Abstract
The role of awake prone positioning (aPP) in patients with acute hypoxemic respiratory failure is debated. We performed a systematic review and meta-analysis to evaluate the role of aPP in acute respiratory failure related to COronaVIrus Disease-19 (COVID-19). Studies reporting on the clinical course of patients with acute respiratory failure related to COVID-19 treated or not treated by aPP were included in the systematic review and meta-analysis (ProsperoID: CRD42022333211). The primary study outcome was the composite of in-hospital death or orotracheal intubation; the individual components of the primary outcome were secondary study outcomes. The composite of in-hospital death or orotracheal intubation was available for 6 studies (1884 patients), five randomized and one prospective; a significant reduction in the risk of this outcome was observed in patients treated vs. not treated by aPP (33.5% vs. 39.8%; OR 0.73, 95% CI 0.60–0.89; I2 0%). In-hospital death was reported in 34 studies (6808 patients) and occurred in 17.4% vs. 23.5% of patients treated or not treated with aPP (random effect OR 0.60, 95% CI 0.46–0.79; I2 59%); orotracheal intubation was observed in 25.8% vs. 32.7% of patients treated or not treated with aPP (27 studies, 5369 patients; random effect OR 0.85, 95% CI 0.56–1.27; I2 84%). aPP reduces the risk for death or orotracheal intubation in patients with acute respiratory failure related to COVID-19. Further studies should be conducted to confirm the clinical benefit of aPP outside the ICU.
Registration Prospero ID: CRD42022333211.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronavirus 19 infection (COVID-19) is responsible for severe acute respiratory syndrome (SARS-CoV-2) that can evolve to progressive hypoxemic respiratory failure and to severe acute respiratory distress syndrome (ARDS) in about 17% of unvaccinated patients [1].
In the pre-COVID-19 era, a number of studies demonstrated a significant improvement in oxygenation and pulmonary mechanics by the use of prone positioning in patients requiring invasive mechanical ventilation for ARDS [2]. Prone positioning allows more even distribution of the gas–tissue ratios along the dependent–non-dependent axis and a more homogeneous distribution of lung stress and strain. In a randomized study, early and prolonged prone positioning sessions (of at least 16 h) were associated with a reduction of about 61% in mortality with no increase in adverse events in intubated patients admitted to intensive care units (ICUs) [3]. These results were later confirmed in several meta-analyses [4]. Based on this evidence, prone positioning has been used for more than 40 years to improve oxygenation in intubated patients with ARDS [5] and is now strongly advocated in the management of moderate-to-severe ARDS [6].
During SARS-CoV-2 pandemic, several cohort studies claimed an effect of prone positioning in reducing mortality in intubated patients with SARS-CoV-2-related ARDS [7]. The World Health Organization guidelines recommend prone positioning for the management of intubated COVID-19 patients with ARDS as a beneficial practice despite the lack of evidence from randomized clinical trials [8]. The use of prone positioning has also been proposed in awake COVID-19 patients with severe respiratory failure, to improve oxygenation and reduce progression to orotracheal intubation [9]. However, conflicting results are currently available on the role of awake prone positioning in this setting. As for today, the effectiveness of prone positioning in reducing progression to intubation and mortality in awake COVID-19 patients remains unclear [10, 11].
The aim of this systematic review and meta-analysis is to assess the role of awake prone positioning in reducing death or orotracheal intubation in patients with acute respiratory failure related to COVID-19.
Methods
A protocol for this study was prospectively developed detailing the specific objectives, criteria for study selection, approach to assess study quality, outcomes, and statistical methods (PROSPERO registration number CRD42022333211).
This study was conducted according to the methodology suggested by the Providing Innovative Service Models and Assessment (PRISMA) criteria [12].
Data sources and searches
We performed an unrestricted search in Pubmed, Web of Science, OVID, MedRxiv, and ClinicalTrials.gov, from inception through March 22, 2023. No language restrictions were applied. Reference lists of retrieved articles and review articles were manually searched for other relevant studies. The search strategy is reported in the Supplementary material.
