Abstract
Purpose of Review
Although gut microbiota have been associated with the etiology of some diseases, the influence of foods on gut microbiota, especially among pregnant women, remains unclear. Hence, a systematic review was performed to investigate the association between diet and gut microbiota and their influence on metabolic health in pregnant women.
Recent Findings
We performed the systematic review using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 protocol to investigate the association between diet and gut microbiota and their influence on metabolic role in pregnant women. Five databases were searched for relevant peer-reviewed articles published in English since 2011. Two-staged screening of 659 retrieved records resulted in the inclusion of 10 studies. The collated findings suggested associations between nutrient intakes and four key microbes: Collinsella, Lachnospira, Sutterella, Faecalibacterium, and the Firmicutes/Bacteroidetes ratio in pregnant women.
Summary
Dietary intakes in pregnancy were found to modify the gut microbiota and positively influence the cell metabolism in pregnant women. This review, however, emphasizes the importance of conducting well-designed prospective cohorts to investigate the role of changes in dietary intakes within the pregnancy and the influence of such changes on gut microbiota.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity and gestational diabetes mellitus (GDM) have been established as severe public health issues and have a high risk of adverse consequences when occurring during pregnancy. Glucose and lipid metabolism-related diseases among pregnant women have repeatedly been vital indicators of several adverse maternal and established neonatal outcomes. Maternal obesity and GDM are associated with unfavourable pregnancy outcomes such as pre-eclampsia, caesarean delivery, preterm birth, and perinatal death [1–4]. Additionally, GDM raises the risk of postpartum type 2 diabetes mellitus (T2DM) in expectant mothers and the risk of obesity and other metabolic abnormalities in their offspring [5]. At 9 years following delivery, the risk of T2DM was around 20% for women with a history of GDM. Epidemiological evidence has consistently shown that among mothers with prior history of GDM, 30–84% of them had GDM recurrence in subsequent pregnancies [6], and 20–40% developed metabolic syndrome within 2–20 years [7, 8] and obesity within 5–16 years [9–11].
Prevention initiatives mainly focused on lifestyle modifications such as dietary changes and increased physical activity. Diet modifications are extensively utilized as the primary therapeutic option. Nutritional approaches for gestational hyperglycaemia share a common goal of improving blood glucose control and health outcomes for mothers and their infants. Despite the widely recognized function of medical nutrition therapy (MNT) in managing GDM, no agreement exists on the appropriate dietary nutrient advice for maintaining pregnant women’s normal glucose levels [12••], and dietary changes to prevent hyperglycaemia in pregnancy vary according to potential risk factors.
Several studies have found a substantial correlation between gut microbes and metabolic diseases [13–16]. During gestation, the gut microbiota undergoes considerable changes, which may affect the long-term metabolism of pregnant women and their newborns. The makeup of the intestinal microbiota is correlated to maternal obesity and hyperglycaemia. Various therapies, including antibiotic treatment and non-compliance intake of probiotics or prebiotic supplements, may alter metabolic function during pregnancy since all act on the gut microbiome and impact overall health [17]. The inappropriate use of antibiotics can lead to bacteria resistance, domination of microbial composition by pathogenic bacteria, loss of bacterial makeup, and decrease or even loss of certain bacterial species [18]. Hence, changes in the gut microbes might largely explain those alterations.
Diet also has been shown to alter the gut microbiota makeup within a short period [19, 20]. Studies suggest that food influence on metabolic responses differs according to the individual microbiome profile, providing a potential moderator between diet and metabolic health during pregnancy. These findings suggest that a customized strategy for human nutrition may optimize outcomes by demonstrating that a diet is not necessarily effective for all individuals or situations. The effect of specific nutritional changes on the role and makeup of gut bacteria is of great interest in the quest for the ideal strategy for preventing and managing GDM, and maternal obesity, and other metabolic disorders during gestation. Currently, very few data are available, and those that exist have conflicting findings.
Therefore, this review synthesizes recent evidence in this area. Specifically, we conducted a systematic review to examine associations between diet and gut microbiota during healthy pregnancies and pregnancies complicated by metabolic dysfunction. Additionally, we explored the possibility that specific nutrients modifying the makeup of the intestinal microbiota could have implications for pregnant women’s metabolic health.
Methods
We used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement 2020 [21] and the checklist (Supplementary Table S1) [21]. The systematic review protocol has been registered with the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42021276459) and can be retrieved via https://www.crd.york.ac.uk/prospero/.
Data Sources and Search Strategy
We included experimental or observational studies that reported on the role of dietary intake in modulating the gut microbiota and their impact on measures of metabolic function or glucose control (e.g. glycosylated haemoglobin (HbA1c), fasting blood glucose (FBG), oral glucose tolerance test (OGTT), insulin, Homeostatic Model Assessment for Insulin Resistance (HOMA-IR, lipid metabolism, and inflammatory profile). Studies were included if the population included pregnant women, with no exclusions based on maternal glucose levels. To be included in the review, the gut microbiota had to have been quantified from stool samples using any sequencing approach targeting the 16S ribosomal RNA gene. Studies that reported on pharmacotherapy, herbal remedies, and surgery were excluded.
We searched peer-reviewed papers from 2011 to 2022 using the following data sources: Ovid Medline, Scopus, PubMed, Cochrane Library, and Web of Science. The search strategy was built using the following MeSH terms and keywords: (gestational diabetes mellitus) OR (gestational diabetes) OR (diabetes in pregnancy) AND ((gut microbiota) OR (microbiome) OR (microbes) OR (microbial dysbiosis) OR (microbiota) AND ((diet) OR (dietary intake) OR (nutrition) OR (fats) OR (high fat diet) OR (glycemic index) OR (carbohydrate) OR (fiber) OR (fibre) OR (vitamin) OR (vegetarian) OR (fruits) OR (vegetables) OR (protein).
