Abstract
Introduction
Intravenous (IV) iron is the recommended treatment for patients with iron deficiency anemia (IDA) unresponsive to oral iron treatment, in whom oral iron is contraindicated, or where rapid iron replenishment is required. Ferric derisomaltose (FDI) and ferric carboxymaltose (FCM) are high-dose, rapid-infusion, IV iron formulations that have recently been compared in three head-to-head randomized controlled trials (RCTs), which showed significantly higher incidence of hypophosphatemia after administration of FCM than FDI. The present study objective was to evaluate the cost–utility of FDI versus FCM in a population of patients with IDA in China.
Methods
A previously-published patient-level simulation model was used to model the cost–utility of FDI versus FCM in China. The number of infusions of FDI and FCM was modeled based on the approved posology of the respective formulations using simplified tables of iron need in a population of patients with body weight and hemoglobin levels informed by a Chinese RCT of FCM. Data on the incidence of hypophosphatemia was obtained from the PHOSPHARE-IDA RCT, while data on disease-related quality of life were obtained from SF-36v2 data from the PHOSPHARE-IBD RCT.
Results
Over the 5-year time horizon, patients received 3.98 courses of iron treatment on average, requiring 0.90 fewer infusions of FDI than FCM (7.69 vs. 6.79). This resulted in iron procurement and administration cost savings of renminbi (RMB) 206 with FDI (RMB 3,519 vs. RMB 3,312). Reduced incidence of hypophosphatemia-related fatigue resulted in an increase of 0.07 quality-adjusted life years and further cost savings of RMB 782 over 5 years, driven by reduced need for phosphate testing and replenishment. FDI was therefore the dominant intervention.
Conclusions
The results showed that FDI would improve patient quality of life and reduce direct healthcare expenditure versus FCM in patients with IDA in China.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Iron deficiency anaemia (IDA) is estimated to affect 176 million people in China and intravenous (IV) iron is indicated where oral iron is contra-indicated or ineffective, or where rapid iron replenishment is required. |
The aim of the present analysis was to evaluate the cost-effectiveness of two IV iron formulations — ferric derisomaltose (FDI) and ferric carboxymaltose (FCM) — in the treatment of patients with IDA in China. |
What was learned from the study? |
Patients treated with FDI required fewer iron infusions and therefore incurred lower iron administration costs versus FCM. FDI was also associated with cost savings arising from the avoidance of serum phosphate testing and reduced incidence of hypophosphatemia. |
Quality of life improvements with FDI versus FCM arose from reduced hypophosphatemia-related fatigue and the reduced need for healthcare system interactions to received iron infusions. |
FDI was the dominant treatment strategy at up to a 31% discount on the FCM list price, and FDI was cost-effective versus FCM even when FCM was modeled as having no cost from the Chinese healthcare system perspective. |
Introduction
One of the most common causes of anemia is iron deficiency (ID) [1]. Iron deficiency anemia (IDA) affects 30% of the worldwide population, is the most common nutritional deficiency in the world, and is a significant contributor to the global disease burden [2,3,4]. In China, IDA is estimated to affect 176 million people [5] and 13.9% of pregnant women [6]. This already substantial IDA burden is likely to increase, based in part on the rising prevalence of childhood obesity prevalence in China [7], and children with obesity have been found to be at a relatively higher risk of developing ID and IDA [8, 9].
Risk factors that have been linked to IDA include menstruation in women, gastrointestinal bleeding, decreased dietary iron intake, and absorption issues [10]. Symptoms of IDA can vary from patient to patient, but may include shortness of breath, palpitations, fatigue, and tachycardia due to lower blood oxygen levels, with more serious manifestations including angina, abdominal pain, and motility disorders [2]. Evidence from the published literature demonstrates that IDA can significantly impact the quality of life (QoL) of those living with the condition, particularly pregnant or heavily menstruating women [11,12,13], individuals with chronic heart failure [14], and those with inflammatory bowel disease (IBD) [15]. Despite these impacts, however, treating individuals living with IDA has been shown to lead to QoL improvements, regardless of the underlying cause of the condition [16, 17].
Treatment for IDA conventionally involves the use of oral iron supplementation, which is effective in most patients [18]. However, in patients in whom oral iron is contra-indicated or is ineffective [19, 20], or where rapid iron replenishment is required, intravenous (IV) iron therapy is indicated, and has been demonstrated to be clinically effective [21, 22].
