Abstract
Introduction
This study aimed to evaluate the effect of baseline body mass index (BMI) and glycated hemoglobin (HbA1c) on the effectiveness and safety of initiating iGlarLixi (insulin glargine 100 U/ml and lixisenatide) in people with type 2 diabetes (T2D) in routine clinical practice.
Methods
We pooled patient-level data from 1406 people with inadequately controlled T2D, initiating a 24-week iGlarLixi treatment. Analysis sets were based on baseline BMI and HbA1c. In the BMI set, 894 (64%) people had a BMI ≥ 30 kg/m2 and 510 (36%) a BMI < 30 kg/m2; in the HbA1c set, 615 (44%) people had an HbA1c >9%, 491 (35%) between 8 and 9%, and 298 (21%) < 8%.
Results
After initiating iGlarLixi, HbA1c decreased in all participants, with the greatest least-squares mean reduction at 2.15% from baseline to week 24 in those with baseline HbA1c > 9% (using a mixed model for repeated measures). Overall, mean ± standard deviation body weight decreased by 1.9 ± 4.8 kg, with the most prominent loss of 2.6 ± 4.9 kg recorded in people presenting with obesity. Reported hypoglycemia rates were low across all groups.
Conclusions
Initiation of iGlarLixi in people with uncontrolled T2D is effective and safe in clinical practice, across different baseline HbA1c and BMI categories.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Pharmacological therapies in type 2 diabetes (T2D) should address both individualized glycemic and weight goals. |
iGlarLixi (insulin glargine 100 U/ml and lixisenatide) expands the available options for therapeutic intensification in T2D. |
Here, we evaluated how baseline glycated hemoglobin (HbA1c) and body mass index (BMI) may influence treatment outcomes of iGlarLixi in people with T2D who were not adequately controlled in a real-life setting. |
What was learned from this study? |
In this pooled analysis of 1406 people with T2D starting 24-week iGlarLixi treatment, iGlarLixi was effective and safe with inadequately controlled T2D, regardless of HbA1c or BMI. |
Healthcare providers can consider iGlarLixi for a broad range of patients with T2D. |
Introduction
Poor glycemic control in people with type 2 diabetes (T2D) is highly prevalent, with reported rates varying widely from 45% to 93% according to cross-sectional studies [1,2,3]. Factors that contribute to poor glycemic control are diverse, mainly relating to individual characteristics, therapeutic inertia, and effectiveness of the medications being used [3]. Despite intensification of glucose-lowering therapy, many people with T2D remain uncontrolled due to increased treatment burden and non-adherence to therapy, especially when switching to complex insulin regimens with multiple daily injections [4]. In this context, several options have been made available to simplify complex treatment regimens including the transition to once-daily fixed-ratio combinations of basal insulin (BI) and glucagon-like peptide 1 receptor agonist (GLP1-RA). For instance, the American Diabetes Association (ADA) recommends the use of fixed-ratio combinations, either iGlarLixi (insulin glargine 100 U/ml [iGlar] and lixisenatide) or IDegLira (insulin degludec and liraglutide), in its algorithm of intensifying to injectable therapy in people with T2D [5].
Clinical evidence from randomized clinical trials (RCTs, LixiLan trials) and real-world studies demonstrated the efficacy as well as the effectiveness of iGlarLixi, which delivered greater HbA1c reductions compared with its individual components (iGlar and lixisenatide) alone [6]. The LixiLan RCTs showed that more patients achieved glycated hemoglobin (HbA1c) target < 7% without additional risk of hypoglycemia compared either with continued prior GLP1-RA [7] or with iGlar alone [8]. The clinical findings from the LixiLan RCTs also highlight a good safety and tolerability profile of iGlarLixi. As such, treatment with iGlarLixi extends the suitable therapeutic intensification options by offering both glycemic control and weight benefits in people with T2D, regardless of baseline HbA1c, duration of diabetes, and prior insulin use [7,8,9,10,11].
Considering the heterogeneity of T2D, the latest consensus report from the ADA and the European Association for the Study of Diabetes (EASD) emphasizes personalizing treatment strategies to incorporate individual-specific factors while selecting the appropriate glucose-lowering treatment [12]. Hence, pharmacological therapies should address both individualized glycemic and weight goals in non-specific populations of T2D [5]. In the iGlarLixi phase 3 RCTs, the efficacy and safety of iGlarLixi was consistent across age, diabetes duration, baseline HbA1c, and baseline body mass index (BMI) categories in people with inadequately controlled T2D [7,8,9,10,11]. Understanding the underlying factors that may influence response to iGlarLixi in the real-life setting is critical to tailor treatment regimens more effectively [11]. Prior pooled analyses of the European REALI program in people with uncontrolled T2D revealed clinically meaningful results on treatment outcome of iGlarLixi by age [13] and prior insulin therapy [14]. Here, we evaluated how baseline HbA1c and BMI may influence treatment outcomes of iGlarLixi in people with T2D who were not adequately controlled in a real-life setting.