Study selection
Seven reviewers (M.G., A.G.R., D.B., F.B., L.L., R.R., C.C.) performed study selection independently, with disagreements solved through discussion and the opinion of an additional reviewer (C.B.). Studies in patients with COVID-19 were considered eligible for the systematic review and meta-analysis if they met the following predetermined criteria: (a) inclusion of hospitalized and non-intubated patients with acute respiratory failure related to COVID-19; (b) inclusion of patients treated and non-treated with prone positioning; and (c) reporting on study outcome events in patients treated and not treated with prone positioning. Studies were excluded in case of (a) diagnosis of COVID-19 not confirmed by molecular swab testing; (b) case reports; and (c) inclusion of less than 20 patients.
Study outcome
The primary study outcome was the composite of in-hospital death or need for endotracheal intubation.
Secondary study outcomes were the individual components of the primary outcome: in-hospital death and need for orotracheal intubation.
Need for orotracheal intubation was reported according to the definition used in the individual studies.
For duplicate publications, the most complete was considered.
Data extraction and risk of bias assessment
For each study, the following data were extracted independently by two authors: general study data (design, year of publication), population characteristics (mean age, gender, severity of respiratory failure, use of non-invasive ventilation), clinical setting (intensive care unit [ICU], non-ICU), data on prone positioning (number of patients and duration), and study outcomes (in-hospital death or endotracheal intubation and the individual components of the composite outcome in patients treated and not treated with prone positioning).
Risk of bias of selected studies was independently assessed by three reviewers (A.G.R., M.G., and D.B.) using the Cochrane Collaboration’s tools (ROBIS-I for non-randomized and ROB-II for randomized studies [RCTs]), which cover the following bias domains: selection bias, performance bias, detection bias, attrition bias, and reporting bias [13]. Each potential source of bias was graded as high, low, or some concerns, which determined whether the studies were considered at high, low, or moderate risk of bias.
We resolved disagreements in study data extraction and risk of bias assessment by consensus or by discussion with an additional reviewer (C.B.).
Statistical analysis
Study outcomes were compared in patients treated or not treated by awake prone positioning.
Estimates of pooled effect sizes were obtained by the Mantel–Haenszel method. Pooled odds ratios (ORs) were reported with 95% confidence intervals (CIs). Forest plots were created for each outcome. Statistically significant heterogeneity was considered present at I2 > 50% or Cochran’s chi2 test p < 0 [14, 15]. Results were reported according to fixed-effects model in the absence of significant heterogeneity and to random-effects model in the presence of significant heterogeneity. Correction for zero cells was performed by adding 0.5 to all zeros, when risk measures were not estimable [16]. Publication bias was assessed visually by funnel plots inspection.
To assess potential sources of heterogeneity, pre-defined sensitivity analyses were conducted as it follows: (i) studies including patients admitted to ICU vs. non-ICU; (ii) duration of prone positioning lower than 6 hours, between 6 and 12 h or ≥ 12 h/day; (iii) studies recruiting from 1/2020 to 12/2020 vs. beyond January 2021; (iv) retrospective vs. prospective vs. RCTs; (v) follow-up lower than seven days vs. between 7 and 14 days vs. between 14 and 28 days vs. over 28 days; (vi) studies including ≤ 100 patients vs. > 100 patients; (vii) studies with low risk of bias vs. moderate vs. high; and (viii) studies excluding vs. including do-not-resuscitate (DNR) patients.
The statistical analyses, forest plots, and funnel plots were produced by using Review Manager release 5.4 (The Cochrane Collaboration, Oxford, England) and STATA/SE 12 (StataCorp LP, College Station, TX, USA).
Results
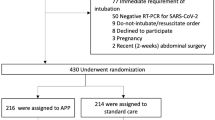
Overall, 9443 studies were retrieved by electronic searches and 111 were selected as candidates for inclusion in the study after title and abstract review. After full text review, 34 studies (6808 patients) were finally identified for inclusion in the systematic review and meta-analysis [17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50]. The flow of study selection is reported in e-Fig. 1 reported on Supplementary material.
The main features of included studies are reported in e-Table 1. Six studies were RCTs and 10 were prospective and 18 retrospective cohorts. Fifteen studies reported on non-intubated patients in the setting of ICU [17, 19,20,21,22, 25, 27, 30, 33, 36, 46, 48, 49] and two studies a mixed ICU–non-ICU population [24, 40]. The number of included patients varied across the included studies between 20 and 1121. The duration of follow-up was available for 31 studies and was less than 7 days, between 7 and 14 days, between 14 and 28 days, and more than 28 days, in six, ten, six, and six studies, respectively.
The proportion of patients treated with awake prone positioning, as well as the methods for prone positioning (duration, number of sessions), largely varied across the included studies (e-table 1).