Ferric derisomaltose (FDI) and ferric carboxymaltose (FCM) are two IV iron formulations that are used in the treatment of IDA, each allowing a high dose of iron to be administered rapidly per infusion [23], leading to faster anemia correction than oral iron. The formulations have been demonstrated to have comparable effectiveness in terms of hematological response, but FCM is associated with significantly higher rates of hypophosphatemia [24,25,26]. Indeed, the PHOSPHARE-IDA randomized controlled trials (RCTs) found that 74.4% of patients receiving FCM and only 8.0% of patients receiving FDI experienced hypophosphatemia (defined as a serum phosphate level of < 2.0 mg/dL) [27]. Repeated use of FCM may therefore result in hypophosphatemia-related osteomalacia, which can lead to symptoms including bone pain and fracture [23]. A further advantage of FDI relative to FCM is the higher dose per infusion that can be administered. Specifically, the maximum dose of FCM per infusion is the lower of either 20 mg/kg body weight or 1000 mg of iron (usually administered over 15 min) [28]. For FDI, elemental iron amounts administered per infusion can exceed 1000 mg based on a weight-related dose of 20 mg/kg [29] (although doses exceeding 1000 mg would require 30 min or more for administration).
Cost–utility analyses are a widely-used method to determine how best to allocate scarce financial resources for healthcare interventions, by evaluating the comparative costs of using different health technologies to improve health-related outcomes [30]. Given the high prevalence of IDA in China, as well as its significant QoL and cost implications, there is a need to determine the most cost-effective IV iron replacement therapy for individuals living with IDA. The objective of the present study was therefore to evaluate the cost–utility of FDI versus FCM in patients with IDA in China.
Methods
Patient-Level Simulation Model
A patient-level simulation model was developed in Microsoft Excel, based on a previously-published cost–utility model of a similar design [31]. The rationale for using a patient-level simulation model was informed by the National Institute for Health and Care Excellence Decision Support Unit’s technical guidance document [32], particularly the non-linear relationship between patient baseline characteristics (e.g., hemoglobin levels and body weight) and intermediate model outcomes (e.g., iron need). Other facets of the analysis that informed the decision to utilize a patient-level simulation model were the need to incorporate parameter-level stochastic variation, stochastic uncertainty, and individual patient variability.
Each simulated patient was assigned baseline values for age, body weight, and hemoglobin randomly sampled from baseline distributions. The mean iron need for each patient was then determined using these assigned baseline values combined with the simplified tables of iron need from the respective summaries of product characteristics (Table 1), alongside the total number of treatment courses that each patient would require.
Based on the modeled number of infusions administered per cycle, process-related QoL disutilities (decrements in QoL associated with patients engaging with a particular treatment process) and costs associated with the administration of IV iron were calculated. An equal proportion of patients in both treatment arms were assumed to achieve hematological response based on the findings of the PHOSPHARE-IBD RCT, which showed no significant difference in hematological response at any time point [33]. PHOSPHARE-IBD RCT results were also used as the basis of disease-related QoL data specific to each iron formulation. Monte Carlo methods were employed to explore alternative results and outcomes for simulated patients, using the built-in individual-level variability and parameter-level stochastic variation. QoL outcomes and costs over the complete time horizon were determined for each patient in each model cycle. Results were recorded and analyzed based on the entire patient cohort results dataset.
Cost outcomes were reported in 2023 Renminbi (RMB) and were reported and summarized alongside quality-adjusted life expectancy outcomes expressed in quality-adjusted life years (QALYs), and survival outcomes. The final incremental cost–utility ratio (ICUR) was calculated using the differences in these outcomes between the FDI and FCM arms.
Clinical Data and Patient Characteristics
A pragmatic search of the published literature was conducted to identify data on the safety and effectiveness of FDI and FCM. Specifically, a 2019 systematic review [34] and 2020 network meta-analysis investigating IV iron-related hypophosphatemia [35] were used to identify studies to parameterize the model. Data on hypophosphatemia incidence and the safety of the two IV iron formulations were also obtained from two additional literature reviews [24, 36]. To ensure that all clinical information was current, a further supplementary search was conducted to identify any RCTs published after the original pragmatic search was completed. The present study is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Both FDI and FCM were assumed to result in the same time to recurrence of anemia, and an equivalent initial increase in hemoglobin levels. Chinese life tables were used to model background mortality. Simulated baseline patient characteristics were obtained from the NCT03591406 RCT, which investigated FCM compared with iron sucrose in patients with IDA in China [37]. These characteristics included body weight (60.07 kg), mean age (39.4 years), and pre-treatment hemoglobin levels (7.9 g/dL; Table 2). The median time to iron retreatment was taken to be 16 months [38]. Regarding adverse events, 3.4% of patients receiving FDI and 65.1% of patients receiving FCM had hypophosphatemia at day 14, informed by the findings of the PHOSPHARE-IDA RCTs [27]. Severe hypophosphatemia was modeled in 0.0% of patients receiving FDI, and 7.3% of patients receiving FCM, also based on the findings of the PHOSPHARE-IDA RCTs [27]. Hypophosphatemic osteomalacia was omitted from the analysis.
Perspective, Time Horizon, and Discounting
Costs were investigated from the perspective of the Chinese healthcare system. All costs were calculated and reported in 2023 RMB. An annual discount rate of 5.0% was applied to future QoL effects and costs, based on 2020 guidelines for pharmaco-economic evaluations in China [39]. As no formal willingness-to-pay (WTP) threshold is currently published in China, a WTP threshold of RMB 85,698 per QALY gained was used, representing the 2022 Chinese Gross Domestic Product per capita [40].
