Abstract
Introduction
The Nucala Effectiveness Study (NEST) assessed the effectiveness of mepolizumab in patients with severe asthma (SA) in countries previously underrepresented in real-world studies.
Methods
A multi-country, bi-directional, self-controlled, observational cohort study conducted in Colombia, Chile, India, Türkiye, Saudi Arabia, United Arab Emirates, Kuwait, Oman, and Qatar. Historical and/or prospective data from patients with SA were assessed 12 months pre- and post-mepolizumab initiation. Primary endpoint: incident rate ratio (IRR) of clinically significant exacerbations (CSEs). Key secondary endpoints: healthcare resource utilisation (HCRU), oral corticosteroid (OCS) use, lung function and symptom control (Asthma Control Test [ACT] scores).
Results
Overall, 525 patients with SA burden pre-initiation (geometric mean blood eosinophil count [BEC] 490.7 cells/µl; 31.4% prior biologic use; 37.3% obese) received at least one dose of mepolizumab 100 mg subcutaneously. Post-initiation, a significant reduction in CSEs was observed (76% [p < 0.001]; IRR [95% confidence interval] 0.24 [0.19–0.30]); 72.0% of patients had no CSEs. Mepolizumab treatment led to a reduction in OCS use (52.8% pre-initiation vs. 16.6% post-initiation) and a mean (standard deviation [SD]) change in OCS dose of − 18.1 (20.7) mg post-initiation; 36.1% of patients became OCS-free. Fewer patients were hospitalised post-initiation (22.5% pre-initiation vs. 6.9% post-initiation). Improvements in mean (SD) forced expiratory volume in 1 s (62.8 [20.2]% pre-initiation vs. 73.0 [22.7]% post-initiation) and ACT scores (15.0% pre-initiation vs. 64.5% of patients post-initiation with well-controlled asthma) were observed. Proportion of patients with BEC ≥ 500 cells/µl decreased from 84.4% pre-initiation to 18.1% post-initiation.
Conclusion
Mepolizumab was effective in reducing the burden of SA by significantly reducing CSEs, reducing OCS use and HCRU, and improving lung function and asthma control, which could translate to improvements in health-related quality of life in patients with SA and high OCS dependency in the countries studied. A graphical abstract is available with this article.
Plain Language Summary
Severe asthma occurs when asthma symptoms remain uncontrolled despite optimised treatment. In many low-middle income countries, and in some countries in the Middle East, Asia, Latin America and the Arab Gulf, the management and treatment of patients with severe asthma remain poor, with many patients having unscheduled hospital visits or admission, and use of steroids for a prolonged period. Mepolizumab is an injectable monoclonal antibody approved as an add-on treatment for severe asthma in patients ≥ 6 years of age. In clinical trials, mepolizumab has demonstrated reductions in the risk of clinically significant exacerbations (CSE; an asthma exacerbation that requires systemic corticosteroids and/or an emergency room visit and/or hospitalisation) and the need for oral corticosteroid (OCS) treatment in patients with severe asthma by reducing inflammation caused by eosinophil (a type of white blood cell) production. The Nucala Effectiveness Study (NEST) was performed to observe the effectiveness of mepolizumab in people with severe asthma in Colombia, Chile, India, Turkey, Saudi Arabia, United Arab Emirates, Kuwait, Oman and Qatar. The frequency of CSEs and other outcomes was compared 12 months pre- and post-mepolizumab initiation. Post-initiation, the risk of CSEs was significantly reduced by 76% (p < 0.001), and 72% of patients had no CSEs. Fewer patients were dependent on OCS, with 36.1% of patients not using OCS at all, and fewer patients were hospitalised. Lung function and asthma control also improved. NEST shows that mepolizumab could benefit people with severe asthma living in countries where disease-related burden and OCS use remain high.
AbstractSection Graphical Abstract
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
In many countries in the Middle East, Asia, Latin America and the Arab Gulf, asthma-related burden is high; there is an urgent need to optimise management in these regions |
Mepolizumab is a humanised anti-interleukin-5 monoclonal antibody that has been approved as an add-on treatment for severe asthma with an eosinophilic phenotype in patients ≥ 6 years of age |
In the Nucala Effectiveness Study, 525 patients with severe asthma burden received at least one dose of mepolizumab 100 mg subcutaneously; data were collected for 12 months pre- and post-mepolizumab initiation |
What was learned from the study? |
Post-initiation, a significant reduction in clinically significant exacerbations (CSE) was observed (76% [p < 0.001]; incident rate ratio [95% confidence interval] 0.24 [0.19–0.30]) |
Post-initiation, 36.1% of patients became oral corticosteroid-free and 72.0% had no CSEs; mepolizumab treatment led to reductions in hospitalisations and an improvement in overall asthma management |
Digital Features
This article is published with digital features, including a graphical abstract, to facilitate understanding of the article. To view digital features for this article, go to https://doi.org/10.6084/m9.figshare.26510320.
Introduction
An estimated 5–10% of patients with asthma have severe asthma [1], characterised by frequent exacerbations despite controller medication (including high dose of inhaled corticosteroids [ICS]/long-acting beta2-agonist combination therapy) [2], high oral corticosteroid (OCS) use and poor quality of life (QoL) [1, 3,4,5]. Among patients with asthma, asthma-related healthcare resource use (HCRU) and costs are substantially greater for patients with severe asthma. Studies from the UK and France have reported morbidity and mortality of severe asthma to constitute > 50% of the total healthcare costs of asthma management [6, 7].