Methods
Study Design and Study Population
This analysis pooled patient-level data from three real-life, prospective, observational studies [15,16,17], part of the comprehensive European REALI program [18,19,20,21]. The rationale, methodology, and detailed description of the analyzed variables are provided in previous published data on the REALI project [19, 22].
The pooled studies included adult participants with inadequately controlled T2D, who were either insulin-naïve or previously treated with BI, with or without non-insulin glucose-lowering agents [15,16,17]. Participants were treated with iGlarLixi (Suliqua®, Sanofi, Paris, France) for 24 weeks, and used iGlarLixi pens (SoloStar® pen injectors) to self-administer iGlarLixi [21, 23]. iGlarLixi was available as two fixed-ratio combinations: 100 units/ml iGlar plus 50 µ/ml lixisenatide (Suliqua® SoloStar® pen 10–40 units; iGlarLixi 100/50) and 100 units/ml iGlar plus 33 µ/ml lixisenatide (Suliqua® SoloStar® pen 30–60 units; iGlarLixi 100/33). The choice of the iGlarLixi pen and the starting dose were left at the discretion of the treating physician. iGlarLixi was also titrated at the discretion of the treating physician.
Analysis Sets
For the purpose of this pooled analysis, two analysis sets were constructed. In the analysis set based on baseline HbA1c, participants were classified into the following groups: HbA1c < 8%, HbA1c [8–9%], and HbA1c > 9% (defined as people with poor glycemic control [5]). In the analysis set based on baseline BMI, participants were classified into the two following groups: BMI < 30 kg/m2 or ≥ 30 kg/m2 (defined as people presenting with obesity [5]).
Ethics
Studies included in the pooled analysis were conducted according to the principles of the Declaration of Helsinki and the Good Clinical Practice guidelines and were approved by the appropriate ethics committees and institutional review boards [15,16,17]. All participants provided written informed consent. As the primary analysis was conducted within the parameters of the initial participant consent, no additional ethical approval was deemed necessary for this pooled anonymized data analysis.
Assessments
Demographics and baseline characteristics included age, sex, duration of diabetes, body weight, BMI, diabetic complications, and cardiovascular comorbidities, as well as details of prior glucose-lowering medications. Data on iGlarLixi treatment, such as iGlarLixi dose and concomitant use of other non-insulin glucose-lowering medications were also collected at baseline, at 12 weeks, and at 24 weeks.
The primary endpoint of this analysis was the change in HbA1c from baseline to week 24. Secondary effectiveness endpoints included HbA1c change from baseline to week 12, proportions of participants achieving HbA1c targets of < 7.0% (< 53 mmol/mol), < 7.5% (< 59 mmol/mol) and < 8.0% (< 64 mmol/mol) at week 24, and changes from baseline to weeks 12 and 24 in fasting plasma glucose (FPG). Safety endpoints included the incidence of hypoglycemic events (symptomatic and severe) and gastrointestinal adverse events (AEs). Hypoglycemic events were defined on the basis of the ADA classification [24], and were reported according to their time of occurrence (during the night and at any time of the day). The pooled analysis also evaluated changes in body weight and in iGlar dose provided by iGlarLixi (expressed in both U/day and in U/kg/day) from baseline to weeks 12 and 24.
Statistical Analysis
The change in HbA1c from baseline was analyzed using a mixed model for repeated measures (MMRM) with unstructured covariance matrix, fixed categorical effects of visit, prior insulin use (naïve vs pre-treated), prior insulin-use-by-visit interaction, subgroup category and subgroup category-by-visit interaction, as well as continuous fixed covariates of baseline HbA1c and baseline HbA1c value-by-visit interaction for the analysis set by BMI.
On the basis of this MMRM, we estimated the least-squares (LS) mean HbA1c changes from baseline to weeks 12 and 24 with the corresponding 95% confidence intervals (CIs) for each group. This same MMRM approach with the corresponding baseline FPG value-by-visit interaction as a covariate was used to estimate LS mean FPG changes. Hypoglycemic event rates were reported as percentages of participants with at least one event and calculated as annualized rates (number of events per patient-year of exposure).
