Abstract
Objectives
Maternal mortality remains an unfinished global agenda and postpartum hemorrhage (PPH) remains one of the leading causes. The aims of this study were to describe the incidence, underlying causes, and case fatality rate of PPH in public hospitals in eastern Ethiopia.
Methods
This study was part of a larger Ethiopian Obstetric Surveillance System (EthOSS) project — a multicenter surveillance of women admitted to 13 public hospitals in eastern Ethiopia due to any of the five major obstetric conditions: obstetric hemorrhage, eclampsia, uterine rupture, sepsis, and severe anemia – conducted from April 1, 2021 to March 31, 2022. All registers in maternity units of those hospitals were reviewed to identify eligible women and collect data on sociodemographic and obstetric characteristics, management and maternal outcomes at discharge or death. Findings were reported using descriptive statistics.
Results
Among 38,782 births registered during the study period, 2043 women were admitted with at least one of the five major obstetric conditions. Of these 2043, 306 women (15%) had PPH corresponding with an incidence rate of 8 (95% CI: 7–9) per 1000 births. Uterine atony was the main underlying cause in 77%; 81% of women with PPH received at least one uterotonic drug, and 72% of women for whom blood was requested received at least one unit. Of the 70 hospital based maternal deaths, 19 (27%) died from PPH, making a case fatality rate of 6 per 100.
Conclusions
Although the overall incidence of PPH appeared low, it was still the underlying cause of death in one out of four women who died. The contributing factors might be that one in five women with PPH did not receive any uterotonic drug and the low blood transfusion. Ongoing audit, followed by targeted action, is essential to improve care quality and reduce adverse maternal outcome. The relatively low incidence may reflect under-recording in paper-based records, implying that further research into methods to optimize the surveillance is needed.
Significance
Although PPH remains the leading cause of maternal mortality in many low-resource settings, systems to track progress and effects of interventions to reduce its burden are lacking. Identifying the incidence, underlying contributing factors and management outcomes would assist in devising tailored interventions.
AbstractSection What this Study adds?While an inadequate administration of uterotonics and low blood transfusion could have contributed to PPH causing significant proportion of maternal death in the study settings, audit of care, context specific interventions and improving paper based recording and research to optimize the surveillance need due attention.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Although the global maternal mortality ratio (MMR) is declining, it remains disproportionately high in low-and-middle-income countries. In 2020, sub-Saharan Africa (SSA) was the region with the highest MMR globally, estimated to be 545 per 100,000 live births accounting for more than 70% of the global 287,000 maternal deaths (World Health Organization, 2023; Zarocostas, 2023). Likewise, although Ethiopia’s MMR of 267 per 100,000 live births showed a one-third reduction from its level in 2016 (401 per 100,000), an estimated 10,000 annual maternal deaths occurred in Ethiopia in 2020 (World Health Organization, 2023b). Moreover, for each maternal death, 20 or 30 women develop severe obstetric complications, but survive (Ashford, 2002; Firoz et al., 2013).
Postpartum hemorrhage (PPH), commonly defined as an excessive bleeding from the genital tract following the birth of the neonate (> 500 ml in case of vaginal birth or > 1000 ml in case of cesarean section), remained one of the leading causes of maternal deaths in Ethiopia (Federal Ministry of Heath of Ethiopia, 2021; World Health Organization, 2018). Although PPH affects about 5% of global births (Carroli et al., 2008; Mavrides, 2016; Souza et al., 2013; World Health Organization, 2012, 2018), it is the leading cause of maternal deaths in many low- and middle-income countries (Say et al., 2014). Preventing PPH related deaths and complications requires early recognition and management (Andrikopoulou & D’Alton, 2019; Higgins et al., 2019; Mavrides, 2016; World Health Organization, 2012). In Ethiopia, PPH has been reported to complicate 3 to 17% of all births, with considerable variation depending on context, facility type, study design and case definition (Achamyelesh & Nebiyu, 2021; Amanuel et al., 2021; Asrat & Shimeles, 2021; Bewket et al., 2022a, Bewket et al., 2022b; Biruk et al., 2019; Habitamu et al., 2019; Jemberu et al., 2022; Sinetibeb et al.,2021; Tadesse et al., 2022). In 2020, 47% of maternal deaths in Ethiopia were due to hemorrhage (Ethiopian Public Health Institute, 2020).
Whilst the contribution of PPH to maternal deaths and complications in Ethiopia is well-documented in the literature, a robust and efficient system for continuously monitoring the frequency of PPH is not currently in place (Amanuel et al., 2021; Bewket et al., 2022a; Jemberu et al., 2022; Sinetibeb et al., 2021; Temesgen, 2017). This hampers rapid evaluation of efforts to reduce the incidence of such conditions. Lack of robust numbers, including the number of women who have PPH but survive, hampers a comprehensive understanding of the burden of PPH and its case fatality rate (CFR).
