Abstract
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by impairments in social communication and behavior, frequently accompanied by restricted and repetitive patterns of interests or activities. The gut microbiota has been implicated in the etiology of ASD due to its impact on the bidirectional communication pathway known as the gut-brain axis. However, the precise involvement of the gut microbiota in the causation of ASD is unclear. This study critically examines recent evidence to rationalize a probable mechanism in which gut microbiota symbiosis can induce neuroinflammation through intermediator cytokines and metabolites. To develop ASD, loss of the integrity of the intestinal barrier, activation of microglia, and dysregulation of neurotransmitters are caused by neural inflammatory factors. It has emphasized the potential role of neuroinflammatory intermediates linked to gut microbiota alterations in individuals with ASD. Specifically, cytokines like brain-derived neurotrophic factor, calprotectin, eotaxin, and some metabolites and microRNAs have been considered etiological biomarkers. We have also overviewed how probiotic trials may be used as a therapeutic strategy in ASD to reestablish a healthy balance in the gut microbiota. Evidence indicates neuroinflammation induced by dysregulated gut microbiota in ASD, yet there is little clarity based on analysis of the circulating immune profile. It deems the repair of microbiota load would lower inflammatory chaos in the GI tract, correct neuroinflammatory mediators, and modulate the neurotransmitters to attenuate autism. The interaction between the gut and the brain, along with alterations in microbiota and neuroinflammatory biomarkers, serves as a foundational background for understanding the etiology, diagnosis, prognosis, and treatment of autism spectrum disorder.
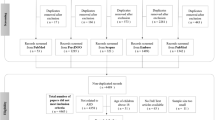
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The human gut microbiota is a complex biome and variable collection of microorganisms interacting with one another and the human host, including bacteria, fungi, archaea, and viruses. The gut microbiome influences many aspects of host health, including immune system control, gut hormone regulation, and neuronal transmission. It modifies the ingested medications and their metabolism, toxin clearance, and the generation of numerous host-affecting agents [1]. The gut microbial load can directly or indirectly influence the brain via a mutual relationship known as the "gut-brain axis." The gut microbiota can directly influence the brain by producing neuroactive substances such as neurotransmitters, amino acids, and microbial metabolites. These substances can potentially interfere with the host immune system and metabolism, affecting the gastrointestinal (GI), nervous system and vagus nerve. The gut microbiota can also influence the integrity of the gut barrier, which limits the passage of luminal substances into the bloodstream. Accessibility of such bacterial structural components like lipopolysaccharides or by-products of metabolic activities like short-chain fatty acids (SCFAs) may result in an inflammatory cascade that affects the CNS [2].
Autism spectrum disorder (ASD) is a persistent psychological abnormality characterized by impaired social communication and limiting and repetitive behavior patterns, hobbies, or activities [3]. Both genetic and environmental variables have been involved in ASD. Recent studies have shown that inflammation and inflammatory mediators have a role in disease genesis. Inflammatory elements that contribute to ASD include unusual microglia activation and polarization phenotypes, higher systemic levels of pro-inflammatory mediators, and altered patterns of immune cell responsiveness to activation triggers [4].
Numerous types of research in recent years have implicated gut bacteria in the etiology of ASD. However, studies have found that the structure of the gut microbiota is meaningfully changed in ASD; the significance of the gut microbiota as an etiology of ASD is yet unclear. It has been accepted that the microbiome of autistic children differs from healthy individuals [4]. Inflammatory deviations are potential etiology candidates in how gut microbiota can influence the gut-brain axis of ASD patients. Neuroinflammatory factors in ASD result from changes in the regulation of intestinal barriers, activation and function of microglia, and levels of neurotransmitters [5, 6].
ASD is currently diagnosed based on clinical symptoms, which can lead to delays and misinterpretation. Biomarkers based on neuroinflammatory processes associated with gut microbiota may provide a more objective and precise way of detecting ASD. Several examples of these markers include microRNAs that modulate immune signaling; brain-derived neurotrophic factor (BDNF), which promotes brain growth; S100B, which reflects neural immunity; and chemokines that facilitate immunological activation, such as RANTES and eotaxin [7]. This review aims to evaluate and discuss neuroinflammatory biomarkers in the pathogenesis and potential diagnostic trials of ASD in more detail.
Gut Microbiota, Inflammation, and ASD
Nearly two decades earlier, a potential association between gut microbiota and ASD was proposed [8]. While the exact cause of ASD is still unknown, existing literature has shown that gut dysbiosis, along with a neuroinflammatory condition, is found in individuals with ASD [9]. Studies found inconsistent differences in the gut microbiota composition of ASD cases. Overall, the ASD population shows signs of dysbiosis, with a different abundance of Bacteroidetes/Firmicutes, Prevotella, Clostridium, Lactobacillus, Bifidobacterium, Faecalibacterium, Streptococcus, Enterobacteriaceae, Verrucomicrobia, Fusobacteria, Escherichia coli, Enterococcus, Akkermansia, Phascolarctobacterium, and lots of other microbes compared to healthy controls [10,11,12]. Nonetheless, specific microbial patterns associated with ASD remain unidentified.
Moreover, Cuomo et al. [9] recently indicated that gut dysbiosis and inflammation were identified by host fecal DNA-specific methylation in autistic children. They revealed that autistic patients with dysbiosis significantly enriched inflammatory and immune pathways, including the production of interleukin (IL)-2, 6, and 12 and the activation of the toll-like receptor (TLR) 3 signaling pathway. Consistently, several studies corroborated earlier findings of the neuroinflammation caused by dysbiosis in various neurodegenerative and neuropsychiatric conditions [12, 13]. Disruptions in immune signaling pathways like the NLRP3 inflammasome, type 1 interferon, and nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) signaling pathways are among the possible dysbiotic consequences. Alterations to the T-helper 17 cell/T-reg proportion and imbalances in macrophage polarization, tumor necrosis factor (TNF)-α, IL-1β, 18, and 6 are also possible [14, 15].
On the other hand, the involvement of inflammation and immunological dysregulation has been indicated in the development and/or severity of ASD [16, 17]. Prior investigations on autistic cases have shown elevated levels of inflammatory markers such as TNF-α, interferon-γ, IL-2,4,5,6,8,17, and 10 [12, 18, 19]. A study also reported that autistic children with an innate proinflammatory response or impaired T cell activation indicate more severe behavioral issues compared to those with noninflamed or non-T cell-activated immunological profiles [20]. Given the lack of research on gut microbial composition and metabolites in autistic patients concerning inflammatory conditions (Table 1), the precise relationship between these three factors remains unclear and requires further investigation. Overall, gut microbiota seems to play a crucial role in ASD through inflammation.
S100B
Protein and peptide-based biomarkers have been the subject of some research for early diagnosis of ASD [7]. The S100 calcium-binding protein beta subunit (S100B) is expressed in astrocytes and other extra-neural cells, including enteric glial cells (EGCs). It affects neurons depending on the concentration, which can be trophic up to a few nanomolar doses and toxic at micromolar levels. Extracellular protein S100B contributes considerably to neuroinflammation by acting synergistically with pro-inflammatory cytokines and, at higher concentrations, acting as a cytokine [32]. Despite the existing conflict [33,34,35], multiple studies have found a significant elevation of S100B in autistic individuals compared to healthy cases, supporting the possible role of this factor in the etiology and development of ASD [36,37,38,39,40]. The source of this elevated S100B concentration in the periphery can be injured neurons or EGCs. In a recent study, the correlation between plasma S100B levels and fecal concentrations of calprotectin (an objective marker of GI inflammation status) revealed that not only brain astrocytes but also EGCs might be involved in the pathophysiology of autism [41]. One hypothesis says that the alternation of enteric glial-derived S100B expression in autistic patients can result from changed microbiota, disruption of the intestinal barrier, and even pathogenic bacteria, altogether inducing intestinal inflammation and converting EGCs to reactive EGCs [38]. Another in vivo study in mice showed that gut microbiota biodiversity increases with S100B levels or oral administration. Firmicutes phylum, including Lactobacillus and Bacteroidetes, including Barnesiella and Butyricimonas spp, are affected by S100B levels [42]. However, higher levels of Bacteroidetes and lower levels of Firmicutes were observed in a group of children with autism [43]. No study clarified the correlation between gut microbial alternation and the effect of probiotic use and S100B levels in autistic patients. Studies can be directed to know the effects of probiotic administration as a manipulative factor of gut microbiota on the levels of S100B in ASD patients. Furthermore, it is suggested that S100B can be investigated as a potential biomarker both in the diagnosis and treatment of autism.
Brain-derived Neurotrophic Factor
BDNF is a protein member of the nerve growth factor family (neurotrophins). BDNF has a key role in both the pre-synaptic site (modulates neurotransmitter release) and post-synaptic site (augments the function of ion channels), so it generally contributes to affect neuroplasticity and, thereby, behavior-related conditions [44]. Abnormal levels of BDNF were seen in a wide range of neurological diseases, including schizophrenia, depression, and even autism [45]. According to recent studies, altered BDNF levels were observed in ASD patients compared to the controls, revealing that BDNF might play a role in autism pathophysiology [46,47,48,49,50]. A relatively higher level of BDNF was seen in mild phenotypes compared to severe autism, emphasizing the probable protective function of this factor [51]. Downregulation of the BDNF in the antiapoptotic signaling pathway in the brains of autistic individuals is one of the possible underlying mechanisms in the pathophysiology of autism [52]. The reduction of BDNF expression as a neuroprotective agent can be caused by raised inflammatory factors, including IL-1β and TNF; therefore, it may have a negative regulatory role in neuroinflammation [53, 54]. The dysbiotic gut microbiota in autistic patients may contribute to this inflammatory condition through immune dysregulation and the release of inflammatory factors such as IL-1β, which crosses the BBB [55]. Animal studies showed that BDNF has been lower in germ-free mice's cortex and hippocampus [56]. Probiotic administration in these sterile mice also resulted in partial and complete normalization of behavior and BDNF levels, respectively. It has also been suggested that probiotics, specifically a combination of the Lactobacillus and Bifidobacterium genera, may be effective in increasing BDNF levels and improving mental health parameters in patients with depression and neurological disorders [57, 58]. Balance of fecal Clostridium spp. and normal BDNF expression were both achieved through fecal microbiota transplantation or Bifidobacterium treatment in an animal model of autism [21]. In another rat model study, Lactobacillus supplementation could increase BDNF levels and attenuate behavioral anomalies [59]. Regarding these relations, further studies are needed to know if the induction and modification of microbial alteration in the gut of autistic patients can be monitored and controlled by BDNF levels.
