Abstract
Introduction
Anemia is a common comorbidity of chronic kidney disease (CKD) that has been associated with increased risk of complications, healthcare expenditure, and reduced quality of life. In China, the treatment of anemia of CKD has been reported to be suboptimal in part because of a lack of awareness of the condition and its management. It is therefore important to raise awareness of the condition by estimating the future health and economic burden of anemia of CKD and also to understand how it may be addressed through proactive policies. This study aims to project the health and economic burden of anemia of CKD, in China, from 2023 to 2027 and to estimate the impact of a hypothetical intervention on related clinical and cost outcomes.
Methods
A virtual Chinese population was simulated using demographic, clinical, and economic statistics within a validated CKD microsimulation model. Each individual was assigned a CKD stage, anemia stage, comorbidity status (type 2 diabetes, hypertension), complication status (stroke, heart failure, and/or myocardial infarction), and a probability of receiving treatments and therapies. Annual direct healthcare costs were assigned and based on these factors. The hypothetical intervention reduced the prevalence of moderate and severe anemia by 5% annually. This hypothetical scenario was chosen to highlight the impact of implementing policies that could reduce anemia of CKD, and is aligned with the Healthy China 2030 policy, which aims to reduce mortality from noncommunicable diseases by 30%. Interventions could consist of early screening and intervention to reduce the escalation of anemia from mild to moderate or severe. Results were compared with a baseline “no change” scenario which reflects current trends.
Results
The number of patients with moderate/severe anemia of CKD was projected to increase from 3.0 to 3.2 million patients, with associated costs increasing from ¥22.0 billion (B) to ¥24.4B between 2023 and 2027, respectively. Compared with the no change scenario, the hypothetical intervention reduced the prevalence of moderate and severe anemia of CKD, saving ¥3.9B in healthcare costs in 2027 (¥24.4B vs ¥20.6B, respectively).
Conclusions
Consistent with trends in CKD burden in China, the prevalence of anemia of CKD is projected to increase, leading to greater related healthcare costs. The introduction of healthcare interventions designed to screen for and treat anemia more effectively could therefore reduce its future burden and related costs.
Plain Language Summary
Anemia, a common issue in chronic kidney disease, can lead to complications and increased healthcare costs. In China, anemia treatment for chronic kidney disease is often suboptimal because of a lack of awareness. This study aimed to estimate the future health and economic impact of anemia in chronic kidney disease in China from 2023 to 2027 and assess the effects of a hypothetical intervention. The research used a computer model to simulate a virtual Chinese population based on demographics, clinical data, and economic statistics. In the “no change” scenario, the prevalence of moderate/severe anemia in chronic kidney disease was projected to increase, with associated healthcare costs rising from ¥22.0B to ¥24.4B. A hypothetical intervention, reducing anemia prevalence by 5% annually, resulted in cost savings, lowering healthcare costs to ¥20.58B in 2027. In conclusion, anemia in chronic kidney disease is expected to increase in China, raising healthcare costs. Implementing interventions, such as early screening and treatment, could significantly reduce future burdens and related costs, emphasizing the need for proactive healthcare policies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The Inside ANEMIA of CKD microsimulation is a model that projects the future changes in epidemiology and cost of anemia of chronic kidney disease (CKD) to increase disease awareness and inform healthcare policy. |
We hypothesized that modeling the epidemiological and economic burden of anemia of CKD and its associated medical costs was feasible given data availability and microsimulation methods. |
Under the no change scenario, the prevalence of anemia of stage 3a–5 CKD in China was projected to rise by 8%, from 10.9 million to 11.8 million people, between 2023 and 2027, respectively. Cumulative events of the modeled comorbidities were high with large proportions of people with anemia of CKD living with heart failure, myocardial infarction, and/or stroke. |
The relatively large projected increase in prevalence of more pronounced anemia of stage 3a–5 CKD (moderate or severe as opposed to mild anemia) and an increase in related cardiovascular (CV) complications could increase the burden on healthcare services. |
The annual direct healthcare costs associated with anemia of CKD were projected to increase by 11.0%, from ¥64.5B to ¥71.6B, between 2023 and 2027, respectively. Compared with the no change scenario, the hypothetical intervention reduced the prevalence of moderate and severe anemia of CKD, offsetting medical costs by ¥3.9B in 2027 (¥24.4B vs ¥20.6B, respectively). |
This study projected the likely burden of anemia of CKD over the next 5 years and demonstrated a need for healthcare policy that promotes more efficient use of healthcare resources. |
Policy-driven interventions in China may include screening services and/or rapid adoption of innovative treatments such as hypoxia-inducible factor–prolyl hydroxylase inhibitors (HIF-PHI) to improve the management of this patient population and reduce the overall burden of anemia of CKD. |
Introduction
Chronic kidney disease (CKD), defined by the patient’s estimated glomerular filtration rate (eGFR) and urine albumin excretion rate (UACR), is a progressive disease and is graded from stage 1 to 5 [1]. Approximately 700 million people, roughly 9.1% of the global population, have CKD. In China, an estimated 122.7 million people, approximately 8.5% of the total population, have CKD [2]. Additionally, patients with pre-existing conditions, such as type 2 diabetes, obesity, and hypertension, are more likely to have CKD [4,5,6]. Patients with stage 5 CKD suffer from the most severe form of the disease and are most likely to be dependent on kidney replacement therapy (KRT), requiring hemodialysis, peritoneal dialysis, or a kidney transplant [1, 7]. Additionally, many patients are on a waiting list for KRT, with a waiting time longer than a year to obtain matched kidney [8, 9]. KRT is also associated with a significant economic burden in China, with each case of dialysis costing between $20,608 and $24,507 each year, and once an appropriate kidney is identified, a kidney transplant costs $23,320 [7].
