Abstract
Background
Recent studies have identified the presence of cancer-associated fibroblasts (CAFs) within glioblastoma (GBM), yet their biological roles and underlying mechanisms remain poorly understood. This study aimed to construct a CAF-related prognostic model to guide patient prognosis and treatment strategies.
Method
We employed various bioinformatics methods, including enrichment analysis, Weighted Gene Co-expression Network Analysis (WGCNA), Lasso regression analysis, and machine learning techniques such as XGBoost and Random Forest, to develop a novel risk index termed CAFscore. Patients were stratified into high and low CAFscore groups for subsequent survival analysis. The area under the curve (AUC) and concordance index (C-index) for CAFscore were calculated and compared against other clinical characteristics and existing prognostic models. Drug sensitivity assessments were conducted using the Oncopredict package. Functional validation of key genes was performed through scratch and invasion assays in GBM cells.
Results
Our analyses revealed four core CAF-related genes, leading to the establishment of CAFscore. Notably, patients in the high CAFscore group exhibited significantly reduced survival and exhibited enrichment in epithelial-mesenchymal transition (EMT) and inflammation response pathways. Furthermore, CAFscore showed a significant negative correlation with the sensitivity to irinotecan and its analogs, while demonstrating a positive correlation with sensitivity to 505,124 (a TGFβRI inhibitor). LRP10 emerged as a central gene within the CAFscore, displaying markedly elevated expression in GBM and a strong association with CAF infiltration. Silencing LRP10 significantly inhibited the invasive capabilities of GBM cells.
Conclusion
This study presented the first CAF related prognostic model (CAFscore) in GBM, and demonstrated that the model could effectively guide patient prognosis and potentially inform personalized treatment strategies. The core gene of CAFscore, LRP10, was significantly overexpressed in GBM and might play a pivotal role in regulating CAF infiltration as well as tumor invasion and metastasis, highlighting LRP10 as a promising therapeutic target for GBM management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Glioblastoma (GBM), classified as World Health Organization (WHO) grade IV brain tumor, exhibits a notoriously poor prognosis. Previous studies revealed that the median survival duration after surgical resection alone was approximately four months, while the incorporation of adjuvant radiotherapy and chemotherapy could extend this median survival to around 15 months [1, 2]. This alarming statistic underscores the aggressive nature of this malignancy, which is not only resistant to conventional therapies but also prone to early recurrence following treatment [3]. The challenges in managing GBM are multifaceted. First, the tumor's location within the cranial cavity poses significant surgical risks, often leading to substantial impairments in neurological and functional capacities post-operation. This not only complicates surgical interventions but also affects patients' quality of life significantly [4]. Furthermore, the development of effective pharmacological treatments remains sluggish; apart from Bevacizumab and the chemotherapeutic agent Temozolomide, novel approaches such as immunotherapy and targeted therapies have yet to yield meaningful improvements in patient outcomes [3, 5, 6]. Compounding these difficulties is the still-elusive understanding of the mechanisms underlying GBM's onset and progression, which hampers the development of more effective therapeutic strategies. Therefore, it is crucial to enhance our understanding of the tumor microenvironment and the complex interactions between GBM cells and surrounding cellular constituents. Deepening this knowledge holds the potential to unveil novel therapeutic targets and inform clinical strategies, ultimately leading to improved prognoses for patients suffering from this devastating disease.
Cancer-associated fibroblasts (CAFs) are a critical component of the tumor microenvironment (TME), playing a pivotal role in various malignancies [7]. In most tumors, CAFs have been identified as facilitators of tumor invasion and metastasis, while also contributing to the formation of an immunosuppressive microenvironment that assists in tumor progression [8,9,10]. The interaction between CAFs and cancer cells leads to an altered extracellular matrix and promotes a supportive niche for tumor development. In recent studies, the presence of CAFs in GBM has been increasingly recognized, revealing their significant contribution to tumor growth and progression [11, 12]. For instance, proteomic analyses have indicated that CAFs in GBM may exert their pro-tumoral effects through the secretion of fibronectin-1 (FN1), a key extracellular matrix protein that enhances tumor cell proliferation and survival [11]. This aligns with the increasingly acknowledged role of CAFs in modulating the TME and influencing tumor behavior [13]. However, despite these advancements, our understanding of the precise mechanisms by which CAFs operate in the context of GBM remains limited. Comprehensive investigations are required to further elucidate the interactions between CAFs and GBM cells, as well as the downstream signaling pathways involved. This gap in knowledge presents both a challenge and an opportunity for future research directed towards targeted therapeutic strategies aimed at disrupting the fibrotic tumor microenvironment and improving clinical outcomes in GBM patients.
In this work, we employed marker genes associated with CAFs identified by Saket Jain et al. in GBM [12] and calculated the enrichment scores in this malignancy. Our findings indicated a significant correlation between the enrichment scores related to CAFs and the prognosis of GBM patients. To further explore this relationship, we utilized Weighted Gene Co-Expression Network Analysis (WGCNA) alongside machine learning techniques to develop a novel CAF-related risk score (CAFscore). This risk score might offer an effective tool for guiding prognostic assessments in GBM patients and have the potential to inform personalized treatment strategies. Additionally, we investigated the role of a core constituent gene from the CAF-related risk score, LRP10, in the context of GBM.