RANTES AND Eotaxin
Regulated upon Activation, Normal T Cell Expressed and Secreted, RANTES (CCL5), and eotaxin (CCL11) are pro-inflammatory chemokines released by a variety of cells, including blood cells, fibroblasts, endothelium, epithelium, neurons, and glial cells [60, 61]. RANTES [60, 62,63,64,65,66] and eotaxin [65,66,67,68] plasma levels are considerably higher in autistic children. Since RANTES and eotaxin act as pro-inflammatory mediators, their rise implies that both play a neuroinflammatory role in ASD [60, 61, 69, 70]. Although Shen et al. [63] reported no significant correlations between RANTES or eotaxin and behavioral patterns of ASD, Han et al. [64, 65] and Hu et al. [67] found RANTES and eotaxin related to ASD, respectively. Besides, other studies demonstrated that the rise of both factors is ASD related [66]. Moreover, gut microbiota seems to induce RANTES-mediated inflammation [71,72,73]. Earlier studies uncovered the NOD‐like receptor family pyrin domain containing 6–gut microbiota axis and subsequent IL-6 and TNF release as one possible connection of gut microbiota dysbiosis with RANTES-mediated immune dysregulation [74, 75]. Concerning the expression of gene encoding, it has been found that gut microbiota can manipulate eotaxin expression levels [76]. On this matter, antibiotic-treated mice had an altered microbiome with elevated eotaxin and different structures in their microglia [77]. Also, it has been found that mice's eotaxin levels changed after fecal microbiota transfer [78]. Regarding gut microbiota and ASD relation, modified anxiety-like and repetitive behaviors were observed while the levels of RANTES and eotaxin were improved through gut microbiota transplant in ASD mice. These results showed that RANTES and eotaxin play important roles in CNS synaptic transmission and development, and their levels are associated with the structure of microbiota in mice [22]. Clostridiaceae, Erysipelotrichaceae Prevotella families, Candidatus Arthromitus, and Proteus genus were found to be inversely associated with the level of RANTES and eotaxin [22]. In-vivo topical and oral probiotic administrations have reported a connection of RANTES with strains Lactobacillus paracasei SGL 04, Lactobacillus plantarum SGL 07, Lactobacillus fermentum SGL 10, and Lactobacillus brevis SGL 12 lysates, and Lactobacillus rhamnosus GG [79, 80]. Similarly, Probiotics containing Lactobacillus acidophilus, Lactobacillus rhamnosus GG, and Bifidobacterium also changed eotaxin gene expression in an animal [81]. Overall, the important findings implied from these studies suggest a potential mechanism of gut microbiota in ASD pathogenesis and severity through inflammatory factors of RANTES and eotaxin.
GM-CSF
The cytokine granulocyte–macrophage colony-stimulating factor (GM-CSF) drives many aspects of myeloid hemopoietic cell biology, including survival, proliferation, differentiation, and functional activity. It also affects the immune system through dendritic and T-cell functions [82, 83]. GM-CSF triggers chronic inflammation in the CNS and acts as a neuronal growth factor to stimulate neuronal and glial differentiation [82,83,84].
Although some earlier studies presented a low GM-CSF level in autistic patients [85, 86], higher levels of GM-CSF were found consequently in the brains of ASD patients [70, 82,83,84]. Perroud et al. reported higher levels of GM-CSF- IL-1α, TNF-α, and interferon-α among ASD children experiencing co-morbid GI symptoms [87]. The changes in GM-CSF levels in ASD can indicate that an inflammatory process may be involved in developmental and neuroimmune impairment [83]. Results of co-culture experiments by Takada et al. are the first to show that GM-CSF-induced macrophages inhibit the dendritic outgrowth of neurons in autistic individuals. This phenomenon is mediated through the secretion of pro-inflammatory cytokines, IL-1α and TNF-α, and may lead to more severe behavioral effects [88].
Interestingly, GM-CSF levels vary with alterations in gut microbiota [89,90,91,92] and mostly with IL-17a, a cytokine that correlated with the severity of behavioral symptoms in individuals with ASD [89, 90]. Different species of gut bacteria have been linked to GM-CSF, including Parabacteroide, Prevotella, Streptococcus, Clostridium, Lactobacillus reuteri, Lactobacillus crispatus Enterococcus faecalis, Blautia, Butyricimonass, Roseburia, Anaerotruncus, and Blautia [89, 92]. An important finding showed that gut microbiota-derived metabolites like SCFAs may alter GM-CSF levels [90]. Within a study, GM-CSF as a neuroimmune factor was increased with the administration of probiotics containing Bifidobacterium longum, Lactobacillus delbrueckii bulgaricus, and Streptococcus thermophilus [93]. Altogether, the change of GM-CSF neuroinflammatory factors by gut microbiota alteration provides insight into the mechanism of pathogenesis in this way in ASD patients.
HMGB-1
The high mobility group box 1 protein (HMGB-1) is one of the most abundant members of the HMGB protein family and has many potential roles [94]. It has a key role in DNA regulatory activities as a nuclear protein [95]. As an extracellular factor, it is actively released when immune cells respond to an inflammatory condition [96] and also passively released by necrotic or damaged cells [95]. HMGB1 has numerous membrane receptors called pathogen recognition receptors, TLR4, TLR9, and receptors for advanced glycation end products (RAGE) are the dominant ones. Through its interactions with these receptors, HMGB1 promotes inflammation in cells [97]. HMGB1 can cross the blood–brain barrier, promote neurite outgrowth and cell migration, or mediate neuroinflammation after injury [98].
It has been understood that plasma levels of HMGB-1 can elevate in ASD patients [99] and positively correlated with the severity of autism [100]. Another effective inflammatory molecule, the epidermal growth factor receptor, was considered to be related to symptom severity in children with autism, and the HMGB1 level seems to correlate with that [101, 102]. Interestingly, higher HMGB1 levels are found to be associated with higher GI dysfunctions in individuals with autism, which can imply an intestinal concept of pathogenesis [23, 103]. It is similarly studied that fecal levels of HMGB1 were correlated with GI sign severity in ASD children, which regards ASD-related dysbiosis [23]. Microbiome dysbiosis accompanied by intestinal inflammation can lead to the activation of monocytes, upregulating HMGB1 excretion for a pro-inflammatory feedback loop [104].
Higher levels of HMGB1 and TLR4 have also been reported to be associated with autistic-like behaviors in mice, possibly through activation of the HMGB1/TLR4 signaling cascade [105]. Serum levels of TLR4 were elevated in ASD children and positively associated with their hyperactivity scores [106]. Activation of the HMGB1/RAGE/TLR4 axis leads to leukocyte infiltration into nerve cells and results in persistent CNS inflammation. It is suggested that neuroinflammation is strongly related to ASD occurrence [107] through activating the inflammasome system as a mechanism [108]. In addition, it is described that HMGB1 can bind to endogenous secretory RAGE, resulting in a decline in plasma RAGE levels. This may contribute to the pathophysiology of autism by interfering with neuropeptide oxytocin transport from the periphery to the brain [109].
The effect of probiotics and gut microbiota alteration on HMGB1 levels in ASD patients can strengthen the idea and can be further studied. HMGB1 might play a key role in ASD pathogenesis through neuroinflammation and can conduct treatment strategies. However, it is a highly potential factor in the pathophysiology of autism, not precisely clarified, and more research is needed.
Osteopontin
Osteopontin (OPN) is both a soluble proinflammatory cytokine with a well-established role in autoimmune neuroinflammatory diseases and a component of the non-collagenous bone matrix that controls biomineralization in bone tissue [110]. Depending on its location and context, OPN is involved in local inflammation, cell adhesion, immune response, chemotaxis, and protection from apoptosis [111]. Heilmann et al. hypnotized that OPN can activate the immune system, reduce tissue damage, and stimulate mucosal repair during acute inflammation while promoting the Th1 response and strengthening inflammation under chronic circumstances [112].
OPN has been related to the pathogenesis of neuropsychological disorders like multiple sclerosis and Alzheimer's disease [110, 113]. Expression of secreted phosphoprotein 1 and its encoded protein OPN by CD11c + cells were associated with cognitive impairment and common neuropathologies in Alzheimer’s disease [114]. Studies on OPN levels in autistic patients are limited. However, Al-ayadhi and Mostafa [111] found an association between elevated serum levels of OPN and disease severity, indicating the role of OPN in neuroinflammation and the development of brain-specific auto-antibodies. Their findings can support the idea of OPN as an important neuroinflammation factor in the mechanism of ASD.
The possible interaction of OPN with gut microbiota has been discussed in metabolic disorders [115]. However, the role of OPN is not yet studied in association with gut microbiota in neurological disorders, especially in ASD patients, and can be a potential target for future studies. The finding of alterations in specific strains of gut microbiota connected to OPN and symptoms of ASD may help to improve diet, treatment methods, and probiotic supplements.
Calprotectin
Calprotectin is a protein that binds to calcium and is mainly found in neutrophils, which are white blood cells that increase when inflammation and cell damage occur. Calprotectin in stool can indicate intestinal inflammation and serve as a biomarker [116]. Considering the possible role of gut inflammation in the development of ASD, a number of research have studied the association of calprotectin levels in ASD patients, but their results were inconsistent. Some reports show that ASD patients and their relatives may have higher calprotectin levels than control groups [41, 117]. Interestingly, Babinská et al. found that calprotectin levels of ASD individuals were significantly related to all domains of autism diagnostic interview-revised, which measures social interaction, communication, and restricted and repetitive behaviors [41].
Similarly, Iovene et al. reported a significant correlation between autism severity, calprotectin level, and Clostridium spp—abundance [24]. Contrarily, Azouz et al. found no relation between calprotectin and disease severity, though they revealed a moderate correlation between calprotectin and GI symptoms [118]. Tomova et al. also revealed a positive correlation between Costridiacae bacteria, the severity of GI manifestations, and behavioral symptoms of ASD children. Calprotectin levels were also moderately correlated with higher expression of macrophage inflammatory protein 1β, which was associated with communication subscale and total score of autism diagnostic observation schedule, indicating that it may play a role in microbial-neuronal cross-talk [25]. Unlikely, some investigations found no statistically significant difference in calprotectin levels between ASD patients and controls [119,120,121,122] and, consequently, no appreciable variation in calprotectin levels of ASD patients with and without GI symptoms.
