Abstract
Background
Immersive Virtual Reality (IVR) has shown promise in the assessment, understanding, and treatment of eating disorders (EDs), providing a dynamic platform for clinical innovation. This scoping review aims to synthesize the recent advancements and applications of IVR in addressing these complex psychological disorders.
Methods
This review followed the Preferred Reporting Items for Systematic Reviews and Meta-analysis Protocols, focusing on studies published in the past five years. It included peer-reviewed papers that used IVR for ED assessment, examination, or treatment. A comprehensive database search provided a selection of relevant articles, which were then methodically screened and analyzed.
Results
Twenty studies met the inclusion criteria, with a primary focus on Anorexia Nervosa (AN), Bulimia Nervosa (BN), and Binge Eating Disorder (BED). The application of IVR was categorized into three areas: assessment, understanding, and treatment. IVR was found to be an effective tool in assessing body image distortions and emotional responses to food, providing insights that are less accessible through traditional methods. Furthermore, IVR offers innovative treatment approaches by facilitating exposure therapy, modifying body-related biases, and enabling emotional regulation through embodied experiences. The studies demonstrate IVR’s potential to improve body image accuracy, reduce food-related anxieties, and support behavioral changes in ED patients.
Conclusion
IVR stands out as a transformative technology in the field of EDs, offering comprehensive benefits across diagnostic, therapeutic, and experiential domains. The IVR’s ability to simulate the brain’s predictive coding mechanisms provides a powerful avenue for delivering embodied, experiential interventions that can help recalibrate distorted body representations and dysfunctional affective predictive models implicated in EDs. Future research should continue to refine these applications, ensuring consistent methodologies and wider clinical trials to fully harness IVR’s potential in clinical settings.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Eating disorders (EDs) are complex psychopathological conditions characterized by abnormal eating habits and a distorted body image (BI), significantly affecting individuals’ physical health and psychosocial well-being. EDs include a broad spectrum of conditions, of which Anorexia Nervosa (AN), Bulimia Nervosa (BN) and Binge Eating Disorder (BED) are the primary types. AN is classified into two primary subtypes: the restrictive subtype, where individuals achieve extreme body weight through dieting, fasting, or excessive exercise; and the purging subtype, characterized by an unhealthy low body weight with episodes of binge eating followed by compensatory behaviors such as vomiting or the use of laxatives to prevent weight gain. BN is distinguished by recurrent episodes of binge eating accompanied by compensatory behaviors to counteract the effects of overeating and weight gain. In contrast, BED involves repeated episodes of binge eating without subsequent compensatory actions [1].
In Western countries, a substantial proportion of young women and men, up to 17.9%, meet the diagnostic criteria for an ED in early adulthood [2], and the number of diagnoses is dramatically increasing after Covid-19 [3]. What underscores these conditions as a mental health emergency is the increasing prevalence combined with the limited effectiveness of available prevention, assessment, and treatment procedures. This is partially linked to multifaceted factors that contributes to EDs etiology and maintenance.
EDs manifest primarily across two dimensions: behavioral and experiential. The behavioral domain encompasses the actions undertaken by individuals to exert control over their bodies, including, food elimination, food restriction, and episodes of binge eating. These behaviors are the visible manifestations of the disorder, observable and quantifiable. However, the complexity of EDs also reaches the experiential domain, namely the internal, subjective experiences of individuals with EDs. Specifically, the experiential domain includes the emotional, perceptual, and cognitive aspects that shape individuals’ relationships with food and their bodies, which in turn influence overall daily functioning.
On one side, EDs are characterized by profound food-related dysfunctional emotional reactions [4]. The fear of gaining weight, the anxiety or disgust triggered by certain foods in certain situations, and the guilt following eating are emblematic of the disordered relationship with food that characterizes EDs. This complex emotional experience significantly impacts the individual’s ability to maintain a healthy eating behavior, often leading to avoidance, restriction, compensatory or uncontrolled behaviors that further exacerbate the disorder.
On the other side, a critical and pervasive issue is BI distortion [5, 6], where individuals inaccurately perceive their bodies as larger or more flawed than reality and deeply link their self-esteem and self-worth to distorted BI. This distortion is deeply linked to a significant difficulty in developing a stable sense of self, exacerbated by a lack of coherent, first-person experience of their body [7]. Individuals with EDs often struggle to feel a direct, personal connection to their bodily sensations and emotions. Instead, they adopt an external, object-centered perspective (self-objectified) influenced by societal ideals and past observations [8].
Intriguingly, two separate longitudinal studies conducted over four years, each involving upwards of 2000 participants [9, 10] revealed that self-objectification held a significantly higher predictive value for both the remission and emergence of EDs when compared to other widely acknowledged factors - body dissatisfaction, thin-ideal internalization, negative affectivity and lower self-esteem - that demonstrated significant less predictive power. This suggests a potentially essential role for self-objectification in the progression and mitigation of EDs, meriting further investigation within the field.
