Abstract
Sexualized substance use or “chemsex” may contribute to the HIV epidemic among men who have sex with men (MSM) in Thailand. Specific patterns of chemsex use may be associated with different HIV/STI transmission risks. We examined typologies and correlates of sexualized substance use among a sample of high-risk MSM (n = 532) who had attended a private sex party or circuit party in the past three years using latent class analysis. Multinomial regression was used to adjust for variables associated with the 3-class latent class model. We identified a 3-class model as the best fitting model, which included: (1) “negligible sexualized substance users” (36.7%), who had never engaged in chemsex in the past six months; (2) “sexualized substance users” (13.9%), who had a high level of sexualized alcohol use and a wide range of other substances before or during sex in the past six months; and (3) “exclusive chemsex users” (49.4%), who predominantly used crystal methamphetamine, amyl nitrite, and erectile dysfunctional drugs before or during sex in the past six months. Compared to negligible sexualized substance users, exclusive chemsex users were more likely to be HIV-positive, more likely to have six or more sexual partners in the past six months, less likely to have condom use at last anal intercourse, and more likely to have provided sex work. Relative to negligible sexualized substance users, sexualized substance users reported more frequent online sex-seeking behaviors. These subgroups of Thai MSM have unique substance use patterns and HIV-related risk profiles, underscoring the importance of targeted HIV prevention strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In Thailand, men who have sex with men (MSM) have a disproportionately high incidence of HIV, compared to the general population (Seekaew et al., 2018; Van Griensven et al., 2013, 2022). Epidemic trends in HIV infection indicate high rates of new infections among young MSM, those who use methamphetamines and other stimulant drugs, and those who sell or exchange sex (Dunne et al., 2019; Holtz et al., 2019; Piyaraj et al., 2018; Van Griensven et al., 2022). Sexualized substance use or “chemsex” among MSM may contribute to the HIV epidemic among MSM in Thailand (Kelly-Hanku, 2021). MSM engaging in sexualized substance use often engage in condomless anal sex, which increases their vulnerability to HIV transmission (Kelly-Hanku, 2021; Maviglia et al., 2022; Wang et al., 2023; Wong et al., 2020). This heightened risk of exposure to HIV is further exacerbated by the potential for multiple sexual partners and group sex during chemsex sessions (Lim et al., 2015; Scholz-Hehn et al., 2022; Wong et al., 2020) as well as an increased likelihood of having a sexually transmitted infection (STI) (Achterbergh et al., 2020; Lim et al., 2015; Scholz-Hehn et al., 2022; Tan et al., 2021; Wong et al., 2020). Additionally, the use of drugs such as methamphetamine can lead to prolonged sexual activity, thereby increasing the duration and intensity of potential HIV exposure (Semple et al., 2009). The combination of these factors creates a perfect storm for the rapid spread of HIV among MSM engaged in chemsex in Asia, highlighting the urgent need for targeted interventions to address this critical public health concern (Van Griensven et al., 2017).
Specific combinations of substance use may lead MSM to heighten their risk of HIV and STI transmission (Achterbergh et al., 2020; Melendez-Torres et al., 2018; Scholz-Hehn et al., 2022; Tan et al., 2021; Wong et al., 2020). For example, previous studies have found that MSM having a more intense and broader range of usage of substances, particularly the use of stimulant drugs, were more likely to report living with HIV and engage in condomless anal sex (Achterbergh et al., 2020; Melendez-Torres et al., 2018; Scholz-Hehn et al., 2022; Tan et al., 2021; Wong et al., 2020). Delineating the specific patterns of drug use can shed light on MSM’s differing risk levels, to which tailored interventions can be developed to reduce harm. For example, Wong et al. found that MSM belonging to latent classes of “medium threshold” and “intense users” were more likely to take preexposure prophylaxis (PrEP) or intend to use PrEP than other drug user types. Using latent class analysis (LCA) allows researchers to identify distinct subgroups or classes within a sample based on shared characteristics or behaviors (Lanza & Rhoades, 2013). The social hierarchy and power dynamics within the subculture of sexualized substance use and chemsex among Thai MSM could expose them to different sexual risks. For example, ice parties (crystal methamphetamine is referred to as “ice” in Thai) or “hi fun” (chemsex group session) is associated with a higher social class status and elite social network among Thai MSM as opposed to “yaba” (amphetamine tablets used by Southeast Asian blue-collar workers) (Guadamuz & Boonmongkon, 2018). An LCA approach can be used to determine the heterogeneity among these socially patterned sexualized substance use patterns to identify subgroups of Thai MSM who may have unique patterns of sexualized substance use. It is especially crucial to include rare but unique substances utilized by Thai MSM to inform the construction of a more culturally nuanced LCA model, as previous studies on Asian MSM utilizing the same latent indicator variables tended to reproduce results from Europe and North America (Guerras et al., 2021; Lim et al., 2015; Tan et al., 2021; Wong et al., 2020).
