Abstract
Increasing the proportion of culturally and linguistically diverse (CALD) health practitioners is identified as one strategy to address healthcare disparities that individuals from minority or under-represented backgrounds experience. However, professional and institutional cultures and structures are known to contribute to the challenges for CALD practitioners who work in dominant culture practice contexts. This scoping review used the theory of Legitimate Peripheral Participation to describe and interpret literature about the experiences of CALD health practitioners in view of informing strategies to increase their representation. A systematised search was conducted across four allied health, medicine and nursing databases. Following abstract and full text screening, articles which fit the inclusion criteria (n = 124) proceeded to data extraction. Categories relating to the experiences of practitioners were extracted, and three themes were identified that were subsequently theoretically interpreted: Discrimination, Consequences and Hierarchy. Discrimination functioned as a barrier to CALD practitioners being legitimised and able to participate equally in healthcare practice, retaining their position at the periphery of the practice community; Consequences reinforced this peripheral position and further impeded legitimation and participation; and Hierarchy was maintained through structures that reinforced and reproduced these barriers. The findings summarise how these barriers are reinforced through the intersections of professional and racial hierarchies, and highlight a need for strategies to address discrimination and structures that marginalise CALD practitioners’ identity, practices and participation in their health professional communities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
The professionalisation of medicine, nursing and allied health has contributed to improving patient safety, increasing accountability, and expanding knowledge (Gunderman & Streicher, 2012; Khalili et al., 2014). However, the resultant professional cultures may also perpetuate pre-existing inequities, as knowledge generated by professionalisation derives from the gender, class and racial hierarchies of the context in which they develop (Grosfoguel, 2002; Khalili et al., 2014). Understanding how practitioners from under-represented backgrounds operate within the dominant culture contexts of their health professions assists to shine light on both the nature and impact of this; and enables the unpacking of the structures that sustain these hierarchies from the perspectives of the individuals most affected by them. This review critically examines the literature describing experiences of health practitioners from culturally and/or linguistically diverse (CALD) backgrounds and their experiences in dominant culture healthcare settings. In this paper, health professionals who are culturally and linguistically diverse include those from populations who are not from the dominant cultural and/or linguistic population of the country in which they practice or work. This may include individuals from racial/ethnic/cultural backgrounds that differ to the dominant group within a country, and/or those who speak a home language that differs from the official language of the country, or of health practice. This definition is intended to capture how individuals who are not from the dominant culture/ethnicity/race/language of a country experience healthcare practice, and is not limited to practice in white, English-speaking contexts.
In Western countries, a lack of diversity, not just in the health workforce, but in organisational and leadership roles has led to a system that is designed by and for the dominant white population, and disadvantages minority groups (Abrahams et al., 2019; Betancourt et al., 2003). Whilst many professional bodies have prioritised strategies to recruit and retain CALD practitioners (e.g. American Association of Colleges of Nursing, 2019; Australian Physiotherapy Association, 2020; Canadian Medical Association, 2021; Royal College of General Practitioners, 2021), to date, actions have failed to ensure health professions represent the communities they serve (Colby & Ortman, 2015). Existing research suggests that the experiences of CALD practitioners are underreported and misunderstood (Wyatt et al., 2021), and limited evidence that CALD health workforce participation has substantially increased suggests that current strategies to problematise and draw solutions may be failing to address deeply recursive social structures (Kyere & Fukui, 2023). Health workforce diversity has been addressed in recent review studies that have mapped workforce diversity (e.g. physician workforce Silver et al., 2019); surgical workforce (Burks et al., 2022); and broader health workforce, including nursing and allied health (Wilbur, et al., 2020), and in studies that have critically examined racialized organisational structures that impede workforce diversity (Kyere & Fukui, 2023). These review studies have examined the implications of continued poor workforce diversity on healthcare outcomes for CALD minority populations, but have not explored the CALD health practitioner’s experiences in practice within dominant culture healthcare settings. A synthesis of this latter literature may illuminate how, where and why structures and hierarchies of dominant cultures in healthcare are most impactful, and how CALD individuals respond and adapt to accommodate their experiences. These insights are critical, and largely missing voices in problematising why health workforce diversity remains stubbornly unaddressed, and to inform education, interventions and culture change strategies.
In this scoping review study, literature describing the experiences of CALD practitioners in dominant practice contexts is interpreted using the theory of Legitimate Peripheral Participation (LPP) (Lave & Wenger, 1991). This theory posits that learning is an outcome of participating in situated practice communities. Individuals commence as members at the periphery of their community, develop and demonstrate relevant knowledge and skills through participating in practice, and eventually progress towards acceptance as legitimate, full members. As such, the community sanctions permitted knowledges, practices and identities, which enable these to be replicated. Full membership then, reflects the desire of individuals to participate, but also relies on individuals being legitimised and accepted by the internal hierarchy of the community (Davies, 2005). This necessitates individuals to undertake a process of becoming a certain kind of person -a full participant, where their fundamental identity within the community is also (re)constructed (Lave & Wenger, 1991).
These dynamics of participation, legitimacy and hierarchy, as presented in LPP, provide a framework to describe CALD practitioners’ experiences within their practice communities. This scoping review study therefore aims to review the literature regarding the experiences of CALD practitioners working within health practice contexts, using LPP as an explanatory framework.
Methods
Study design
Scoping review methodology was considered appropriate for this study due to the diverse knowledges and positionalities related to the research aim, and the varied nature of the literature (Thomas et al., 2020). The grey literature was considered particularly important, as a means of gathering first-person accounts of CALD health practitioners, and to reduce the impact of publication bias borne from structures that preference dominant culture perspectives (Mulimani, 2019). A scoping review was conducted, informed by the frameworks described by Levac et al. (2010) and Arksey and O’Malley (2005). This review further drew on the work of Westphaln et al. (2021) in using a team-based, mixed-methods approach, and in applying a theoretical approach, using LPP to interpret the data. The research team were from the health professions of radiography, nursing and speech-language pathology; and were from Persian, Chinese and Anglo-Australian backgrounds. In this scoping review, the sociocultural theory of Legitimate Peripheral Participation was used as a theoretical and reflexive heuristic that helped to centre the subjectivist worldview of each researcher (Chambers et al., 2018; Meyer & Ward, 2014; Thomas et al., 2020), and purpose the knowledge synthesis within a critical sociocultural framework. This use of theory enabled the research team to examine and interpret the literature for concepts related to participation, legitimacy and hierarchy; an approach observed in other scoping review studies that have critically explored concepts of cultural safety, structural racism and healthcare disparities, where applying theory, paired with a reflexive approach, enables a critical methodology that can also produce knowledge discovery (Chambers, et al., 2018; Marcewicz, et al., 2022; Zupan et al., 2021). In this review, the use of theory also enabled the research team to challenge their biases, borne from their situation within the very healthcare structures that were being examined.
Inclusion and exclusion criteria were informed by related literature, intending to capture articles describing the experiences of qualified, practicing health practitioners of CALD background as shown in Table 1. The search terms were intentionally broad, aiming to capture empirical and review studies, and grey literature (Levac et al., 2010). To represent contemporary practice experience, literature published prior to 2000 was excluded, but the language and/or country of publication was not limited. Health professions that did not require a minimum Bachelor, three year qualification were excluded, to ensure the ‘healthcare assistant’ and enrolled nurse or carer populations were not captured, as the research team perceived that power relations may impact this population differently to those in healthcare professions. To capture experiences broadly, there were no limits applied to the nature of the reported experiences, CALD health practitioner’s years from qualification, or their practice environment(s). This review did not explore the experiences of First Nations peoples, who have distinct historical and contemporary contexts that are imperative to recognise in order that they are effectively addressed (Pham et al., 2021). CALD populations were identified according to the a) ethnic groups sorted according to majority status categories in ‘The World Factbook: Field Listing—Ethnic groups’ (Central Intelligence Agency, n.d.); and where included literature indicated that participants’ language differed to the preferred language of the healthcare setting.
Search strategy
Search terms as shown in Table 2 and Appendix A were co-constructed with a medical librarian, and the search executed with Medline, Scopus, Emcare and CINAHL databases. The first 200 articles were screened as a pilot to test and refine the search strategy. The primary search was conducted in May 2021, and updated in August 2022. Final search results were imported into Endnote (Clarivate, 2011) and subsequently into Covidence (Veritas Health Innovation, 2021) and duplicates removed. A search for the grey literature was completed in Google, using analogous search terms and limited to the first 200 results (Haddaway, et al., 2015). Cross referencing the results identified that the grey literature yield was entirely represented in the database search, as the article type was not restricted in the search strategy, and a differentiated study selection procedure was not required for the grey literature.
Study selection
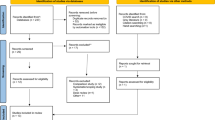
Abstract screening was conducted by two independent reviewers. Conflicts (n = 303) were discussed by the reviewers (Levac et al., 2010), and inclusion and exclusion criteria further refined. The search results represented in the Fig. 1 PRISMA chart yielded 337 articles for full text review, which then excluded a further 223 articles. Snowball sampling identified two additional articles, and one of these was included. There were 124 articles included for data extraction.