Recently, the Allocentric Lock Hypothesis (ALH) proposed that EDs may arise from difficulties in multisensory body integration [11]. This integration process involves combining internal bodily signals (e.g. hunger, proprioception) with external sensory information (e.g. vision, touch) and autobiographical memories (e.g., remembering past experiences related to body image or eating, such as recalling past comments about one’s appearance or feeling shame during social eating situations) to form a coherent representation of one’s physical self [12].
According to predictive coding theories, the brain continuously generates and updates an internal model of the body and surroundings, allowing it to predict and integrate diverse sensory inputs through embodied simulations [13]. The ALH proposes that in EDs, there is a disruption in these predictive mechanisms underlying multisensory integration [11]. As a result, individuals with EDs become locked into an observer-based (allocentric) embodied simulation of their body [14, 15]. Negative experiences like teasing, objectification through social media exposure, or distorted autobiographical memories originally shape the allocentric perspective. This outdated model remains rigid, failing to update accurately despite contradictory information from current sensory inputs about the individual’s actual bodily state. This persistent allocentric representation can cause ongoing BI disturbances, leading to persistent dissatisfaction and shame. These experiences trigger anxiety and drive maladaptive behaviors aimed at controlling perceived bodily flaws based on memory rather than true corporeal reality.
In this context, a key advantage of Immersive Virtual Reality (IVR) for EDs is that it can simulate virtual bodies and the worlds around them that dynamically adjust to the user’s actions, providing predicted multisensory feedback just as the brain generates and updates internal body models to anticipate sensory inputs [16]. This is particularly supported by advanced IVR technologies, such as head-mounted displays (HMDs), that enable real-time interaction with the virtual world through motion tracking, hand controllers, and sensory feedback devices.This alignment makes IVR an unprecedented “playground” to directly apply principles of predictive coding.
Through carefully constructed virtual environments, it is possible a controlled delivery of challenging multimodal experiences (e.g., exposure to high-calorie food) that induce modest prediction errors in a safe, immersive manner [17]. For example, IVR can recreate triggering situations, such as mealtimes, in personalized environments, placing patients in a range of contexts from kitchens to restaurants, whether alone or with others, and presenting various types of food [18]. These environments have the potential to elicit patients’ authentic emotional reactions that allow clinicians to understand deeper the patient’s emotional difficulties and to work with them on managing the emotional responses.
Moreover, IVR allows the embodiment in bodies different from the actual one (e.g., full body illusions) providing disconfirming multisensory feedback, that create opportunities to update the internal body models of the user iteratively [19]. For example, by embodying virtual avatars that closely mirrors or subtly adjusts their physical form, users can experience a different perspective on their body size, shape, or appearance [20]. This “re-training” of the predictive mechanisms can foster more accurate modeling of reality with reduced predictive biases that contribute to ED psychopathology [21].
Initial review works have focused on outlining and summarizing the application of IVR in EDs [18, 22, 23], and preliminary studies suggest its efficacy in addressing core EDs symptoms [16]. These data suggest that IVR could be a supportive tool for clinical practice, as it can offer an alternative or an addition to available assessment and intervention approaches.
Rationale
This scoping review aims to explore the current use of IVR technology across various aspects of eating disorders (EDs). This work moves beyond previous theoretical works, that either provided a general description of the techniques [23], or focused on specific techniques [20], specific EDs [18] or specific outcomes [24], aiming at providing a more updated and comprehensive representation of the field [22].
Specifically, it offers a detailed analysis of novel IVR methods in EDs assessment, understanding and treatment, evaluating their effectiveness across various disorders. Furthermore, it not only evaluates the effectiveness of IVR in key aspects of EDs, including body image distortion and food-related anxiety, but also discusses its integration with established treatments.
Methods
Protocol
The protocol of this scoping review was crafted following the Preferred Reporting Items for Scoping Reviews (PRISMA-ScR). By adopting this methodology, we aimed to provide an extensive analysis of the developments in IVR for EDs over the past five years, focusing on the range still not covered by other theoretical works [18, 22, 23].
Eligibility Criteria
Data extraction was performed on March 30th, 2024. Peer-reviewed journal papers were included if they were published from January 1st, 2019, up to the extraction date, written in English, involved human participants, and described a measure for ED treatment or assessment using IVR. Both experimental and quasi-experimental studies were selected, including randomized controlled trials and pre-post design studies. Papers were excluded if they did not fit into the conceptual framework of the study or if they did not present empirical data (e.g., background articles). Papers focusing on non-immersive virtual reality were also excluded to maintain the focus on immersive VR experiences specifically.
Information Sources
To identify potentially relevant documents, the following bibliographic databases were searched: Scopus, Web of Science, PsychInfo, Pubmed. The search strategies were drafted by A.F.D.N. and further refined through team discussion. The final search results were exported directly into Rayyan, and duplicates were removed by A.F.D.N.
Search
The following string was used for the search: (“virtual reality” OR vr) AND (“eating disorder*” OR bulimia OR “binge eating” OR anorexia) and adapted for each database. Notably, the term “immersive” was intentionally omitted in favor of the broader term “VR” to avoid prematurely excluding relevant studies. This approach acknowledges that some research may refer to VR in a way that implicitly includes IVR, despite not combining the term “immersive” and “virtual reality” one after the other. The aim was to encompass a wider range of studies, subsequently refining the selection to focus on immersive experiences as needed, based on the context provided within individual papers. The final string for each database can be found in “Supplementary Materials”.