Whilst prevalence is likely underestimated, a high proportion of patients with asthma reside in low-middle-income countries (LMICs). Patients from these countries represent approximately 90% of the global burden of asthma with disproportionately high asthma-related morbidity and mortality [4, 5, 8, 9]. Moreover, asthma-related burden is substantial in many countries in the Middle East, Asia, Latin America and the Arab Gulf [4] and there is an urgent need to optimise therapy. Here, poor asthma control and management is common, as evidenced by frequent exacerbations, high OCS use (for example, in a multicentre, observational study in the Gulf region, OCS was used by 37.3% of patients in the United Arab Emirates [10], whereas in a UK-based historical follow-up study, the proportion of patients with severe uncontrolled eosinophilic asthma aged 18–64 who used maintenance OCS was reported to be 16.5% [6]) and low Asthma Control Test (ACT) scores [3, 4, 10,11,12,13,14,15]. Literature on the impact of severe asthma on HCRU and costs for patients from these countries is limited [10, 13]; however, treatment costs are considerably higher in LMICs than in high-income countries [16,17,18]. A systematic review of 60 LMICs reported a 1-month supply of ICS to cost 2–7 days’ worth of wages in most countries for which treatment affordability was assessed [19]. Furthermore, in a study conducted in Colombia, the mean annual direct costs of outpatient care for severe asthma was 4743.6 ± 6331.1 US dollars, with medication constituting 98% of overall costs [16]. Furthermore, an unmet need exists to improve prescription practices in countries in the Middle East, where under-prescription of ICS, poor adherence to prescribed medication and patient-perceived lack of guidance from physicians is common [20].
Prolonged OCS use is associated with an increased risk of adverse events (AEs), complications and OCS-induced morbidity including stroke, heart failure, diabetes, cataracts, osteoporosis, depression, anxiety and infections, as well as a reduction in QoL over time [21,22,23,24]. Even receipt of short courses of OCS treatment can significantly increase the risk of AEs in patients [24]. Despite this, OCS use remains high in LMICs and countries in the Middle East, Asia, Latin America and the Arab Gulf, likely because of low cost and greater accessibility compared to biologic treatment options [4, 8, 25, 26].
Type 2 inflammation is a key feature of severe asthma, which can be categorised as either eosinophilic or neutrophilic [27, 28]. Most patients with severe asthma (> 80%) present with an eosinophilic phenotype (severe asthma with an eosinophilic phenotype [SAEP]) [29]. The cytokine, interleukin-5 (IL-5) is a key factor in regulating the growth, differentiation, activation and survival of eosinophils, the production of which results in inflammation and triggers asthma exacerbations [30, 31]. Often, treatment with inhaled and/or systemic corticosteroids is ineffective in patients with severe asthma (with or without an eosinophilic phenotype) [27]. In these patients, add-on biologic therapy is recommended [2]. Mepolizumab is an anti-IL-5 antibody used to treat SAEP by binding to and neutralising soluble IL-5, inhibiting its interaction with its receptor, IL-5Rα [32]. This action suppresses the downstream signalling cascade thereby inhibiting eosinophil proliferation [27]. Mepolizumab is approved as an add-on treatment for SAEP in patients ≥ 6 years of age [33, 34].
Evidence from the randomised controlled trial (RCT) Dose Ranging Efficacy And safety with Mepolizumab in severe asthma (DREAM) demonstrated significant reductions in rates of clinically significant exacerbations (CSEs; defined as an asthma exacerbation that requires systemic corticosteroids [OCS for ≥ 3 days or a single dose of intravenous/intramuscular corticosteroid] and/or an emergency room (ER) visit and/or hospitalisation) [35] and clinically meaningful improvements in health-related QoL in patients with SAEP following treatment with mepolizumab [36]. Furthermore, The Steroid Reduction with Mepolizumab Study (SIRIUS) demonstrated significant reductions in exacerbations and a median reduction in OCS dose of 50% (p = 0.007) following 20 weeks of treatment with mepolizumab [37].
Real-world evidence (RWE) studies in Europe and North America have further demonstrated effectiveness of mepolizumab in patients with SAEP [38, 39]. The REAL world effectiveness of mepolizumab In paTIent care (REALITI-A) study was a 24-month multi-country, prospective, observational cohort study investigating the real-world OCS-sparing effect of mepolizumab in adults with severe asthma across 84 sites in Europe, Canada and the US [38]. REALITI-A reported significant reductions in the rates of CSEs as well as the use of OCS [38, 40]. Similar results were observed in the REal-worlD Effectiveness and Safety (REDES) study, a multicentre, observational cohort study designed to evaluate the effectiveness and safety of mepolizumab in patients with severe asthma in Spain, whereby significant reductions in CSEs (77.5% [p < 0.001]) and OCS use were reported [39].
Patients from LMICs and countries in the Middle East, Asia, Latin America and the Arab Gulf have been underrepresented in previous RWE studies [10]. The objective of the Nucala Effectiveness Study (NEST; GSK study number 213475) was to generate evidence of the effectiveness of mepolizumab in optimising asthma management and reducing CSEs in a diverse and heterogeneous population of patients with severe asthma living in underrepresented countries.
Methods
Study Design and Setting
NEST was a multi-country, bi-directional (both historical and prospective data considered), self-controlled, observational cohort study conducted in Colombia, Chile, India, Türkiye, Saudi Arabia and Arab Gulf countries (United Arab Emirates, Kuwait, Oman and Qatar). From each participating country, patients with a clinical diagnosis of severe asthma who had already been prescribed mepolizumab as add-on therapy for severe asthma as per their physician’s decision, and already received at least one dose were considered for recruitment by convenience sampling. To address potential sources of enrolment bias, physicians were not encouraged to prescribe mepolizumab to enrol patients into NEST.
The enrolment date was defined as the date patients entered the study; the index date was defined as the date of mepolizumab treatment initiation (Fig. 1). Data collection was from 1 November 2021, to 1 March 2023. Data were extracted from medical records (paper or electronic) 12 months prior to the index date for all patients (pre-initiation). This allowed for a standardised period of baseline history to describe patient demographics, disease burden and previous medication use. Data were collected from medical records up to 12 months following the index date (post-initiation). All data up to 12 months post-index were included in these analyses, including patients who discontinued prematurely. All patients were followed for 12 months following index, meaning for a patient who enrolled on the last day of the enrolment period, the data collection could have lasted up to 18 months following the start. Data were collected using a study electronic case report form (eCRF). All centres underwent standardised training and utilised standardised documentation for completion of eCRFs at enrolment and for each assessment during the observation period.