This study sought to understand the typology of chemsex patterns among a sample of Thai MSM who had attended a private sex party or a circuit party in the past three years. Private sex parties and circuity parties are social venues where the use of substances is prevalent (Colfax et al., 2001; Knox et al., 2020; Meunier, 2018). Circuit parties are large-scale events primarily geared toward the gay community, characterized by multi-day dance parties held in metropolitan areas with a high density of MSM. These parties are characterized by sexualized music, sexualized performances, naked bodies, and opportunities for sexual encounters (Cheung et al., 2015). In recent years, circuit parties have gained significant popularity in Asia, with attendance growing from a few thousand participants per night in 2007 to claims of over 25,000 attendees per night in 2023 (Cheung et al., 2015; Gcircuit Songkran 2024, n.d.; White Party Bangkok 2024, n.d.). On the other hand, our team’s previous qualitative research described the socioecological risks of “ice” parties where sexual orientation, unprotected sex, and ice use were enmeshed by a social pattern of desire, self-worth, and group conformity (Guadamuz & Boonmongkon, 2018). These social venues have been identified as high HIV risk environments due to prevailing social norms that discourage condom use negotiation and disclosure of HIV serostatus (Cheung et al., 2015; Colfax et al., 2001; Meunier, 2018; O’Byrne & Holmes, 2011). The current study sought to understand the sociodemographic and behavioral characteristics and patterns of chemsex usage of Thai MSM engaged in these social venues to inform tailored interventions.
Method
Participants and Procedure
A cross-sectional anonymous online self-administered survey (n = 532) was conducted. Inclusion criteria included men who were at least 18 years old, attended private sex parties (group sex of more than three persons), attended one of the circuit parties offered in Thailand (e.g., White Party, Gcircuit party, XXO Party) in the past three years, had anal intercourse with a man in the past year, ability to read Thai, and currently residing in Thailand. Data were collected from September to December 2021, and participants were recruited with the assistance of community-based partners and social media platforms (private Line® chat groups, private Facebook® groups, and private Twitter® groups). A web-based survey was delivered using Qualtrics software (Qualtrics headquarters, Australia [www.qualtrics.com]). To ensure the quality of data and prevent fraudulent entries, only relevant online groups were sent invitation links to the survey, and data validation features from Qualtrics (2024) were employed in flagging possible fraudulent responses, such as abnormal response speed, defined as more than two standard deviations from the median duration, and non-human activities. Upon completion of the survey, participants received incentives through a care package that included syringes, alcohol pads, condoms, and water-based lubricants. Informed consent was obtained from all participants after they reviewed the participant information sheet detailing risks and benefits of study participation, and then clicked “consent” to the online survey.
Measures
Data on age, employment status, education, income, and sexual orientation were collected along with self-reported HIV-related risk behaviors. Participants were asked how many casual sex partners they had anal sex within the past six months; participants were allowed to choose a drop-down list ranged 0–100; and responses were categorized based on distributional features. Participants were also asked whether they had used a condom at last anal intercourse and the frequency of their participation in group sex (“often,” “occasionally” or “never”). Participants self-reported their HIV testing behaviors, HIV status, and STI diagnoses (gonorrhea, genital warts, genital herpes, syphilis, hepatitis B (HBV), hepatitis C (HCV), chlamydia, and pubic lice symptoms). Those reporting any of the above diagnoses were categorized as having an STI (excluding HIV). Participants were asked whether they had been given or received things or opportunities (e.g., mobile phones, money, clothes, bags, grades, or educational/work opportunities) in exchange for sex. They were also asked whether they had ever agreed to meet people from the Internet (Facebook) or geo-location social networking applications (apps) (Hornet, Jack’D) to have sex. Among those reporting a negative HIV status, participants were asked whether they had heard of PrEP, had taken PrEP, and whether they wanted to take PrEP.
Participants were asked whether they had ever used substances before or during sex in the past six months based on a list of options reported in our previous research (Guadamuz & Boonmongkon, 2018; Kongjareon et al., 2022). These options include amphetamine (“Yaba”/“Yama”), crystal meth (“Ice”), ecstasy, ketamine, GHB (gamma-hydroxybutyrate), Xanax/alprazolam, mephedrone, cocaine, heroin, opium, marijuana, amyl nitrite (“poppers”), erectile dysfunction medication, Kratom cocktail (“Fatal 4 × 100”), hormone medication (steroids, progesterone, estrogen), alcohol, and “never use substance before/during sex.”
Data Analysis
LCA was used to identify patterns of substance use before or during sex (chemsex) among Thai MSM who attended a private sex party or circuit party in the past three months. A bias-adjusted classify–analyze approach was implemented in the poLCA package in R (Bray et al., 2015; Linzer & Lewis, 2011; Nylund-Gibson et al., 2019). First, an LCA model with only the latent class indicators (chemsex substance use variables) was fitted to determine the optimal number of latent classes based on the model fit criteria and theoretical interpretability. Models with two to six classes were evaluated with 20 random starts and a maximum of 5000 iterations per model. Model selection was based on log-likelihood (LL), approximate weight of evidence criteria (AWE), Bayesian information criteria (BIC), sample size-adjusted BIC (aBIC), and consistent Akaike information criteria (CAIC), with better fit indicated by higher LL and AWE values and lower BIC, aBIC, and CAIC values. A relative entropy above 0.70 provided evidence of adequate class separation as a model diagnostic. After identifying the optimal class solution, covariates were included in a second LCA model to derive bias-adjusted posterior probabilities that accounted for the relationships between covariates and latent classes. The participants were assigned to latent classes based on bias-adjusted posterior probabilities. Finally, multivariable multinomial logistic regression was used to relate participant characteristics to latent class membership, purposefully selecting covariates based on univariate analyses and theoretical relevance.