Selection of Sources of Evidence
We performed a two-step screening of all the references generated by the search strategy. In step 1, two authors (A.F.D.N. and S.F.M.P.) independently screened the titles and abstracts to exclude any irrelevant references that did not meet eligibility criteria. Conflicts were resolved through discussion. In step 2, two authors (A.F.D.N., S.F.M.P.) independently screened the full texts of the references selected in Step 1 against the eligibility criteria. To minimize bias during the selection process, the screening was blind, using the option “blind status on’’ in Rayyan. Once all authors have completed the selection process, the blinding status was turned off, and any disagreement was resolved through consensus.
Data Charting
The team developed a data-charting form to decide on the variables for extraction. Two authors (A.F.D.N., S.F.M.P.) independently gathered the data, then discussed their findings with the rest of the team, refining the charting form through an iterative process to ensure comprehensive data collection and analysis.
Synthesis of Results
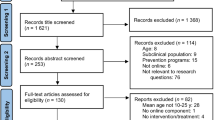
A total of 423 papers were found. Two-hundred and nine were removed as duplicates and 147 were removed after screening Step 1 (titles and abstracts). A total of 67 were sought for retrieval and 3 were not found. As a result, a total of 64 full texts were screened for eligibility. After full text screening a total of 20 articles met the inclusion criteria and were included in our scoping review. The flowchart of paper selection is shown in Fig. 1.
Sixteen papers included participants with AN, 2 studies included patients affected by BED and only 1 study considered individuals with solely BN and 1 with BN and BED. Table 1 summarizes the sociodemographic information of the population of the included studies.
Overall, the included articles comprise a total sample of 661 participants, (479 with AN, 75 with BN, or BED, and 107 healthy controls), aged 14 to 65. The female gender was the most represented (638 females, 10 males, 3 non binary or others). Most of the studies were conducted in Europe (Spain, Italy, Germany, and French), two were carried out in the United States, and one in the United Kingdom.
To systematize results and better understand the impact of new IVR approaches in EDs treatment, we pooled the results according to three mutually exclusive categories: (1) studies where IVR is used as a diagnostic or assessment tool to identify patients and/or assess their symptoms (assessment), (2) Studies where IVR is used to better analyze certain aspects or processes which characterize people with EDS that might shape IVR treatment efficacy for EDs (understanding), and (3) studies aimed at testing the efficacy of IVR treatment on ED symptoms (treatment). Although some papers could fall into multiple categories, such as understanding and treatment [25] or assessment and treatment [26], we have placed each of them in the most representative category, based on the main aim of the study. An overview of the included studies is available in Table 2 and an overview of the IVR technology and procedure used is detailed in Table 3.
Assessment
All studies included in this category explored how IVR can be employed to assess specific characteristics of AN. Four studies, among those identified, fell into this category. Specifically, three studies used body-swapping procedure and avatars to assess perceptual and affective BI disturbance [21, 26, 27], while one study used virtual food exposure (VR-FE) to evaluate emotional reactions to food related stimuli [28].
Fisher and colleagues [27] assessed BI (i.e., body distortions and body dissatisfaction) in AN patients with avatars or paper-based rating scales. The authors asked patients to select the Fig. (3D avatar vs. 2D image) that better fitted their real and ideal body shape, finding that the virtual avatar that patients selected corresponded closely to the silhouette they chose on a paper-based rating scale, thus yielding comparable self-rating results.
Provenzano and colleagues [26] used IVR to assess and measure the perceptual and cognitive-emotional components of BI disturbance in patients with AN. Through the creation of personalized avatars that vary in size, participants’ perceptions of their body size and shape were assessed. This allowed for a detailed assessment of how patients perceived their own body size (real body) versus how it actually appeared (ideal body), which is crucial for understanding the perceptual components of BI distortion in patients with AN. Although primarily designed as an assessment tool, the study also observed the influence of inducing a body ownership illusion on body dissatisfaction and perceptual distortions among patients with AN. Specifically, the authors observed that patients expressed more negative emotions after being embodied in the fattest avatar, especially in patients with more severe symptoms. This finding suggests that IVR can not only assess BI disturbances but also potentially influence them, indicating a dual role for IVR in both evaluating and addressing BI issues in therapeutic setting.
Similarly, Matamala-Gomez and colleagues [21] explored the use of IVR to modulate BI disturbances through a pilot study focusing on user experience. In their study, patients with AN were embodied in virtual avatars reflecting their perceived body size, and high levels of embodiment were reported. The results emphasized that immersive experiences with a high degree of body ownership can significantly affect how patients perceive their bodies, highlighting IVR’s potential to assess BI distortions in therapeutic settings.
As concerns VR-FE, Bektas and colleagues [28] used IVR to measure and assess food disgust in AN patients. The authors presented patients with a virtual kitchen, with or without other avatars. Results revealed a correlation between food disgust and patients’ symptoms severity, regardless of the presence of avatars in the virtual scenario, showing the clinical potential of IVR for in-depth exploration of food disgust in patients with AN.
