Abstract
Immune checkpoint inhibitors (ICIs), including anti-programmed cell death protein 1 and its ligand (PD-1/PD-L1) as well as anti-cytotoxic T lymphocyte-associated protein 4 (CTLA-4), have been widely used for treating solid tumors. Myocarditis is a potentially lethal immune-related adverse events (irAEs) caused by ICIs therapy. The treatment of steroid-refractory myocarditis is challenging. We reported two non-small-cell lung cancer patients with steroid-refractory myocarditis induced by ICI. The symptoms were not resolved after pulse corticosteroid therapy and subsequent treatment including intravenous immunoglobulin and mycophenolate mofetil. Considering the level of serum interleukin (IL)-6 decreased by > 50% and level of serum tumor necrosis factor-α (TNF-α) increased during the course of the disease, infliximab was used. Myocarditis gradually alleviated after infliximab treatment. The cases revealed that specific cytokine inhibitors have promising roles in the treatment of steroid-refractory myocarditis. Infliximab could be considered for patients with low level of IL-6 and elevated level of TNF-α.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Immune checkpoint inhibitors (ICIs) are a class of monoclonal antibodies that interact with the programmed cell death protein 1 and its ligand (PD-1/PD-L1) as well as cytotoxic T lymphocyte-associated protein 4 (CTLA-4) molecular pathways to enhance T cell-mediated antitumor effects [1]. With the application of ICIs over the last decade, immune-related adverse events (irAEs) have increased, such as myocarditis [2,3,4,5,6].
According to the recommendations of the European Society for Medical Oncology (ESMO), American Society of Clinical Oncology (ASCO), Society for Immunotherapy of Cancer (SITC) and National Comprehensive Cancer Network (NCCN), ICIs need to be discontinued in moderate and severe cases [2, 7,8,9]. For moderate cases, 1 to 2 mg/kg prednisone is recommended as first-line therapy [2, 7,8,9]. In patients without an immediate response to intravenous steroids, a pulse-dose of corticosteroid (methylprednisolone 500–1000 mg/day) should be considered [9, 10]. Due to the treatment of steroid, nearly 50% of patients with myocarditis can be improved without use of additional immunosuppressive drugs [11,12,13]. While remaining patients may be diagnosed with steroid-refractory myocarditis after receiving at least 3 days of adequate steroid treatment on the basis of one of the following situations [2, 7, 10, 11, 14]: (1) troponin T does not significantly decrease (decrease < 50% of the peak); (2) atrioventricular block, ventricular arrhythmia, or left ventricular dysfunction still persists; (3) after normal reduction of steroid, cardiac biomarkers or symptoms worsen. Other immunosuppressive drugs, such as mycophenolate mofetil (MMF), intravenous immunoglobulin (IVIG) or specific cytokine inhibitors (infliximab or tocilizumab), are considered for patients who are severe (grade 3 or grade 4) or refractory to steroid [2, 7,8,9, 15,16,17,18,19,20]. In recent cases, specific cytokine inhibitors showed potential effects on irAEs [21]. However, guidance for irAEs management is based on case reports that lacked of cytokine monitoring [7, 21]. Therefore, the personalized anti-cytokine strategies remain unclear.
Here, we report two cases and present a literature review of steroid-refractory myocarditis induced by ICI. The two cases with elevated TNF-α level benefited from infliximab. In this review, we discussed a potential personalized anti-cytokine strategy that considered the levels of the inflammatory cytokines IL-6 and TNF-α. This study complied with the principles of the Declaration of Helsinki and was approved by the Ethics Committee of West China Hospital (No. 2024-197). Written informed consent was obtained from the patients for publication of this case report and any accompanying images. We present this article in accordance with the CARE reporting checklist.
Case Presentation
Case 1
A 62-year-old male (height: 165 cm; weight: 65 kg), with a history of hypertension, diabetes and an allergy to sulfanilamide, was diagnosed with lung squamous cell carcinoma (cT4N2M0, stage IIIB) in June 2020. The patient had been treated with amlodipine besylate (10 mg/day), glimepiride (2 mg/day) and metformin hydrochloride (2000 mg/day) for 5 years and was subsequently treated with pembrolizumab plus carboplatin and paclitaxel without radiotherapy. Two weeks after 2 cycles of ICIs combination treatment, the patient presented to the emergency department with dizziness, bilateral ptosis and eye movement disorders. Physical examination did not reveal lower-extremity swelling or jugular vein distention bilaterally. An initial examination revealed that levels of serum troponin T, creatine kinase-myocardial band and myoglobin were elevated at 442.1 ng/L (reference value: 0–14.0 ng/L), 75.21 ng/mL (reference value < 4.94 ng/mL) and 892.3 ng/mL (reference value: 28.0–72.0 ng/mL), respectively. The level of N-terminal pro-B-type natriuretic peptide (BNP) was normal (40.00 ng/L, reference value: 0–227.00 ng/L). Echocardiography revealed normal left systolic function (ejection fraction, 68%) without wall motion abnormalities. Electrocardiogram and coronary contrasted computed tomography (CT) did not show abnormalities. The patient denied any family history of autoimmune rheumatic diseases. The diagnosis of ICI-induced myocarditis (grade 3) was considered according to recent usage of ICIs. Repetitive nerve stimulation decreased the amplitude by 77%. The acetylcholine receptor (AchR) antibody was positive (1.526 nmol/L), and myositis-myasthenia gravis overlap syndrome was diagnosed.
Consequently, pembrolizumab was discontinued, and the patient was treated with respiratory support, cardiac monitoring and methylprednisolone (80 mg/day) immediately. While aggravated clinical symptoms and increased troponin T level even reached a maximum value of 934.0 ng/L on day 9, the patient was treated with pulse-dose methylprednisolone (500 mg/day) for 7 days (Fig. 1A). Heart failure due to steroid-related fluid retention, pulmonary embolism or infection was excluded after symptoms of dizziness and bilateral ptosis without chest pain, elevated body temperature or lower-extremity swelling were observed. BNP, echocardiography, chest CT and respiratory pathogen panels revealed no significant abnormalities. Owing to the rapid increase in troponin T after the discontinuation of pulse-dose steroids, he was diagnosed with steroid-refractory myocarditis induced by ICI and treated with IVIG (20 g/day) and MMF (1,000 mg/day) for 6 days. On day 23, symptoms persisted and a high troponin T level (561.9 ng/L) was maintained. Laboratory examination revealed an elevated TNF-α level (40.9 pg/ml, reference value < 8.1 pg/ml) and decreased IL-6 level (< 1.5 pg/ml, baseline level: 4.74 pg/ml, reference value: 0-7 pg/ml), and infliximab (at a dose of 200 mg per 2 weeks) was administered (Fig. 1B). Symptoms of ptosis and eye movement disorders gradually disappeared, and the troponin T level gradually decreased to 487.9 ng/L on day 35. Oral prednisone (50 mg/day, with gradually decreasing doses) was maintained. The second and third infusions of infliximab were administered on days 37 and 64, respectively.