Studies on probiotic effects on calprotectin levels and autism are limited in the literature. Laghi et al. showed that greater calprotectin levels were associated with more Prevotella and fewer Akkermansia bacteria in the gut, indicating these bacteria may have inflammatory or protective effects, respectively [26]. However, Santocchi et al. found probiotic therapy, including eight strains of Streptococcus, Bifidobacterium, and Lactobacillus, to have a favorable impact on adaptive functioning in ASD patients but no discernible impact on calprotectin levels with or without GI symptoms [123]. This indicates that the probiotic effect on autistic patients is more complex than the reduction of gut inflammation, and the role of calprotectin as a probable neuroinflammatory mediator should be more studied.
Overall, the heterogeneities of calprotectin studies could be due to the diversity of trialed individuals, the accuracy of the used methods, and insufficient simultaneous studies of microbiota alterations and calprotectin. However, it is still possible to understand that host-microbiota dysbiosis and inflammation-induced calprotectin trigger neuroinflammatory mechanisms that cause autistic aspects.
Gut Microbiota Metabolites and ASD
Many gut microbiota-derived metabolites are highlighted in ASD, such as complex polysaccharides or metabolic amino acids, which can be neurotransmitters [124]. Several of them have been recently discussed as early diagnostic biomarkers of ASD [7]. One significant group of metabolites through which gut microbiota regulates the host physiology is short-chain fatty acids, which primarily constitute acetate (AA), butyrate (BTA), and propionate (PPA).
The genera Prevotella, Bifidobacterium, and Ruminococcus are the primary producers of acetate [125], the most prevalent SCFA, which is reported to be decreased in ASD [29, 126]. BTA is mainly produced by the Firmicutes phylum, more precisely by Lachnospiraceae and Ruminococcaceae families [127], and PPA is synthesized by the Bacteroidetes phylum (including Bacteroides and Prevotella) and Firmicutes phylum (including Roseburia, Blautia and Coprococcus) [128]. However, alongside Bacteroides, the elevated level of PPA is associated with increased Clostridium and Desulfovibrio species in autistic individuals [129]. Also, a study on autistic children revealed lower Bifidobacterium and higher PPA levels, both of which attenuated at older ages [27].
Unlike some studies [28, 29, 126], others reported higher levels of AA, PPA, and BTA in autistic patients compared to control groups [27, 30, 31, 130, 131]. These gut microbiota-related SCFAs exhibit conflicting pro-inflammatory and anti-inflammatory effects in the host's inflammatory response, possibly due to the differences in binding receptors and local concentrations [132]. Some animal studies revealed that supplementation with the microbial metabolites AA and BTA could reverse the social behavioral phenotypes [133,134,135,136]. In contrast, intracerebroventricular injection of PPA in rat brains has induced ASD-like symptoms, including reactive gliosis [137]. It has been understood that PPA can lead to gliosis, disturbed neuro-circuitry, and neuroinflammatory response through modulation of the PTEN/AKT pathway in ASD [138]. As the finding data regarding SCFA levels in autistic patients are inconsistent and yet to be studied [7, 28, 124, 139], additional research is required to verify the potential role of SCFAs in the pathophysiology of ASD. They might be considered as neuroinflammatory biomarkers and indicators of gut microbiota modification in autism patients.
MicroRNAs and ASD
Over 60% of human genes are controlled by microRNAs (miRNAs), small, non-coding RNAs of around 18–24 nucleotides that function as epigenetic regulators. MiRNAs modify brain plasticity and neuronal development, and their dysregulation causes a broad spectrum of neurological impairments, including ASD [140,141,142,143,144]. The importance of miRNAs as regulators of numerous cellular and physiological processes, including hematopoiesis, immune reactions, and inflammation, is well-established [145]. Additionally, miRNAs are affected by host-microbiota interactions and play a key role in dysbiosis and induced inflammations [146,147,148,149]. An intensive study found over-expressed miRNAs in ASD and their possible role in impaired neurodevelopment through dysregulated inflammatory genes [150]. Besides, several studies have identified that miRNAs directly and indirectly activate inflammasomes through their interaction with 3'-UTR genes that modulate inflammasome expression [151].
In detail, animal studies suggest that an increase or decrease of miR-146a can be a potential cause of ASD [152]. A clinical study of the postnatal period compared miRNAs of ASD and healthy controls and confirmed miR-146a as the most dysregulated miRNA in ASD [152]. Using in vitro models and postmortem human brain tissues, another study also found that miR-146a overexpression in the brains of ASD patients is detectable as early as childhood [153]. The changes in Gut microbiota-host interaction could induce miR-146a and consequently promote neuroinflammatory pathways [154]. It is highlighted that miR-146a-induced nuclear factor kappa-B augments the inflammation signaling pathway in the gut-brain axis. It has been shown that Bacteroides fragilis, Lactobacillus rhamnosus GG, Lactobacillus acidophilus, Lactobacillus delbrueckii Bulgaricus, and Escherichia coli Nissle 1917 were linked to miR-146a expression [149, 154, 155]. Another research indicates that miR-146a is essential for certain inflammatory cytokine expression and that its absence in the brain leads to an overall compensatory upregulation of miR-155. Enhanced protein carbonylation and decreased cysteine thiol levels were additional indicators of this elevated neuroinflammatory flux due to an upsurge in oxidative stress mediators [156].
Several studies have identified miR-146a and miR-155 to various pathologic conditions indicated by chronic inflammation [157]. A possible explanation is that gut-derived toxins, such as LPS, capable of traversing the blood–brain barrier and are in systemic circulation, can potentially activate the NF-kB-miRNA-146a-miRNA-155 signaling pathway. This pathway would then transmit pathogenic signals originating from the microbiome to the brain, which might disturb the innate immune reactions and lead to neuroinflammatory conditions [158]. MiR-155 could also be altered by gut microbiota dysbiosis [159]. One study added evidence of increased miR-155 expression in the amygdala, frontal cortex, and cerebellum of children with ASD [62]. miRNA-155 is involved in TLR activation by bacterial lipopolysaccharides, activation of tumor necrosis factor-alpha and IL-6, and regulation of suppressor of cytokine signaling 1 on dendritic cells. These activities, alongside the variation with microbiota dysbiosis, can give a candidate role to miRNA-155 in the neuroinflammatory mechanism of the gut-brain axis and ASD [152, 159]. Earlier studies identified probiotics of Lactobacillus fermentum, Lactobacillus salivarius, Lactobacillus rhamnosus GG, Lactobacillus acidophilus, Lactobacillus delbrueckii, Bifidobacterium bifidum, and E coli Nissle 1917 could change the level of miR-155 [149, 155, 159, 160].
Moreover, studies found upregulated miR-181 in ASD patients, expected to impact the ASD-related neurexin 1 gene [152, 161, 162]. Neuroinflammation and immunological dysregulation are two of the many physiological processes linked to the miR-181 family [163,164,165]. On the other hand, some studies show that gut microbiota could regulate miR-181 in mice [148, 166, 167]. It has also been revealed that Lactobacillus rhamnosus and Lactobacillus delbrueckii probiotics affect the miR-181a expression in inflammatory diseases [160]. Additionally, metabolites derived from gut microbiota could affect miR-181 expression in different states [148]. Altogether, these pieces of evidence strengthen the argument about the possible miR-mediated role of gut microbiota through the neuroinflammatory process in ASD.
Probiotics and ASD
Living microorganisms known as probiotics can influence host health through various mechanisms. According to recent research, they can be used as a therapeutic tool to treat ASD by restoring a healthy balance in the gut microbiota, adjusting the levels of neurotransmitters in the tissues, and reducing inflammation in the gut [168, 169].
Animal models revealed that probiotic supply considerably modified the social and emotional behaviors of the rats as well as blood levels of cytokines like IL-6, IL-17a, and IL-10 [59, 170, 171]. On the other hand, only a few trials assessed the impact of probiotics on ASD with the aspect of inflammatory modulation and immune system regulation (Table 2). Sanctuary et al. evaluated the use of Bifidobacterium infantis in combination with a bovine colostrum product in autistic children. Some patients revealed lower frequency of GI symptoms and aberrant behavior, possibly due to a reduction in TNF-α and IL-13 [172]. Tomova et al. also showed a strong correlation between fecal levels of TNF-α and the severity of autism, indicating the possible involvement of GI inflammation and permeability in ASD through inflammatory pathways. They could significantly decrease the TNF-α levels in the feces of autistic children through probiotic supplementation involving strains of Lactobacillus, Bifidobacteria, and Streptococcus [173]. However, Santocchi et al. found the plasma levels of plasma inflammatory biomarkers, including TNF-α, IL-6, leptin, and plasminogen activator inhibitor 1, and fecal calprotectin contrarily unaffected by the probiotic treatment, involving the same genera as Tomova et al.… Nevertheless, there is a greater improvement in some GI symptoms, adaptive functioning, and sensory profiles in the group treated with probiotics compared to placebo in the subgroup of autistic children with GI problems [123]. Similarly, using strains of Bifidobacterium and Lactobacillus alongside an oligosaccharide could improve disease severity and GI problems in autistic children [174].
Limosilactobacillus genus can also lead to improvement in adaptive symptoms of ASD [175, 177]. However, Schmitt et al. did not see any relevant changes in the plasma TNF-α and HS-CRP, fecal calprotectin, and lactoferrin with the use of this probiotic [175]. Synergic use of Lactiplantibacillus plantarum and oxytocin was also revealed to have an anti-inflammatory effect through the reduction of IL-1β [176]. The probiotic mixture containing five strains of Bifidobacterium longum with anti-inflammatory and high homeostatic intestinal activity, along with Limosilactobacillus fermentum, Lactiplantibacillus plantarum, and Ligilactobacillus salivarius, showed significantly alternation the diversity of gut microbiota. The species that are consistent with this formulation of probiotics were found in the feces of autistic children, including Streptococcus thermophilus, Bifidobacterium longum, Limosilactobacillus fermentum, and Ligilactobacillus salivarius [177].
