within the lingual soft tissue. This study confirmed the feasibility of AC on the lingual side of the lower incisors. None of the nineteen subjects in the LLAC group experienced significant bleeding during or after the surgery. There were no complications such as abnormal neural sensation or saliva secretion following the surgery. After lingual bone grafting, the floor of the mouth became slightly shallower, but it did not cause difficulty in swallowing, breathing, or speech disorders for the patients.
LLAC presents challenges to the soft tissue blood supply, healing effects, and postoperative aesthetics in surgical areas. This study employed a modified preserved gingival papilla incision technique. The flap was meticulously elevated, coronally repositioned, and finely positioned to enhance the early wound healing index (EHI). Two weeks postoperatively, 17 subjects achieved an EHI of 1, with no instances of open wounds. Additionally, LLAC did not lead to gingival recession or open gingival embrasures, aligning with our previous findings on the effects of labial AC [24]. These results suggest that simultaneous LLAC can enhance postoperative soft tissue aesthetics.
To achieve the best surgical results and reduce complications, the authors propose the following suggestions. 1.Timing of surgery: the width of the gingival papilla is a crucial factor affecting wound healing in the gingival papilla area. Therefore, surgery should be scheduled after preoperative orthodontic treatment to alleviate dental crowding, thereby improving the chances of early wound healing. 2. Minimally invasive techniques: use minimally invasive instruments for flap flipping during surgery to maintain the integrity of the gingival papilla as much as possible. 3. Tension reduction and suturing: ensure complete intraoperative tension reduction, employ bilateral suspension sutures, and use intermittent sutures to achieve incision tension dispersion and tight alignment. 4. Gingival thickness and bone Loss: gingival thickness and the level of bone loss impact the healing process. Patients with thick gingiva and mild bone loss tend to heal better. 5. Operation time: the operation time should not exceed 60 min.
In summary, the author believes that in skeletal Class III patients, the decision to undergo AC primarily hinges on the condition of the basal bone in the mandibular anterior teeth. If the patient possesses ample alveolar bone, ensuring the tooth root remains within the alveolar bone during orthodontic tooth movement, AC may not be required. However, if there is insufficient labial alveolar bone, labial AC is recommended. LLAC is indicated when both labial and lingual alveolar bone are inadequate, dehiscenced or fenestrated. However, this study was historically controlled and did not include a control group at the beginning of the study. Subsequent randomized clinical trial experiments may be needed to validate these results further. This study’s observation period was before orthognathic surgery, and further observation is required for the long-term efficacy of LLAC.
Conclusion
During the presurgical orthodontic treatment for patients with alveolar bone thickness of the labial and lingual sides of the lower anterior teeth of < 0.5 mm, LLAC can significantly increase the labio-lingual alveolar bone contour area of the mandibular anterior teeth, to facilitate healthy periodontal tissue and foundation of safe orthodontic decompensation in skeletal Class III patients.
Data availability
No datasets were generated or analysed during the current study.