We limited our search to human studies and English-language publications. Additionally, we conducted manual searches for the papers using reference lists from the articles included and from earlier reviews. The complete database search strategy is provided in Supplementary Table S2.
Study Selection
Two authors (T.K. and A.R.) eliminated duplicated studies and checked retrieved reference titles and abstracts using Endnote Version X9. Following that, T.K. and A.R. independently assessed the full texts according to the review’s eligibility. Disagreements about whether an article was eligible were resolved through discussion. Studies were considered if the following conditions were met: (1) experimental or observational studies of dietary intake among pregnant women; (2) conducted metagenomics sequencing; (3) reported maternal metabolic outcomes such as glycosylated haemoglobin (HbA1c), fasting blood glucose level, lipid profiles, or gestational weight gain; 4) published between 1 January 2011 and 5 July 2022; and (5) published in the English language. Publications not reviewed by peers, including conference proceedings, online abstracts, and book chapters, were excluded. Studies conducted among non-pregnant people with type 1 or type 2 diabetes mellitus, probiotic/prebiotic supplements, and without defined dietary patterns /nutrient composition by class or amount were also rejected.
Data Extraction and Synthesis
T.K. and A.R. independently collected pertinent details from gathered studies using a Microsoft Excel spreadsheet: author, country, study design, number of participants, and primary and secondary outcomes. The primary outcomes were changes in the gut microbiota, including changes in relative bacterial abundance and diversity (α and β) and macro- and micronutrient levels. The nutrition levels could also be reported as a secondary outcome. Other secondary outcomes were changes in glucose–lipid metabolic profiles and weight. The data on the diverse gut microbiota and their association to metabolic variables and nutrient intakes in pregnant women, as well as the research features, were comprehensively synthesized.
Quality Assessment and Risk of Bias
We used the National Institutes of Health (NIH) quality assessment tool for case–control, observational cohort, and cross-sectional studies to assess the included studies’ methodological quality [22]. The study population, eligibility requirements, sample size rationale, observation period, exposure and outcome data, and additional sources of bias are all considered when evaluating the study’s quality. Every considered study was given a quality rating of good, fair, or poor. Two reviewers (T.K. and A.R.) independently assessed all analyses for methodological quality.
Results
Study Selection and Characteristics
The database search retrieved 655 records. Four hundred seventy-two titles and abstracts were evaluated after duplicate entries of 183 articles were removed. A manual search yielded four additional records. Full texts and the reference lists of the remaining 31 records were reviewed using the eligibility criteria. Ten studies fulfilled the eligibility criteria and were included in this review (Fig. 1). The citations of excluded full texts have been listed in Supplementary Table S3.
Table 1 provides an overview of the study’s characteristics. Our search did not retrieve any experimental studies involving a dietary intervention and its influence on the gut microbiota and metabolic health of pregnant women. Two prospective cohorts [23, 24••], seven cross-sectional studies [25–29, 30••, 31], and a case–control were included in this review [32••]. Four of these studies were conducted in Australia (40%), two in China (20%), and others in Finland, Italy, Spain, and Norway. The majority of the studies had a sample size of below 100 [23, 24••, 25, 29, 30••, 31, 32••], two studies had a sample size between 100 and 150 [26, 28], and one [27] included 210 pregnant women.
The age range of study participants was between 24 and 38 years old, with a BMI range of 24–35 kg/m2. Four studies recruited pregnant women with overweight and obesity [26–28, 31], while three recruited pregnant women diagnosed with GDM [23, 24••, 32••]. Three studies recruited pregnant women without GDM [25, 29, 30••]. Six studies included pregnant women who followed habitual dietary intake [26–29, 30••, 31], and three studies included MNT in their protocol [23, 24••, 32••]. Barret et al. compared vegetarian pregnant women with women who consumed omnivorous diets [25].
Methodological Quality Assessment
The mean score on the NIH Quality Assessment Scale was 52.5% (50–71%). There were no studies with poor quality; seven had acceptable quality, and three had good quality (Supplementary Tables S4 and S5).
Correlation Between Nutrients and Gut Microbial Abundance in Pregnant Women
Maternal nutrition and dietary intake are associated with maternal gut bacteria during pregnancy. Each study reported macro-/micronutrient or diet pattern associations with specific microbial makeup, relative abundances, and metabolic outcomes (Table 2).
Normal Healthy Pregnancy
All studies that included normal-weight women without GDM (normal pregnancy) reported a standard dietary intake [29, 30••], except for one study that included strict vegetarian intake [25]. Higher intake of carbohydrates in normal healthy pregnancy was positively associated with Proteobacteria [30••], Bacteroides [30••], and Firmicutes, but negatively linked with Roseburia [30••]. Barret et al. [25] noticed a richness in Roseburia in the vegetarian. However, there was no difference in total intake of carbohydrates or fibre between the vegetarian and omnivore groups. A lower intake of total carbohydrates was associated with a higher relative abundance of Lachnospira [30••].
Selma and team found that high-fat intake had higher Firmicutes [30••], Romboutsia (high monounsaturated fatty acids (MUFA) intake), and lower Proteobacteria [29, 30••] relative abundance in their microbiota [30••]. MUFA was also positively correlated with relative increases in Proteobacteria [29] and Romboutsia [30••]. Lachnospira also had a positive connection with total fat intake, including saturated fatty acid (SFA) and MUFA, but not polyunsaturated fatty acids (PUFA) [30••]. According to Barret et al., vegetarians consume diets high in PUFA, especially ω-6 fatty acids such as linoleic acid, compared to MUFA [25]. In their investigation, Roseburia richness was strongly associated with PUFA intake.