The risk of bias for the included RCTs was low and moderate in four and two studies each (e-table 4); the risk of bias was moderate for the majority of cohort studies (e-table 4). Overall, the risk of bias was critical in two and serious in four studies.
Clinical course with vs. without awake prone positioning
The composite of in-hospital death or orotracheal intubation was reported in two studies and was available after contact with the authors in additional four studies [17, 24, 25, 33, 34, 43]. Five of these studies were randomized, open-label studies and one prospective study, overall including 1884 patients, 961 treated with and 923 without awake prone positioning. The analysis of these studies showed a significant reduction in the incidence of in-hospital death or orotracheal intubation in favor of awake prone positioning (fixed effect OR 0.74, 95% CI 0.60–0.90; I2 0%) (Fig. 1).
Incidences of in-hospital death and of orotracheal intubation in each study by use of awake prone positioning are reported in Table 1.
In-hospital death was reported in 34 studies and occurred in 17.4% of 3169 patients receiving and in 23.5% of 3639 patients not receiving awake prone positioning, respectively; in these studies, awake prone positioning was associated with a significant reduction in mortality (random effect OR 0.60, 95% CI 0.46–0.79, I2 59%) [17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50] (Fig. 2). These results were confirmed after correction for zero cells (random effect OR 0.61, 95% CI 0.49–0.76, I2 50%) (e-Fig. 2).
Orotracheal intubation was reported in 27 studies (5369 patients) and occurred in 25.8% and in 32.7% of patients treated or not treated by awake prone positioning (random effect OR 0.85, 95% CI 0.56–1.27; I2 84%) [17,18,19,20,21,22,23,24,25,26,27,28, 30, 33,34,35,36, 38,39,40,41, 43, 44, 47,48,49,50] (Fig. 3). These results were confirmed after correction for zero cells (random effect OR 0.78, 95% CI 0.53–1.15, I2 83.3%) (e-Fig. 3).
No evidence of publication bias was observed at funnel plot inspection for these analyses (Supplementary material e-Fig. 4).
Sensitivity analyses
Sensitivity analyses were conducted for the secondary outcomes (Table 2; e-Fig. 5 to e-Fig. 16).
When the analysis was conducted by study design, awake prone positioning was associated with reduction of in-hospital death in retrospectives studies (18 studies, 3597 patients; 16.8% vs. 25.6%; random effect OR 0.45, 95% CI 0.30–0.66; I2 57%) and not in prospective studies and in RCTs (Fig. 1; e-Fig. 4a); awake prone positioning was associated with reduction of orotracheal intubation in RCTs (six studies, 1934 patients; 28.5% vs. 34.0%; random effect OR 0.76, 95% CI 0.62–0.93; I2 0%) and not in prospective or retrospective studies (Fig. 2; e-Fig. 4b).
In studies conducted in the ICU setting, awake prone positioning was associated with significant reduction of both in-hospital death (15 studies, 2397 patients; 18.2% vs. 23.3%; random effect OR 0.62, 95% CI 0.43–0.89, I 2 36%) and orotracheal intubation (12 studies, 1541 patients; 28.5% vs. 46.0%; random effect OR 0.53, 95% CI 0.30–0.93; I2 72%); in studies conducted outside the ICU setting or in mixed ICU or non-ICU patients, no association with mortality was observed (e-Fig. 5a significant reduction in orotracheal intubation was observed with awake prone positioning in studies reporting both ICU or non-ICU patients (two studies, 1945 patients; 27.5% vs. 40.2%; random effect OR 0.55, 95% CI 0.31–0.98; I2 88%), while no effect was observed in studies conducted outside the ICU (Table 2; e-Fig. 6).
Concerning duration of awake prone positioning, a reduction in mortality was observed in studies using sessions lasting less than six hours or in studies using sessions lasting between 6 and 12 h, while no effect in mortality was observed in studies using awake prone positioning over 12 h (e-Fig. 7). No association was observed between duration of proning and orotracheal intubation (e-Fig. 8).
Awake prone positioning was associated with significant reduction in mortality in both studies including less than 100 patients and studies including more than 100 patients (Table 2; e-Fig. 9). No association was observed between the number of included patients and orotracheal intubation (e-Fig. 10).