Timeline of major events in Case 1 (Patient No. 11). A The main treatment for Case 1 (Patient No. 11) who presented with symptoms of myocarditis. B Levels of inflammatory cytokine Inflammatory cytokine levels (TNF-α and IL-6) of Case 1 (Patient No. 11) during the treatment. The red line represents the dose of steroids used during the patient's treatment. The blue line represents the troponin T level during the patient's treatment. The green block represents the MMF treatment. The yellow block represents the IVIG treatment. The pink arrow represents the IFX treatment. ①, ② and ③ represent the first, second and third infusions of IFX, respectively. The dark green line represents IL-6 levels during the treatment. The purple line represents the TNF-α levels during the treatment. Steroid: including methylprednisolone sodium succinate, methylprednisolone, oral prednisone. TNF-α tumor necrosis factor-α, IL-6 interleukin-6, IVIG intravenous immunoglobulin, MMF mycophenolate mofetil, IFX infliximab
At the five-month follow-up, the patient was alive, with a troponin T level of 34 ng/L, and did not experience any recurrence of adverse cardiac events or myositis. CT scan revealed significant regression of the primary tumor > 30% reduction, and the therapeutic evaluation indicated partial response (PR) (Fig. 2A, B). Unfortunately, progressive disease of the primary tumor was detected via CT scan in February 2022 (Fig. 2C). He subsequently received carboplatin and paclitaxel. Chest CT revealed progression of the pulmonary lesions, which were 7.2 × 3.3 cm in size (Fig. 2D). Thereafter, the patient received 3 cycles of gemcitabine and cisplatin and 25 cycles of thoracic radiation without an increase in troponin T.
Dynamic imaging of thoracic computed tomography (CT) scan of a patient with lung squamous cell carcinoma (Case 1, Patient No. 11). A The primary tumor was 10.3 × 5.2 cm in size before the patient received immunotherapy in July 2020. B The primary tumor with unmeasurable tumor size after the patient received three doses of infliximab in November 2020. C The primary tumor was 3.0 × 1.9 cm in size before the patient received chemotherapy in February 2022. D The primary tumor was 7.8 × 3.2 cm in size after three cycles of gemcitabine and cisplatin-treated with the patient in November 2023. The white arrow in the figure highlights the area of the primary tumor
Case 2
A 57-year-old female (height: 155 cm; weight: 62.5 kg), without a history of coronary disease, chronic heart disease, autoimmune rheumatic diseases or allergies, who presented with right-sided chest pain, was diagnosed with lung adenocarcinoma (cT4N2M1a, stage IVA, EGFRL858R) in September 2022. After resistance to icotinib, the patient was treated with SHR-1701(anti-PD-L1/TGF-βR fusion protein) plus carboplatin and paclitaxel. Prior to receiving the fourth cycle, she presented with a one-week symptom of dyspnea. A physical examination did not reveal lower-extremity swelling, jugular vein distention or rales in her lower lung lobes bilaterally. An initial examination revealed the levels of troponin T and creatine kinase-myocardial band were elevated at 299.5 ng/L (reference value: 0–14.0 ng/L) and 77.92 ng/mL (reference value < 2.88 ng/mL), respectively, whereas BNP was normal (236.00 ng/L, reference value: 0–334.00 ng/L). Echocardiography revealed an enlarged left atrium, a thickened interventricular septum, a widened ascending aorta, pulmonary artery, and the ejection fraction mildly decreased from 73 to 63%. Coronary contrasted CT did not show any abnormalities in the coronary arteries. The diagnosis of ICI-induced myocarditis (grade 3) was considered.
Consequently, SHR-1701 was discontinued, and the patient was treated with methylprednisolone (80 mg/day for 9 days, with gradually decreasing doses) (Fig. 3A). After the symptom of dyspnea resolved and troponin T level gradually decreased to 123.2 ng/L, she was discharged on day 10. However, she returned on day 16 for severe dyspnea and chest tightness with increased troponin T (210.0 ng/L, reference value: 0–14.0 ng/L), no signs of lower-extremity swelling or jugular vein distention. She was diagnosed with steroid-refractory myocarditis induced by ICI according to a nonsignificant reduction in troponin T after adequate steroid for 16 days. Primary cardiac diseases and serious infections were excluded according to the examination including the electrocardiogram, serological respiratory pathogen panel and chest CT. She was treated with pulse-dose methylprednisolone (500 mg/day) for 3 days, MMF (1,000 mg/day) for 11 days and IVIG (20 g/day) for 3 days. The patient's dyspnea has not been relieved and the level of troponin T was 169.1 ng/L. Laboratory testing revealed an increasing trend of TNF-α (1.2 pg/ml, baseline level: 0.72 pg/ml, reference values < 8.5 pg/ml) and a decreasing trend of IL-6 (< 1.5 pg/ml, baseline level: 6.81 pg/ml, reference value: 0–7.0 pg/ml) (Fig. 3B). Infliximab (at a dose of 200 mg per 2 weeks) was administered on day 31. Oral prednisone (50 mg/day, with gradually decreasing doses) was maintained. The second and third infusions of infliximab were administered on days 45 and 73, respectively.
Timeline of major events in Case 2 (Patient No. 12). A The main treatment for Case 2 (Patient No. 12) who presented with symptoms of myocarditis. B Levels of inflammatory cytokine (TNF-α and IL-6) of Case 2 (Patient No. 12) during the treatment. The red line represents the dose of steroids used during the patient's treatment. The blue line represents the troponin T level during the patient's treatment. The green block represents the MMF treatment. The yellow block represents the IVIG treatment. The pink arrow represents the IFX treatment. ①, ② and ③ represent the first, second and third infusions of IFX, respectively. The dark green line represents IL-6 levels during the treatment. The purple line represents the TNF-α levels during the treatment. Steroid: including methylprednisolone sodium succinate, methylprednisolone, oral prednisone. TNF-α tumor necrosis factor-α, IL-6 interleukin-6, IVIG intravenous immunoglobulin, MMF mycophenolate mofetil, IFX infliximab
At the five-month follow-up, the patient denied any episodes of chest tightness or dyspnea. The efficacy evaluation was PR based on the image of CT scan (Fig. 4A, B). She subsequently started pemetrexed, carboplatin and bevacizumab for antitumor therapy.
Dynamic imaging of thoracic CT scan of a patient with lung adenocarcinoma in Case 2 (Patient No. 12). A The primary tumor was 7.9 × 4.0 cm in size before the patient received immunotherapy in March 2023. B The primary tumor was 5.4 × 4.5 cm size after three doses of infliximab in August 2023. The white arrow in the figure highlights the area of the primary tumor
Discussion
We reported two cases of steroid-refractory myocarditis induced by ICI that were not affected by immunosuppressant drugs such as IVIG and MMF. Considering the elevated TNF-α and lower IL-6 levels, patients were treated with the personalized anti-cytokine inhibitors of infliximab. After three cycles of infliximab treatment, our patients’ symptoms resolved, and the troponin T and TNF-α levels gradually returned to normal. Infliximab as a potential strategy could be considered for patients with low IL-6 level and elevated TNF-α level.
A previous study reported that the incidence of cardiotoxicity caused by paclitaxel was nearly 0.5% within 1 h to 14 days following therapy [22]. The events that were most commonly reported were decreases in heart rate and blood pressure, whereas myocarditis was rare [22]. In addition, several cases reported that myocarditis occurred during the administration of ICI combination with carboplatin/paclitaxel [23,24,25]. Moreover, randomized controlled trials and retrospective studies have indicated that the use of ICI alone or ICI plus chemotherapy resulted in greater risk of cardiotoxicity than chemotherapy alone [26, 27]. On the basis of previous studies and the clinical course, we consider that our patients had ICI-induced myocarditis and the combination of ICI and chemotherapy may increase the risk of myocarditis. ICI-induced myocarditis is rare and fatal, with a reported incidence of 0.06–1.00% and a maximum fatality rate of 37% [2,3,4,5, 28]. Most cases occur after the first or second ICI infusion, with a median duration of 30 days [29]. However, the exact mechanism remains unclear, and further evidence is needed. The PD-1/PD-L1 and CTLA-4 signaling pathways were shown to play key roles in protecting the myocardium from excessive immune responses [30,31,32]. This effect is likely associated with a systemic inflammatory response with increased levels of cytokines [33, 34]. Recent studies have demonstrated that increased IL-6 and decreased PD-1 levels lead to decreased regulatory T cell (Tregs) with an aggravated inflammatory response [35,36,37,38,39,40]. Several studies have suggested that TNF-α, IL-6, interferon (IFN)-γ and C-reactive protein should be used as monitoring indicators to detect and manage cytokine release syndrome (CRS) induced by immunotherapy [34, 41,42,43,44]. Endomyocardial biopsy and autopsy results from multiple series revealed more PD-1− CD4+ T cells, PD-1− CD8+ T cells, inflammatory macrophages and less Treg infiltration (Table 1) [16, 18, 19, 32, 35, 45,46,47,48,49,50].