References
Nimigean VR, Nimigean V, Bencze MA, Dimcevici-Poesina N, Cergan R, Moraru S (2009) Alveolar bone dehiscences and fenestrations: an anatomical study and review. Rom J Morphol Embryol 50:391–397
Worms FW, Isaacson RJ, Speidel TM (1976) Surgical orthodontic treatment planning: profile analysis and mandibular surgery. Angle Orthod 46:1-25. https://doi.org/10.1043/0003-3219(1976)046%3C0001:sotppa%3E2.0.co;2
Jing WD, Xu L, Li XT, Xu X, Jiao J, Hou JX et al (2021) Prevalence of and risk factors for alveolar fenestration and dehiscence in the anterior teeth of Chinese patients with skeletal class III malocclusion. Am J Orthod Dentofac Orthop 159:312–320. https://doi.org/10.1016/j.ajodo.2019.11.018
Chung CJ, Jung S, Baik HS (2008) Morphological characteristics of the symphyseal region in adult skeletal class III crossbite and openbite malocclusions. Angle Orthod 78:38–43. https://doi.org/10.2319/101606-427.1
Kaya Y, Alkan Ö, Keskin S (2017) An evaluation of the gingival biotype and the width of keratinized gingiva in the mandibular anterior region of individuals with different dental malocclusion groups and levels of crowding. Korean J Orthod 47:176–185. https://doi.org/10.4041/kjod.2017.47.3.176
Pereira-Stabile CL, Ochs MW, de Moraes M, Moreira RW (2012) Presurgical incisor inclination in patients with Class III dentofacial deformities treated with orthognathic surgery. Br J Oral Maxillofac Surg 50:533–536. https://doi.org/10.1016/j.bjoms.2011.10.016
Choi YJ, Chung CJ, Kim KH (2015) Periodontal consequences of mandibular incisor proclination during presurgical orthodontic treatment in Class III malocclusion patients. Angle Orthod 85:427–433. https://doi.org/10.2319/021414-110.1
Rothe LE, Bollen RM, Herring SW, Herring SW, Chaison JB, Chen CS et al (2006) Trabecular and cortical bone as risk factors for orthodontic relapse. Am J Orthod Dentofac Orthop 130:476–484. https://doi.org/10.1016/j.ajodo.2005.03.023
Lee JB, Baek SJ, Kim M, Pang EK (2020) Correlation analysis of gingival recession after orthodontic treatment in the anterior region: an evaluation of soft and hard tissues. J Periodontal Implant Sci 50:146–158. https://doi.org/10.5051/jpis.2020.50.3.146
Murphy KG, Wilcko MT, Wilcko WM, Ferguson DJ (2009) Periodontal accelerated osteogenic orthodontics: a description of the surgical technique. J Oral Maxillofac Surg 67:2160–2166. https://doi.org/10.1016/j.joms.2009.04.124
Wilcko MT, Wilcko WM, Pulver JJ, Bissada NF, Bouquot JE (2009) Accelerated osteogenic orthodontics technique: a 1-stage surgically facilitated rapid orthodontic technique with alveolar augmentation. J Oral Maxillofac Surg 67:2149–2159. https://doi.org/10.1016/j.joms.2009.04.095
Sun L, Yuan L, Wang B, Zhang L, Shen G, Fang B (2019) Changes of alveolar bone dehiscence and fenestration after augmented corticotomy-assisted orthodontic treatment: a CBCT evaluation. Prog Orthod 20:7. https://doi.org/10.1186/s40510-019-0259-z
Ma HM, Lyu HM, Xu L, Hou JX, Wang XX, Li WR et al (2023) Effect of augmented corticotomy-assisted presurgical orthodontic treatment on alveolar bone fenestration and dehiscence in skeletal class III patients. J Dent Sci 18:997–1007. https://doi.org/10.1016/j.jds.2022.12.005
Lee KM, Kim YI, Park SB, Son WS (2012) Alveolar bone loss around lower incisors during surgical orthodontic treatment in mandibular prognathism. Angle Orthod 82:637–644. https://doi.org/10.2319/081711-526.1
Ma H, Li W, Xu L, Hou J, Wang X, Ding S et al (2021) Morphometric evaluation of the alveolar bone around central incisors during surgical orthodontic treatment of high-angle skeletal class III malocclusion. Orthod Craniofac Res 24:87–95. https://doi.org/10.1111/ocr.12408
Wilcko MT, Wilcko WM, Bissada NF (2008) An Evidence-Based Analysis of Periodontally Accelerated Orthodontic and osteogenic techniques: a synthesis of scientific perspectives. Semin Orthod 14:305–316. https://doi.org/10.1053/j.sodo.2008.07.007