Total protein intake, especially those from an animal source, was negatively associated with Actinobacteria [30••] and Proteobacteria [29]. Proteobacteria was positively linked with vitamin D intake. However, the richness is reduced through higher vitamin E intake in healthy pregnant women [29]. Conversely, a low abundance of Collinsella was recorded in vegetarian women who consume a relatively high diet rich in fibre, according to Barret et al. [25] study.
Overweight/Obese Pregnant Women
Similar to women without metabolic risk factors, studies on overweight and obese pregnant women reported on standard diets, representative of habitual intake [26–28, 31]. Gomez-Arango et al. [26] reported that the prevalence of Collinsella was higher in women with low fibre consumption. Roytio et al. [28] also observed a positive correlation with Firmicutes in high-fibre/moderate-fat intake group. They also observed a low abundance of Barnsiellaceae in the high-fat intake group and a high abundance of Firmicutes strongly linked with vitamin A consumption [28].
Robinson et al. [31] found that Roseburia is more prevalent in the intestinal microbiota of overweight/obese pregnant women with ketonuria. However, the intake of carbohydrates did not differ significantly between women with ketonuria and those without ketonuria. The researchers speculated that it might result from the small sample population (n = 22).
Lastly, Roytio et al. [28] stated a significantly low abundance of Ruminococcus and Roseburia in pregnant women who consume high iron supplements. In the gut microbiota of pregnant women with minimal supplemental iron intake, bacteria generating short-chain fatty acids, including Lachnospira, Sutterella, and the lactate producer Lactobacillus, were dominant, according to their findings by network analyses.
GDM Pregnant Women
Women with GDM are generally given dietary advice based on MNT. The women with GDM recruited in the study by Wu et al. [24••] were asked to follow a diet with the target composition of 35–45% carbohydrates (80% complex carbohydrates with a low glycaemic index and 20% simple carbohydrates), 18–20% protein (50% animal and 50% plants), and 35% fat (16% monounsaturated, 10% polyunsaturated and 9% saturated) with moderately low saturated fat levels, fibre intake of at least 20–25 g/day. Acidaminococcaceae, Enterobacteriaceae, and Bacteroidaceae were less common in GDM pregnant women who followed the MNT for 2 weeks, while Bifidobacteriaceae and butyric acid-producing bacteria (Prevotellaceae and Lachnospiraceae) were more common than in GDM microbial samples at enrolment.
The GDM women recruited in Chen et al. [32••] had a proportion of carbohydrates of about 50–60%, and the remaining energy supplying nutrients contained 15–20% protein and 25–30% fat, with a reasonable distribution of cereals and potatoes, eggs, legumes, fish, dairy products, vegetables, and oils. The portions of cereals and potatoes, egg, beans, fish, and vegetables were evenly distributed over three meals, while milk and products were spread over 2–3 additional meals. Before the MNT, there were more Rosella, Bifidobacterium, Clostridium, Holdemania, and Proteus in the guts of pregnant women who adhered to the MNT. There were also more bacteria in the intestines of pregnant women who did not adhere to MNT recommendations. These bacteria, such as Leuconostocaceae, Weissella, Prevotella, and Bacillus cereus, help the body improve its blood sugar level. Pathogens like Desulfovibrio, Aeromonas, and Gemella, which can cause weight gain, poor glucose tolerance, and insulin resistance, were also more common in GDM pregnant women who did not adhere to their treatment plans.
The nutritional recommendation given to GDM women under Ferrocino et al. [23] study was 45% total energy from carbohydrates, < 10% of energy from rapidly absorbed sugars, 18–20% energy from protein, 35% energy from fats, at least 20–25 g/day fibre intake, and no alcohol intake. Ferrocino et al. reported a strong correlation between protein intake and Faecalibacterium in GDM pregnant women in the second and third trimesters [23]. Alistipes, on the other hand, revealed a positive correlation with fat intake after adjusting for weight and age of the GDM pregnant women [23]. They also observed a direct correlation between Roseburia and fibre consumption, although it did not meet the statistical thresholds.
Discussion
This systematic review aimed to assess the effect of nutrition on gut microbiota modulation and its influence on metabolism in pregnant women. Several previous analyses examined the impact of lifestyle treatments on their ability to improve glucose control in pregnant women with GDM [33–35]. To the best of our knowledge, no systematic reviews are available on gut microbiota-targeted diets influencing the metabolic function of pregnant women. The evidence generated by this review demonstrates that dietary intake is associated with differences in the gut microbiota, which, in turn, is associated with metabolic health in pregnant women. If repeated in intervention study designs (i.e. randomized controlled trials and feeding studies), the current findings could contribute to more effective management targeting the risk of metabolic dysfunction in pregnant women.
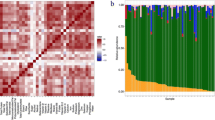
In this systematic review, a few gut microbes were related to the significance of a major nutrient intake and to metabolic markers in pregnant women (Fig. 2). Higher fibre intake was associated with a lower abundance of Collisella in healthy pregnant women, in the study by Barret et al. [25]. Similarly, researchers noticed a higher abundance of Collisella in oveweight or obese pregnant women [26] and pregnant women with GDM who did not adhere to MNT [23]. Dietary fibre is necessary for microbes to generate short-chain fatty acids (SCFAs) and to surpass the adipose tissue’s natural capacity for lipid storage rather than energy expenditure, resulting in a good energy balance that can significantly impact the gut microbe [36]. It decreases cholesterol absorption by increasing faecal mass and binding to bile acids in the digestive tract. [37–39]. Additionally, fermentation of dietary fibre has been demonstrated to decrease postprandial blood glucose and insulin levels [37,37,]. Low fibre intake also promotes bacterial growth that can utilize host-secreted mucus glycoproteins and other “non-fibre” energy sources, which may influence the colonic mucus barrier and microbial overgrowth and proliferation [40].