We conducted a comprehensive literature search of PubMed and Embase for cases of steroid-refractory myocarditis induced by ICI. Patients with “steroid-refractory myocarditis induced by ICI” were defined as those who were refractory to steroid with a new diagnosis of ICI-induced myocarditis. We used the following keywords to search for articles in PubMed and Embase: “pembrolizumab”, “nivolumab”, “ipilimumab”, “atezolizumab”, “tislelizumab”, “durvalumab”, “avelumab”, “tremelimumab”, “sintilimab”, “toripalimab”, “cemiplimab”, “PD-1/PD-L1 inhibitors”, “anti-CTLA4 antibody”, “immune checkpoint inhibitor”, “ICI”, “immunotherapy” and “myocarditis”. A total of 76 cases were initially selected; 23 cases were excluded because of the unjustifiable use of steroid and immunosuppressive drugs (n = 6), lack of treatment with other immunosuppressive drugs (n = 9) or lack of detailed case presentation (n = 8). Ultimately, we reviewed 53 cases of steroid-refractory myocarditis induced by ICI including 2 cases in our hospital and 51 cases in literatures [11, 12, 16,17,18,19, 45,46,47,48, 51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75] in Table 2.
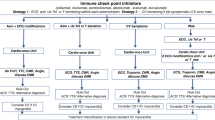
In previous cases and studies, 53 patients who were diagnosed with steroid-refractory myocarditis, 45.5% (10/22) of patients benefited from immunosuppressive drugs (IVIG, MMF, plasmapheresis or tacrolimus), and 71.4% (15/21) of patients benefited from infliximab. Three patients were treated with tocilizumab, and 7 patients received abatacept, alemtuzumab or rituximab. A summary of these cases is provided in Table 2. Recently, an international multicenter retrospective observational study showed that early and high-dose steroid treatment can mitigate myocardial injury and reduce the risk of cardiac adverse events [76]. Studies have suggested that earlier initiation of other additional immunosuppressive drugs combined with initial high-dose steroid may reduce the total duration of steroid exposure and may not decrease the efficacy of ICI [12, 77, 78]. Compared with immunosuppressive drugs, specific cytokine inhibitors, such as infliximab and tocilizumab, have demonstrated better therapeutic efficacy in resolving steroid-refractory myocarditis induced by ICI in previous studies (Table 2). However, patient No.17 deteriorated progressively and succumbed to multiple organ failure with infliximab. The case proposed prompt tocilizumab treatment in addition to steroid for patients on the basis of elevated serum levels of IL-6 and normal TNF-α [16]. Therefore, we aimed to investigate the clinical characteristics and inflammatory cytokine levels of patients to predict the effects of infliximab or tocilizumab (Table 1). A summary of IL-6 and TNF-α in the serum is provided (Fig. 5A, B).
Changes in inflammatory cytokines (TNF-α and IL-6) in patients No. 11, No. 12, No. 17, No. 20, and No. 22. A Levels of TNF-α in patients during the process of myocarditis. B Levels of IL-6 in patients during the process of myocarditis. The horizontal axis represents the time point at which the patient was tested for TNF-α/IL-6. The vertical axis represents the level of TNF-α/IL-6. Initial: the level of TNF-α/IL-6 when the patient was tested for the first time. Top: the top level of TNF-α/IL-6 during the process of myocarditis. After: the level of TNF-α/IL-6 when patient with normal troponin T. TNF-α tumor necrosis factor-α, IL-6 interleukin-6
The patients were divided into two groups (Group I and Group II) according to their levels of IL-6 and TNF-α (No. 11 and No. 12.; No. 17, No. 20 and No. 22). In Group I, patients No. 20 and No. 22 had elevated levels of IL-6 and TNF-α. Patient No. 17 had elevated levels of IL-6 and stable TNF-α. In Group II, patients No. 11 and No. 12 were characterized by decreasing trend in IL-6 and an increasing trend in TNF-α. Patients No. 20 and No. 22 in Group I improved from tocilizumab, and the patients in Group II benefited from infliximab. It seems that infliximab is effective in patients with elevated TNF-α levels but not in those with elevated IL-6 levels. Tocilizumab is more likely suitable for patients with elevated IL-6 level and elevated/lower TNF-α level.
Infliximab (anti-TNF-α Ab), the first monoclonal antibody that blocks TNF/tumor necrosis factor receptor (TNFR)-1 signaling, reverses CD8+T-cell dysfunction and decreases the levels of proinflammatory cytokines produced by fibroblasts, leading to the amelioration of myocardial injury and improved antitumor immunity [79,80,81,82]. Zinc finger (de)ubiquitinating enzyme A20/TNF-α-induced protein 3 (TNFAIP3) is associated with autoinflammation and autoimmunity by controlling nuclear factor-κB (NF-κB) activity [83]. We reviewed 21 patients who were treated with infliximab, 5 (23.8%) of whom died from cardiovascular events. The dose of 10 mg/kg of infliximab is likely harmful in patients with class III-IV heart failure and should be avoided [13, 84, 85]. Given that the use of infliximab in patients with heart failure is controversial, we discussed the patients grouped by heart failure status. Cardiovascular-related mortality was greater in patients with heart failure, while the difference was not statistically significant (33.3% vs. 25.0%, P > 0.05). Short-term infliximab may not adversely affect the clinical condition of these patients [85, 86]. Prior studies suggested that optimized infliximab treatment (5 mg/kg) reduces inflammatory activity and was safe without worsening prevalent heart failure in patients with colitis, ICI-induced myocarditis, rheumatoid arthritis and refractory cardiac sarcoidosis [12, 87,88,89,90]. In a recent study, 4 patients with severe steroid-resistant colitis who received infliximab and ICI therapy improved, and disease stability [87]. This effect was related to preventing the activation-induced death of tumor-infiltrating lymphocytes induced by anti-PD-1 therapy and decreasing the expression of PD-L1 and TIM-3 [91]. Thus, low-dose infliximab seems safe and effective for ICI-induced myocarditis in prior studies and in our cases. Since the patients were diagnosed with serve myocarditis (grade 3 or grade 4), immunotherapy was discontinued according to the guidelines of the ASCO, NCCN, ESMO and SITC [2, 7,8,9].
Tocilizumab (anti-IL-6 receptor Ab), a humanized anti-human IL-6 receptor monoclonal antibody, has been successfully used to treat CRS associated with ICI-induced myocarditis [17,18,19]. Previous studies have indicated that targeting IL-6R could be an effective and safe approach for treating several types of irAEs without severe adverse events or hindering antitumor immunity [92,93,94]. Mechanistically, combined blockade of the IL-6 and PD-1/PD-L1 signaling pathways can regulate immunosuppressive activities and enhance antitumor effects, especially the Th1 response in tumor-bearing mice [95]. Clinical trials (NCT04940299 and NCT03999749) to evaluate the safety and efficacy of tocilizumab in combination with ICIs are currently underway [96, 97]. It has been confirmed that tocilizumab decreases the levels of the inflammatory cytokines TNF-α and IL-1β and the infiltration of CD3+ T cells and CD68+ macrophages by blocking signaling pathways [98, 99]. Therefore, tocilizumab is effective in patients with high levels of IL-6 and TNF-α. On the basis of these findings, considering the levels of inflammatory cytokines (TNF-α and IL-6) is a potential personalized cytokine inhibitor strategy.