Understanding
Four studies focused on examining cognitive and emotional processes and variables relevant to the treatment of EDs in IVR. Two studies assessed cognitive processes related to BI in samples of individuals with AN [29, 30], while two explored the impact of interacting with foods during VR-FE in BED [31] or food avoidance in AN patients [32]. Ferrer-Garcia and colleagues [29] investigated body-selective visual attention bias and how it influenced clinical outcomes in patients with AN undergoing VR body exposure therapy (VR-BE). They observed that higher pre-intervention body-related attentional bias predicted less favorable clinical outcomes. Di Lernia and colleagues [30] used VR-induced body illusions to deepen the link between interoception and body distortions in patients with AN. Participants with AN exhibited greater interoceptive metacognition compared to healthy participants. The authors concluded that the presence of a strong interoceptive metacognition might impair the possibility of revising bodily distorted expectations with real-time multisensory bottom-up bodily information during IVR treatment. Max and colleagues [31] studied the presence of dysfunctional interaction patterns in the interaction with virtual foods in BED, revealing pathology-specific patterns in manual interaction with food (i.e., slower picking up of food items compared to non-food items), even though no significant link between interactions and behaviors or BED features emerged. Finally, [32] Schroeder and colleagues studied the phenomenon of food avoidance among individuals diagnosed with AN-restrictive type, compared with healthy controls, by employing a IVR stopping task. Results showed that AN patients had both persistent food avoidance tendencies and increased inhibitory control. Indeed, individuals with AN-R consistently displayed patterns of avoiding food, alongside an enhanced ability to exert inhibitory control over their eating behaviors compared to healthy participants.
Treatment
Twelve of the included studies aimed to investigate the effectiveness of VR in treating EDs. They used VR-BE or body swapping (VR-BS) [25, 33,34,35,36,37], food exposure [38, 39], attentional bias training [40], or CBT combined with IVR [41] or psychological rescripting approaches combined with VR-BS to modify emotions and cognition [42].
Four studies utilized body exposure approaches with patients with AN. In a single case study on a patient with AN, Porras-Garcia and others [35, 37] observed that seeing one’s body from an external (observer) perspective diminished negative beliefs associated with the “self” and enhance body acceptance. They also noted that VR-BE therapy facilitated an increase in BMI reaching healthy levels and reduced fear of gaining weight (FGW); moreover decrease in body-related anxiety, drive for thinness, and BI disturbances were maintained after 5 months. A subsequent RCT with the same approach [43] revealed that patients with AN in the VR-BE group exhibited significant reductions in FGW and BI disturbances compared to the control. The exposure to healthy-weight virtual bodies was confirmed to elicit body concerns and treat and diminish FGW in the study by Behrens and colleagues [33], suggesting that VR-BE could be an effective technique in AN treatment. Three studies focused on VR-BS approach in AN. VR-BS sessions, integrated into a multidisciplinary AN treatment, influenced a patient’s body perception and multisensory body integration in Serino and colleagues [25], while the combination of autobiographical recall techniques and VR-BS was pilot-tested by Malighetti and colleagues [34], showing reductions in negative emotions and body shame, improvements in body satisfaction, and accuracy of body perception after VR sessions. Furthermore, the with a virtual avatar matching one’s BMI proved to be a useful intervention tool, as it resulted in a reduction of fear of weight gain, body anxiety, and attentional bias towards weight-related body parts in patients with AN compared to healthy controls, according to Porras-Garcia and colleagues [36].
Concerning VR-FE studies, a good feasibility and acceptability in treating BED with IVR cue exposure therapy in clinical settings emerged, with promising preliminary results in reducing binge episodes in the short-term and loss of benefits at follow-up [38]. While concerning AN patients, Natali and colleagues [39] (REF) investigated whether positive mood induction or social support can amplify the effect of VR-FE on food-related anxiety. Results showed that participants in the positive mood condition experienced lower levels of anxiety compared to baseline. Specifically, they reported reduced virtual food-related anxiety after exposure, with a medium effect size.
Concerning eye-movements and attentional aspects, two studies proved the effectiveness of IVR-based attention modification training with eye-tracking to reduce body-related attention bias and levels of body dissatisfaction in adolescents with AN [40].
Finally, the positive effect of combining traditional psychological treatments with IVR for BN and BED patients emerged in two papers. Specifically, CBT treatments and IVR for BN patients resulted in a more consistent BMI over time compared to the standard treatment, where BMI fluctuated significantly, and reduced preoccupation with weight, fear of weight gain, and instances of binge eating and purging [41], while combining VR-BS with the reshaping of emotional experience in immersive environments led to an improvement in emotion regulation and binge episodes [42]. These findings suggest that these interventions may enhance therapeutic outcomes and contribute to overall patient well-being.
Discussion
The present scoping review aimed to investigate the use of IVR in addressing the complex nature of EDs. IVR tools resulted useful to target particularly the emotional, perceptual and cognitive aspects characterizing the experiential domain of EDs symptoms. Within the papers included in the review, three categories of IVR utilization were identified (assessment, understanding, and treatment).