Collinsella, on the other hand, is frequently referred to as a strictly anaerobic pathobiont that produces lactate (instead of butyrate or other SCFA). Increases in lactate amounts induce insulin resistance in skeletal muscle by suppressing glycolysis and impairing insulin signalling [41]. The present data suggest that a diet low in dietary fibre in pregnant women may influence the intestinal microbiota, particularly the Collinsella species. Gomez et al. [41] reported that changing Collinsella abundance may affect lipid and glucose metabolism and may serve as markers of poor glucose metabolism during pregnancy. As a result, we predict that decreased dietary fibre intake during early pregnancy results in abundant Collinsella spp., which disrupts gut integrity, resulting in increased inflammation and the beginning of maternal hyperglycaemia.
Secondly, high fibre and less carbohydrate consumption were related to the increased abundance of Lachnospira in healthy pregnant women and those with overweight/obesity and were negatively associated with very low-density lipoprotein (VLDL) cholesterol in these pregnant women [25, 28, 30••]. Barret et al. concluded that Lachnospira is favourably associated with vegetarian diets in their study since vegetarians consume less protein and sugar than omnivores, with modest changes in fatty acid intake [25] in healthy pregnant women. Similarly, Roytio et al. studied the connection between maternal gut microbiota and diet composition as determined by a 3-day food diary in overweight and obese pregnant women with varied fibre and fat intakes [28]. In their study, the high abundance of Lachnospira had an inverse relation with VLDL particles, triglyceride concentration, and total triglyceride levels [28]. In the same line, the Medika Study reported that several species of Lachnospiraceae were positively associated with fibre-, potassium-, and vegetable-based protein intakes in adults with chronic kidney disease [42, 43].
In contrast to these studies, high abundances of Lachnospiraceae were positively associated with glucose and/or lipid metabolism in women with obesity and metabolic syndrome [44], in individuals with glucose metabolism disorders [45], and in male patients [46], indicating the vital role of Lachnospiraceae in metabolic disturbance condition. Roseburia, one of the species under the Lachnospiraceae family, has also been elevated in obese pregnant women with ketonuria. However, the carbohydrate intake was not comparable to that of pregnant women without ketonuria [31].
According to a recently reviewed study, Lachnospiraceae species metabolize fermentable carbohydrates, i.e. dietary fibre, and create butyrate and other short-chain fatty acids that alter glucose metabolism and diabetes risk [47]. Metagenomics research has also demonstrated its ability to use complex organic materials and transport breakdown products of different sizes and components [48]. This was most likely accomplished through ATP binding cassette (ABC) transporter proteins expressed by the genomes of several Lachnospiraceae species [49]. However, the involvement of the beneficial Lachnospiraceae bacteria in high-fat/protein metabolism is less clear among pregnant women, leading to the controversial role of Lachnospiraceae between pregnant women and the adult population (older adults, individuals with metabolic diseases, and non-pregnant women). Further studies on this topic are required.
Thirdly, the pro-inflammatory-type bacteria, Sutterella (proteobacteria phylum), have been strongly correlated with high protein intake and C-reactive protein (CRP) levels in women with GDM [23]. Likewise, the predicted metagenomes revealed a link between Sutterella and KEGG genes involved in lipopolysaccharide production (LPS). Gram-negative bacteria (proteobacteria) can produce pro-inflammatory LPS, resulting in an inflammatory condition linked to type 2 diabetes and obesity [50]. Nevertheless, the linkage between high protein intake and increased abundance of Sutterella is undetermined in those pregnant women with GDM [23]. On the other hand, a high abundance of Sutterella was observed in overweight/obese pregnant women who had minimal consumption of iron supplements, according to the network analysis done by Nitert et al. [27]. The iron status could be essential in developing chronic inflammatory diseases [51]. Iron deficiency is associated with chronic inflammatory indicators and other well-known risk factors for diabetes, obesity, and metabolic syndrome [52–54]. Therefore, the evidence suggests that high protein intake and low iron levels lead to a high abundance of Sutterella in GDM and obese pregnant women. However, the conclusive mechanisms of this relationship remain unclear.
Diet therapy is widely assumed to influence the intestinal microbiota in GDM [55]. Metabolites generated from microbiota alter glucose homeostasis via intestinal gluconeogenesis [56]. Women who do not comply with a recommended dietary change (e.g. carbohydrate restriction) to treat GDM have a higher abundance of the Leuconostocaceae, Weissella, Prevotella, Bacillus cereus, and Faecalibacterium, implying that diet’s function on maternal blood sugar control may be mediated via the gut microbes [23, 32••]. Supporting that, Benno et al. reported that the intake of more meat, animal fat, sugar, processed foods, and low fibre foods (the usual westernized diet) is associated with a lower count of Faecalibacterium prausnitzii. In contrast, a high-fibre (vegetables and fruits) and low meat diet increase the count [57]. The increased abundance of Faecalibacterium, an anti-inflammatory bacterium, in a study done by Ferrocino et al., suggested that this rise may be a corrective mechanism to combat the pro-inflammatory condition that could harm the unborn [23]. Indeed, Faecalibacterium abundance and fasting glucose levels were found to have an inverse connection, considering the established relationship between inflammation and metabolic impairment. Accordingly, metagenomic investigations found Faecalibacterium prausnitzii highly discriminating in diagnosing type 2 diabetes [58, 59]. In human studies of faecal microbiota, these butyrate-producing bacteria were inversely related to diabetes [13, 60–62].