Results
Sociodemographic and behavioral characteristics are summarized in (Table 1). The distribution of age, educational attainment, and prevalence of HIV testing behaviors resemble other studies involving Thai MSM recruited from a gay sauna and over the Internet (Khawcharoenporn et al., 2019; Weiss et al., 2017). However, our participants tended to earn a lower income and have a higher self-reported prevalence of STI diagnosis (59.2%) and HIV (20.3%) than other samples of Thai MSM (Khawcharoenporn et al., 2019; Seekaew et al., 2018). Our participants also had higher rates of condomless anal sex and reported higher numbers of casual sex partners than other Thai MSM (Khawcharoenporn et al., 2019; Weiss et al., 2017). Moreover, less than half of participants (44.7%) had received things or opportunities in exchange for sex. In comparison, more than half (54.7%) had provided things or opportunities in exchange for sex at elevated rates compared to representative Thai MSM samples (Seekaew et al., 2018). Almost all participants reported meeting their sexual partners online (97.2%). These results correspond to our qualitative findings on personal accounts of sexual transactions among ice party attendees (Guadamuz & Boonmongkon, 2018). Participants also reported a high willingness for PrEP use; among those without a positive HIV status, most of them had heard of PrEP (88.9%), 25.9% had taken PrEP, and among those who had not taken PrEP and had heard of PrEP, 83.1% wanted to take PrEP.
Most participants reported using at least one of the substances listed in (Table 2) with only 9% of the participants reporting never using any substance before or during sex. The prevalence of methamphetamine (40.2% by injection and 23.9% by inhalation) was the highest reported among studies on Thai MSM (Dunne et al., 2019; Fongkaew et al., 2022; Piyaraj et al., 2018; Thienkrua et al., 2018; Wansom et al., 2020). The most common substance used before or during sex in the last six months was amyl nitrite (45.9%), followed by the injection of crystal meth (40.2%). Alcohol use was moderate (29.9%), while erectile dysfunction medication (25.6%) was less prevalent than in another study among young Thai MSM in Bangkok (Thienkrua et al., 2018). Kratom cocktail use was 11.3%. Ecstasy, ketamine, GHB, Xanax, marijuana, and hormone medication usage were less frequently reported by participants. These characteristics of our participant sample reflect our recruitment strategy and study objectives in characterizing circuit party and private sex party attendees (Table 3).
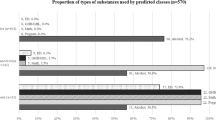
Based on the fit indices (see Supplementary Table 1) and respective elbow plots (see Supplementary Fig. 1), a 3-class model was supported by its lowest BIC and CAIC, with the lowest AWE among models with a number of parameters at 50 or higher, suggesting it to be the best fitting model. The 3-class model was refitted with covariates (the bias-adjusted inclusive 3-class model), which has improved LL, BIC, and RE, indicating that it provides a better fit and less classification uncertainty than the non-inclusive 3-class model. In the inclusive 3-class model (see Table 4), 36.7% (n = 195) were classified as “negligible sexualized substance users,” 13.9% (n = 74) were classified as “sexualized substance users,” and 49.4% (n = 263) were classified as “exclusive chemsex users.” Members of the “negligible sexualized substance users” subgroup reported the highest probabilities of never using any substance before or during sex, with 31% endorsing poppers and 22% endorsing alcohol before or during sex. Members in the “sexualized substance users” subgroup reported 9% and 22% of inhaling and injecting crystal meth and a variety of other substances (ranged 1%-19%) before or during sex, including Xanax, marijuana, amyl nitrite, erectile dysfunction medication, and hormone medication, and have the highest probabilities of using Kratom cocktail (79%) and alcohol (76%) before or during sex. “Exclusive chemsex users” subgroup had the highest probabilities (45% and 69%) of reporting both inhalation and injection of crystal meth before or during sex, the highest probability of using poppers (65%) and erectile dysfunctional drugs (40%) before or during sex, and low probabilities of reporting other substances before or during sex.
In our final multivariable model (see Table 4), compared to “negligible sexualized substance users,” “exclusive chemsex users” were more likely to be aged 30–39, compared to those aged 18–29, and self-reported HIV-positive status, compared to those self-reported to be HIV-negative, were more likely to have six or more sexual partners in the past six months, compared to having 0–1 sexual partner, and more likely to have ever provided sex work and more likely to not use a condom during last anal sex. “Exclusive chemsex users” were less likely to not know their HIV status compared to those self-reported to be HIV-negative. Compared to “negligible sexualized substance users,” “sexualized substance users” were more likely not to use condoms during last anal intercourse, more likely to have ever received or provided things or opportunities in exchange for sex, and more likely to report “often” to ever meet sexual partners online. For univariate analyses, please refer to Supplementary Table 2.