2 Method
2.1 Public data acquisition and processing
The RNA sequence data and clinical information of The Cancer Genome Atlas (TCGA) Glioblastoma (GBM) cohort were accessible at https://portal.gdc.cancer.gov. The CGGA-301, CGGA-325, and CGGA-693 datasets were obtained from the Chinese Glioma Genome Atlas (CGGA) database (http://www.cgga.org.cn/index.jsp). The TCGA-GBM datasets were processed as described in previous study [14]. For the RNA mRNA sequencing data from CGGA-325 and CGGA-693, we utilized the “sva” package in R software to consolidate these datasets into a unified cohort, which was named as “CGGA-Meta” cohort. Importantly, since all data utilized in this study were sourced from public databases, no additional ethical approval was required, ensuring compliance with ethical standards in biomedical research.
2.2 Construction of CAFscore in GBM
The process of constructing CAFscore was summarized in the flowchat (supplementary Fig. 1A). Firstly, Gene Set Variation Analysis (GSVA) by the “GSVA” R package was used to assess the enrichment score based on 18 CAF marker genes [12]: Actin Alpha Cardiac Muscle 2 (ACTA2), Fibroblast Activation Protein Alpha (FAP), Platelet-Derived Growth Factor Receptor Alpha (PDGFRA), Platelet-Derived Growth Factor Receptor Beta (PDGFRB), Podoplanin (PDPN), S100 Calcium Binding Protein A4 (S100A4), Tenascin C (TNC), Vimentin (VIM), Collagen Type I Alpha 1 Chain (COL1A1), Coiled-Coil Domain Containing 80 (CCDC80), Biglycan (BGN), Collagen Type IV Alpha 2 Chain (COL4A2), Collagen Type V Alpha 1 Chain (COL5A1), Nuclear Receptor Subfamily 2 Group F Member 2 (NR2F2), Collagen Type III Alpha 1 Chain (COL3A1), Inhibin Subunit Beta A (INHBA), Stanniocalcin 2 (STC2), and Lysyl Oxidase Like 2 (LOXL2). The enrichment score was named as CAF enrichment score (CAF ES).
Weighted Gene Co-expression Network Analysis (WGCNA) was then employed to identify co-expressed gene modules associated with CAF ES in three GBM datasets (TCGA-GBM, CGGA-301, and CGGA-Meta). Generally, the gene expression data were filtered for genes with a minimum variance to remove low-expression noise, and the top 10, 000 genes ranked by mean expression were then used for construction of the similarity matrix, followed by the application of a soft-thresholding power to obtain an adjacency matrix. We selected an optimal power by evaluating scale-free topology, ensuring a high degree of connectivity among genes. The adjacency matrix was transformed into a topological overlap matrix (TOM) to measure gene pairwise similarities. Hierarchical clustering was performed on the TOM, allowing us to identify distinct gene modules. We employed dynamic tree cutting to delineate modules, establishing a minimum module size of 30 genes for robust detection. Module-trait associations were evaluated by correlating the module eigengenes with CAF ES, using a Pearson correlation approach. Statistical significance was determined through permutation tests.
The genes in modules highly correlated with CAF ES were then intersected to obtain the common genes, which were then further selected by three machine learning methods, namely Least absolute shrinkage and selection operator (LASSO) regression model by the ‘glmnet’ R package, XGBoost by the ‘xgboost’ R package, and Random Forest by the ‘randomForestSRC’ R package. Four genes were commonly selected by these methods and were then underwent multi-variate Cox regression analyses. The risk score for each patient was calculated by the formula: score = \(\sum {_{i} } \,Coefficient\,(Gene\,i)\,\,*\,Expression(Gene\,\,i)\). The CAFscore of patients in each cohort was calculated with the formula: CAFscore = (score-Min) / absolute (Max), as reported in previous studies [14, 15].
2.3 Gene set enrichment analysis (GSEA)
GSEA on GBM patient datasets was conducted by utilizing the ‘clusterProfiler’ package within R. We selected the c5.go.bp.v2022.1.Hs.symbols.gmt as our gene set database to investigate the biological processes associated with gene expression alterations in GBM. Visualizations were achieved by using the ‘GseaVis’ package in R [16].
2.4 Cell transfection and qRT-PCR
Human glioma cells U251 and U-87MG were obtained from the Cell Bank of the Shanghai Institute of Biological Sciences, Chinese Academy of Sciences. Cells were cultured in a DMEM medium containing 10% FBS under humidified conditions of 5% CO2 and 37 °C. The si-LRP10 and negative control sequences were acquired from Shanghai Gemma Gene. The transfection of siRNAs into GBM cells was conducted using Lipo8000™ transfection reagent (Beyotime, C0533, China). Quantitative PCR (qPCR) was utilized to assess the expression levels of target genes, employing BeyoFast™ SYBR Green qPCR Mix (Beyotime, D7262, China). The specific sequences for siRNA and qPCR primers are detailed in Supplementary Table 1.
2.5 Cell scratch test
GBM cells were seeded in 6-well plates and subjected to a scratch assay utilizing a 200 μL pipette tip to create a wound. Following this, the cells were maintained in medium containing 1% fetal bovine serum (FBS). Images of the scratched area were captured at baseline (0 h) and at subsequent 24-h time points to assess cell migration.