Charting, summarising and synthesising the data
Demographic and methodological data were extracted from the included articles and analysed with descriptive statistics to broadly describe the data. Qualitative coding of the results from included studies was conducted using the conventions of Kiger and Varpio (2020) which guided textual familiarisation, coding, reviewing and defining the themes in accordance with the research question. The first author initially re-read each of the included articles, recording memos and reflective notes about how the text addressed the research question. Qualitative data that were identified as describing experiences of CALD health practitioners were then inductively coded to ensure the focus of qualitative analysis remained centred on CALD health practitioners, particularly as some articles included both CALD participants and those from the dominant culture. Each passage of relevant literature was read and annotated with a ‘code’ and grouped into categories to derive broader patterns of meaning. This was an active process whereby the first author undertook interpretation and analysis to order the data in a way that derived meaning and answered the research question, and the research team then generated and discussed potential themes in order to gain consensus and ensure that they accurately represented the coded data (Kiger & Varpio, 2020). Themes were then cross-referenced with the raw data extracts to ensure they were grounded in the data. Themes were subsequently theoretically interpreted using LPP which was operationalised into the concepts of legitimacy, peripherality and participation. These core concepts of LPP were used as a heuristic to determine if the theory explained the results (Lave & Wenger, 1991; Meyer & Ward, 2014). Finally, patterns and relationships to the theory were described to synthesise conclusions in line with the research aims.
This research was conducted in Australia, by a female research team including CALD and white-Anglo members. The research team collaborated to interpret literature that were expressed through different health professional, geographical and cultural contexts, however, this was limited by the team’s knowledge about the population/s of the regions referred. To identify CALD groups, and in interpreting the data, the team referred to The World Factbook: Field Listing—Ethnic groups’ (Central Intelligence Agency, n.d.), and took a reflexive position to examine and bracket potential cultural and professional power relations, and to sense-check the data analysis from multiple perspectives. Nonetheless, we acknowledge that bias, and the values of own practice communities may have influenced the findings. The findings were presented in a multidisciplinary research forum that included a range of student and qualified health practitioners from nursing and allied health (including several participants from CALD backgrounds), and participants from a range of professions provided feedback that the findings helped to explain their experiences. The two CALD practitioner researchers (second and third authors) further verified that the themes aligned with their understanding of their own practice experiences.
Results
The literature yielded was prominently from English speaking countries, most frequently from the United States and Britain, followed by Australia (Table 3), using qualitative methodologies that gathered data via semi-structured interviews (Table 4). The grey literature was prominently represented by commentary and opinion pieces authored by CALD practitioners. Most articles investigated broad workplace experiences (n = 41) or multiple workplace features (n = 19), with others investigating experiences of discrimination (n = 16), career progression (n = 14), mentoring (n = 1) and professional identity formation (n = 1), and these concepts were strongly represented in the themes.
The experiences of CALD nurses (n = 66) and medical practitioners (n = 30) were most frequently reported (78% of included articles). Other health professions included psychology (n = 11), social workers (n = 6), dentistry (n = 1) and physiotherapy (n = 1). Four articles reported the experiences of practitioners from multiple professions.
A range of racial/ethnic groups were represented across professions (Table 5), and some articles included participants from different backgrounds, including articles that included both participants from CALD backgrounds and those from the dominant culture. Table 6 shows that Asian practitioners from a range of countries were most frequently included (n = 42), followed by North American (n = 31) and African (n = 30) participants. However, much of the included literature did not attribute any country of origin (n = 64) or ethnicity (n = 18). Articles prominently explored the adjustment experiences of immigrant CALD practitioners (n = 119) and less frequently reflected experiences of practitioners who were from a racial, ethnic or cultural minority population in their home country (n = 37). Over a third of studies about practitioners who were from a racial or cultural minority group in their home country included participants from multiple racial groups (n = 14).
Qualitative themes
Theme 1: discrimination
As the most prominent theme, ‘Discrimination’ captured the overarching experiences of CALD practitioners, whilst also relating to the two remaining themes of ‘Consequences’ and ‘Hierarchies’. Three subthemes comprised the ‘Discrimination’ theme: ‘Overt Discrimination’, ‘Covert Discrimination’ and ‘Barriers to addressing Discrimination’.
Overt discrimination
CALD practitioners described discrimination as occurring overtly and stemming from several workplace sources. Discriminatory experiences with patients often took the form of refusal of care due to the practitioner’s race or other identifiers (Frimpong, 2016; Nunez-Smith et al., 2007; Tuttas, 2015) extending to racist remarks and harassment (Cabral & Smith, 2011; Mbarushimana & Robbins, 2015; Wingfield & Chavez, 2020). Experiences of overt discrimination from patients were reported in settings where the practitioner was treating white patients (Wingfield & Chavez, 2020), those with mental health (Cottingham et al., 2018) or drug and alcohol problems, such as in emergency departments (Frimpong, 2016; Wingfield & Chavez, 2020).
‘He was a very difficult patient in that he was racially and sexually inappropriate with staff... he called me a “nigger,” a “humpbacked monkey” several times.’ (Cottingham et al., 2018, p150)
Several studies reported experiences of overt discrimination from colleagues and supervisors including verbal assault, marginalisation and bullying due to race, culture or communication (Frimpong, 2016; Lewenson & Graham-Perel, 2020; Tuttas, 2015; Zhong et al., 2017), and instances of colleagues leaving or refusing to work alongside a CALD practitioner (Lewenson & Graham-Perel, 2020; Newland, 2020). In one study, more than 40% of CALD nurses perceived some form of racial harassment from colleagues (Tuttas, 2015).
‘The most painful discrimination occurred in the forms of jokes to demean Africans. “I like to laugh with people, but not at the expense of others; how do you laugh when a colleague shouts ‘Ebola!’ as you walk towards him in a hospital?”’ (Frimpong, 2016 p76)
Covert discrimination
Covert discrimination was reported as including perceived resentment and distrust from colleagues (Mapedzahama et al., 2012) feeling unsupported in decisions (Frimpong, 2016) being ‘surveilled’, excessively watched and monitored by peers and supervisors (Mapedzahama et al., 2012; Xiao et al., 2014) with an undercurrent of fault finding (Cottingham et al., 2018; Holmes & Grech, 2015), and unfair or undue criticism or complaint from colleagues (Alexis & Vydelingum, 2005; Pedrotti & Burnes, 2016). This scrutiny resulted in stress that impacted performance of CALD practitioners (Holmes & Grech, 2015; Mapedzahama et al., 2012), described as ‘perpetuating the myth of incompetence’ (Mapedzahama et al., 2012 p157).
‘[workmates] will be following you like they don’t trust what you are doing, or they can even ask you … a question which really annoys like: Can you do blood pressure? Obviously! How could you ask that question? And that person will repeat, keep asking you the same question!’ (Mapedzahama et al., 2012 p160).
In some studies, CALD practitioners reported being subjected to unfair treatment or unequal workload distribution, for example being allocated difficult patients, working overtime or unpopular shifts (Alexis & Vydelingum, 2005; Frimpong, 2016), and lacking acknowledgement despite undertaking the same or additional workload as their peers (Alexis & Vydelingum, 2005; Tuttas, 2015). CALD practitioners were further marginalised through unspoken rules and group norms that contributed to their lacking confidence with social and ‘lunchroom’ interactions, This resulted in…’an overwhelming sense of isolation and separateness from… colleagues’ (Frimpong, 2016, p72) that was exacerbated if they lacked experience with informal English (Xiao et al., 2014).
CALD practitioners reported experiencing microaggressions founded in unacknowledged racialised stereotypes relating to their inferiority or ‘backwardness’, or assumptions about their educational background and (in)competence (Cottingham et al., 2018; Nunez-Smith et al., 2007). Black practitioners reported being perceived as ‘lazy’, ‘not serious’ (Wingfield & Chavez, 2020) p43, ‘stupid’ (Frimpong, 2016) p78 or from underdeveloped nations (Mapedzahama et al., 2012).
‘Some of them [have] no clue … they think we came from trees, that we used to live with monkeys, and then we just got off the tree and boarded an aeroplane and came here.’ (Mapedzahama et al., 2012) p158
Other microaggressions reflected covert behaviours that generated discomfort for the CALD practitioner, including instances of colleagues using racial slurs in their presence (Wingfield & Chavez, 2020), or asking culturally inappropriate questions (Tuttas, 2015).
Barriers to challenging discrimination
Denial, acceptance and the minimisation of workplace discrimination presented barriers for CALD practitioners to challenge discrimination (Mbarushimana & Robbins, 2015; Nunez-Smith et al., 2007; Pedrotti & Burnes, 2016; Tuttas, 2015). The literature identified workplace actions that conveyed an underlying acceptance and condonation of discrimination.
'I was a triage nurse in the emergency room for many years and the nurse manager would transfer patients to other nurses when patients openly said they wouldn’t allow the African nurse to triage them' (Frimpong, 2016, p78).
The absence of clear organisational policy or procedures presented additional barriers to challenging discrimination (Mbarushimana & Robbins, 2015; Nunez-Smith et al., 2007), further compounded as CALD practitioners reported uncertainty about how to manage covert or less explicit discrimination that was difficult to prove (Frimpong, 2016). Conversely, some articles reported CALD practitioners resisted actions they perceived would result in negative repercussions. For example, one medical practitioner reported that challenging discrimination would ‘get him in trouble’ (Anderson, 2020, p1610) and described experiences throughout his career of being warned of marginalisation for speaking out (Anderson, 2020). Similarly, multiple studies about immigrant health practitioners described visa and financial pressures as barriers to challenging discrimination (Pedrotti & Burnes, 2016; Tuttas, 2015; Xiao et al., 2014), and these factors also enabled exploitative working conditions (Tuttas, 2015).