Discussion
From a sexually active sample of Thai MSM who attended private sex parties or circuit parties in the past three years, we identified three distinct substance use typologies: “negligible sexualized substance users,” “sexualized substance users,” and “exclusive chemsex users” with differing levels of HIV and STI transmission risks. Those in the “exclusive chemsex users” group were more likely to be HIV-positive, have ever provided things or opportunities in exchange for sex, have a higher number of sexual partners, and report more inconsistent use of condoms. Corroborating evidence shows MSM that were classified into latent classes by endorsing any methamphetamine use were associated with HIV positivity, a higher number of sexual partners, condomless anal sex, and group sex (Achterbergh et al., 2020; Blair et al., 2022; Card et al., 2023; Goldshear et al., 2023; Lim et al., 2015; Melendez-Torres et al., 2018; Tan et al., 2021; Wong et al., 2020). The sexualized substance users characterized in the “exclusive chemsex user” class is indicative of the “ice party” subculture, where methamphetamine is predominately used to enhance and prolong sexual arousal and performance and to have sex with multiple partners (Guadamuz & Boonmongkon, 2018; Wang et al., 2023). Erectile dysfunction drugs are used to maintain erection, whereas amyl nitrite is used to facilitate penetrative anal sex (Guadamuz & Boonmongkon, 2018). This combination of sexualized substance use is associated with a heightened risk of HIV positivity, and among those not diagnosed with HIV, they could be exposed to substantial HIV risks (Fisher et al., 2010; Swartz & McCarty-Caplan, 2018). Men in this latent class membership may be aware of their heightened HIV risk and are more likely to be engaged in protective behaviors; thus, HIV-negative and sero-unknown participants who were classified in this latent class membership were more likely to be HIV tested, heard of PrEP, and have taken PrEP. This finding is consistent with studies examining chemsex prevalence and PrEP awareness among MSM in Malaysia (Maviglia et al., 2022) and Hong Kong (Wong et al., 2020). However, only 25.9% of our MSM sampled had ever taken PrEP, which is higher than previously reported by a study among Thai MSM engaged in sex work (Weir et al., 2022), but still far from UNAIDS’s 2030 goal of providing 50% PrEP coverage for high-risk MSM (UNIADS, 2022).
Those classified as “sexualized substance users” reported high levels of alcohol use and moderate levels of usage of a range of other substances. These substances included those typically seen in Europe and the USA, such as marijuana, amphetamine, and benzodiazepine, as well as substances unique to the Southeast Asian context, such as the Kratom cocktail and hormone medications. Kratom cocktails contain boiled Kratom leaves, cola soft drinks or iced tea, codeine, and a range of substances that could include mosquito coils, anxiolytic drugs, and antidepressants (Tungtananuwat & Lawanprasert, 2018). Together, these ingredients produce sedative and euphoric effects similar to alcohol consumption. Hormone medications, such as anabolic androgenic steroids, are used to boost physical performance and libido (Zaami et al., 2021). They are used to overcome unwanted side effects of methamphetamine, such as erectile dysfunction (Zaami et al., 2021). MSM in this subgroup could be using androgenic steroids to replace erectile dysfunctional medication due to over-the-counter accessibility of androgenic steroids. However, the use of anabolic androgenic steroids has been associated with violent behavior, which may contribute to the worsening epidemic of intimate partner violence among MSM (Parent & Johnson, 2023; Zaami et al., 2021).
Moreover, men classified into the “sexualized substance users” group tended to be part-time employed, less educated, and earning less income. These data indicate that these men are of a different socioeconomic class than the “negligible sexualized substance users” and “exclusive chemsex users” groups. This is consistent with our qualitative finding that those who uses “yaba” (amphetamine tablets) have a lower socioeconomic status (Guadamuz & Boonmongkon, 2018). Unlike “exclusive chemsex users,” these men are more likely to have never been tested for HIV, have an unknown HIV status, and are less likely to have heard of PrEP, possibly compounded by a lower socioeconomic status and decreased exposure to community-based resources such as HIV testing and PrEP awareness campaigns. In addition, these men could be relatively less aware of their HIV risk and face higher levels of barriers to accessing preventive and healthcare resources than “exclusive chemsex users” [16,17]. HIV risk perception is essential for engagement in HIV testing and acceptance of PrEP (Guadamuz et al., 2015; Khawcharoenporn et al., 2019; Plotzker et al., 2017). Public health interventions, such as voluntary HIV testing and PrEP promotion targeting this group of MSM, should raise awareness of their HIV risk perception to facilitate their acceptance of utilizing these services. Our data show that these men frequently meet sexual partners online; interventions can reach this group of men via online campaigns on geo-location social networking apps such as GRINDR, Jack’D, and Hornet (Guadamuz et al., 2015; Weiss et al., 2017).
Among our sample of Thai MSM, we found a very high prevalence of crystal meth use before or during sex (23.9% inhaled and 40.2% injected). The use of this chemical substance is among the highest in Asia (Wang et al., 2023). This finding corresponds to our recruitment strategy, which uses private sex parties and circuit parties as inclusion criteria, where substance use is the norm (Guadamuz & Boonmongkon, 2018; O’Byrne & Holmes, 2011). Nearly half of our sample of men had ever received things or opportunities in exchange for sex (44.7%) and more than half had provided things or opportunities in exchange for sex (54.7%). These factors are characteristic of chemsex epidemics in Asia (Maviglia et al., 2022; Wang et al., 2023). The power differential that occurs during transactional sex may further facilitate condomless anal sex (Dunne et al., 2019; Tan & Melendez-Torres, 2016; Weir et al., 2022). The combined social norm and transactional nature of these men’s engagement with chemsex may further subjugate their self-efficacy in negotiating condom use (Liu et al., 2009). Remarkably, only a quarter of the HIV-negative men sampled had taken PrEP, while 83.1% of those who had not taken PrEP wanted to take PrEP. This demonstrates the unmet need for PrEP coverage in high-risk men. Tailored interventions to promote PrEP uptake are urgently required.