2.6 Cell invasion assay
1 × 10^5 transfected cells were plated in 500 μl of RPMI-1640 medium within the upper chamber of Corning® BioCoatTM Matrigel® Invasion Chambers (8 mm pore size; Corning, USA). The lower chamber was supplemented with 750 μl of RPMI-1640 medium enriched with 30% FBS. The cells were incubated for 24 h at 37 °C in a 5% CO2 atmosphere. Following incubation, the cells were fixed using 4% paraformaldehyde and subsequently stained with Giemsa Stain solution (Sigma, USA). Cell invasion was assessed by examining the bottom of the membrane under a microscope, and the number of cells was quantified by counting in three randomly selected fields at 100 × magnification. All experiments were conducted in triplicate to ensure reproducibility.
2.7 Statistical analysis
All data were processed, analyzed, and visualized using R software (version 4.4.1). Key R packages employed include “tidyverse”, “enrichplot”, “survival”, “msigdbr”, “org.Hs.eg.db”, “ggplot2”, “VennDiagram”, “aplot”, “survivalROC”, “ggrepel”, “corrplot”, “survminer”, “timeROC”, “rms”, “pec”, “ggalluvial”, “Oncopredict”, and “CompareC”. Prognosis analyses were performed using the Kaplan–Meier method, while Pearson’s correlation method was applied for correlation analyses. Continuous variables were assessed through the Wilcoxon rank-sum test, with statistical significance defined as p < 0.05 (*, p < 0.05; **, p < 0.01; ***, p < 0.001; ****, p < 0.0001).
3 Result
3.1 CAF enrichment score correlated with prognosis of GBM patients
In this study, we firstly calculated the CAF enrichment scores (CAF ES) for GBM patients across three datasets (TCGA-GBM, CGGA-301, and CGGA-meta datasets) using GSVA based on 18 CAF-related marker genes identified by Saket Jain et al. (namely ACTA2, FAP, PDGFRA, PDGFRB, PDPN, S100A4, TNC, VIM, COL1A1, CCDC80, BGN, COL4A2, COL5A1, NR2F2, COL3A1, INHBA, STC2, and LOXL2). As shown in Fig. 1A–C, CAF ES had a strong positive correlation with the expression of three core genes (ACTA2, COL1A1, and TNC) which were most frequently expressed in CAFs in GBM [12]. Besides, a highly positive relationship between CAF ES and CAF infiltration levels was also observed (Fig. 1D–E). Furthermore, inspired by Professor Phillip M Galbo Jr et al.’s work, we indeed observed a highly positive correlation between CAF ES and expression of FN1 (Fig. 1F), a gene which might serve as a mediator of CAFs in GBM [11]. These results reinforce the hypothesis that CAF ES might reflect CAF infiltration in GBM. Further, higher CAF ES correlated with worse patient survival outcomes across the three datasets (Fig. 1G-1I), further supporting a potential pro-tumor role of CAF in GBM.
CAF enrichement score correlated with survival outcome of GBM patients. (A–C) Correlation analyses between CAF enrichment score and expression of TNC (A), COL1A1 (B), and ACTA2 (C). (D-E) Correlation analyses between CAF enrichment score and infiltration of CAF measured by the EPIC (D) and MCPcounter (E) methods. (F) Correlation analyses between CAF enrichment score and expression of FN1. (G-I) Prognosis analyses of CAF enrichment score (CAF ES) in GBM cohorts: TCGA-GBM (G), CGGA-Meta (H), and CGGA-301 (I)
3.2 Construction of CAFscore in GBM
To investigate the core genes involving in the biological process of CAF in GBM, we utilized WGCNA across multiple datasets (Fig. 2A–C). In the CGGA-301 dataset, the blue and magenta modules were found to be the top two ones highly, positively associated with CAF-ES (Fig. 2D–G). In the CGGA-Meta dataset, the green and brown modules exhibited strongest correlation with CAF-ES (Fig. 2E–H). Furthermore, in the TCGA-GBM dataset, the light cyan and purple modules were identified as highly relevant to CAF-ES (Fig. 2F–I).
WGCNA analyses of CAF ES in GBM datasets. (A-C) Cluster dendrogram plot of CAF ES in TCGA-GBM (A), CGGA-Meta (B), and CGGA-301 (C). (D-F) Module-trait relationship plot of CAF ES in TCGA-GBM (D), CGGA-Meta (E), and CGGA-301 (F). (G-I) Correlation analyses between gene significance of CAF ES and module membership in purple module from TCGA-GBM (G), green module from CGGA-Meta (H), and blue module from CGGA-301 (I) datasets
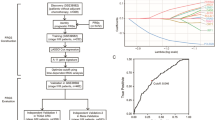
A total of 164 common genes were then identified by intersecting the module genes across three datasets (Supplementary Table 2). To further refine our findings, we employed three machine learning techniques: LASSO regression, XGBoost, and Random Forest. These methods yielded 20 (Fig. 3A), 15 (Fig. 3B), and 66 (Fig. 3C) key genes, respectively. Notably, four genes—SOCS3, LRP10, GADD45A, and OCIAD2—were consistently identified as core genes across all three methodologies (Fig. 3D). Subsequent multivariate regression analysis revealed that SOCS3, LRP10, and GADD45A served as independent prognostic factors, maintaining their significance in predicting patient outcomes (Fig. 3E). We then constructed a risk score, termed CAFscore, by multiplying the expression levels of these four genes by their respective coefficients (details provided in the Methods section). Consistent with findings in a previous study by Phillip M. Galbo, Jr et al. that CAFs are associated with a proneural-to-mesenchymal transition in GBM [11], CAFscores were highest in the mesenchymal subtype and lowest in the proneural subtype (supplementary Fig. 1B). Utilizing the median CAFscore as a cutoff value, we categorized GBM patients into high-CAFscore and low-CAFscore groups in each cohort. Prognostic analysis indicated that patients in the high-CAFscore group demonstrated significantly shorter survival times across three cohorts: CGGA-301 (Fig. 3F, p < 0.0001), TCGA-GBM (Fig. 3G, p = 0.0016), and CGGA-meta (Fig. 3H, p = 0.017).