Our study shows that cytokine inhibitors combined with the level of cytokines have the potential to benefit patients. A limitation of our review should be noted. The majority of the clinical information was based on case reports, and more cases and studies need to be conducted to verify and confirm the efficacy of these treatments in the future. In addition, owing to the retrospective study, the data of cytokines was uncompleted, and standardized and dynamic monitoring of cytokine changes is essential in the further study.
Conclusions
Infliximab shows therapeutic effects for selected patients with steroid-refractory myocarditis induced by ICI. The serum levels of cytokine, including IL-6 and TNF-α, have potential value in guiding the selection of cytokine inhibitors.
Data Availability
All the data supporting our findings are contained within the manuscript.
Abbreviations
- ICIs:
-
Immune checkpoint inhibitors
- PD-1/PD-L1:
-
Programmed cell death protein 1
- CTLA-4:
-
Cytotoxic T-lymphocyte associated protein 4
- irAEs:
-
Immune-related adverse events
- IVIG:
-
Intravenous immunoglobulin
- MMF:
-
Mycophenolate mofetil
- TNF-α:
-
Tumor necrosis factor-α
- IL:
-
Interleukin
- ESMO:
-
European Society for Medical Oncology
- ASCO:
-
American Society of Clinical Oncology
- SITC:
-
Society for Immunotherapy of Cancer
- NCCN:
-
National Comprehensive Cancer Network
- BNP:
-
N-terminal pro-B-type natriuretic peptide
- AchR:
-
Acetylcholine receptor
- CT:
-
Computed tomography
- PR:
-
Partial response
- IFN:
-
Interferon
- CRS:
-
Cytokine release syndrome
- Tregs:
-
Regulatory T cell
- NF-κB:
-
Nuclear factor-κB
References
Diesendruck, Y., & Benhar, I. (2017). Novel immune check point inhibiting antibodies in cancer therapy-opportunities and challenges. Drug Resistance Updates: Reviews and Commentaries in Antimicrobial and Anticancer Chemotherapy, 30, 39–47. https://doi.org/10.1016/j.drup.2017.02.001
Schneider, B. J., Naidoo, J., Santomasso, B. D., Lacchetti, C., Adkins, S., Anadkat, M., & Bollin, K. (2021). Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: ASCO guideline update. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 39(36), 4073–4126. https://doi.org/10.1200/JCO.21.01440
Puzanov, I., Diab, A., Abdallah, K., Bingham, C. O., Brogdon, C., Dadu, R., Society for Immunotherapy of Cancer Toxicity Management Working Group. (2017). Managing toxicities associated with immune checkpoint inhibitors: Consensus recommendations from the society for immunotherapy of cancer (SITC) toxicity management working group. Journal for Immunotherapy of Cancer, 5(1), 95. https://doi.org/10.1186/s40425-017-0300-z
Michot, J. M., Bigenwald, C., Champiat, S., Collins, M., Carbonnel, F., Postel-Vinay, S., & Lambotte, O. (2016). Immune-related adverse events with immune checkpoint blockade: A comprehensive review. European Journal of Cancer, 54, 139–148. https://doi.org/10.1016/j.ejca.2015.11.016
Ganatra, S., & Neilan, T. G. (2018). Immune checkpoint inhibitor-associated myocarditis. The Oncologist, 23(8), 879–886. https://doi.org/10.1634/theoncologist.2018-0130
Luo, W., Wang, Z., Zhang, T., Yang, L., Xian, J., Li, Y., & Li, W. (2021). Immunotherapy in non-small cell lung cancer: Rationale, recent advances and future perspectives. Precision Clinical Medicine, 4(4), 258–270. https://doi.org/10.1093/pcmedi/pbab027
Haanen, J., Obeid, M., Spain, L., Carbonnel, F., Wang, Y., Robert, C., ESMO Guidelines Committee. (2022). Management of toxicities from immunotherapy: ESMO clinical practice guideline for diagnosis, treatment and follow-up. Annals of Oncology: Official Journal of the European Society for Medical Oncology, 33(12), 1217–1238. https://doi.org/10.1016/j.annonc.2022.10.001
Brahmer, J. R., Abu-Sbeih, H., Ascierto, P. A., Brufsky, J., Cappelli, L. C., Cortazar, F. B., & Ernstoff, M. S. (2021). Society for immunotherapy of cancer (SITC) clinical practice guideline on immune checkpoint inhibitor-related adverse events. Journal for Immunotherapy of Cancer, 9(6), e002435. https://doi.org/10.1136/jitc-2021-002435
Thompson, J. A., Schneider, B. J., Brahmer, J., Andrews, S., Armand, P., Bhatia, S., & Engh, A. (2020). NCCN guidelines insights: Management of immunotherapy-related toxicities, version 1.2020. Journal of the National Comprehensive Cancer Network: JNCCN, 18(3), 230–241. https://doi.org/10.6004/jnccn.2020.0012
Brahmer, J. R., Lacchetti, C., Schneider, B. J., Atkins, M. B., Brassil, K. J., Caterino, J. M., National Comprehensive Cancer Network. (2018). Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American society of clinical oncology clinical practice guideline. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 36(17), 1714–1768. https://doi.org/10.1200/JCO.2017.77.6385
Agrawal, N., Khunger, A., Vachhani, P., Colvin, T. A., Hattoum, A., Spangenthal, E., & Puzanov, I. (2019). Cardiac toxicity associated with immune checkpoint inhibitors: Case series and review of the literature. Case Reports in Oncology, 12(1), 260–276. https://doi.org/10.1159/000498985
Zhang, R. S., Padegimas, A., Murphy, K. M., Evans, P. T., Peters, C. J., Domenico, C. M., & O’Quinn, R. P. (2021). Treatment of corticosteroid refractory immune checkpoint inhibitor myocarditis with Infliximab: A case series. Cardio-Oncology, 7(1), 13. https://doi.org/10.1186/s40959-021-00095-x
Cautela, J., Zeriouh, S., Gaubert, M., Bonello, L., Laine, M., Peyrol, M., & Thuny, F. (2020). Intensified immunosuppressive therapy in patients with immune checkpoint inhibitor-induced myocarditis. Journal for Immunotherapy of Cancer, 8(2), e001887. https://doi.org/10.1136/jitc-2020-001887
Malandrino, D., Bello, F., Lopalco, G., Cantarini, L., Olivotto, I., Emmi, G., & Prisco, D. (2024). Effectiveness and safety of IL1 inhibition with anakinra in chronic refractory idiopathic myocarditis. Internal and Emergency Medicine, 19(2), 583–588. https://doi.org/10.1007/s11739-023-03514-2
Wu, Y., Xu, Y., & Xu, L. (2023). Drug therapy for myocarditis induced by immune checkpoint inhibitors. Frontiers in Pharmacology, 14, 1161243. https://doi.org/10.3389/fphar.2023.1161243
Saibil, S. D., Bonilla, L., Majeed, H., Sotov, V., Hogg, D., Chappell, M. A., & Butler, M. O. (2019). Fatal myocarditis and rhabdomyositis in a patient with stage IV melanoma treated with combined ipilimumab and nivolumab. Current Oncology, 26(3), e418–e421. https://doi.org/10.3747/co.26.4381
Doms, J., Prior, J. O., Peters, S., & Obeid, M. (2020). Tocilizumab for refractory severe immune checkpoint inhibitor-associated myocarditis. Annals of Oncology: Official Journal of the European Society for Medical Oncology, 31(9), 1273–1275. https://doi.org/10.1016/j.annonc.2020.05.005
Wang, H., Tian, R., Gao, P., Wang, Q., & Zhang, L. (2020). Tocilizumab for fulminant programmed death 1 inhibitor-associated myocarditis. Journal of Thoracic Oncology: Official Publication of the International Association for the Study of Lung Cancer, 15(3), e31–e32. https://doi.org/10.1016/j.jtho.2019.09.080
Wu, S. J., Liu, X. H., Wu, W., Qian, M., Li, L., Zhang, L., & Liu, Y. X. (2022). Tocilizumab therapy for immune checkpoint inhibitor associated myocarditis: A case report. Zhonghua Xin Xue Guan Bing Za Zhi, 50(4), 397–400. https://doi.org/10.3760/cma.j.cn112148-20210511-00412
Baclig, N. V., Ngo, C., Yeh, A. C., Chung, S. H., Cheng, A., Grim, J., & Yang, K. C. (2019). Steroid-refractory autoimmune myocarditis after pembrolizumab therapy: Failure of equine anti-thymocyte globulin to prevent heart failure. Journal of Clinical Case Reports, 2(1), 1–4.