Anemia of CKD, defined as a hemoglobin (Hb) level of less than 13.0 g/dl in male individuals and less than 12.0 g/dl in female individuals [10], is highly prevalent in patients with CKD. In China, over half of patients seeking specialist treatment for CKD had anemia [11]. Anemia in CKD can be present at any stage of the disease, but increases in prevalence and severity (mild, moderate, or severe) as eGFR declines [12]. For example, in a multicenter, cross-sectional study conducted in China including 2420 patients, 52% of people with CKD also had anemia, ranging from 22.4% of patients with stage 1 CKD to 90.2% of patients with stage 5 CKD [11]. A recently published 2023 national cohort study reported that 10.3% of people with CKD have moderate or severe anemia (Hb < 10 g/dL) increasing as CKD worsened from 4.0% in people with grade 3a CKD to 23.4% in those with grade 4 CKD [13].
Anemia of CKD is associated with debilitating symptoms, which contribute to a reduced quality of life (QoL) [14,15,16]. It is also associated with an increased risk of developing several serious complications, including myocardial infarction (MI), heart failure (HF), and stroke, and is also linked to higher rates of mortality [17, 18]. Consequently, anemia of CKD presents a high economic burden through increased healthcare utilization, costs of treatments to correct Hb levels, and the costs of associated comorbidities and complications [19, 20].
Treatment options for anemia of CKD that are included in the Kidney Disease Improving Global Outcomes (KDIGO) guidelines [10] are currently limited: the condition is typically treated with iron-replacement therapy or erythropoiesis-stimulating agents (ESAs), which supplement the insufficient levels of erythropoietin or iron, without fully addressing the underlying pathophysiological factors causing anemia in patients with CKD [10, 21]. Some of these treatments also come with risks. For example, iron supplements are known to lead to adverse effects in 35–60% of patients [22, 23]; iron administration can lead to toxicity. ESAs are associated with hyporesponsiveness and relatively low patient compliance due to the need for an injection, a challenge that an oral HIF-PHI would likely overcome [24,25,26]. Iron supplements show significantly reduced efficacy in patients with CKD due to elevated hepcidin concentrations, caused by attenuated kidney clearance, blockading intestinal iron absorption [27]. As a last resort, patients may be offered a blood transfusion, which is associated with an elevated risk of serious adverse events and may even make it more difficult for a future kidney transplant [28]. Physicians need to carefully consider the risk–benefit of administering these treatments to patients with anemia of CKD, and the outcome is that many people with CKD who are not dependent on dialysis may not be offered treatment for associated anemia [29].
In China, the treatment of anemia of CKD has been reported as suboptimal with only between 34% and 45% of patients receiving any treatment [11, 13]. In China there is currently no screening for anemia of CKD and low diagnosis rates. Compared with other countries, CKD treatment rate in China is very low, with only 44.9% of non-dialysis patients treated and the initiation of this treatment is late [11]. There are no specific guidelines in China for anemia of CKD, but clinical practice is based on European Best Practice Guidelines, Kidney Disease Outcomes Quality Initiative, World Health Organization (WHO) guidelines, and Chinese expert consensus [30]. It has been reported that treatment for anemia is more likely as CKD progresses [13] but as many as 23% of the patients have been reported not to receive any treatment until their Hb level reaches as low as 7 g/dL [11]. Among patients with stage 3–5 CKD with anemia, only 12% were reported to receive iron therapy, and 5% received ESA within 12 months after anemia was diagnosed [31]. Additionally, this treatment deficit may be driven, in part, by the patient’s lack of awareness of anemia and limited in-depth discussions with healthcare providers which would facilitate better management of CKD and optimization of treatment plans [32].
To overcome the risks associated with existing treatment options, a new oral treatment class, hypoxia-inducible factor (HIF) prolyl hydroxylase inhibitors (HIF-PHIs), has recently become available in China [33]. This class targets the physiological mechanism that underpins the pathophysiology of anemia of CKD, by inhibiting the degradation of HIF, a key mediator that modulates the body’s response to hypoxia [34]. In a systematic review and meta-analysis of non-dialysis patients with CKD, HIF-PHIs have been shown to significantly increase Hb levels (improving anemia); they also reduce hepcidin concentrations (reducing iron absorption in the intestines) and improve cholesterol with an acceptable safety profile and no increase in the incidence of treatment-emergent adverse events in patients treated with HIF-PHIs relative to ESAs or placebo in patients dependent on dialysis [35]. Additional studies show HIF-PHIs may also have cost-saving benefits and have been shown to be cost-effective [35].
In order to raise awareness and promote earlier diagnosis and management with current treatment or new innovative treatments such as HIF-PHIs, in line with national initiatives to improve population health, this study builds the quantitative evidence to demonstrate the epidemiological and economic outcomes if the number of moderate to severe anemia cases in China were reduced.
Methods
The study objectives were to further develop a validated anemia of CKD model [36,37,38] to quantify the health and economic burden of anemia of CKD between 2023 and 2027 in China, and to use this model to analyze the potential impact of a hypothetical intervention related to anemia in CKD. As this study did not use any primary clinical data but was based on published data and a virtual, modeled population, ethics approval was not required.
Microsimulation Model Overview
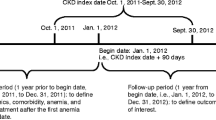
This study employed an individual patient-level microsimulation approach by modifying the Inside CKD validated microsimulation model that has previously been used to model CKD in 31 regions globally, and to model anemia of CKD in the USA, Canada, and the UK [36,37,38]. The microsimulation model is illustrated in Fig. 1. The model was adapted to include Chinese data and to represent the general population of China (including but not limited to those with CKD or anemia of CKD). Where Chinese data were not available, then data representing proxy countries were used, as specified. A list of data inputs and assumptions is shown in Supplemental Appendix S1.
The virtual population progressed through the microsimulation (Fig. 1), aging every year from the start year (2023) to the end year (2027). The microsimulation was designed to allow for dynamic population changes such as births and deaths, in line with national Chinese demographics [39]. Every individual in the microsimulation was assigned a probability of dying of an unspecified cause (unrelated to CKD) or specified cause (HF, stroke, or MI) in line with national statistics. Mortality rates by eGFR/UACR category were also applied, to determine an individual’s probability of dying according to their CKD stage.
The clinical status of each individual was updated on an annual basis. Each individual’s eGFR was stable or declined over time in line with their epidemiological status (e.g., age and health status), meaning that some individuals who did not have CKD at baseline developed CKD, and some individuals with CKD at baseline progressed into more advanced CKD stages.