Limitations
Despite the importance of these findings, this study had some limitations. Our sample was drawn from a convenience sample of community partners. Although our study’s sociodemographic characteristics resemble those of other studies with similar recruitment strategies, they may not represent the true population of Thai MSM who attend private sex parties and circuit parties. They may have more distinct characteristics in terms of sociodemographic characteristics, risk behaviors, and substance use patterns that may extend the relationship between latent class and other covariates. We attempted to account for this heterogeneity by including the circuit party/sex party attendance variable in the inclusive LCA model and our final multivariable model. Our data were self-reported, which is subject to social desirability bias. Our use of computer-assisted self-interviews may have minimized this bias. Notably, our questionnaire asked participants to report their lifetime prevalence of chemsex engagement; it should not be interpreted as recent chemsex engagement. Nonetheless, participants who reported general use instead of chemsex-related use may still be subject to misclassification bias. Future research should utilize a more nuanced measure, such as the duration of regular substance use and chemsex-related substance use, for measure validation and to provide further insights into their overlap to evaluate the impact of chemsex on chronic substance use. Lastly, the cross-sectional nature of our study does not address potential changes in substance-using patterns, sexual behaviors, and HIV/STI statuses over time, nor does it establish causality between these variables and latent class membership.
Conclusions
Our findings suggest that different strategies should be employed to target specific subgroups of MSM who use various substances. For MSM who primarily engage in the inhalation and injection of crystal meth before or during sex, interventions should focus on increasing their PrEP coverage to lower their HIV transmission risks. For MSM who engage in alcohol consumption and a range of various substances before or during sex, interventions should focus on increasing their HIV risk perceptions and PrEP awareness while scaling up their HIV testing uptake by engaging them via HIV self-testing and online platforms (Samoh et al., 2021). MSM in Thailand are experiencing a high burden of multiple health disparities related to HIV risk and substance use. Tailored interventions are urgently needed to reverse health trajectories.
Data Availability
Data are available upon request to the corresponding author at thomas.gua@mahidol.edu (Thomas E. Guadamuz).
References
Achterbergh, R. C. A., Drückler, S., Van Rooijen, M. S., Van Aar, F., Slurink, I. A. L., De Vries, H. J. C., & Boyd, A. (2020). Sex, drugs, and sexually transmitted infections: A latent class analysis among men who have sex with men in Amsterdam and surrounding urban regions, the Netherlands. Drug and Alcohol Dependence, 206, 107526. https://doi.org/10.1016/j.drugalcdep.2019.06.028
Blair, C. S., Needleman, J., Javanbakht, M., Comulada, W. S., Ragsdale, A., Bolan, R., Shoptaw, S., & Gorbach, P. M. (2022). Risk behaviors associated with patterns of sexualized stimulant and alcohol use among men who have sex with men: A latent class analysis. Journal of Urban Health, 99(2), 293–304. https://doi.org/10.1007/s11524-021-00600-8
Bray, B. C., Lanza, S. T., & Tan, X. (2015). Eliminating bias in classify-analyze approaches for latent class analysis. Structural Equation Modeling: A Multidisciplinary Journal, 22(1), 1–11. https://doi.org/10.1080/10705511.2014.935265
Card, K. G., Shen, T., Barath, J., Sang, J., Lal, A., Moore, D. M., & Lachowsky, N. J. (2023). Patterns of event-level concurrent substance use during sex among gay, bisexual, and other men who have sex with men in metro Vancouver. AIDS and Behavior, 27, 3157–3170. https://doi.org/10.1007/s10461-023-04036-w
Cheung, D. H., Lim, S. H., Guadamuz, T. E., Koe, S., & Wei, C. (2015). The potential role of circuit parties in the spread of HIV among men who have sex with men in Asia: A call for targeted prevention. Archives of Sexual Behavior, 44(2), 389–397.
Colfax, G. N., Mansergh, G., Guzman, R., Vittinghoff, E., Marks, G., Rader, M., & Buchbinder, S. (2001). Drug use and sexual risk behavior among gay and bisexual men who attend circuit parties: A venue-based comparison. JAIDS Journal of Acquired Immune Deficiency Syndromes, 28(4), 373–379.
Dunne, E. F., Pattanasin, S., Chemnasiri, T., Varangrat, A., Raengsakulrach, B., Wichuda, S., Ungsedhapand, C., Sirivongrangson, P., Chitwarakorn, A., & Holtz, T. H. (2019). Selling and buying sex in the city: Men who have sex with men in the Bangkok Men Who Have Sex with Men Cohort Study. International Journal of STD & AIDS, 30(3), 212–222. https://doi.org/10.1177/0956462418796440
Fisher, D. G., Reynolds, G. L., & Napper, L. E. (2010). Use of crystal methamphetamine, Viagra, and sexual behavior. Current Opinion in Infectious Diseases, 23(1), 53–56. https://doi.org/10.1097/QCO.0b013e328334de0b
Fongkaew, K., Lind, De., van Wijngaarden, J. W., Tepjan, S., Chonwanarat, N., Akkakanjanasupar, P., & Newman, P. A. (2022). ‘No test, no disease’: Multilevel barriers to HIV testing among young men who have sex with men and transgender women in three semi-urban areas in Thailand. Culture, Health & Sexuality, 24(9), 1199–1214. https://doi.org/10.1080/13691058.2021.1938237
GCIRCUIT SONGKRAN 2024. (n.d.). Retrieved December 15, 2023, from https://www.gcircuit.com/about-gcircuit.php
Goldshear, J. L., Westmoreland, D. A., Carrico, A. W., & Grov, C. (2023). Drug use typology, demographic covariates, and associations with condomless anal sex: A latent class analysis among a U.S. national cohort of men who have sex with men. International Journal of Drug Policy, 112, 103949. https://doi.org/10.1016/j.drugpo.2022.103949
Guadamuz, T. E., & Boonmongkon, P. (2018). Ice parties among young men who have sex with men in Thailand: Pleasures, secrecy and risks. International Journal of Drug Policy, 55, 249–255. https://doi.org/10.1016/j.drugpo.2018.04.005
Guadamuz, T. E., Cheung, D. H., Wei, C., Koe, S., & Lim, S. H. (2015). Young, online and in the dark: Scaling up HIV testing among MSM in ASEAN. PLoS ONE, 10(5), e0126658.