It is noteworthy that many high-income countries now have obstetric surveillance systems for monitoring progress and effects of interventions. The UK Obstetric Surveillance System (UKOSS), for instance, has demonstrated importance in improving clinical care and maternal outcomes in the UK and beyond (Knight et al., 2005; Knight & Lindquist, 2013). Based on UKOSS methodology, the Ethiopian Obstetric Surveillance System (EthOSS) was established in April 2021 in hospitals with maternity units in eastern Ethiopia through prospective registration of five major obstetric conditions: obstetric hemorrhage, eclampsia, uterine rupture, sepsis, and severe anemia (Abera et al., 2023a). This study aimed to describe the incidence, underlying causes, and the CFR of PPH among women admitted to any of the 13 public hospitals in eastern Ethiopia with any of the five major conditions as part of the EthOSS project.
Methods
Study Settings
This study was conducted as part of the EthOSS project, a study covering a network of 13 public hospitals with maternity units from April 1, 2021 to March 31, 2022. EthOSS is a multicenter study established for monitoring pregnancy outcomes among women hospitalized during pregnancy, childbirth or within 42 days postpartum in eastern Ethiopia. In these 13 public hospitals, 38,782 women gave birth during the one-year study period. Details of the EthOSS methodology, type or level of hospitals included and characteristics of women admitted were described elsewhere (Abera et al., 2023a, b). In brief, data on five priority obstetric conditions—obstetric hemorrhage, eclampsia, uterine rupture, sepsis, and severe anemia—were registered daily by designated clinicians in the consenting hospitals followed by detailed data collection by EthOSS research assistants at the end of each reporting month. Based on the 2019 Ethiopian mini-demographic and health survey, only half (48%) gave birth in health facilities in Ethiopia, ranging from 41 to 69% in different areas in eastern Ethiopia. In this study, we focused on women admitted for PPH to any of these hospitals.
Study Design, Population and Data Collection
This was a multicenter cohort study. All women who were admitted to any of the 13 participating hospitals during pregnancy, childbirth or within 42 days postpartum were the source population whereas the study population were women who were admitted for PPH (and who either gave birth at the same hospital or were referred from other facilities or came in after home birth) in any of these 13 hospitals. PPH was defined as excessive bleeding following childbirth (> 500 ml following vaginal birth or > 1000 ml following cesarean section) (Federal Ministry of Health of Ethiopia, 2021a; World Health Organization, 2018) recorded based on the diagnosis documented by the managing clinician in the woman’s case file. We reviewed records of all women admitted with PPH and all registers in the labor and gynecology wards, operating theatres and the intensive care units of each hospital.
At each hospital, a designated midwife recorded the total number of women admitted with PPH along with their medical registration numbers and date of admission or date of diagnosis daily. At the end of each month, the midwife reported the number of women with PPH and their details to the EthOSS team in a protected online system: the Kobo Toolbox. After receiving the reports, EthOSS research assistants visited respective hospitals to screen the medical records of each woman for eligibility (if the case file is truly of PPH, in this case) and collected detailed data on socio-demographic characteristics, past obstetric history, underlying causes, management (active management of third stage of labor, use of uterotonics, manual and surgical interventions) and outcomes of PPH. Causes of PPH and interventions given were picked as documented in the charts by the managing clinicians. These data were entered into Kobo Toolbox offline and later uploaded to the central EthOSS database of the Kobo Toolbox system, which is password-protected and only accessed by the EthOSS investigators. The data abstraction form used in EthOSS was adapted from the UKOSS data abstraction forms (Knight et al., 2005) and the Ethiopian Maternal and Perinatal Death Surveillance and Response (MPDSR) guideline (Ethiopian Public Health Institute, 2017).
Data Processing and Analysis
The data were exported to and analyzed using Stata 14 (Statacorp: College Station, Texas 77845 USA). Missing values and outliers were checked by running frequencies, and cross tabulations. Descriptive statistics was used to present results in tables, figures, graphs, and charts as appropriate. Incidence of PPH was calculated as the number of women admitted for PPH per 1000 births, and CFR was defined as the proportion of women who died from PPH among all women hospitalized for PPH.
Ethics Approval
The study was conducted in accordance with the Declaration of Helsinki. The study protocol was reviewed and approved by the Institutional Health Research Ethics Review Committee (IHRERC) of the College of Health and Medical Sciences of Haramaya University, Ethiopia (Ref No. IHRERC/024/2021); and the University of Oxford’s Oxford Tropical Research Ethics Committee (OxTREC); (Reference 530 − 21). Informed consent for the study was obtained from medical director and head of maternity units of each hospital. This study is based on review of case files and therefore the need for consent from woman was waived.