Individuals in the CKD population were deemed to have a higher risk of cardiovascular complications than the non-CKD population in the model based on relative risks connecting CKD and related outcomes. As well, the likelihood of developing a relevant complication was assessed on an annual basis; therefore, HF, MI, and stroke risk increased as individuals’ eGFR temporally declined. Model outputs relating to the 20 million virtual population were extrapolated to represent the entire population of China.
Data Inputs
Population A virtual population (Fig. 1) was created to replicate the general population of China (0–110-year-olds) using national Chinese demographic statistics [39] . Within this broad population, the microsimulation included a representative proportion of individuals with CKD/anemia of CKD.
CKD status, CKD progression At the start of the microsimulation, each individual within the virtual population was tagged with age-sex-stratified eGFR, using cross-sectional Chinese data and UACR data representing a proxy country (Japan). Japan was selected on the basis of an algorithm developed for the Inside CKD project, as well as expert recommendations [40] (Supplementary Appendix S2).
These data were used to categorize individuals as having either no CKD or as having CKD, with a focus on stages 3a, 3b, 4, or 5 [41]. CKD stages were defined according to KDIGO categories: CKD stage 1 (eGFR ≥ 90 mL/min/1.73 m2, UACR ≤ 30 mg/24 h), stage 2 (eGFR = 60–89 mL/min/1.73 m2, UACR ≥ 30 mg/24 h), stage 3a (eGFR = 45–59 mL/min/1.73 m2, all UACR), stage 3b (eGFR = 30–44 mL/min/1.73 m2, all UACR), stage 4 (eGFR = 15–29 mL/min/1.73 m2, all UACR), and stage 5 (eGFR < 15 mL/min/1.73 m2, all UACR) [10, 42]. To account for differences in risk by age, eGFR values were distributed across ages and sexes on the basis of the age-sex distribution of a proxy country (UK).
In terms of CKD disease progression, projections of individual UACR levels were created using a multinomial static logistic regression model, based on measured trend data from annual health survey data (outlined in Supplemental Appendix S2). Rates of eGFR decline within the microsimulation were influenced by age, sex, anemia, and the presence of comorbidities, specifically type 2 diabetes (T2D), hypertension, and cardiovascular complications such as heart failure (HF), myocardial infarction, and stroke. These rates of eGFR decline were individually modeled according to the relevant characteristics of each virtual individual. These rates were based on a retrospective regression analysis of data from a comprehensive patient database, DISCOVER CKD [36]. As eGFR declined over time, individuals could develop a need for KRT. The thresholds used to define treatment pathways and other relevant parameters are shown in Supplemental Appendix S2 [43,44,45,46,47].
Anemia of CKD status Anemia levels for the Chinese population were obtained from Lin et al. [12]. These data defined anemia status, assigned according to the WHO criteria and measured in grams of hemoglobin per liter of blood: mild (11.0–12.99 g/dl in men, 11.0–11.99 g/dl in non-pregnant women), moderate (8.0–10.99 g/dl in both men and non-pregnant women), or severe (< 8.0 g/dl in both men and non-pregnant women); see Supplemental Appendix S2 [42].
Complications and Comorbidities
A range of relevant complications and comorbidities were assigned to each virtual individual of the microsimulation population.
The virtual population were stratified into those with T2D, hypertension, or both, at baseline.
The proportion of people with CKD with T2D and hypertension was obtained from China-specific sources [44, 48,49,50]. More details are shown in Supplemental Appendix S2.
Similarly, the presence of HF, MI, and stroke was assigned to each individual in line with China-specific data sources described in more detail in Supplemental Appendix S2 [51, 52]. Each individual was also assigned a relative risk of developing complications as a result of their eGFR and UACR categories, using globally relevant data sources [52, 53]. Each individual was assigned a probability of receiving ESAs, intravenous iron infusions, and red blood cell transfusions, based on CKD stage. More details are shown in Supplemental Appendix S2.
Health Economic Data
The health economic module employed a semi-Markov-type simulation to quantify the direct costs due to anemia in CKD by stage and related complications (dialysis [9]; kidney transplant [54]; HF [55]; MI [55, 56]; and stroke [57]) by assigning an annual healthcare cost to each individual in the model depending on their health status [58]. Healthcare costs were derived from the published literature (Supplementary Appendix S2). The direct costs of anemia include the cost associated with screening, examination, and treatment (including costs of iron replacement, ESA, blood transfusion proportioned according to values in Table 18 of Supplementary Appendix S2); the intervention reduced anemia prevalence and therefore the direct costs savings could be quantified. Cost prices of different units or volumes were corrected for inflation between the year of the data and start year of the microsimulation by inflating costs. Limited data on HIF-PHI price were available at the time of analysis, so data relating to use of this treatment option was not included in this analysis.
“No Change” and Hypothetical “Intervention” Scenarios
The “no change” baseline projected changes in outcomes over the 5-year time horizon if no changes were made to the management of anemia of CKD in China. The 5-year timeframe reflects an appropriate period to track and capture key clinical outcomes as well as to identify pivot points for health policy interventions [59]. Five years is also the approximate length of a typical political term of office across the legislative and administrative bodies in China, so this work is helpful for policy planning across that period. The “no change” scenario was compared with a hypothetical “intervention” scenario where there was a 5% annual reduction in the prevalence of moderate and severe anemia from 2023 to 2027. The intervention was designed to be aligned with the Healthy China 2030 policy which aims to reduce mortality from noncommunicable diseases such as diabetes, a risk factor of CKD, by 30% [60,61,62]. The focus on impacting moderate and severe anemia of CKD was chosen because of the feasibility of a range of interventions (e.g., HIF-PHIs) that might reduce the risk of escalation of anemia from mild to moderate and severe. All individuals with anemia of CKD had a probability of being subject to the intervention. If an individual’s anemia level changed as a result of the hypothetical intervention, their probability of receiving ESAs, intravenous iron infusions, and red blood cell transfusions changed in line with anemia status. Their change in anemia level did not impact CKD-related complications or renal function in the model.
