Abstract
Background
Nivolumab monotherapy is the standard second-line treatment for advanced esophageal squamous cell carcinoma (ESCC) after failure of platinum-based chemotherapy without anti-PD-1 antibody. Fixed dosing with 240 mg every 2 weeks was approved initially, followed by fixed dosing with 480 mg every 4 weeks based on pharmacokinetics data. However, information on the comparative efficacy and safety of the two doses remains limited.
Methods
We compared progression-free survival (PFS), overall survival (OS), objective response rate (ORR), and the incidence of adverse events (AEs) between the two doses in 117 patients who received second-line (n = 85) or later-line (n = 32) nivolumab monotherapy at our institution between January 2016 and December 2021.
Results
In the second-line group, patient characteristics for the 240 mg and 480 mg groups were as follows (240 mg vs. 480 mg): performance status (PS) 0/1/2 was 34/61/5% vs. 54/42/4%, and prior fluoropyrimidine plus platinum therapy (FP) was 81.3% vs. 42.3%. In the later-line group, the characteristics were: PS 0/1/2 was 28/60/12% vs. 14/86/0%, and prior FP was 60.0% vs. 42.8%. ORR was 11.9 vs. 24.0% in the second-line group (p = 0.19) and 0 vs. 14.3% in the later-line group (p = 0.22). Median PFS was 1.7 vs. 4.1 months on second-line (hazard ratio [HR] 0.60, 95% confidence interval [CI] 0.35–1.01, p = 0.056) and 1.4 vs. 1.8 months on later-line (HR 0.58, 95% CI 0.23–1.46, p = 0.25); AEs of any grade were observed in 58.3 vs. 69.7%, respectively.
Conclusions
The efficacy and safety of the two doses of nivolumab monotherapy were comparable in patients with advanced ESCC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The annual incidence of newly diagnosed esophageal cancer (EC) was estimated to be 26,382 in Japan in 2019, ranking 11th among all cancers [1], and to be 20,640 in the US in 2022, accounting for 1.1% of all cancers [2]. EC is classified histologically into squamous cell carcinoma (ESCC) and adenocarcinoma. ESCC has been reported to account for 87.8% of all EC and is more common in Japan than in Western countries [3]. Smoking and alcohol consumption are known to be major risk factors for ESCC, while Barrett's epithelium, reflux esophagitis, and high body mass index are known to be major risk factors for adenocarcinoma [4,5,6,7]. Fluoropyrimidine plus platinum combination therapy was traditionally considered to be first-line therapy for patients with advanced ESCC [8, 9]. However, more recently, fluoropyrimidine plus platinum, nivolumab, nivolumab plus ipilimumab, fluoropyrimidine plus platinum, and pembrolizumab have become established as first-line treatments based on the results of the CheckMate 648 and KEYNOTE-590 trials [10, 11]. Taxanes, nivolumab monotherapy, and pembrolizumab monotherapy can also be used as second-line therapy [12,13,14]. In the 2022 Japanese guidelines for EC, nivolumab monotherapy is strongly recommended for ESCC with no prior anti-PD-L1 therapy and pembrolizumab monotherapy is weakly recommended for ESCC with a combined positive score of ≥ 10 and no prior anti-PD-L1 therapy or microsatellite instability-high or tumor mutational burden-high with no prior anti-PD-L1 antibody. Paclitaxel is weakly recommended for patients with no history of taxane use with or without prior anti-PD-L1 antibody therapy.
Nivolumab was initially approved at a fixed dosage of 240 mg every 2 weeks (Q2W) in February 2020 based on the results of the ATTRACTION-3 trial [12]. A fixed dosage of 480 mg every 4 weeks (Q4W) became available in September 2020 based on pharmacokinetics data [15]. However, there is little clinical information on the difference of efficacy and safety between two dosages in patients with advanced ESCC.
Methods
Design and Patients
This study had a single-center, retrospective design and analyzed data from patients with advanced ESCC treated with second-line or later-line nivolumab monotherapy at the National Cancer Center Hospital in Japan between January 2016 and December 2021. Performance status (PS) was assessed according to the Eastern Cooperative Oncology Group criteria, and the eighth edition of the Union for International Cancer Control TNM classification was used for cancer staging. This study was approved by the National Cancer Center Hospital’s institutional review board (approval number 2020–287) and conducted in accordance with the ethical principles outlined in the Declaration of Helsinki. Although informed consent was not obtained, patients were provided with the opportunity to opt out.