All other effectiveness and safety endpoints, as well as baseline characteristics, were summarized descriptively as mean ± standard deviation (SD) or as median (quartile 1–quartile 3) for continuous variables and as counts and percentages for categorical variables. No imputation of missing data was performed, and no adjustment for multiple testing was made. All statistical tests were two-sided, with a p-value < 0.05 considered statistically significant. All analyses were performed using SAS version 9.4 (SAS Institute Inc, Cary, NC, USA).
Results
Disposition of Participants
The present patient-level pooled analysis included 1406 participants with uncontrolled T2D who were initiated with iGlarLixi for 24 weeks. Table 1 summarizes demographics and baseline characteristics for each group of the analysis sets, based on a total of 1404 patients, considering that data on baseline BMI and HbA1c was missing for two patients. The overall mean ± SD age of the study population was 61.2 ± 9.0 years, the mean ± SD BMI was 32.4 ± 5.6 kg/m2, and the median diabetes duration was 9.0 years (interquartile range, 5.0 to 13.0 years). All participants had inadequately controlled T2D, with a mean ± SD baseline HbA1c of 9.1 ± 1.4%. Almost all study participants (n = 1387; 99%) who initiated iGlarLixi were using non-insulin glucose-lowering agents, which were discontinued at iGlarLixi initiation, except for biguanides that were maintained for the majority of participants (n = 1349; 97%). Overall, participants were almost equally distributed between insulin-naïve and insulin pre-treated, whereby all insulin pre-treated participants received BI alone with a median insulin treatment duration of 2.5 years prior to iGlarLixi initiation. Insulin glargine was the most frequently used BI (n = 476; 69%) followed by detemir (n = 108; 16%), and Neutral Protamine Hagedorn insulin (n = 94; 14%). There were differences within the groups of both analysis sets, with respect to prior insulin use, cardiovascular risk factors/events, and diabetic complications (Table 1). Approximately 80% of study participants were prescribed the iGlarLixi 100/50 pen at baseline.
Glycemic Control in the Analysis Set According to Baseline HbA1c
After initiation of iGlarLixi treatment, mean ± SD HbA1c decreased from 7.58 ± 0.32% at baseline to reach 7.07 ± 0.81% at week 24 for people with baseline HbA1c < 8% (absolute mean change of − 0.52%), from 8.47 ± 0.3% to reach 7.59 ± 0.98% for people with HbA1c [8–9%] (absolute mean change of − 0.88%), and from 10.28 ± 1.10% to reach 8.09 ± 1.36% for people with HbA1c > 9% (absolute mean change of − 2.17%). HbA1c decreased mostly during the first 12 weeks; absolute mean HbA1c change was − 0.34%, − 0.73%, and − 1.89%, respectively. The LS mean difference [95% CI] between HbA1c groups was − 0.31% [− 0.50; − 0.11] for the HbA1c [8–9%] group and − 1.55% [− 1.75; − 1.36] for the HbA1c > 9% group compared to the HbA1c < 8% group (p < 0.05). Figure 1 illustrates mean HbA1c values at baseline and at week 24 across HbA1c groups and the corresponding LS mean changes.
Mean glycated hemoglobin (HbA1c) and least-squares (LS) mean change (95% confidence interval [CI]) in HbA1c from baseline to week 24 of iGlarLixi treatment by baseline HbA1c group. *LS means change from baseline to week 24 and corresponding 95% CI were derived from a mixed model for repeated measures (MMRM) with unstructured covariance matrix, fixed categorical effects of visit, prior insulin use (naïve vs. pre-treated), prior insulin-use-by-visit interaction, subgroup category, and subgroup category-by-visit interaction. The bar graph values correspond to descriptive statistics for HbA1c values at baseline and week 24
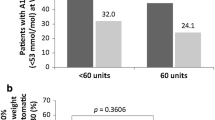
More people in the lower baseline HbA1c group were able to reach HbA1c targets < 7.0%, < 7.5%, and < 8.0%, at week 24 (Fig. 2). The majority of people with HbA1c < 8% (91%) and HbA1c [8–9%] (73%), and more than half of people with HbA1c > 9% (54%) reached HbA1c target < 8%. FPG reductions showed similar patterns as HbA1c across the HbA1c groups (Table S1 in the supplementary material).