A 5-year time horizon was adopted to ensure that the chronic and long-term impacts of IDA and its treatment could be effectively captured, by allowing multiple IDA treatment cycles to be modeled in patients with IDA secondary to chronic conditions. A monthly cycle length was adopted in the model, allowing iron treatment courses and hypophosphatemia-related monitoring and treatment to be captured over multiple intra-annual cycles to more precisely reflect real-world practice. This also allowed a gradual reversion to baseline hemoglobin levels in patients with chronic underlying etiologies of IDA to occur within a single year, whilst alleviating computational burden relative to shorter cycle lengths.
Resource Use
For each patient receiving FCM, it was assumed that two phosphate tests would be performed during each treatment course, based on recommendations from the published literature [41], a 2020 Drug Safety Update from the UK Medicines and Healthcare products Regulatory Agency (MHRA) focused on hypophosphatemia (and subsequent osteomalacia) associated with FCM [42], and the Chinese summary of product characteristics for FCM [43]. The phosphate tests were assumed to be performed ahead of the first infusion and at day 14, facilitating the detection of iatrogenic hypophosphatemia 14 days after the first iron infusion. It was assumed that no serum phosphate tests would be conducted in patients treated with FDI, and that no patients would therefore receive either phosphate tests or treatment with exogenous phosphate. This assumption was informed by the absence of any severe (and therefore more likely symptomatic) hypophosphatemia in patients treated with FDI in the PHOSPHARE-IDA RCTs. Conversely, with FCM, it was assumed that all patients in whom moderate or severe hypophosphatemia was present at day 14 (in line with the incidence rates from the PHOSPHARE-IDA RCTs) would receive IV phosphate therapy in line with recommendations from clinicians in China. For patients experiencing moderate hypophosphatemia, four phosphate infusions were assumed to be required for treatment, with six phosphate infusions assumed for patients experiencing severe hypophosphatemia [44].
Health-Related Quality of Life
Health state utility values were derived from the SF-36v2 generic patient-reported outcome questionnaire as administered in the PHOSPHARE-IBD RCT [45]. Participants in the trial were subject to identical dosage regimens based on their weight and hemoglobin levels, and received either FDI or FCM at two defined time intervals (baseline and day 35). SF-6Dv2 utility values were used as the basis for calculating differences in QoL for FDI and FCM recipients. To determine the SF-6Dv2 health state utility values (HSUVs), the study used ten items from the SF-36v2 questionnaire. The ten items were combined to form six health dimensions, each comprising 5–6 distinct health levels. To calculate the final SF-6Dv2 HSUVs, utility weights were applied, before summing the weighted scores for each of the six dimensions. Each weight comprised a negative value and would result in a decrement from the initial utility score of 1 (which represents full health). However, if the worst score for any dimension was experienced by patients, then an additional utility decrement was also applied [41]. The study applied China-specific process disutilities (decrements in QoL associated with patients engaging with or experiencing a particular treatment process, rather than due to the disease itself) [46]. A previously published diminishing marginal utility model was incorporated into the model for this purpose, and used to determine QoL decrements associated with IV iron infusions [47]. Specifically, as patients received more IV iron infusions, they experienced a marginal disutility that decreased on a logarithmic scale as the total number of infusions received increased. The premise for this diminishing marginal disutility was to capture how patients may adapt to receiving regular IV iron infusions over time, resulting in a gradually reducing treatment-related QoL burden.
Costs
The analysis was based on a unit price of RMB 63.60 per 100 mg of FDI and RMB 58.51 per 100-mg pack of FCM [48, 49]. The cost of administering the iron was assumed to be equal for both FDI and FCM on a per infusion basis, at RMB 33.66 per infusion [50]. The cost of one serum phosphate test was taken to be RMB 5.00 in line with the median charge for public medical services across Beijing, Guangzhou, Shanghai, Shenzhen, and Xiamen.
Hypophosphatemia treatment costs included the cost of intravenous phosphate in addition to the costs associated with administering the infusion. Specifically, a cost of RMB 431.09 was established for six IV phosphate infusions (in cases of severe hypophosphatemia treatment), and RMB 281.28 for four IV phosphate infusions (in cases of moderate hypophosphatemia treatment) [51].
Sensitivity Analysis
A series of one-way sensitivity analyses (OWSA) was conducted to assess the effects of varying individual model parameter values on the base case ICUR. Discount rates, baseline body weight and hemoglobin levels, and intravenous phosphate costs were among the parameters varied for the OWSA. In the probabilistic sensitivity analysis (PSA), 1000 Monte Carlo iterations were conducted to explore the effect of simultaneously varying model parameters by random sampling.
FCM Price Breakeven Analysis
As drug prices are subject to change over time, a series of analyses were conducted in which the list price of FCM was reduced from 100% of the base case value (of RMB 292.56) to 0% of the base case interval in 10% intervals. Results of the analyses were presented in the forms of incremental costs, ICURs, and the net monetary benefit of FDI versus FCM to establish the FCM price points at which FDI and FCM would be at overall cost parity from the payer perspective, and if there were any scenarios in which the conclusions regarding the cost-effectiveness findings from the base case analysis would change as a result of the reduced price of FCM.
