Abstract
Objective
This study seeks to explain the relationship between systemic conditions and hard exudate formations in diabetic macular edema patients. Besides, the study aimed to quantitatively examine changes in the area, location, and impact on visual function of hard exudates following intravitreal dexamethasone implant injections.
Methods
A retrospective analysis was conducted, including 40 patients (40 eyes) diagnosed with non-proliferative diabetic retinopathy and concurrent macular edema between January 1, 2022, and January 1, 2024. Preoperative evaluations included glycated hemoglobin, lipid profile, and renal function examinations. Based on the location of HE, patients were divided into two groups: Group A, with HE in 1 mm of the central fovea, and Group B, with HE outside 1 mm of the central fovea. Selected eyes were subject to pre- and postoperative examinations, including best-corrected visual acuity (BCVA), intraocular pressure, slit-lamp biomicroscopy, scanning laser ophthalmoscopy (SLO), optical coherence tomography, and multifocal electroretinography. Following screening and examination, patients received an immediate intravitreal injection of the DEX implant, with an injection administered at the four-month mark. Hard exudate (HE) areas were measured utilizing SLO fundus imaging.
Results
Total cholesterol, low-density lipoprotein, and triglyceride levels were found to be positively correlated with the presence of HE. Following surgical intervention, all patients demonstrated an improvement in BCVA. The mean BCVA increased from a preoperative measurement of 0.79 ± 0.04 to 0.39 ± 0.02 at the 6 month follow-up, indicating a statistically significant difference (p < 0.001). The baseline HE area for the entire patient cohort was 2.28 ± 0.22. One month post-operation, the HE area exhibited a slight increase to 2.27 ± 0.22. However, by the 6 month follow-up, the HE area had significantly decreased to 0.8 ± 0.87, representing a 35.09% reduction from the baseline measurement (p < 0.001). It is worth noting that Patient P1 did not exhibit a statistically significant difference between preoperative and six-month postoperative HE area (p = 0.032). Preoperative BCVA measurements for Group A and Group B were 0.81 ± 0.03 and 0.77 ± 0.03, respectively, with no statistically significant intergroup difference (p = 0.333). The baseline HE area for Group A was 2.61 ± 0.16, which decreased to 0.38 ± 0.20 at the six-month follow-up, representing a 14.60% reduction from the baseline total area. For Group B, the baseline HE area was measured at 1.95 ± 0.09, then decreasing to 1.21 ± 0.13 at the six-month follow-up, indicating a 62.05% reduction from the baseline total area. A statistically significant difference in the postoperative 6 month HE area was observed between Group A and Group B (p < 0.001). In Group A, the reduction in HE area (initial HE area-final HE area) was positively correlated with the improvement in P1 (initial P1-final P1) (r = 0.610, p = 0.004). In Group B, a similar positive correlation was found (initial HE area-final HE area with initial P1-final P1) (r = 0.488, p = 0.029). In Group B, the reduction in HE area (initial HE area-final HE area) correlated positively with the improvement in BCVA (initial BCVA-final BCVA) (r = 0.615, p = 0.004). Additionally, in Group B, the reduction in HE area (initial HE area-final HE area) was positively correlated with the improvement in CMT (initial CMT-final CMT) (r = -0.725, p< 0.001). Aggravated cataracts were observed in thirteen eyes during a follow-up examination 6 months later.
Conclusion
HE formation is associated with lipid levels. Dexamethasone implants demonstrate effectiveness in reducing HE areas in the short term, reducing macular edema, improving retinal structure, and enhancing visual function. The incidence of postoperative complications such as cataracts and glaucoma remains low.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Approximately 3.6% of individuals with diabetes develop diabetic retinopathy [1], among which diabetic macular edema (DME) is a principal cause of visual impairment, accounting for 6.8% of cases among those with diabetic retinal diseases [2]. DME can lead to a decline in visual acuity and distortion of vision, severely affecting the quality of life. Research indicates that inflammation is a critical factor in DME, where prolonged hyperglycemia can induce retinal ischemia, hypoxia, and chronic inflammation. This cascade releases numerous inflammatory mediators that compromise the blood-retinal barrier, damage retinal neural cells, and increase retinal vascular permeability, resulting in macular edema [3]. Typically, DME arises from leakage in retinal capillaries often associated with the deposition of large molecular substances such as lipids and proteins, thus frequently accompanied by hard exudates (HE) [4].