Glycemic Control in the Analysis Set According to Baseline BMI
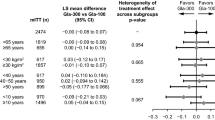
Figure 3A illustrates mean HbA1c values at baseline and at week 24 for the two BMI groups and the corresponding LS mean changes. Mean ± SD HbA1c decreased from 9.03 ± 1.33% at baseline to reach 7.62 ± 1.10% at week 24 for people with baseline BMI < 30 kg/m2 (absolute mean HbA1c change of -1.39%), and from 9.10 ± 1.37% to reach 7.75 ± 1.25% for people with BMI ≥ 30 kg/m2 (absolute mean HbA1c change of − 1.34%). HbA1c decreased mostly during the first 12 weeks; absolute mean HbA1c change was − 1.20% and − 1.12%, respectively. The LS mean difference [95% CI] between BMI groups was not statistically significant at + 0.09% [− 0.04; 0.22].
A Mean glycated hemoglobin (HbA1c) and least-squares (LS) mean change (95% confidence interval [CI]) in HbA1c from baseline to week 24 of iGlarLixi treatment by baseline body mass index (BMI) group; B Mean ± standard deviation (SD) body weight change (kg) from baseline to week 24 by baseline BMI group. *LS means change from baseline and corresponding 95% CI were derived from a mixed model for repeated measures (MMRM) with unstructured covariance matrix, fixed categorical effects of visit, prior insulin use (naïve vs pre-treated), prior insulin-use-by-visit interaction, subgroup category and subgroup category-by-visit interaction as well as continuous fixed covariates of baseline HbA1c, and baseline HbA1c value-by-visit interaction. The bar graph values correspond to descriptive statistics for HbA1c values at baseline and week 24
The proportion of participants reaching HbA1c target < 7% at week 24 was similar in both BMI groups (26%), with slight differences for the higher HbA1c targets (< 7.5% and < 8.0%) (Fig. 2). FPG reductions showed similar patterns as HbA1c across the BMI groups (Table S1 in the supplementary material).
iGlarLixi Dose and Safety
In all people initiating iGlarLixi, irrespective of baseline HbA1c and BMI, mean iGlarLixi dose increased essentially in the first 12 weeks and continued to increase rather slightly up to week 24. Figure 4 shows the change in iGlar dose provided by iGlarLixi from baseline to weeks 12 and 24 in the two analysis sets. In the analysis set by baseline HbA1c, mean iGlar starting daily dose was 0.22 U/kg (19.5 U), increasing to 0.41 U/kg (35.9 U) in the baseline HbA1c > 9% group, 0.38 U/kg (33.4 U) in the HbA1c [8–9%] group, and 0.34 U/kg (29.9 U) in the HbA1c < 8% group (Fig. 4A). In the analysis set by baseline BMI, mean iGlar daily dose increased from 0.21 U/kg (20.5 U) at baseline to 0.38 U/kg (35.6 U) at week 24 in the BMI ≥ 30 kg/m2 group and from 0.23 U/kg (17.7 U) to 0.40 U/kg (30.4 U) in the BMI < 30 kg/m2 group (Fig. 4B).
Hypoglycemia reports and gastrointestinal AEs were low in all participants. Nausea was reported in only 1% of participants. Overall, symptomatic hypoglycemia was reported in 3.8% of participants. Only one severe hypoglycemia event was reported overall. Overall, 24 out of 510 participants with BMI < 30 kg/m2 (4.7%) and 30 out of 893 participants with BMI ≥ 30 kg/m2 (3.4%) reported a total of 132 symptomatic hypoglycemia events (event rate: 0.2).
Body Weight
Body weight decreased in participants initiating iGlarLixi, regardless of baseline HbA1c and BMI, by an overall mean ± SD of 1.9 ± 4.8 kg over 24 weeks. Body weight decreased essentially during the first 12 weeks recording a mean ± SD weight loss of 1.4 ± 3.7 kg. Among the groups in the analysis set by baseline HbA1c, a comparable decrease in body weight was noted from 91.0 kg at baseline to 89.3 kg at week 24. In the analysis set by baseline BMI, a remarkable reduction was recorded at a mean ± SD of 2.6 ± 4.9 kg in the BMI ≥ 30 kg/m2 group over 24 weeks, and 0.7 ± 4.4 kg in the BMI < 30 kg/m2 group (Fig. 3B).