Results
Base Case
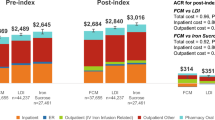
Over a 5-year time horizon, patients treated with FDI required 0.9 fewer iron infusions versus FCM over an average of 3.98 courses of iron (7.69 infusions with FCM vs. 6.79 infusions with FDI). Differences in the simplified tables of iron need between the two IV iron formulations resulted in an average of 6088 mg of FCM being administered per patient over 5 years versus 5297 mg of FDI.
The difference in the number of infusions resulted in iron procurement and administration cost savings of RMB 206 (RMB 3519 for FCM vs. RMB 3312 for FDI) and a process utility-driven gain of 0.0042 QALYs with FDI versus FCM. FDI was also associated with an additional 0.0663 QALYs based on hypophosphatemia-related fatigue as reported in the PHOSPHARE-IBD SF-6D data, and further cost savings of RMB 782, driven by the absence of serum phosphate testing and the administration of exogenous phosphate in patients treated with FDI. Overall, FDI therefore resulted in cost savings of RMB 989 and an improvement in quality-adjusted life expectancy of 0.0705 QALYs over 5 years. FDI was therefore the dominant intervention, associated with increased clinical benefit at a lower cost than FCM. A summary of the base case results is presented in Table 3.
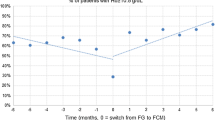
Probabilistic Sensitivity Analysis
In the PSA, ICURs from all model iterations fell within the south-eastern quadrant of the cost–utility plane (representing reduced costs and QALY gains), with FDI consistently being the dominant intervention relative to FCM (Fig. 1). At all WTP thresholds between RMB 0.00 and RMB 161,952 per QALY gained, FDI was 100% likely to be a cost-effective strategy.
One-way Sensitivity Analysis
The ten model parameters with the largest impact on the final base case ICUR in OWSA are presented in Fig. 2. Baseline body weight was the parameter with the largest effect on the ICUR. Specifically, a baseline body weight of 54.06 kg changed the ICUR by RMB −5649.48 per QALY gained, while a baseline body weight of 66.08 kg resulted in a change in the ICUR of RMB + 4621.09 per QALY gained. The cost discount rate was associated with the second greatest variation in the final ICUR; a cost discount rate of 0% changed the ICUR by RMB − 1201.69 per QALY gained, while a cost discount rate of 8% changed the ICUR by RMB + 619.31 per QALY gained.
FCM Price Breakeven Analysis
Results of the FCM price breakeven analyses are presented in Fig. 3. The analyses showed that FCM and FDI broke even with regard to the absolute costs from the Chinese healthcare system perspective with a 31% discount on the FCM list price used in the base case; however, there was no positive FCM price point at which FCM would be considered cost-effective relative to FDI based on a WTP threshold of RMB 85,698 per QALY, nor was there any price point at which there would be a net monetary benefit of using FCM versus FDI (Fig. 3).
Incremental costs, incremental cost–utility ratios, and net monetary benefit outcomes from analyses in which the unit price of ferric carboxymaltose was varied from 100 to 0% of the base case value. FCM ferric carboxymaltose, FDI ferric derisomaltose, ICUR incremental cost–utility ratio, IDA iron deficiency anemia, QALY quality-adjusted life year, RMB Renminbi
Discussion
The present study determined that FDI was the dominant intervention relative to FCM, driven in part by the significantly lower incidence of hypophosphatemia with FDI. FDI was projected to result in iron procurement and administration cost savings of RMB 206 (RMB 3519 for FCM vs. RMB 3312 for FDI) and an increase of 0.07 QALY versus FCM (2.50 QALYs for FCM and 2.57 QALYs for FDI) over a 5-year time horizon. An additional cost difference of RMB 782 arose from hypophosphatemia monitoring and treatment (RMB 782 for FCM, and RMB 0.0 for FDI). The lower iron administration costs with FDI were driven by patients receiving FCM requiring 0.9 additional infusions over a 5-year time horizon versus patients receiving FDI. The additional 0.9 infusions for FCM treatment may also be associated with increased productivity losses (specifically absenteeism) due to hospital visits, although these costs were not incorporated into the present analysis as they are not borne by the Chinese healthcare system. Similarly, cardiovascular (CV) and hypersensitivity (HSR) events (and the related costs and effects on quality of life) were also omitted from the analysis; recent indirect comparisons have shown FCM to be associated with higher risk of CV and HSR events than FDI, but further direct comparative evidence would be required to conclusively demonstrate this [52, 53].