There are no medicines indicated for the core deficits of ASD. Therefore, there is a substantial requirement for the creation of novel pharmacological approaches for patients with ASD. Overall, these findings support that probiotics may serve as a promising therapy due to their beneficial impact on symptoms of ASD. Considering the existing association between immune system dysfunction and behavioral abnormalities [178] and the possible impact of gut microbiota on ASD through inflammatory mediators, it is suggested that neuroinflammatory variables be examined during probiotic administration and the most effective formulation to alter them be determined.
Conclusion
Given the complexity and lack of clarity surrounding the pathophysiology of ASD, research into the role of inflammatory mechanisms and immunological dysregulation has been raised in recent years. Dysregulation pathways in ASD may also be etiologically traced back to gut microbial alterations and host-microbiota dysbiosis. These changes have been associated with ASD symptoms and severities probably through the released metabolites, neural signaling pathway by BDNF, and neuroinflammatory biomarkers, including S100B, HMGB-1, OPN, miRNAs, RANTES, eotaxin, and GM-CSF. In this review, the role of mediators as a triggering mechanism and bridging cause between gut microbiota dysbiosis-induced inflammation from one side, and neuroinflammatory processes of CNS in autism from the other side is emphasized. Probiotics as an applicable therapeutic option to recover microbiota in ASD suggest the relevance of gut microbiota and potential beneficial impacts. However, further studies are essential to evaluate the efficacy of different probiotic formulations considering microbiota alteration types, coincidence neuroinflammatory mediators, intervention length, and autistic age and symptoms. In fact, many ideas have been proposed to explain ASD pathogenesis, but there is currently a lack of intensive immunological, neurochemical, and microbiota studies in the field. This approach can clinically explain the trajectory through microbiota alteration, related metabolites, neurological inflammatory mediators, and the CNS process of ASD. This constructed dogma can be used to create etiologic, diagnostic, prognostic, or therapeutic targets for ASD.
Data Availability
Not applicable.
Abbreviations
- ASD:
-
Autism spectrum disorder
- SCFAs :
-
Short-Chain Fatty Acids
- BDNF :
-
Brain-derived neurotrophic Factor
- GI:
-
Gastrointestinal
- IL:
-
Interleukin
- TLR:
-
Toll-like receptor
- TNF:
-
Tumor necrosis factor
- S100B:
-
S100 calcium-binding protein beta subunit
- EGCs :
-
Enteric glial cells
- RANTES :
-
Regulated upon Activation, Normal T Cell Expressed and Secreted
- GM-CSF :
-
Granulocyte–macrophage colony-stimulating factor
- HMGB-1 :
-
High mobility group box 1 protein
- OPN:
-
Osteopontin
- AA:
-
Acetate
- BTA :
-
Butyrate
- PPA:
-
Propionate
- miRNA :
-
MicroRNA
References
Fan, Y., and O. Pedersen. 2021. Gut microbiota in human metabolic health and disease. Nature Reviews Microbiology 19 (1): 55–71.
Morais, L.H., H.L. Schreiber IV., and S.K. Mazmanian. 2021. The gut microbiota–brain axis in behaviour and brain disorders. Nature Reviews Microbiology 19 (4): 241–255.
Iglesias-Vázquez, L., Riba G. Van Ginkel, V. Arija, and J. Canals. 2020. Composition of gut microbiota in children with autism spectrum disorder: A systematic review and meta-analysis. Nutrients 12 (3): 792.
Prata, J., A.S. Machado, O. von Doellinger, M.I. Almeida, M.A. Barbosa, R. Coelho, et al. 2019. The contribution of inflammation to autism spectrum disorders: recent clinical evidence. Psychiatric Disorders: Methods and Protocols, 493–510.
Siniscalco, D., S. Schultz, A.L. Brigida, and N. Antonucci. 2018. Inflammation and neuro-immune dysregulations in autism spectrum disorders. Pharmaceuticals. 11 (2): 56.
Doenyas, C. 2018. Gut microbiota, inflammation, and probiotics on neural development in autism spectrum disorder. Neuroscience 374: 271–286.
Shen, L., X. Liu, H. Zhang, J. Lin, C. Feng, and J. Iqbal. 2020. Biomarkers in autism spectrum disorders: Current progress. Clinica Chimica Acta 502: 41–54.
Sharon, G., N.J. Cruz, D.W. Kang, M.J. Gandal, B. Wang, Y.M. Kim, et al. 2019. Human gut microbiota from autism spectrum disorder promote behavioral symptoms in mice. Cell 177 (6): 1600–1618.
Cuomo, M., L. Coretti, D. Costabile, R. Della Monica, G. De Riso, M. Buonaiuto, et al. 2023. Host fecal DNA specific methylation signatures mark gut dysbiosis and inflammation in children affected by autism spectrum disorder. Scientific Reports [Internet] 13 (1): 18197. Available from: https://doi.org/10.1038/s41598-023-45132-0.
Dargenio, V.N., C. Dargenio, S. Castellaneta, A. De Giacomo, M. Laguardia, F. Schettini, et al. 2023. Intestinal Barrier Dysfunction and Microbiota–Gut–Brain Axis: Possible Implications in the Pathogenesis and Treatment of Autism Spectrum Disorder. Nutrients 15 (7): 1620.
Caputi, V., L. Hill, M. Figueiredo, J. Popov, E. Hartung, and N. Pai. 2024. Functional contribution of the intestinal microbiome in autism spectrum disorder, attention deficit hyperactivity disorder, and Rett syndrome: A systematic review of pediatric and adult studies. Frontiers in Neuroscience 18: 1341656.
De Sales-Millán, A., J.F. Aguirre-Garrido, R.M. González-Cervantes, and J.A. Velázquez-Aragón. 2023. Microbiome–Gut–Mucosal–Immune–Brain Axis and Autism Spectrum Disorder (ASD): A Novel Proposal of the Role of the Gut Microbiome in ASD Aetiology. Behavioral Sciences. 13 (7): 548.
Carloni, S., and M. Rescigno. 2023. The gut-brain vascular axis in neuroinflammation. In Seminars in Immunology, 101802. Elsevier.
Chu, J., S. Feng, C. Guo, B. Xue, K. He, and L. Li. 2023. Immunological mechanisms of inflammatory diseases caused by gut microbiota dysbiosis: A review. Biomedicine and Pharmacotherapy 164: 114985.
Anand, N., V.R. Gorantla, and S.B. Chidambaram. 2022. The role of gut dysbiosis in the pathophysiology of neuropsychiatric disorders. Cells 12 (1): 54.
Than, U.T.T., L.T. Nguyen, P.H. Nguyen, X.H. Nguyen, D.P. Trinh, D.H. Hoang, et al. 2023. Inflammatory mediators drive neuroinflammation in autism spectrum disorder and cerebral palsy. Science and Reports 13 (1): 22587.
Usui, N., H. Kobayashi, and S. Shimada. 2023. Neuroinflammation and oxidative stress in the pathogenesis of autism spectrum disorder. International Journal of Molecular Sciences 24 (6): 5487.
Lungba, R.M., S.Z.A. Khan, U. Ajibawo-Aganbi, M.V.P. Bastidas, S. Veliginti, S. Saleem, et al. 2020. The role of the gut microbiota and the immune system in the development of autism. Cureus 12 (10).
Cao, X., K. Liu, J. Liu, Y.W. Liu, L. Xu, H. Wang, et al. 2021. Dysbiotic gut microbiota and dysregulation of cytokine profile in children and teens with autism spectrum disorder. Frontiers in Neuroscience 15: 635925.
Careaga, M., S. Rogers, R.L. Hansen, D.G. Amaral, J. Van de Water, and P. Ashwood. 2017. Immune endophenotypes in children with autism spectrum disorder. Biological Psychiatry 81 (5): 434–441.
Abuaish, S., N.M. Al-Otaibi, T.S. Abujamel, S.A. Alzahrani, S.M. Alotaibi, Y.A. AlShawakir, et al. 2021. Fecal transplant and Bifidobacterium treatments modulate gut Clostridium bacteria and rescue social impairment and hippocampal BDNF expression in a rodent model of autism. Brain Sciences 11 (8): 1038.
Chen, K., Y. Fu, Y. Wang, L. Liao, H. Xu, A. Zhang, et al. 2020. Therapeutic effects of the in vitro cultured human gut microbiota as transplants on altering gut microbiota and improving symptoms associated with autism spectrum disorder. Microbial Ecology 80: 475–486.
Carissimi, C., I. Laudadio, F. Palone, V. Fulci, V. Cesi, F. Cardona, et al. 2019. Functional analysis of gut microbiota and immunoinflammation in children with autism spectrum disorders. Digestive and Liver Disease 2019 07 16th ed 51 (10): 1366–74.
Iovene, M.R., F. Bombace, R. Maresca, A. Sapone, P. Iardino, A. Picardi, et al. 2017. Intestinal dysbiosis and yeast isolation in stool of subjects with autism spectrum disorders. Mycopathologia 182: 349–363.
Tomova, A., K. Soltys, G. Repiska, L. Palkova, D. Filcikova, G. Minarik, et al. 2020. Specificity of gut microbiota in children with autism spectrum disorder in Slovakia and its correlation with astrocytes activity marker and specific behavioural patterns. Physiology and Behavior 214: 112745.
Laghi, L., P. Mastromarino, M. Prosperi, M.A. Morales, S. Calderoni, E. Santocchi, et al. 2021. Are fecal metabolome and microbiota profiles correlated with autism severity? A cross-sectional study on asd preschoolers. Metabolites 11 (10).
Chamtouri, M., N. Gaddour, A. Merghni, M. Mastouri, S. Arboleya, and C.G. De Los Reyes-Gavilán. 2023. Age and severity-dependent gut microbiota alterations in Tunisian children with autism spectrum disorder. Science and Reports 13 (1): 18218.
Liu, S., E. Li, Z. Sun, D. Fu, G. Duan, M. Jiang, et al. 2019. Altered gut microbiota and short chain fatty acids in Chinese children with autism spectrum disorder. Scientific Reports [Internet] 9 (1): 287. Available from: https://doi.org/10.1038/s41598-018-36430-z.