‘The first priority for immigrant nurses is to survive and gain employment. As a consequence they are often more accepting of ‘discrimination’, less likely to be assertive, or critical of their peers, or to take on leadership roles.’ (Xiao et al., 2014, p646)
The impacts of discrimination and the challenges for CALD practitioners in acting on or removing themselves from such experiences were situated within a struggle to be recognised as having legitimacy in contributing to their healthcare settings. These experiences often manifested in the marginalisation of CALD practitioners, who were not always fully accepted as healthcare members.
Theme 2: consequences
The theme ‘Consequences’ captured the cognitive, emotional, behavioural, interpersonal and self-perceptual adjustments that CALD practitioners enacted through experiencing discrimination; or transitioning into workplaces. These adjustments are broadly categorised into ‘professional identity’, and ‘behaviours and coping strategies’.
Professional identity
In this study, professional identity is used to describe internal changes that were reported to occur as a consequence of CALD practitioners’ experiences. Many of these changes impacted negatively, however, positive adjustments that empowered individuals within their workplace were also identified.
CALD practitioners often reported that workplace discrimination impacted their self-perception as practitioners. Multiple studies reported affective consequences, including decreased self-efficacy (Cottingham et al., 2018; Pedrotti & Burnes, 2016; Tuttas, 2015), increased self-doubt and rumination (Beagan, et al. 2022; Cottingham et al., 2018), erosion of confidence (Zhong et al., 2017) and feelings of inadequacy (Alexis & Vydelingum, 2005). Studies also reported that CALD practitioners who continued to work in the context of discrimination experienced internal conflict and emotional exhaustion that interfered with their work (Beagan, et al., 2022; Cottingham et al., 2018; Pedrotti & Burnes, 2016).
‘“I’ve encountered four instances of systemic racism and it’s only eleven o’clock in the morning. How do you think I’m doing?”…Really, really heavy… I am currently in a space of moral fatigue’ (Beagan, et al. 2022, p7).
These feelings of inadequacy and low self-efficacy were partnered with perceptions of needing to ‘prove’ oneself to colleagues and make additional efforts to be accepted (Mbarushimana & Robbins, 2015; McKenzie-Mavinga, 2005; Pedrotti & Burnes, 2016).
‘I have to think that I will one day I will be right there. I have to prove myself that I can be one of them’ (Alexis & Vydelingum, 2005, p469).
Experiences of discrimination negatively impacted CALD practitioners’ perceptions of their profession, their work and job satisfaction (Pedrotti & Burnes, 2016; Ying, 2015; Zhong et al., 2017), and were associated with thoughts of leaving the profession (Frimpong, 2016) or returning to home country (Zhong et al., 2017).
‘Chinese nurses… got stuck in their career, failed to fit into the host community, submitted to their families’ demands, or simply filled with longing for home, where they were not identified as outsiders’ (Zhong et al., 2017, p108).
Conversely, in some studies CALD practitioners reported satisfaction from aspects of their work that were less enjoyed by their peers. In particular, they derived meaning from the intercultural environments in which they worked (Mbarushimana & Robbins, 2015), in utilising culture and language skills (Hu, 2016), or engaging with patients from minority backgrounds (Nunez-Smith et al., 2007). In these aspects, CALD practitioners identified themselves as assets to the healthcare team (Xiao et al., 2014).
‘Being a member of that culture gave me insights to handle that situation in a culturally sensitive manner.… Serving the Chinese-speaking community has given me much fulfillment. It is an obligation that I feel in my heart.’ (Hu, 2016, p200).
Behaviours and coping strategies
CALD practitioners developed behaviours and coping strategies to respond to discrimination. These adjustments were empowering or disempowering, either facilitating the contesting of barriers and stereotypes, or the acceptance of discrimination and struggle.
CALD practitioners reported using strategies that increased their control or agency, that were ‘empowering’ despite compromising features of their cultural, racial or gender identity (Anderson, 2020; O’Neill, 2011) as they facilitated their ‘fit’ within their professional communities. These strategies included using formal professional attire and titles (Anderson, 2020; Pedrotti & Burnes, 2016), altering communication and speech (Almutairi et al., 2013; Zhong et al., 2017), adapting to cultural expectations of professionalism, such as being chatty with patients (O’Neill, 2011), or modifying public behaviours to align with western values (Zhong et al., 2017).
CALD practitioners also generated professional support networks, including subcultures of similar racial, cultural and language groups within their workplaces to manage their exclusion (Beagan, et al., 2022; Xiao et al., 2014) and protect their cultural identity (Alexis & Vydelingum, 2005). These informal networks were noted across nursing and medical, and allied health professions enabling CALD practitioners to cope with discrimination when institutional support was lacking (Alexis & Vydelingum, 2005; Beagan, et al., 2022; Cottingham et al., 2018; Duffin, 2012; Lewenson & Graham-Perel, 2020; Nunez-Smith et al., 2007; Pedrotti & Burnes, 2016).
BME (black and minority ethnic) colleagues also supported each other in carrying out their work… to say, you know, ‘This is what I’m being faced with. What would you advise?’’ (Mbarushimana & Robbins, 2015, p147).
Several studies reported career changes as empowering CALD practitioners to manage discrimination or leave unsupportive workplaces. Whilst career changes were often perceived negatively, they empowered individuals to reclaim agency (Anderson, 2020; Nunez-Smith et al., 2007).
‘I transferred from the emergency room to intensive care after my first year because I couldn’t tolerate the discrimination in the department. It came from the patients, EMT workers and physicians.’ (Frimpong, 2016, p78).
CALD practitioners were also empowered through intentionally ignoring or disregarding discrimination to minimise its burden and reclaim control (Cottingham et al., 2018; Nunez-Smith et al., 2007), actively challenging discrimination by speaking out or educating those around them (Anderson, 2020; Beagan et al., 2022; Mbarushimana & Robbins, 2015), or making conscious efforts to highlight their strengths (Hu, 2016; Mapedzahama et al., 2012).
‘I make a point…of interjecting the importance of race and culture and cultural competence in how we interface with patients especially’ (Nunez-Smith et al., 2007 p48).
However, CALD practitioners reported being disempowered when they were unable to express or manage the consequences of discrimination (Almutairi et al., 2015; Frimpong, 2016; Holmes & Grech, 2015; O’Neill, 2011), with some employing strategies to cope that resulted in professional isolation (Frimpong, 2016) or withdrawing to subordinate roles (Holmes & Grech, 2015; O’Neill, 2011) that impacted their self-identity.
‘Some relinquished responsibilities and critical thinking skills, a safe position where the risk of communication breakdown would be minimised.’ (O’Neill, 2011, p1124).
CALD practitioners also reported physical and psychological consequences of workplace discrimination, manifesting in sleep problems, weight loss and chest pain (Holmes & Grech, 2015) and psychological disturbances (Zhong et al., 2017).
The categories that described the Consequences reflected the peripherality of the position of many CALD practitioners in their practice communities. Consequences and strategies could further distance CALD practitioners from others in their workplace, or adaptively respond to better ‘fit’ into their community.
Theme 3: hierarchy
The final theme identified racial hierarchies that existed within and between health professions, where some professions and individuals were ascribed to hold more power and status than others. These concepts intersected, as CALD practitioners reported their experiences as influenced by both professional status and race.
Racial hierarchy
Intersections between professional hierarchies and CALD identity were often reported (Almutairi et al., 2015; Cottingham et al., 2018; McGinnis & Moore, 2009; Nunez-Smith et al., 2007; Tuttas, 2015). For example, CALD nurses reported more frequent experiences of overt discrimination than CALD doctors, regardless of their gender (Agrawal et al., 2018; Nunez-Smith et al., 2007; Wingfield & Chavez, 2020). The concept of hierarchy also captured inter-racial power differences, that elevated career and work opportunities for ethnic groups with high status, and resulted in further experiences of discrimination for groups with lower status (Almutairi et al., 2015; Frimpong, 2016; Tuttas, 2015).
'Some nationalities also look down on the Filipinos as if they are stupid, less knowledge like that'. (Almutairi et al., 2015, p 21).
CALD practitioners across professions reported stereotypical associations about the nature of their role, skills and work, including assumptions that they were employed as cleaners, unregistered nurses or healthcare assistants (Cottingham et al., 2018; O’Neill, 2011; Pedrotti & Burnes, 2016; Wingfield & Chavez, 2020).
‘As a black physician you keep getting mistaken for other people….Some of my white female [colleagues] were always getting mistaken for nurses and everyone thought that was funny. But I was always mistaken for the person who brought the trays or the janitor person. So I think the things for which they mistake us is much more disparate for black women.’ (Nunez-Smith et al., 2007, p48).
Several articles reported that CALD practitioners’ qualifications, experience and their professional skills were under-valued compared with their peers (de Figueiredo, 2011; Mbarushimana & Robbins, 2015; Tuttas, 2015; Xiao et al., 2014; Zhong et al., 2017). Career progression was impeded by bureaucracy that prevented skill utilisation (Alexis & Vydelingum, 2005; de Figueiredo, 2011) and marginalisation or lack of promotion (Alexis & Vydelingum, 2005; Johnson, et al., 2021; Tuttas, 2015). Racial hierarchies were reported in hiring and recruitment structures (Tuttas, 2015; Wingfield & Chavez, 2020; Yeowell, 2013).
‘There is no person in leadership or management or a VP role of a visible minority. None. Not one manager. So I’m pretty angry at that. I’m angry at the fact that they won’t even acknowledge that that’s a problem.’ (Beagan et al., 2022, p6).