To the knowledge of the authors, this cost–utility study of FCM versus FDI in patients with IDA is the first to be conducted within a Chinese healthcare setting. The final results were aligned with those from similar studies conducted within European healthcare settings, which also found FDI to be the dominant intervention versus FCM. In the European studies, additional costs associated with FCM primarily stemmed from the increased number of infusions required [54, 55]. The collective evidence suggests that FDI is likely to be cost-effective compared to FCM across a wide range of countries and healthcare settings, even as modeled patient characteristics in terms of hemoglobin levels, body weight, and co-morbidities vary substantially.
A key strength of this study was the use of China-specific sources for key model inputs. Specifically, costs associated with hospital stays, hypophosphatemia treatment, IV iron infusions, and serum phosphate tests were all obtained from sources specific to China. Regarding utility values, the disutilities associated with infusions were obtained from a time trade-off valuation study conducted with Chinese patient participants. In cases where data specific to China were unavailable, efforts were made to identify suitable proxies, although the generalizability of these to the Chinese setting could be considered a limitation of the study. Disease-related health state utility values were derived from the PHOSPHARE-IBD RCT, which enrolled a subpopulation of people living with IDA (i.e., those also living with IBD) and was conducted across five European countries [45]. When interpreting the results of the present study, the European provenance of the QoL data, and the etiology of the IDA (i.e., IBD) should be considered; populations with different underlying etiologies of IDA in different geographies may experience different QoL effects versus a general IDA population in China. For instance, fatigue is a known driver of reduced QoL in patients with IBD and IDA [56] and has been shown to be exacerbated by hypophosphatemia; however, it may not rank among the largest drivers of reduced QoL in a population of patients with IBD who also commonly experience symptoms such as diarrhea and constipation, abdominal pain, bleeding, or abnormal discharge [57]. In patients with IDA secondary to other conditions (where the range of symptoms and sequelae may be narrower than those of IBD), for instance, fatigue may be the dominant contributor to diminished QoL.
One further limitation of the analysis was that the model did not incorporate adherence and attendance rates for IV iron infusion appointments. As FCM can require more appointments relative to FDI to achieve correction of iron levels (particularly at higher doses) [28, 29], it is plausible that patients receiving FCM would have lower adherence rates than patients receiving FDI. The analysis was also based on relatively conservative estimates of the costs and downstream consequences of hypophosphatemia. Hypophosphatemia-related complications (e.g., hypophosphatemic osteomalacia and subsequent fractures) were omitted from the model, due to limited publicly-available clinical data. The omission was driven by the lack of robust, published data on the fracture rates associated with hypophosphatemia associated with IV iron administration in China; however, while the omission of costs associated with treating fractures still resulted in an analysis in which FDI was the dominant IV iron formulation, emerging data on fracture incidence after administration of FCM versus FDI suggest that the cost savings with FDI may have been greater still had fractures been incorporated into the analysis [58]. Similarly, the sources used in this study demonstrate that hypophosphatemia rates (particularly severe hypophosphatemia) are significantly higher for patients receiving FCM than for patients receiving FDI; if osteomalacia-related QoL and costs were to be included in the model proportionately to the rates of hypophosphatemia, it is plausible that FDI may be associated with additional cost savings and further increases in QoL relative to FCM.
A key characteristic of this analysis was that the model focused primarily on patients experiencing chronic IDA (i.e., IDA secondary to chronic underlying causes). In this patient group, there is a greater need for multiple, high-dose IV iron doses, which may contribute to the results showing the dominance of FDI over FCM. However, the outcome of dominance for FDI would also likely hold for acute causes of IDA requiring only one-off or short-term treatment with IV iron (e.g., peri-operative IV iron administration); the proportional clinical QoL and cost impacts would remain the same for patients with non-chronic acute IDA, simply occurring over a shorter timeframe. The more serious sequelae of chronic hypophosphatemia may not occur in patients with acute IDA, but the omission of these sequelae from the present analyses does not materially affect the results and yields outcomes that are less sensitive to the choice of time horizon [58].
Finally, the patient-level simulation approach selected for the present analysis allowed factors such as individual patient variability, stochastic uncertainty, and stochastic variation to be captured in the model [32]. This allowed for increased uncertainty around individual patient-projected outcomes to be incorporated as compared to a cohort-level model design. The use of such a model, alongside the incorporation of parameters informing the incidence of iron-related hypophosphatemia and its treatment facilitated a robust and comprehensive characterisation of the cost–utility of FDI versus FCM. The model structure used for this analysis also serves as a strong foundation for future studies aiming to determine the cost-effectiveness of various IV iron infusions.
Conclusion
The results showed that FDI would improve patient QoL and reduce direct healthcare expenditure versus FCM in patients with IDA in China, driven by FDI requiring comparatively fewer infusions over 5 years, incurring no hypophosphatemia-related monitoring or treatment costs, and not inducing hypophosphatemia-related fatigue.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
DeLoughery TG. Iron deficiency anemia. Med Clin North Am. 2017;101:319–32.
Kumar A, Sharma E, Marley A, et al. Iron deficiency anaemia: pathophysiology, assessment, practical management. BMJ Open Gastroenterol. 2022;9: e000759.