HE represent a common funduscopic manifestation in diabetic retinopathy, appearing as yellow-white deposits in the retina. Typically, HE clusters or forms circular patterns around microaneurysms [5]. The occurance of HE is attributed to diabetic-induced abnormalities in retinal capillaries, where lipids leak and accumulate in the retinal layers. Firstly, HE is located between the layers of Henle's fiber, and since the outer plexiform layer is avascular, HE can take months to years to resolve without intervention. Prolonged lipid deposition in the retina can lead to tissue fibrosis, potentially causing permanent visual impairment [6]. While previous studies have primarily focused on the correlation between central retinal thickness and visual acuity [7, 8], research on HE has been limited. Despite improvements in macular edema following treatment, the area and location of HE continue to affect visual acuity. This study aims to observe the systemic conditions associated with HE in patients with diabetic macular edema and to quantitatively analyze changes in the area, location, and visual function of HE following the intravitreal injection of dexamethasone implants.
Methods
This analysis was conducted as a retrospective study, approved by the Ethics Committee of Foshan Aier Eye Hospital (Approval No.: 2024-Hospital Ethical Review-03–16), adhering to the principles of the Declaration of Helsinki. Informed consent was obtained in writing from all patients and their families.
Data were collected from January 1, 2022, to January 1, 2024, on 40 patients (40 eyes) at the Aier Eye Hospital Group, Foshan Aier Eye Hospital, diagnosed with non-proliferative diabetic retinopathy with macular edema who underwent intravitreal injection of a dexamethasone implant. The cohort included 24 males (24 eyes) and 16 females (16 eyes), with an average age of 60.48 ± 7.00 years. Preoperative BCVA was 0.79 ± 0.25, and intraocular pressure was 15 mmHg (range 14–16 mmHg). Inclusion criteria: (1) Diagnosed with DME-HE; (2) Optical Coherence Tomography (OCT) detected central macular thickness (CMT) > 275 μm; (3) OCT and SLO confirmed the presence of hyperreflective material in and/or beneath the retina in the posterior pole. Exclusion criteria: (1) Concurrent other retinal diseases; (2) History of ocular surgery in the previous 6 months; (3) Refractive error ≥ −6D; (4) Cataract opacity affecting SLO imaging quality; (5) Severe systemic disease precluding tolerance of examination. Based on the location of HE, patients were divided into two groups: Group A, with HE in 1 mm of the central fovea, and Group B, with HE outside 1mm of the central fovea.
Treatment Protocol: All patients were subject to preoperative examinations of blood pressure, glycated hemoglobin, and lipid profile. Eligible eyes received an intravitreal injection of the DEX implant (Ozurdex; Allergan, Irvine, California, USA) following screening and examination, with a second injection administered at the fourth month. Observations continued for 6 months post-initial injection. Evaluations of BCVA, intraocular pressure (IOP), slit-lamp biomicroscopy, SLO, OCT, and multifocal electroretinography (mf-ERG) were performed preoperatively, and at one, three, and 6 months postoperatively.
Best Corrected Visual Acuity (BCVA) examinations were conducted utilizing the standard logarithm visual acuity chart, with results converted to the logarithm of the minimum angle of resolution (logMAR) for statistical analysis. Fundus imaging was performed utilizing a Scanning Laser Ophthalmoscope (SLO, model: P200DTx), following standardized procedures.
OCT Examination: Performed utilizing Heidelberg Spectralis-OCT (Heidelberg Engineering, Germany), CMT was measured three times and averaged. SD-OCT divided the macular region into concentric circles centered on the fovea (ETDRs grid) (Fig. 1), with regions classified into Groups A and B based on the location of HE, with Group A HE located in the 0–1 mm zone, and Group B HE beyond the 1 mm zone.
Mf-ERG examination
The multifocal electroretinography (mf-ERG) was conducted utilizing the RETIsan system from Roland Consult, Germany. After pupil dilation, refractive correction was applied, and the study covered a 60° field (30° on either side of the fixation point) utilizing a 61-hexagon stimulus pattern. The luminance of the bright and dark hexagons was maintained at 100 cd/m2 and < 1 cd/m2, respectively, to record the retinal electrophysiology. The first positive wave, designated as P1, was measured for its amplitude density in the first ring.
Measurement of macular HE area
The area of HE was mesured utilizing ImageJ software (Rasband, W.S., ImageJ, U.S. National Institutes of Health, Bethesda, Maryland, USA). All measurements were performed by the same skilled technician. Reference scales and the location of the foveal depression were obtained by overlaying OCT images on SLO images (Fig. 2). OCT report images included retinal images of the scanning area and the macular fovea. After uploading fundus photographs to ImageJ (Fig. 3A), the Fiji software was utilized to quantify the areas of HE and the optic disc. The images with the green channel are adjusted for threshold to identify the HE and optic disc areas (Fig. 3B). Less clear HE areas were selected utilizing the ROI manager function, outlined in yellow (Fig. 3C), and the areas of the optic disc (PD) and HE were automatically measured [9, 10]. The ratio of HE area to optic disc area (HE/PD) was calculated as a relative area.