A significant reduction of in-hospital mortality (9 studies, 2592 patients, 14.6% vs. 29.6%; random effect OR 0.26, 95% CI 0.11–0.64, I2 86%) (e-Fig. 11) and of orotracheal intubation was observed in studies reporting on study outcome events occurring at 14–28 days ( 9 studies, 2568 patients, 26.3% vs. 41.1%; random effect OR 0.46, 95% CI 0.26–0.82, I2 80%) (e-Fig. 12).
Awake prone positioning was associated with reduction in mortality in studies including patients until December 31, 2020, while this benefit disappeared in studies including patients beyond December 31, 2020 (e-Fig. 13). In addition, awake prone positioning was associated with a significant reduction in orotracheal intubation in studies including patients until December 31, 2020 (20 studies, 4260 patients; 27.0% vs. 34.0%; random effect OR 0.75, 95% CI 0.65–0.87, I 2 86%) and beyond December 31, 2020 (five studies, 619 patients; 10.2% vs. 19.9%; random effect OR 0.48, 95% CI 0.30–0.76, I2 41%)(e-Fig. 14).
Awake prone positioning was associated with a 50% reduction in mortality in studies with moderate risk of bias (19 studies, 3214 patients; 16.9% vs. 25.3%; random effect OR 0.50, 95% CI 0.33–0.75, I2 56%), while no effect was observed in the remaining studies (e-Fig. 15). No association was observed with orotracheal intubation by quality of the studies (e-Fig. 16).
Of note, awake prone positioning was associated with a reduction in the risk of death and of orotracheal intubation in the 6 studies (2137 patients) that excluded DNR patients [17, 38, 39, 43, 48, 49].
Discussion
Our systematic review and meta-analysis show that awake prone positioning reduces the composite of in-hospital death or orotracheal intubation in patients with acute respiratory failure due to COVID-19; in addition, our results suggest a reduced risk of in-hospital mortality by the use of awake prone positioning, mainly driven by retrospective studies and not observed in RCTs. Awake prone positioning was not associated with orotracheal intubation in the overall analysis, but it was in RCTs. The clinical benefits of awake prone positioning were more consistent for studies conducted in the setting of ICU in comparison to studies conducted outside the ICU.
Awake prone positioning has been proposed for the management of ARDS based on the hypothesis that the expected improvement in oxygenation would have led to an improvement in survival [51]. Reduction in mortality by prone positioning had been demonstrated in studies conducted with strict application of protective lung ventilation in non-COVID-19 intubated patients [52]. The COVID-19 outbreak led to a dramatic increase in the proportion of patients presenting with ARDS, probably due to the loss of hypoxic vasoconstriction leading to blood maldistribution and shunt effect. Prone positioning may improve ventilation/perfusion mismatch by increasing alveolar recruitment of basal regions and reduce dorsal over-distension. The high proportion of patients presenting with or progressing to ARDS during the COVID-19 outbreak led to change the use of awake prone positioning from a salvage therapy for refractory hypoxemia to an upfront lung-protective strategy intended to improve survival in severe respiratory failure. Of note, the benefit of medical treatments, if any, in improving clinical outcome in COVID-19 patients was dependent on early use, before progression to severe disease and in particular before the need for orotracheal intubation [53, 54]. For these reasons, the use of awake prone positioning was extended to awake patients in and out of ICUs, in an attempt to prevent disease progression [55].
Our meta-analysis shows that prone positioning reduces the composite of in-hospital death or orotracheal intubation. This composite outcome has been largely used in the COVID-19 era to assess the role of different treatment strategies. In fact, progression to orotracheal intubation was a common event and was strongly associated with mortality, mainly in the pre-vaccine era [56].
The analyses of aggregate data show a reduction in mortality by the use of awake prone positioning. This result is promising, as it suggests the effectiveness of a non-pharmacological management strategy in patients with acute hypoxemic respiratory failure. However, before encouraging a worldwide use of awake prone positioning in this setting, further evidence from high-quality studies is required. In fact, a reduction in mortality was not achieved in RCTs and is mainly driven by retrospective studies. Retrospective studies cannot be used to demonstrate the efficacy of clinical interventions as their results are likely to be influenced by confounding factors and the standardization of treatment is not guaranteed; in addition, in awake patients with acute hypoxemic respiratory failure [57], maintaining prone position can be particularly challenging and poor comfort has been reported mainly in those patients assisted by non-invasive ventilation. Finally, it should be noted that the use of prone positioning has been associated with delay in intubation, probably due to initial improvement in oxygenation. This delay can be harming for patients as delayed intubation increases work of breathing [58]and may increase mortality [59].