These hierarchies limited leadership opportunities afforded to CALD practitioners (Anderson, 2020; Duffin, 2012; Wingfield & Chavez, 2020), underpinning pay differences, where white followed by Asian health practitioners were reported as earning more than Hispanic and Black health practitioners despite equivalent education and experience (McGinnis & Moore, 2009; Waldman, 2000), and white university graduates were preferred over CALD graduates (Wingfield & Chavez, 2020). However, CALD practitioners also reported feeling obliged to employers who provided them work opportunities, rendering many unable to discuss issues of workplace discrimination (Mbarushimana & Robbins, 2015).
Across the health professions, CALD practitioners reported being funnelled into ‘diversity’ related workloads or unfulfilling career pathways (Anderson, 2020; Erhunmwunsee et al., 2019; Mbarushimana & Robbins, 2015; Pedrotti & Burnes, 2016). This was likened to a ‘cultural taxation’ whereby the practitioner experiences increased workload or burden as an ‘ambassador’ for their cultural group (Pedrotti & Burnes, 2016 p145), leading to reflections of being ‘just a diversity statistic?’(Anderson, 2020 p1610). Whilst these interventions often intended to address workplace disparities, or shine light on the skills that CALD practitioners bring to diverse populations, they may also perpetuate existing hierarchies.
‘Participants also described being involuntarily “cast” into race-based roles in the workplace… include[ing] helping with minority physician recruitment, serving on numerous diversity committees, intervening in difficult situations with minority colleagues or trainees, and assisting nonminority colleagues in the care of minority patients.’ (Nunez-Smith et al., 2007 p48).
Professional and gender hierarchies
Intersections between professional hierarchies with gender-based power imbalances were prominently reported in the medical and nursing professions, and this amplified experiences of discrimination. The character traits associated with medicine were considered masculine, i.e. including competence, intelligence and strength, that were protective against discrimination.
“It is hard being a physician of color because you have the issue of race and the issue of power. When you are a physician, you have a power position that other people don’t have, whether they are of the same race or different race or whatever” (Nunez-Smith et al., 2007) p47.
Conversely, in professions considered feminine, including nursing, societal stereotypes characterise deference, submission and caring, that can generate perceptions of a lack of professionalism (Shannon et al., 2019; Wingfield & Chavez, 2020). In nursing, male CALD nurses have reported a ‘glass escalator’ effect in which they identified greater likelihood of promotion to leadership positions (Frimpong, 2016). Conversely, female CALD nurses reported greater frequency of discrimination, experiencing the ‘emotional double shift’ of race and gender (Cottingham et al., 2018). As such, having a high-status profession and being male gender may have a protective effect from discrimination experiences for CALD practitioners.
The theme of hierarchy embodies notions of ‘power over’ that for CALD practitioners relate inherently to their capacity to participate in the activities of their practice community, be recognised as having a legitimate and valued contribution, and be enabled to progress and demonstrate leadership from the centre of the community.
Discussion
This scoping review describes the experiences of CALD practitioners in dominant culture healthcare settings, revealing themes of discrimination, consequences, and hierarchy. The included literature was overwhelmingly derived from Western countries, in the fields of medicine and nursing, and predominantly describing the experiences of CALD practitioners from African, Asian and North American backgrounds. There was comparatively little literature pertaining to other health professions. In this discussion, the theory of Legitimate Peripheral Participation (Lave & Wenger, 1991) is used to conceptualise how CALD practitioners are facilitated or hindered in becoming legitimate members of their professional community, and the identities they inhabit to pursue this.
Discrimination was a barrier to participation and legitimacy, with CALD practitioners reporting both positive and negative personal and structural consequences. Lave and Wenger (1991) theorised that learning and integration into a practice community occurs when individuals can access legitimate opportunities to participate. Instances of overt discrimination resulted in reduced practice opportunities that maintained the position of CALD practitioners at the periphery of the community. For example, reallocating racially abusive patients from CALD practitioners reinforces and legitimises these patient behaviours and concurrently impedes opportunities for CALD practitioners to demonstrate complex practice skills, which may contribute to challenges in career progression. Experiences of covert discrimination perpetuated notions of illegitimacy and incompetence through stereotyping, negative associations, and bias (Lennartz et al., 2019; Wingfield & Chavez, 2020). Consequently, CALD practitioners reported experiencing social exclusion within their practice communities – both self-initiated and community-instigated. This positioning at the periphery of the practice community, may further legitimise negative bias in hiring, employment and career progression opportunities (Tuttas, 2015; Wingfield & Chavez, 2020; Yeowell, 2013). Conversely, affirmative action employment and progression interventions that intend to facilitate professional diversity may leave CALD practitioners feeling fraudulent or indebted for their place in their practice community (Standing & Baume, 2001). These perceptions of ‘being permitted’ entry, may ascribe CALD practitioners to tolerate discrimination and structures that hold their position at the periphery of their community.
Identity adjustments that CALD practitioners enacted in response to discrimination either enhanced their legitimacy as members of their practice community or compounded their position at the periphery. Identity formation is critical for professional socialisation, as new community members acquire the knowledge, skills and identity attributes that are both endorsed by, and permit acceptance into the community (Davies, 2005; Lave & Wenger, 1991). The structural consequences of discrimination and resulting negative self-perceptions reduce CALD practitioners’ opportunities to participate and effectively demonstrate the practice attributes required for endorsement (Davies, 2005). Conversely, CALD practitioners who adjust to fit within their professional community, such as through their masking of culturally-derived behaviours, dress and discourses may be perceived as more legitimate, as they demonstrate identity attributes aligned with the dominant culture community. Such adjustments may be rewarded with further participation opportunities that improve the position and stature of the CALD practitioner, whilst further perpetuating dominant culture practices and biases (Attrill et al., 2022). In both scenarios, this compromise of the CALD person’s values and identity to respond to the values or perceptions of the dominant community are reported as psychologically depleting, and may contribute to professional attrition (Frimpong, 2016; Nunez-Smith et al., 2007; Pedrotti & Burnes, 2016; Tuttas, 2015; Zhong et al., 2017).
The findings also suggested that some CALD practitioners derive satisfaction from serving diverse communities and often bridge cultural and linguistic barriers, verifying research that identifies CALD practitioners as potential cultural brokers with patients (Berger, 2008; Cabral & Smith, 2011; Nápoles-Springer et al., 2005). They reported their shared language and lived experiences as facilitating connection with CALD patients that elevated the quality of care (Hu, 2016; Mbarushimana & Robbins, 2015). Prior research suggests that “giving back” to CALD communities provides meaning that is foundational in constructing the professional identities of CALD practitioners (Wyatt et al., 2021). These identities appear to differ from those of the dominant practice community, and evidence exists that the skills of CALD practitioners in working with CALD patients are both valued (Xiao et al., 2014) or create further marginalisation (Mbarushimana & Robbins, 2015; Nunez-Smith et al., 2007). Lave and Wegner (1991) theorised that communities can adopt knowledges and practices of new members, and these new practices may become legitimised if they have value and are repeated through members’ participation. Celebrating and elevating the knowledge and skills that CALD practitioners contribute may inform and model culturally responsive practices for the broader practice community. This may in-turn legitimise CALD practitioners, whilst also protecting against the deleterious impacts of discrimination (Hu, 2016; Mapedzahama et al., 2012; Nunez-Smith et al., 2007). Recognition that these knowledge, skills and attributes are critical to address healthcare inequities may reduce the ‘cultural-taxation’ (Pedrotti & Burnes, 2016 p145) that CALD practitioners report in enacting their advocacy for diverse communities. This requires these behaviours to be legitimised, valued and endorsed at all levels of the community, including those who benefit from professional hierarchies and high status.
The professional and racial hierarchies identified in this study reiterate boundaries that CALD practitioners experience in participating in healthcare practice. These boundaries act to reinforce dominant culture knowledge and practices that hold CALD practitioners at the periphery of their community. Wingfield and Chavez (2020) noted that these barriers become more prominent as CALD practitioners seek increasingly senior opportunities. Davies (2005) observed that an individual’s identity within a community is mediated by their relationship with the recursive meanings and social structures of that community, and by extension, the world in which it exists. Power and internal hierarchies that present and are maintained in organisational and leadership structures may present greater identity and value conflicts for CALD practitioners, generating further barriers to their participation and success in these positions. Thus, the poor visibility of CALD practitioners in leadership is not only a symptom of hierarchy, but perpetuates hierarchy, where dominant culture practitioners who are members of high-status professions retain power, and power subsequently diminishes through intersections between professional, racial and gender hierarchies. These persistent and intersecting power structures are also visible in the education programs that CALD health professional students encounter during training, and are particularly pervasive during clinical practice training experiences (Attrill, et al., 2022; Joseph et al., 2021). In this study, as for previous research about CALD students, CALD health practitioners often demonstrated adaptive strategies within the environments in which their power imbalance was impactful, but these strategies often sought to reduce their personal impact from being discriminated against – there were few examples where adaptive responses enabled the participants’ greater personal power or success. It is likely that future strategies to address workforce diversity will need to accommodate the full trajectory from student training to workforce participation, and address power as it intersects across and through hierarchies.
Further marginalisation is likely experienced by practitioners with added disadvantage, such as through experiencing disability. These multiple intersections create new dynamics of power and forms of discrimination that cannot be addressed by attending to each element in isolation (Collins, 1990). This review suggests that these intersections compounded the CALD practitioners’ experiences of discrimination and their resultant impacts on participation and legitimation. Additionally, whilst this review was largely grounded in literature from medicine and nursing, the broader summarised literature suggests that these intersectional issues are common to other health professions, including social work (Mbarushimana & Robbins, 2015), physiotherapy (Yeowell, 2013) and psychology (Pedrotti & Burnes, 2016). Meaningful change will require these intersectional barriers that reinforce and sustain dominant health professional hierarchies and cultures to be reflexively examined with actions designed with CALD practitioners and grounded in their perspectives (Wyatt et al., 2021).