Concerning IVR as an assessment tool, studies revealed that immersive experience can efficiently assess both perceptual and cognitive-emotional BI components [26,27,28, 44]. This aligns with previous research [30, 45], suggesting that IVR can provide ecological, reliable, and engaging assessment tools [46]. The latter aspect is critical in disorders such as AN, in which building therapeutic alliances and having genuine responses is often complicated [47]. Thus, technology offers advantages for both the clinician (i.e., accurate measurements less subject to bias) and the patient (i.e., active participation, engagement). Furthermore, following the trend of personalized medicine, IVR allows the development of tools tailored to patients’ needs, such as exposure to customized bodies [26] or specific foods [48].
As regards the understanding of the complex processes and features that characterize the psychopathology of EDs, the multisensory capabilities of IVR have emerged as a promising tool for enhancing our understanding of both inner and outer body perceptions [49]. In particular, the present scoping review confirmed the potential of eye-tracking integrated IVR tools in understanding attentional biases in EDs, which already emerged in a previous systematic review [20, 22].
The use of IVR as a treatment tool aligns with previous systematic reviews [22, 23, 50]. IVR has indeed demonstrated considerable promise in modifying the maladaptive behaviors characteristic of EDs. The studies included in this review consistently highlight IVR’s efficacy in creating realistic, controlled environments that facilitate BI retraining, exposure therapy, and cognitive restructuring within a clinical setting. IVR environments can indeed trigger genuine physiological and psychological responses like those experienced in real-world situations, providing a powerful platform confronting fears and practicing coping strategies [48]. Going a step further, we tried to understand why IVR might be so impactful by thinking about IVR features.
First, by experiencing VR-BS and VR-BE with avatars that represent either their actual or healthier BMI, patients are exposed to new perspectives on their BI. This exposure is crucial as it helps recalibrate the brain’s internal models of the body by providing real-time, accurate body-related sensory feedback, encouraging the brain to update these internal predictions, often reliant on distorted body internal representation [6]. In particular, IVR allows users to ‘change’ their bodies in unexpected ways, leading to discrepancies between expected and actual sensory feedback (prediction errors). These prediction errors can prompt significant updates in the brain’s internal body model51 , which may result in a more accurate body perception and healthier body interactions. This process can be further supported and enhanced by integrating autobiographical rescripting techniques, which help reshape personal experiences and improve emotion regulation in patients [34].
Second, the use of IVR in food exposure therapy has been particularly effective. By simulating environments that trigger disordered eating behaviors, such as settings that involve food interaction, IVR allows patients to navigate their anxieties in a safe and controlled manner. This method has been beneficial for patients with both AN and BED helping them to manage their fear of eating and reduce binge-eating episodes, respectively. Considering the efficacy of food exposure in IVR and the foundational role of prediction error in the treatment of EDs, as demonstrated in studies involving body illusions, future research might explore integrating food exposure with the deliberate creation of prediction errors. For example, combining food exposure with the predictive coding framework could involve altering expected sensory characteristics of foods within VR environments. This approach has the potential to induce unexpected discrepancies between anticipated and actual sensory feedback.
Considering both bodies focused approaches (VR-BS and VR-BE) and food exposure (VR-FE), IVR is distinguished as a deeply experiential and embodied technology. It enables direct modifications of perceptions, emotions, beliefs, and memories, bypassing the need for patients to consciously recall these elements or rely on metacognitive skills, which are often impaired in individuals with EDs.
In conclusion, this scoping review highlights the potential of IVR as a complementary tool in clinical practice in addressing the experiential domain that characterizes EDs. In this respect, it is crucial to emphasize that IVR should be viewed as an adjunctive resource rather than a standalone treatment. The primary benefit of IVR lies in its ability to offer a multisensory, embodied, and cognitive experience. This rich, immersive experience can significantly influence the brain’s predictive mechanisms related to body perception and emotional responses to key stimuli. However, it should be used judiciously and in conjunction with established therapeutic interventions to ensure a holistic and effective assessment and treatment approach for those suffering from EDs.
Limitations
It is important to interpret the reported results considering some limitations. Firstly, there are few randomized controlled trials among the included studies. Additionally, many studies have small sample sizes, limiting statistical power and potentially introducing bias. Furthermore, the lack of standardized treatment protocols or consistent follow-up assessments across studies impacts the possibility to conclude on interventions efficacy. Moreover, male participants are underrepresented in these studies, which may influence the applicability of the findings to this population. Further research with larger and more diverse samples, as well as the implementation of standardized protocols, is needed to enhance the reliability and validity of IVR applications to EDs.