The analysis of aggregate data shows no significant effect of awake prone positioning in the risk for orotracheal intubation in all the studies; of note, a reduction in the risk for orotracheal intubation was observed in the analysis conducted in RCTs and in studies in patients managed in the ICU setting. It is conceivable that the use of standardized criteria for orotracheal intubation and the homogeneity of the study populations could have driven the results of the RCTs. In addition, a reduction in the risk for orotracheal intubation was observed in the analysis of studies that excluded DNR patients. Whether the failure to find a benefit in terms of progression to orotracheal intubation in the overall studies analysis is due to an actual limit of prone positioning or whether it is related to the high heterogeneity in study populations remains to be defined.
Concerning the sensitivity analyses, their results show that the association of awake prone positioning with the study outcomes substantially differ in RCTs in comparison to cohort studies; heterogeneity disappeared when the analysis was limited to RCTs. In addition, the benefits of awake prone positioning were mainly driven by studies conducted in the ICU setting, despite significant heterogeneity. Expertise in prone positioning could have driven the favorable results obtained in death and in orotracheal intubation in this setting. Despite no definite standardization exists on criteria for ICU admission, it is conceivable that COVID-19 patients admitted to ICU were probably more homogeneous in terms of severity of respiratory failure, reduced prevalence of DNR patients, and comorbidities respect to non-ICU patients. Sensitivity analysis by risk of bias showed persistence of significant heterogeneity regardless of the estimated risk of bias. Of note, the majority of the studies included in our meta-analysis had moderate risk of bias according to the Cochrane Collaboration’s Tools.
Our study has some limitations. Firstly, the intrinsic limit of the meta-analysis approach which combines heterogeneous datasets. This limit is particularly evident in our study, reporting a significant degree of heterogeneity in several analyses. In particular, the heterogeneity is lower when combining RCTs. It should be considered that our meta-analysis probably reports on first experience on prone positioning practiced outside the ICU and this may have required a time for acquisition of skillness and expertise. In addition, protocols of prone positioning were heterogeneous among studies, mainly concerning duration of cycles and duration of treatment, and this may have influenced the study results. Data in DNR patients and in vaccinated patients are not separately reported in the included studies and sensitivity analyses were not feasible. Furthermore, as these are aggregated data, meta-analysis with adjustment for age, comorbidities, severity of disease, or concomitant treatments was allowed. Finally, all included studies had an open design, that could have influenced decision making on orotracheal intubation.
Our study also has some strengths. The meta-analysis includes more than 30 studies, allowing analyses on over 5000 patients and the conduction of several sensitivity analyses that may generates hypotheses for future properly designed trials in this setting.
Conclusion
Awake prone positioning reduces the risk for death or orotracheal intubation and, probably, the risk for death in patients with acute respiratory failure related to COVID-19, mainly when used in the setting of ICU. Further randomized studies should be conducted to confirm the clinical benefit of awake prone positioning and to validate standardized protocols for this procedure.
Data availability
The database is available on reasonable request to the corresponding author.