Guerras, J.-M., Hoyos, J., García De Olalla, P., De La Fuente, L., Herrero, L., Palma, D., Del Romero, J., García-Pérez, J.-N., Belza, M.-J., & The Methysos Project Group. (2021). Comparison of polydrug use prevalences and typologies between men who have sex with men and general population men, in Madrid and Barcelona. International Journal of Environmental Research and Public Health, 18(21), 11609. https://doi.org/10.3390/ijerph182111609
Joint United Nations Programme on HIV/AIDS (UNAIDS). (2022). HIV prevention 2025–road map: Getting on track to end AIDS as a public health threat by 2030. https://www.unaids.org/sites/default/files/media_asset/prevention-2025-roadmap_en.pdf
Holtz, T., Wimonsate, W., Mock, P., Pattanasin, S., Chonwattana, W., Thienkrua, W., Sukwicha, W., Curlin, M., Chitwarakorn, A., & Dunne, E. (2019). Why we need pre-exposure prophylaxis: Incident HIV and syphilis among men, and transgender women, who have sex with men, Bangkok, Thailand, 2005–2015. International Journal of STD & AIDS, 30(5), 430–439. https://doi.org/10.1177/0956462418814994
Kelly-Hanku, A. (2021). A qualitative scoping review of sexualised drug use (including Chemsex) of men who have sex with men and transgender women in Asia. https://www.aidsdatahub.org/sites/default/files/resource/apcom-qualitative-scoping-review-sexualised-drug-useincluding-chemsex-2021.pdf
Khawcharoenporn, T., Mongkolkaewsub, S., Naijitra, C., Khonphiern, W., Apisarnthanarak, A., & Phanuphak, N. (2019). HIV risk, risk perception and uptake of HIV testing and counseling among youth men who have sex with men attending a gay sauna. AIDS Research and Therapy, 16(1), 13. https://doi.org/10.1186/s12981-019-0229-z
Knox, J., Boyd, A., Matser, A., Heijman, T., Sandfort, T., & Davidovich, U. (2020). Types of group sex and their association with different sexual risk behaviors among hiv-negative men who have sex with men. Archives of Sexual Behavior, 49(6), 1995–2003. https://doi.org/10.1007/s10508-020-01744-5
Kongjareon, Y., Samoh, N., Peerawaranun, P., & Guadamuz, T. E. (2022). Pride-based violence, intoxicated sex and poly-drug use: A vocational school-based study of heterosexual and LGBT students in Bangkok. BMC Psychiatry, 22(1), 148. https://doi.org/10.1186/s12888-022-03777-7
Lanza, S. T., & Rhoades, B. L. (2013). Latent class analysis: an alternative perspective on subgroup analysis in prevention and treatment. Prevention Science, 14(2), 157–168. https://doi.org/10.1007/s11121-011-0201-1
Lim, S. H., Cheung, D. H., Guadamuz, T. E., Wei, C., Koe, S., & Altice, F. L. (2015). Latent class analysis of substance use among men who have sex with men in Malaysia: findings from the Asian Internet MSM Sex Survey. Drug and Alcohol Dependence, 151, 31–37.