Furthermore, while the integration of IVR into clinical protocols for EDs holds great promise, it is necessary to consider potential side effects to ensure safe and effective implementation. Firstly cybersickness, a form of motion sickness originating from the sensory mismatch between visual input and physical movement, can be an issue for some patients, potentially exacerbating discomfort and hindering treatment progress. However, the current implementations of food exposure and body swap in IVR do not involve movement; patients remain stationary, which significantly limits the occurrence of cybersickness. Also, with the technical advances in IVR tools and the development of more sophisticated devices, this risk should be minimal, but is important for clinical centers to consider using devices that minimize this risk. Secondly, the realism of VR content, while creating authentic experiences, might induce stress or anxiety in patients, particularly during exposure to food-related stimuli. Tailoring treatments to individual patient needs or establishing a hierarchy of stimuli, as in the case of food exposure, can help mitigate these adverse effects. Implementing a hierarchy of stimuli and adjusting it based on the patient’s responses can help reduce anxiety and ensure a more comfortable and effective therapeutic experience. Lastly, the successful application of IVR in ED treatment necessitates specific training for healthcare professionals. Clinicians may lack the necessary expertise to effectively use this technology, highlighting the importance of comprehensive training programs. These programs should cover various aspects, including the technical operation of IVR equipment, understanding the therapeutic protocols, and being able to troubleshoot common issues. Additionally, training should emphasize strategies for managing possible side effects, such as cybersickness or anxiety induced by realistic VR content. By equipping clinicians with this practical knowledge, we can prevent misuse, optimize patient outcomes and make clinicians confident in using technological tools and managing possible side effects.
Conclusion
In summary, the IVR’s ability to simulate embodied experiences that align with the brain’s predictive coding mechanisms provides a powerful avenue for delivering immersive, experiential interventions that can help recalibrate distorted body representations and affective predictive models implicated in eating disorders. This innovative approach holds significant potential for more effective and engaging treatments, particularly through their ability to immerse patients in experiences that directly address and integrate the experiential domain into comprehensive treatment plans. By offering innovative ways to confront and alter distorted BI and food-related negative reactions, IVR technology holds the potential to significantly impact the landscape of ED treatment, making it a valuable tool in the quest for more effective therapeutic interventions.
Data Availability
No datasets were generated or analysed during the current study.
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5 (Vol. 5, No. 5). Wash DC Am Psychiatr Assoc; 2013.
Silén Y, Keski-Rahkonen A. Worldwide prevalence of DSM-5 eating disorders among young people. Curr Opin Psychiatry. 2022;35(6):362–71.
McLean CP, Utpala R, Sharp G. The impacts of COVID-19 on eating disorders and disordered eating: a mixed studies systematic review and implications. Front Psychol. 2022;13:926709.
Esposito R, Cieri F, di Giannantonio M, Tartaro A. The role of body image and self-perception in anorexia nervosa: the neuroimaging perspective. J Neuropsychol. 2018;12(1):41–52.
Dakanalis A, Gaudio S, Serino S, Clerici M, Carrà G, Riva G. Body-image distortion in anorexia nervosa. Nat Rev Dis Primer. 2016;2(1):1–2.
Brizzi G, Sansoni M, Di Lernia D, Frisone F, Tuena C, Riva G. The multisensory mind: a systematic review of multisensory integration processing in Anorexia and Bulimia Nervosa. J Eat Disord. 2023;11(1):204.
Mancini M, Esposito CM. Lived body and the other’s gaze: a phenomenological perspective on feeding and eating disorders. Eat Weight Disord-Stud Anorex Bulim Obes. 2021;26(8):2523–9.
Calogero RM. Objectification theory, self-objectification, and body image. 2012.
Dakanalis A, Pla-Sanjuanelo J, Caslini M, Volpato C, Riva G, Clerici M, et al. Predicting onset and maintenance of men’s eating disorders. Int J Clin Health Psychol. 2016;16(3):247–55.
Dakanalis A, Clerici M, Bartoli F, Caslini M, Crocamo C, Riva G, et al. Risk and maintenance factors for young women’s DSM-5 eating disorders. Arch Womens Ment Health. 2017;20:721–31.
Riva G, Dakanalis A. Altered Processing and Integration of multisensory bodily representations and signals in eating disorders: a possible path toward the understanding of their underlying causes. Front Hum Neurosci. 2018;12:49.
Repetto C, Riva G. The neuroscience of body memory: recent findings and conceptual advances. EXCLI J. 2023;22:191.
Talsma D. Predictive coding and multisensory integration: an attentional account of the multisensory mind. Front Integr Neurosci. 2015;9:19.
Riva G. Neuroscience and eating disorders: the allocentric lock hypothesis. Med Hypotheses. 2012;78(2):254–7.
Riva G, Gaudio S. Locked to a wrong body: eating disorders as the outcome of a primary disturbance in multisensory body integration. Conscious Cogn. 2018;59:57–9.
Riva G, Wiederhold BK, Mantovani F. Neuroscience of virtual reality: from virtual exposure to embodied medicine. Cyberpsychology Behav Soc Netw. 2019;22(1):82–96.
Cerasa A, Gaggioli A, Pioggia G, Riva G. Metaverse in Mental Health: the beginning of a long history. Curr Psychiatry Rep. 2024;1–10.
de Carvalho MR, Dias TR, de Duchesne S, Nardi M, Appolinario AE. JC. Virtual reality as a Promising Strategy in the Assessment and Treatment of Bulimia Nervosa and binge eating disorder: a systematic review. Behav Sci Basel Switz. 2017;7(3).
Mottelson A, Muresan A, Hornbæk K, Makransky G. A systematic review and meta-analysis of the effectiveness of body ownership illusions in virtual reality. ACM Trans Comput-Hum Interact. 2023;30(5):1–42.