Patients
Eligible patients were aged ≥ 18 years, had a clinical diagnosis of severe asthma, were prescribed ≥ 1 dose (any dosage) of mepolizumab and had 12 months of historical data (obtained from paper and electronic medical records) prior to the index date (pre-initiation). Patients had to provide written informed consent and were required to have already initiated mepolizumab treatment for severe asthma, based on their physician’s decision. In countries where a waiver for informed consent was requested or granted, informed consent was not obtained for each patient. Patients who were participating in a clinical trial for which the treatment regimen and/or monitoring took place during the periods pre- and post-initiation were not eligible for inclusion.
Populations
Patients who met the eligibility criteria and received at least one dose of 100 mg subcutaneous mepolizumab following physician decision are the focus of this analysis. The target sample size for this multi-country study was 550 patients. An initial sample size calculation estimated a final number of 219 patients, assuming an effect size of 0.6, or 315 patients, assuming an effect size of 0.5.
Endpoints
The primary outcome was the overall rate of CSEs. The frequency of CSEs was collected pre- and post-initiation to calculate the rate of CSEs for both periods.
Key secondary outcomes included: asthma-related HCRU including count and length of hospital admissions, intensive care unit and ER visits, and visits with healthcare professionals; change in OCS dose from pre- to post-initiation among patients receiving OCS maintenance treatment at index; and changes in lung function (forced expiratory volume in one second [FEV1] and forced vital capacity [FVC]) were compared using the historical value nearest to the index date pre-initiation and available data post-initiation. ACT scores were collected in all participating countries during the pre-initiation period and at 12 months post-initiation; in the Arab Gulf countries, ACT scores were collected pre-initiation and at 3, 6 and 12 months post-initiation. As the total number of doses received across the study population may have varied, only patients who received 12 doses of mepolizumab 100 mg over the 12-month period were included in the analyses of asthma control (ACT scores) to minimise bias.
Additional endpoints included: physicians’ perceptions of how patients responded to mepolizumab treatment and patterns of mepolizumab treatment (including dose, treatment duration, adherence [defined as the proportion of days covered] and total number of doses over 12 months) were described. Where available, peripheral blood eosinophil count (BEC) was collected using the closest historical value to the index date pre-initiation.
Statistical Analyses
The mean and 95% confidence intervals (CI) of CSEs were estimated from a univariate negative binomial regression. CSE rates were estimated via generalised estimating equation models assuming a negative binomial distribution of CSEs and a log link function. A covariate for treatment period (i.e. pre- or post-initiation) was included and the logarithm of time was used as an offset variable. An autoregressive correlation structure of order 1 was used to correct for within-participant correlation. All other exposure and outcome variables were analysed descriptively.
A sensitivity analysis was performed to compare differences between the primary endpoint in patients who were followed from index until the date of last mepolizumab dose + 28 days (referred to as the ‘on-treatment’ group) vs. those who were followed for 12 months irrespective of when their last mepolizumab dose was received (Supplementary Results).
Ethics and Good Clinical Practice Declarations
The study protocol was reviewed and approved by the respective institutional review boards and ethics committees of the participating countries, and the study was conducted in accordance with the International Conference on Harmonisation, Good Pharmacoepidemiology Practice, Good Clinical Practice and all applicable patient privacy requirements and country-specific requirements relevant for an observational study.
Results
Patient Disposition
Of 581 patients screened, 531 met the eligibility criteria and received at least one dose of subcutaneous mepolizumab following physician decision and were enrolled in the study; six of these received at least one dose of 300 mg mepolizumab. The treated population comprised 525 patients who received at least one dose of mepolizumab 100 mg.
Patient Characteristics Pre-initiation
The mean (standard deviation [SD]) age of the study population patients was 49.6 (13.4) years and most patients were female (72.8%) (Table 1). Overall, 69.4% of patients had at least one comorbidity, of which rhinosinusitis (n = 226; 62.3%) and self-reported nasal polyps (n = 144; 39.7%) were the most common. Furthermore, 27.8% (n = 101) of the study population had a history of allergies. Of note, four (1.1%) patients had hypereosinophilic syndrome. Overall, 37.3% of patients were obese (defined as having a body mass index score of ≥ 30 kg/m2).
Patients demonstrated substantial severe asthma burden pre-initiation with 306 of 524 (58.4%) patients recorded as being OCS-dependent, i.e. were receiving OCS at the time of mepolizumab initiation or had received OCS for 26 weeks in the past year. For 277 patients with available data, the mean (SD) OCS dose was 23.2 (20.0) mg/day (Table 2). Of these, 167 (60.3%) patients were using maintenance OCS in the pre-initiation period at a mean (SD) dose of 22.8 (21.9) mg/day. Most patients reported using ICS in the pre-initiation period (521 of 525 [99.4%]), with 291 (56.0%) of those patients receiving a high dose. Of 466 patients with available data, the geometric mean BEC was 490.7 cells/µl (value nearest to the index date in the pre-initiation period); 264 of 479 (55.1%) patients with available data reported a BEC of ≥ 500 cells/µl pre-initiation. Overall, 165 of 525 patients (31.4%) had reported previous use with omalizumab; one patient reported use of dupilumab in the pre-initiation period. Of the patients with available data (n = 240), most had poor asthma control (ACT score < 20) at baseline (n = 204 [85.0%]). Pre-initiation, the mean (SD) predicted pre-bronchodilator FEV1 was 62.8% (20.2) for 129 patients with available data.
Characteristics of Patients with No CSEs Pre-initiation
Of patients for whom asthma CSE information was documented at baseline, 178 of 472 (37.7%) had no CSEs. Over half (53.4%) of patients without CSEs at baseline were OCS dependent. Of those, the mean dose of OCS was 21.6 mg/day with 37.6% of patients receiving a dose of ≥ 30 mg/day. Overall, 33.2% of these patients were biologic-experienced. Of the patients with reported BEC (n = 156), the geometric mean (geometric SD) BEC was 485.9 (3.0) cells/µl with 91 of 156 (58.3%) patients with ≥ 500 cells/µl. There was a paucity of other measures such as ACT scores for these patients.
Patterns of Mepolizumab Use
Most patients (491 of 519 [94.6%]; 6 patients from the treated population were excluded from this calculation as they had missing data regarding their last dose of mepolizumab) had ≥ 90% adherence over 12 months; the mean (SD) number of days covered was 360 (74.3) days. Further details regarding the number of refills/doses over 12 months and the reasons why patients were prescribed mepolizumab are provided in the Supplementary Material.