Assessments
We compared the objective response rate (ORR), progression-free survival (PFS), and adverse event (AE) rate between the fixed dosage of 240 mg Q2W and the fixed dosage of 480 mg Q4W in the second-line or later-line setting. The ORR was defined as the proportion of patients with a complete or partial response to treatment according to RECIST (Response Evaluation Criteria in Solid Tumors) version 1.1. The response was evaluated on computed tomography scans obtained every 2–3 months. Overall survival was defined as the interval between the date of initiation of treatment and death (from any cause) or censored at the last date of confirmed survival. PFS was defined as the interval between the start of treatment and the date of the first documentation of disease progression or death (from any cause), whichever occurred first, or was censored at the last date of confirmed survival without disease progression. AEs were graded according to the CTCAE (Common Terminology Criteria of Adverse Events) version 5.0.
Statistical Analysis
The median follow-up duration was estimated using the reversed Kaplan-Meier method. Survival curves were drawn using Kaplan-Meier methods, and these difference between groups was evaluated using the log-rank test. Differences in the distribution of ordinal variables were analyzed using the Chi-squared test or Fisher's exact test. All statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan) [16]. A p-value of < 0.05 was considered statistically significant.
Results
Patient Characteristics
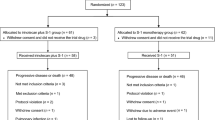
In total, 117 patients with ESCC received nivolumab monotherapy between January 2016 and December 2021. Of the 85 patients who received nivolumab monotherapy as a second-line treatment, 59 received 240 mg Q2W and 26 received 480 mg Q4W. Of the remaining 32 patients who received nivolumab monotherapy as a later-line treatment, 25 received 240 mg Q2W and 7 received 480 mg Q4W (Fig. 1). Patients who switched from 240 mg Q2W to 480 mg Q4W during treatment were excluded. The patient characteristics are shown in Tables 1 and 2. In the second-line group, the median age was 68 (range, 46–85) years in the patients who received 240 mg Q2W and 68.5 (range, 51–84) years in those who received 480 mg Q4W. PS was 0, 1 and 2, respectively, in 34%, 61%, and 5% of patients who received 240 mg Q2W and in 54%, 42%, and 4% of those who received 480 mg Q4W. There was a history of FP therapy in 81.3% of those who received 240 mg Q2W and in 42.3% of those who received 480 mg Q4W. In the later-line group, the median age was 63.5 (range, 47–85) years in the patients who received 240 mg Q2W and 58 (range, 46–80) years in those who received 480 mg Q4W. PS was 0, 1 and 2, respectively, in 28%, 60%, and 12% of patients who received 240 mg Q2W and 14%, 86%, and 0% in those who received 480 mg Q4W. There was a history of FP therapy in 60.0% of patients who received 240 mg Q2W and in 42.8% of those who received 480 mg Q4W. The backgrounds between the 240 mg Q2W and 480 mg Q4W fixed dosages of nivolumab were found to have no significant differences.
Efficacy
In the second-line group, 62 patients had measurable lesions according to RECIST version 1.1 at the start of treatment. The ORR was 11.9% in patients who received 240 mg Q2W and 24.0% in those who received 480 mg Q4W (p = 0.193). In the later-line group, there were 21 patients. The ORR was 0% in patients who received 240 mg Q2W and 14.3% in those who received 480 mg Q4W (p = 0.219). The median follow-up duration was 10.3 months in patients who received 240 mg Q2W and 8.1 months in those who received 480 mg Q4W; median PFS was 1.7 months and 4.1 months, respectively (hazard ratio [HR] 0.60, 95% confidence interval [CI] 0.35–1.01; p = 0.056) (Fig. 2A). In the later-line group, the median follow-up duration was 4.0 months in patients who received 240 mg Q2W and 5.8 months in those who received 480 mg Q4W; median PFS was 1.4 months and 1.8 months, respectively (HR 0.58, 95% CI 0.23–1.46; p = 0.25) (Fig. 2B). In the second-line group, the median OS was 22.7 months in patients who received 240 mg Q2W as compared with Not Available (NA) in those who received 480 mg Q4W (HR 1.00, 95% CI 11.8-NA; P = 0.25) (Fig. 3A). In the later-line group, the median OS was 5.6 months in patients who received 240 mg Q2W as compared with 5.7 months in those who received 480 mg Q4W (HR 1.00, 95% CI 1.97-NA; P = 0.753) (Fig. 3B). There was no significant difference in ORR, PFS, or OS between the fixed dosages of 240 mg Q2W and 480 mg Q4W in either treatment line.