Consent to Participate
This study is based on a review of case files after a woman’s discharge or death, and therefore the need for consent from the individual woman was waived. The facility’s consent to be part of the study was signed by the medical director and head of the maternity unit of each hospital. Data collectors also signed data privacy consent forms to keep confidentiality of the information they accessed during data abstraction.
Results
Socio-demographic Characteristics
In the one-year period, 38,782 births and 34,090 live births were registered in the 13 hospitals participated in the EthOSS. A total of 2043 women (including 70 women who died) were admitted to these hospitals with at least one of the five EthOSS conditions (2043/38,782; 5%), 306 (15%) had PPH. Among the 306 women with PPH, 234 (76%) gave birth at a health facility, 43 (14%) were < 20 years of age and another 43 (14%) were aged 35 years or above; 226 (74%) had no antenatal care (ANC) consultations attended. Slightly more than half were primiparous (158; 52%). We found that six of 306 women (2%) were admitted to an intensive care unit (ICU) for critical care (rather than for mere recovery after cesarean section) (Table 1). Of the six ICU admissions, three were in a tertiary/academic hospital, one in a referral hospital, one in a general hospital and one in a primary hospital. Tertiary and referral hospitals have a well-established ICU with mechanical ventilation, and well-trained anesthesiologists and emergency and critical care doctors, whereas the availability of ICU equipment and trained health workers are rare or none at all in general and primary hospitals. None of these three hospitals where ICU admissions happened had any renal replacement therapy available.
Of the 306 women with PPH, 132 (43%) were admitted to eight general hospitals, followed by 89 (29%) to a tertiary/academic hospital, and 31(10%) to a referral hospital. Nine out of 19 PPH-related maternal deaths happened in one tertiary/academic hospital (Table 2).
Incidence, Causes, and Management of PPH
The incidence of PPH during the study period was 8 (95% CI: 7–9) per 1000 births (306 in 38,782 births). In almost eight out of ten women (236/306;77%) PPH was primarily caused by uterine atony (Fig. 1).
All women with PPH (n = 306), received at least one of the available PPH management options, and 48 had received more than one. Eight in ten(81%) of them received at least one uterotonic drug (oxytocin, ergometrine or misoprostol). Of 236 women with uterine atony, 85% (n = 200) received therapeutic oxytocin. Manual removal of the placenta or a placental remnant was done for all the 13 women in whom a retained placenta or placental tissue was identified as a cause (Table 3). Furthermore, uterine atony was the leading cause of PPH in 15 of the 19 maternal deaths from PPH. Regarding interventions for women who died from PPH, 14/19 (74%) received therapeutic uterotonic drugs (oxytocin and ergometrine) (Table 4).
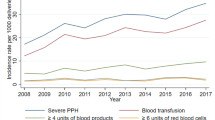
From 122 (122/306; 40%) women for whom blood was requested for transfusion, only 72% (88/122) received at least one unit of blood. In 82% (72/88) women, only one or two units of blood were transfused. In the remaining 184 (60%) women, no request for blood was made or no documentation was found whether blood for transfusion was requested or not, or given (Fig. 2).
Active management of third stage of labor (uterine massage, uterotonics and controlled cord traction) to prevent PPH was documented in 169 (55%) women. More specifically, of 236 women in whom uterine atony was identified as the primary cause, only 130 (55%) had received active management of the third stage of labor. Of the 306 women admitted to hospitals with PPH, 19 died corresponding with a CFR of 6 per 100. Moreover, PPH was found to be the underlying cause in 27% (19/70) of all hospital-based maternal deaths during the same period.
Discussion
We estimated the incidence of PPH in public hospitals in eastern Ethiopia as part of the EthOSS project (Abera et al., 2023a). We found the incidence of PPH to be 8 per 1000 births, with a CFR for PPH of 6%. Uterine atony was the underlying cause in the majority of women with PPH. Despite the overall apparently low incidence, PPH was found to be the cause of death in a quarter of all hospital-based maternal deaths during the study period. To the best of our knowledge, this is the first regional multicenter prospective hospital-based obstetric surveillance study of PPH in a low-resource setting in sub-Saharan Africa.