Kang, D.W., Z.E. Ilhan, N.G. Isern, D.W. Hoyt, D.P. Howsmon, M. Shaffer, et al. 2018. Differences in fecal microbial metabolites and microbiota of children with autism spectrum disorders. Anaerobe 49: 121–131.
De Angelis, M., M. Piccolo, L. Vannini, S. Siragusa, A. De Giacomo, D.I. Serrazzanetti, et al. 2013. Fecal microbiota and metabolome of children with autism and pervasive developmental disorder not otherwise specified. PLoS ONE 8 (10): e76993.
Deng, W., S. Wang, F. Li, F. Wang, Y.P. Xing, Y. Li, et al. 2022. Gastrointestinal symptoms have a minor impact on autism spectrum disorder and associations with gut microbiota and short-chain fatty acids. Frontiers in Microbiology 13: 1000419.
Donato, R., B. R cannon, Hsu, K., J Weber, D., G. Sorci, F. Riuzzi, K. Hsu, D. J Weber, et al. 2013. Functions of S100 proteins. Current Molecular Medicine 13 (1): 24–57.
Esnafoglu, E., S.N. Ayyıldız, S. Cırrık, E.Y. Erturk, A. Erdil, A. Daglı, et al. 2017. Evaluation of serum Neuron-specific enolase, S100B, myelin basic protein and glial fibrilliary acidic protein as brain specific proteins in children with autism spectrum disorder. International Journal of Developmental Neuroscience. 61: 86–91.
Kartalcı, G., A. Çalışkan Demir, Ş Kartalcı, N. Üremiş, and Y. Türköz. 2022. Evaluation of blood Zonulin levels, inflammatory processes and neuronal changes in children with autism spectrum disorder. Psychiatria Danubina 34 (2): 279–287.
Pan, M., J.M. Roe, R. Nudel, A.J. Schork, O. Iakunchykova, A.M. Fjell, et al. 2023. Circulating S100B levels at birth and risk of six major neuropsychiatric or neurological disorders: A two-sample Mendelian Randomization Study. Translational Psychiatry 13 (1): 174.
Al-Ayadhi, L.Y., and G.A. Mostafa. 2012. A lack of association between elevated serum levels of S100B protein and autoimmunity in autistic children. Journal of Neuroinflammation 9: 1–8.
Shaker, N.M., G. Taha, H. Kholeif, N.M. Sayed, M.M. El-Sheikh, and M.L. Abulmagd. 2016. Serum levels of S100b, interleukin-6 and anti-transglutaminase Ii IgA as immune markers in a sample of Egyptian children with autistic spectrum disorders. Autism Open Access. 6 (5): 1–7.
Tomova, A., P. Keményová, D. Filčíková, Ž Szapuová, A. Kováč, K. Babinská, et al. 2019. Plasma levels of glial cell marker S100B in children with autism. Physiological Research 68: S315–S323.
Abou-Donia, M.B., H.B. Suliman, D. Siniscalco, N. Antonucci, P. ElKafrawy, and M.V. Brahmajothi. 2019. De novo blood biomarkers in autism: Autoantibodies against neuronal and glial proteins. Behavioral Sciences 9 (5): 47.
Ayaydın, H., A. Kirmit, H. Çelik, İ Akaltun, İ Koyuncu, and ŞB. Ulgar. 2020. High serum levels of serum 100 beta protein, neuron-specific enolase, Tau, active caspase-3, M30 and M65 in children with autism spectrum disorders. Clinical Psychopharmacology and Neuroscience. 18 (2): 270.
Babinská, K., A. Tomova, H. Celušáková, J. Babková, G. Repiská, A. Kubranská, et al. 2017. Fecal calprotectin levels correlate with main domains of the autism diagnostic interview-revised (ADI-R) in a sample of individuals with autism spectrum disorders from Slovakia. Physiological Research 66 (Suppl 4): S517–S522.
Romano Spica, V., F. Valeriani, M. Orsini, M.E. Clementi, L. Seguella, G. Gianfranceschi, et al. 2023. S100B Affects Gut Microbiota Biodiversity. International Journal of Molecular Sciences 24 (3): 2248.
Berding, K., and S.M. Donovan. 2016. Microbiome and nutrition in autism spectrum disorder: Current knowledge and research needs. Nutrition Reviews 74 (12): 723–736.
Lu, B. 2003. BDNF and activity-dependent synaptic modulation. Learning & memory. 10 (2): 86–98.
Angelucci, F., S. Brene, and A.A. Mathe. 2005. BDNF in schizophrenia, depression and corresponding animal models. Molecular Psychiatry 10 (4): 345–352.
Maussion, G., J.M. Moalic, M. Simonneau, P. Gorwood, and N. Ramoz. 2019. Increased expression of BDNF mRNA in the frontal cortex of autistic patients. Behavioural Brain Research [Internet] 359: 903–9. Available from: https://www.sciencedirect.com/science/article/pii/S0166432818302304.
Barbosa, A.G., R. Pratesi, G.S.C. Paz, M.A.A.L. dos Santos, R.H. Uenishi, E.Y. Nakano, et al. 2020. Assessment of BDNF serum levels as a diagnostic marker in children with autism spectrum disorder. Scientific Reports [Internet] 10 (1): 17348. Available from: https://doi.org/10.1038/s41598-020-74239-x.
Farmer, C.A., A.E. Thurm, B. Honnekeri, P. Kim, S.E. Swedo, and J.C. Han. 2021. The contribution of platelets to peripheral BDNF elevation in children with autism spectrum disorder. Scientific Reports [Internet]. 11 (1): 18158. Available from: https://doi.org/10.1038/s41598-021-97367-4.
Elhamid, S.A.A., M.M. Alkherkhisy, and R.E. Kasem. 2024. Assessment of brain-derived neurotrophic factor levels in serum of children with autism spectrum disorders. Middle East Current Psychiatry. 31 (1): 18.
Cui, T., Z. Liu, Z. Li, Y. Han, W. Xiong, Z. Qu, et al. 2024. Serum brain-derived neurotrophic factor concentration is different between autism spectrum disorders and intellectual disability children and adolescents. Journal of Psychiatric Research 170: 355–360.
Kasarpalkar, N.J., S.T. Kothari, and U.P. Dave. 2014. Brain-derived neurotrophic factor in children with autism spectrum disorder. Annals of Neurosciences 21 (4): 129.
Singh, R., A. Kisku, H. Kungumaraj, V. Nagaraj, A. Pal, S. Kumar, et al. 2023. Autism Spectrum Disorders: A Recent Update on Targeting Inflammatory Pathways with Natural Anti-Inflammatory Agents. Biomedicines 11 (1): 115.
Calabrese, F., A.C. Rossetti, G. Racagni, P. Gass, M.A. Riva, and R. Molteni. 2014. Brain-derived neurotrophic factor: A bridge between inflammation and neuroplasticity. Frontiers in Cellular Neuroscience 8: 430.
Porter, G.A., and J.C. O’Connor. 2022. Brain-derived neurotrophic factor and inflammation in depression: Pathogenic partners in crime? World Journal of Psychiatry 12 (1): 77.
Mehra, A., G. Arora, G. Sahni, M. Kaur, H. Singh, B. Singh, et al. 2023. Gut microbiota and Autism Spectrum Disorder: From pathogenesis to potential therapeutic perspectives. Journal of Traditional & Complementary Medicine 13 (2): 135–149.
Sudo, N., Y. Chida, Y. Aiba, J. Sonoda, N. Oyama, X. Yu, et al. 2004. Postnatal microbial colonization programs the hypothalamic–pituitary–adrenal system for stress response in mice. Journal of Physiology 558 (1): 263–275.
Dehghani, F., S. Abdollahi, F. Shidfar, C.C.T. Clark, and S. Soltani. 2022. Probiotics supplementation and brain-derived neurotrophic factor (BDNF): a systematic review and meta-analysis of randomized controlled trials. Nutritional Neuroscience 1–11.
Maqsood, R., and T.W. Stone. 2016. The Gut-Brain Axis, BDNF, NMDA and CNS Disorders. Neurochemical Research [Internet] 41 (11): 2819–35. Available from: https://doi.org/10.1007/s11064-016-2039-1.
Sunand, K., G.K. Mohan, and V. Bakshi. 2020. Supplementation of lactobacillus probiotic strains supports gut-brain-axis and defends autistic deficits occurred by valproic acid-induced prenatal model of autism. Pharmacognosy Journal 12 (6s).
Wang, B., Y. Qin, Q. Wu, X. Li, D. Xie, Z. Zhao, et al. 2022. mTOR signaling pathway regulates the release of proinflammatory molecule CCL5 implicated in the pathogenesis of autism spectrum disorder. Frontiers in Immunology 13: 818518.
Roy-O’Reilly, M., R.M. Ritzel, S.E. Conway, I. Staff, G. Fortunato, and L.D. McCullough. 2017. CCL11 (Eotaxin-1) levels predict long-term functional outcomes in patients following ischemic stroke. Translational Stroke Research 8: 578–84.
Rastegari, M., N. Salehi, and F. Zare-Mirakabad. 2023. Biomarker prediction in autism spectrum disorder using a network-based approach. BMC Medical Genomics 16 (1): 12.
Shen, Y., J. Ou, M. Liu, L. Shi, Y. Li, L. Xiao, et al. 2016. Altered plasma levels of chemokines in autism and their association with social behaviors. Psychiatry Research 244: 300–305.
Han, Y.M.Y., W.K.Y. Cheung, C.K. Wong, S.L. Sze, T.W.S. Cheng, M.K. Yeung, et al. 2017. Distinct cytokine and chemokine profiles in autism spectrum disorders. Frontiers in Immunology 8: 11.
Han, Y.M.Y., S.Y. Yau, M.M.Y. Chan, C.K. Wong, and A.S. Chan. 2022. Altered Cytokine and BDNF Levels in Individuals with Autism Spectrum Disorders. Brain Sciences 12 (4): 460.
Ashwood, P., P. Krakowiak, I. Hertz-Picciotto, R. Hansen, I.N. Pessah, and J. Van de Water. 2011. Associations of impaired behaviors with elevated plasma chemokines in autism spectrum disorders. Journal of Neuroimmunology 232 (1–2): 196–199.