Abbreviations
- aPP:
-
Awake prone positioning
- ARDS:
-
Acute respiratory distress syndrome
- COVID-19:
-
COronaVIrus Disease-19
- ICU:
-
Intensive care unit
- P/F :
-
Partial pressure arterial oxygen and fraction of inspired oxygen
- RR:
-
Respiratory rate
References
Tenforde MW, Self WH, Adams K, Influenza and Other Viruses in the Acutely Ill (IVY) Network et al (2021) Association between mRNA vaccination and COVID-19 hospitalization and disease severity. JAMA 326(20):2043–2054
Guérin C, Albert RK, Beitler J, Gattinoni L, Jaber S, Marini JJ, Munshi L, Papazian L, Pesenti A, Vieillard-Baron A, Mancebo J (2020) Prone position in ARDS patients: why, when, how and for whom. Intensive Care Med 46(12):2385–2396
Guérin C, Reignier J, Richard JC et al (2013) Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 368(23):2159–2168
Munshi L, Del Sorbo L, Adhikari NKJ et al (2017) Prone position for acute respiratory distress syndrome. A systematic review and meta-analysis. Ann Am Thorac Soc 14:S280–S288
Bryan AC (1974) Conference on the scientific basis of respiratory therapy. Pulmonary physiotherapy in the pediatric age group. Comments of a devil’s advocate. Am Rev Respir Dis 110(6 Pt 2):143–144
Shelhamer MC, Wesson PD, Solari IL, Jensen DL, Steele WA, Dimitrov VG, Kelly JD, Aziz S, Gutierrez VP, Vittinghoff E, Chung KK, Menon VP, Ambris HA, Baxi SM (2021) Prone positioning in moderate to severe acute respiratory distress syndrome due to COVID-19: a cohort study and analysis of physiology. J Intensive Care Med 36(2):241–252
Astasio-Picado Á, del Rocío Sánchez-Sánchez M (2021) Effectiveness of prone positioning in patients with COVID-19-related acute respiratory distress syndrome undergoing invasive mechanical ventilation. Appl Sci 11(21):10263
World Health Organization (2020) Clinical management of severe acute respiratory infection when novel coronavirus (nCoV) infection is suspected: interim guidance. https://apps.who.int/iris/handle/10665/330893. Accessed Oct 2020
McGuire WC, Pearce AK, Malhotra A (2021) Prone positioning might reduce the need for intubation in people with severe COVID-19. Lancet Respir Med 9(12):e110
Fazzini B, Page A, Pearse R, Puthucheary Z (2022) Prone positioning for non-intubated spontaneously breathing patients with acute hypoxaemic respiratory failure: a systematic review and meta-analysis. Br J Anaesth 128(2):352–362
Touchon F, Trigui Y, Prud’homme E et al (2021) Awake prone positioning for hypoxaemic respiratory failure: past, COVID-19 and perspectives. Eur Respir Rev 30(160):210022
Hutton B, Salanti G, Caldwell DM et al (2015) The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 162(11):777–784
Cochrane Scientific Committee (2017) Recommendation statement/report
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558
Leeflang MM, Deeks JJ, Rutjes AW, Reitsma JB, Bossuyt PM (2012) Bivariate meta-analysis of predictive values of diagnostic tests can be an alternative to bivariate meta-analysis of sensitivity and specificity. J Clin Epidemiol 65(10):1088–1097
Altman DG, Chalmers I, Egger M, Smith GD (2001) Systematic reviews in health care: meta-analysis in context, 2nd edn. Blackwell BMJ Books, London
Alhazzani W, Parhar KKS, Weatherald J, COVI-PRONE Trial Investigators and the Saudi Critical Care Trials Group et al (2022) Effect of awake prone positioning on endotracheal intubation in patients with COVID-19 and acute respiratory failure: a randomized clinical trial. JAMA 327(21):2104–2113
Altinay M, Sayan I, Turk HS, Cinar AS, Sayın P, Yucel T, Islamoglu S, Ozkan MT, Cetiner I (2022) Effect of early awake prone positioning application on prognosis in patients with acute respiratory failure due to COVID-19 pneumonia: a retrospective observational study. Braz J Anesthesiol 72(2):194–199
Ateş İ, Erden A, Gürler EK et al (2021) Compliance to not only prone but also lateral and supine positioning improves outcome in hospitalised COVID-19 patients. Int J Clin Pract 75(11):e14673
Bahloul M, Kharrat S, Hafdhi M et al (2021) Impact of prone position on outcomes of COVID-19 patients with spontaneous breathing. Acute Crit Care 36(3):208–214
Barker J, Pan D, Koeckerling D et al (2021) Effect of serial awake prone positioning on oxygenation in patients admitted to intensive care with COVID-19. Postgrad Med J 98:360–364
Burton-Papp HC, Jackson AIR, Beecham R, University Hospital Southampton Critical Care Team; REACT COVID Investigators et al (2020) Conscious prone positioning during non-invasive ventilation in COVID-19 patients: experience from a single centre. F1000Res 9:859