CSE Rates Pre- and Post-initiation
Overall, 472 and 493 patients had pre- and post-initiation CSE data, respectively. The number of patients who experienced at least one CSE was lower in the post-initiation period (138 [28.0%] patients) compared to the pre-initiation period (294 [62.3%] patients; Fig. 2). The mean (95% CI) number of CSEs per patient was lower post-initiation (1.8 [1.5–2.0]) compared to the pre-initiation period (3.1 [2.7–3.4]). The incidence rate ratio (95% CI) of CSEs pre- vs. post-initiation was 0.24 (0.19–0.30; p < 0.001), representing a 76% reduction in the CSE rate post-initiation. The proportion of patients who experienced no CSEs increased from 37.7% pre-initiation to 72.0% post-initiation.
Of the patients that had no CSEs documented at baseline (n = 178), 141 of 172 (82.0%) with available data reported no CSEs post-initiation; 31 of 172 (18.0%) patients reported ≥ 1 CSE post-initiation.
Asthma-related HCRU: CSEs Requiring Hospitalisation or an ER Visit
Overall, there was a reduction in the number of patients who required an ER visit or hospitalisation due to CSE. In total, 106 of 472 (22.5%) patients were hospitalised pre-initiation vs. 34 out of 493 (6.9%) patients post-initiation (Fig. 3). The mean (SD) length of hospital stay was lower post-initiation compared to pre-initiation (8.2 [5.0] days vs. 11.3 [10.0] days). Of the 294 patients with at least one CSE in the pre-initiation period, 36.1% (n = 106) were hospitalised, 51.4% (n = 151) visited the ER and 23.1% (n = 68) visited their physician. In comparison, HCRU for the patients with at least one CSE post-initiation (n = 138) was lower, with 24.6% (n = 34) of patients being hospitalised, 36.2% (n = 50) of patients visiting the ER and 33.3% (n = 46) of patients visiting their physician.
Changes in OCS Dose and Usage From Pre- to Post-initiation
Pre-initiation, 132 (25.2%) patients had previously used OCS (defined as ≥ 26 weeks of use in the 12 months pre-initiation) and 174 (33.2%) patients were receiving OCS at mepolizumab initiation. Of 525 patients, the proportion who received OCS was lower post-initiation compared with pre-initiation (16.6% vs. 52.8%; Fig. 4); the mean (SD) OCS dose was also lower (16.3 [17.4] mg/day vs. 23.2 [20.0] mg/day; Table 2). Of the patients who used OCS, 67 of 277 patients (24.2%) used 5 mg OCS pre-initiation compared with 39 of 87 patients (44.8%) post-initiation. Of 274 patients with available data, 226 (82.5%) patients were able to have their OCS dose reduced by ≥ 50% post-initiation; 11 (4.0%) patients had their dose reduced by < 50%. The remaining 37 (13.5%) patients had no change to their OCS dose. Overall, 188 of 521 patients (36.1%) were OCS-free post-initiation.
Only 66 of the 167 patients (39.5%) who used maintenance OCS therapy at index continued its use post-initiation. Of those using maintenance OCS at index (n = 167), the mean change in maintenance OCS dose post-initiation was − 17.7 (22.4) mg, representing a mean (SD) reduction of 87.5 (22.0)%.
Of the 31 patients who reported ≥ 1 CSE post-initiation despite having no CSEs documented pre-initiation, 61.3% (n = 19) were on OCS maintenance therapy pre-initiation compared to 35.5% (n = 11) post-initiation.
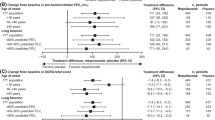
Changes in Lung Function
Change in Pre-bronchodilator FEV1
Overall, 129 of 340 (37.9%) patients pre-initiation and 87 of 229 (38.0%) patients post-initiation had pre-bronchodilator FEV1 (%) results. The mean (SD) predicted pre-bronchodilator FEV1 was 62.8 (20.2)% pre-initiation compared to 73.0 (22.7)% post-initiation (Fig. 5); the mean (SD) change in pre-bronchodilator FEV1 between the pre- and post-initiation periods was 23.8 (59.0)%.
Pre-bronchodilator FEV1 and pre-bronchodilator FVC pre- vs. post-mepolizumab initiation. FEV1 data only available for 129 and 87 patients pre- and post-mepolizumab initiation, respectively. FVC data only available for 131 and 88 patients pre- and post-mepolizumab initiation, respectively. FEV1 forced expiratory volume in one second, FVC forced vital capacity, SD standard deviation
For patients with no documented CSEs pre-initiation (n = 178) and who had available pre-bronchodilator FEV1 data (pre-initiation, n = 41; post-initiation, n = 28), the mean (SD) pre-bronchodilator FEV1 was 68.6 (21.3)% pre-initiation vs. 80.54 (24.9)% post-initiation.
Change in Pre-bronchodilator FVC
In total, 131 of 341 (38.4%) patients pre-initiation and 88 of 227 (38.8%) patients post-initiation had pre-bronchodilator FVC (%) results. The mean (SD) predicted pre-bronchodilator FVC was 72.6 (18.7)% and 81.1 (20.8)% pre- and post-initiation, respectively. From pre- to post-initiation, a mean (SD) difference of 16.0 (41.5)% was observed for pre-bronchodilator FVC.
For patients with no CSEs documented pre-initiation (n = 178), 41 and 29 patients had pre-bronchodilator FVC data pre- and post-initiation, respectively. The mean (SD) pre-bronchodilator FVC of these patients was 75.6 (18.0)% pre-initiation, vs. 84.0 (28.5)% post-initiation.
Measures of Asthma Control and Overall Health State Post-initiation
In patients who received 12 doses of mepolizumab 100 mg over 12 months (data available for 240 patients pre-initiation and 172 patients post-initiation), an improvement in ACT score was observed (Fig. 6). The proportion of patients with a score of 20–25, i.e. well-controlled asthma, increased (15.0% pre-initiation vs. 64.5% post-initiation). The mean (SD) difference in ACT score between the pre- and post-initiation periods was 7.6 (5.8).