Statistical analysis
Statistical analyses and graphical representations were performed utilizing R software (version 4.3.3). For quantitative data, if the distribution was normal, the mean ± standard deviation (± SD) was used; comparisons between groups were made utilizing independent sample t-tests. For non-normally distributed data, the median (P25, P75) was described, and comparisons between groups were conducted utilizing independent sample rank-sum tests. For repeated measures data such as logMAR BCVA, HE area, and CMT before and after treatment, a generalized estimating equation model was employed for statistical analysis. Mean values estimated from the generalized estimating equations were utilized to create line graphs and bar charts. Pearson or Spearman correlation analyses were utilized to assess relationships between different variables, with scatter plots and heat maps generated for visualization. Graphs were produced utilizing the ggplot2 package. A p-value of < 0.05 was considered statistically significant.
Results
Based on the inclusion and exclusion criteria, 40 participants (40 eyes) were enrolled in this study, comprising 24 males (24 eyes) and 16 females (16 eyes), with an average age of 60.48 ± 7.00 years. Preoperative BCVA was 0.79 ± 0.25, and intraocular pressure was 15 mmHg (range 14–16). Of these, 15 individuals had hypertension, representing 37.5% of the sample. Glycated hemoglobin was 8.16 ± 2.48%, total cholesterol was 5.04 ± 0.98 mmol/L, with triglycerides at 1.7 mmol/L, high-density lipoprotein (HDL) at 1.2 mmol/L, and low-density lipoprotein (LDL) at 1.96 mmol/L. Group A consisted of 20 individuals, aged 59.95 ± 6.44 years, including 9 males (9 eyes) and 11 females (11 eyes), with a preoperative BCVA of 0.83 ± 0.62 and intraocular pressure of 16 mmHg (range 14–16.25). Group B also included 20 individuals, aged 61.00 ± 7.66 years, comprising 7 males (7 eyes) and 13 females (13 eyes), with a preoperative BCVA of 0.76 ± 0.25 and intraocular pressure of 15 mmHg (range 14–15). The average age, gender distribution, preoperative BCVA, intraocular pressure, glycated hemoglobin, total cholesterol, LDL, HDL, and triglycerides demonstrated no significant differences between the groups (P > 0.05) (Table 1).
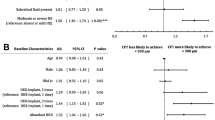
Analysis of all patients indicated a positive correlation between triglyceride levels and HE area (OR = 0.005, p = 0.023); total cholesterol also demonstrated a positive correlation with HE area (OR = 2.343, p = 0.006). LDL levels were positively correlated with HE area (OR = 0.172, p = 0.032). Hypertension demonstrated a positive correlation with HE area (OR = 2.730, p = 0.061). There was no significant correlation between HbA1c levels and HE area (OR = −0.384, p = 0.095), nor between HDL levels and HE area (OR = −0.200, p = 0.387).
All patients experienced a significant improvement in BCVA from a preoperative average of 0.79 ± 0.04 to 0.39 ± 0.02 6 months postoperatively (p < 0.001) (Fig. 4E). Preoperative CMT was 426.05 ± 18.24 mm, which decreased to 348.95 ± 13.07 mm at one month postoperatively, demonstrated a rising trend at 3 months, but decreased to 315.60 ± 10.79 mm at 6 months postoperatively, representing a statistically significant change (p < 0.001) (Fig. 4C). Baseline HE area was 2.28 ± 0.22, increased to 2.27 ± 0.22 at one month postoperatively, and decreased to 0.8 ± 0.87 at 6 months postoperatively (p < 0.001) (Fig. 4A), constituting 35.09% of the baseline total area (Fig. 5). Baseline HE/PD was 0.95 ± 0.11, increased to 0.91 ± 0.09 at one month postoperatively, and continuously declined to 0.29 ± 0.04 at 6 months postoperatively (p < 0.001) ((Fig. 4B), representing a 30.53% reduction from baseline. However, there was no statistically significant difference in P1 between preoperative and 6 months postoperative measurements (p = 0.032) (Fig. 4D; Table 2).