Riva G, Malighetti C, Serino S. Virtual reality in the treatment of eating disorders. Clin Psychol Psychother. 2021;28(3):477–88.
Matamala-Gomez M, Maselli A, Malighetti C, Realdon O, Mantovani F, Riva G. Virtual Body Ownership Illusions for Mental Health: a narrative review. J Clin Med. 2021;10(1).
Clus D, Larsen ME, Lemey C, Berrouiguet S. The use of virtual reality in patients with eating disorders: systematic review. J Med Internet Res. 2018;20(4):e157.
Ciążyńska J, Maciaszek J. Various types of virtual reality-based therapy for eating disorders: a systematic review. J Clin Med. 2022;11(17).
Ferrer-García M, Gutiérrez-Maldonado J. The use of virtual reality in the study, assessment, and treatment of body image in eating disorders and nonclinical samples: a review of the literature. Body Image. 2012;9(1):1–11.
Serino S, Polli N, Riva G. From avatars to body swapping: the use of virtual reality for assessing and treating body-size distortion in individuals with anorexia. J Clin Psychol. 2019;75(2):313–22.
Provenzano L, Porciello G, Ciccarone S, Lenggenhager B, Tieri G, Marucci M et al. Characterizing body image distortion and bodily self-plasticity in Anorexia Nervosa via Visuo-Tactile Stimulation in virtual reality. J Clin Med. 2019;9(1).
Fisher S, Abdullah A, Charvin I, Da Fonseca D, Bat-Pitault F. Comparison of body image evaluation by virtual reality and paper-based figure rating scales in adolescents with anorexia nervosa: retrospective study. Eat Weight Disord EWD. 2020;25(3):735–43.
Bektas S, Natali L, Rowlands K, Valmaggia L, Di Pietro J, Mutwalli H et al. Exploring correlations of Food-Specific Disgust with Eating Disorder psychopathology and Food Interaction: a preliminary Study using virtual reality. Nutrients. 2023;15(20).
Ferrer-Garcia M, Porras-Garcia B, Miquel H, Serrano-Troncoso E, Carulla-Roig M, Gutiérrez J. The way we look at our own body really matters! Body-related attentional bias as a predictor of worse clinical outcomes after a virtual reality body exposure therapy. Annu Rev Cybertherapy Telemed. 2021;19:99.
Di Lernia D, Serino S, Tuena C, Cacciatore C, Polli N, Riva G. Mental health meets computational neuroscience: a predictive bayesian account of the relationship between interoception and multisensory bodily illusions in anorexia nervosa. Int J Clin Health Psychol. 2023;23(4):100383.
Max SM, Schag K, Giel KE, Plewnia C. Behavioural biases in the interaction with food objects in virtual reality and its clinical implication for binge eating disorder. Eat Weight Disord EWD. 2023;28(1):46.
Schroeder PA, Collantoni E, Meregalli V, Rabarbari E, Simonazzi C, Svaldi J et al. Persistent avoidance of virtual food in anorexia nervosa-restrictive type: results from motion tracking in a virtual stopping task. Int J Eat Disord. 2024.
Behrens SC, Tesch J, Sun PJB, Starke S, Black MJ, Schneider H, et al. Virtual reality exposure to a healthy weight body is a Promising Adjunct Treatment for Anorexia Nervosa. Psychother Psychosom. 2023;92(3):170–9.
Malighetti C, Chirico A, Serino S, Cavedoni S, Matamala-Gomez M, Stramba-Badiale C et al. Manipulating body size distortions and negative body-related memories in patients with Anorexia Nervosa: a virtual reality-based pilot study. Annu Rev CyberTherapy Telemed. 2020.
Porras-Garcia B, Serrano-Troncoso E, Carulla-Roig M, Soto-Usera P, Ferrer-Garcia M, Figueras-Puigderrajols N, et al. Virtual reality body exposure therapy for Anorexia Nervosa. A Case Report with Follow-Up results. Front Psychol. 2020;11:956.
Porras-Garcia B, Ferrer-Garcia M, Serrano-Troncoso E, Carulla-Roig M, Soto-Usera P, Miquel-Nabau H et al. Validity of virtual reality body exposure to elicit fear of gaining weight, body anxiety and body-related attentional Bias in patients with Anorexia Nervosa. J Clin Med. 2020;9(10).
Porras-Garcia B, Ferrer-García M, Serrano-Troncoso E, Carulla-Roig M, Soto-Usera P, Fernández-Del Castillo Olivares L, et al. Virtual reality body exposure therapy for anorexia nervosa. A single case study. In Springer; 2020. pp. 108–15.
Nameth K, Brown T, Bullock K, Adler S, Riva G, Safer D et al. Translating virtual reality cue exposure therapy for binge eating into a Real-World setting: an uncontrolled pilot study. J Clin Med. 2021;10(7).
Natali L, Meregalli V, Rowlands K, Di Pietro J, Treasure J, Collantoni E et al. Virtual food exposure with positive mood induction or social support to reduce food anxiety in anorexia nervosa: a feasibility study. Int J Eat Disord. 2024.