The incidence of PPH in our study was lower than findings from single-center studies in Ethiopia: 3–17% (Achamyelesh & Nebiyu, 2021; Amanuel et al., 2021; Bewket et al., 2022a; Biruk et al., 2019; Habitamu et al., 2019; Sinetibeb et al., 2021) and Zimbabwe (2%) (Ngwenya, 2016). Variations between these studies might be related to possible underreporting of PPH in the current study. From our discussions with obstetric care providers during review meetings and progress reports, it has been repeatedly described that birth attendants and clinicians are too occupied by the focus on lifesaving treatment during these emergencies with little attention to documentation and record-keeping. Moreover, the incidence of PPH we found is also lower compared to reports from high-income countries such as Wales (8.6%) (Bell et al., 2020) and the Netherlands in 2013 (6.4%) (van Stralen et al., 2016). This gap could be due to differences in study participants’ characteristics, definitions of PPH and/or methods used for quantifying or estimating blood loss. We relied on the clinician’s diagnosis of PPH based on visually estimated blood loss, while quantitative blood loss measurements might have been used in those studies from high-income settings. Visual estimation of blood loss is inaccurate in determining amount of blood loss (Prasertcharoensuk et al., 2000; Razvi et al., 1996), and could have contributed to the very low rate of PPH found in our study.
Although we were proactive in putting efforts to reduce the undercount by instituting prospective case identification through daily registration by an assigned midwife in each labor ward, underreporting of PPH in this paper-based surveillance system might happen where details for women admitted or managed for PPH in the hospitals were not properly documented on the admission-discharge, operating theatre, intensive care unit, or birth registers. Similar documentation and record keeping challenges were previously encountered and reported in one of the hospitals included in this surveillance study (Abera et al., 2020).
In line with previous studies (Biruk et al., 2019; Ngwenya, 2016; Sinetibeb et al., 2021), uterine atony was the main underlying cause of PPH in more than three quarter of the women included in this study. We found that the management of PPH, including the use of uterotonics and active management of third state of labor, could be improved. Low use of these management options was particularly evident among women who died. Although prophylactic oxytocin and active management of the third stage should be part of routine immediate postpartum care (Escobar et al., 2022; Federal Ministry of Health of Ethiopia, 2021b, 2022), further research is required to explore whether these are genuinely less frequently practiced than recommended, or whether their use is not well documented.
In this setting with reported shortage of blood for transfusion, both the proportion of blood requested for transfusions and the number of units of blood transfused were low. A low number of transfusions below the required units of blood, might reflects lack of available blood or blood products which could leads to refraining from requesting blood or only request fewer units than actually needed. Ineffective blood transfusion services and lack of voluntary blood donors were common problems reported in other similar settings (Barro et al., 2018; Bates et al., 2008; Getie & Wondmieneh, 2020; Osaro & Charles, 2011; Taye et al., 2017).
Despite many strategic initiatives (Federal Ministry of Health of Ethiopia, 2021b) and interventions such as improved access to Comprehensive Emergency Obstetric Care (CEmOC), and presence of an updated PPH prevention and treatment protocol in Ethiopia (Federal Ministry of Health of Ethiopia, 2021a, b, 2022) the fact that more than a quarter of all hospital-based maternal deaths occurred due to PPH during the study period were due to PPH illustrates that PPH continued to be a major cause of death of women in the study settings. Several interventions have been shown to reduce PPH and its resulting maternal deaths (Bibi et al., 2007; Dupont et al., 2011; Knight & Tuffnell, 2018; Moodley et al., 2014; Seim et al., 2023; Shakespeare & Knight, 2017; Willcox et al., 2020). A care bundle combining interventions was recently shown to have a particularly positive effect (Gallos et al., 2023). This might partly be due to considerable deficiencies in care at baseline: among women in this study 74% had no antenatal care consultations attended, and 45% of women with PPH due to uterine atony didn’t get active management of the third stage of labour. Lack of antenatal care consultations might increase the risk of PPH by letting risk factors go undetected prior to birth (Federal Ministry of Health of Ethiopia, 2021a; Liu et al., 2021). Delays in identifying and referring women at risk of PPH were previously identified as barriers to receiving appropriate and quality care (Bewket et al., 2022a).
A strength of our study is the inclusion of different levels of hospitals, ranging from a rural primary hospital to a tertiary/academic hospital, which helps to obtain a comprehensive perspective on clinical practice across facilities. It should, however, be noted that this study has some limitations. Firstly, blood loss was not quantified and/or estimates were not documented in these settings, and we relied on paper-based hospitals’ charts for the diagnosis of PPH and registers or log books to identify cases of PPH, which might result in under diagnosis or not reporting mild PPH. We also described interventions for women who survived and those who died from PPH based on what is documented in women’s medical records, but were unable to evaluate the timeliness of the interventions due to no or poorly recorded time. Secondly, although we tried our best to include all women hospitalized with PPH through review of all available hospital records, women with PPH might have been missed if they were not included in at least one of these registers, since there is no other mechanism to trace such women. These limitations indicate need for instituting an electronic client chart and record keeping system to improve medical records and registers, to optimize our surveillance system.