Model Outputs
The prevalence and incidence of relevant endpoints were projected year-on-year over a 5-year horizon (2023–2027). Data outputs reflected these endpoints and included:
-
Annual burden of anemia in CKD by stage (3–5), and by comorbidity
-
Annual incidence of HF, MI, and stroke in patients with anemia of CKD
-
Annual direct and management costs of anemia in CKD
These endpoints were also quantified for the intervention scenario, and the difference between the no change scenario and the intervention scenario was quantified and expressed in terms of prevalence and costs avoided. The analysis focused on projections related to moderate and severe anemia, and CKD stages 3a to 5, where the burden is greatest.
Model Validation
The microsimulation underwent model validations. Face validity was ensured by validating all inputs and outputs of the model with expert nephrologists. Additionally, the assumptions of the CKD model were based on the best available peer-reviewed papers, with Chinese data where available (Supplemental Table S3). Internal validity was confirmed by checking the accuracy of coding using GitHub as version control and unit testing by two coders. Cross validity was confirmed by comparing results with other models analyzing the same problem (as exemplified in Garcia Sanchez et al. [63], in which the microsimulation and Markov modeling approaches were compared). The external validity of the microsimulation assumptions was conducted by comparing model results with real-world results in a test country [36].
Ethics
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Results
Prevalence of Anemia with CKD in China
Under the no change scenario, the number of people with anemia of CKD (CKD 3–5) in China (overall regardless of severity of anemia) was projected to rise by 8.0%, from 10.9 million to 11.8 million people, between 2023 and 2027, respectively. The prevalence of moderate and severe anemia was projected to increase by 7.7%, from 3.0 to 3.3 million people by 2027 (Fig. 2).
Projected prevalence of moderate and severe anemia of CKD in China by CKD stage between 2023 and 2027. Anemia severity was categorized into mild, moderate, or severe, consistent with KDIGO definition of anemia in CKD and with WHO guidelines [10, 42]. Only moderate and severe anemia of CKD are represented here. CKD stage was categorized according to KDIGO definition [1]. CKD chronic kidney disease, KDIGO Kidney Disease Improving Global Outcomes, WHO World Health Organization
Incidence of Complications Related to Anemia of CKD
Under the no change scenario, the prevalence of HF, MI, and stroke was high in the anemia of CKD population. In 2023, the model estimated the prevalence of HF in the anemia of CKD population at 1.0 million, MI at 3.2 million, and stroke at 1.1 million, regardless of severity, in China. Between 2023 and 2027, the prevalence of HF among people with anemia of CKD was projected to increase by 16.2% to 1.20 million cases. MI and stroke were projected to increase by 5.4% (to 3.4 million cases) and 8.7% (to 1.2 million) respectively, in people with anemia of CKD (Fig. 3).
Projected increase in complications associated with moderate and severe anemia of CKD, in China between 2023 and 2027. Severity of anemia (moderate or severe), defined according to KDIGO [10] and WHO guidelines [42]. Stratified by CKD stage, categorized according to KDIGO definition [10]. CKD chronic kidney disease, WHO World Health Organization, KDIGO Kidney Disease Improving Global Outcomes
Costs
Under the no change scenario, the annual direct healthcare costs associated with anemia of CKD were projected to increase by 11.0%, from ¥64.5B to ¥71.6B, between 2023 and 2027, respectively. Direct costs associated with treatment of moderate and severe anemia of CKD were ¥22.0B in 2023 and were projected to rise to ¥24.4B by 2027; an increase of 11.3%. Stratification by stage of CKD identified that people in more progressive stages of CKD (stages 4 and 5) accounted for more than half the costs associated with anemia of CKD (Fig. 4).
Annual costs for patients with diagnosed CKD and moderate and severe anemia in China. Showing overall costs of treating anemia of CKD regardless of severity (a, b), and costs associated with treating moderate and severe anemia only (c, d). No change scenario (a, c); intervention scenario in which prevalence of moderate and severe anemia of CKD decreases by 5% year on year (b, d). The dotted line, presented to aid comparison, represents the projected costs by 2027 under the no change scenario. CKD chronic kidney disease
Similarly, under the no change scenario, the costs associated with managing anemia of CKD with intravenous iron infusion, red blood cell transfusions, and ESAs were projected to increase by 7.6%, 7.7%, and 7.5% respectively, in China, between 2023 and 2027 (Fig. 5).
Healthcare costs associated with complications of anemia of CKD were also projected to increase between 2023 and 2027 under the no change scenario. Healthcare costs associated with HF in the anemia of CKD population in China were projected to increase by 17.2%, from ¥33.7B to ¥39.5B, between 2023 and 2027, respectively. The costs of HF in patients with moderate and severe anemia of CKD accounted for ¥9.5B in 2023, and ¥11.2B in 2027. Healthcare costs associated with MI in the anemia of CKD population in China were projected to increase by 6.5%, from ¥89.7B to ¥95.5B, between 2023 and 2027, respectively. The costs of MI in patients with moderate and severe anemia of CKD accounted for ¥25.4 in 2023, and ¥27.1 in 2027.
Healthcare costs associated with stroke in the anemia of CKD population in China were projected to increase by 10.0% from ¥13.4B to ¥14.7B, between 2023 and 2027, respectively. The costs of stroke in patients with moderate and severe anemia of CKD accounted for ¥3.9B in 2023, and ¥4.3B in 2027.
Intervention Results
Under the hypothetical scenario, the number of people with anemia of CKD (CKD 3–5) in China (overall regardless of severity of anemia) was projected to increase (from 10.9 million in 2023) to 11.2 million people in 2027 (versus 11.8 million in the no change scenario). More specifically, the prevalence of moderate and severe anemia was projected to decrease from 3.0 million people in 2023 to around 2.7 million by 2027 in the intervention scenario (versus an increase to 3.3 million people in the no change scenario).
The intervention scenario resulted in a cost saving from ¥22.0B to ¥20.6B. When compared to the no change scenario (in which costs increased from ¥22.0B to ¥24.4B), this represents a cumulative saving of ¥3.9B in direct healthcare costs (Fig. 4) equating to a 18.7% decrease in associated direct costs in the population with moderate and severe anemia of CKD by 2027. The greatest cost reduction from the modeled scenario was in those with moderate and severe anemia of CKD; similarly, the direct healthcare costs in the entire anemic CKD population reduced by 5.9% from ¥71.7B to ¥67.5 in 2027. Cost savings were primarily driven by a reduction in the costs of managing moderate and severe anemia of CKD in people with CKD stages 3 to 5.