Limitations
Clustering CALD practitioners together for this research helped to amplify their experiences in dominant culture healthcare settings. However, the cultural, ethnic, linguistic and historical backgrounds of individuals and populations included in this research are diverse and their reductive grouping inadvertently diminishes important distinguishing features, and masks differences in their needs and experiences. The intention of this review was not to diminish the experiences of particular cultural or ethnic groups, or indeed, individuals, but rather to provide evidence of their interactions within dominant practice constructs to inform practice and policy change. Whilst this review intended to amplify the perspectives of CALD practitioners, the research team acknowledge that their own subjectivity and bias may have had the affect of amplifying or quelling this through the interpretative process. The grey literature produced a large volume of first-person CALD practitioner accounts which were highly valued inclusions in this research, and we acknowledge that more extensive grey literature searching may have produced further variety of perspectives.
Conclusion
CALD practitioners are often participating in healthcare communities whose professional identities are structured around a Western, English-speaking framework. Given the need to embody these practice-situated identities to progress and gain experiences for legitimacy, the barriers to legitimation are greater for practitioners who are not from the dominant culture. The findings of this review highlighted the structural nature of discrimination that CALD practitioners experience, and their entrenched and disempowered positions within recursive professional health hierarchies (Attrill et al., 2022). To respond, institutional policy and procedures should address the multiple, intersectional configurations of discrimination that inform the experiences of CALD practitioners. However, meaningful change can be achieved only through critically examining the structures and practices, and the dominant discourses and narratives that sustain institutional and health professional cultures and marginalise those at the periphery (Wyatt et al., 2021).
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Abrahams, K., Kathard, H., Harty, M., & Pillay, M. (2019). Inequity and the professionalisation of speech-language pathology. Professions and Professionalism. https://doi.org/10.7577/pp.3285
Abu Rabia, R., Hendel, T., & Kagan, I. (2021). Views of Bedouin physicians and nurses on nursing as a profession in Israel: There is more to strive for. Nursing & Health Sciences, 23(2), 498–505. https://doi.org/10.1111/nhs.12834
Agnew, T. (2019). As BME people we need to put ourselves forward. Nursing Standard, 34(1), 14–17.
Agrawal, R., Foresti, K., Rajadurai, J., & Zubaran, C. (2018). Assessing workplace discrimination among medical practitioners in Western Sydney. Australasian Psychiatry, 26(5), 491–495. https://doi.org/10.1177/1039856218772248
Alexis, O., & Shillingford, A. (2015). Internationally recruited neonatal nurses. International Journal of Nursing Practice, 21, 419–425. https://doi.org/10.1111/ijn.12284
Alexis, O., & Vydelingum, V. (2005). The experiences of overseas black and minority ethnic registered nurses in an English hospital: a phenomenological study. Journal of Research in Nursing, 10(4), 459–472.
Alexis, O., Vydelingum, V., & Robbins, I. (2006). Overseas nurses’ experiences of equal opportunities in the NHS in England. Journal of Health Organization and Management, 20(2), 130–139. https://doi.org/10.1108/14777260610661529
Ali, P. A., & Johnson, S. (2017). Speaking my patient’s language: Bilingual nurses’ perspective about provision of language concordant care to patients with limited English proficiency. Journal of Advanced Nursing, 73(2), 421–432. https://doi.org/10.1111/jan.13143
Almutairi, A. F., Gardner, G., & McCarthy, A. (2013). Perceptions of clinical safety climate of the multicultural nursing workforce in Saudi Arabia: A cross-sectional survey. Collegian, 20(3), 187–194. https://doi.org/10.1016/j.colegn.2012.08.002
Almutairi, A. F., McCarthy, A., & Gardner, G. E. (2015). Understanding cultural competence in a multicultural nursing workforce: Registered nurses’ experience in Saudi Arabia. Journal of Transcultural Nursing, 26(1), 16–23. https://doi.org/10.1177/1043659614523992
Alshehry, A. S., Alquwez, N., Almazan, J., Namis, I. M., Moreno-Lacalle, R. C., & Cruz, J. P. (2019). Workplace incivility and its influence on professional quality of life among nurses from multicultural background: A cross-sectional study. Journal of Clinical Nursing., 28(13–14), 2553–2564.
American Association of Colleges of Nursing. (2019). Enhancing diversity in the workforce. Retrieved October 25 from https://www.aacnnursing.org/news-information/fact-sheets/enhancing-diversity
Anderson, C. T. M. (2020). Taking back our voices—#HumanityIsOurLane. New England Journal of Medicine, 383(17), 1609–1611. https://doi.org/10.1056/NEJMp2021291
Anionwu, E. (2017). White managers must tackle discrimination. Nursing Standard, 31(21), 27.
Argueza, B. R., Saenz, S. R., & McBride, D. (2021). From diversity and inclusion to antiracism in medical training institutions. Academic Medicine, 96(6), 798.
Arriaza, P. (2015). Spanish language self-efficacy beliefs among Spanish-speaking social workers: Implications for social work education. Journal of Social Work Education, 51(3), 550–565.
Arksey, H., & O’Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. https://doi.org/10.1080/1364557032000119616
Attrill, S., Davenport, R., & Brebner, C. (2022). Professional socialisation and professional fit: Theoretical approaches to address student learning and teaching in speech-language pathology. International Journal of Speech Language Pathology, 24(5), 472–483. https://doi.org/10.1080/17549507.2021.2014965
Australian Physiotherapy Association. (2020). What Physiotherapy looks like in 2020. Australian Physiotherapy Association. Retrieved 15 October 2021 from https://australian.physio/inmotion/what-physiotherapy-looks-2020#:~:text=Recent%20registrant%20data%20from%20the,by%20Victoria%2C%2025%20per%20cent
Beagan, B. L., Sibbald, K. R., Bizzeth, S. R., & Pride, T. M. (2022). Systemic racism in Canadian occupational therapy: A qualitative study with therapists. Canadian Journal of Occupational Therapy (1939), 89(1), 51–61. https://doi.org/10.1177/00084174211066676
Berger, J. T. (2008). The influence of physicians’ demographic characteristics and their patients’ demographic characteristics on physician practice: Implications for education and research. Academic Medicine, 83(1), 100–105. https://doi.org/10.1097/ACM.0b013e31815c6713
Betancourt, J. R., Green, A. R., Carrillo, J. E., & Ananeh-Firempong, O., II. (2003). Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public Health Reports, 118(4), 293–302. https://doi.org/10.1093/phr/118.4.293
Brooks, M. E. (2016). Voices of perseverance: A phenomenological exploration of the life histories of female African-American registered nurses. Eastern Michigan University (Dissertation).
Brown, T., Liu, J. X., & Scheffler, R. M. (2009). Does the under-or overrepresentation of minority physicians across geographical areas affect the location decisions of minority physicians? Health Services Research, 44(4), 1290–1308.
Burks, C. A., Russell, T. I., Goss, D., et al. (2022). Strategies to increase racial and ethnic diversity in the surgical workforce: A state of the art review. Otolaryngology-Head and Neck Surgery, 166(6), 1182–1191. https://doi.org/10.1177/01945998221094461
Cabral, R. R., & Smith, T. B. (2011). Racial/ethnic matching of clients and therapists in mental health services: A meta-analytic review of preferences, perceptions, and outcomes. Journal of Counseling Psychology, 58(4), 537–554. https://doi.org/10.1037/a0025266
Canadian Medical Association, (2021). Equity and diversity in medicine. Retrieved October 25 from https://www.cma.ca/physician-wellness-hub/topics/equity-and-diversity-in-medicine
Central Intelligence Agency. (n.d.). The world Factbook: Field listing—Ethnic groups. Retrieved from https://www.cia.gov/the-world-factbook/field/ethnic-groups/
Chambers, L. A., Jackson, R., Worthington, C., et al. (2018). Decolonizing scoping review methodologies for literature with, for, and by Indigenous peoples and the African diaspora: Dialoguing with the tensions. Qualitative Health Research, 28(2), 175–188. https://doi.org/10.1177/1049732317743237
Champion, A. (2021). Representation Matters. Increasing diversity in oral and maxillofacial surgery. Journal of Oral and Maxillofacial Surgery, 79(4), 743–744. https://doi.org/10.1016/j.joms.2020.12.005
Chang, H., Hutchinson, C., & Gullick, J. (2021). Pulled away: The experience of bilingual nurses as ad hoc interpreters in the emergency department. Ethnicity & Health, 26(7), 1045–1064.
Charleston, I. V. L., Spears, R. C., & Flippen, C. (2020). Equity of African American men in headache in the United States: A perspective from African American headache medicine specialists (part 1). Headache: the Journal of Head and Face Pain., 60(10), 2473–2485.
Chen, P. G., Nunez-Smith, M., Bernheim, S. M., Berg, D., Gozu, A., & Curry, L. A. (2010). Professional experiences of international medical graduates practicing primary care in the United States. Journal of General Internal Medicine., 25, 947–953.
Clarivate. (2011). Endnote 20. In from https://endnote.com/product-details
Cohen, B. (2013). Torah true: the lived experience of orthodox jewish registered nurses. ProQuest Dissertations Publishing.
Coghill, Y. (2013). Voices. Nursing Standard, 28(14), 26.
Colby, S., & Ortman, J. M. (2015). Projections of the size and composition of the US population: 2014 to 2060. US Department of Commerce, Economics and Statistics Administration, US.
Collins, E. M. (2004). Career mobility among immigrant registered nurses in Canada: Experiences of Caribbean women (Doctoral dissertation).