Hu, C., X. Xu, G. Xiong, Q. Xu, B. Zhou, C. Li, et al. 2018. Alterations in plasma cytokine levels in chinese children with autism spectrum disorder. Autism Research. 11 (7): 989–999.
Masi, A., D.S. Quintana, N. Glozier, A.R. Lloyd, I.B. Hickie, and A.J. Guastella. 2015. Cytokine aberrations in autism spectrum disorder: A systematic review and meta-analysis. Molecular Psychiatry 20 (4): 440–446.
Shahi, S.K., S. Ghimire, P. Lehman, and A.K. Mangalam. 2022. Obesity induced gut dysbiosis contributes to disease severity in an animal model of multiple sclerosis. Frontiers in Immunology 13: 966417.
Ye, J., H. Wang, L. Cui, S. Chu, and N. Chen. 2021. The progress of chemokines and chemokine receptors in autism spectrum disorders. Brain Research Bulletin 174: 268–280.
Ge, Y., X. Wang, Y. Guo, J. Yan, A. Abuduwaili, K. Aximujiang, et al. 2021. Gut microbiota influence tumor development and Alter interactions with the human immune system. Journal of Experimental & Clinical Cancer Research 40 (1): 1–9.
Tremaroli, V., and F. Bäckhed. 2012. Functional interactions between the gut microbiota and host metabolism. Nature 489 (7415): 242–249.
Al Bander, Z., M.D. Nitert, A. Mousa, and N. Naderpoor. 2020. The gut microbiota and inflammation: An overview. International Journal of Environmental Research and Public Health 17 (20): 7618.
Elinav, E., T. Strowig, A.L. Kau, J. Henao-Mejia, C.A. Thaiss, C.J. Booth, et al. 2011. NLRP6 inflammasome regulates colonic microbial ecology and risk for colitis. Cell 145 (5): 745–757.
Hu, B., E. Elinav, S. Huber, T. Strowig, L. Hao, A. Hafemann, et al. 2013. Microbiota-induced activation of epithelial IL-6 signaling links inflammasome-driven inflammation with transmissible cancer. Proceedings of the National Academy of Sciences. 110 (24): 9862–9867.
Takahashi, K., Y. Sugi, K. Nakano, T. Kobayakawa, Y. Nakanishi, M. Tsuda, et al. 2020. Regulation of gene expression through gut microbiota-dependent DNA methylation in colonic epithelial cells. Immunohorizons 4 (4): 178–190.
Goyal, D., S.A. Ali, and R.K. Singh. 2021. Emerging role of gut microbiota in modulation of neuroinflammation and neurodegeneration with emphasis on Alzheimer’s disease. Progress in Neuro-Psychopharmacology and Biological Psychiatry 106: 110112.
Parker, A., S. Romano, R. Ansorge, A. Aboelnour, G. Le Gall, G.M. Savva, et al. 2022. Fecal microbiota transfer between young and aged mice reverses hallmarks of the aging gut, eye, and brain. Microbiome 10 (1): 1–25.
Brandi, J., S. Cheri, M. Manfredi, C. Di Carlo, V. Vita Vanella, F. Federici, et al. 2020. Exploring the wound healing, anti-inflammatory, anti-pathogenic and proteomic effects of lactic acid bacteria on keratinocytes. Scientific Reports [Internet] 10: 11572. https://doi.org/10.1038/s41598-020-68483-4.
Wei, L., L. Fei, X. Ning, T. Haiming, G. Lixin, and M. Xianqin. 2017. Antiallergic effects of probiotic Lactobacillus rhamnosus GG (LGG) on allergic rhinitis induced by ovalbumin in rats. Biomedical Research 28 (1): 111–117.
Wu, Z., E. Mehrabi Nasab, P. Arora, and S.S. Athari. 2022. Study effect of probiotics and prebiotics on treatment of OVA-LPS-induced of allergic asthma inflammation and pneumonia by regulating the TLR4/NF-kB signaling pathway. Journal of Translational Medicine 20 (1): 130.
Xu, N., X. Li, and Y. Zhong. 2015. Inflammatory cytokines: potential biomarkers of immunologic dysfunction in autism spectrum disorders. Mediators of Inflammation 2015.
Ahmad, S.F., M.A. Ansari, A. Nadeem, S.A. Bakheet, L.Y. Al-Ayadhi, A.F. Alasmari, et al. 2020. Involvement of CD45 cells in the development of autism spectrum disorder through dysregulation of granulocyte-macrophage colony-stimulating factor, key inflammatory cytokines, and transcription factors. International Immunopharmacology 83: 106466.
Alomar, H.A., M.A. Ansari, A. Nadeem, S.M. Attia, S.A. Bakheet, H.A. Al-Mazroua, et al. 2023. A potent and selective CXCR2 antagonist improves neuroimmune dysregulation through the inhibition of NF-κB and notch inflammatory signaling in the BTBR mouse model of autism. Journal of Neuroimmunology 377: 578069.
Rose, D., and P. Ashwood. 2014. Potential cytokine biomarkers in autism spectrum disorders. Biomarkers in Medicine 8 (9): 1171–1181.
Manzardo, A.M., R. Henkhaus, S. Dhillon, and M.G. Butler. 2012. Plasma cytokine levels in children with autistic disorder and unrelated siblings. International Journal of Developmental Neuroscience 30 (2): 121–127.
Ashwood, P. 2023. Preliminary findings of elevated inflammatory plasma cytokines in children with autism who have co-morbid gastrointestinal symptoms. Biomedicines 11 (2): 436.
Takada, R., M. Toritsuka, T. Yamauchi, R. Ishida, Y. Kayashima, Y. Nishi, et al. 2024. Granulocyte macrophage colony-stimulating factor-induced macrophages of individuals with autism spectrum disorder adversely affect neuronal dendrites through the secretion of pro-inflammatory cytokines. Molecular Autism 15 (1): 1–16.
Dehhaghi, M., H. Kazemi Shariat Panahi, B. Heng, and G.J. Guillemin. 2020. The gut microbiota, kynurenine pathway, and immune system interaction in the development of brain cancer. Frontiers in Cell and Developmental Biology 8: 562812.
Dery, K.J., K. Kadono, H. Hirao, A. Górski, and J.W. Kupiec-Weglinski. 2020. Microbiota in organ transplantation: An immunological and therapeutic conundrum? Cellular Immunology 351: 104080.
Wang, J., X. Chen, J. Li, and M. Ishfaq. 2021. Gut microbiota dysbiosis aggravates mycoplasma gallisepticum colonization in the chicken lung. Frontiers in Veterinary Science 8: 788811.
Wu, Y.N., L. Zhang, T. Chen, X. Li, L.H. He, and G.X. Liu. 2020. Granulocyte-macrophage colony-stimulating factor protects mice against hepatocellular carcinoma by ameliorating intestinal dysbiosis and attenuating inflammation. World Journal of Gastroenterology 26 (36): 5420.
Chen, Y., Z. Li, K.D. Tye, H. Luo, X. Tang, Y. Liao, et al. 2019. Probiotic supplementation during human pregnancy affects the gut microbiota and immune status. Frontiers in Cellular and Infection Microbiology 9: 254.
Di Salvo, E., M. Casciaro, S. Quartuccio, L. Genovese, and S. Gangemi. 2018. Do Alarmins Have a Potential Role in Autism Spectrum Disorders Pathogenesis and Progression? Biomolecules 2018 12 20th ed 9 (1): 2.
Kang, R., R. Chen, Q. Zhang, W. Hou, S. Wu, L. Cao, et al. 2014. HMGB1 in health and disease. Molecular Aspects of Medicine 2014 07 08th ed 40: 1–116.
Fang, P., M. Schachner, and Y.Q. Shen. 2012. HMGB1 in development and diseases of the central nervous system. Molecular Neurobiology 2012 05 13th ed 45 (3): 499–506.
Xue, J., J.S. Suarez, M. Minaai, S. Li, G. Gaudino, H.I. Pass, et al. 2021. HMGB1 as a therapeutic target in disease. Journal of Cellular Physiology 2020 10 26th ed 236 (5): 3406–19.
Dipasquale, V., M.C. Cutrupi, L. Colavita, S. Manti, C. Cuppari, and C. Salpietro. 2017. Neuroinflammation in autism spectrum disorders: role of high mobility group box 1 protein. International Journal of Molecular and Cellular Medicine 2017 09 26th ed 6 (3): 148–55.
Emanuele, E., M. Boso, N. Brondino, S. Pietra, F. Barale, S. Ucelli di Nemi, et al. 2010. Increased serum levels of high mobility group box 1 protein in patients with autistic disorder. Progress in Neuro-Psychopharmacology and Biological Psychiatry 2010 03 17th ed 34 (4): 681–3.
Makris, G., G. Chouliaras, F. Apostolakou, C. Papageorgiou, G.P. Chrousos, I. Papassotiriou, et al. 2021. Increased serum concentrations of high mobility group box 1 (HMGB1) protein in children with autism spectrum disorder. Children (Basel) 2021 06 05th ed 8 (6).
Russo, A.J. 2014. Increased Epidermal Growth Factor Receptor (EGFR) Associated with Hepatocyte Growth Factor (HGF) and Symptom Severity in Children with Autism Spectrum Disorders (ASDs). Journal of Central Nervous System Disease 2014 09 09th ed 6: 79–83.
Russo, A.J. 2013. Decreased epidermal growth factor (EGF) associated with HMGB1 and increased hyperactivity in children with autism. Biomark Insights 2013 04 04th ed 8 (1): 35–41.
Babinská, K., M. Bucová, V. Ďurmanová, S. Lakatošová, D. Jánošíková, J. Bakoš, et al. 2014. Increased plasma levels of the high mobility group box 1 protein (HMGB1) are associated with a higher score of gastrointestinal dysfunction in individuals with autism. Physiological Research 63 (Suppl 4): S613–S618.
Rubas, N.C., R. Peres, B.P. Kunihiro, N.P. Allan, K. Phankitnirundorn, R.K. Wells, et al. 2024. HMGB1 mediates microbiome-immune axis dysregulation underlying reduced neutralization capacity in obesity-related post-acute sequelae of SARS-CoV-2. Science and Reports 14 (1): 355.