Overall, under the intervention scenario, costs of managing anemia of CKD increased at a slower rate, from ¥62.4B to ¥67.5B, an increase of 8.0%. This increase was less than projected in the no change scenario (11.1%) from ¥64.5B to ¥71.7.
Discussion
To our knowledge, this is the first modeling study to project the health and economic burden of mild, moderate, and severe anemia of CKD in China and to quantify the impact of proactive management of anemia via a hypothetical intervention which would improve the management of anemia of CKD over the next 5 years. Assuming the status quo, the number of patients with CKD with moderate and severe anemia in China was projected to increase from 3.0 to 3.2 million patients, with associated costs increasing from ¥22.0B to ¥24.4B, between 2023 and 2027, respectively. Under a hypothetical intervention, the number of people with moderate and severe anemia in China fell to 2.7 million. Associated costs were ¥3.9B lower than in the no change scenario, by 2027. This may represent a call for action for more effective management of anemia of CKD in China. Such action would be consistent with the Healthy China 2030 initiative [64,65,66,67]. This national program aims to shift the focus of health services from disease treatment to health promotion and health management. Elements of this initiative could include robust screening programs as well as an emphasis on the primary prevention of NCDs such as obesity and diabetes, which are closely associated with CKD, and the wider public health policies which might address them [64]. Initiation of policies to tackle the burden of CKD, including anemia of CKD would be consistent with this wider, national level initiative.
Our modeled prevalence data are aligned with the literature. Historical trends for China indicated a growth in the prevalence of CKD between 1990 and 2019, likely driven, at least in part, by increasing rates of obesity and diabetes [60, 68, 69], as well as a shift in the distribution of CKD cases towards more severe stages [2]. Diabetes can cause microvascular and macrovascular complications, which in the kidney often lead to CKD [70]. Furthermore, the prevalence of CKD was previously projected to increase further between 2020 (10.7%) and 2029 (11.7%), using ARIMA models [71].
Compared with no change, the hypothetical intervention resulted in a saving of ¥3.9B in healthcare costs in 2027. In the no change scenario, these costs were disproportionately driven by the management of people in more progressive stages of CKD (stages 4 and 5) [35]. This was not only due to the high burden of anemia of CKD in later stages but also that current treatment patterns are skewed towards treating patients with later stage CKD and more severe of anemia of CKD. Interventions aimed at increasing awareness of anemia of CKD and improving access and adherence to therapies at earlier stages of CKD, such as stage 3, have previously been shown to be cost-effective [35] owing to improved health outcomes. Our data therefore supports the more proactive management of anemia of CKD and the value of earlier intervention to prevent progression to more advanced stages of CKD, which are associated with higher costs.
This study has several strengths: this study used a well-validated microsimulation method that captured the heterogeneity of disease progression in patients with anemia of CKD. Microsimulation modeling is an important complement to clinical studies since it enables population-level analysis to be carried out and expected outcomes to be projected into the future using a wide range of data sources. This makes microsimulation very versatile. Scenarios can be carried out that may not be feasible in real-world population-level settings.
The model incorporated data from multiple sources, including epidemiological studies, published datasets, and observational data, which were validated by experts. This study was able to extract the most recent and representative data to accurately replicate the population of China. Using the best available data, this study was able to include subgroups of patients with CKD, with moderate and severe anemia who have different characteristics from other subgroups, and who may benefit most from specific interventions. Finally, while the majority of comparable models in the literature identified focused on the cost-effectiveness of interventions rather than the burden of disease [35, 72,73,74,75], our microsimulation model was able to track changes in individual health status over time so that the human burden could also be considered.
Some limitations were apparent. Although the best data available was utilized where possible, data gaps still existed, for example, the availability of Chinese-specific epidemiological inputs by anemia level such as mortality, relative risks of complications and new treatments. In addition, some treatment costs were not included in the total costs, as the price is changed every 2 years via national price negotiation. Price reduction has in the past varied significantly from a few percent to as much as a 94% increase [76] and so was not possible to model. However, the data gaps were mitigated by applying a proxy country algorithm to select the most appropriate alternative data source. For MI incidence data we used a Japan proxy. We used modeled IHME data for stroke incidence data which is often underestimated [77]. Further, recent real-world data confirmed that our stroke estimates may be conservative and consequently this might explain why MI cases exceed stroke cases in this study [78]. Relative risks of complications were available for eGFR and albuminuria but these were not available for anemia. The model could be adapted to include more China-specific data sources when they become available. It was beyond the scope of this study to include quality of life estimates; nevertheless, the microsimulation is flexible so can be adapted to include measures of quality life improvements because of better anemia management.
Predictive models rely on modeling epidemiological assumptions where evidence is not available in the literature, which can introduce a level of uncertainty into the results. However, this was mitigated by validating the model assumptions with experts, conducting sensitivity analyses, and comparing the results against published literature where possible. The intervention modeled was a hypothetical reduction in anemia. No specific strategy was modeled, but we recommend that one way to reach a 5% reduction would be earlier screening, diagnosis, and proactive management of anemia of CKD. While this study is specific to the population of China, the model can easily be adapted to other countries and regions where different trends in anemia of CKD may be observed.
Conclusions
Achieving a 5% annual reduction in the prevalence of moderate and severe anemia in CKD could result in a reduction in the cost of the condition by 5.9% overall. To do this, interventions such as earlier screening, diagnosis, and effective treatment are needed. There is the potential to align more robust screening with easier access to innovative treatments such as HIF-PHIs; the Healthy China 2030 initiative provides a useful opportunity for advocating for action to reduce anemia of CKD. The economic implications of reducing the burden of this condition should be considered by policymakers, practitioners, and government payers in China to advocate for, and leverage, policy change in order to improve patient health.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
KDIGO 2012. Clinical practice guideline for the evaluation and management of chronic kidney disease. https://kdigo.org/wp-content/uploads/2017/02/KDIGO_2012_CKD_GL.pdf. Accessed 20 Feb 2023.