Wu et al. [24••] explored the ratio of Firmicutes to Bacteroidetes to comprehend the role of diet management during GDM pregnancy. A higher ratio of Firmicutes to Bacteroidetes was suggested as a possible biomarker of obesity and other metabolic syndromes compared with the normal BMI of pregnant women. The ratio of Firmicutes to Bacteroidetes changed differently in the GDM and non-GDM groups. At the end of the study, healthy samples with no diet management demonstrated an almost significant rise in the ratio of Firmicutes to Bacteroidetes, which suggests energy homeostasis changes during pregnancy. Zheng et al. [55] found that the Firmicutes/Bacteroidetes ratio was higher in the second (T2) trimester than in the first (T1) trimester, which was similar to what Wu et al. [24••] found in healthy pregnant women. In the study by Wu et al. [24••], the ratio of Firmicutes to Bacteroidetes did not change in GDM managed with diet intervention. This suggests that diet intervention could be helpful in GDM management by affecting the Firmicutes/Bacteroidetes ratio.
Nevertheless, in a study by Ferrocino et al. [23], there was an increase in the number of Firmicutes and a decrease in the number of Bacteroidetes in MNT-adherent patients whose total and saturated fat intake and CRP levels went down during pregnancy. This could be because the patients gained excessive weight during pregnancy even though they were already overweight at the enrolment stage, which is nearly similar in obese people [63, 64••]. However, Chen et al. [32••] did not analyse and compare the ratio of Firmicutes/Bacteroides in obese women with GDM, which restricts us from reaching a conclusion. Thus, this theory has to be further explored to gain and update the knowledge on the influence of MNT on GDM intestinal microbiota.
There were substantial connections between different microorganisms’ macronutrients and metabolic function in all the studies analysed. Nevertheless, the gut microbiota field and its investigation in pregnant women are still in its early stages, and the precise mechanisms involved are difficult to be confirmed. Heterogeneity among individuals was a possible concern in the gut microbiota–diet analysis conducted. Research findings are hard to compare due to the diverse ethnicities and dietary habits of the researched cohorts, which result in multi-variations in the pattern of the intestinal microbiota, and the different methods used to analyse the microbiota, both of which produce sometimes contradicting findings. Moreover, to identify a significant effect of the treatment in this field, a sufficient sample size is required to account for the significant variability between studies reported on gut microbes.
Conclusions
Lifestyle changes can alter gut flora and affect blood glucose homeostasis. To fully exploit the gut microbiota’s potency and influence on disease pathophysiology and health, research must examine a proper intervention timeframe, sample size, and long-term follow-up (throughout gestational duration) to thoroughly understand the relationship between the host and its microbes. We have previously demonstrated that altering the gut microbiota significantly affects the pathogenesis of GDM [39]. The current review supported the significant role of dietary intake in modifying gut microbiota composition and its influence on metabolic reactions among pregnant women. However, the implications of the current findings for every pregnant woman remained undetermined due to the diversity of food intake across cultures and ethnic groups worldwide. Another unsolved topic is why some people respond more profoundly to treatments than others. Research has focused mostly on preclinical models, restricting their translation into individuals for use as therapeutic approaches. The number of articles included in this systematic review limits a firm conclusion about the microbial species and metabolic outcomes. It emphasizes the importance of conducting further well-designed human trials. As the frequency of metabolic disorders and adverse obstetric outcomes grows, and our awareness of the gut microbes improves, there is an excellent opportunity to evaluate the relevance of certain bacteria and their activity within a given bacterial population. This, in return, will set the groundwork for transferring preclinical findings into clinical practice by combining numerous methodologies and individual features into a molecular genetics approach to give individually tailored lifestyle therapies.
Data Availability
Data related to this systematic review are available within the article and as supplementary materials.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Marchi J, Berg M, Dencker A, Olander EK, Begley C. Risks associated with obesity in pregnancy, for the mother and baby: a systematic review of reviews. Obes Rev. 2015;16:621–38. https://doi.org/10.1111/obr.12288.
Stamilio DM, Scifres CM. Extreme obesity and postcesarean maternal complications. Obstet Gynecol. 2014;124:227–32. https://doi.org/10.1097/aog.0000000000000384.
American Diabetes Association. Management of diabetes in pregnancy: standards of medical care in diabetes. Diabetes Care. 2018;41:S137–43. https://doi.org/10.2337/dc18-S013.
Spaight C, Gross J, Horsch A, Puder JJ. Gestational diabetes mellitus. Endocr Dev. 2016;31:163–78. https://doi.org/10.1159/000439413.
Hummel S, Much D, Rossbauer M, Ziegler AG, Beyerlein A. Postpartum outcomes in women with gestational diabetes and their offspring: POGO study design and first-year results. Rev Diabet Stud. 2013;10:49–57. https://doi.org/10.1900/rds.2013.10.49.
Kim C, Berger DK, Chamany S. Recurrence of gestational diabetes mellitus: a systematic review. Diabetes Care. 2007;30:1314–9. https://doi.org/10.2337/dc06-2517.
Gunderson EP, Jacobs DR, Chiang V, Lewis CE, Feng J, et al. Duration of lactation and incidence of the metabolic syndrome in women of reproductive age according to gestational diabetes mellitus status: a 20-year prospective study in CARDIA (coronary artery risk development in young adults). Diabetes. 2010;59:495–504. https://doi.org/10.2337/db09-1197.