Reisi-Vanani, V., Z. Lorigooini, E. Bijad, and H. Amini-Khoei. 2023. Maternal separation stress through triggering of the neuro-immune response in the hippocampus induces autistic-like behaviors in male mice. International Journal of Developmental Neuroscience.
Kıyat, E., E. Aktepe, D. Kumbul Doğuç, M. Bedir, E. Ertürk, and Ü. Işık. 2024. Comparison of HMGB1, RAGE, TLR4, and NF-κB levels in children and adolescents diagnosed with autism spectrum disorder with healthy controls. International Journal of Developmental Disabilities 1–8.
Saresella, M., I. Marventano, F.R. Guerini, R. Mancuso, L. Ceresa, M. Zanzottera, et al. 2009. An autistic endophenotype results in complex immune dysfunction in healthy siblings of autistic children. Biological Psychiatry 2009 08 22nd ed 66 (10): 978–84.
Saresella, M., F. Piancone, I. Marventano, M. Zoppis, A. Hernis, M. Zanette, et al. 2016. Multiple inflammasome complexes are activated in autistic spectrum disorders. Brain, Behavior, and Immunity 57: 125–33.
Mao, D., Y. Zheng, F. Xu, X. Han, and H. Zhao. 2022. HMGB1 in nervous system diseases: A common biomarker and potential therapeutic target. Frontiers in Neurology 13: 1029891.
Wesson, J.A., R.J. Johnson, M. Mazzali, A.M. Beshensky, S. Stietz, C. Giachelli, et al. 2003. Osteopontin is a critical inhibitor of calcium oxalate crystal formation and retention in renal tubules. Journal of the American Society of Nephrology 14 (1): 139–147.
Al-ayadhi, L.Y., and G.A. Mostafa. 2011. Increased serum osteopontin levels in autistic children: relation to the disease severity. Brain, Behavior, and Immunity 25 (7): 1393–8.
Heilmann, K., U. Hoffmann, E. Witte, C. Loddenkemper, C. Sina, S. Schreiber, et al. 2009. Osteopontin as two-sided mediator of intestinal inflammation. Journal of Cellular and Molecular Medicine 13 (6): 1162–1174.
Yu, H., X. Liu, and Y. Zhong. 2017. The Effect of Osteopontin on Microglia. BioMed Research International 2017: 1879437.
Lopes, K.D., L. Yu, X. Shen, Y. Qiu, S. Tasaki, A. Iatrou, et al. 2024. Associations of cortical SPP1 and ITGAX with cognition and common neuropathologies in older adults. Alzheimer’s and Dementia 20 (1): 525–37.
Chen, J., P. Zeng, L. Gong, X. Zhang, Z. Ling, K. Bi, et al. 2022. Osteopontin exacerbates high-fat diet-induced metabolic disorders in a microbiome-dependent manner. mBio 13 (6): e02531-22.
Sidler, M.A., S.T. Leach, and A.S. Day. 2008. Fecal S100A12 and fecal calprotectin as noninvasive markers for inflammatory bowel disease in children. Inflammatory Bowel Diseases 14 (3): 359–366.
De Magistris, L., V. Familiari, A. Pascotto, A. Sapone, A. Frolli, P. Iardino, et al. 2010. Alterations of the intestinal barrier in patients with autism spectrum disorders and in their first-degree relatives. Journal of Pediatric Gastroenterology and Nutrition 51 (4): 418–424.
Azouz, H.G., N.H.E. Zakaria, A.F. Khalil, S.M. Naguib, and M. Khalil. 2021. Gastrointestinal manifestations and their relation to faecal calprotectin in children with autism. Gastroenterology Review/Przegląd Gastroenterologiczny 16 (4): 352–7.
Fernell, E., U.L. Fagerberg, and P.M. Hellström. 2007. No evidence for a clear link between active intestinal inflammation and autism based on analyses of faecal calprotectin and rectal nitric oxide. Acta Paediatrica, International Journal of Paediatrics 96 (7): 1076–1079.
Pusponegoro, H.D., S. Ismael, S. Sastroasmoro, A. Firmansyah, and Y. Vandenplas. 2015. Maladaptive behavior and gastrointestinal disorders in children with autism spectrum disorder. Journal of Pediatric Gastroenterology and Nutrition 18 (4): 230–237.
Strati, F., D. Cavalieri, D. Albanese, C. De Felice, C. Donati, J. Hayek, et al. 2017. New evidences on the altered gut microbiota in autism spectrum disorders. Microbiome 5: 1–11.
Alookaran, J., Y. Liu, T.A. Auchtung, A. Tahanan, M. Hessabi, P. Asgarisabet, et al. 2022. Fungi: Friend or foe? A mycobiome evaluation in children with autism and gastrointestinal symptoms. Journal of Pediatric Gastroenterology and Nutrition 74 (3): 377–382.
Santocchi, E., L. Guiducci, M. Prosperi, S. Calderoni, M. Gaggini, F. Apicella, et al. 2020. Effects of probiotic supplementation on gastrointestinal, sensory and core symptoms in autism spectrum disorders: A randomized controlled trial. Front Psychiatry 11: 550593.
Peralta-Marzal, L.N., N. Prince, D. Bajic, L. Roussin, L. Naudon, S. Rabot, et al. 2021. The impact of gut microbiota-derived metabolites in autism spectrum disorders. International Journal of Molecular Sciences 22 (18): 10052.
Koh, A., F. De Vadder, P. Kovatcheva-Datchary, and F. Bäckhed. 2016. From dietary fiber to host physiology: Short-chain fatty acids as key bacterial metabolites. Cell 165 (6): 1332–1345.
Adams, J.B., L.J. Johansen, L.D. Powell, D. Quig, and R.A. Rubin. 2011. Gastrointestinal flora and gastrointestinal status in children with autism–comparisons to typical children and correlation with autism severity. BMC Gastroenterology 11: 1–13.
Louis, P., and H.J. Flint. 2017. Formation of propionate and butyrate by the human colonic microbiota. Environmental Microbiology 19 (1): 29–41.
Louis, P., G.L. Hold, and H.J. Flint. 2014. The gut microbiota, bacterial metabolites and colorectal cancer. Nature Reviews Microbiology 12 (10): 661–672.
MacFabe, D.F. 2012. Short-chain fatty acid fermentation products of the gut microbiome: Implications in autism spectrum disorders. Microbial Ecology in Health and Disease 23 (1): 19260.
Coretti, L., L. Paparo, M.P. Riccio, F. Amato, M. Cuomo, A. Natale, et al. 2018. Gut microbiota features in young children with autism spectrum disorders. Frontiers in Microbiology 9: 3146.
Wang, L., C.T. Christophersen, M.J. Sorich, J.P. Gerber, M.T. Angley, and M.A. Conlon. 2012. Elevated fecal short chain fatty acid and ammonia concentrations in children with autism spectrum disorder. Digestive Diseases and Sciences 57: 2096–2102.
Yao, Y., X. Cai, W. Fei, Y. Ye, M. Zhao, and C. Zheng. 2022. The role of short-chain fatty acids in immunity, inflammation and metabolism. Critical Reviews in Food Science and Nutrition 62 (1): 1–12.
Osman, A., N.L. Mervosh, A.N. Strat, T.J. Euston, G. Zipursky, R.M. Pollak, et al. 2020. Acetate supplementation rescues social deficits and alters transcriptional regulation in prefrontal cortex of Shank3 deficient mice.
Wang, X., Z. Sun, T. Yang, F. Lin, S. Ye, J. Yan, et al. 2023. Sodium butyrate facilitates CRHR2 expression to alleviate HPA axis hyperactivity in autism-like rats induced by prenatal lipopolysaccharides through histone deacetylase inhibition. mSystems e00415-23.
Cristiano, C., E. Hoxha, P. Lippiello, I. Balbo, R. Russo, F. Tempia, et al. 2022. Maternal treatment with sodium butyrate reduces the development of autism-like traits in mice offspring. Biomedicine & Pharmacotherapy 156: 113870.
Kratsman, N., D. Getselter, and E. Elliott. 2016. Sodium butyrate attenuates social behavior deficits and modifies the transcription of inhibitory/excitatory genes in the frontal cortex of an autism model. Neuropharmacology 102: 136–145.
MacFabe, D.F., K. Rodríguez-Capote, J.E. Hoffman, A.E. Franklin, Y. Mohammad-Asef, A.R. Taylor, et al. 2008. A novel rodent model of autism: Intraventricular infusions of propionic acid increase locomotor activity and induce neuroinflammation and oxidative stress in discrete regions of adult rat brain. American Journal of Biochemistry and Biotechnology 4 (2): 146–166.
Abdelli, L.S., A. Samsam, and S.A. Naser. 2019. Propionic acid induces gliosis and neuro-inflammation through modulation of PTEN/AKT pathway in autism spectrum disorder. Scientific Reports [Internet] 9 (1): 8824. Available from: https://doi.org/10.1038/s41598-019-45348-z.
Wang, J., J. Pan, H. Chen, Y. Li, W.K. Amakye, J. Liang, et al. 2019. Fecal short-chain fatty acids levels were not associated with autism spectrum disorders in chinese children: a case-control study. Frontiers in Neuroscience [Internet] 13. Available from: https://www.frontiersin.org/articles/10.3389/fnins.2019.01216.
Garrido-Torres, N., K. Guzmán-Torres, S. García-Cerro, G. Pinilla Bermúdez, C. Cruz-Baquero, H. Ochoa, et al. 2023. miRNAs as biomarkers of autism spectrum disorder: a systematic review and meta-analysis. European Child and Adolescent Psychiatry, 1–34.
Mehmetbeyoglu, E., A. Duman, S. Taheri, Y. Ozkul, and M. Rassoulzadegan. 2023. From data to insights: Machine learning empowers prognostic biomarker prediction in Autism. Journal of Personalized Medicine 13 (12): 1713.
Vaccaro, T.D., J.M. Sorrentino, S. Salvador, T. Veit, D.O. Souza, and R.F. De Almeida. 2018. Alterations in the microRNA of the blood of autism spectrum disorder patients: effects on epigenetic regulation and potential biomarkers. Behavioral Sciences 8 (8): 75.
Seno, M.M.G., P. Hu, F.G. Gwadry, D. Pinto, C.R. Marshall, G. Casallo, et al. 2011. Gene and miRNA expression profiles in autism spectrum disorders. Brain Research 1380: 85–97.