While the overall low incidence of PPH might be partly explained by under-reporting, the high CFR indicates that under-reporting is likely limited to less severe cases. With the current stagnation in reducing maternal deaths in general and deaths from PPH in particular, meeting the 2030 Sustainable Development Goals target requires a paradigm shift: implementations of the WHO’s road map to combat PPH (World Health Organization, 2023) through research, appropriate context-specific interventions, monitoring and evaluation, and benchmarks for PPH protocols, timely use of uterotonics, tranexamic acid, and procedural placement reduces the risk of severe haemorrhage sequela and the need for additional procedures (Federspiel et al., 2023). There is a need for audit of care to evaluate its quality, identify delays, and design tailored interventions to improve care (Sørensen et al., 2022).
Data Availability
Anonymized data is available from the corresponding author upon a reasonable request.
Code Availability
Coding is available upon request.
References
Abera, K. T., Sagni, G., Yadeta, D., Delayehu, B., Jelle, S., Thomas, A., & The Ethiopian Obstetric Surveillance System Steering Committee. (2023). On behalf of. Establishing the Ethiopian obstetric surveillance system for monitoring maternal outcomes in Eastern Ethiopia: A pilot study. J Global Health: Science Practice, 11(2).
Abera, K.T., Knight, M., Sagni, G., Redwan, A., Mohammed, Y., Delayehu,B., Tahir,A.H., Stekelenburg,Y., & Van den Akker,T. (2023b). Characteristics and outcomes of pregnant women hospitalized with severe maternal outcomes in eastern Ethiopia: Results from the Ethiopian Obstetric Surveillance System study. International Journal of Gynaecology and Obstetrics, 1–7. https://doi.org/10.1002/ijgo.15240
Tura AK, Aboul-Ela Y, Fage SG, Ahmed SS, Scherjon S, van Roosmalen J, Stekelenburg J, Zwart J, van den Akker T.(2020). Introduction of Criterion-based audit of postpartum hemorrhage in a University Hospital in Eastern Ethiopia: Implementation and methodological considerations. International Journal of Environmental Research and Public Health, 17, 9281. https://doi.org/10.3390/ijerph17249281
Achamyelesh, G., & Nebiyu, M. (2021). Factors of primary postpartum hemorrhage among women delivered at Yirgalem General Hospital Southern, Ethiopia: A case control study. Journal of Maternal and Child Health, 6(6), 739–748.
Amanuel, T., Dache, A., & Dona, A. (2021). Postpartum hemorrhage and its associated factors among women who gave birth at Yirgalem General Hospital, Sidama Regional State, Ethiopia. Health Services Research and Managerial Epidemiology, 8, 23333928211062777.
Andrikopoulou, M., & D’Alton, M. E. (2019). Postpartum hemorrhage: Early identification challenges. Seminars in Perinatology, 43(1), 11–17. https://doi.org/10.1053/j.semperi.2018.11.003
Ashford, L. S. (2002). Hidden suffering: Disabilities from pregnancy and childbirth in less developed countries. Retrieved from: http://www.prb.org/pdf/hiddensufferingeng.pdf
Asrat, H. D., & Shimeles, B. Z. (2021). Postpartum haemorrhage and associated factors among mothers who gave birth in South Gondar Zone public health facilities, Ethiopia: A cross-sectional study. Postgraduate Medical Journal, postgradmedj–2020. https://doi.org/10.1136/postgradmedj-2020-139382
Barro, L., Drew, V. J., Poda, G. G., Tagny, C. T., El-Ekiaby, M., Owusu-Ofori, S., & Burnouf, T. (2018). Blood transfusion in sub-saharan Africa: Understanding the missing gap and responding to present and future challenges. Vox Sanguinis, 113(8), 726–736. https://doi.org/10.1111/vox.12705
Bates, I., Chapotera, G. K., McKew, S., & van den Broek, N. (2008). Maternal mortality in sub-saharan Africa: The contribution of ineffective blood transfusion services. Bjog, 115(11), 1331–1339. https://doi.org/10.1111/j.1471-0528.2008.01866.x
Bell, S. F., Watkins, A., John, M., Macgillivray, E., Kitchen, T. L., James, D., & Collins, P. W. (2020). Incidence of postpartum haemorrhage defined by quantitative blood loss measurement: A national cohort. BMC Pregnancy and Childbirth, 20(1), 271. https://doi.org/10.1186/s12884-020-02971-3
Bewket, T., Ensieh, F., Gayle, M., & Virginia, P. (2022a). Incidence, mortality, and factors associated with primary postpartum haemorrhage following in-hospital births in northwest Ethiopia. PloS One, 17(4), e0266345. https://doi.org/10.1371/journal.pone.0266345
Bewket, T., Ensieh, F., Virginia, P., & Gayle, M. (2022b). Barriers to effective management of primary postpartum haemorrhage following in-hospital births in northwest Ethiopia: healthcare providers’ views using a qualitative approach. BMC pregnancy and childbirth, 22(1), 755. https://doi.org/10.1186/s12884-022-05071-6
Bibi, S., Danish, N., Fawad, A., & Jamil, M. (2007). An audit of primary post partum hemorrhage. J Ayub Med Coll Abbottabad, 19(4), 102–106.