ACT scores pre- vs. post-mepolizumab initiation. Results from patients that received 12 doses of mepolizumab 100 mg over the 12-month period post-mepolizumab initiation (data available for: pre-mepolizumab initiation, n = 240; post-mepolizumab initiation, n = 172); proportions calculated with appropriate denominator. ACT Asthma Control Test
Based on physicians’ evaluation, the overall health state (regarding asthma) for 447 of 484 (92.4%) patients from the total enrolled population (n = 531) had improved following mepolizumab treatment, with the majority of physicians reporting “much better” results (289 of 484 [59.7%] patients).
Key Biomarkers
The highest recorded BEC values were reported for 141 and 276 patients in the pre- and post-initiation periods, respectively. The mean (SD) highest value recorded decreased from 1247.1 (1235.1) cells/µl in the pre-initiation period to 316.0 (654.3) cells/µl in the post-initiation period. Of those with available data, the number of patients with BEC ≥ 500 cells/µl pre-initiation was 119 of 141 (84.4%) compared with 50 of 276 (18.1%) post-initiation.
At baseline, 29 of 31 patients who experienced ≥ 1 CSE post-initiation (but who had no documented CSEs pre-initiation) had BEC data; the geometric mean (geometric SD) BEC for these patients was 526.1 (2.5) cells/µl.
Discussion
In this real-world study of patients with severe asthma from countries in the Middle East, Asia, Latin America and the Arab Gulf, a significant reduction in CSE rates was observed (76%; p < 0.001). Following treatment with mepolizumab, the proportion of patients receiving OCS treatment decreased. The mean OCS dose decreased post-initiation (mean [SD] change in OCS dose, − 18.1 [20.7] mg) and 36.1% of patients became OCS-free.
The results of NEST were comparable with RCTs, including the DREAM study [36] and other RWE studies investigating mepolizumab treatment in patients with severe asthma. REALITI-A demonstrated a significant reduction in CSEs by 71% (rate ratio [95% CI], 0.29 [0.26, 0.32]) and a reduction in median maintenance OCS dose by 75% 1 year post-initiation [38]. In REDES, a significant reduction in the number of CSEs was observed (77.5% [p < 0.001]) and 50.6% of patients experienced no CSEs within the first year of mepolizumab treatment [39]. This proportion is comparatively higher in NEST whereby 72.0% of patients reported no CSEs in the 12 months post-initiation.
As noted, OCS use is common in LMICs and countries in the Middle East, Asia, Latin America and the Arab Gulf despite the fact that prolonged use is associated with an increased risk of adverse events [21,22,23,24]. The results observed in NEST revealed substantial reductions in OCS use and dosage post-initiation, reinforcing the effectiveness of mepolizumab. Furthermore, the overall HCRU and burden on healthcare systems in LMICs and the countries involved in NEST are considerably high [13, 15]. The proportion of patients hospitalised due to CSEs was reduced following receipt of at least one dose of 100 mg mepolizumab. Moreover, 94.6% of patients had ≥ 90% treatment adherence and the overall health state of 92.4% of patients had improved according to their physician, illustrating mepolizumab as an effective treatment option that could help to improve prescription practices in the countries studied [20]. Together, these results reinforce the benefits of mepolizumab for this population of patients with severe asthma whilst also highlighting the importance of optimal biologic intervention which is essential to improve patient outcomes and to avoid the systemic corticosteroid-associated morbidity.
In NEST, mepolizumab treatment led to improved lung function and asthma control, as evidenced by the improved pre-bronchodilator FEV1 and FVC results observed post-initiation and improvements in ACT scores with more patients achieving well-controlled asthma (score of 20–25) post-initiation. The mean (SD) difference in ACT score between the pre- and post-initiation periods was greater than the minimally important difference (post-initiation, 7.6 [5.8]; minimally important difference, 3.0) [41].
The benefits of mepolizumab for these patients with severe asthma are further evidenced by the substantial reduction in BEC (mean [SD] highest value recorded pre-initiation, 1247.1 [1235.1] cells/µl vs. post-initiation, 316.0 [654.3] cells/µl). As a marker of eosinophilic airway inflammation and a predictor of clinical outcomes (including exacerbations and treatment response) in severe asthma [42], it is pertinent to note the reduction in mean BEC post-initiation which may be associated with fewer CSEs following biologic treatment.
Achieving clinical remission (meaning to have a high level of disease control [including no asthma symptoms or exacerbations] and optimisation of lung function without the need for ongoing treatment [43]) is an advanced care goal in asthma and is of increasing interest within clinical and real-world trials [44, 45]. Although not specifically assessed, the endpoints considered in NEST align with those that are used to assess clinical remission, which suggests that these data could form the basis for future analyses to estimate the proportion of patients who may achieve clinical remission.
In NEST, a high proportion of patients experienced no CSEs pre-initiation (178 of 472 [37.7%] patients). This could simply be due to recall bias, which is more likely to occur in a real-world setting than within the conditions of an RCT. Another potential reason is that a large proportion of these patients were biologic-experienced (33.2%) and there may have been residual effects of previous biologic treatment for severe asthma pre-initiation. Overall, 53.4% of these patients were OCS-dependent prior to mepolizumab initiation and may have been switched to mepolizumab therapy to reduce the burden of OCS dependence. Together, this demonstrates that despite having no CSEs documented prior to mepolizumab initiation, these patients presented with asthma severity for which the treating physicians in actual clinical practice made the decision to prescribe mepolizumab. In these patients, mepolizumab was effective in improving outcomes (including CSEs, OCS use and lung function). Among the 31 patients who experienced ≥ 1 CSE post-initiation (despite having no CSEs documented pre-initiation), there was a reduction in the proportion of patients using maintenance OCS post-initiation. A plausible explanation for the number of documented CSEs among these patients post-initiation could be the result of OCS sparing. Notably, these patients had a higher geometric mean BEC at baseline (526.1 cells/µl) than those who experienced no CSEs pre- and post-initiation (485.9 cells/µl). As higher BEC levels are associated with an increased risk of exacerbations [42], this could explain the increase in CSEs post-initiation in these patients.