Construction of CAFscore. (A-C) Identification of core CAF related genes via LASSO regression (A), XGBoost (B) and Randomforest (C) methods. (D) Venn diagram of core genes identified by three machine learning methods. (E) Multi-variate Cox regression analysis of the four core genes in CGGA-301 cohort. (F–H) Prognosis analyses of CAFscore in GBM cohorts: CGGA-301 (F), TCGA-GBM (G), and CGGA-Meta (H)
3.3 Comparison of CAFscore with other prognostic models
In the analysis of GBM prognosis across various datasets, the CAFscore demonstrated promising predictive capabilities. In the CGGA301 cohort, the Area Under the Curve (AUC) values for CAFscore were 0.76 at one year, 0.77 at three years, and 0.782 at five years (Fig. 4A). Besides, in the TCGA-GBM dataset, the AUC values were 0.63, 0.75, and 0.681 for the corresponding time points (Fig. 4A). The CGGA-meta dataset presented AUCs of 0.63 at one year, 0.65 at three years, and 0.698 at five years (Fig. 4A).
Comparison of CAFscore and other models. (A) The 1-, 3-, and 5-year AUC value of the CAFscore in the CGGA-301, CGGA-Meta, and TCGA-GBM cohorts. (B) The performance of CAFscore was compared with other clinical features in predicting overall survival of GBM patients in the CGGA-301, CGGA-Meta, and TCGA-GBM cohorts. (C–E) C-index analyses of the CAFscore and 26 published mRNA signatures in the CGGA-301 (C), CGGA-Meta (D), and TCGA-GBM (E) cohorts
Moreover, CAFscore exhibited superior C-index values compared to most clinical factors, such as gender, age, and TCGA subtype classifications (Fig. 4B). Furthermore, we extracted 26 mRNA signatures from the Pubmed database for additional comparison (supplementary Table 3). These signatures were associated with various biological processes, such as ferroptosis, immune process, DNA methylation, RNA methylation, and invasion. The C-index for CAFscore in the three datasets was calculated as 0.678 ± 0.027, 0.60 ± 0.024, and 0.588 ± 0.027, respectively. Among all analyzed models, CAFscore secured the highest C-index ranking in the CGGA301 dataset (Fig. 4C), while it was ranked third and fifth in CGGA-Meta (Fig. 4D) and TCGA-GBM (Fig. 4F) datasets, respectively.
3.4 Guidance of CAFscore in anti-tumor therapy
We further aimed to elucidate the biological differences between high CAFscore and low CAFscore GBM patient groups by performing enrichment analysis on their differentially expressed genes. Results from both the CGGA-301 dataset (Fig. 5A) and TCGA-GBM dataset (Fig. 5B) revealed that the high CAFscore cohort was primarily enriched in pathways related to inflammatory response and epithelial-mesenchymal transition (EMT). Conversely, the low CAFscore group showed significant enrichment in proliferation-associated signaling pathways, such as mitotic spindle formation (Fig. 5A, B).
Biological features of CAFscore in GBM. (A–B) GSEA of patients in the high-CAFscore and low-CAFscore groups of GBM patients from the CGGA-301 (A) and TCGA-GBM (B) cohorts. (C) Enrichment analysis of four core genes in GBM patients by utilizing the CancerSEA database. (D–G) Correlation analyses between CAFscore and drug sensitivity of Irinotecan (D), camptothecin (E), topotecan (F), and SB505124 (G). *p < 0.05, **p < 0.01
Furthermore, utilizing the CancerSEA database (http://biocc.hrbmu.edu.cn/CancerSEA/home.jsp), which specializes in decoding distinct functional states of cancer cells at single-cell resolution [17], we conducted enrichment analysis on four core genes. The findings indicated that these genes in GBM were closely associated with metastasis, EMT, and inflammation (Fig. 5C). Additionally, we explored the correlation between CAFscore and drug sensitivity. Our results showed a significant negative correlation between CAFscore and sensitivity to irinotecan and its analogs (Fig. 5D–F), while a positive correlation was observed with the sensitivity to SB505124, an selective inhibitor of TGFβRI (Fig. 5G). This suggested that GBM patients with high CAFscores might exhibit resistance to irinotecan treatment, yet may be more responsive to TGFβRI inhibitors, highlighting potential therapeutic implications for stratifying GBM patients based on CAFscore.