BCVA for Group A was 0.81 ± 0.03 and for Group B was 0.77 ± 0.03, with no significant differences between the groups (p = 0.333). At three and 6 months postoperatively, there were no significant differences in BCVA between the groups (p = 0.447, p = 0.440) (Fig. 6A). The CMT in both groups significantly decreased postoperatively compared to preoperative values, with no significant differences between the groups at one, three, and 6 months postoperatively (p = 0.724, p = 0.193, p = 0.330). Baseline HE/PD ratio in Group A was 0.14 ± 0.68, which decreased at 6 months postoperatively to 0.34 ± 0.25. In Group B, the baseline area was 0.48 ± 0.29, decreasing at 6 months postoperatively to 0.23 ± 0.20 (Fig. 6B). Baseline HE area in Group A was 2.61 ± 0.16, which decreased at 6 months postoperatively to 0.38 ± 0.20, representing 14.60% of the baseline total area. In Group B, the baseline area was 1.95 ± 0.09, decreasing at 6 months postoperatively to 1.21 ± 0.13, representing 62.05% of the baseline total area, with significant differences between the groups at 6 months postoperatively (p < 0.001) (Fig. 6C). Baseline P1 in Group A was 45.39 ± 2.43, and in Group B was 49.47 ± 5.26, with significant differences between the groups preoperatively (p = 0.046). At 6 months postoperatively, P1 increased in Group A to 48.36 (0.58) and in Group B to 49.64 (1.12), with no significant differences between the groups (p = 0.472) (Fig. 6D; Table 3).
A: Comparison of mean changes in BCVA between Groups A and B during monthly follow-ups. B: Comparison of mean changes in HE/PD ratio between Groups A and B during monthly follow-ups. C: Comparison of mean changes in HE area between Groups A and B during monthly follow-ups. D: Comparison of mean changes in P1 wave amplitude between Groups A and B during monthly follow-ups
A: Correlation between changes in HE area and improvement in BCVA in Group A. B: Correlation between changes in HE area and improvement in BCVA in Group B. C: Correlation between changes in HE area and improvement in CMT in Group A. D: Correlation between changes in HE area and improvement in CMT in Group B. E: Correlation between changes in HE area and improvement in P1 wave amplitude in Group A. F: Correlation between changes in HE area and improvement in P1 wave amplitude in Group B
There was no correlation between the reduction in HE area (HE area pre—HE area 6 m) and the improvement in BCVA (BCVA pre—BCVA 6 m) in all patients (R = 0.261, P = 0.131); there was no correlation between HE (HE area pre—HE area 6 m) and CMT improvement (initial CMT—final CMT) in all patients (R = 0.001, p = 0.092), and there was no correlation between the reduction in all HE areas (initial HE area—final HE area) and P1 improvement (initial P1—final P1) (R = 0.270, P = 0.092); among them, there was no correlation between the reduction in HE area (initial HE area—final HE area) and BCVA improvement (BCVA—BCVA 4) in group A patients (R = 0.384, P = 0.094) (Fig. 7A). There was a positive correlation between the reduction in HE area (initial HE area—final HE area) and BCVA improvement (initial BCVA—final BCVA) in group B patients (R = 0.615, P = 0.004) (Fig. 7B); there was no correlation between the reduction in HE area (initial HE area—final HE area) and CMT improvement (initial CMT—final CMT) in group A (R = 0.292, P= 0.211) (Fig. 7C). There was a positive correlation between (initial HE area—final HE area) and CMT improvement (initial CMT—final CMT) in group B (R = −0.725, P < 0.001) (Fig. 7D). There was a positive correlation between the reduction in HE area (initial HE area—final HE area) and P1 improvement (initial P1—final P1) in group A (R = 0.610, P = 0.004) (Fig. 7E). There was a positive correlation between the reduction in HE area (initial HE area—final HE area) and P1 improvement (initial P1—final P1) in group B (R = 0.488, P = 0.029) (Fig. 7F).
Thirteen eyes, representing 39%, experienced an exacerbation of cataracts 6 months postoperatively. Increased intraocular pressure (26.8–33.5 mmHg, 1 mmHg = 0.133 kPa) occurred in three eyes one month after injection, accounting for 23% of cases. Treatment with Carteolol Hydrochloride eye drops twice daily promptly reduced the pressure to below 21 mmHg. After maintaining this level for 2 weeks, the dosage was reduced to once daily. Following another week, medication was discontinued, and no rebound increase in pressure was observed over an additional 2 week period.
Discussion
This study marks the first utilization of SLO for fundus photography to examine posterior pole HE pre- and post-surgery. SLO employs three different laser wavelengths (λ = 488; 518; 820 nm) to represent various retinal lesions across different retinal layers. Compared to traditional fundus photography, SLO is less affected by transparent media, offering enhanced contrast and resolution, thus offering clearer images of fundus structures [11, 12]. Besides, the combined use of Confocal Scanning Laser Ophthalmoscopy (CSLO) and Spectral-Domain Optical Coherence Tomography (SD-OCT) platforms enables the capture of multimodal images, facilitating more reliable examinations of changes in macular edema and HE pre- and post-surgery. Research by Gong et al. also found that MCI surpasses traditional CFP in detecting HEs and analyzing the correlation between HEs and lipid levels in DME [13].