Linzer, D. A., & Lewis, J. B. (2011). poLCA: An R package for polytomous variable latent class analysis. Journal of Statistical Software, 42(10), 1–29. https://doi.org/10.18637/jss.v042.i10
Liu, H., Liu, H., Cai, Y., Rhodes, A. G., & Hong, F. (2009). Money boys, hiv risks, and the associations between norms and safer sex: A respondent-driven sampling study in Shenzhen China. AIDS and Behavior, 13(4), 652–662. https://doi.org/10.1007/s10461-008-9475-0
Maviglia, F., Wickersham, J. A., Azwa, I., Copenhaver, N., Kennedy, O., Kern, M., Khati, A., Lim, S. H., Gautam, K., & Shrestha, R. (2022). Engagement in chemsex among men who have sex with men (MSM) in Malaysia: Prevalence and associated factors from an online national survey. International Journal of Environmental Research and Public Health, 20(1), 294. https://doi.org/10.3390/ijerph20010294
Melendez-Torres, G. J., Bourne, A., Reid, D., Hickson, F., Bonell, C., & Weatherburn, P. (2018). Typology of drug use in United Kingdom men who have sex with men and associations with socio-sexual characteristics. International Journal of Drug Policy, 55, 159–164. https://doi.org/10.1016/j.drugpo.2018.01.007
Meunier, É. (2018). Social interaction and safer sex at sex parties: Collective and individual norms at gay group sex venues in NYC. Sexuality Research and Social Policy, 15(3), 329–341. https://doi.org/10.1007/s13178-017-0300-2
Nylund-Gibson, K., Grimm, R. P., & Masyn, K. E. (2019). Prediction from latent classes: A demonstration of different approaches to include distal outcomes in mixture models. Structural Equation Modeling: A Multidisciplinary Journal, 26(6), 967–985. https://doi.org/10.1080/10705511.2019.1590146
O’Byrne, P., & Holmes, D. (2011). Drug use as boundary play: A qualitative exploration of gay circuit parties. Substance Use & Misuse, 46(12), 1510–1522. https://doi.org/10.3109/10826084.2011.572329
Parent, M. C., & Johnson, N. L. (2023). Anabolic steroid use and intimate partner violence among sexual minority men. Journal of Interpersonal Violence, 38(9–10), 6676–6694. https://doi.org/10.1177/08862605221137704
Piyaraj, P., van Griensven, F., Holtz, T. H., Mock, P. A., Varangrat, A., Wimonsate, W., Thienkrua, W., Tongtoyai, J., McNamara, A., & Chonwattana, W. (2018). The finding of casual sex partners on the internet, methamphetamine use for sexual pleasure, and incidence of HIV infection among men who have sex with men in Bangkok, Thailand: An observational cohort study. The Lancet HIV, 5(7), e379–e389.
Plotzker, R., Seekaew, P., Jantarapakde, J., Pengnonyang, S., Trachunthong, D., Linjongrat, D., Janyam, S., Nakpor, T., Charoenying, S., Mills, S., Vannakit, R., Cassell, M., Phanuphak, P., Lertpiriyasuwat, C., & Phanuphak, N. (2017). Importance of risk perception: predictors of PrEP acceptance among Thai MSM and TG women at a community-based health service. JAIDS Journal of Acquired Immune Deficiency Syndromes, 76(5), 473–481. https://doi.org/10.1097/QAI.0000000000001536
Qualtrics. (2024). Response Quality-Qualitrics. https://www.qualtrics.com/support/survey-platform/survey-module/survey-checker/response-quality/
Samoh, N., Peerawaranun, P., Jonas, K. J., Lim, S. H., Wickersham, J. A., & Guadamuz, T. E. (2021). Willingness to use HIV self-testing with online supervision among app-using young men who have sex with men in Bangkok. Sexually Transmitted Diseases, 48(3), e41–e44. https://doi.org/10.1097/OLQ.0000000000001271
Scholz-Hehn, A. D., Milin, S., Schulte, B., Reimer, J., Buth, S., & Schäfer, I. (2022). Substance use and chemsex in MSM - a latent class analysis. Journal of Drug Issues, 52(1), 83–96. https://doi.org/10.1177/00220426211040564
Seekaew, P., Pengnonyang, S., Jantarapakde, J., Sungsing, T., Rodbumrung, P., Trachunthong, D., Cheng, C., Nakpor, T., Reankhomfu, R., Lingjongrat, D., Janyam, S., Charoenying, S., Mills, S., Cassell, M., Phanuphak, P., Vannakit, R., & Phanuphak, N. (2018). Characteristics and HIV epidemiologic profiles of men who have sex with men and transgender women in key population-led test and treat cohorts in Thailand. PLoS ONE, 13(8), e0203294. https://doi.org/10.1371/journal.pone.0203294
Semple, S. J., Zians, J., Strathdee, S. A., & Patterson, T. L. (2009). Sexual marathons and methamphetamine use among HIV-positive men who have sex with men. Archives of Sexual Behavior, 38(4), 583–590. https://doi.org/10.1007/s10508-007-9292-y
Swartz, J. A., & McCarty-Caplan, D. (2018). A study of the longitudinal patterns of stimulant and amyl nitrite use and sexual behavior pre- and post-HIV seroconversion among MSM. AIDS and Behavior, 22(4), 1395–1409. https://doi.org/10.1007/s10461-017-2008-y
Tan, R. K. J., O’Hara, C. A., Koh, W. L., Le, D., Tan, A., Tyler, A., Tan, C., Kwok, C., Banerjee, S., & Wong, M. L. (2021). Delineating patterns of sexualized substance use and its association with sexual and mental health outcomes among young gay, bisexual and other men who have sex with men in Singapore: A latent class analysis. BMC Public Health, 21(1), 1026. https://doi.org/10.1186/s12889-021-11056-5
Tan, S. Y., & Melendez-Torres, G. J. (2016). A systematic review and metasynthesis of barriers and facilitators to negotiating consistent condom use among sex workers in Asia. Culture, Health & Sexuality, 18(3), 249–264. https://doi.org/10.1080/13691058.2015.1077994
The Circuit Party Men’s Health Survey. (2001). Findings and implications for gay and bisexual men. American Journal of Public Health, 91(6), 953–958. https://doi.org/10.2105/AJPH.91.6.953
Thienkrua, W., Van Griensven, F., Mock, P. A., Dunne, E. F., Raengsakulrach, B., Wimonsate, W., Howteerakul, N., Ungsedhapand, C., Chiwarakorn, A., & Holtz, T. H. (2018). Young men who have sex with men at high risk for HIV, Bangkok MSM Cohort Study, Thailand 2006–2014. AIDS and Behavior, 22(7), 2137–2146. https://doi.org/10.1007/s10461-017-1963-7
Tungtananuwat, W., & Lawanprasert, S. (2018). FATAL 4x100; home-made kratom juice cocktail. Journal of Health Research, 24(1), 43–47.