Biruk, A. K., Ritbano, A. A., Abebe, A. A., & Beminet, M. G. (2019). Prevalence and predictors of primary postpartum hemorrhage: An implication for designing effective intervention at selected hospitals, Southern Ethiopia. PloS one, 14(10), e0224579. https://doi.org/10.1371/journal.pone.0224579
Carroli, G., Cuesta, C., Abalos, E., & Gulmezoglu, A. M. (2008). Epidemiology of postpartum haemorrhage: A systematic review. Best Pract Res Clin Obstet Gynaecol, 22(6), 999–1012. https://doi.org/10.1016/j.bpobgyn.2008.08.004
Dupont, C., Deneux-Tharaux, C., Touzet, S., Colin, C., Bouvier-Colle, M. H., Lansac, J., & Rudigoz, R. C. (2011). Clinical audit: A useful tool for reducing severe postpartum haemorrhages? International Journal for Quality in Health Care, 23(5), 583–589. https://doi.org/10.1093/intqhc/mzr042
Escobar, M. F., Nassar, A. H., Theron, G., Barnea, E. R., Nicholson, W., Ramasauskaite, D., & Nasner, D. (2022). FIGO recommendations on the management of postpartum hemorrhage 2022. International Journal of Gynaecology and Obstetrics, 157(Suppl 1), 3–50. https://doi.org/10.1002/ijgo.14116. Suppl 1.
Ethiopian Public Health Institute (EPHI) (2020). National Maternal and Perinatal Death Surveillance and Response (MPDSR) System Annual Report 2012 EFY. Federal Ministry of Health of Ethiopia.
Ethiopian Public Health Institute (EPHI). (2017). National technical guidance for maternal and perinatal death surveillance and response. Federal Ministry of Health of Ethiopia.
Federal Ministry of Health of Ethiopia (FMoH). (2021a). Obstetrics management protocol for hospitals. Federal Ministry of Health of Health of Ethiopia.
Federal Ministry of Health of Ethiopia (FMoH). (2021b). Health sector transformation plan II,2020/21–2024/2025 (2013–2017 EFY). Federal Ministry of Health of Ethiopia.
Federal Ministry of Health of Ethiopia (FMoH). (2022). National guideline on prevention and management of postpartum hemorrhage. Federal Ministry of Health of Ethiopia.
Federspiel, J. J., Eke, A. C., & Eppes, C. S. (2023). Postpartum hemorrhage protocols and benchmarks: Improving care through standardization. American Journal of Obstetrics & Gynecology, 5(2), 100740.
Firoz, T., Chou, D., von Dadelszen, P., Agrawal, P., Vanderkruik, R., Tunçalp, O., & Maternal Morbidity Working, G. (2013). Measuring maternal health: Focus on maternal morbidity. Bulletin of the World Health Organization, 91(10), 794–796. https://doi.org/10.2471/blt.13.117564
Gallos, I., Devall, A., Martin, J., Middleton, L., Beeson, L., Galadanci, H., & Moran, N. (2023). Randomized trial of early detection and treatment of postpartum hemorrhage. New England Journal of Medicine, 389(1), 11–21.
Getie, A., & Wondmieneh, A. (2020). Blood donation practice and associated factors in Ethiopia: A systematic review and meta-analysis. 2020, 8852342. https://doi.org/10.1155/2020/8852342
Habitamu, D., Goshu, Y. A., & Zeleke, L. B. (2019). The magnitude and associated factors of postpartum hemorrhage among mothers who delivered at Debre Tabor general hospital 2018. BMC Research Notes, 12(1), 618. https://doi.org/10.1186/s13104-019-4646-9
Higgins, N., Patel, S. K., & Toledo, P. (2019). Postpartum hemorrhage revisited: New challenges and solutions. Current Opinion in Anaesthesiology, 32(3), 278–284. https://doi.org/10.1097/aco.0000000000000717
Jemberu, N., Bekahegn, G., Alemayehu, M., Takla, T., & Ruth, T. (2022). Magnitude of postpartum hemorrhage and its associated factors in Ethiopia: A systematic review and meta-analysis. Reprod Health, 19(1), 63. https://doi.org/10.1186/s12978-022-01360-7
Knight, M., & Lindquist, A. (2013). The UK Obstetric Surveillance System: Impact on patient safety. Best Pract Res Clin Obstet Gynaecol, 27(4), 621–630. https://doi.org/10.1016/j.bpobgyn.2013.03.002
Knight, M., & Tuffnell, D. (2018). A View from the UK: The UK and Ireland Confidential Enquiry into maternal deaths and morbidity. Clinical Obstetrics and Gynecology, 61(2), 347–358. https://doi.org/10.1097/grf.0000000000000352
Knight, M., Kurinczuk, J. J., Tuffnell, D., & Brocklehurst, P. (2005). The UK Obstetric Surveillance System for raredisorders of pregnancy. BJOG: An International Journal of Obstetrics & Gynaecology, 112(3), 263–265.