The results of this study indicate that 1 month postoperatively, there was an increase in the area of HE and the ratio of HE area to optic disc area (HE/PD), while these changes were not statistically significant. However, a significant reduction in both HE and HE/PD was observed 6 months after treatment. To enhance the accuracy of HE area calculations, the HE/PD ratio was incorporated into this study to reduce discrepancies caused by factors such as axial length and refractive errors, which can magnify retinal images. It was also noted that one month postoperatively, there was an increase in both HE area and HE/PD compared to preoperative values, but these changes were not statistically significant. By 6 months postoperatively, both HE area and HE/PD had significantly decreased. One month postoperatively, the increase in HE area was attributed to a specific inflammatory response triggered by lipid exudation following the absorption of macular fluid. This inflammation is critical in the formation of DME and HE. During the development of DME, inflammatory markers such as CAM-1, VEGF, IL-1β, IL-6, and IL-8 are increased, disrupting the blood-retinal barrier and exacerbating leakage [14]. Lipoproteins leak from highly permeable capillaries into the extracellular space of the retina and accumulate extensively in the posterior pole, leading to the formation of HE. Histopathologically, HE is characterized by the accumulation of lipid-laden macrophages around microvascular aneurysms, primarily located in the outer plexiform layer (OPL) and the inner nuclear layer (INL) adjacent to the foveal depression. Due to the avascular nature of the outer plexiform layer, HE is challenging to absorb without treatment [15]. In the RIDE and RISE Phase III clinical trials, HE area increased in 3 months postoperatively, then decreased back to baseline levels, with HE areas at baseline and 3 months postoperatively being similar [16]. However, in this study, HE area began to increase one month postoperatively and significantly decreased by the 3 month, demonstrating that dexamethasone implants are more effective in absorbing HE in diabetic retinopathy than anti-VEGF medications. Dexamethasone implants, utilized to treat DME with HE, are administered as a second injection at the third month and can continuously release in the eye for three to 6 months. They reduce macular edema by inhibiting various inflammatory factors, reducing fibrin deposition, capillary leakage, and inflammatory cell migration [17]. Besides, they suppress macrophages in HE, prevent extracellular matrix remodeling, and induce macrophage differentiation, leading to a significant reduction in HE 6 months postoperatively. In addition, this study found that the area of HE located more than 1 mm from the foveal depression decreased more significantly after 6 months compared to HE in 1 mm of the foveal depression. This observation is attributed to non-proliferative HE primarily arising from leakage due to microvascular abnormalities, primarily distributed on the temporal side of the macula. As leakage reduces, HE begins to decrease in areas with higher microvascular density, eventually reaching near the foveal depression [18].
This study demonstrates that 3 months after the intravitreal implantation of dexamethasone, there was a significant reduction in macular edema and an initial improvement in visual acuity. 6 months post-treatment, there was a significant decrease in HE compared to preoperative levels, accompanied by significant enhancements in visual acuity [19]. The area of HE located more than 1 mm from the foveal center was positively correlated with CMT and BCVA. The significance of HE lies in their close association with macular edema and visual acuity. As indicators of past or present macular edema, hard exudates are included in the international clinical severity scales for diabetic macular edema, representing a critical indicator. While typically associated with retinal macular edema, an increase in HE alone can also heighten the risk of visual impairment. Studies both domestically and internationally have identified non-proliferative diabetic retinopathy HE as a primary factor affecting vision, with a significant correlation between the extent of HE and visual acuity [20, 21]. Besides, this research found that patients with HE located in 1mm of the foveal center experienced less improvement in postoperative visual acuity compared to those with HE located further from the foveal center. This may be due to the reduction in CMT leading to the gradual absorption of retinal cystic spaces, interlayer hyperreflective points, and subretinal fluid, but the migration of HE towards the foveal center affects the repair of the external limiting membrane and ellipsoid zone. In Sasaki's study [22], the location of HE significantly affected visual acuity, while the total area of HE had a minimal effect, aligning with the findings of this study. It was also observed that while macular edema decreased 1 month postoperatively, there was no significant improvement in visual acuity, potentially due to the choroid being thicker beneath the fovea than in other areas. The choroid's higher colloidal osmotic pressure facilitates fluid accumulation in the macular region, and lipid substances tend to migrate towards the foveal center. Research by Khairallah M et al.[23]. Suggests that the distribution of HE in the retina might be dynamic, with HE accumulating around the edema, forming HE. HE typically gathers on either side of the edematous OPL rather than at the center, indicating that changes in regional osmotic pressure cause HE to move and deposit in structurally denser tissues. 6 months into the study, both HE and CMT were significantly reduced compared to preoperative levels, and visual acuity was significant improved. This improvement is hypothesized to result from the prolonged macular edema increasing the concentration of inflammatory cytokines and vascular endothelial growth factors in the vitreous humor. The dexamethasone implant enhances tight junction proteins to stabilize the blood-retinal barrier and utilizes arachidonic acid for its anti-inflammatory effects, inducing the differentiation of specific anti-inflammatory macrophages, thus facilitating the absorption of HE [24].