Lauenborg J, Mathiesen E, Hansen T, Glümer C, Jørgensen T, et al. The prevalence of the metabolic syndrome in a Danish population of women with previous gestational diabetes mellitus is three-fold higher than in the general population. J Clin Endocrinol Metab. 2005;90:4004–10. https://doi.org/10.1210/jc.2004-1713.
Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. 2009;373:1773–9. https://doi.org/10.1016/S0140-6736(09)60731-5.
Hanna FW, Peters JR. Screening for gestational diabetes; past, present and future. Diabet Med. 2002;19:351–8. https://doi.org/10.1046/j.1464-5491.2002.00684.x.
Lee AJ, Hiscock RJ, Wein P, Walker SP, Permezel M. Gestational diabetes mellitus: clinical predictors and long-term risk of developing type 2 diabetes: a retrospective cohort study using survival analysis. Diabetes Care. 2007;30:878–83. https://doi.org/10.2337/dc06-1816.
•• Ponzo V, Fedele D, Goitre I, Leone F, Lezo A, Monzeglio C, et al. Diet-gut microbiota interactions and gestational diabetes mellitus (GDM). Nutrients. 2019;11:330. https://doi.org/10.3390/nu11020330. This review highlights the importance of finding a personalized dietary treatment based on gut microbiota and diet response in pregnancy complicated by GDM.
Qin J, Li Y, Cai Z, Li S, Zhu J, Zhang F, et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature. 2012;490:55–60. https://doi.org/10.1038/nature11450.
Schwiertz A, Taras D, Schafer K, Beijer S, Bos NA, Donus C, et al. Microbiota and SCFA in lean and overweight healthy subjects. Obesity. 2010;18:190–5. https://doi.org/10.1038/oby.2009.167.
Le KA, Li Y, Xu X, Yang W, Liu T, Zhao X, et al. Alterations in fecal Lactobacillus and Bifidobacterium species in type 2 diabetic patients in Southern China population. Front Physiol. 2012;3:496. https://doi.org/10.3389/fphys.2012.00496.
Gu Y, Wang X, Li J, et al. Analyses of gut microbiota and plasma bile acids enable stratification of patients for antidiabetic treatment. Nat Commun. 2017;8:1785. https://doi.org/10.1038/s41467-017-01682-2.
Griffin C. Probiotics in obstetrics and gynaecology. Aust N Z J Obstet Gynaecol. 2015;55:201–9. https://doi.org/10.1111/ajo.12303.
Pilmis B, Le Monnier A, Zahar JR. Gut microbiota, antibiotic therapy and antimicrobial resistance: a narrative review. Microorganisms. 2020;8:269. https://doi.org/10.3390/microorganisms8020269.
Singh RK, Chang HW, Yan D, Lee KM, Ucmak D, Wong K, et al. Influence of diet on the gut microbiome and implications for human health. J Transl Med. 2017;15:73. https://doi.org/10.1186/s12967-017-1175-y.
Scott KP, Gratz SW, Sheridan PO, Flint HJ, Duncan SH. The influence of diet on the gut microbiota. Pharmacol Res. 2013;69:52–60. https://doi.org/10.1016/j.phrs.2012.10.020.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
National Institute of Health. Study quality assessment tools. Available from: http://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed on 1 Sept 2021.
Ferrocino I, Ponzo V, Gambino R, Zarovska A, Leone F, Monzeglio C, et al. Changes in the gut microbiota composition during pregnancy in patients with gestational diabetes mellitus (GDM). Sci Rep. 2018;8:12216. https://doi.org/10.1038/s41598-018-30735-9.
•• Wu N, Zhou J, Mo H, Mu Q, Su H, Li M, et al. The gut microbial signature of gestational diabetes mellitus and the association with diet intervention. Front Cell Infect Microbiol. 2022;11:800865. https://doi.org/10.3389/fcimb.2021.800865. This prospective cohort study highlights the changes in the Firmicutes/Bacteroides ratio and some specific taxa, rather than a change in the whole gut microbial pattern among GDM patients with a short-term diet management.
Barrett HL, Gomez-Arango LF, Wilkinson SA, McIntyre HD, Callaway LK, Morrison M, et al. A vegetarian diet is a major determinant of gut microbiota composition in early pregnancy. Nutrients. 2018;10:890. https://doi.org/10.3390/nu10070890.
Gomez-Arango LF, Barrett HL, Wilkinson SA, Callaway LK, McIntyre HD, Morrison M, et al. Low dietary fibre intake increases Collinsella abundance in the gut microbiota of overweight and obese pregnant women. Gut Microbes. 2018;9:189–201. https://doi.org/10.1080/19490976.2017.1406584.
Nitert MD, Gomez-Arango LF, Barrett HL, McIntyre HD, Anderson GJ, Frazer DM, et al. Iron supplementation has minor effects on gut microbiota composition in overweight and obese women in early pregnancy. Br J Nutr. 2018;120:283–9. https://doi.org/10.1017/S0007114518001149.
Roytio H, Mokkala K, Vahlberg T, Laitinen K. Dietary intake of fat and fibre according to reference values relates to higher gut microbiota richness in overweight pregnant women. Br J Nutr. 2017;118:343–52. https://doi.org/10.1017/S0007114517002100.
Mandal S, Godfrey KM, McDonald D, Treuren WV. Bjornholt JV, Midtvedt T, et al. Fat and vitamin intakes during pregnancy have stronger relations with a pro-inflammatory maternal microbiota than does carbohydrate intake. Microbiome. 2016:55. https://doi.org/10.1186/s40168-016-0200-3.