Pasricha S-R, Tye-Din J, Muckenthaler MU, et al. Iron deficiency. Lancet. 2021;397:233–48.
World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity [Internet]. Geneva: World Health Organization; 2011 [cited 2021 Sep 10]. Report No.: WHO/NMH/NHD/MNM/11.1. Available from: https://apps.who.int/iris/bitstream/handle/10665/85839/WHO_NMH_NHD_MNM_11.1_eng.pdf?sequence=22&isAllowed=y.
Kassebaum NJ, GBD 2013 Anemia Collaborators. The global burden of anemia. Hematol Oncol Clin North Am. 2016;30:247–308.
Tan J, He G, Qi Y, et al. Prevalence of anemia and iron deficiency anemia in Chinese pregnant women (IRON WOMEN): a national cross-sectional survey. BMC Pregnancy Childbirth. 2020;20:670.
Zheng H, Long W, Tan W, et al. Anaemia, iron deficiency, iron-deficiency anaemia and their associations with obesity among schoolchildren in Guangzhou. China Public Health Nutr. 2020;23:1693–702.
Nead KG, Halterman JS, Kaczorowski JM, et al. Overweight children and adolescents: a risk group for iron deficiency. Pediatrics. 2004;114:104–8.
Zhao L, Zhang X, Shen Y, et al. Obesity and iron deficiency: a quantitative meta-analysis. Obes Rev. 2015;16:1081–93.
Shokrgozar N, Golafshan HA. Molecular perspective of iron uptake, related diseases, and treatments. Blood Res. 2019;54:10–6.
Ando K, Morita S, Higashi T, et al. Health-related quality of life among Japanese women with iron-deficiency anemia. Qual Life Res. 2006;15:1559–63.
Cooke AG, McCavit TL, Buchanan GR, et al. Iron deficiency anemia in adolescents who present with heavy menstrual bleeding. J Pediatr Adolesc Gynecol. 2017;30:247–50.
Mirza FG, Abdul-Kadir R, Breymann C, et al. Impact and management of iron deficiency and iron deficiency anemia in women’s health. Expert Rev Hematol. 2018;11:727–36.
Anker SD, Kirwan B-A, van Veldhuisen DJ, et al. Effects of ferric carboxymaltose on hospitalisations and mortality rates in iron-deficient heart failure patients: an individual patient data meta-analysis. Eur J Heart Fail. 2018;20:125–33.
Danese S, Hoffman C, Vel S, et al. Anaemia from a patient perspective in inflammatory bowel disease: results from the European Federation of Crohn’s and Ulcerative Colitis Association’s online survey. Eur J Gastroenterol Hepatol. 2014;26:1385.
Gisbert JP, Bermejo F, Pajares R, et al. Oral and intravenous iron treatment in inflammatory bowel disease: hematological response and quality of life improvement. Inflamm Bowel Dis. 2009;15:1485–91.
García-López S, Bocos JM, Gisbert JP, et al. High-dose intravenous treatment in iron deficiency anaemia in inflammatory bowel disease: early efficacy and impact on quality of life. Blood Transfus. 2016;14:199–205.
Taylor S, Rampton D. Treatment of iron deficiency anemia: practical considerations. Pol Arch Med Wewn. 2015;125:452–60.
Onken JE, Bregman DB, Harrington RA, et al. A multicenter, randomized, active-controlled study to investigate the efficacy and safety of intravenous ferric carboxymaltose in patients with iron deficiency anemia. Transfusion (Paris). 2014;54:306–15.
Rozen-Zvi B, Gafter-Gvili A, Paul M, et al. Intravenous versus oral iron supplementation for the treatment of anemia in CKD: systematic review and meta-analysis. Am J Kidney Dis. 2008;52:897–906.
Koutroubakis IE, Oustamanolakis P, Karakoidas C, et al. Safety and efficacy of total-dose infusion of low molecular weight iron dextran for iron deficiency anemia in patients with inflammatory bowel disease. Dig Dis Sci. 2010;55:2327–31.
Schröder O, Mickisch O, Seidler U, et al. Intravenous iron sucrose versus oral iron supplementation for the treatment of iron deficiency anemia in patients with inflammatory bowel disease–a randomized, controlled, open-label, multicenter study. Am J Gastroenterol. 2005;100:2503–9.
Boots JMM, Quax RAM. High-dose intravenous iron with either ferric carboxymaltose or ferric derisomaltose: a benefit-risk assessment. Drug Saf. 2022;45:1019–36.
Schaefer B, Tobiasch M, Wagner S, et al. Hypophosphatemia after intravenous iron therapy: comprehensive review of clinical findings and recommendations for management. Bone. 2022;154: 116202.
Zoller H, Schaefer B, Glodny B. Iron-induced hypophosphatemia: an emerging complication. Curr Opin Nephrol Hypertens. 2017;26:266–75.