Liu, C. N., Yu, F. B., Xu, Y. Z., Li, J. S., Guan, Z. H., Sun, M. N., & Chen, D. J. (2021). Prevalence and risk factors of severe postpartum hemorrhage: A retrospective cohort study. Bmc Pregnancy and Childbirth, 21(1), 332. https://doi.org/10.1186/s12884-021-03818-1
Mavrides, E., Chandraharan, A. S., Collins, E., Green, P., Hunt, L., Riris, B. J., & Thomson, S. AJ (2016). Prevention and Management of Postpartum Haemorrhage: Green-top Guideline 52. Bjog, 124(5), e106–e149. https://doi.org/10.1111/1471-0528.14178
Moodley, J., Pattinson, R. C., Fawcus, S., Schoon, M., Moran, N., Shweni, P., & Africa, N. C. (2014). o. C. E. i. M. D. i. S. The confidential enquiry into maternal deaths in S outh A frica: a case study. BJOG: An International Journal of Obstetrics & Gynaecology, 121, 53–60.
Ngwenya, S. (2016). Postpartum hemorrhage: Incidence, risk factors, and outcomes in a low-resource setting. Int J Womens Health, 8, 647.
Osaro, E., & Charles, A. T. (2011). The challenges of meeting the blood transfusion requirements in Sub-saharan Africa: The need for the development of alternatives to allogenic blood. J Blood Med, 2, 7–21. https://doi.org/10.2147/jbm.s17194
Prasertcharoensuk, W., Swadpanich, U., & Lumbiganon, P. (2000). Accuracy of the blood loss estimation in the third stage of labor. International Journal of Obstetrics & Gynecology, 71(1), 69–70.
Razvi, K., Chua, S., Arulkumaran, S., & Ratnam, S. (1996). A comparison between visual estimation and laboratory detennination of blood loss during the third stage of labour. Australian and New Zealand Journal of Obstetrics and Gynaecology, 36(2), 152–154.
Say, L., Chou, D., Gemmill, A., Tunçalp, Ö., Moller, A. B., Daniels, J., & Alkema, L. (2014). Global causes of maternal death: A WHO systematic analysis. Lancet Glob Health, 2(6), e323–333. https://doi.org/10.1016/s2214-109x(14)70227-x
Seim, A. R., Alassoum, Z., Souley, I., Bronzan, R., Mounkaila, A., & Ahmed, L. A. (2023). The effects of a peripartum strategy to prevent and treat primary postpartum haemorrhage at health facilities in Niger: A longitudinal, 72-month study. The Lancet Global Health, 11(2), e287–e295.
Shakespeare, J., & Knight, M. (2017). The Confidential Enquiry into maternal deaths 2015: Lessons for GPs. British Journal of General Practice, 67(658), 233–234. https://doi.org/10.3399/bjgp17X690845
Sinetibeb, M., Merga, D., Sagni, G. F., & Abera, K. T. (2021). Assessment of Postpartum Hemorrhage in a University Hospital in Eastern Ethiopia: A cross-sectional study. Int J Womens Health, 13, 663–669. https://doi.org/10.2147/IJWH.S300143
Sørensen, J. B., Housseine, N., Maaløe, N., Bygbjerg, I. C., Pinkowski Tersbøl, B., Konradsen, F., & Kidanto, L., H (2022). Scaling up locally adapted clinical practice guidelines for improving Childbirth Care in Tanzania: A protocol for Programme Theory and qualitative methods of the PartoMa scale-up study. Global Health Action, 15(1), 2034136. https://doi.org/10.1080/16549716.2022.2034136
Souza, J. P., Gülmezoglu, A. M., Vogel, J., Carroli, G., Lumbiganon, P., & Qureshi, Z. (2013). e. a. Moving beyond essential interventions for reduction of maternal mortality (the WHO Multicountry Survey on Maternal and Newborn Health): a cross-sectional study. Lancet, 381(9879), 1747–1755. https://doi.org/10.1016/s0140-6736(13)60686-8
Tadesse, T., Getahun, F., Edgeit, A. Z., Merga, B., & Tafese, D. J. (2022). Magnitude of postpartum hemorrhage and associated factors among women who gave birth in Ethiopia: A systematic review and meta-analysis. Reproductive Health, 19(1), 194. https://doi.org/10.1186/s12978-022-01498-4
Taye Makuria, A., Gebremichael, D., Demoz, H., Hadush, A., Abdella, Y., Berhane, Y., & Kamani, N. (2017). Obstetric hemorrhage and safe blood for transfusion in Ethiopia: The challenges of bridging the gap. Transfusion, 57(10), 2526–2531. https://doi.org/10.1111/trf.14219
Temesgen, M. (2017). Magnitude of postpartum hemorrhage among women delivered at Dessie referral hospital, South Woll, Amhara region, Ethiopia. J Women’s Health Care, 6(391), 2167–04201000391.