Ozkul, Y., S. Taheri, K.K. Bayram, E.F. Sener, E. Mehmetbeyoglu, D.B. Öztop, et al. 2020. A heritable profile of six miRNAs in autistic patients and mouse models. Science and Reports 10 (1): 9011.
Chatterjee, B., M. Sarkar, S. Bose, M.T. Alam, A.A. Chaudhary, A.K. Dixit, et al. 2024. MicroRNAs: Key modulators of inflammation-associated diseases. In Seminars in Cell and Developmental Biology, 364–73. Elsevier.
Wortelboer, K., G.J. Bakker, M. Winkelmeijer, N. van Riel, E. Levin, M. Nieuwdorp, et al. 2022. Fecal microbiota transplantation as tool to study the interrelation between microbiota composition and miRNA expression. Microbiological Research 257: 126972.
Nikolaieva, N., A. Sevcikova, R. Omelka, M. Martiniakova, M. Mego, and S. Ciernikova. 2022. Gut Microbiota–MicroRNA Interactions in Intestinal Homeostasis and Cancer Development. Microorganisms 11 (1): 107.
Fardi, F., L.B. Khasraghi, N. Shahbakhti, A.S. Naseriyan, S. Najafi, S. Sanaaee, et al. 2023. An interplay between non-coding RNAs and gut microbiota in human health. Diabetes Research and Clinical Practice 110739.
Behrouzi, A., F. Ashrafian, H. Mazaheri, A. Lari, M. Nouri, F.R. Rad, et al. 2020. The importance of interaction between MicroRNAs and gut microbiota in several pathways. Microbial Pathogenesis 144: 104200.
Chiappori, F., F.A. Cupaioli, A. Consiglio, N. Di Nanni, E. Mosca, V.F. Licciulli, et al. 2022. Analysis of Faecal Microbiota and Small ncRNAs in Autism: Detection of miRNAs and piRNAs with Possible Implications in Host-Gut Microbiota Cross-Talk. Nutrients 14 (7): 1340.
Yi, Y.S. 2024. MicroRNA-mediated epigenetic regulation of inflammasomes in inflammatory responses and immunopathologies. In Seminars in Cell and Developmental Biology, 227–38. Elsevier.
Li, J., X. Xu, J. Liu, S. Zhang, X. Tan, Z. Li, et al. 2022. Decoding microRNAs in autism spectrum disorder. Molecular Therapy-Nucleic Acids 30: 535–546.
Nguyen, L.S., J. Fregeac, C. Bole-Feysot, N. Cagnard, A. Iyer, J. Anink, et al. 2018. Role of miR-146a in neural stem cell differentiation and neural lineage determination: Relevance for neurodevelopmental disorders. Molecular Autism 9: 1–12.
Li, M., W.D. Chen, and Y.D. Wang. 2020. The roles of the gut microbiota–miRNA interaction in the host pathophysiology. Molecular Medicine 26: 1–9.
Davoodvandi, A., H. Marzban, P. Goleij, A. Sahebkar, K. Morshedi, S. Rezaei, et al. 2021. Effects of therapeutic probiotics on modulation of microRNAs. Cell Communication and Signaling [Internet] 19 (1): 4. Available from: https://doi.org/10.1186/s12964-020-00668-w.
Zhao, W., J.G. Spiers, N. Vassileff, A. Khadka, E.J. Jaehne, M. van den Buuse, et al. 2023. microRNA-146a modulates behavioural activity, neuroinflammation, and oxidative stress in adult mice. Molecular and Cellular Neuroscience 124.
Testa, U., E. Pelosi, G. Castelli, and C. Labbaye. 2017. miR-146 and miR-155: Two key modulators of immune response and tumor development. Noncoding RNA 3 (3): 22.
Alexandrov, P., Y. Zhao, W. Li, and W. Lukiw. 2019. Lipopolysaccharide-stimulated, NF-kB-, miRNA-146a-and miRNA-155-mediated molecular-genetic communication between the human gastrointestinal tract microbiome and the brain. Folia neuropathologica 57 (3): 211–9.
Yan, X.Y., J.P. Yao, Y.Q. Li, W. Zhang, M.H. Xi, M. Chen, et al. 2022. Global trends in research on miRNA–microbiome interaction from 2011 to 2021: A bibliometric analysis. Frontiers in Pharmacology 13: 974741.
Vahidi, Z., M. Samadi, M. Mahmoudi, Z. RezaieYazdi, M. Sahebari, N. Tabasi, et al. 2018. Lactobacillus rhamnosus and Lactobacillus delbrueckii ameliorate the expression of miR-155 and miR-181a in SLE patients. Journal of functional foods [Internet] 48: 228–33. Available from: https://www.sciencedirect.com/science/article/pii/S1756464618303608.
Schepici, G., E. Cavalli, P. Bramanti, and E. Mazzon. 2019. Autism spectrum disorder and miRNA: An overview of experimental models. Brain Sciences 9 (10): 265.
Frye, R.E., S. Rose, S. McCullough, S.C. Bennuri, P.A. Porter-Gill, H. Dweep, et al. 2021. MicroRNA expression profiles in autism spectrum disorder: Role for miR-181 in immunomodulation. Journal of Personalized Medicine 11 (9): 922.
Zhu, J., F.L. Wang, H.B. Wang, N. Dong, X.M. Zhu, Y. Wu, et al. 2017. TNF-α mRNA is negatively regulated by microRNA-181a-5p in maturation of dendritic cells induced by high mobility group box-1 protein. Scientific Reports [Internet] 7 (1): 12239. Available from: https://doi.org/10.1038/s41598-017-12492-3.
Hutchison, E.R., E.M. Kawamoto, D.D. Taub, A. Lal, K. Abdelmohsen, Y. Zhang, et al. 2013. Evidence for miR-181 involvement in neuroinflammatory responses of astrocytes. Glia 61 (7): 1018–1028.
Williams, A., J. Henao-Mejia, C.C.D. Harman, and R.A. Flavell. 2013. miR-181 and metabolic regulation in the immune system. In Cold Spring Harbor symposia on quantitative biology, 223–30. Cold Spring Harbor Laboratory Press.
Virtue, A.T., S.J. McCright, J.M. Wright, M.T. Jimenez, W.K. Mowel, J.J. Kotzin, et al. 2019. The gut microbiota regulates white adipose tissue inflammation and obesity via a family of microRNAs. Science Translational Medicine 11 (496): eaav1892.
Fan, Y., M. Qin, J. Zhu, X. Chen, J. Luo, T. Chen, et al. 2022. MicroRNA sensing and regulating microbiota-host crosstalk via diet motivation. Critical Reviews in Food Science and Nutrition 1–18.
Dinan, T.G., C. Stanton, and J.F. Cryan. 2013. Psychobiotics: A novel class of psychotropic. Biological Psychiatry 74 (10): 720–726.
Ng, Q.X., Soh AY, W. Loke, D.Y. Lim, and W.S. Yeo. 2018. The role of inflammation in irritable bowel syndrome (IBS). The Journal of Inflammation Research 345–9.
Adıgüzel, E., B. Çiçek, G. Ünal, M.F. Aydın, and D. Barlak-Keti. 2022. Probiotics and prebiotics alleviate behavioral deficits, inflammatory response, and gut dysbiosis in prenatal VPA-induced rodent model of autism. Physiology and Behavior 256: 113961.
Wang, X., J. Yang, H. Zhang, J. Yu, and Z. Yao. 2019. Oral probiotic administration during pregnancy prevents autism-related behaviors in offspring induced by maternal immune activation via anti-inflammation in mice. Autism Research. 12 (4): 576–588.
Sanctuary, M.R., J.N. Kain, S.Y. Chen, K. Kalanetra, D.G. Lemay, D.R. Rose, et al. 2019. Pilot study of probiotic/colostrum supplementation on gut function in children with autism and gastrointestinal symptoms. PLoS ONE 14 (1): e0210064.
Tomova, A., V. Husarova, S. Lakatosova, J. Bakos, B. Vlkova, K. Babinska, et al. 2015. Gastrointestinal microbiota in children with autism in Slovakia. Physiology and Behavior 138: 179–187.
Wang, Y., N. Li, J.J. Yang, D.M. Zhao, B. Chen, G.Q. Zhang, et al. 2020. Probiotics and fructo-oligosaccharide intervention modulate the microbiota-gut brain axis to improve autism spectrum reducing also the hyper-serotonergic state and the dopamine metabolism disorder. Pharmacological Research 157: 104784.
Schmitt, L.M., E.G. Smith, E.V. Pedapati, P.S. Horn, M. Will, M. Lamy, et al. 2023. Results of a phase Ib study of SB-121, an investigational probiotic formulation, a randomized controlled trial in participants with autism spectrum disorder. Science and Reports 13 (1): 5192.
Kong, X.J., J. Liu, K. Liu, M. Koh, H. Sherman, S. Liu, et al. 2021. Probiotic and oxytocin combination therapy in patients with autism spectrum disorder: A randomized, double-blinded, placebo-controlled pilot trial. Nutrients 13 (5): 1552.
Guidetti, C., E. Salvini, M. Viri, F. Deidda, A. Amoruso, A. Visciglia, et al. 2022. Randomized double-blind crossover study for evaluating a probiotic mixture on gastrointestinal and behavioral symptoms of autistic children. Journal of Clinical Medicine 11 (18): 5263.
Gładysz, D., A. Krzywdzińska, and K.K. Hozyasz. 2018. Immune abnormalities in autism spectrum disorder—could they hold promise for causative treatment? Molecular Neurobiology 55: 6387–6435.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
F. Z, R. R, and M. M. performed literature searching and analysis, M. D, S. B, and M. M: Data curation, F. Z and R. R. illustrated figure and tables, F. Z, R. R., F. Sh, and S. Kh, wrote the primary draft. I. A. designed, conceptualized, and supervised the study's technical details, edited, and submitted the manuscript as the correspondence. All authors have reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zarimeidani, F., Rahmati, R., Mostafavi, M. et al. Gut Microbiota and Autism Spectrum Disorder: A Neuroinflammatory Mediated Mechanism of Pathogenesis?. Inflammation (2024). https://doi.org/10.1007/s10753-024-02061-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10753-024-02061-y