Glaspy JA, Lim-Watson MZ, Libre MA, et al. Hypophosphatemia associated with intravenous iron therapies for iron deficiency anemia: a systematic literature review. Ther Clin Risk Manag. 2020;16:245–59.
Wolf M, Rubin J, Achebe MM, et al. Effects of iron isomaltoside vs ferric carboxymaltose on hypophosphatemia in iron-deficiency anemia: two randomized clinical trials. JAMA. 2020;323:432–43.
emc. Ferinject (ferric carboxymaltose)—Summary of Product Characteristics (SmPC) [Internet]. [cited 2022 Oct 18]. Available from: https://www.medicines.org.uk/emc/product/5910/smpc.
emc. Ferric derisomaltose Pharmacosmos 100 mg/ml solution for injection/infusion - Summary of Product Characteristics (SmPC) [Internet]. [cited 2023 Jul 12]. Available from: https://www.medicines.org.uk/emc/product/5676/smpc.
Greenhawt M, Oppenheimer J, Codispoti CD. A practical guide to understanding cost-effectiveness analyses. J Allergy Clin Immunol Pract. 2021;9:4200–7.
Hu S, Liu L, Pollock RF, et al. Intravenous iron for the treatment of iron deficiency anemia in China: a patient-level simulation model and cost–utility analysis comparing ferric derisomaltose with iron sucrose. J Med Econ. 2022;25:561–70.
Davis S, Stevenson M, Tappenden P, et al. NICE DSU Technical Support Document 15: Cost-Effectiveness Modelling Using Patient-Level Simulation. Sheffield; 2014.
Zoller H, Wolf M, Blumenstein I, et al. Hypophosphataemia following ferric derisomaltose and ferric carboxymaltose in patients with iron deficiency anaemia due to inflammatory bowel disease (PHOSPHARE-IBD): a randomised clinical trial. Gut. 2023;72:644–53.
Pollock RF, Muduma G. A systematic literature review and indirect comparison of iron isomaltoside and ferric carboxymaltose in iron deficiency anemia after failure or intolerance of oral iron treatment. Expert Rev Hematol. 2019;12:129–36.
Bellos I, Frountzas M, Pergialiotis V. Comparative risk of hypophosphatemia following the administration of intravenous iron formulations: a network meta-analysis. Transfus Med Rev. 2020;34:188–94.
Blumenstein I, Shanbhag S, Langguth P, et al. Newer formulations of intravenous iron: a review of their chemistry and key safety aspects—hypersensitivity, hypophosphatemia, and cardiovascular safety. Expert Opin Drug Saf. 2021;20:757–69.
Vifor International. To assess the impact of ferric carboxymaltose compared with iron sucrose in Chinese subjects on correcting iron deficiency anaemia: study results [Internet]. Vifor International; 2021 [cited 2023 Jul 10]. Available from: https://clinicaltrials.gov/ct2/show/results/NCT03591406.
Kulnigg S, Teischinger L, Dejaco C, et al. Rapid recurrence of IBD-associated anemia and iron deficiency after intravenous iron sucrose and erythropoietin treatment. Am J Gastroenterol. 2009;104:1460–7.
Chen Y, Guan H, Han S, et al. China guidelines for pharmacoeconomic evaluations: 2020 edition [Internet]. Chinese Pharmaceutical Association and China Society for Pharmacoeconomics and Outcomes Research and ISPOR Beijing Chapter; 2020 [cited 2022 Jan 4]. Available from: https://tools.ispor.org/PEguidelines/source/China-Guidelines-for-Pharmacoeconomic-Evaluations-2020.pdf.
National Bureau of Statistics of China. China Statistical Yearbook 2022 [Internet]. [cited 2023 Jul 11]. Available from: http://www.stats.gov.cn/sj/ndsj/2022/indexeh.htm.
Kassianides X, Bhandari S. Hypophosphataemia, fibroblast growth factor 23 and third-generation intravenous iron compounds: a narrative review. Drugs Context. 2021;10:1–29.
Medicines and Healthcare products Regulatory Agency. Drug safety update: ferric carboxymaltose (Ferinject▼): risk of symptomatic hypophosphataemia leading to osteomalacia and fractures [Internet]. GOV.UK. 2020 [cited 2021 Aug 12]. Available from: https://www.gov.uk/drug-safety-update/ferric-carboxymaltose-ferinject-risk-of-symptomatic-hypophosphataemia-leading-to-osteomalacia-and-fractures.
Vifor (International) Inc. 羧基麦芽糖铁注射液说明书 (Ferric Carboxymaltose Injection Instructions) [Internet]. 2022 [cited 2024 May 11]. Available from: https://www.cde.org.cn/main/xxgk/postmarketpage?acceptidCODE=6478f58c64df7738227a2feb78a4214a.
Fresenius Kabi China. 格利福斯® - 费森尤斯卡比中国 (Glifos® Fresenius Kabi China) [Internet]. [cited 2024 May 11]. Available from: https://www.fresenius-kabi.com/cn/我们的产品/格利福斯.