NEST was the first study to our knowledge in which physicians described the management of patients with severe asthma and to evaluate the effectiveness of mepolizumab in patients in real-world clinical practice from LMICs and countries underrepresented in previous RWE studies of mepolizumab. The clinically meaningful results of NEST can benefit asthma research groups in these countries, helping to strengthen the evidence base for asthma treatment in this specific population. Patients enrolled in NEST were reflective of those in the real world, where 69.0% of patients with severe asthma are reported to have at least 1 type-2 related comorbidity, such as chronic rhinosinusitis and nasal polyposis [46]. Similarly, in NEST, 69.1% of patients reported ≥ 1 comorbidity at baseline, of which rhinosinusitis and nasal polyps were the two most common. NEST demonstrated the effectiveness of mepolizumab in improving outcomes for these patients, reinforcing the value of these results for real-life patients and healthcare professionals in the countries studied. Furthermore, utilisation of the same eCRF across all countries enabled standardised data collection. Finally, unlike other RWE studies that do not typically have a control population, patients in NEST acted as their own control, which helped to provide internal validity, making it possible to see clear improvements in multiple outcomes post-initiation.
There are limitations to this study including the fact patients were selected by a convenience sampling method, meaning it is possible that despite being reflective of the general population of patients with severe asthma, the study population may not be fully representative of the target severe asthma population per country. Furthermore, all data were collected retrospectively from medical charts which could have led to information bias associated with patients with the earliest index dates who may have had different baseline characteristics to those whose index date was closer to the enrolment period. Finally, despite training and adoption of a standard eCRF, inconsistent interpretation of the eCRF by participating centres may have occurred.
Conclusion
These results confirm that mepolizumab treatment is effective in reducing CSEs, hospitalisations due to CSEs and OCS use as well as improving lung function and asthma control in patients with severe asthma in countries in the Middle East, Asia, Latin America and the Arab Gulf. These results further support the use of biologic treatment in patients with severe asthma and high disease burden, thus providing evidence for healthcare practitioners to inform their treatment decision-making for patients in the countries studied.
References
Wang E, Wechsler ME, Tran TN, et al. Characterization of severe asthma worldwide: Data from the international severe asthma registry. Chest. 2020;157(4):790–804.
Global Initiative for Asthma (GINA). 2023 gina report, global strategy for asthma management and prevention. https://ginasthma.org/2023-gina-main-report/. Accessed 1 Mar 2024.
Athanazio R, Stelmach R, Antila M, et al. Prevalence of the eosinophilic phenotype among severe asthma patients in Brazil: the BRAEOS study. J Bras Pneumol. 2022;48(3): e20210367.
Al-Ahmad M, Al Zaabi A, Madkour A, et al. Expert consensus on oral corticosteroids stewardship for the treatment of severe asthma in the Middle East and Africa. Respir Med. 2024;228: 107674.
Mortimer K, Reddel HK, Pitrez PM, Bateman ED. Asthma management in low and middle income countries: case for change. Eur Respir J. 2022;60(3):2103179.
Kerkhof M, Tran TN, Soriano JB, et al. Healthcare resource use and costs of severe, uncontrolled eosinophilic asthma in the UK general population. Thorax. 2018;73(2):116–24.
Roche N, Garcia G, de Larrard A, et al. Real-life impact of uncontrolled severe asthma on mortality and healthcare use in adolescents and adults: findings from the retrospective, observational resonance study in France. BMJ Open. 2022;12(8): e060160.
Caminati M, Morais-Almeida M, Bleecker E, et al. Biologics and global burden of asthma: a worldwide portrait and a call for action. World Allergy Organ J. 2021;14(2): 100502.
Meghji J, Mortimer K, Agusti A, et al. Improving lung health in low-income and middle-income countries: from challenges to solutions. Lancet. 2021;397(10277):928–40.
Al-Ahmad M, Mobayed H, Al Busaidi N, et al. Severe asthma treatment patterns: a multicenter observational study in the Gulf region. World Allergy Organ J. 2022;15(5): 100647.
Solé D, Aranda CS, Wandalsen GF. Asthma: Epidemiology of disease control in Latin America—short review. Asthma Res Pract. 2017;3:4.
Cooper PJ, Figueiredo CA, Rodriguez A, et al. Understanding and controlling asthma in Latin America: a review of recent research informed by the scaala programme. Clin Transl Allergy. 2023;13(3): e12232.
Mungan D, Aydin O, Mahboub B, et al. Burden of disease associated with asthma among the adult general population of five Middle Eastern countries: results of the SNAPSHOT program. Respir Med. 2018;139:55–64.
de Carvalho-Pinto RM, Cukier A, Angelini L, et al. Clinical characteristics and possible phenotypes of an adult severe asthma population. Respir Med. 2012;106(1):47–56.
Neffen H, Moraes F, Viana K, et al. Asthma severity in four countries of Latin America. BMC Pulm Med. 2019;19(1):123.
Alvis-Zakzuk NJ, Carrasquilla Sotomayor M, Zakzuk Sierra J, et al. Prs69 direct medical costs of severe asthma in two Colombian reference centers. Value Health. 2020;23:S361.
Koul PA, Dhar R. Economic burden of asthma in India. Lung India. 2018;35(4):281–3.
Mortimer K, Reddel HK, Pitrez PM, Bateman ED. Asthma management in low and middle income countries: case for change. Eur Respir J. 2022;60(3):2103179.
Stolbrink M, Thomson H, Hadfield RM, et al. The availability, cost, and affordability of essential medicines for asthma and copd in low-income and middle-income countries: a systematic review. Lancet Glob Health. 2022;10(10):e1423–42.
Zeitouni MO, Al-Moamary MS, Coussa ML, et al. Challenges and recommendations for the management of asthma in the Middle East and Africa. Ann Thorac Med. 2022;17(2):71–80.
Volmer T, Effenberger T, Trautner C, Buhl R. Consequences of long-term oral corticosteroid therapy and its side-effects in severe asthma in adults: a focused review of the impact data in the literature. Eur Respir J. 2018;52(4):1800703.
Hew M, McDonald VM, Bardin PG, et al. Cumulative dispensing of high oral corticosteroid doses for treating asthma in Australia. Med J Aust. 2020;213(7):316–20.