A Progression-free survival in patients receiving nivolumab as second-line monotherapy for advanced esophageal squamous cell carcinoma. The median follow-up duration was 10.3 months in the 240 mg Q2W group and 8.1 months in the 480 mg Q4W group; median progression-free survival was 1.7 months (95% CI 1.38–2.30) and 4.1 months (95% CI 1.81–7.79), respectively (hazard ratio 0.60, 95% CI 0.35–1.01, p = 0.056). CI, confidence interval; Q2W, fixed dosage every two weeks; Q4W, fixed dosage every four weeks. B Progression-free survival in patients receiving nivolumab as later-line monotherapy for advanced esophageal squamous cell carcinoma. The median follow-up duration was 4.0 months in the 240 mg Q2W group and 5.8 months in the 480 mg Q4W group; median progression-free-survival was 1.4 months (95% CI 1.22–1.84) and 1.8 months (95% CI 0.23–5.55), respectively (hazard ratio 0.58, 95% CI 0.23–1.46, p = 0.251). CI, confidence interval; Q2W, fixed dosage every two weeks; Q4W, fixed dosage every four weeks
A Overall survival in patients receiving nivolumab as second-line monotherapy for advanced esophageal squamous cell carcinoma. The median overall survival was 22.8 months (95% CI 11.8-NA) and NA, respectively (hazard ratio 0.99, 95% CI 0.99–1.00, p = 0.26). NA, not available; CI, confidence interval; Q2W, fixed dosage every two weeks; Q4W, fixed dosage every four weeks. B Overall survival in patients receiving nivolumab as later-line monotherapy for advanced esophageal squamous cell carcinoma. The median overall survival was 5.6 months (95% CI 1.98-NA) and 5.7 months (95% CI 1.18-NA), respectively (hazard ratio 0.99, 95% CI 0.99–1.00, p = 0.75). NA, not available; CI, confidence interval; Q2W, fixed dosage every two weeks; Q4W, fixed dosage every four weeks
Safety
Safety was compared between the dosage regimens independent of treatment line. Treatment-related AEs of any grade were observed in 58.3% of patients in the 240 mg Q2W group and in 69.7% of those in the 480 mg Q4W group (Table 3). The frequencies of grade 1, 2, 3, and 4 AEs were as follows: rash, 11.9%, 4.8%, 0%, and 0%, respectively, in the 240 mg Q2W group and 3.0%, 3.0%, 0%, and 0% in the 480 mg Q4W group; pruritus, 14.3%, 6.0%, 0%, and 0% in the 240 mg Q2W group and 12.1%, 0%, 0%, and 0% in the 480 mg Q4W group; diarrhea, 3.6%, 4.8%, 1.2%, and 0% in the 240 mg Q2W group and 3.0%, 3.0%, 0%, and 0% in the 480 mg Q4W group; and interstitial pneumonia, 0%, 0%, 3.6%, and 0% in the 240 mg Q2W group and 0%, 9.1%, 6.1%, and 0% in the 480 mg Q4W group. There were no treatment-related deaths in either dosage group.
Discussion
This study found no statistically significant differences in efficacy and safety between the 240 mg Q2W and 480 mg Q4W fixed dosages of nivolumab when used as salvage-line monotherapy for advanced ESCC. Nivolumab monotherapy was first approved at a dosage of 2 mg/kg every 3 weeks for melanoma based on the results of a Phase II trial [17]. Next, a dosage of 3 mg/kg every 2 weeks was approved for lung cancer based on the results of a Phase III trial [18]. Subsequently, a fixed dosage of 240 mg Q2W became available based on population pharmacokinetics and exposure-response analyses showing comparability of exposure, safety, and efficacy between dosages of 3 mg/kg every 2 weeks and a fixed dosage of 240 mg Q2W [19]. Finally, a fixed dosage of 480 mg Q4W was approved based on modeling and simulation showing that the benefit-risk of a fixed dosage of 480 mg Q4W was a similar to that of 3 mg/kg Q2W [2]. In this study, since the approval of 480 mg Q4W regimen, 480 mg Q4W regimen has been predominantly chosen.