Collins, P. H. (1990). Black feminist thought: Knowledge, consciousness, and the politics of empowerment. Unwin Hyman.
Connor, J. B., & Miller, A. M. (2014). Occupational stress and adaptation of immigrant nurses from the Philippines. Journal of Research in Nursing., 19(6), 504–515.
Cortés-Guiral, D., Mayol, J., & Wexner, S. D. (2021). Diversity in surgery: A historical, international, and contemporary perspective. Current Surgery Reports, 9(5), 14.
Cooper, S., Wilson-Stark, K., Peterson, D. B., O’Roark, A. M., & Pennington, G. (2008). Consulting competently in multicultural contexts. Consulting Psychology Journal: Practice and Research, 60(2), 186.
Cottingham, M. D., & Andringa, L. (2020). “My color doesn’t lie”: Race, gender, and nativism among nurses in the Netherlands. Global Qualitative Nursing Research, 7, 233339362097295–2333393620972958. https://doi.org/10.1177/2333393620972958
Cottingham, M. D., Johnson, A. H., & Erickson, R. J. (2018). “I can never be too comfortable”: Race, gender, and emotion at the hospital bedside. Qualitative Health Research, 28(1), 145–158. https://doi.org/10.1177/1049732317737980
Cowan, R., Dessources, K., Stasenko, M., Lee, J., Iasonos, A., Roche, K. L., Chapman-Davis, E., & Brown, C. (2021). Listening to our peers so we can listen to our patients: A survey of racism experienced by gynecologic oncologists. Gynecologic Oncology, 162, S14–S15.
Crawford, T., Roger, P., & Candlin, S. (2016). “Are we on the same wavelength?” International nurses and the process of confronting and adjusting to clinical communication in Australia. Communication & Medicine, 13(3), 263–274.
Criddle, T. R., Gordon, N. C., Blakey, G., & Bell, R. B. (2017). African Americans in oral and maxillofacial surgery: Factors affecting career choice, satisfaction, and practice patterns. Journal of Oral and Maxillofacial Surgery., 75(12), 2489–2496.
Das, S. (2020). Multilingual matrix: Exploring the process of language switching by family therapists working with multilingual families. Journal of Family Therapy, 42(1), 39–53. https://doi.org/10.1111/1467-6427.12249
Davies, B. (2005). Communities of practice: Legitimacy not choice. Journal of Sociolinguistics, 9(4), 557–581. https://doi.org/10.1111/j.1360-6441.2005.00306.x
de Figueiredo, J. M. (2011). The making of a multicultural psychiatrist. Transcultural Psychiatry, 48(1–2), 160–176. https://doi.org/10.1177/1363461510388544
Deegan, J., & Simkin, K. (2010). Expert to novice: Experiences of professional adaptation reported by non-English speaking nurses in Australia. The Australian Journal of Advanced Nursing, 27(3), 31–37.
Duffin, C. (2012). Having the views of BME nurses is vital to improve patient care. Nursing Standard, 27(5), 12–13.
Dyrbye, L. N., West, C. P., Sinsky, C. A., Trockel, M., Tutty, M., Satele, D., Carlasare, L., & Shanafelt, T. (2022). Physicians’ experiences with mistreatment and discrimination by patients, families, and visitors and association with burnout. JAMA Network Open, 5(5), e2213080.
El Gindy, G. (2006). Cultural competence. Are NCLEX testing policies culturally insensitive? Minority Nurse. Summer, 48–51.
Engstrom, D. W., Piedra, L. M., & Min, J. W. (2009). Bilingual social workers: Language and service complexities. Administration in Social Work, 33(2), 167–185. https://doi.org/10.1080/03643100902768832
Erhunmwunsee, L., Backhus, L. M., Godoy, L., Edwards, M. A., & Cooke, D. T. (2019). Report from the workforce on diversity and inclusion—The society of thoracic surgeons members’ bias experiences. Annals of Thoracic Surgery, 108(5), 1287–1291. https://doi.org/10.1016/j.athoracsur.2019.08.015
Estacio, E. V., & Saidy-Khan, S. (2014). Experiences of racial microaggression among migrant nurses in the United Kingdom. Global Qualitative Nursing Research, 1, 2333393614532618–2333393614532618. https://doi.org/10.1177/2333393614532618
Esterhuizen, J., Van Rensburg, G. H., & Tjallinks, J. E. (2013). A historical perspective on the professional development of black South African nurses: 1908–1994. Africa Journal of Nursing and Midwifery, 15(2), 16–29.
Etowa, J. B., Sethi, S., & Thompson-Isherwood, R. (2009). The substantive theory of surviving on the margin of a profession. Nursing Science Quarterly, 22(2), 174–181. https://doi.org/10.1177/0894318409332781
Foong, L. H. (2022). Anti-racism in the emergency department: Navigating clinician experiences of racism. Emergency Medicine Australasia, 34(1), 116–119.
Frimpong, D. K. (2016). Men in a female-dominated profession: The lived experiences of Ghanaian male nurses in the United States. Men in a Female-dominated Profession: The Lived Experiences of Ghanaian Male Nurses in the United States, 1–1. http://ezproxy.flinders.edu.au/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=cin20&AN=124418495&site=ehost-live
Gasiorek, J., & Van de Poel, K. (2018). Language-specific skills in intercultural healthcare communication: Comparing perceived preparedness and skills in nurses’ first and second languages. Nurse Education Today, 61, 54–59.
Gould, W., Kirkley, R.. (2017). The emergence of diverse male nurse anesthetists: Increasing cultural competence and improving the gender gap. Minority Nurse. Winter/Spring 23–31.
Grosfoguel, R. (2002). Colonial difference, geopolitics of knowledge, and global coloniality in the modern/colonial capitalist world-system. Review (fernand Braudel Center), 25(3), 203–224.
Gunderman, R. B., & Streicher, D. A. (2012). Accountability in Professionalism. American Journal of Roentgenology, 198(4), W344–W346. https://doi.org/10.2214/AJR.11.7767
Haddaway, N. R., Collins, A. M., Coughlin, D., & Kirk, S. (2015). The role of google scholar in evidence reviews and its applicability to grey literature searching. PLoS ONE, 10(9), e0138237. https://doi.org/10.1371/journal.pone.0138237
Hagey, R., Choudhry, U., Guruge, S., Turrittin, J., Collins, E., & Lee, R. (2001). Immigrant nurses’ experience of racism. Journal of Nursing Scholarship, 33(4), 389–394. https://doi.org/10.1111/j.1547-5069.2001.00389.x
Handley, A. (2015). The long road to equality. Nursing Standard, 30(5), 64–65.
Harrison, G. (2007). A postcolonial perspective on language and difference in social work: Bilingual practitioners working in the linguistic borderlands. European Journal of Social Work, 10(1), 73–88. https://doi.org/10.1080/13691450601143682
Henry, L. (2007). Institutionalized disadvantage: Older Ghanaian nurses’ and midwives’ reflections on career progression and stagnation in the NHS. Journal of Clinical Nursing, 16(12), 2196–2203. https://doi.org/10.1111/j.1365-2702.2007.02094.x
Ho, Y.-Y.C., & Coady, M. R. (2018). English as a second language nurses in the United States: Culture, communication, and needs for continuing education. Studies in Continuing Education, 40(2), 212–233. https://doi.org/10.1080/0158037X.2018.1460721
Holmes, T., & Grech, C. (2015). CaLD nurses transition to Australian tertiary hospital practice: Exposing the reality—A mixed methods study. Collegian, 22(4), 387–396. https://doi.org/10.1016/j.colegn.2014.08.001
Hu, A. (2016). Reflections: Using a second language to build a practice. Otolaryngology-Head & Neck Surgery, 154(2), 199–200. https://doi.org/10.1177/0194599815618390
Iheduru‐Anderson, K. (2020). Barriers to career advancement in the nursing profession: Perceptions of Black nurses in the United States. In Nursing Forum (vol. 55, No. 4, pp. 664–677).
Iordan, D. (2018). Eastern European immigrants’ advancement into U.S. nursing practice. ProQuest Dissertations Publishing.
Isaac, D. (2020). One size DOES NOT fit all: Black British-born mental health nurses and factors influencing their ‘national’ health service career progression. Journal of Ethnic and Cultural Studies, 7(3), 88–111.
Johnson, J., Mitchinson, L., Parmar, M., Opio-Te, G., Serrant, L., & Grange, A. (2021). Do Black, Asian and minority ethnic nurses and midwives experience a career delay? A cross-sectional survey investigating career progression barriers. Contemporary Nurse., 57(1–2), 99–112.
Jones, D. (2013). The critical need for black nurses. ABNF Journal., 24(3), 67.
Jones-Berry, S. (2016). Directors of nursing key to success of equality strategies. Nursing Management., 23(4), 6.
Joseph, O. R., Flint, S. W., Raymond-Williams, R., Awadzi, R., & Johnson, J. (2021). Understanding healthcare students’ experiences of racial bias: A narrative review of the role of implicit bias and potential interventions in educational settings. International Journal of Environmental Research and Public Health, 18(23), 12771. https://doi.org/10.3390/ijerph182312771
Khalili, H., Hall, J., & DeLuca, S. (2014). Historical analysis of professionalism in western societies: Implications for interprofessional education and collaborative practice. Journal of Interprofessional Care, 28(2), 92–97. https://doi.org/10.3109/13561820.2013.869197
Kelly, J. F., & Greene, B. (2010). Diversity within African American, female therapists: Variability in clients’ expectations and assumptions about the therapist. Psychotherapy: Theory, Research, Practice, Training., 47(2), 186.