Sullivan PW, Ghushchyan VH, Globe G, Schatz M. Oral corticosteroid exposure and adverse effects in asthmatic patients. J Allergy Clin Immunol. 2018;141(1):110-6.e7.
Price DB, Trudo F, Voorham J, et al. Adverse outcomes from initiation of systemic corticosteroids for asthma: long-term observational study. J Asthma Allergy. 2018;11:193–204.
Maspero JF, Cruz AA, Beltran CFP, et al. The use of systemic corticosteroids in asthma management in Latin American countries. World Allergy Organ J. 2023;16(4): 100760.
Dhar R, Rhee CK, Perng D-W, et al. The burden of systemic corticosteroid use in asthma management in Asia. Respirology. 2023;28(8):744–57.
Pelaia C, Paoletti G, Puggioni F, et al. Interleukin-5 in the pathophysiology of severe asthma. Front Physiol. 2019;10:1514.
Pelaia G, Vatrella A, Busceti MT, et al. Cellular mechanisms underlying eosinophilic and neutrophilic airway inflammation in asthma. Mediators Inflamm. 2015;879783.
Heaney LG, Perez de Llano L, Al-Ahmad M, et al. Eosinophilic and noneosinophilic asthma: an expert consensus framework to characterize phenotypes in a global real-life severe asthma cohort. Chest. 2021;160(3):814–30.
Nakagome K, Nagata M. Involvement and possible role of eosinophils in asthma exacerbation. Front Immunol. 2018;9:2220.
Choy MS, Dixit D, Bridgeman MB. Mepolizumab (Nucala) for severe eosinophilic asthma. P t. 2016;41(10):619–22.
Roufosse F. Targeting the interleukin-5 pathway for treatment of eosinophilic conditions other than asthma. Front Med (Lausanne). 2018;5:49.
FDA. Nucala (mepolizumab) for injection, for subcutaneous use. https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/125526Orig1s021,761122Orig1s011Corrected_lbl.pdf. Accessed 2 July 2024.
EMA. Nucala (mepolizumab) an overview of nucala and why it is authorised in the EU. https://www.ema.europa.eu/en/medicines/human/EPAR/nucala. Accessed 2 July 2024.
Reddel HK, Taylor DR, Bateman ED, et al. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med. 2009;180(1):59–99.
Pavord ID, Korn S, Howarth P, et al. Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo-controlled trial. Lancet. 2012;380(9842):651–9.
Bel EH, Wenzel SE, Thompson PJ, et al. Oral glucocorticoid-sparing effect of mepolizumab in eosinophilic asthma. N Engl J Med. 2014;371(13):1189–97.
Pilette C, Canonica GW, Chaudhuri R, et al. REALITI-A study: real-world oral corticosteroid-sparing effect of mepolizumab in severe asthma. J Allergy Clin Immunol Pract. 2022;10(10):2646–56.
Domingo Ribas C, Carrillo Díaz T, Blanco Aparicio M, et al. Real world effectiveness and safety of mepolizumab in a multicentric Spanish cohort of asthma patients stratified by eosinophils: the REDES study. Drugs. 2021;81(15):1763–74.
Caruso C, Canonica GW, Patel M, et al. International, prospective study of mepolizumab in severe asthma: REALITI-A at 2yrs. Eur Respir J. 2022;60(suppl 66):4589.
Schatz M, Kosinski M, Yarlas AS, Hanlon J, Watson ME, Jhingran P. The minimally important difference of the Asthma Control Test. J Allergy Clin Immunol. 2009;124(4):719-23.e1.
Hirano T, Matsunaga K. Measurement of blood eosinophils in asthma and chronic obstructive pulmonary disease. Intern Med. 2023;62(1):21–5.
Thomas D, McDonald VM, Pavord ID, Gibson PG. Asthma remission: what is it and how can it be achieved? Eur Respir J. 2022;60(5):2102583.
McDowell PJ, McDowell R, Busby J, et al. Clinical remission in severe asthma with biologic therapy: an analysis from the UK Severe Asthma Registry. Eur Respir J. 2023;62(6):2300819.
Perez-de-Llano L, Scelo G, Tran TN, et al. Exploring definitions and predictors of severe asthma clinical remission post-biologic in adults. Am J Respir Crit Care Med. 2024. https://doi.org/10.1164/rccm.202311-2192OC.
Scelo G, Torres-Duque CA, Maspero J, et al. Analysis of comorbidities and multimorbidity in adult patients in the International Severe Asthma Registry. Ann Allergy Asthma Immunol. 2024;132(1):42–53.