The findings of this analysis further indicate that, following treatment, all patients exhibited a trend toward improvement in multifocal electroretinogram (mf-ERG) parameters over time. Typically, ischemia and hypoxia in the retinal macular region lead to edema, severely impairing visual function. Previous studies have demonstrated that patients with HE exhibit significantly lower mf-ERG amplitudes than those observed in the normal population [25]. However, post-treatment, these amplitudes tend to increase, suggesting a restoration and enhancement of macular function, thereby indicating that mf-ERG could represent a key indicator for assessing the functionality of DME associated with HE. The fundamental pathological changes in diabetic retinopathy (DR) involve disarray in the structure and function of the retinal microcirculation, with early disruptions to the blood-retinal barrier affecting the inner nuclear layer and the outer plexiform and nerve fiber layers. Ischemia and hypoxia exacerbate these effects, progressing toward proliferative stages. The P1 wave is likely derived from the inner retinal layers, while the N1 wave may originate from the outer retinal layers [26]. The selection of the P1 wave as a research focus is predicated on its amplitude density abnormalities appearing earlier than those of the N1 wave, highlighting its sensitivity as a diagnostic indicator for early-stage DR. This study also observes that HE located in 1 mm of the central fovea may lead to poorer vision and mf-ERG outcomes, potentially due to severe macular edema which, upon resolution, results in significant HE deposition beneath the macula, causing subretinal tissue fibrosis [27]. Therefore, the reduction of macular edema and the absorption of HE are equally crucial in the treatment of DME. Dexamethasone implants not only reduce inflammation but also reduce leakage from microaneurysms (MA) and downregulate VEGF production and expression, thereby exerting a vascular inhibitory effect which may continuously facilitate the absorption of HE [28].
This study demonstrates that serum total cholesterol and low-density lipoprotein cholesterol are independent risk factors for macular hard exudates in patients with type 2 diabetes. Cholesterol can lead to the formation of hard exudates in the retina. A prospective study by YS[29] et al. demonstrated that higher blood lipid levels, especially higher levels of low-density lipoprotein cholesterol and triglycerides, are independent risk factors for hard exudates in DR. While high blood lipids have limited effect on the progression of DR and the development of proliferative DR, they significantly increase the probability of CSME and macular HE. Lipid-lowering therapy can reduce these risks and prevent vision loss. The ETDRS study confirms that increased levels of triglycerides, low-density lipoprotein, and very low-density lipoprotein increase the risk of HE and vision decline, consistent with the findings of this study [30]. Long-term observations indicate that diabetic patients with hyperlipidemia experience an increase in intraocular HE. High lipid levels or excessive fat intake may induce endothelial dysfunction through lipid peroxidation reactions, triggering local inflammatory responses that release cytokines or growth factors, activate biomolecules on the vascular wall, and lead to an increase in oxidized low-density lipoprotein [31].
In addition, this research analyzed postoperative complications associated with dexamethasone implants: Three patients presented with increased intraocular pressure post-procedure, all of which were managed through topical administration of a single antiglaucoma medication, without necessitating antiglaucoma surgery. Thirteen individuals demonstrated cataract progression, which, beyond the intraocular steroid use, may also be attributable to the advanced age of the participants and the increased susceptibility to cataract development in diabetics. Specifically, none of the patients reported drug allergies, retinal detachment, vitreous hemorrhage, endophthalmitis, or other severe ocular complications or systemic adverse effects.
This study group is not without certain limitations: (1) As a retrospective case series, this study is subject to potential sampling bias; (2) The limited sample size and short follow-up duration may not be representative of the broader population, and stratification by HE location could increase the likelihood of Type II errors due to the small sample size; (3) The study did not differentiate patients based on varying types of macular edema, an aspect that warrants exploration in future research; (4) No control groups, such as those receiving anti-VEGF therapies, were established for comparative analysis; (5) Optimal parameters for mf-ERG recording require further ongoing analysis; (6) The study did not account for the duration of DME in participant selection; (7) Lack of comparison of systemic conditions before and after surgery; changes in blood glucose and lipids may cause changes in hard exudates; (8) As a clinic-based analysis, this study may not fully represent the entire DME population. Community-based epidemiological studies are needed to corroborate the findings of this research. Future studies should involve multicenter, large-sample, randomized controlled trials to confirm the effectiveness and safety of dexamethasone implants in the treatment of HE.