Mennini FS, Cabrera C, Card-Gowers J, et al. Inside CKD: projecting the economic burden of chronic kidney disease using patient-level microsimulation modelling. [Poster] 2021. https://www.healthlumen.com/wp-content/uploads/2022/06/posb68-inside-ckdispor-eucost-burdenposterrevised-submission-pdf.pdf. Accessed 22 Apr 2024.
GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395(10225):709–33.
Chang A, Kramer H. CKD progression: a risky business. Nephrol Dial Transpl. 2012;27(7):2607–9.
Vivante A, Golan E, Tzur D, et al. Body mass index in 1.2 million adolescents and risk for end-stage renal disease. Arch Intern Med. 2012;172(21):1644–50.
Ku E, Lee BJ, Wei J, Weir MR. Hypertension in CKD: core curriculum 2019. Am J Kidney Dis. 2019;74(1):120–31.
Jha V, Al-Ghamdi SMG, Li G, et al. Global economic burden associated with chronic kidney disease: a pragmatic review of medical costs for the inside CKD research programme. Adv Ther. 2023;40:4405.
Chen L, Cheng J, Qiu T, et al. Clinical research progress on xenogeneic kidney transplantation. Pract J Organ Transpl (Electronic Version). 2023;11(2):171–4.
Wang F, Yang C, Long J, et al. Executive summary for the 2015 Annual Data Report of the China Kidney Disease Network (CK-NET). Kidney Int. 2019;95(3):501–5.
KDIGO. KDIGO Clinical practice guideline for anemia in chronic kidney disease. https://kdigo.org/wp-content/uploads/2016/10/KDIGO-2012-Anemia-Guideline-English.pdf Accessed 20 Feb 2023. 2012.
Li Y, Shi H, Wang WM, et al. Prevalence, awareness, and treatment of anemia in Chinese patients with nondialysis chronic kidney disease: first multicenter, cross-sectional study. Medicine (Baltimore). 2016;95(24):e3872.
Lin P, Ding X-Q, Yuan M, Liu H. A cross-sectional study on anemia and its risk factors in chronic kidney disease. Fudan Univ J Med Sci. 2009;36(5):562–5.
Shen Y, Wang J, Yuan J, et al. Anemia among Chinese patients with chronic kidney disease and its association with quality of life—results from the Chinese cohort study of chronic kidney disease (C-STRIDE). BMC Nephrol. 2021;22(1):64.
Eriksson D, Goldsmith D, Teitsson S, Jackson J, van Nooten F. Cross-sectional survey in CKD patients across Europe describing the association between quality of life and anaemia. BMC Nephrol. 2016;17(1):97.
Hoshino J, Muenz D, Zee J, et al. Associations of hemoglobin levels with health-related quality of life, physical activity, and clinical outcomes in persons with stage 3–5 nondialysis CKD. J Ren Nutr. 2020;30(5):404–14.
van Haalen H, Jackson J, Spinowitz B, Milligan G, Moon R. Impact of chronic kidney disease and anemia on health-related quality of life and work productivity: analysis of multinational real-world data. BMC Nephrol. 2020;21(1):88.
Krishnan AR, Trinder D, Chua ACG, Chakera A, Ramm GA, Olynyk J. Anaemia of chronic kidney disease: what we know now. J Renal Hepat Disord. 2017;1(1):11–9.
Yamamoto H, Nishi S, Tomo T, et al. 2015 Japanese Society for Dialysis Therapy: guidelines for renal anemia in chronic kidney disease. Ren Replace Ther. 2017;3(1):1–46.
Wish J, Schulman K, Law A, Nassar G. Healthcare expenditure and resource utilization in patients with anaemia and chronic kidney disease: a retrospective claims database analysis. Kidney Blood Press Res. 2009;32(2):110–8.
Pergola PE, Pecoits-Filho R, Winkelmayer WC, et al. Economic burden and health-related quality of life associated with current treatments for anaemia in patients with CKD not on dialysis: a systematic review. Pharmacoecon Open. 2019;3(4):463–78.
Locatelli F, Del Vecchio L. An expert opinion on the current treatment of anemia in patients with kidney disease. Expert Opin Pharmacother. 2012;13(4):495–503.
Barton JC, Barton EH, Bertoli LF, Gothard CH, Sherrer JS. Intravenous iron dextran therapy in patients with iron deficiency and normal renal function who failed to respond to or did not tolerate oral iron supplementation. Am J Med. 2000;109(1):27–32.
Henry DH, Dahl NV, Auerbach M, Tchekmedyian S, Laufman LR. Intravenous ferric gluconate significantly improves response to epoetin alfa versus oral iron or no iron in anemic patients with cancer receiving chemotherapy. Oncologist. 2007;12(2):231–42.
Kaplan JM, Sharma N, Dikdan S. Hypoxia-inducible factor and its role in the management of anemia in chronic kidney disease. Int J Mol Sci. 2018;19(2):389.
FDA. FDA Drug Safety Communication: Modified dosing recommendations to improve the safe use of Erythropoiesis-Stimulating Agents (ESAs) in chronic kidney disease. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-modified-dosing-recommendations-improve-safe-use-erythropoiesis. Accessed 20 Feb 2023. 2017.
Palmer SC, Saglimbene V, Mavridis D, et al. Erythropoiesis-stimulating agents for anaemia in adults with chronic kidney disease: a network meta-analysis. Cochrane Database Syst Rev. 2014;2014(12):CD010590.
Gutiérrez OM. Treatment of iron deficiency anemia in CKD and end-stage kidney disease. Kidney Int Rep. 2021;6(9):2261–9.
Leffell MS, Kim D, Vega RM, et al. Red blood cell transfusions and the risk of allosensitization in patients awaiting primary kidney transplantation. Transplantation. 2014;97(5):525–33.
St Peter WL, Guo H, Kabadi S, et al. Prevalence, treatment patterns, and healthcare resource utilization in Medicare and commercially insured non-dialysis-dependent chronic kidney disease patients with and without anemia in the United States. BMC Nephrol. 2018;19(1):67.