Kiger, M. E., & Varpio, L. (2020). Thematic analysis of qualitative data: AMEE Guide No. 131. Medical Teacher, 42(8), 846–854. https://doi.org/10.1080/0142159X.2020.1755030
Ko, M., & Dorri, A. (2019). Primary care clinician and clinic director experiences of professional bias, harassment, and discrimination in an underserved agricultural region of California. JAMA Network Open, 2(10), e1913535–e1913535. https://doi.org/10.1001/jamanetworkopen.2019.13535
Kyere, E., & Fukui, S. (2023). Structural racism, workforce diversity, and mental health disparities: A critical review. Journal of Racial and Ethnic Health Disparities, 10, 1985–1996. https://doi.org/10.1007/s40615-022-01380-w
Lave, J., & Wenger, E. (1991). Situated learning: Legitimate peripheral participation. Cambridge University Press.
Le, Q., & Kilpatrick, S. (2008). Vietnamese-born health professionals: Negotiating work and life in rural Australia. Rural and Remote Health, 8(4), 1062–1062. https://doi.org/10.22605/RRH1062
Lee, S.-Y., Kim, E., & Chen, W.-T. (2010). Research strategies: Lessons learned from the studies of Chinese Americans and Korean Americans. Journal of Transcultural Nursing, 21(3), 265–270. https://doi.org/10.1177/1043659609358786
Lennartz, C., Proost, K., & Brebels, L. (2019). Decreasing overt discrimination increases covert discrimination: Adverse effects of equal opportunities policies. International Journal of Selection and Assessment, 27(2), 129–138. https://doi.org/10.1111/ijsa.12244
Levac, D., Colquhoun, H., & O’Brien, K. K. (2010). Scoping studies: Advancing the methodology. Implementation Science, 5(1), 69. https://doi.org/10.1186/1748-5908-5-69
Lévesque, M., & Negura, L. (2021). The unsuspected ties between linguistic affiliation and professional distress in healthcare social workers. Canadian Ethnic Studies, 53(1), 111–133. https://doi.org/10.1353/ces.2021.0005
Lewenson, S. B., & Graham-Perel, A. (2020). “You don’t have any business being this good”: An oral history interview with bernardine lacey. AJN American Journal of Nursing, 120(8), 40–47. https://doi.org/10.1097/01.naj.0000694564.56696.ad
Liebschutz, J. M., Darko, G. O., Finley, E. P., Cawse, J. M., Bharel, M., & Orlander, J. D. (2006). In the minority: Black physicians in residency and their experiences. Journal of the National Medical Association, 98(9), 1441–1448.
Likupe, G. (2006). Experiences of African nurses in the UK National Health Service: A literature review. Journal of Clinical Nursing, 15, 1213–1220. https://doi.org/10.1111/j.1365-2702.2006.01380.x
Likupe, G. (2015). Experiences of African nurses and the perception of their managers in the NHS. Journal of Nursing Management, 23(2), 231–241. https://doi.org/10.1111/jonm.12119
Lim, S., Boutain, D. M., Kim, E., Evans-Agnew, R. A., Parker, S., & Maldonado, N. R. (2022). Institutional procedural discrimination, institutional racism, and other institutional discrimination: A nursing research example. Nursing Inquiry., 29, e12474.
Mapedzahama, V., Rudge, T., West, S., & Perron, A. (2012). Black nurse in white space? Rethinking the in/visibility of race within the Australian nursing workplace. Nursing Inquiry, 19(2), 153–164. https://doi.org/10.1111/j.1440-1800.2011.00556.x
Marcewicz, L., Kunihiro, S. K., Curseen, K. A., Johnson, K., & Kavalieratos, D. (2022). Application of critical race theory in palliative care research: A scoping review. Journal of Pain and Symptom Management, 63(6), e667–e684. https://doi.org/10.1016/j.jpainsymman.2022.02.018
Matza, M. R., Garon, M. B., & Que-Lahoo, J. (2018). Developing minority nurse leaders: The anchor and the rope. Nursing Forum (hillsdale), 53(3), 348–357. https://doi.org/10.1111/nuf.12261
Mbarushimana, J.-P., & Robbins, R. (2015). “We have to work harder”: Testing assumptions about the challenges for black and minority ethnic social workers in a multicultural society. Practice (09503153), 27(2), 135–152. https://doi.org/10.1080/09503153.2015.1014336
McGinnis, S. L., & Moore, J. (2009). An analysis of racial/ethnic pay disparities among hospital nurses in New York city. Policy, Politics, and Nursing Practice, 10(4), 252–258. https://doi.org/10.1177/1527154409358627
McKenzie-Mavinga, I. (2005). Understanding black issues in postgraduate counsellor training. Counselling & Psychotherapy Research, 5(4), 295–300. https://doi.org/10.1080/14733140500492581
Meyer, S., & Ward, P. (2014). ‘How to’ use social theory within and throughout qualitative research in healthcare contexts. Sociology Compass, 8, 525–539.
Morris, S., Goudie, R., Sutton, M., Gravelle, H., Elliott, R., Hole, A. R., Ma, A., Sibbald, B., & Skåtun, D. (2011). Determinants of general practitioners’ wages in England. Health Economics., 20(2), 147–160.
Mulimani, P. (2019). Publication bias towards Western populations harms humanity. Nature Human Behaviour, 3, 1026–1027. https://doi.org/10.1038/s41562-019-0720-5
Myers, J. (2011). Diversity in action. Nursing Management., 18(4), 9.
Nápoles-Springer, A. M., Santoyo, J., Houston, K., Pérez-Stable, E. J., & Stewart, A. L. (2005). Patients’ perceptions of cultural factors affecting the quality of their medical encounters. Health Expectations : An International Journal of Public Participation in Health Care and Health Policy, 8(1), 4–17. https://doi.org/10.1111/j.1369-7625.2004.00298.x
Ncube, E. (2017). Influence of Leadership styles on expatriate nurses' professional integration in the UAE. ProQuest Dissertations Publishing.
Newland, J. A. (2020). #BlackLivesMatter. Nurse Practitioner, 45(9), 6–6. https://doi.org/10.1097/01.NPR.0000694732.28548.f9
Nezu, A. M. (2010). Cultural influences on the process of conducting psychotherapy: Personal reflections of an ethnic minority psychologist. Psychotherapy: Theory, Research, Practice, Training., 47(2), 169.
Nunez-Smith, M., Curry, L. A., Berg, D., Krumholz, H. M., & Bradley, E. H. (2008). Healthcare workplace conversations on race and the perspectives of physicians of African descent. Journal of General Internal Medicine, 23(9), 1471–1476. https://doi.org/10.1007/s11606-008-0709-7
Nunez-Smith, M., Curry, L. A., Bigby, J., Berg, D., Krumholz, H. M., & Bradley, E. H. (2007). Impact of race on the professional lives of physicians of African descent. Annals of Internal Medicine, 146(1), 45–51.
Nunez-Smith, M., Pilgrim, N., Wynia, M., Desai, M. M., Jones, B. A., Bright, C., Krumholz, H. M., & Bradley, E. H. (2009). Race/ethnicity and workplace discrimination: Results of a national survey of physicians. Journal of General Internal Medicine., 24, 1198–1204.
O’Neill, F. (2011). From language classroom to clinical context: The role of language and culture in communication for nurses using English as a second language—A thematic analysis. International Journal of Nursing Studies, 48(9), 1120–1128. https://doi.org/10.1016/j.ijnurstu.2011.02.008
Odusanya, S. O. E., Winter, D., Nolte, L., & Shah, S. (2018). The experience of being a qualified female BME clinical psychologist in a national health service: an interpretative phenomenological and repertory grid analysis. Journal of Constructivist Psychology, 31(3), 273–291. https://doi.org/10.1080/10720537.2017.1304301
Oladeji, L. O., Ponce, B. A., Worley, J. R., & Keeney, J. A. (2018). Mentorship in orthopedics: A national survey of orthopedic surgery residents. Journal of Surgical Education., 75(6), 1606–1614.
Olayiwola, J. N. (2016). Racism in medicine: Shifting the power. The Annals of Family Medicine., 14(3), 267–269.
Oshikanlu, R. (2020). BAME or BME—How about just being me? Nursing times, 116(8), 14.
Pedrotti, J. T., & Burnes, T. R. (2016). The new face of the field: Dilemmas for diverse early-career psychologists. Training & Education in Professional Psychology, 10(3), 141–148. https://doi.org/10.1037/tep0000120
Pendleton, J. (2017). The experiences of black and minority ethnic nurses working in the UK. British Journal of Nursing., 26(1), 37–42.
Pham, T. T. L., Berecki-Gisolf, J., Clapperton, A., O’Brien, K. S., Liu, S., & Gibson, K. (2021). Definitions of culturally and linguistically diverse (CALD): A literature review of epidemiological research in Australia. International Journal of Environmental Research and Public Health, 18(2), 737. https://doi.org/10.3390/ijerph18020737
Philip, S., Woodward-Kron, R., & Manias, E. (2019). Overseas qualified nurses’ communication with other nurses and health professionals: An observational study. Journal of Clinical Nursing, 28(19–20), 3505–3521.
Phillips, L. (2004). Take it to the top: Lynette Phillips looks at the experiences and challenges facing black and minority ethnic nursing managers in the NHS. Nursing Standard, 18(30), 96–97.
Pickersgill, F. (2004). A certain’go-get’attitude. Nursing Standard, 18(45), 20–22.