Kang, J. H., Bluestone, J. A., & Young, A. (2021). Predicting and preventing immune checkpoint inhibitor toxicity: Targeting cytokines. Trends in Immunology, 42(4), 293–311. https://doi.org/10.1016/j.it.2021.02.006
Pai, V. B., & Nahata, M. C. (2000). Cardiotoxicity of chemotherapeutic agents: Incidence, treatment and prevention. Drug Safety, 22(4), 263–302. https://doi.org/10.2165/00002018-200022040-00002
Long, H.-D., Du, Y.-P., Wang, L.-Y., Liu, G.-C., Liang, S.-X., Zeng, Z.-H., & Lin, Y.-E. (2024). Successful management of camrelizumab-induced immune-checkpoint-inhibitors-related myocarditis. Journal of Oncology Pharmacy Practice: Official Publication of the International Society of Oncology Pharmacy Practitioners, 30(3), 597–604. https://doi.org/10.1177/10781552231216104
Ye, Y., Li, Y., Zhang, S., & Han, G. (2022). Teriprizumab-induced myocarditis in a patient with cholangiocarcinoma: A case report. The Journal of International Medical Research, 50(10), 3000605221133259. https://doi.org/10.1177/03000605221133259
Xu, J., Kato, K., Raymond, E., Hubner, R. A., Shu, Y., Pan, Y., & Yoon, H. H. (2023). Tislelizumab plus chemotherapy versus placebo plus chemotherapy as first-line treatment for advanced or metastatic oesophageal squamous cell carcinoma (RATIONALE-306): A global, randomised, placebo-controlled, phase 3 study. The Lancet. Oncology, 24(5), 483–495. https://doi.org/10.1016/S1470-2045(23)00108-0
Sharma, A., Alexander, G., Chu, J. H., Markopoulos, A., Maloul, G., Ayub, M. T., & Okwuosa, T. M. (2024). Immune checkpoint inhibitors and cardiotoxicity: A comparative meta-analysis of observational studies and randomized controlled trials. Journal of the American Heart Association, 13(10), e032620. https://doi.org/10.1161/JAHA.123.032620
Zhang, X.-T., Ge, N., Xiang, Z.-J., & Liu, T. (2022). Immune checkpoint inhibitor-related adverse cardiac events in patients with lung cancer: A systematic review and meta-analysis. Cancer Cell International, 22(1), 363. https://doi.org/10.1186/s12935-022-02760-2
Wang, D. Y., Salem, J.-E., Cohen, J. V., Chandra, S., Menzer, C., Ye, F., & Johnson, D. B. (2018). Fatal toxic effects associated with immune checkpoint inhibitors: A systematic review and meta-analysis. JAMA oncology, 4(12), 1721–1728. https://doi.org/10.1001/jamaoncol.2018.3923
Escudier, M., Cautela, J., Malissen, N., Ancedy, Y., Orabona, M., Pinto, J., & Thuny, F. (2017). Clinical features, management, and outcomes of immune checkpoint inhibitor-related cardiotoxicity. Circulation, 136(21), 2085–2087. https://doi.org/10.1161/CIRCULATIONAHA.117.030571
Tarrio, M. L., Grabie, N., Bu, D., Sharpe, A. H., & Lichtman, A. H. (2012). PD-1 protects against inflammation and myocyte damage in T cell-mediated myocarditis. Journal of Immunology, 188(10), 4876–4884. https://doi.org/10.4049/jimmunol.1200389
Okazaki, T., Tanaka, Y., Nishio, R., Mitsuiye, T., Mizoguchi, A., Wang, J., & Honjo, T. (2003). Autoantibodies against cardiac troponin I are responsible for dilated cardiomyopathy in PD-1-deficient mice. Nature Medicine, 9(12), 1477–1483. https://doi.org/10.1038/nm955
Grabie, N., Gotsman, I., DaCosta, R., Pang, H., Stavrakis, G., Butte, M. J., & Lichtman, A. H. (2007). Endothelial programmed death-1 ligand 1 (PD-L1) regulates CD8+ T-cell–mediated injury in the heart. Circulation, 116(18), 2062–2071. https://doi.org/10.1161/CIRCULATIONAHA.107.709360
Shimabukuro-Vornhagen, A., Gödel, P., Subklewe, M., Stemmler, H. J., Schlößer, H. A., Schlaak, M., & von Bergwelt-Baildon, M. S. (2018). Cytokine release syndrome. Journal for Immunotherapy of Cancer, 6(1), 56. https://doi.org/10.1186/s40425-018-0343-9
Lim, S. Y., Lee, J. H., Gide, T. N., Menzies, A. M., Guminski, A., Carlino, M. S., & Rizos, H. (2019). Circulating cytokines predict immune-related toxicity in melanoma patients receiving anti-PD-1-based immunotherapy. Clinical Cancer Research: An Official Journal of the American Association for Cancer Research, 25(5), 1557–1563. https://doi.org/10.1158/1078-0432.CCR-18-2795
Liu, Y.-X., Song, Y.-J., Liu, X.-H., Xu, S.-C., Kong, C., Chen, L.-F., & Wu, W. (2022). PD-1 inhibitor induces myocarditis by reducing regulatory T cells, activating inflammatory responses, promoting myocardial apoptosis and autophagy. Cytokine, 157, 155932. https://doi.org/10.1016/j.cyto.2022.155932
Khoury, T., Molho-Pessach, V., Ramot, Y., Ayman, A. R., Elpeleg, O., Berkman, N., & Ilan, Y. (2017). Tocilizumab promotes regulatory T-cell alleviation in STAT3 gain-of-function-associated multi-organ autoimmune syndrome. Clinical Therapeutics, 39(2), 444–449. https://doi.org/10.1016/j.clinthera.2017.01.004
Stathopoulou, C., Gangaplara, A., Mallett, G., Flomerfelt, F. A., Liniany, L. P., Knight, D., & Amarnath, S. (2018). PD-1 inhibitory receptor downregulates asparaginyl endopeptidase and maintains foxp3 transcription factor stability in induced regulatory T cells. Immunity, 49(2), 247-263.e7. https://doi.org/10.1016/j.immuni.2018.05.006
van Gulijk, M., van Krimpen, A., Schetters, S., Eterman, M., van Elsas, M., Mankor, J., & van Hall, T. (2023). PD-L1 checkpoint blockade promotes regulatory T cell activity that underlies therapy resistance. Science Immunology, 8(83), eabn6173. https://doi.org/10.1126/sciimmunol.abn6173
Chen, X., Das, R., Komorowski, R., Beres, A., Hessner, M. J., Mihara, M., & Drobyski, W. R. (2009). Blockade of interleukin-6 signaling augments regulatory T-cell reconstitution and attenuates the severity of graft-versus-host disease. Blood, 114(4), 891–900. https://doi.org/10.1182/blood-2009-01-197178
Miyabe, C., Miyabe, Y., Strle, K., Kim, N. D., Stone, J. H., Luster, A. D., & Unizony, S. (2017). An expanded population of pathogenic regulatory T cells in giant cell arteritis is abrogated by IL-6 blockade therapy. Annals of the Rheumatic Diseases, 76(5), 898–905. https://doi.org/10.1136/annrheumdis-2016-210070
Davila, M. L., Riviere, I., Wang, X., Bartido, S., Park, J., Curran, K., & Brentjens, R. (2014). Efficacy and toxicity management of 19–28z CAR T cell therapy in B cell acute lymphoblastic leukemia. Science Translational Medicine, 6(224), 224ra25. https://doi.org/10.1126/scitranslmed.3008226
Grupp, S. A., Kalos, M., Barrett, D., Aplenc, R., Porter, D. L., Rheingold, S. R., & June, C. H. (2013). Chimeric antigen receptor-modified T cells for acute lymphoid leukemia. The New England Journal of Medicine, 368(16), 1509–1518. https://doi.org/10.1056/NEJMoa1215134