Chinese Experts Group of the Guideline for the Management of ‘CKD-PeriDialysis’, Chinese Non-government Medical Institutions Association. Chinese clinical practice guideline for the management of “CKD-PeriDialysis”—the periods prior to and in the early-stage of initial dialysis. Kidney Int Rep. 2022;7(12 Suppl):S531–S58.
Chai YF, Lin HB, Ding GH, et al. Prevalence and treatment of anemia in chronic kidney disease patients based on regional medical big data. Zhonghua Liu Xing Bing Xue Za Zhi. 2023;44(7):1046–53.
Hao CM, Wittbrodt ET, Palaka E, Guzman N, Dunn A, Grandy S. Understanding patient perspectives and awareness of the impact and treatment of anemia with chronic kidney disease: a patient survey in China. Int J Nephrol Renovasc Dis. 2021;14:53–64.
Nephrology Physicians Branch of Chinese Medical Doctor Association Nephrology Guidelines Working Group. Clinical practice guidelines for the diagnosis and treatment of renal anemia in China. Chin Med J. 2021;101:1463–502.
Haase VH. Hypoxia-inducible factor-prolyl hydroxylase inhibitors in the treatment of anemia of chronic kidney disease. Kidney Int Suppl. 2021;11(1):8–25.
Hu Z, Tao H, Shi A, Pan J. The efficacy and economic evaluation of roxadustat treatment for anemia in patients with kidney disease not receiving dialysis. Expert Rev Pharmacoecon Outcomes Res. 2020;20(4):411–8.
Tangri N, Chadban S, Cabrera C, Retat L, Sánchez JJG. Projecting the epidemiological and economic impact of chronic kidney disease using patient-level microsimulation modelling: rationale and methods of inside CKD. Adv Ther. 2023;40(1):265–81.
Retat L, Webber L, Garcia Sanchez JJ, et al. Quantifying the epidemiological burden of anemia of CKD in the USA and Canada via microsimulation modelling. 2021. https://www.healthlumen.com/wp-content/uploads/2022/04/NKF-Inside-ANEMIA-of-CKD-EPI-burden-US-and-CANADA.pdf. Accessed 22 Apr 2024.
Garcia Sanchez JJ, et al. Inside Anemia of CKD: Quantifying the epidemiological burden of anemia of CKD in Canada via microsimulation modelling. https://www.sciencedirect.com/science/article/pii/S2468024921004824#:~:text=Inside%20ANEMIA%20of%20CKD%20is,disease%20will%20increase%20in%20parallel. Accessed Dec 2023.
United Nations. UN World Population Prospects data. https://population.un.org/wpp/. Accessed 21 Feb 2023.
Zhang L, Wang F, Wang L, et al. Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet. 2012;379(9818):815–22.
Portolés J, Martín L, Broseta JJ, Cases A. Anemia in chronic kidney disease: from pathophysiology and current treatments, to future agents. Front Med (Lausanne). 2021;8:642296.
World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Geneva: World Health Organization; 2011 2011. Contract No.: WHO/NMH/NHD/MNM/11.1.
国家肾脏病医疗质量控制中心 [Internet]. http://www.cnrds.net/TxLogin. Accessed 22 Feb 2023.
Zhang L, Zhao MH, Zuo L, et al. China Kidney Disease Network (CK-NET) 2015 annual data report. Kidney Int Suppl (2011). 2019;9(1):e1–81.
Xue W, Tian P, Xiang H, et al. Outcomes for primary kidney transplantation from donation after citizens’ death in China: a single center experience of 367 cases. BMC Health Serv Res. 2017;17(1):250.
Yin H, Yusheng Y. [Peritoneal dialysis opportunity and challenge]. http://qikan.cqvip.com/Qikan/Article/Detail?id=664763526. Accessed 22 Feb 2022.
Watanabe Y, Yamagata K, Nishi S, et al. Japanese society for dialysis therapy clinical guideline for “hemodialysis initiation for maintenance hemodialysis.” Ther Apher Dial. 2015;19(Suppl 1):93–107.
Yang C, Gao B, Zhao X, et al. Executive summary for China Kidney Disease Network (CK-NET) 2016 annual data report. Kidney Int. 2020;98(6):1419–23.
Zhang L, Zuo L. Current burden of end-stage kidney disease and its future trend in China. Clin Nephrol. 2016;86(13):27–8.
NHS Digital. Health Survey for England, 2016. https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/health-survey-for-england-2016. Accessed 22 Feb 2023.
Sun XQ, Li JS, Lang YJ, et al. Investigation of epidemiologic features and treatment of chronic heart failure in some rural parts of Liaoning province. Chin J Pract Intern Med. 2009;29(11):1000–2.
Institute for Health Metrics and Evaluation. Global burden of disease. http://www.healthdata.org/ Accessed 22 Feb 2023.
Masson P, Webster AC, Hong M, Turner R, Lindley RI, Craig JC. Chronic kidney disease and the risk of stroke: a systematic review and meta-analysis. Nephrol Dial Transpl. 2015;30(7):1162–9.
Zhao W, Zhang L, Han S, et al. Cost analysis of living donor kidney transplantation in China: a single-center experience. Ann Transpl. 2012;17(2):5–10.
Huang J, Yin H, Zhang M, Ni Q, Xuan J. Understanding the economic burden of heart failure in China: impact on disease management and resource utilization. J Med Econ. 2017;20(5):549–53.
Yuan-yuan LIU, Jun MA, Chang-ping LI. Hospitalization expense and its influencing factors among myocardial infarction patients. China Public Heal. 2013;29(3):322–24. https://doi.org/10.11847/zgggws2013-29-03-05.
Zhu D, Shi X, Nicholas S, et al. Medical service utilization and direct medical cost of stroke in urban China. Int J Health Policy Manag. 2022;11(3):277–86.
Zheng X, Zhang JCL. Disease composition and medical expenses of chronic kidney disease in People’s Hospital of Xinjiang uygur autonomous region from 2012 to 2017: a cross-sectional survey. Chin J Evid Based Med. 2018;18(9).
Hill KG, Woodward D, Woelfel T, Hawkins JD, Green S. Planning for long-term follow-up: strategies learned from longitudinal studies. Prev Sci. 2016;17(7):806–18.