Ascione M, Carulla-Roig M, Miquel-Nabau H, Porras-Garcia B, Meschberger-Annweiler FA, Serrano-Troncoso E et al. Attentional Bias Modification Training based on virtual reality and Eye Tracking in Anorexia Nervosa patients. J Clin Med. 2023;12(18).
Sansoni M, Varallo G, Malighetti C, Tuena C, Di Lernia D, Cesa GL, et al. Unlocking the potential of virtual reality to expand treatment frontiers for bulimia nervosa: a pilot study to explore the impact of virtual reality-enhanced cognitive-behavioral therapy. Virtual Real. 2024;28(2):79.
Malighetti C, Schnitzer C, Potter G, Nameth K, Brown T, Vogel E, et al. Rescripting emotional eating with virtual reality: a case study. Annu Rev Cybertherapy Telemed. 2021;19:117–21.
Porras-Garcia B, Ferrer-Garcia M, Serrano-Troncoso E, Carulla-Roig M, Soto-Usera P, Miquel-Nabau H et al. AN-VR-BE. A randomized controlled trial for reducing fear of gaining weight and other Eating disorder symptoms in Anorexia Nervosa through virtual reality-based body exposure. J Clin Med. 2021;10(4).
Matamala-Gomez M, Brivio E, Chirico A, Malighetti C, Realdon O, Serino S, et al. Assessing user experience of a virtual reality training in patients with anorexia nervosa: insigths from a pilot study. Annu Rev CyberTherapy Telemed. 2020;18(A):171–5.
Keizer A, van Elburg A, Helms R, Dijkerman HC. A virtual reality full body illusion improves body image disturbance in Anorexia Nervosa. PLoS ONE. 2016;11(10):e0163921.
Brizzi G, Riva G, Romano D. The body image virtual reality Assessment (BIVRA): measuring the body representation through virtual reality. J Neuropsychol. 2024.
Brizzi G, Boltri M, Castelnuovo G, Riva G. Case Study ME_BS. PsyArXiv [Internet]. 2024; osf.io/preprints/psyarxiv/2gj4e.
Gutiérrez-Maldonado J, Pla-Sanjuanelo J, Ferrer-García M. Cue-exposure software for the treatment of bulimia nervosa and binge eating disorder. Psicothema. 2016;28(4):363–9.
Brizzi G, Sansoni M, Riva G. The BODY-FRIEND project: using new technology to learn about how people with anorexia feel about their bodies. Cyberpsychology Behav Soc Netw. 2023;26(2):141–3.
Butler RM, Heimberg RG. Exposure therapy for eating disorders: a systematic review. Clin Psychol Rev. 2020;78:101851.
Riva G, Serino S, Di Lernia D, Pavone EF, Dakanalis A. Embodied medicine: mens sana in corpore virtuale sano. Front Hum Neurosci. 2017;11:120.
Funding
This work was partially supported by the Italian Ministry of Health—Ricerca Corrente and by the research project “Arcadia VR—Assistenza e Riabilitazione del Comportamento Alimentare tramite Dispositivi basati sull’Intelligenza Artificiale e Realtà Virtuale” (Arcadia VR—Assistance and Rehabilitation of Eating Behaviour through Artificial Intelligence-based Devices and Virtual Reality)—MISE (Prog. N.ro F/310025/01–05/X56), Fondo crescita sostenibile—Accordi per l’Innovazione, a.i. sensi del Decreto Ministeriale del 31 dicembre 2021 e del successivo DD 721 del 18 marzo 2022, N. Pos. 25.
Open access funding provided by Università Cattolica del Sacro Cuore within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
A.F.D.N. - Conceptualization, methodology, protocol development, literature search strategy, screening of articles, data extraction, data synthesis, writing: original draft preparation, writing: review and editing.S.F.M.P. - Conceptualization, methodology, protocol development, literature search strategy, screening of articles, data extraction, data synthesis, writing: original draft preparation, writing: review and editing.G.B. - Protocol development, literature search strategy, screening of articles, data extraction, data synthesis, writing: original draft preparation, writing: review and editing.D.D.L. - Conceptualization, methodology, protocol development, supervision, writing: review and editing.F.F. - Protocol development, literature search strategy, screening of articles, data extraction, data synthesis, writing: original draft preparation.A.G. - Conceptualization, methodology, protocol development, supervision.E.R. - Conceptualization, methodology, protocol development.O.O.- Conceptualization, methodology, protocol development, supervision.C.R. - Conceptualization, methodology, protocol development, supervision, writing: review and editing.C.R.- Conceptualization, methodology, protocol development.E.S. - Conceptualization, methodology, protocol development.D.V. - Conceptualization, methodology, protocol development, supervision, writing: review and editing.G.R. - Conceptualization, methodology, protocol development, supervision, writing: review and editing, project administration.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Di Natale, A.F., Pizzoli, S.F.M., Brizzi, G. et al. Harnessing Immersive Virtual Reality: A Comprehensive Scoping Review of its Applications in Assessing, Understanding, and Treating Eating Disorders. Curr Psychiatry Rep 26, 470–486 (2024). https://doi.org/10.1007/s11920-024-01523-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11920-024-01523-2