Discussion
The present pooled analysis highlights the importance of understanding how baseline factors influence the effectiveness and safety of iGlarLixi in real-world settings. Our analysis demonstrated that iGlarLixi treatment improved glycemic control and decreased body weight, with no new safety concerns, in insulin-naïve and insulin pre-treated adults with inadequately controlled T2D, across different baseline HbA1c and BMI categories. The greatest HbA1c reduction was noted in people with baseline HbA1c > 9% reporting a mean change of − 2.17% at week 24, compared to − 0.88% in people with HbA1c [8–9%], and − 0.52% in people with HbA1c < 8%. These HbA1c findings were in line with those of the subpopulation analyses of the LixiLan-L [10] and LixiLan-O [11] RCTs, in which people with HbA1c ≥ 8% had a greater HbA1c reduction (− 1.9% in insulin pre-treated participants and − 1.4% in insulin-naïve, respectively) compared to people with HbA1c < 8% (− 1.2% and − 0.8%, respectively) at week 30 [11].
In the LixiLan-O trial, nearly 80% of participants with a baseline HbA1c < 8% achieved an HbA1c target of < 7% [11]. Similarly, in the LixiLan-L trial, 68% of participants with a baseline HbA1c < 8% reached the same target [10]. In our analysis, 48% reached HbA1c target < 7%. This difference between studies in reaching HbA1c targets may be due to the lower mean baseline HbA1c in the RCTs, ranging from 7.5% to 8.7% [10, 11], compared to a mean baseline HbA1c between 7.6% and 10.3% across HbA1c groups in our analysis. Moreover, corresponding to routine clinical practice, rigid titration of iGlarLixi was not followed in the pooled observational studies [15,16,17]. Hence, less tight titration may also explain the lower percentage of participants reaching target HbA1c < 7.0% in the present pooled analysis compared to the LixiLan RCTs.
Our study findings align with real-world evidence highlighting the practical efficacy of combination therapies like iGlarLixi and IDegLira in achieving glycemic targets in individuals with inadequately controlled T2D [25, 26]. A retrospective cohort study from Hungary found that people with T2D initiating IDegLira had 2–3 times greater odds of achieving an HbA1c ≤ 7.0% at 3, 6, 12, and 18 months compared to those on intensified conventional insulin therapy [25]. Similarly, the EXTRA study, a European multicenter, multinational, retrospective chart review, assessed the effectiveness of IDegLira in controlling glycemia 6 months after initiation in routine clinical practice [26]. The study found that reductions in HbA1c were significantly greater in patients with higher baseline HbA1c levels: − 2.5% for those with baseline HbA1c ≥ 9.5%, − 0.9% for those between 8.5% and 9.5%, and − 0.6% for those between 7.5% and 8.5% (all between-group comparisons p < 0.001) [26]. These results highlight that patients with higher baseline HbA1c levels tend to achieve more substantial reductions in HbA1c, consistent with our findings for iGlarLixi.
In our study, we observed that mean HbA1c reductions were similar across BMI categories, reporting a − 1.39% mean HbA1c change in individuals with a BMI < 30 kg/m2 and − 1.34% in those with a BMI ≥ 30 kg/m2 at week 24 of iGlarLixi treatment. Likewise, in the LixiLan-L RCT, mean HbA1c reductions were comparable across BMI categories, reporting a − 1.1% mean HbA1c change in people presenting with BMI < 30 kg/m2 and in those presenting with BMI ≥ 30 kg/m2 at week 30 [10]. Moreover, in our study, a comparable proportion of people across the two BMI categories achieved HbA1c targets, with slight differences favoring the lower BMI group for higher HbA1c targets (< 7.5% and < 8.0%). Specifically, a quarter of participants in both BMI groups in our analysis reached HbA1c target < 7% at week 24, compared to a higher proportion reported in RCT subgroup analyses, in which three quarters of LixiLan-O participants in both BMI groups [11], and more than half of LixiLan-L participants [10] reached HbA1c target < 7% at week 30. Consistently, a real-world study from Italy performed in individuals with T2DM treated with IDegLira found no differences in HbA1c after 6 and 12 months between patients with baseline BMI > 30 kg/m2 and those with baseline BMI ≤ 30 kg/m2, highlighting the similar efficacy of combination therapies across different BMI categories [27].