Delyon, J., & Lebbe, C. (2022). IL-6 blockade in cancer patients treated with immune checkpoint blockade: A win-win strategy. Cancer Cell, 40(5), 450–451. https://doi.org/10.1016/j.ccell.2022.04.010
Miao, K., & Zhang, L. (2023). Pathogenesis, pathological characteristics and individualized therapy for immune-related adverse effects. Chinese Medical Journal Pulmonary and Critical Care Medicine, 1(4), 215–222. https://doi.org/10.1016/j.pccm.2023.08.002
Gallegos, C., Rottmann, D., Nguyen, V. Q., & Baldassarre, L. A. (2019). Myocarditis with checkpoint inhibitor immunotherapy: Case report of late gadolinium enhancement on cardiac magnetic resonance with pathology correlate. European Heart Journal. Case Reports, 3(1), yty149. https://doi.org/10.1093/ehjcr/yty149
Johnson, D. B., Balko, J. M., Compton, M. L., Chalkias, S., Gorham, J., Xu, Y., & Moslehi, J. J. (2016). Fulminant myocarditis with combination immune checkpoint blockade. The New England Journal of Medicine, 375(18), 1749–1755. https://doi.org/10.1056/NEJMoa1609214
Martinez-Calle, N., Rodriguez-Otero, P., Villar, S., Mejías, L., Melero, I., Prosper, F., & San-Miguel, J. (2018). Anti-PD1 associated fulminant myocarditis after a single pembrolizumab dose: The role of occult pre-existing autoimmunity. Haematologica, 103(7), e318–e321. https://doi.org/10.3324/haematol.2017.185777
Tay, R. Y., Blackley, E., McLean, C., Moore, M., Bergin, P., Gill, S., & Haydon, A. (2017). Successful use of equine anti-thymocyte globulin (ATGAM) for fulminant myocarditis secondary to nivolumab therapy. British Journal of Cancer, 117(7), 921–924. https://doi.org/10.1038/bjc.2017.253
Ma, P., Liu, J., Qin, J., Lai, L., Heo, G. S., Luehmann, H., & Lavine, K. J. (2023). Expansion of pathogenic cardiac macrophages in immune checkpoint inhibitor myocarditis. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.122.062551
Feng, Y., Zheng, P., Zhang, W., Yang, S., You, Y., Chen, Y., & Ye, Y. (2024). Immune checkpoint inhibitor myocarditis in thymic epithelial tumors: A case report and literature review. Translational Cancer Research, 13(2), 1208–1218. https://doi.org/10.21037/tcr-23-2212
Frigeri, M., Meyer, P., Banfi, C., Giraud, R., Hachulla, A.-L., Spoerl, D., & Dietrich, P.-Y. (2018). Immune checkpoint inhibitor-associated myocarditis: A new challenge for cardiologists. The Canadian Journal of Cardiology, 34(1), 92.e1-92.e3. https://doi.org/10.1016/j.cjca.2017.09.025
Kadokawa, Y., Takagi, M., Yoshida, T., Tatsumi, A., Fujita, K., Inoue, T., & Imamura, F. (2021). Efficacy and safety of Infliximab for steroid-resistant immune-related adverse events: A retrospective study. Molecular and Clinical Oncology, 14(4), 65. https://doi.org/10.3892/mco.2021.2227
Padegimas, A., Agarwal, P., Fleitman, J., Carver, J., Rao, S., Mather, P., & O’Quinn, R. (2019). Case series of ventricular tachycardia and myocarditis from programmed cell-death protein-1 inhibitor treated with infliximab. JACC. Clinical electrophysiology, 5(8), 989–992. https://doi.org/10.1016/j.jacep.2019.05.001
Puzanov, I., Subramanian, P., Yatsynovich, Y. V., Jacobs, D. M., Chilbert, M. R., Sharma, U. C., & Schentag, J. J. (2021). Clinical characteristics, time course, treatment and outcomes of patients with immune checkpoint inhibitor-associated myocarditis. Journal for Immunotherapy of Cancer, 9(6), e002553. https://doi.org/10.1136/jitc-2021-002553
Giancaterino, S., Abushamat, F., Duran, J., Lupercio, F., DeMaria, A., & Hsu, J. C. (2020). Complete heart block and subsequent sudden cardiac death from immune checkpoint inhibitor-associated myocarditis. HeartRhythm Case Reports, 6(10), 761–764. https://doi.org/10.1016/j.hrcr.2020.07.015
Lipe, D. N., Galvis-Carvajal, E., Rajha, E., Wechsler, A. H., & Gaeta, S. (2021). Immune checkpoint inhibitor-associated myasthenia gravis, myositis, and myocarditis overlap syndrome. The American Journal of Emergency Medicine, 46, 51–55. https://doi.org/10.1016/j.ajem.2021.03.005
Salem, J.-E., Allenbach, Y., Vozy, A., Brechot, N., Johnson, D. B., Moslehi, J. J., & Kerneis, M. (2019). Abatacept for severe immune checkpoint inhibitor-associated myocarditis. The New England Journal of Medicine, 380(24), 2377–2379. https://doi.org/10.1056/NEJMc1901677
Esfahani, K., Buhlaiga, N., Thébault, P., Lapointe, R., Johnson, N. A., & Miller, W. H. (2019). Alemtuzumab for immune-related myocarditis due to PD-1 therapy. The New England Journal of Medicine, 380(24), 2375–2376. https://doi.org/10.1056/NEJMc1903064
Liu, S., Chan, J., Brinc, D., Gandhi, S., Izenberg, A., Delgado, D., & Thavendiranathan, P. (2020). Immune checkpoint inhibitor-associated myocarditis with persistent troponin elevation despite abatacept and prolonged immunosuppression. JACC. CardioOncology, 2(5), 800–804. https://doi.org/10.1016/j.jaccao.2020.10.013
Nguyen, L. S., Bretagne, M., Arrondeau, J., Zahr, N., Ederhy, S., Abbar, B., & Salem, J.-E. (2022). Reversal of immune-checkpoint inhibitor fulminant myocarditis using personalized-dose-adjusted abatacept and ruxolitinib: Proof of concept. Journal for Immunotherapy of Cancer, 10(4), e004699. https://doi.org/10.1136/jitc-2022-004699
Arora, P., Talamo, L., Dillon, P., Gentzler, R. D., Millard, T., Salerno, M., & Gaughan, E. M. (2020). Severe combined cardiac and neuromuscular toxicity from immune checkpoint blockade: An institutional case series. Cardio-Oncology, 6, 21. https://doi.org/10.1186/s40959-020-00076-6
Chen, R., Peng, L., Qiu, Z., Wang, Y., Wei, F., Zhou, M., & Zhu, F. (2021). Case report: Cardiac toxicity associated with immune checkpoint inhibitors. Frontiers in Cardiovascular Medicine, 8, 727445. https://doi.org/10.3389/fcvm.2021.727445
Diaz-Rodriguez, P. E., Muns-Aponte, C. M., Velazquez-Acevedo, S. I., Ortiz-Malave, C. M., Acevedo, J., & Merced-Ortiz, F. G. (2023). An uncommon case of myocarditis secondary to durvalumab plus tremelimumab. Cureus, 15(8), e43628. https://doi.org/10.7759/cureus.43628
Edahiro, R., Shiroyama, T., Hijiki, S., Nojima, S., Shirai, Y., Koyama, S., & Kumanogoh, A. (2020). Severe myocarditis with slight lymphocytic infiltration after nivolumab treatment. Lung Cancer, 140, 116–117. https://doi.org/10.1016/j.lungcan.2019.12.004