Conclusion
HE exhibits a correlation with serum total cholesterol and low-density lipoprotein levels. HE can lead to visual function impairment, with HE in 1 mm of the central fovea having a more significant effect on vision. Dexamethasone implants demonstrate effectiveness in short-term reduction of HE area in DME patients, alleviating macular edema, improving retinal structure, and significantly enhancing visual function. The incidence of postoperative complications, such as cataracts and glaucoma, is low. Further in-depth exploration through large-sample prospective studies is still necessary to examine long-term effectiveness and recurrence rates.
References
Magliano DJ, Boyko EJ, Atlas ID (2021) What is diabetes? In IDF DIABETES. Diahetes atlas, 10th edn. Intemational Diahetes Federation, Brussels
Ning C, Paul M, Tien Yin W (2010) Diabetic retinopathy. Lancet 376:124. https://doi.org/10.1016/S0140-6736(09)62124-3
Francesco B, Daniele V, Cristiana et al (2024) Management of treatment-naïve diabetic macular edema patients: review of real-world clinical data. Eur J Ophthalmol. https://doi.org/10.1177/11206721241237069
Moncef K, Hatem Z et al (2005) Primary intravitreal triamcinolone acetonide for diabetic massive macular hard exudates. Retina 25:835. https://doi.org/10.1097/00006982-200510000-00003
Yanko L, Ungar H, Michaelson IC (1974) The exudative lesions in diabetic retinopathy with special regard to the hard exudate. Acta Ophthalmol 52:150. https://doi.org/10.1111/j.1755-3768.1974.tb00362.x
Jaskirat K, Deepti M et al (2023) Automated detection and segmentation of exudates for the screening of background retinopathy. J Healthc Eng. https://doi.org/10.1155/2023/4537253
Jackson RG, Scott IU et al (2011) Inner retinal visual dysfunction is a sensitive marker of non-proliferative diabetic retinopathy. Br J Ophthalmol. https://doi.org/10.1136/bjophthalmol-2011-300467
Wael S, Pascal H, Birgit S, Michael L (2010) Local retinal sensitivity in relation to specific retinopathy lesions in diabetic macular oedema. Acta Ophthalmol. https://doi.org/10.1111/j.1755-3768.2010.01912.x
Thomas W, Jean-Claude K, Pascale M, Ali E (2003) A contribution of image processing to the diagnosis of diabetic retinopathy–detection of exudates in color fundus images of the human retina. IEEE Trans Med Imaging 21:1236. https://doi.org/10.1109/TMI.2002.806290
Sánchez IC, García M, Mayo A et al (2009) Retinal image analysis based on mixture models to detect hard exudates. Med Image Anal 13:650. https://doi.org/10.1016/j.media.2009.05.005
Tan SC, Sadda SR, Hariprasad SM (2014) Ultra-widefield retinal imaging in the management of diabetic eye diseases. Ophthalmic Surg Lasers Imaging Retina 45:363. https://doi.org/10.3928/23258160-20140909-07
Shuting Li, Xiangning W, Xinhua Du, Qiang Wu (2018) Clinical application of multicolour scanning laser imaging in diabetic retinopathy. Lasers Med Sci 33:1371
Ruowen G, Ruyi H, Jingli G, Wei L, Gezhi X (2021) Quantitative evaluation of hard exudates in diabetic macular edema by multicolor imaging and their associations with serum lipid levels. Acta Diabetol 58:1161. https://doi.org/10.1007/s00592-021-01697-8
Yinchen S, Hanying W, Junwei F, Kun L, Xun Xu (2023) Novel insights into the mechanisms of hard exudate in diabetic retinopathy: findings of serum lipidomic and metabolomics profiling. Heliyon 9:15123. https://doi.org/10.1016/j.heliyon.2023.e15123
Michael C, Chew EY, Chi-Chao C et al (2003) Histopathology and regression of retinal hard exudates in diabetic retinopathy after reduction of elevated serum lipid levels. Ophthalmology 110(11):2126–2133. https://doi.org/10.1016/j.ophtha.2003.01.001
Gardner WT, Sander B, Larsen ML et al (2006) An extension of the Early Treatment Diabetic Retinopathy Study (ETDRS) system for grading of diabetic macular edema in the Astemizole Retinopathy Trial. Curr Eye Res. https://doi.org/10.1080/02713680600746112
Smith RJ, Thorne JE, Flaxel CJ et al (2024) Treatment of noninfectious uveitic macular edema with periocular and intraocular corticosteroid therapies: a report by the american academy of ophthalmology. Ophthalmology. https://doi.org/10.1016/j.ophtha.2024.02.019
Shuting Li, Yuan T, Mengyao Y et al (2024) Aflibercept 5+PRN with retinal laser photocoagulation is more effective than retinal laser photocoagulation alone and aflibercept 3+PRN with retinal laser photocoagulation in patients with high-risk proliferative diabetic retinopathy and diabetic macular edema: a 12-month clinical trial. Front Endocrinol. https://doi.org/10.3389/fendo.2024.1286736