A particularly noteworthy finding from our study is the discontinuation of sulphonylureas in nearly all patients when initiating iGlarLixi. This discontinuation may potentially contribute to the observed low incidence of hypoglycemia in our analysis [5, 12]. Having a less rigid iGlar dose titration may also explain the low hypoglycemia events observed in our analyses. Overall symptomatic hypoglycemia was reported in less than 5.0% of participants, irrespective of baseline HbA1c and BMI. The LixiLan trials have shown a higher incidence of documented symptomatic hypoglycemia, ranging from 25.6% to 40.0% [7,8,9,10,11]. Despite the less stringent method for reporting hypoglycemic events encountered in observational studies, our study was able to demonstrate the good safety profile of iGlarLixi across the spectrum of people with different baseline HbA1c and BMI. In real-life clinical practice, the EXTRA study of IDegLira reported an incidence of hypoglycemia of less than 1 event per patient-year [26]. This supports the notion that flexible dosing regimens in routine clinical practice have a favorable safety profile while achieving glycemic targets.
In addition to a favorable safety profile, iGlarLixi was able to reduce body weight. The more prominent weight loss was observed in people with obesity who are known to struggle with reducing body weight especially with insulin treatment. Therefore, the combination of iGlar and Lixi in iGlarLixi mitigates the weight gain associated with the insulin component, offering an advantage for iGlarLixi in people with overweight or obesity.
The main strength of our pooled analysis is its large sample size (N = 1406) coming from observational studies that may reflect the real-life population of European adults with inadequately controlled T2D. Furthermore, the MMRM approach, used to assess the change in glycemic parameters with adjustment to key confounding factors, reduces the degree of bias in the results. Despite adjusting for baseline glycemic variables (HbA1c and FPG), BMI, and prior insulin use, unmeasured confounding factors cannot be ruled out. Other limitations typical of observational studies include potential reporting bias, which may lead to missing data and underreporting, especially of AEs including hypoglycemia. Our pooled analysis may also be limited by the relatively short treatment duration, as a 24-week study duration may be short for full titration in real-life practice. Further investigation on the effectiveness, tolerability, and safety of iGlarLixi in people with different baseline characteristics of T2D may provide additional insights into the long-term iGlarLixi treatment.
Conclusions
This European pooled analysis, performed in people with inadequately controlled T2D in routine clinical practice, confirms the effectiveness and safety of iGlarLixi across different baseline HbA1c and BMI categories. iGlarLixi treatment demonstrated notable improvements in HbA1c levels, with greater reductions seen in those with higher baseline HbA1c levels. While hypoglycemia and gastrointestinal side effects were infrequent, weight loss was more pronounced in individuals with obesity. Overall, iGlarLixi effectively enhanced glycemic control and supported meaningful weight reduction among varying baseline HbA1c levels and BMIs.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Achila OO, Ghebretinsae M, Kidane A, Simon M, Makonen S, Rezene Y. Factors associated with poor glycemic and lipid levels in ambulatory diabetes mellitus type 2 patients in Asmara, Eritrea: a cross-sectional study. J Diabetes Res. 2020;2020:5901569.
Fang M, Wang D, Coresh J, Selvin E. Trends in diabetes treatment and control in U.S. adults, 1999–2018. N Engl J Med. 2021;384(23):2219–28.
Rakhis SA, AlDuwayhis NM, Aleid N, AlBarrak AN, Aloraini AA. Glycemic control for type 2 diabetes mellitus patients: a systematic review. Cureus. 2022;14(6): e26180.
Taybani Z, Bótyik B, Katkó M, Gyimesi A, Várkonyi T. Simplifying complex insulin regimens while preserving good glycemic control in type 2 diabetes. Diabetes Ther. 2019;10(5):1869–78.
American Diabetes Association Professional Practice Committee. Pharmacologic approaches to glycemic treatment Standards of Care in Diabetes 2024. Diabetes Care. 2024;47(Suppl 1):S158–78.
Skolnik N, Del Prato S, Blonde L, Galstyan G, Rosenstock J. Translating iGlarLixi evidence for the management of frequent clinical scenarios in type 2 diabetes. Adv Ther. 2021;38(4):1715–31.
Blonde L, Rosenstock J, Del Prato S, et al. Switching to iGlarLixi versus continuing daily or weekly GLP-1 RA in type 2 diabetes inadequately controlled by GLP-1 RA and oral antihyperglycemic therapy: the LixiLan-G randomized clinical trial. Diabetes Care. 2019;42(11):2108–16.
Aroda VR, Rosenstock J, Wysham C, et al. Efficacy and safety of LixiLan, a titratable fixed-ratio combination of insulin glargine plus lixisenatide in type 2 diabetes inadequately controlled on basal insulin and metformin: the LixiLan-L randomized trial. Diabetes Care. 2016;39(11):1972–80.