Acknowledgements
The authors would like to acknowledge Ms. Patricia Menezes (GSK, Rio de Janeiro, Brazil) for contributions to the study. The authors would also like to acknowledge Prof. Arzu Yorgancioglu (Celal Bayar University School of Medicine, Manisa, Türkiye), Prof. Fatma Merve Tepetam (Clinic of Immunology and Allergy, Süreyyapaşa Chest Diseases and Thoracic Surgery Training and Research Hospital, Istanbul, Türkiye), Prof. Özlem Göksel (Division of Immunology, Allergy and Asthma, Faculty of Medicine, Ege University, İzmir, Türkiye), Prof. Dilşad Mungan (Ankara University School of Medicine, Ankara, Türkiye), Prof. Yavuz Havlucu (Celal Bayar University School of Medicine, Manisa, Türkiye), Prof. Canturk Tasci (University of Health Sciences, Gulhane Training and Research Hospital, Ankara, Türkiye), Prof. Kurtulus Aksu (University of Health Sciences Atatürk Sanatoryum Education and Research Hospital, Ankara, Türkiye), Dr Berfin Torun (Koc University, Istanbul, Türkiye), Prof. Ismet Bulut (University of Health Sciences Süreyyapaşa Chest Diseases and Thoracic Surgery Training and Research Hospital, Istanbul, Türkiye), Dr Consuelo Rodriguez Matinez (GSK Chile, Santiago, Chile), Dr Daniela Escrig (GSK Chile, Santiago, Chile), Dr Emilio Feres (Clínica Dávila, Santiago Chile), Dr Felipe Moraes dos Santos (GSK Chile, Santiago, Chile), Dr Jose Romero (GSK Chile, Santiago, Chile), Dr Nicolás Sandoval (GSK Chile, Santiago, Chile), Dr Valentina Poblete Fernandez (Instituto Nacional del Tórax, Santiago, Chile), Dr Libardo José Jiménez Maldonado (Fundación Neumológica Colombiana, Bogotá, Colombia), Nataly Preciado Quintero (GSK Colombia, Bogotá, Colombia), Dr Andrés González Rangel (GSK Colombia, Bogotá, Colombia), Prof. Carlos Andrés Celis-Preciado (Hospital Universitario San Ignacio, Bogotá, Colombia), Dr Azmat Karim (Dr. Azmat Karim Clinic, New Delhi, India), Dr Disha Gupta (GSK, Mumbai, India), Dr Priti Meshram (Grant Government Medical College & Sir JJ Group of Hospitals, Mumbai, India), Dr Samir Adsule (GSK, Mumbai, India), Dr Mousa Khadadah (Al Mubarak Hospital, Kuwait), Dr Sana Al Mutairi (Al Amiri Hospital, Kuwait), Dr Nasser Al Busaidi (The Royal Hospital, Oman), Dr Ramzi Abdulasaad Khashkhusha (Tawam Hospital, Abu Dhabi, United Arab Emirates), Dr Zaid Zoumot (Cleveland Clini, Abu Dhabi, United Arab Emirates), Prof. Samaha Hala (Qassimi Hospital, Sharjah, United Arab Emirates), Dr Tayseer Sabah Alsaeed Mohmmed Ibrahim (Hamad Medical Corporation, Doha, Qatar), Dr Ahmed Rufai Nadama (King Khalid University Hospital, Saudi Arabia), Dr Ahmed Altawil (GSK, Jeddah, Saudi Arabia), Dr Manal Al-Hazmi (King Fahad Specialist Hospital, Dammam, Saudi Arabia), Dr Siraj Omar Wali (King Abdulaziz University, Jeddah, Saudi Arabia), Dr Ali Alhammad (GSK, Riyadh, Saudi Arabia), Alexander Ford (Adelphi Real World, UK), Sarah Weatherby (Adelphi Real World, UK), and Beth Dibben (Adelphi Real World, UK), and all other principal investigators for their contributions to patient recruitment for the study.
Medical writing, Editorial and Other Assistance
Medical writing support for the development, under the guidance of the authors, was provided by Niamh Southern, MPhil of Ashfield MedComms, an Inizio company, and funded by GSK. Trademarks are the property of their respective owners (ACT [QualityMetric incorporated]).
Author Contributions
Bassam Mahboub, Elizabeth Garcia, Claudia Soares, Gabriela Abreu, Juliana Queiroz, Alejandro Raimondi and Saeed Noibi contributed to the conception and/or design of the study. Riyad Omar Al-Lehebi, Mona Al Ahmad, Venkata Nagarjuna Maturu, Alejandra Galeano Mesa, Bassam Mahboub, Elizabeth Garcia, Patricia Fernandez and Sevim Bavbek contributed to the acquisition of the data. Gabriela Abreu, Debora dos Santos, Juliana Queiroz, Maria Laucho-Contreras, Saeed Noibi and Gur Levy contributed to the data analysis and/or interpretation. All authors were involved in drafting the work or reviewing it critically for important intellectual content and gave final approval of the version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
GSK funded this research (study number 213475) and were responsible for all costs associated with the development and the publishing of this manuscript, including the rapid service fee and the open access fee.
Data Availability
The study data may be provided by reasonable request to the corresponding author.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Riyad Omar Al-Lehebi has given lectures at meetings supported by AstraZeneca, Boehringer Ingelheim, GSK and Sanofi, and received advisory board fees from GSK. Mona Al Ahmad received lecture and advisory board honoraria from Sanofi, GSK and AstraZeneca. Venkata Nagarjuna Maturu has given lectures at meetings supported by AstraZeneca, GSK, Novartis, Sun Pharma, Cipla and Lupin, and participated in advisory boards with AstraZeneca and GSK. Alejandra Galeano Mesa has no conflicts of interest to report. Bassam Mahboub is a speaker for AstraZeneca, GSK and Sanofi. Elizabeth Garcia reports having been a speaker for Sanofi, Novartis, and Pfizer and received advisory board fees from GSK, Sanofi and Novartis. Patricia Fernandez reports having been a speaker for AstraZeneca, GSK, Sanofi and Teva, and participated in advisory boards with AstraZeneca, GSK and Sanofi. Claudia Soares, Alejandro Raimondi, Maria Laucho-Contreras, Saeed Noibi and Gur Levy are employed by GSK and hold financial equities in GSK. Gabriela Abreu and Juliana Queiroz are complementary employees of GSK and do not hold financial equities in GSK. Debora dos Santos was a complementary worker of GSK at the time of the study analysis. Debora dos Santos’ current affiliation is a postdoctoral fellowship at University of Brasilia under the Program of Collective Health. Sevim Bavbek has given lectures at meetings supported by AstraZeneca, GSK and Novartis, and reports receipt of advisory board fees from AstraZeneca, GSK and Novartis.
Ethical Approval
The study protocol was reviewed and approved by the respective institutional review boards and ethics committees of the participating countries and the study was conducted in accordance with the International Conference on Harmonization, Good Pharmacoepidemiology Practice, Good Clinical Practice and all applicable patient privacy requirements and country-specific requirements relevant for an observational study.
Additional information
Debora dos Santos: Affiliation at time of the study conduct.
Prior Presentation
A subset of these data have been presented previously at ERS 2023 (Bavbek S, et al. Multi-country self-controlled study of exacerbation rates in severe asthma patients treated with mepolizumab: NEST interim analysis. European Respiratory Journal. 2023; 62 (suppl 67) PA1907; https://doi.org/10.1183/13993003.congress-2023.PA1907).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Al-Lehebi, R.O., Al Ahmad, M., Maturu, V.N. et al. Real-World Effectiveness of Mepolizumab in Severe Asthma: Results from the Multi-country, Self-controlled Nucala Effectiveness Study (NEST). Adv Ther (2024). https://doi.org/10.1007/s12325-024-02967-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12325-024-02967-x