•• Selma-Royo M, García-Mantrana I, Calatayud M, Parra-Llorca A, Martínez-Costa C, Collado MC. Maternal diet during pregnancy and intestinal markers are associated with early gut microbiota. Eur J Nutr. 2021;60:1429–42. https://doi.org/10.1007/s00394-020-02337-7. This cross-sectional study highlights the positive correlation of Firmicutes in the neonatal microbiota to fat intake (SFA and MUFA) in the maternal diet. A maternal diet defines the neonatal microbial profile with potential health outcomes.
Robinson H, Barrett H, Gomez-Arango L, McIntyre HD, Callaway L, Nitert MD. Ketonuria is associated with changes to the abundance of Roseburia in the gut microbiota of overweight and obese women at 16 weeks gestation: a cross-sectional observational study. Nutrients. 2019;11:1836. https://doi.org/10.3390/nu11081836.
•• Chen J, Yang YY, Yu NN, Sun WX, Yang YY, Zhao M. Relationship between gut microbiome characteristics and the effect of nutritional therapy on glycemic control in pregnant women with gestational diabetes mellitus. PLoS One. 2022;17:e0267045. https://doi.org/10.1371/journal.pone.0267045. This study found that the decrease in the abundance of the characteristic gut microbiome was positively correlated with blood glucose. It may be a factor influencing the poor hypoglycaemic effect of MNT in pregnant women with GDM.
Brown J, Alwan NA, West J, Brown S, McKinlay CJ, Farrar D, et al. Lifestyle interventions for the treatment of women with gestational diabetes. Cochrane Database Syst Rev. 2017;5(5):CD011970. https://doi.org/10.1002/14651858.CD011970.pub2.
Martis R, Crowther CA, Shepherd E, Alsweiler J, Downie MR, Brown J. Treatments for women with gestational diabetes mellitus: an overview of Cochrane systematic reviews. Cochrane Database Syst Rev. 2018;8:CD012327. https://doi.org/10.1002/14651858.CD012327.pub2.
Dolatkhah N, Hajifaraji M, Shakouri SK. Nutrition therapy in managing pregnant women with gestational diabetes mellitus: A literature review. 2018;12:57–72.
Tarini J, Wolever TM. The fermentable fibre inulin increases postprandial serum short-chain fatty acids and reduces free-fatty acids and ghrelin in healthy subjects. Appl Physiol Nutr Metab. 2010;35:9–16. https://doi.org/10.1139/h09-119.
Alminger M, Eklund-Jonsson C. Whole-grain cereal products based on a high-fibre barley or oat genotype lower postprandial glucose and insulin responses in healthy humans. Eur J Nutr. 2008;47:294–300. https://doi.org/10.1007/s00394-008-0724-9.
Martínez I, Lattimer JM, Hubach KL, Case JA, Yang J, Weber CG, et al. Gut microbiome composition is linked to whole grain-induced immunological improvements. ISME J. 2013;7:269–80. https://doi.org/10.1038/ismej.2012.104.
Desai MS, Seekatz AM, Koropatkin NM, Kamada N, Hickey CA, Wolter M, et al. A dietary fiber-deprived gut microbiota degrades the colonic mucus barrier and enhances pathogen susceptibility. Cell. 2016;167:1339-53. https://doi.org/10.1016/j.cell.2016.10.043.
Choi CS, Kim YB, Lee FN, Zabolotny M, Kahn BB, Youn JH. Lactate induces insulin resistance in skeletal muscle by suppressing glycolysis and impairing insulin signaling. Am J Physiol Endocrinol Metab. 2002;283:E233–40. https://doi.org/10.1152/ajpendo.00557.2001.
Gomez-Arango LF, Barrett HL, McIntyre HD, Callaway LK, Morrison M, Dekker Nitert M. Connections between the gut microbiome and metabolic hormones in early pregnancy in overweight and obese women. Diabetes. 2016;65:2214–23. https://doi.org/10.2337/db16-0278.
Di Iorio BR, Rocchetti MT, De Angelis M, Cosola C, Marzocco S, Di Micco L, et al. Nutritional therapy modulates intestinal microbiota and reduces serum levels of total and free indoxyl sulfate and P-Cresyl sulfate in chronic kidney disease (Medika Study). J Clin Med. 2019;8:1424. https://doi.org/10.3390/jcm8091424.
Chavez-Carbajal A, Nirmalkar K, Perez-Lizaur A, Hernandez-Quiroz F, Ramirez-del-Alto S, Garcia-Mena J, et al. Gut microbiota and predicted metabolic pathways in a sample of Mexican women affected by obesity and obesity plus metabolic syndrome. Int J Mol Sci. 2019;20:438. https://doi.org/10.3390/ijms20020438.
Lippert K, Kedenko L, Antonielli L, Kedenko I, Gemeier C, Leitner M, et al. Gut microbiota dysbiosis associated with glucose metabolism disorders and the metabolic syndrome in older adults. Benef Microbes. 2017;8:545–56. https://doi.org/10.3920/bm2016.0184.
Salonen A, Lahti L, Salojarvi J, Holtrop G, Korpela K, Duncan SH, et al. Impact of diet and individual variation on intestinal microbiota composition and fermentation products in obese men. ISME J. 2014;8:2218–30. https://doi.org/10.1038/ismej.2014.63.
Utzschneider KM, Kratz M, Damman CJ, Hullar M. Mechanisms linking the gut microbiome and glucose metabolism. J Clin Endocrinol Metab. 2016;101:1445–54. https://doi.org/10.1210/jc.2015-4251.