Rosenstock J, Aronson R, Grunberger G, et al. Benefits of LixiLan, a titratable fixed-ratio combination of insulin glargine plus lixisenatide, versus insulin glargine and lixisenatide monocomponents in type 2 diabetes inadequately controlled on oral agents: the LixiLan-O randomized trial. Diabetes Care. 2016;39(11):2026–35.
Wysham C, Bonadonna RC, Aroda VR, et al. Consistent findings in glycaemic control, body weight and hypoglycaemia with iGlarLixi (insulin glargine/lixisenatide titratable fixed-ratio combination) vs insulin glargine across baseline HbA1c, BMI and diabetes duration categories in the LixiLan-L trial. Diabetes Obes Metab. 2017;19(10):1408–15.
Davies MJ, Leiter LA, Guerci B, et al. Impact of baseline glycated haemoglobin, diabetes duration and body mass index on clinical outcomes in the LixiLan-O trial testing a titratable fixed-ratio combination of insulin glargine/lixisenatide (iGlarLixi) vs insulin glargine and lixisenatide monocomponents. Diabetes Obes Metab. 2017;19(12):1798–804.
Davies MJ, Aroda VR, Collins BS, et al. Management of hyperglycemia in type 2 diabetes, 2022 A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2022;45(11):2753–86.
Guja C, Kis JT, Haluzík M, et al. iGlarLixi (insulin glargine 100 U/ml plus lixisenatide) is effective and well tolerated in people with uncontrolled type 2 diabetes regardless of age: A REALI pooled analysis of prospective real-world data. Diabetes Obes Metab. 2023;25(6):1723–30.
Seufert J, Freemantle N, Guja C, et al. Real-life effectiveness of iGlarLixi (insulin glargine 100 U/ml and lixisenatide) in people with type 2 diabetes according to prior insulin use. Diabetes Obes Metab. 2024;26(7):2988–92.
Kis JT, Nagy G, Kovacs G. Effectiveness of iGlarLixi, a fixed-ratio combination of insulin glargine 100 U/ml and lixisenatide, in people with type 2 diabetes. Diabetes Ther. 2021;12(9):2517–29.
Bala C, Cerghizan A, Mihai BM, Moise M, Guja C. Real-world evidence on the use of a fixed-ratio combination of insulin glargine and lixisenatide (iGlarLixi) in people with suboptimally controlled type 2 diabetes in Romania: a prospective cohort study (STAR.Ro). BMJ Open. 2022;12(5): e060852.
Weisner T, Pfohl M, Pegelow K, Muller J, Seufert J. Effectiveness and safety of iGlarLixi in people with type 2 diabetes (PwT2D), Not at target on basal insulin (BI) and oral antidiabetic therapy (BOT)—Results from the Observational, Prospective Study CHANCE. Poster 794-P in American Diabetes Association (ADA). 2023; https://eacademy.sanofi.de/s3fs-public/pdf/64df5e266881e313628072.pdf
Bonadonna RC, Mauricio D, Müller-Wieland D, et al. Impact of age on the effectiveness and safety of insulin glargine 300 U/ml: results from the REALI European pooled data analysis. Diabetes Ther. 2021;12(4):1073–97.
Gourdy P, Bonadonna RC, Freemantle N, et al. Does gender influence the effectiveness and safety of insulin glargine 300 U/ml in patients with uncontrolled type 2 diabetes? Results from the REALI European pooled analysis. Diabetes Ther. 2022;13(1):57–73.
Müller-Wieland D, Freemantle N, Bonadonna RC, et al. Glycaemic control in people with type 2 diabetes mellitus switching from basal insulin to insulin glargine 300 U/ml (Gla-300): results from the REALI pooled database. Diabetes Ther. 2023;14(2):401–13.
Haluzík M, Seufert J, Guja C, et al. Effectiveness and safety of iGlarLixi (insulin glargine 100 U/ml plus lixisenatide) in type 2 diabetes according to the timing of daily administration: data from the REALI pooled analysis. Diabetes Ther. 2023;14(4):639–52.
Freemantle N, Bonadonna RC, Gourdy P, et al. Rationale and methodology for a European pooled analysis of postmarketing interventional and observational studies of insulin glargine 300 U/ml in diabetes: protocol of REALI project. BMJ Open. 2020;10(4): e033659.