Yoon CK, Sagong M, Shin JP et al (2021) Title: efficacy of intravitreal dexamethasone implant on hard exudate in diabetic macular edema. BMC Ophthalmol. https://doi.org/10.1186/s12886-020-01786-2
Kim HR, Yoon CK, Kim HW et al (2019) New method of quantitative analysis of hard exudate using optical coherence tomography: application in diabetic macular edema. Korean J Ophthalmol 33:399. https://doi.org/10.3341/kjo.2019.0049
Samuel C, Laurent K, Cécile R et al (2024) Real-life experience of dexamethasone implant under a proactive treatment regimen: the ProDEX Study. Ophthalmol Retina. https://doi.org/10.1016/j.oret.2024.03.019
Mariko S, Ryo K, Jonathan E et al (2013) Quantitative measurement of hard exudates in patients with diabetes and their associations with serum lipid levels. Invest Ophthalmol Vis Sci 54:5544. https://doi.org/10.1167/iovs.13-11849
Khairallah M, Zeghidi H et al (2005) Primary intravitreal triamcinolone acetonide for diabetic massive macular hard exudates. Retina 25:835. https://doi.org/10.1097/00006982-200510000-00003
Owen AL, Hartnett ME (2013) Soluble mediators of diabetic macular edema: the diagnostic role of aqueous VEGF and cytokine levels in diabetic macular edema. Curr Diab Rep 13:476. https://doi.org/10.1007/s11892-013-0382-z
Rong-Rong Li, Yang Y, Meng-Ge Z, Jie et al (2024) Abnormalities of retinal function in type 2 diabetes mellitus patients without clinical diabetic retinopathy detected by multifocal electroretinogram. BMC Ophthalmol. https://doi.org/10.1186/s12886-024-03335-7
Itou J, Furushima K, Haruta M et al (2023) Reduced size of telangiectatic cappillaries after intravitreal injection of anti—vascular endothelial growth factor agents in diabetic macular edema. Clin ophthalmol 17:239–245
Sema TK, Gabriele P, Celeste L, Sofia G, Simone C, Luigi B, Emanuele T, Louise O, Paolo N, Stela V (2024) Clinical features related to oct angiography artifacts in patients with diabetic macular edema. Ophthalmol Retina. https://doi.org/10.1016/j.oret.2024.02.017
Li-Rui K, Yan Z, Feng Wu, Xue-Qin W, Da-Hai He, Chao-Qiong Z, Lin W (2020) Correlation between glycosylated serum albumin and glycosylated haemoglobin in the southwest Chinese population: establishment of a regression model. J Diabet Complicat. https://doi.org/10.1016/j.jdiacomp.2020.107796
Yinchen S, Hanying W, Junwei F, Kun L, Xun Xu (2023) Novel insights into the mechanisms of hard exudate in diabetic retinopathy: findings of serum lipidomic and metabolomics profiling. Heliyon. https://doi.org/10.1016/j.heliyon.2023.e15123
Soares RM, Ferreira CC, Fernandes JDS et al (2024) Real-world evidence of the long-term effectiveness of 0.2 μg/day fluocinolone acetonide implant in persistent and recurrent diabetic macular edema—a single center study. Clin Ophthalmol 18:1057–1066. https://doi.org/10.2147/OPTH.S382920
Xinyuan Z, Kaiyue W, Ling Z, Qiyun W (2021) Reverse cholesterol transport pathway and cholesterol efflux in diabetic retinopathy. J Diabetes Res. https://doi.org/10.1155/2021/8746114
Funding
Science and Technology Program of Guangzhou (subject number: 202201020075) and Hunan Provincial Natural Science Foundation of China (subject number: 2023JJ70049).
Author information
Authors and Affiliations
Contributions
JZ provided guidance and overall direction throughout the study design, paper writing and revision. SZ handled the literature review, data collection, data analysis and interpretation, and manuscript writing. SZ provided expertise on data collection and review the manuscript.SZ collected data and reviewed the manuscript. XL collected data and provided guidance on writing. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Confict of interest
The authors have no relevant fnancial or non-fnancial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted Aier eye hospital Jinan university.
Consent to participate
Written informed consent was obtained from the parents / guardians for all participants.
Consent for publication
This manuscript contains no personaldata or images that may disrupt participants’ confdentiality.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhao, S., Liang, X. & Zhang, J. Effectiveness of dexamethasone implants in treating diabetic macular edema with hard exudates: a clinical observation. Int Ophthalmol 44, 377 (2024). https://doi.org/10.1007/s10792-024-03278-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10792-024-03278-4