Pharmacosmos A/S. A trial comparing the incidence of hypophosphatemia in relation to treatment with iron isomaltoside and ferric carboxymaltose in subjects with iron deficiency anaemia due to inflammatory bowel disease [Internet]. 2021 [cited 2023 Jul 11]. Available from: https://clinicaltrials.gov/ct2/show/NCT03466983.
Brennan VK, Dixon S. Incorporating process utility into quality adjusted life years: a systematic review of empirical studies. Pharmacoeconomics. 2013;31:677–91.
Hu S, Wu D, Wu J, et al. Disutilities associated with intravenous iron infusions: results from a time trade-off survey and diminishing marginal utility model for treatment attributes in China. Patient Relat Outcome Meas. 2023;14:253–67.
Kangzhou Big Data (Group) Co., Ltd. 健康产业大数据服务与赋能平台 (Health industry big data service and empowerment platform): Ferric Derisomaltose [Internet]. [cited 2024 May 11]. Available from: https://www.yaozh.com/.
Kangzhou Big Data (Group) Co., Ltd. 健康产业大数据服务与赋能平台 (Health industry big data service and empowerment platform): Ferric Carboxymaltose [Internet]. [cited 2024 May 11]. Available from: https://www.yaozh.com/.
博鳌恒大国际医院 (Boao Evergrande International Hospital). Public procurement platform of Hainan Boao Evergrande International Hospital [Internet]. [cited 2024 May 11]. Available from: http://boaohospital.com/.
Kangzhou Big Data (Group) Co., Ltd. 健康产业大数据服务与赋能平台 (Health industry big data service and empowerment platform): Sodium Glycerophosphate Injection [Internet]. [cited 2024 May 11]. Available from: https://www.yaozh.com/.
Pollock RF, Kalra PA, Kalra PR, et al. A systematic review, meta-analysis, and indirect comparison of blindly adjudicated cardiovascular event incidence with ferric derisomaltose, ferric carboxymaltose, and iron sucrose. Adv Ther. 2022;39:4678–91.
Pollock RF, Biggar P. Indirect methods of comparison of the safety of ferric derisomaltose, iron sucrose and ferric carboxymaltose in the treatment of iron deficiency anemia. Expert Rev Hematol. 2020;13:187–95.
Pollock RF, Muduma G. An economic analysis of ferric derisomaltose versus ferric carboxymaltose in the treatment of iron deficiency anemia in patients with inflammatory bowel disease in Norway, Sweden, and Finland. Clin Outcomes Res. 2021;13:9–18.
Pollock RF, Muduma G. A patient-level cost-effectiveness analysis of iron isomaltoside versus ferric carboxymaltose for the treatment of iron deficiency anemia in the United Kingdom. J Med Econ. 2020;23:751–9.
Nocerino A, Nguyen A, Agrawal M, et al. Fatigue in inflammatory bowel diseases: etiologies and management. Adv Ther. 2020;37:97–112.
McDowell C, Farooq U, Haseeb M. Inflammatory bowel disease. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 [cited 2023 Dec 15]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK470312/.
Zoller H, Pammer LM, Schaefer B, et al. Incidence of fractures after intravenous iron: a retrospective analysis comparing ferric carboxymaltose and ferric derisomaltose. Blood [Internet]. ASH; 2023 [cited 2023 Nov 10]. p. 3838. Available from: https://ash.confex.com/ash/2023/webprogram/Paper174508.html.
Funding
Pharmacosmos A/S funded the development of the health economic model and analysis, preparation of the manuscript, and the article processing charge and open access fee for the manuscript.
Author information
Authors and Affiliations
Contributions
Richard F. Pollock conceived and designed the analysis. Fengkui Zhang and Aizong Shen provided input on the clinical assumptions and resource utilization in China. Richard F. Pollock developed the simulation model and conducted statistical and health economic analyses. Waqas Ahmed conducted health economic and sensitivity analyses, generated tables and figures, and prepared the first draft of the manuscript, which was revised critically for intellectual content by all authors. All authors approved the final version to be published. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of Interest
Richard F. Pollock is a full-time employee, director, and shareholder in, and Waqas Ahmed is a full-time employee of, Covalence Research Ltd, which received consultancy fees from Pharmacosmos A/S to develop the patient-level simulation model and analysis and to prepare the manuscript. Fengkui Zhang and Aizong Shen have no competing interests to declare.
Ethical Approval
The present study is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Additional information
Prior presentation: Select analyses presented here were presented previously at ISPOR Europe 2023 (Copenhagen, November 12 to November 15, 2023) as poster EE266. A preprint version of this article was made available in medRxiv on July 11, 2024 here: https://www.medrxiv.org/content/10.1101/2024.07.11.24310267v1.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zhang, F., Shen, A., Ahmed, W. et al. A Cost-Utility Analysis of Ferric Derisomaltose Versus Ferric Carboxymaltose in Patients with Iron Deficiency Anemia in China. Adv Ther (2024). https://doi.org/10.1007/s12325-024-02987-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12325-024-02987-7