A retrospective cohort study of nivolumab as an adjuvant treatment for melanoma compared the duration of therapy and safety of four different dosage (de novo nivolumab 480 mg Q4W, switched to nivolumab 480 mg Q4W after nivolumab 240 mg or 3 mg/kg Q2W, de novo nivolumab 3 mg/kg Q2W, and de novo nivolumab 240 mg Q2W) [20]. The safety profiles of nivolumab 240 mg Q2W and 480 mg Q4W were similar and comparable with the safety profile of nivolumab 3 mg/kg Q2W [20]. In the present study, ORR was 11.9% in patients who received 240 mg Q2W and 24.0% in those who received 480 mg Q4W (p = 0.193) in the second-line setting and 0% and 14.3%, respectively (p = 0.219) in the later-line setting; the difference according to treatment line was not statistically significant. Median PFS was 1.7 months in patients who received 240 mg Q2W and 4.1 months in those who received 480 mg Q4W as a second-line treatment (HR 0.60, 95% CI 0.35–1.01; p = 0.056) and 1.4 months and 1.8 months, respectively, in those who received nivolumab as a later-line treatment (HR 0.58, 95% CI 0.23–1.46; p = 0.25). Although there was no statistically significant difference between the two fixed dosages, 480 mg Q4W showed a trend of slightly better efficacy. This finding may reflect differences in patient background characteristics or differences in the timing of standard treatment. This is the first study to demonstrate the efficacy and safety of nivolumab at these dosages for advanced ESCC, and its findings are similar to those in melanoma and other solid and hematological tumors [20, 21].
Our finding of no significant difference in AEs between the two dosages of nivolumab is consistent with a previous report [22]. Interstitial pneumonia cases tended to be more frequent in patients who received 480 mg Q4W. However, chart review revealed that patients who developed interstitial pneumonia had pre-existing poor lung function because of underlying collagen disease or chronic obstructive pulmonary disease. When there was evidence of pneumonia and an increased oxygen demand, there was a tendency to administer steroids early before the pneumonia became severe. This could reflect implementation of methods to manage immune-related AEs potentially caused by nivolumab.
This study has some limitations. First, it had a single-center retrospective cohort design and a small number of patients. In the second-line cohort of the 480 mg group, there was a trend towards improved PFS and OS; however, this did not reach statistical significance. The study may have been underpowered to detect small differences, potentially resulting in a Type II error. Second, it included a number of patients with poor PS who were started on nivolumab third-line or later-line treatment immediately after the drug received regulatory approval for use in this setting. In several studies of nivolumab in patients with various types of cancer, subgroup analyses in Japanese patients have identified more cases with good PS and an association between PS and overall survival [17, 18, 23]. Patients with better PS are more likely to receive further treatment. Our present findings indicate that the efficacy and safety of the two currently approved fixed dosages of nivolumab were comparable when used as monotherapy in patients with advanced ESCC. Moreover, they are based on real-world data and confirm that the dosages of nivolumab that have been used up to now are safe and effective.
In conclusion, the two fixed dosages of nivolumab monotherapy currently approved for patients with advanced ESCC were comparable in terms of efficacy and safety.
Data Availability
Individual participant data underpinning the results reported in this article will be shared, after de-identification, with investigators whose proposed data usage has been approved. Proposals for data access should be directed to kenkato@ncc.go.jp.
References
Cancer Information Service. Cancer statistics in Japan. https://ganjoho.jp/reg_stat/statistics/stat/cancer/4_esophagus.html. Accessed 30 Jan 2023.
Cancer Statics. National Cancer Institute. https://seer.cancer.gov/statfacts/html/esoph.html. Accessed 15 Feb 2023.
Watanabe M, Tachimori Y, Oyama T, et al. Comprehensive registry of esophageal cancer in Japan, 2013. Esophagus. 2021;18(1):1–24.
Oze I, Charvat H, Matsuo K, et al. Does cigarette smoking and alcohol drinking have interaction for the risk of esophageal cancer? Cancer Med. 2019;8(14):6414–25.
Yousef F, Cardwell C, Cantwell MM, et al. The incidence of esophageal cancer and high-grade dysplasia in Barrett’s esophagus: A systematic review and meta-analysis. Am J Epidemiol. 2008;168(3):237–49.
Lagergren J, Bergström R, Lindgren A, et al. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Engl J Med. 1999;340(11):825–31.
Nakamura Y, Kitano S, Takahashi A, et al. Nivolumab for advanced melanoma: Pretreatment prognostic factors and early outcome markers during therapy. Oncotarget. 2016;7:77404–15.
Kitagawa Y, Ishihara R, Ishikawa H, et al. Esophageal cancer practice guidelines 2022 edited by the Japan Esophageal Society: Part 1. Esophagus. 2023;20:343–72.