Hardy, T., Yin, M., Chavez, J. A., Ivanov, I., Chen, W., Nadasdy, T., & Brodsky, S. V. (2020). Acute fatal myocarditis after a single dose of anti-PD-1 immunotherapy, autopsy findings: A case report. Cardiovascular Pathology: The Official Journal of the Society for Cardiovascular Pathology, 46, 107202. https://doi.org/10.1016/j.carpath.2020.107202
Liu, S., Ma, G., Wang, H., Yu, G., Chen, J., & Song, W. (2022). Severe cardiotoxicity in 2 patients with thymoma receiving immune checkpoint inhibitor therapy: A case report. Medicine, 101(46), e31873. https://doi.org/10.1097/MD.0000000000031873
Szuchan, C., Elson, L., Alley, E., Leung, K., Camargo, A. L., Elimimian, E., & Sadler, D. (2020). Checkpoint inhibitor-induced myocarditis and myasthenia gravis in a recurrent/metastatic thymic carcinoma patient: a case report. European Heart Journal. Case Reports, 4(3), 1–8. https://doi.org/10.1093/ehjcr/ytaa051
Yamaguchi, S., Morimoto, R., Okumura, T., Yamashita, Y., Haga, T., Kuwayama, T., & Murohara, T. (2018). Late-onset fulminant myocarditis with immune checkpoint inhibitor nivolumab. The Canadian Journal of Cardiology, 34(6), 812.e1-812.e3. https://doi.org/10.1016/j.cjca.2018.03.007
Aggarwal, N., Bianchini, D., Parkar, R., & Turner, J. (2024). Immunotherapy-induced overlap syndrome: Myositis, myasthenia gravis, and myocarditis-a case series. Case Reports in Medicine, 2024, 5399073. https://doi.org/10.1155/2024/5399073
Mahmood, S. S., Chen, C. L., Shapnik, N., Krishnan, U., Singh, H. S., & Makker, V. (2018). Myocarditis with tremelimumab plus durvalumab combination therapy for endometrial cancer: A case report. Gynecologic Oncology Reports, 25, 74–77. https://doi.org/10.1016/j.gore.2018.05.014
Saito, S., Hontsu, S., Hiraoka, J., Yamanaka, A., Fujioka, N., Shimada, D., & Muro, S. (2024). A rare case of overlapping durvalumab-induced myositis, takotsubo-like morphological changes caused by myocarditis, and myasthenia gravis. Internal Medicine. https://doi.org/10.2169/internalmedicine.3028-23
Gao, P., Li, X., He, Z., Zhang, H., Zhang, Z., & Liu, Z. (2024). Lethal immune myocarditis and myasthenia gravis due to anti-pd-1 treatment for a bladder cancer patient: A case report and possible treatment inspiration. International Medical Case Reports Journal, 17, 359–365. https://doi.org/10.2147/IMCRJ.S449525
Glynn, S. M., Gaillard, S., Stone, R. L., Fader, A. N., & Beavis, A. L. (2024). Pembrolizumab with bevacizumab and cyclophosphamide for the treatment of recurrent ovarian clear cell carcinoma: A case series. Gynecologic Oncology Reports, 53, 101374. https://doi.org/10.1016/j.gore.2024.101374
Shibuya, R., Baba, K., Furuta, R., Maesaka, H., Hirosawa, H., Bando, T., & Nakatsuji, Y. (2024). A case of liver cancer with overlapping myasthenia gravis, myocarditis, seronegative autoimmune autonomic ganglionopathy, and myositis symptoms induced by atezolizumab: A case report. Internal Medicine. https://doi.org/10.2169/internalmedicine.1801-23
Cuenca, J. A., Hanmandlu, A., Wegner, R., Botdorf, J., Tummala, S., Iliescu, C. A., & Reddy, D. R. (2023). Management of respiratory failure in immune checkpoint inhibitors-induced overlap syndrome: A case series and review of the literature. BMC Anesthesiology, 23(1), 310. https://doi.org/10.1186/s12871-023-02257-z
Zhang, L., Zlotoff, D. A., Awadalla, M., Mahmood, S. S., Nohria, A., Hassan, M. Z. O., & Neilan, T. G. (2020). Major adverse cardiovascular events and the timing and dose of corticosteroids in immune checkpoint inhibitor-associated myocarditis. Circulation, 141(24), 2031–2034. https://doi.org/10.1161/CIRCULATIONAHA.119.044703
Scott, S. C., & Pennell, N. A. (2018). Early use of systemic corticosteroids in patients with advanced NSCLC treated with nivolumab. Journal of Thoracic Oncology: Official Publication of the International Association for the Study of Lung Cancer, 13(11), 1771–1775. https://doi.org/10.1016/j.jtho.2018.06.004
Arbour, K. C., Mezquita, L., Long, N., Rizvi, H., Auclin, E., Ni, A., & Hellmann, M. D. (2018). Impact of baseline steroids on efficacy of programmed cell death-1 and programmed death-ligand 1 blockade in patients with non-small-cell lung cancer. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 36(28), 2872–2878. https://doi.org/10.1200/JCO.2018.79.0006
Kroll-Palhares, K., Silvério, J. C., da Silva, A. A., Michailowsky, V., Marino, A. P., Silva, N. M., & Lannes-Vieira, J. (2008). TNF/TNFR1 signaling up-regulates CCR5 expression by CD8+ T lymphocytes and promotes heart tissue damage during trypanosoma cruzi infection: Beneficial effects of TNF-alpha blockade. Memorias Do Instituto Oswaldo Cruz, 103(4), 375–385. https://doi.org/10.1590/s0074-02762008000400011
Bertrand, F., Montfort, A., Marcheteau, E., Imbert, C., Gilhodes, J., Filleron, T., & Ségui, B. (2017). TNFα blockade overcomes resistance to anti-PD-1 in experimental melanoma. Nature Communications, 8(1), 2256. https://doi.org/10.1038/s41467-017-02358-7
Vredevoogd, D. W., Kuilman, T., Ligtenberg, M. A., Boshuizen, J., Stecker, K. E., de Bruijn, B., & Peeper, D. S. (2019). Augmenting immunotherapy impact by lowering tumor TNF cytotoxicity threshold. Cell, 178(3), 585-599.e15. https://doi.org/10.1016/j.cell.2019.06.014
Povoleri, G. A. M., Lalnunhlimi, S., Steel, K. J. A., Agrawal, S., O’Byrne, A. M., Ridley, M., & Taams, L. S. (2020). Anti-TNF treatment negatively regulates human CD4+ T-cell activation and maturation in vitro, but does not confer an anergic or suppressive phenotype. European Journal of Immunology, 50(3), 445–458. https://doi.org/10.1002/eji.201948190
Das, T., Chen, Z., Hendriks, R. W., & Kool, M. (2018). A20/tumor necrosis factor α-induced protein 3 in immune cells controls development of autoinflammation and autoimmunity: Lessons from mouse models. Frontiers in Immunology, 9, 104. https://doi.org/10.3389/fimmu.2018.00104
de Clari, F., Salani, I., Safwan, E., & Giannacco, A. (2002). Sudden death in a patient without heart failure after a single infusion of 200 mg infliximab: Does TNF-alpha have protective effects on the failing heart, or does infliximab have direct harmful cardiovascular effects? Circulation, 105(21), E183. https://doi.org/10.1161/01.cir.0000017216.41471.df