Peng W, Chen S, Chen X, et al. Trends in major non-communicable diseases and related risk factors in China 2002–2019: an analysis of nationally representative survey data. Lancet Region Health Western Pac. 2023;43:100809.
Quan J, Zhao Z, Wang L, et al. Potential health and economic impact associated with achieving risk factor control in Chinese adults with diabetes: a microsimulation modelling study. Lancet Regional Health Western Pac. 2023;33:100630.
Jiang Y, Guo H, Zhang W, et al. Gaps and directions in addressing non-communicable and chronic diseases in China: a policy analysis. Int J Environ Res Public Health. 2022;19(15):9761.
Garcia Sanchez JJ, Xu M, Sorstadius E, et al. Estimating the Burden of Chronic Kidney Disease (CKD) in the UK: comparison of two health economic analysis methods. Nephrol Dial Transpl. 2020;35(Suppl 3).
Tan X, Liu X, Shao H. Healthy China 2030: a vision for health care. Value Health Reg Issues. 2017;12:112–4.
Goodchild M, Zheng R. Tobacco control and Healthy China 2030. Tob Control. 2019;28(4):409–13.
Jiang Z, Jiang W. Health education in the healthy China initiative 2019–2030. China CDC Wkly. 2021;3(4):78–80.
Wang L, Wang H, Wang Z, et al. Interpretation of healthy diet campaign in healthy China initiative 2019–2030. China CDC Wkly. 2021;3(16):346–9.
Jian Y, Zhu D, Zhou D, et al. ARIMA model for predicting chronic kidney disease and estimating its economic burden in China. BMC Public Health. 2022;22(1):2456.
Zhang L, Long J, Jiang W, et al. Trends in chronic kidney disease in China. N Engl J Med. 2016;375(1):905–6.
Anders HJ, Huber TB, Isermann B, Schiffer M. CKD in diabetes: diabetic kidney disease versus nondiabetic kidney disease. Nat Rev Nephrol. 2018;14(6):361–77.
Li Y, Ning Y, Shen B, et al. Temporal trends in prevalence and mortality for chronic kidney disease in China from 1990 to 2019: an analysis of the Global Burden of Disease Study 2019. Clin Kidney J. 2023;16(2):312–21.
Yarnoff BO, Hoerger TJ, Simpson SA, et al. The cost-effectiveness of anemia treatment for persons with chronic kidney disease. PLoS ONE. 2016;11(7):e0157323.
McEwan P, Darlington O, Miller R, et al. Cost-effectiveness of dapagliflozin as a treatment for chronic kidney disease: a health-economic analysis of DAPA-CKD. Clin J Am Soc Nephrol. 2022;17(12):1730–41.
Naci H, de Lissovoy G, Hollenbeak C, et al. Historical clinical and economic consequences of anemia management in patients with end-stage renal disease on dialysis using erythropoietin stimulating agents versus routine blood transfusions: a retrospective cost-effectiveness analysis. J Med Econ. 2012;15(2):293–304.
Thaweethamcharoen T, Sakulbumrungsil R, Nopmaneejumruslers C, Vasuvattakul S. Cost-utility analysis of erythropoietin for anemia treatment in thai end-stage renal disease patients with hemodialysis. Value Health Reg Issues. 2014;3:44–9.
National Healthcare Security Administration. Homepage 2023. http://www.nhsa.gov.cn/. Accessed 22 Apr 2024.
Institute for Health Metrics and Evaluation (IHME). IHME Client Services: Our Data 2023. https://www.ihmeclientservices.org/ihmedata.html. Accessed 22 Apr 2024.
Wang YJ, Li ZX, Gu HQ, et al. China stroke statistics 2019: a report from the National Center for Healthcare Quality Management in Neurological Diseases, China National Clinical Research Center for Neurological Diseases, the Chinese Stroke Association, National Center for Chronic and Non-communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention and Institute for Global Neuroscience and Stroke Collaborations. Stroke Vasc Neurol. 2020;5(3):211–39.
Medical Writing, Editorial, and Other Assistance
Editorial support was provided by Jenny Smith, JMS Medical Writing Service Ltd. Markiyan Mitchyn and John Guzek provided additional editorial support, who have received support from HealthLumen Limited.
Funding
HealthLumen Limited received funding from AstraZeneca to cover all costs and the journal’s Rapid Service and Open Access fees.
Author information
Authors and Affiliations
Contributions
Laura Webber, Lise Retat, Susan Grandy, Claudia Cabrera, and Juan Jose Garcia Sanchez developed the study protocol. Lise Retat and Alexander Martin carried out the analysis. Dunming Xiao, Joshua Card-Gowers, and Alexander Martin collected the data. Juan Jose Garcia Sanchez, Susan Grandy, and Lise Retat developed scenario assumptions. Yuzheng Zhang, Jiaqi Yao, Naveen Rao, Yuzheng Zhang, Yiqing Wu, Jianwei Xuan, Zuo Li, and Chalet Zhang, reviewed and validated the data inputs and provided policy context. Joshua Card-Gowers and Lise Retat drafted the initial manuscript, all authors reviewed and approved the manuscript prior to submission.
Corresponding authors
Ethics declarations
Conflict of Interest
Jiaqi Yao, Yuzheng Zhang, Chalet Zhang, Juan Jose Garcia Sanchez, Claudia Cabrera, Dunming Xiao, Naveen Rao and Susan Grandy are employees of AstraZeneca at the time of the study. Yiqing Wu is an employee of Fibrogen. Laura Webber, Alex Martin and Joshua Card-Gowers are employees of HealthLumen Limited which has received research support from AstraZeneca. Lise Retat was an employee at HealthLumen Limited at the time of the study, and is now employed at AstraZeneca. Zuo Li and Jianwei Xuan have nothing to disclose.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors. Therefore, ethics approval was not required.
Additional information
Lise Retat was affiliated with HealthLumen Limited at the time of the study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Retat, L., Xiao, D., Webber, L. et al. Inside ANEMIA of CKD: Projecting the Future Burden of Anemia of Chronic Kidney Disease and Benefits of Proactive Management: A Microsimulation Model of the Chinese Population. Adv Ther 41, 3905–3921 (2024). https://doi.org/10.1007/s12325-024-02863-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-024-02863-4