Coppo A, Bellani G, Winterton D, Di Pierro M et al (2020) Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study. Lancet Respir Med 8(8):765–774
Ehrmann S, Li J, Ibarra-Estrada, Awake Prone Positioning Meta-Trial Group et al (2021) Awake prone positioning for COVID-19 acute hypoxaemic respiratory failure: a randomised, controlled, multinational, open-label meta-trial. Lancet Respir Med 9(12):1387–1395
Ferrando C, Mellado-Artigas R, Gea A et al (2020) Awake prone positioning does not reduce the risk of intubation in COVID-19 treated with high-flow nasal oxygen therapy: a multicenter, adjusted cohort study. Crit Care 24(1):597
Fralick M, Colacci M, Munshi L, COVID Prone Study Investigators et al (2022) Prone positioning of patients with moderate hypoxaemia due to covid-19: multicentre pragmatic randomised trial (COVID-PRONE). BMJ 376:e068585
Gad S (2021) Awake prone positioning versus non invasive ventilation for COVID-19 patients with acute hypoxemic respiratory failure. Egypt J Anaesth 37:85–90
Graziani M, Barbieri G, Maraziti G et al (2023) The role of prone positioning in patients with SARS-CoV-2-related respiratory failure in non-intensive care unit. Ther Adv Respir Dis 17:17534666231164536
Hallifax RJ, Porter BM, Elder PJ, Oxford Respiratory Group et al (2020) Successful awake proning is associated with improved clinical outcomes in patients with COVID-19: single-centre high-dependency unit experience. BMJ Open Respir Res 7(1):e000678
Hashemian SM, Jamaati H, Malekmohammad M et al (2021) Efficacy of early prone positioning combined with noninvasive ventilation in COVID-19. Tanaffos 20(2):82–85
Hussain HT (2021) Impact of proning in COVID-19 patients admitted in allama iqbal memorial teaching hospital Sialkot. Pak J Med Health Sci 15(6):1256–1258
Imran M (2021) Determine the impact of prone positioning in covid-19 patients. Pak J Med Health Sci 15(7):1864–1867
Jagan N, Morrow LE, Walters RW, Klein LP, Wallen TJ, Chung J, Plambeck RW (2020) The POSITIONED Study: prone positioning in nonventilated coronavirus disease 2019 patients—a retrospective analysis. Crit Care Explor 2(10):e0229
Jayakumar D, Ramachandran P, Rabindrarajan DNM et al (2021) Standard care versus awake prone position in adult nonintubated patients with acute hypoxemic respiratory failure secondary to COVID-19 infection—a multicenter feasibility randomized controlled trial. J Intensive Care Med 36(8):918–924
Johnson SA, Horton DJ, Fuller MJ et al (2021) Patient-directed prone positioning in awake patients with COVID-19 requiring hospitalization (PAPR). Ann Am Thorac Soc 18(8):1424–1426
Jouffroy R, Darmon M, Isnard F et al (2021) Impact of prone position in non-intubated spontaneously breathing patients admitted to the ICU for severe acute respiratory failure due to COVID-19. J Crit Care 64:199–204
Liu X, Liu H, Lan Q, Zheng X et al (2021) Early prone positioning therapy for patients with mild COVID-19 disease. Med Clin (Barc) 156(8):386–389
Musso G, Taliano C, Molinaro F et al (2022) Early prolonged prone position in noninvasively ventilated patients with SARS-CoV-2-related moderate-to-severe hypoxemic respiratory failure: clinical outcomes and mechanisms for treatment response in the PRO-NIV study. Crit Care 26(1):118
Padrão EMH, Valente FS, Besen BAMP, COVIDTEAM et al (2020) Awake prone positioning in COVID-19 hypoxemic respiratory failure: exploratory findings in a single-center retrospective cohort study. Acad Emerg Med 27(12):1249–1259
Perez-Nieto OR, Escarraman-Martinez D, Guerrero-Gutierrez MA et al (2021) Awake prone positioning and oxygen therapy in patients with COVID-19: the APRONOX study. Eur Respir J 59:2100265
Prud’homme E, Trigui Y, Elharrar X et al (2021) Effect of prone positioning on the respiratory support of nonintubated patients with COVID-19 and acute hypoxemic respiratory failure: a retrospective matching cohort study. Chest 160(1):85–88
Qian ET, Gatto CL, Amusina O, Vanderbilt Learning Healthcare System Platform Investigators et al (2022) Assessment of awake prone positioning in hospitalized adults with COVID-19: a nonrandomized controlled trial. JAMA Intern Med 182(6):612–621
Rosén J, von Oelreich E, Fors D, Jonsson Fagerlund M, Taxbro K, Skorup P, Eby L, Campoccia Jalde F, Johansson N, Bergström G, Frykholm P, PROFLO Study Group (2021) Awake prone positioning in patients with hypoxemic respiratory failure due to COVID-19: the PROFLO multicenter randomized clinical trial. Crit Care 25(1):209