3.5 Role of LRP10 in GBM
We then focused on the four core genes related to CAFscore. Notably, protein expression analysis (https://ualcan.path.uab.edu/analysis-prot.html) revealed that LRP10 was significantly overexpressed in GBM tissues (Fig. 6A). OCIAD2 exhibited a trend of increased expression, though not statistically significant (data not shown). In contrast, there was a lack of proteomic data for SOCS3 and GADD45A. Through resources from GEPIA 2 website (http://gepia2.cancer-pku.cn/#index), we confirmed the elevated mRNA levels of LRP10 in GBM as compared to normal brain tissue (Fig. 6B). Moreover, a strong positive correlation was observed between LRP10's mRNA and protein levels (Fig. 6C), suggesting a significant increase in transcriptional activity leading to higher protein expression in GBM.
Analyses of LRP10. (A–B) Protein (A) and transcriptional (B) level of LRP10 in GBM and normal brains. (C) Correlation analysis of the protein and transcriptional level of LRP10 in GBM. (D) Correlation analyses of the expression of LRP10 and infiltration of CAF in CGGA-301 cohorts. (E) RT-PCR analysis of LRP10 in U251 and U-87MG GBM cells transfected with si-NC or si-LRP10. (F&G) Transwell migration analyses of U251 and U-87MG GBM cells after knocking down LRP10. (H) Wound healing analyses U251 and U-87MG GBM cells. Data are derived from three independent experiments. Columns represent the mean values obtained from three independent experiments; bars represent the SD; asterisks indicate the statistical significance compared to the control. **p < 0.01, ***p < 0.001
In addition, LRP10 expression was closely associated with the infiltration levels of cancer-associated fibroblasts (CAFs) within GBM samples across all the three datasets (Fig. 6D; Supplementary Fig. 1C&1D). Given that CAFscore correlates with tumor invasion and metastasis, we conducted scratch assays and trans-well migration assays to ascertain LRP10’s role in influencing GBM invasion capabilities. As demonstrated in Fig. 6E–H, LRP10 knockout in U251 and U-87MG cell lines resulted in a significant reduction of LRP10 levels (Fig. 6E), ultimately leading to a marked decrease in cellular invasion (Fig. 6F, G) and migration (Fig. 6H). These findings underscored the potential role of LRP10 as a pivotal player in GBM progression and its interaction with CAF within the tumor microenvironment.
4 Discussion
Despite extensive research confirming the critical role of CAFs in various solid tumors, investigations into their function in GBM have only recently gained momentum [7,8,9]. Previously, it was assumed that CAFs might be absent in GBM [18]; however, emerging studies have identified their presence and highlighted their involvement in the tumor's growth and malignancy [11, 12]. Where do CAFs in gliomas originate from? Studies on CAFs in mouse models of other cancers have identified that they can originate from both local and remote sources, such as fibroblasts, endothelial cells, vascular mural cells, or mesenchymal stem cells (MSCs) [19,20,21,22]. However, due to difficulties in obtaining tissue samples, the origin of CAFs in gliomas remains challenging to determine. Mito-SNV analysis has indicated that CAFs did not originate from other stromal cells isolated through serial trypsinization [12]; however, current evidence still cannot confirm whether CAFs arise from a more upstream origin of these stromal cells. Furthermore, whether CAFs originate from blood–brain barrier (BBB) breakdown, leading to the recruitment of MSCs to GBM that subsequently differentiate into CAFs requires further investigation [12]. Nevertheless, this newfound understanding underscores the complexity of the tumor microenvironment in GBM and the need for deeper exploration of CAF dynamics. To further elucidate the impact of CAFs, we performed an enrichment analysis of the marker genes of CAFs in GBM and revealed a strong correlation between the CAF-ES and prognosis in GBM patients. High CAF-ES was associated with poorer outcomes, suggesting that CAFs might play a detrimental role in patient survival (Fig. 1G–I). Through extensive WGCNA across multiple datasets, we identified modules highly correlated with CAF-ES and utilized various machine learning techniques to pinpoint core genes linked to CAF activity (Fig. 2–3). Consistently, our findings indicated that patients exhibiting elevated CAFscores primarily enriched in metastasis-related pathways and are closely associated with inflammatory responses and epithelial-mesenchymal transition (EMT) (Fig. 5A–C), reinforcing earlier observations that CAFs predominantly influence tumor invasiveness [23,24,25]. Thus, building on the findings of this study, future research might dive deeper into the roles these identified genes play in GBM progression, particularly how they modulate CAFs’ behavior within the GBM microenvironment. Such investigations will substantially enhance our understanding of GBM biology and its implications for therapeutic sensitivity.
Numerous studies had made significant strides in constructing prognostic models for GBM, drawing attention to diverse biological factors and patient characteristics [26,27,28,29,30]. However, the model developed in this study presented several distinct advantages. Firstly, it represented the first, to the best of our knowledge, prognostic model associated with the infiltration of CAFs in GBM, offering a more nuanced understanding of the impact that CAFs have on tumor behavior and patients’ outcomes. This CAF-centric approach might facilitate a deeper investigation into tumor microenvironment interactions, ultimately leading to more targeted therapeutic strategies. Secondly, our model had direct clinical implications for personalizing therapy in GBM patients. As shown in Fig. 5D–G, our findings suggested that patients categorized in the high-CAFscore group might exhibit sensitivity to TGFβ inhibitors while demonstrating insensitivity to irinotecan (or its analogs)-based treatments. Given that clinical trials utilizing irinotecan combination therapies are currently underway or have been investigated [31,32,33], this model might be able to serve as a valuable tool for patient stratification, enabling oncologists to better identify individuals likely to benefit from irinotecan-based combination. Lastly, when compared to previously established models, our prognostic framework had shown a relatively superior C-index across multiple datasets, consistently ranking among the top performers (Fig. 4C–E). However, it is crucial to underscore that the utility of this model must be validated through prospective clinical studies with larger cohorts to ascertain its clinical applicability and effectiveness in diverse patient populations.