European Medicines Agency. Suliqua: EPAR - Product information. 2023; Available from: https://www.ema.europa.eu/en/documents/product-information/suliqua-epar-product-information_en.pdf
Seaquist ER, Anderson J, Childs B, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care. 2013;36(5):1384–95.
Szépkúti S, Bandur S, Kovács G, et al. Real-world effectiveness of IDegLira compared with intensified conventional insulin therapy in adults with type 2 diabetes: a retrospective cohort study. BMC Endocr Disord. 2022;22(1):229.
Price H, Blüher M, Prager R, et al. Use and effectiveness of a fixed-ratio combination of insulin degludec/liraglutide (IDegLira) in a real-world population with type 2 diabetes: results from a European, multicentre, retrospective chart review study. Diabetes Obes Metab. 2018;20(4):954–62.
Zenari L, Da Porto A, De Moliner L, et al. Real-world evaluation of glycemic outcomes and extra-glycemic parameters in diabetic patients treated with the combined formulation degludec-liraglutide (IDegLira). Diabetes Ther. 2021;12(1):197–209.
Acknowledgements
Medical Writing and Editorial Assistance
Medical writing support was provided by Cynthia Abi Abdallah and Thomas Rohban of Partner 4 Health (Paris, France), in accordance with current Good Publication Practice (GPP4) guidelines (https://www.ismpp.org/gpp-2022). Medical writing was funded by Sanofi (Paris, France).
Funding
This study, including statistical analysis and medical writing, was funded by Sanofi (Paris, France). The journal’s Rapid Service Fee was also funded by Sanofi (Paris, France).
Author information
Authors and Affiliations
Contributions
All authors (Janos T. Kis, Jochen Seufert, Martin Haluzík, Mireille Bonnemaire, Carine Vera, Mathilde Tournay, Nick Freemantle, and Cristian Guja) contributed to the project design and the analysis plan. Mathilde Tournay performed the statistical analysis of the data. All authors were involved in the interpretation of the data, writing and reviewing drafts of the manuscript, and approved the final version for submission. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Corresponding author
Ethics declarations
Conflict of Interest
Jochen Seufert has received honoraria for talks and/or consultancy and/or research funding from Apitope, AstraZeneca, Bayer, Berlin Chemie, Boehringer Ingelheim, Bristol-Meyers Squibb, Eli Lilly, GI-Dynamics, GlaxoSmithKline, Intarcia, Ipsen, Janssen, LifeScan, MedScape, MSD, Novartis, Novo Nordisk, OmniaMed, Pfizer, Roche, Sanofi, Servier, Takeda, and Ypsomed. Nick Freemantle has received research support and has acted as a consultant for Allergan, Ipsen, Sanofi, AstraZeneca, Vertex, Aimmune, ALK, Gedeon Richter, Abbott Singapore, Galderma, Thea, and Novartis. Cristian Guja has participated in scientific advisory boards for and received consulting fees from AstraZeneca, Boehringer Ingelheim, Berlin-Chemie Menarini, Eli Lilly, KRKA, Merck KGaA, MSD, Novo Nordisk, Pfizer, Sandoz, Sanofi, and Servier. Martin Haluzík has received honoraria for talks and/or consultancy and/or research funding from Eli Lilly, Novo Nordisk, Sanofi, AstraZeneca, Mundipharma, Bristol-Meyers Squibb, Amgen, Boehringer Ingelheim, Janssen, Ypsomed and Johnson & Johnson. Mathilde Tournay is an IDDI employee and has acted as a biostatistics contractor for Sanofi. Carine Vera is an Ividata employee on behalf of Sanofi. Mireille Bonnemaire is a Sanofi employee. Janos T. Kis has received research funding from Sanofi.
Ethical Approval
Studies included in this pooled analysis were conducted according to the principles of the Declaration of Helsinki and the Good Clinical Practice guidelines and were approved by the appropriate ethics committees and institutional review boards. All participants provided written informed consent. As our analysis did not involve primary data collection by the authors, no additional ethical approval was deemed necessary for this pooled anonymized data analysis.
Additional information
Prior Presentation: Preliminary partial results were presented at the American Diabetes Association 84th Scientific Sessions, Orlando, Florida, June 21–24, 2024.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kis, J.T., Seufert, J., Haluzík, M. et al. Real-Life Effectiveness of iGlarLixi (Insulin Glargine 100 U/ml and Lixisenatide) in People with Type 2 Diabetes (T2D) According to Baseline HbA1c and BMI. Diabetes Ther (2024). https://doi.org/10.1007/s13300-024-01644-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13300-024-01644-0