Simioli F, Annunziata A, Langella G, Martino M, Musella S, Fiorentino G (2021) Early prone positioning and non-invasive ventilation in a critical COVID-19 subset. A single centre experience in Southern Italy. Turk Thorac J. 22(1):57–61
Sryma PB, Mittal S, Mohan A, Madan K et al (2021) Effect of proning in patients with COVID-19 acute hypoxemic respiratory failure receiving noninvasive oxygen therapy. Lung India 38(Supplement):S6–S10
Stilma W, van Meenen DMP, Valk CMA, On Behalf Of The PRoVENT-Covid Collaborative Group et al (2021) Incidence and practice of early prone positioning in invasively ventilated COVID-19 patients-insights from the PRoVENT-COVID observational study. J Clin Med 10(20):4783
Thompson AE, Ranard BL, Wei Y, Jelic S (2020) Prone positioning in awake, nonintubated patients with COVID-19 hypoxemic respiratory failure. JAMA Intern Med 180(11):1537–1539. https://doi.org/10.1001/jamainternmed.2020.3030
Tonelli R, Pisani L, Tabbì L, Comellini V et al (2022) Early awake proning in critical and severe COVID-19 patients undergoing noninvasive respiratory support: a retrospective multicenter cohort study. Pulmonology 28(3):181–192
Vianello A, Turrin M, Guarnieri G, Molena B et al (2021) Prone positioning is safe and may reduce the rate of intubation in selected COVID-19 patients receiving high-flow nasal oxygen therapy. J Clin Med 10(15):3404
Zang X, Wang Q, Zhou H, COVID-19 Early Prone Position Study Group et al (2020) Efficacy of early prone position for COVID-19 patients with severe hypoxia: a single-center prospective cohort study. Intensive Care Med 46(10):1927–1929
Gattinoni L, Busana M, Giosa L et al (2019) Prone positioning in acute respiratory distress syndrome. Semin Respir Crit Care Med 40(1):94–100
Guérin C, Reignier J, Richard JC, PROSEVA Study Group et al (2013) Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 368(23):2159–2168
Beigel JH, Tomashek KM, Dodd LE, Study Group Members et al (2020) Remdesivir for the treatment of covid-19—final report. N Engl J Med 383(19):1813–1826
Horby P, Lim WS, Emberson JR et al (2021) Dexamethasone in hospitalized patients with covid-19. N Engl J Med 384(8):693–704
Petrone P, Brathwaite CEM, Joseph DK (2021) Prone ventilation as treatment of acute respiratory distress syndrome related to COVID-19. Eur J Trauma Emerg Surg 47(4):1017–1022
Estenssoro E, Loudet CI, Ríos FG, SATI-COVID-19 Study Group et al (2021) Clinical characteristics and outcomes of invasively ventilated patients with COVID-19 in Argentina (SATICOVID): a prospective, multicentre cohort study. Lancet Respir Med 9(9):989–998
Sartini C, Tresoldi M, Scarpellini P et al (2020) Respiratory parameters in patients with COVID-19 after using noninvasive ventilation in the prone position outside the intensive care unit. JAMA 323(22):2338–2340
Tan W, Xu DY, Xu MJ et al (2021) The efficacy and tolerance of prone positioning in non-intubation patients with acute hypoxemic respiratory failure and ARDS: a meta-analysis. Ther Adv Respir Dis 15:17534666211009408
Le Terrier C, Suh N, Wozniak H et al (2022) Delayed intubation is associated with mortality in patients with severe COVID-19: a single-centre observational study in Switzerland. Anaesth Crit Care Pain Med 41(4):101092
Funding
Open access funding provided by Università degli Studi di Perugia within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
CB is the guarantor. CB made a substantial contribution to the conception and design of the study, the acquisition of data, the analysis and interpretation of data, and to drafting of the article. MG made a substantial contribution to the conception and design of the study, the acquisition of data, the analysis and interpretation of data, and to drafting of the article. AGR, DB, LT, LL, RR, FB, and CC made a substantial contribution to the acquisition of data.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not applicable.
Human and animal rights
There are no human and animal rights issues to declare since this study did not involve any human or animal.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Graziani, M., Rigutini, A.G., Bartolini, D. et al. Awake prone positioning for patients with COVID-19-related respiratory failure: a systematic review and meta-analysis. Intern Emerg Med 19, 147–158 (2024). https://doi.org/10.1007/s11739-023-03434-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-023-03434-1