LRP10, a core CAFscore related gene identified in this study, is predominantly expressed in non-neuronal cells such as astrocytes and neuro-vasculature in the central nervous system [34]. However, its presence in α-synuclein-positive neuronal Lewy bodies in both idiopathic and genetic cases of Parkinson's disease (PD), Parkinson's disease dementia (PDD), and dementia with Lewy bodies (DLB) underscores its potential significance in neurodegenerative processes [34, 35]. A recent study found that overexpression of LRP10 had been linked to increased secretion of monomeric α-synuclein, accompanied by dynamic, stress-related alterations in intracellular α-synuclein concentrations [34]. In addition to its roles in neurodegeneration, LRP10 was also implicated in the biological processes underlying tumors. For instance, it had been shown to downregulate the levels of interleukin 7 receptor (IL7R), consequently inhibiting the proliferation of CD8 T cells and diminishing anti-tumor efficacy [36]. Moreover, LRP10 has also been implicated in drug resistance, particularly in cancer cells. Evidence suggests that aberrant expression of LRP10 is associated with a reduced sensitivity to conventional therapies, including targeted treatments [37]. In our study, we observed that LRP10 was markedly overexpressed in GBM (Fig. 6A, B) and established a significant positive correlation with CAF infiltration levels (Fig. 6D–F). Furthermore, the knockdown of LRP10 led to a substantial reduction in the invasive behavior of GBM cells (Fig. 6H–I), indicating that LRP10 might play a pivotal role in regulating CAF infiltration and tumor invasiveness. However, the precise regulatory mechanisms involved warrant further investigation to validate these findings.
In addition, SOCS3 and GADD45A were also identified as significant genes within the cancer-associated fibroblast (CAF) related prognostic model (Fig. 3E). SOCS3, a key regulator of cytokine signaling, has been implicated in various malignancies, where it appears to modulate inflammatory responses that contribute to immune evasion. The overexpression of SOCS3 in tumors has been associated with the inhibition of pro-inflammatory cytokines, thereby fostering an environment conducive to tumor progression and immune suppression [38,39,40]. Additionally, the interaction between SOCS3 and various signaling pathways, particularly those involving IL-6 and TNF-α, further elucidates its role in creating an immunosuppressive niche within the tumor microenvironment [40]. GADD45A is a stress-responsive protein implicated in various cellular processes, including DNA repair, cell cycle regulation, and apoptosis. Emerging evidence suggests that GADD45A may also play a pivotal role in modulating immune responses within the TME [41, 42]. However, a comprehensive analysis exploring the specific mechanisms by which SOCS3 and GADD45A contribute to the progression and immunosuppressive microenvironment of GBM requires further investigation.
In conclusion, this study presented the first CAF related prognostic model (CAFscore) in GBM, and demonstrated that the model could effectively guide patient prognosis and potentially inform personalized treatment strategies. The core gene of CAFscore, LRP10, was significantly overexpressed in GBM and might play a pivotal role in regulating CAF infiltration as well as tumor invasion and metastasis, highlighting LRP10 as a promising therapeutic target for GBM management.
Data availability
The RNA sequence data and clinical information of The Cancer Genome Atlas (TCGA) Glioblastoma (GBM) cohort were accessible at https://portal.gdc.cancer.gov. The CGGA-301, CGGA-325, and CGGA-693 datasets were obtained from the Chinese Glioma Genome Atlas (CGGA) database (http://www.cgga.org.cn/index.jsp).
References
Arvold ND, Reardon DA. Treatment options and outcomes for glioblastoma in the elderly patient. Clin Interv Aging. 2014;9:357–67.
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987–96.
Omuro A, DeAngelis LM. Glioblastoma and other malignant gliomas: a clinical review. JAMA. 2013;310(17):1842–50.
Brown TJ, Brennan MC, Li M, Church EW, Brandmeir NJ, Rakszawski KL, Patel AS, Rizk EB, Suki D, Sawaya R, et al. Association of the extent of resection with survival in glioblastoma: a systematic review and meta-analysis. JAMA Oncol. 2016;2(11):1460–9.
Le Rhun E, Preusser M, Roth P, Reardon DA, van den Bent M, Wen P, Reifenberger G, Weller M. Molecular targeted therapy of glioblastoma. Cancer Treat Rev. 2019;80: 101896.
Mahmoud AB, Ajina R, Aref S, Darwish M, Alsayb M, Taher M, AlSharif SA, Hashem AM, Alkayyal AA. Advances in immunotherapy for glioblastoma multiforme. Front Immunol. 2022;13: 944452.
Lavie D, Ben-Shmuel A, Erez N, Scherz-Shouval R. Cancer-associated fibroblasts in the single-cell era. Nat Cancer. 2022;3(7):793–807.