Lu Y, Liu H, Liu J, Chen M (2022) Augmented corticotomy on the lingual side in mandibular anterior region assisting orthodontics in protrusive malocclusion: a case report. Med (Kaunas) 581181. https://doi.org/10.3390/medicina58091181
Guo Runzhi Z, Liwen H, Menglong et al (2021) Alveolar bone changes in maxillary and mandibular anterior teeth during orthodontic treatment: a systematic review and meta-analysis [J]. Orthod Craniofac Res 24(2):165–179
Kan JY, Roe P, Rungcharassaeng K, Patel RD, Waki T, Lozada JL et al (2011) Classification of sagittal root position in relation to the anterior maxillary osseous housing for immediate implant placement: a cone beam computed tomography study. Int J Oral Maxillofac Implants 26:873–876
Beckmann SH, Kuitert RB, Prahl-Andersen B, Segner D, The RP, Tuinzing DB (1998) Alveolar and skeletal dimensions associated with lower face height. Am J Orthod Dentofac Orthop 113:498–506. https://doi.org/10.1016/s0889-5406(98)70260-4
Ma H, Lyu H, Xu L, Hou J, Wang X, Li W et al (2023) Augmented corticotomy-assisted presurgical orthodontic treatment to prevent alveolar bone loss in patients with skeletal class III malocclusion. Am J Orthod Dentofac Orthop 163:210–221. https://doi.org/10.1016/j.ajodo.2021.10.021
Wang B, Shen G, Fang B, Yu H, Wu Y (2013) Augmented corticotomy-assisted presurgical orthodontics of class III malocclusions: a cephalometric and cone-beam computed tomography study. J Craniofac Surg 24:1886–1890. https://doi.org/10.1097/scs.0b013e3182a245b3
Jing WD, Jiao J, Xu L, Hou JX, Li XT, Wang XX et al (2020) Periodontal soft- and hard-tissue changes after augmented corticotomy in Chinese adult patients with skeletal Angle class III malocclusion: a non-randomized controlled trial. J Periodontol 91:1419–1428. https://doi.org/10.1002/jper.19-0522
Xu X, Wu JQ, Jiang JH, Liang C, Wang XE, Jing WD et al (2020) Periodontal effect of periodontally accelerated osteogenic orthodontics in skeletal Angle Class III: a nonrandomized, controlled trial. Int J Periodontics Restor Dent 40:e169–e177. https://doi.org/10.11607/prd.4545
Tomljenovic B, Herrmann S, Filippi A, Kuhl S (2016) Life–threatening hemorrhage associated with dental implant surgery: a review of the literature. Clin Oral Implants Res 27:1079–1084. https://doi.org/10.1111/clr.12685
Loukas M, Kinsella CR Jr, Kapos T, Tubbs RS, Ramachandra S (2008) Anatomical variation in arterial supply of the mandible with special regard to implant placement. Int J Oral Maxillofac Surg 37:367–371. https://doi.org/10.1016/j.ijom.2007.11.007
Funding
This study was supported by the New Technology and New Therapeutics of Peking University School and Hospital of Stomatology (PKUSSNCT-22A12) and Capital’s Funds for Health Improvement and Research, CFH (#2024-2-4103).
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to the conception and design of the study. J.L, Y.L, Y.F, and XN.H have been involved in data collection. J.L, X.X, Y.L, L.X and JX.H wrote the main manuscript text. Y.F, and XN.H prepared Figs. 1, 2, 3 and 4; Tables 1, 2, 3 and 4. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Research Ethics Committee of Peking University Health Science Center (approval no PKUSSIRB-202277090) and conducted following the Helsinki Declaration of 1975, as revised in 2013. The study was registered in the National Health Security Information Platform / Medical Research Registration and Filing System (www.medicalresearch.org.cn) [Medical Research Filing Number MR-11-22-007414]. Notably, all protocols were performed following the approved guidelines and regulations, and written informed consent was obtained from all participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, J., Li, Y., Fu, Y. et al. Simultaneous labial and lingual augmented corticotomy assisted presurgical orthodontics in class III patients: the morphological aspects of the mandibular anterior ridge with cone-beam computed tomography. Clin Oral Invest 28, 529 (2024). https://doi.org/10.1007/s00784-024-05805-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-024-05805-0