Qureshi, I., Ali, N., & Randhawa, G. (2020). British South Asian male nurses’ views on the barriers and enablers to entering and progressing in nursing careers. Journal of Nursing Management, 28(4), 892–902. https://doi.org/10.1111/jonm.13017
Robinson, D. B., Hopkins, L., James, O. P., Brown, C., Powell, A. G., Abdelrahman, T., Hemington-Gorse, S., Walsh, L., Egan, R. J., & Lewis, W. (2020). Egalitarianism in surgical training: Let equity prevail. Postgraduate Medical Journal, 96(1141), 650–654.
Robinson, O. V. (2013). Telling the story of role conflict among Black nurses and Black nursing students: A literature review. Journal of Nursing Education, 52(9), 517–524.
Royal College of General Practitioners. (2021). Equality, Diversity and Inclusion. Retrieved October 25 from https://www.rcgp.org.uk/about-us/equality-and-diversity.aspx
Ruzycki, S. M., Roach, P., Holroyd-Leduc, J., Barnabe, C., & Ahmed, S. B. (2023). Experiences and perceptions of racism and Sexism among Alberta physicians: Quantitative results and framework analysis of a cross-sectional survey. Journal of General Internal Medicine, 38(1), 165–175.
Samora, J. B., Van Heest, A., Weber, K., Ross, W., Huff, T., & Carter, C. (2020). Harassment, discrimination, and bullying in orthopaedics: A work environment and culture survey. Journal of the American Academy of Orthopaedic Surgeons, 28(24), e1097–e1104.
Silver, J. K., Bean, A. K., Slocum, C., Poorman, J. A., Tenforde, A., Blauwet, C. A., Kirch, R. A., Parekh, R., Amonoo, H. L., Zafonte, R., & Osterbur, D. (2019). Physician workforce disparities and patient care: A narrative review. Health Equity, 3(1), 360–377.
Simpson, J. M., & Ramsay, J. (2014). Manifestations and negotiations of racism and? Heterophobia? In overseas-born South Asian GPs? Accounts of careers in the UK. Diversity and Equality in Health and Care, 11(3), 177–185. https://doi.org/10.21767/2049-5471.100017
Sinkfield-Morey, T. (2019). The nursing salon experience: A salon for nurses of color. Creative Nursing, 25(4), 308–310.
Snyder, C. R., & Schwartz, M. R. (2019). Experiences of workplace racial discrimination among people of color in healthcare professions. Journal of Cultural Diversity. 26(3).
Song, J., & McDonald, C. (2021). Experiences of New Zealand registered nurses of Chinese ethnicity during the COVID-19 pandemic. Journal of Clinical Nursing, 30(5–6), 757–764. https://doi.org/10.1111/jocn.15607
Standing, H., & Baume, E. (2001). Equity, Equal Opportunities, Gender and Organisation Performance. World Health Organisation.
Sudol, N. T., Guaderrama, N. M., Honsberger, P., Weiss, J., Li, Q., & Whitcomb, E. L. (2021). Prevalence and nature of sexist and racial/ethnic microaggressions against surgeons and anesthesiologists. JAMA Surgery, 156(5), e210265.
Tan, L. L., & Denson, L. (2019). Bilingual and multilingual psychologists practising in Australia: An exploratory study of their skills, training needs and experiences. Australian Psychologist, 54(1), 13–25.
Tanega-Doster, R. (2011). Retention and ethnic diversity: An historical study of Filipino nurse migration to America during 1965–1985. ProQuest Dissertations Publishing.
Tedam, P. (2021). To shield or not to shield? There should be no question—Black African social workers experiences during COVID-19 in England. The British Journal of Social Work, 51(5), 1720–1738. https://doi.org/10.1093/bjsw/bcab107
Teran, V. G., Fuentes, M. A., Atallah, D. G., & Yang, Y. (2017). Risk and protective factors impacting burnout in bilingual, Latina/o clinicians: An exploratory study. Professional Psychology: Research and Practice, 48(1), 22.
Terry, L. M., Carr, G., & Williams, L. (2013). The effect of fluency in English on the continuing professional development of nurses educated overseas. The Journal of Continuing Education in Nursing, 44(3), 137–144.
Thomas, A., Lubarsky, S., Varpio, L., Durning, S. J., & Young, M. E. (2020). Scoping reviews in health professions education: Challenges, considerations and lessons learned about epistemology and methodology. Advances in Health Sciences Education : Theory and Practice, 25(4), 989–1002. https://doi.org/10.1007/s10459-019-09932-2
Timilsina Bhandari, K. K., Xiao, L. D., & Belan, I. (2015). Job satisfaction of overseas-qualified nurses working in Australian hospitals. International Nursing Review, 62(1), 64–74.
Trueland, J. (2012). Unequal opportunities. Nursing Standard, 27(5), 16–18.
Tuttas, C. A. (2015). Perceived racial and ethnic prejudice and discrimination experiences of minority migrant nurses: A literature review. Journal of Transcultural Nursing, 26(5), 514–520. https://doi.org/10.1177/1043659614526757
Ulloa, J. G., Viramontes, O., Ryan, G., Wells, K., Maggard-Gibbons, M., & Moreno, G. (2018). Perceptual and structural facilitators and barriers to becoming a surgeon: A qualitative study of African-American and Latino surgeons. Academic Medicine, 93(9), 1326–1334. https://doi.org/10.1097/ACM.0000000000002282
Veritas Health Innovation. (2021). Covidence systematic review software. www.covidence.org
Villarruel, A. M. (2017). A Framework for Latino nursing leadership. Nursing Science Quarterly, 30(4), 347–352. https://doi.org/10.1177/0894318417724476
Waldman, H. B. (2000). NYSDA Membership Survey provides insight into the composition of the dental profession in New York State. The New York State Dental Journal, 66(9), 24–27.
Wang, S. C., Hubbard, R. R., & Dorazio, C. (2020). Overcoming racial battle fatigue through dialogue: Voices of three counseling psychologist trainees. Training and Education in Professional Psychology, 14(4), 285.
Westphaln, K. K., Regoeczi, W., Masotya, M., Vazquez-Westphaln, B., Lounsbury, K., McDavid, L., Lee, H., Johnson, J., & Ronis, S. D. (2021). From Arksey and O’Malley and Beyond: Customizations to enhance a team-based, mixed approach to scoping review methodology. MethodsX, 8, 101375. https://doi.org/10.1016/j.mex.2021.101375
Wilbur, K., Snyder, C., Essary, A. C., Reddy, S., Will, K. K., & Saxon, M. (2020). Developing workforce diversity in the health professions: A social justice perspective. Health Professions Education, 6(2), 222–229.
Wingfield, A. H., & Chavez, K. (2020). Getting in, getting hired, getting sideways looks: Organizational hierarchy and perceptions of racial discrimination. American Sociological Review, 85(1), 31–57. https://doi.org/10.1177/0003122419894335
Wright, S. M., & Carrese, J. A. (2003). Serving as a physician role model for a diverse population of medical learners. Academic Medicine, 78(6), 623–628. https://doi.org/10.1097/00001888-200306000-00013
Wros, P. (2009). Giving voice: Incorporating the wisdom of Hispanic RNs into practice. Journal of Cultural Diversity, 16(4).
Wyatt, T. R., Balmer, D., Rockich-Winston, N., Chow, C. J., Richards, J., & Zaidi, Z. (2021). ‘Whispers and shadows’: A critical review of the professional identity literature with respect to minority physicians. Medical Education, 55(2), 148–158. https://doi.org/10.1111/medu.14295
Xiao, L. D., Willis, E., & Jeffers, L. (2014). Factors affecting the integration of immigrant nurses into the nursing workforce: A double hermeneutic study. International Journal of Nursing Studies, 51(4), 640–653. https://doi.org/10.1016/j.ijnurstu.2013.08.005
Yan, M. C. (2008). Exploring cultural tensions in cross-cultural social work practice. Social Work, 53(4), 317–328.
Yeowell, G. (2013). “Oh my gosh I’m going to have to undress”: Potential barriers to greater ethnic diversity in the physiotherapy profession in the United Kingdom. Physiotherapy, 99(4), 323–327. https://doi.org/10.1016/j.physio.2013.03.002
Ying, X. (2015). Racial and ethnic minority nurses’ job satisfaction in the U.S. International Journal of Nursing Studies, 52(1), 280–287. https://doi.org/10.1016/j.ijnurstu.2014.10.007
Zhong, Y., McKenna, L., & Copnell, B. (2017). What are Chinese nurses’ experiences whilst working overseas? A narrative scoping review. International Journal of Nursing Studies, 74, 101–111. https://doi.org/10.1016/j.ijnurstu.2017.06.009
Zupan, B., Campbell-Woods, N., & Thompson, H. (2021). Scoping review: Language assessment practices for Aboriginal and Torres Strait Islander children in Australia and guidelines for clinical practice. The Australian Journal of Rural Health, 29(6), 879–895. https://doi.org/10.1111/ajr.12766
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. There are no sources of funding to declare.
Author information
Authors and Affiliations
Contributions
SA conceptualised and supervised the research, supported the screening and analysis of the research and wrote the manuscript. MH conducted the research and wrote the thesis from which the manuscript was derived. FS completed literature screening, supported the verification of the findings and supervised the research. TL completed the secondary search and screening, supported the verification of the findings and the production of the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Harris, M., Lau-Bogaardt, T., Shifaza, F. et al. The experiences of culturally and linguistically diverse health practitioners in dominant culture practice: a scoping review. Adv in Health Sci Educ (2024). https://doi.org/10.1007/s10459-024-10359-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10459-024-10359-7