Van Griensven, F., Guadamuz, T. E., Van Wijngaarden, J. W. D. L., Phanuphak, N., Solomon, S. S., & Lo, Y. R. (2017). Challenges and emerging opportunities for the HIV prevention, treatment and care cascade in men who have sex with men in Asia Pacific. Sexually Transmitted Infections, 93(5), 356. https://doi.org/10.1136/sextrans-2016-052669
Van Griensven, F., Phanuphak, N., Manopaiboon, C., Dunne, E. F., Colby, D. J., Chaiphosri, P., & Mills, S. (2022). HIV prevalence and incidence among men who have sex with men and transgender women in Bangkok, 2014–2018: Outcomes of a consensus development initiative. PLoS ONE, 17(1), e0262694.
Van Griensven, F., Thienkrua, W., McNicholl, J., Wimonsate, W., Chaikummao, S., Chonwattana, W., Varangrat, A., Sirivongrangson, P., Mock, P. A., Akarasewi, P., & Tappero, J. W. (2013). Evidence of an explosive epidemic of HIV infection in a cohort of men who have sex with men in Thailand. AIDS, 27(5), 825–832. https://doi.org/10.1097/QAD.0b013e32835c546e
Wang, H., Jonas, K. J., & Guadamuz, T. E. (2023). Chemsex and chemsex associated substance use among men who have sex with men in Asia: A systematic review and meta-analysis. Drug and Alcohol Dependence, 243, 109741. https://doi.org/10.1016/j.drugalcdep.2022.109741
Wansom, T., Pinyakorn, S., Kolsteeg, C. J., Kroon, E., Sacdalan, C. P., Chomchey, N., Ananworanich, J., Vasan, S., Phanuphak, N., & Colby, D. J. (2020). Group sex and methamphetamine use fuel an explosive epidemic of hepatitis C among HIV-infected men who have sex with men in Bangkok Thailand. JAIDS Journal of Acquired Immune Deficiency Syndromes, 84(4), 331.
Weir, B. W., Dun, C., Wirtz, A. L., Mon, S. H. H., Qaragholi, N., Chemnasiri, T., Pattanasin, S., Sukwicha, W., Varangrat, A., Dunne, E. F., Holtz, T. H., Janyam, S., Jin, H., Linjongrat, D., Mock, P. A., Thigpen, M. C., Rooney, J. F., Sullivan, P. S., Hickey, A. C., & Beyrer, C. (2022). Transactional sex, HIV and health among young cisgender men and transgender women who have sex with men in Thailand. Annals of Epidemiology, 72, 1–8. https://doi.org/10.1016/j.annepidem.2022.03.012
Weiss, K. M., Jonas, K. J., & Guadamuz, T. E. (2017). Playing and never testing: Human immunodeficiency virus and sexually transmitted infection testing among App-using MSM in Southeast Asia. Sexually Transmitted Diseases, 44(7), 406–411. https://doi.org/10.1097/OLQ.0000000000000624
WHITE PARTY BANGKOK. (n.d.). Retrieved December 15, 2023, from https://whitepartybangkok.com/about-wp/
Wong, N. S., Kwan, T. H., Lee, K. C. K., Lau, J. Y. C., & Lee, S. S. (2020). Delineation of chemsex patterns of men who have sex with men in association with their sexual networks and linkage to HIV prevention. International Journal of Drug Policy, 75, 102591. https://doi.org/10.1016/j.drugpo.2019.10.015
Zaami, S., Tini, A., & Varì, M. R. (2021). Commentary—Increasing abuse of anabolic steroids and chemsex drugs as performance and image-enhancing agents. European Review for Medical and Pharmacological Sciences, 25, 455–458.
Acknowledgements
We are grateful to Mookarpa Charoenyang and Verapun Ngammee who assisted in data collection and participant recruitment. We thank Ozone Foundation and Pulse Clinic Thailand for their partnership in this research study.
Funding
Open access funding provided by Mahidol University. The research reported in this publication was supported by Mahidol University (Fundamental Fund: fiscal year 2023 by National Science Research and Innovation Fund (NSRF)) and the U.S. National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Number R21AI140939. Thomas E. Guadamuz, Yamol Kongjareon, and Nattharat Samoh were supported by NIMH Grants R01MH119015 and R34MH123337. The content is solely the authors’ responsibility and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
DHC contributed to the analysis and interpretation of data and drafted the manuscript. YK and NS contributed to the acquisition of data and design of the work. KJJ, SHL, and TEG contributed to the conception and design of the study and substantively revised it. All authors read, edited, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest or competing interests.
Ethical Approval
Mahidol University Social Sciences Institutional Review Board reviewed and approved the study (approval no. 2019/223.2210).
Informed Consent
Informed consent was obtained from all participants after they reviewed the participant information sheet.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cheung, D.H., Samoh, N., Jonas, K.J. et al. Patterns of Chemsex Substance Use and Its Association with HIV Transmission Risk Among Men Who Have Sex with Men in Thailand: A Latent Class Analysis. Arch Sex Behav 53, 3527–3536 (2024). https://doi.org/10.1007/s10508-024-02868-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-024-02868-8