Biddle A, Stewart L, Blanchard J, Leschine S. Untangling the genetic basis of fibrinolytic specialisation by Lachnospiraceae and Ruminococcaceae in diverse gut communities. Diversity. 2013;5:627–40. https://doi.org/10.3390/d5030627.
Vacca M, Celano G, Calabrese FM, Portincas , Gobbetti M, De Angelis M. The controversial role of human gut Lachnospiraceae. Microorganisms. 2020;8:573. https://doi.org/10.3390/microorganisms8040573.
Allin KH, Nielsen T, Pedersen O. Mechanisms in endocrinology: Gut microbiota in patients with type 2 diabetes mellitus. Eur J Endocrinol. 2015;172:R167–77. https://doi.org/10.1530/eje-14-0874.
Wessling-Resnick M. Iron homeostasis and the inflammatory response. Annu Rev. 2010;30:105–22. https://doi.org/10.1146/annurev.nutr.012809.104804.
Denic S, Agarwal MM. Nutritional iron deficiency: an evolutionary perspective. Nutrition. 2007;23:603–14. https://doi.org/10.1016/j.nut.2007.05.002.
Jiang R, Manson JE, Meigs JB, Ma J, Rifai N, Hu FB. Body iron stores in relation to risk of type 2 diabetes in apparently healthy women. JAMA. 2004;291:711–7. https://doi.org/10.1001/jama.291.6.711.
Rajpathak SN, Crandall JP, Wylie-Rosett J, Kabat GC, Rohan TE, Hu FB. The role of iron in type 2 diabetes in humans. Biochim Biophys Acta. 2009;1790:671–81. https://doi.org/10.1016/j.bbagen.2008.04.005.
Zheng W, Xu Q, Huang W, Yan Q, Chen Y, Zhang L, et al. Gestational diabetes mellitus is associated with reduced dynamics of gut microbiota during the first half of pregnancy. mSystems. 2020;5. https://doi.org/10.1128/mSystems.00109-20.
De Vadder F, Kovatcheva-Datchary P, Zitoun C, Duchampt A, Backhed F, Mithieux G. Microbiota-produced succinate improves glucose homeostasis via intestinal gluconeogenesis. Cell Metab. 2016;24:151–7. https://doi.org/10.1016/j.cmet.2016.06.013.
Benno Y, Endo K, Miyoshi H, Okuda T, Koishi H, Mitsuoka T. Effect of rice fiber on human fecal microflora. Microbiol Immunol. 1989;33:435–40. https://doi.org/10.1111/j.1348-0421.1989.tb01992.x.
Lekva T, Norwitz ER, Aukrust P, Ueland T. Impact of systemic inflammation on the progression of gestational diabetes mellitus. Curr Diab Rep. 2016;16:26. https://doi.org/10.1007/s11892-016-0715-9.
Karlsson FH, Tremaroli V, Nookaew I, Bergstrom V, Behre CJ, Fagerberg B, Nielsen J, Backhed F. Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature. 2013;498:99–103. https://doi.org/10.1038/nature12198.
Tilg H, Moschen AR. Microbiota and diabetes: an evolving relationship. Gut. 2014;63:1513–21. https://doi.org/10.1136/gutjnl-2014-306928.
Zhang X, Shen D, Fang Z, Jie Z, Qiu X, Zhang C, Chen Y, Ji L. Human gut microbiota changes reveal the progression of glucose intolerance. PLoS One. 2013;8:e71108. https://doi.org/10.1371/journal.pone.0071108.
Furet JP, Kong LC, Tap J, Poitou C, Basdevant A, Bouillot JL, et al. Differential adaptation of human gut microbiota to bariatric surgery-induced weight loss: links with metabolic and low-grade inflammation markers. Diabetes. 2010;59:3049–57. https://doi.org/10.2337/db10-0253.
Fandriks L. Roles of the gut in the metabolic syndrome: an overview. J Intern Med. 2017;281:319–36. https://doi.org/10.1111/joim.12584.
Dao MC, Everard A, Clément K, Cani PD. Losing weight for a better health: role for the gut microbiota. Clin Nutr Exp. 2016;6:39–58. https://doi.org/10.1016/j.yclnex.2015.12.001.
•• Kunasegaran T, Balasubramaniam V, Arasoo VJT, Palanisamy UD, Ramadas A. The modulation of gut microbiota composition in the pathophysiology of gestational diabetes mellitus: a systematic review. Biology. 2021;10:1027. https://doi.org/10.3390/biology10101027. This scoping review highlights the role of gut microbiota in the pathophysiology of GDM and gave insights on the importance of conducting a well-designed microbiome experiment.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. The study was funded by the Jeffrey Cheah School of Medicine and Health Sciences’ Early Career Researcher (ECR) Grant 2021 (EC-000016).
Author information
Authors and Affiliations
Contributions
Thubasni Kunasegaran conducted the literature search, data synthesis, and manuscript writing. Amutha Ramadas contributed to the literature search, data synthesis, and technical support. Amutha Ramadas, Vinod RMT Balasubramaniam, Valliammai Jayanthi Thirunavuk Arasoo, and Uma Devi Palanisamy were involved in the critical review of the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors do not have any potential conflicts of interest to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kunasegaran, T., Balasubramaniam, V.R.M.T., Arasoo, V.J.T. et al. Diet Gut Microbiota Axis in Pregnancy: A Systematic Review of Recent Evidence. Curr Nutr Rep 12, 203–214 (2023). https://doi.org/10.1007/s13668-023-00453-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13668-023-00453-4