Ma C, Yang C, Peng A, Sun T, Ji X, Mi J, Wei L, Shen S, Feng Q. Pan-cancer spatially resolved single-cell analysis reveals the crosstalk between cancer-associated fibroblasts and tumor microenvironment. Mol Cancer. 2023;22(1):170.
Mao X, Xu J, Wang W, Liang C, Hua J, Liu J, Zhang B, Meng Q, Yu X, Shi S. Crosstalk between cancer-associated fibroblasts and immune cells in the tumor microenvironment: new findings and future perspectives. Mol Cancer. 2021;20(1):131.
Zheng H, An M, Luo Y, Diao X, Zhong W, Pang M, Lin Y, Chen J, Li Y, Kong Y, et al. PDGFRalpha(+)ITGA11(+) fibroblasts foster early-stage cancer lymphovascular invasion and lymphatic metastasis via ITGA11-SELE interplay. Cancer Cell. 2024;42(4):682–700.
Galbo PM Jr, Madsen AT, Liu Y, Peng M, Wei Y, Ciesielski MJ, Fenstermaker RA, Graff S, Montagna C, Segall JE, et al. Functional contribution and clinical implication of cancer-associated fibroblasts in glioblastoma. Clin Cancer Res. 2024;30(4):865–76.
Jain S, Rick JW, Joshi RS, Beniwal A, Spatz J, Gill S, Chang AC, Choudhary N, Nguyen AT, Sudhir S, et al. Single-cell RNA sequencing and spatial transcriptomics reveal cancer-associated fibroblasts in glioblastoma with protumoral effects. J Clin Invest. 2023;133:5.
Biffi G, Tuveson DA. Diversity and biology of cancer-associated fibroblasts. Physiol Rev. 2021;101(1):147–76.
Zhu Z, Li G, Li Z, Wu Y, Yang Y, Wang M, Zhang H, Qu H, Song Z, He Y. Core immune cell infiltration signatures identify molecular subtypes and promote precise checkpoint immunotherapy in cutaneous melanoma. Front Immunol. 2022;13: 914612.
Li X, Kang J, Yue J, Xu D, Liao C, Zhang H, Zhao J, Liu Q, Jiao J, Wang L, et al. Identification and validation of immunogenic cell death-related score in uveal melanoma to improve prediction of prognosis and response to immunotherapy. Aging (Albany NY). 2023;15(9):3442–64.
Jun Z: GseaVis: An Implement R Package to Visualize GSEA Results. 2022.
Yuan H, Yan M, Zhang G, Liu W, Deng C, Liao G, Xu L, Luo T, Yan H, Long Z, et al. CancerSEA: a cancer single-cell state atlas. Nucleic Acids Res. 2019;47(D1):D900–8.
LeBleu VS, Neilson EG. Origin and functional heterogeneity of fibroblasts. FASEB J. 2020;34(3):3519–36.
Li Z, Zhang J, Zhou J, Lu L, Wang H, Zhang G, Wan G, Cai S, Du J. Nodal facilitates differentiation of fibroblasts to cancer-associated fibroblasts that support tumor growth in melanoma and colorectal cancer. Cells. 2019;8:6.
Kim K, Sohn YJ, Lee R, Yoo HJ, Kang JY, Choi N, Na D, Yeon JH. Cancer-associated fibroblasts differentiated by exosomes isolated from cancer cells promote cancer cell invasion. Int J Mol Sci. 2020;21:21.
Hosaka K, Yang Y, Seki T, Fischer C, Dubey O, Fredlund E, Hartman J, Religa P, Morikawa H, Ishii Y, et al. Pericyte-fibroblast transition promotes tumor growth and metastasis. Proc Natl Acad Sci U S A. 2016;113(38):E5618-5627.
Direkze NC, Hodivala-Dilke K, Jeffery R, Hunt T, Poulsom R, Oukrif D, Alison MR, Wright NA. Bone marrow contribution to tumor-associated myofibroblasts and fibroblasts. Cancer Res. 2004;64(23):8492–5.
Li Z, Sun C, Qin Z. Metabolic reprogramming of cancer-associated fibroblasts and its effect on cancer cell reprogramming. Theranostics. 2021;11(17):8322–36.
Li X, Sun Z, Peng G, Xiao Y, Guo J, Wu B, Li X, Zhou W, Li J, Li Z, et al. Single-cell RNA sequencing reveals a pro-invasive cancer-associated fibroblast subgroup associated with poor clinical outcomes in patients with gastric cancer. Theranostics. 2022;12(2):620–38.
Kim HJ, Yang K, Kim K, Lee YJ, Lee S, Ahn SY, Ahn YH, Kang JL. Reprogramming of cancer-associated fibroblasts by apoptotic cancer cells inhibits lung metastasis via Notch1-WISP-1 signaling. Cell Mol Immunol. 2022;19(12):1373–91.
Chen L, Zhao X, Liu Y, Wu M, Li S, Xu C, Shi Y. Comprehensive analysis of HHV-6 and HHV-7-related gene signature in prognosis and response to temozolomide of glioma. J Med Virol. 2023;95(1): e28285.