van Stralen, G., von Schmidt auf Altenstadt, J. F., Bloemenkamp, K. W., van Roosmalen, J., & Hukkelhoven, C. W. (2016). Increasing incidence of postpartum hemorrhage: The Dutch piece of the puzzle. Acta Obstetricia et gynecologica Scandinavica, 95(10), 1104–1110.
Willcox, M. L., Price, J., Scott, S., Nicholson, B. D., Stuart, B., Roberts, N. W., & Harnden, A. (2020). Death audits and reviews for reducing maternal, perinatal and child mortality. Cochrane Database of Systematic Reviews(3).
World Health Organization (WHO) (2023b). Trends in maternal mortality 2000 to 2020: estimates by WHO, UNICEF, UNFPA, World Bank Group and UNDESA/Population Division. Geneva: World Health Organization; 2023. Licence: CC BY-NC-SA 3.0 IGO.
World Health Organization (WHO). (2012). WHO Guidelines approved by the guidelines Review Committee. WHO recommendations for the Prevention and Treatment of Postpartum Haemorrhage. World Health Organization.
World Health Organization (WHO). (2018). WHO recommendations: Uterotonics for the prevention of postpartum haemorrhage. World Health Organization.
World Health Organization (WHO). (2023). A roadmap to combat postpartum haemorrhage between 2023 and 2030. World Health Organization.
Zarocostas, J. (2023). Global maternal mortality rates stagnating. The Lancet, 401(10377), 632.
Acknowledgements
The authors are thankful to medical directors and heads of maternity units of included hospitals, Haramaya University, National Perinatal Epidemiology Unit of the University of Oxford, Leiden University Medical Centre, study participants, data collectors and field supervisors for their inputs into this study.
Funding
The study was funded by the MRC (MR/T037962/1) as part of the 2019 Global Maternal and Neonatal Health Funding call to MK who is a Senior Investigator at National Institute for Health Research (NIHR). SG is funded by Leiden University Medical Center for his PhD study. The funders had no role in the study design, data collection and analysis, manuscript preparation or the decision for publication.
Author information
Authors and Affiliations
Contributions
Conception or design of the work, SG, AKT, MK and TvdA; data collection, SG, RA, and AKT; data analysis and interpretation, SG and AKT; drafting the article, SG; critical revision of the article, AKT, RA, MK and TvdA. All authors read and approved the manuscript prior to submission.
Corresponding author
Ethics declarations
Ethical Approval
The study was conducted in accordance with the Declaration of Helsinki. The study protocol was reviewed and approved by the Institutional Health Research Ethics Review Committee of the College of Health and Medical Sciences of Haramaya University, Ethiopia (Ref No. IHRERC/024/2021); and the University of Oxford’s Oxford Tropical Research Ethics Committee (OxTREC); (Reference 530 − 21). Informed consent for the study was obtained from medical directors and heads of maternity units of each hospital. This study is based on a review of case files after a woman’s discharge or death, and therefore the need for consent from individual woman was waived.
Consent to Participate
This study is based on a review of case files after a woman’s discharge or death, and therefore, the need for consent from individual woman was waived. The facility’s consent to be part of the study was signed by the medical director and the head of the maternity unit of each of the respective hospitals. Data collectors also signed data privacy consent forms to keep confidentiality of the information they accessed during data abstraction.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Girma, S., Tura, A.K., Ahmed, R. et al. Incidence, Causes and Outcomes of Postpartum Hemorrhage in Eastern Ethiopia: A Multicenter Surveillance Study. Matern Child Health J (2024). https://doi.org/10.1007/s10995-024-03986-4
Accepted:
Published:
DOI: https://doi.org/10.1007/s10995-024-03986-4