Kwon, H. J., Coté, T. R., Cuffe, M. S., Kramer, J. M., & Braun, M. M. (2003). Case reports of heart failure after therapy with a tumor necrosis factor antagonist. Annals of Internal Medicine, 138(10), 807–811. https://doi.org/10.7326/0003-4819-138-10-200305200-00008
Chung, E. S., Packer, M., Lo, K. H., Fasanmade, A. A., Willerson, J. T., & Investigators, A.-T. (2003). Randomized, double-blind, placebo-controlled, pilot trial of infliximab, a chimeric monoclonal antibody to tumor necrosis factor-alpha, in patients with moderate-to-severe heart failure: Results of the anti-TNF therapy against congestive heart failure (ATTACH) trial. Circulation, 107(25), 3133–3140. https://doi.org/10.1161/01.CIR.0000077913.60364.D2
Badran, Y. R., Cohen, J. V., Brastianos, P. K., Parikh, A. R., Hong, T. S., & Dougan, M. (2019). Concurrent therapy with immune checkpoint inhibitors and TNFα blockade in patients with gastrointestinal immune-related adverse events. Journal for Immunotherapy of Cancer, 7(1), 226. https://doi.org/10.1186/s40425-019-0711-0
Bakker, A. L. M., Mathijssen, H., Azzahhafi, J., Swaans, M. J., Veltkamp, M., Keijsers, R. G. M., & Grutters, J. C. (2021). Effectiveness and safety of infliximab in cardiac sarcoidosis. International Journal of Cardiology, 330, 179–185. https://doi.org/10.1016/j.ijcard.2021.02.022
Listing, J., Strangfeld, A., Kekow, J., Schneider, M., Kapelle, A., Wassenberg, S., & Zink, A. (2008). Does tumor necrosis factor alpha inhibition promote or prevent heart failure in patients with rheumatoid arthritis? Arthritis and Rheumatism, 58(3), 667–677. https://doi.org/10.1002/art.23281
Dahl, E. K., Abed, O. K., Kjeldsen, J., Donia, M., Svane, I. M., Dige, A., Agnholt, J. S., Bjerrum, J. T., & Seidelin, J. B. (2022). Safety and efficacy of infliximab and corticosteroid therapy in checkpoint inhibitor-induced colitis. Alimentary Pharmacology & Therapeutics. https://doi.org/10.1111/apt.17201
Perez-Ruiz, E., Minute, L., Otano, I., Alvarez, M., Ochoa, M. C., Belsue, V., & Melero, I. (2019). Prophylactic TNF blockade uncouples efficacy and toxicity in dual CTLA-4 and PD-1 immunotherapy. Nature, 569(7756), 428–432. https://doi.org/10.1038/s41586-019-1162-y
Campochiaro, C., Farina, N., Tomelleri, A., Ferrara, R., Lazzari, C., De Luca, G., & Dagna, L. (2021). Tocilizumab for the treatment of immune-related adverse events: A systematic literature review and a multicentre case series. European Journal of Internal Medicine, 93, 87–94. https://doi.org/10.1016/j.ejim.2021.07.016
Faak, F., Buni, M., Falohun, A., Lu, H., Song, J., Johnson, D. H., & Diab, A. (2023). Selective immune suppression using interleukin-6 receptor inhibitors for management of immune-related adverse events. Journal for Immunotherapy of Cancer, 11(6), e006814. https://doi.org/10.1136/jitc-2023-006814
Stroud, C. R., Hegde, A., Cherry, C., Naqash, A. R., Sharma, N., Addepalli, S., & Walker, P. (2019). Tocilizumab for the management of immune mediated adverse events secondary to PD-1 blockade. Journal of Oncology Pharmacy Practice: Official Publication of the International Society of Oncology Pharmacy Practitioners, 25(3), 551–557. https://doi.org/10.1177/1078155217745144
Tsukamoto, H., Fujieda, K., Miyashita, A., Fukushima, S., Ikeda, T., Kubo, Y., & Oshiumi, H. (2018). Combined blockade of IL6 and PD-1/PD-L1 signaling abrogates mutual regulation of their immunosuppressive effects in the tumor microenvironment. Cancer Research, 78(17), 5011–5022. https://doi.org/10.1158/0008-5472.CAN-18-0118
M.D. Anderson Cancer Center. (2023). A Phase II Study to Assess the Safety and Efficacy of Tocilizumab in Combination With Ipilimumab and Nivolumab in Patients With Advanced Melanoma, Non-Small Cell Lung Cancer, or Urothelial Carcinoma (Clinical trial registration No. NCT04940299). clinicaltrials.gov. Retrieved from https://clinicaltrials.gov/study/NCT04940299
NYU Langone Health. (2023). A Phase II Study of the Interleukin-6 Receptor Inhibitor Tocilizumab in Combination With Ipilimumab and Nivolumab in Patients With Unresectable Stage III or Stage IV Melanoma (Clinical trial registration No. NCT03999749). clinicaltrials.gov. Retrieved from https://clinicaltrials.gov/study/NCT03999749
Kishimoto, T. (2006). Interleukin-6: Discovery of a pleiotropic cytokine. Arthritis Research & Therapy. https://doi.org/10.1186/ar1916
Savvatis, K., Müller, I., Fröhlich, M., Pappritz, K., Zietsch, C., Hamdani, N., & Tschöpe, C. (2014). Interleukin-6 receptor inhibition modulates the immune reaction and restores titin phosphorylation in experimental myocarditis. Basic Research in Cardiology, 109(6), 449. https://doi.org/10.1007/s00395-014-0449-2
Funding
This work was supported by the National Natural Science Foundation of China (No. 82072598 to P Tian, 92159302 to W Li), Science and Technology Project of Sichuan, China (No. 2022ZDZX0018 to W Li), and 1–3-5 project for disciplines of excellence, West China Hospital, Sichuan University, China (No. ZYJC21052 to P Tian, No. ZYGD22009 to W Li).
Author information
Authors and Affiliations
Contributions
Conceptualization: Sihan Tan, Chang Qi; methodology: Sihan Tan, Chang Qi, Hao Zeng, Qi Wei; formal analysis and investigation: Qin Huang, Xin Pu; writing—original draft preparation: Sihan Tan, Chang Qi; writing—review and editing: Sihan Tan, Chang Qi, Hao Zeng, Qi Wei; funding acquisition: Weimin Li, Panwen Tian; resources: all authors; supervision: Weimin Li, Panwen Tian, Yalun Li.
Corresponding authors
Ethics declarations
Conflict of interest
All authors have completed the ICMJE uniform disclosure form. The authors have no conflicts of interest to declare.
Ethical Approval
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). This study complied with the principles of the Declaration of Helsinki and was approved by the Ethics Committee of West China Hospital (No.2024–197).
Consent for Publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent form is available for review by the Editor of this journal.
Additional information
Handling Editor: Vera Marisa Costa.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tan, S., Qi, C., Zeng, H. et al. Steroid-Refractory Myocarditis Induced by Immune Checkpoint Inhibitor Responded to Infliximab: Report of Two Cases and Literature Review. Cardiovasc Toxicol (2024). https://doi.org/10.1007/s12012-024-09918-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12012-024-09918-6