Kitagawa Y, Ishihara R, Ishikawa H, et al. Esophageal cancer practice guidelines 2022 edited by the Japan esophageal society: Part 2. Esophagus. 2023;20:373–89.
Doki Y, Ajani JA, Kato K, et al. Nivolumab combination therapy in advanced esophageal squamous-cell carcinoma. N Engl J Med. 2022;386(5):449–62.
Sun JM, Shen L, Shah MA, et al. Pembrolizumab plus chemotherapy versus chemotherapy alone for first-line treatment of advanced oesophageal cancer (KEYNOTE-590): A randomised, placebo-controlled, phase 3 study. Lancet. 2021;398(10302):759–71.
Kato K, Cho BC, Takahashi M, et al. Nivolumab versus chemotherapy in patients with advanced oesophageal squamous cell carcinoma refractory or intolerant to previous chemotherapy (ATTRACTION-3): A multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20:1506–17.
Kojima T, Shah MA, Muro K, et al. Randomized phase III KEYNOTE-181 study of pembrolizumab versus chemotherapy in advanced esophageal cancer. J Clin Oncol. 2020;38(35):4138–48.
Yamamoto S, Kawakami H, Kii T, et al. Randomized phase II study of docetaxel versus paclitaxel in patients with esophageal squamous cell carcinoma refractory to fluoropyrimidine- and platinum-based chemotherapy: OGSG1201. Eur J Cancer. 2021;154:307–15.
Zhao X, Ivaturi V, Gopalakrishnan M, et al. A model-based exposure–response (E–R) assessment of a nivolumab (NIVO) 4-weekly (Q4W) dosing schedule across multiple tumor types. Cancer Res. 2017;77(13 Supplement):abstract CT101.
Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48(3):452–8.
Yamazaki N, Kiyohara Y, et al. Efficacy and safety of nivolumab in Japanese patients with previously untreated advanced melanoma: A phase II study. Cancer Sci. 2017;108(6):1223–30.
Oya Y, Yoshida T, Kuroda H, et al. Predictive clinical parameters for the response of nivolumab in pretreated advanced non-small- cell lung cancer. Oncotarget. 2017;8:103117–28.
Zhao X, Suryawanshi S, Hruska M, et al. Assessment of nivolumab benefit-risk profile of a 240-mg flat dose relative to a 3-mg/kg dosing regimen in patients with advanced tumors. Ann Oncol. 2017;28(8):2002–8.
Samlowski W, Robert NJ, Chen L, et al. Real-World nivolumab dosing patterns and safety outcomes in patients receiving adjuvant therapy for melanoma. Cancer Med. 2023;12(3):2378–88.
Bi Y, Liu J, Furmanski B, et al. Model-informed drug development approach supporting approval of the 4-week (Q4W) dosing schedule for nivolumab (Opdivo) across multiple indications: A regulatory perspective. Ann Oncol. 2019;30(4):644–51.
Long GV, Tykodi SS, et al. Assessment of nivolumab exposure and clinical safety of 480 mg every 4 weeks flat-dosing schedule in patients with cancer. Ann Oncol. 2018;29(11):2208–13.
Takahashi M, Kato K, Okada M, et al. Nivolumab versus chemotherapy in Japanese patients with advanced esophageal squamous cell carcinoma: A subgroup analysis of a multicenter, randomized, open-label, phase 3 trial (ATTRACTION-3). Esophagus. 2021;18:90–9.
Author information
Authors and Affiliations
Contributions
KK, YM, and SY contributed to the conception, design, and planning of the study. All authors contributed to the acquisition of data. YM, and SY contributed to the analysis of data. YM, SY, and YK contributed to the interpretation of results. All authors contributed to the drafting, or critical review and revision of the manuscript. All authors approved the final version to be submitted.
Corresponding author
Ethics declarations
Competing Interests
KK reports funding to the institution from Merck Sharp & Dohme Corp (MSD), Ono Pharmaceuticals, Bristol Myers Squibb (BMS), Beigene, Shionogi, Merck Biopharma, Oncolys BioPharma, Daiichi Sankyo, Novartis, Taiho Pharmaceutical, Janssen, AstraZeneca, and Chugai.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Murashima, Y., Yamamoto, S., Hirose, T. et al. Efficacy and Safety of Salvage-line Nivolumab Monotherapy for Advanced Esophageal Squamous Cell Carcinoma: Comparison of 240 mg Versus 480 mg Doses. J Gastrointest Canc 55, 1345–1351 (2024). https://doi.org/10.1007/s12029-024-01092-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-024-01092-w