Tian R, Li Y, Liu Q, Shu M. Identification and validation of an immune-associated RNA-binding proteins signature to predict clinical outcomes and therapeutic responses in glioma patients. Cancers. 2021;13:7.
Chen J, Chen S, Li B, Zhou S, Lin H. A pyroptosis-related signature predicts prognosis and indicates immune microenvironment infiltration in glioma. Cancer Med. 2023;12(4):5071–87.
Pan D, Fang X, Li J. Identification of a novel gene signature based on kinesin family members to predict prognosis in glioma. Medicina. 2023;59:2.
Wu S, Xu J, Li G, Jin X. Integrating radiosensitivity gene signature improves glioma outcome and radiotherapy response prediction. Medicina. 2022;58:10.
Elinzano H, Toms S, Robison J, Mohler A, Carcieri A, Cielo D, Donnelly J, Disano D, Vatketich J, Baekey J, et al. Nanoliposomal irinotecan and metronomic temozolomide for patients with recurrent glioblastoma: BrUOG329, a phase I brown university oncology research group trial. Am J Clin Oncol. 2021;44(2):49–52.
Friedman HS, Prados MD, Wen PY, Mikkelsen T, Schiff D, Abrey LE, Yung WKA, Paleologos N, Nicholas MK, Jensen R, et al. Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin Oncol. 2023;41(32):4945–52.
Peters KB, Lou E, Desjardins A, Reardon DA, Lipp ES, Miller E, Herndon JE 2nd, McSherry F, Friedman HS, Vredenburgh JJ. Phase II trial of upfront bevacizumab, irinotecan, and temozolomide for unresectable glioblastoma. Oncologist. 2015;20(7):727–8.
Carreras Mascaro A, Grochowska MM, Boumeester V, Dits NFJ, Bilgiҫ EN, Breedveld GJ, Vergouw L, de Jong FJ, van Royen ME, Bonifati V, et al. LRP10 and alpha-synuclein transmission in Lewy body diseases. Cell Mol Life Sci. 2024;81(1):75.
Quadri M, Mandemakers W, Grochowska MM, Masius R, Geut H, Fabrizio E, Breedveld GJ, Kuipers D, Minneboo M, Vergouw LJM, et al. LRP10 genetic variants in familial Parkinson’s disease and dementia with Lewy bodies: a genome-wide linkage and sequencing study. Lancet Neurol. 2018;17(7):597–608.
Russell J, Chen L, Liu A, Wang J, Ghosh S, Zhong X, Shi H, Beutler B, Nair-Gill E. Lrp10 suppresses IL7R limiting CD8 T cell homeostatic expansion and anti-tumor immunity. EMBO Rep. 2024;9:4483.
Li Y, Shen Y, Zhu Z, Wen H, Feng C. Comprehensive analysis of copy number variance and sensitivity to common targeted therapy in clear cell renal cell carcinoma: In silico analysis with in vitro validation. Cancer Med. 2020;9(16):6020–9.
Dai L, Li Z, Tao Y, Liang W, Hu W, Zhou S, Fu X, Wang X. Emerging roles of suppressor of cytokine signaling 3 in human cancers. Biomed Pharmacother. 2021;144: 112262.
Yang X, Tian M, Lin Y, Li L, Sun X, Zhang Z, Kang M, Lin J. Characterization of the roles of suppressor of cytokine signaling-3 in esophageal carcinoma. Hum Gene Ther. 2023;34(11–12):495–517.
Yoshimura A, Ito M, Chikuma S, Akanuma T, Nakatsukasa H. Negative regulation of cytokine signaling in immunity. Cold Spring Harb Perspect Biol. 2018;10:7.
Xu M, Xu X, Pan B, Chen X, Lin K, Zeng K, Liu X, Xu T, Sun L, Qin J, et al. LncRNA SATB2-AS1 inhibits tumor metastasis and affects the tumor immune cell microenvironment in colorectal cancer by regulating SATB2. Mol Cancer. 2019;18(1):135.
Salerno DM, Tront JS, Hoffman B, Liebermann DA. Gadd45a and Gadd45b modulate innate immune functions of granulocytes and macrophages by differential regulation of p38 and JNK signaling. J Cell Physiol. 2012;227(11):3613–20.
Funding
Research Fund of Zhoukou Hospital of Traditional Chinese Medicine, zkszyy2024001, China Postdoctoral Science Foundation, 2020M682334, Henan Postdoctoral Foundation, 202003002
Author information
Authors and Affiliations
Contributions
The study was designed by W.F.P and W.D.S. Data analysis was carried out by L.l. W, Q.j. L, and G.Y. L. The manuscript was drafted by L.L. W., and W.F. P, and was revised by all authors before the final version was approved to be published.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12672_2024_1314_MOESM1_ESM.jpg
Supplementary File 1. Figure 1. Flowchart for constructing CAFscore. (A) Flow chat of constructing CAFscore. (B) Level of CAFscore across subtypes of GBM. (C&D) Correlation analyses of the expression of LRP10 and infiltration of CAF in CGGA-Meta (C), and TCGA-GBM (D) cohorts.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wu, L., Liu, Q., Li, G. et al. A cancer-associated fibroblasts related risk score (CAFscore) helps to guide prognosis and personal treatment for Glioblastoma. Discov Onc 15, 420 (2024). https://doi.org/10.1007/s12672-024-01314-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12672-024-01314-4