Abstract
Introduction
Shorter courses of antimicrobials have been shown to be non-inferior to longer, “traditional” duration of therapies, including for some severe healthcare-associated infections, with a few exceptions. However, evidence is lacking regarding shorter regimes against severe infections by multidrug-resistant Gram-negative bacteria (MDR-GNB), which are often caused by distinct strains and commonly treated with second-line antimicrobials. In the duratiOn of theraPy in severe infecTIons by MultIdrug-reSistant gram-nEgative bacteria (OPTIMISE) trial, we aim to assess the non-inferiority of 7-day versus 14-day antimicrobial therapy in critically ill patients with severe infections caused by MDR-GNB.
Methods
This is a randomized, multicenter, open-label, parallel controlled trial to assess the non-inferiority of 7-day versus 14-day of adequate antimicrobial therapy for intensive care unit (ICU)-acquired severe infections by MDR-GNB. Adult patients with severe infections by MDR-GNB initiated after 48 h of ICU admission are screened for eligibility. Patients are eligible if they proved to be hemodynamically stable and without fever for at least 48 h on the 7th day of adequate antimicrobial therapy. After consenting, patients are 1:1 randomized to discontinue antimicrobial therapy on the 7th (± 1) day or to continue for a total of 14th (± 1) days.
Planned Outcomes
The primary outcome is treatment failure, defined as death or relapse of infection within 28 days after randomization. Non-inferiority will be achieved if the upper edge of the two-tailed 95% confidence interval of the difference between the clinical failure rate in the 7-day and the 14-day group is not higher than 10%.
Conclusion
The OPTIMISE trial is the first randomized controlled trial specifically designed to assess the duration of antimicrobial therapy in patients with severe infections by MDR-GNB.
Trial Registration
ClinicalTrials.gov, NCT05210387. Registered on 27 January 2022. Seven Versus 14 Days of Antibiotic Therapy for Multidrug-resistant Gram-negative Bacilli Infections (OPTIMISE).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
There is a lack of studies addressing shorter regimes against severe infections by multidrug-resistant Gram-negative bacteria (MDR-GNB). |
The duratiOn of theraPy in severe infecTIons by MultIdrug-reSistant gram-nEgative bacteria (OPTIMISE) trial aims to assess the non-inferiority of 7-day versus 14-day antimicrobial therapy in critically ill patients with severe infections caused by MDR-GNB. |
Patients are eligible if they proved to be hemodynamically stable and without fever for at least 48 h on the 7th day of adequate antimicrobial therapy. |
The primary outcome is treatment failure, defined as death or relapse of infection within 28 days after randomization. |
Introduction
Antimicrobial resistance (AMR) has emerged as one of the leading public health threats of the twenty-first century [1,2,3,4]. This is a particular problem in healthcare-associated infections (HCAI) by Gram-negative bacteria (GNB), which are resistant to first- and last-line beta-lactams generally used to treat these infections [1, 4]. In 2017, the World Health Organization (WHO) published a list of priority multidrug-resistant (MDR) pathogens for research and development of new antimicrobials [1]. Carbapenem-resistant Enterobacterales, Acinetobacter baumannii, and Pseudomonas aeruginosa, along with third-generation cephalosporin-resistant Enterobacterales have been listed as critical priority pathogens [1]. Indeed, infections by these carbapenem-resistant GNB challenge effective antimicrobial therapy and have been associated with increased mortality [5,6,7,8,9].
Although the recent launching of new antimicrobial agents, namely the new beta-lactam/beta-lactamase inhibitor combinations and cefiderocol, have attenuated dreaded therapeutic scenarios associated with AMR, and have been recommended as the first options for treating serious infections caused by these organisms, they are not active against all carbapenem-resistant organisms and the access to these new compounds is still limited in low- and middle-income countries, where HCAI and AMR is an even more severe problem [4, 10,11,12]. Therefore, there is still a long way to go to maximize antimicrobial therapeutic options and improve strategies to better use old and new drugs for HCAI for these difficult-to-treat pathogens.
Aiming to decrease unnecessary antimicrobial exposure, which may contribute to further escalation of AMR, as well to reduce antimicrobial-associated adverse effects, in the last 20 years, there have been several randomized clinical trials evaluating shorter-duration treatment regimes in comparison with more “traditional” time of antibiotic therapies [13,14,15]. With few exceptions, most trials have shown that shorter treatment durations (depending on the infection, 5–8 days) are usually non-inferior to longer, more “conventional” times of treatment (14–21 days) [13,14,15].
Despite the promising results of the trials, there are still some gaps that may impair a broader implementation of shorter-duration treatment strategies in HCAIs, particularly in more severely ill patients with multidrug-resistant Gram-negative bacteria (MDR-GNB) infections. More studies are still needed in critically ill patients, particularly those with sepsis [16]. Furthermore, there is ongoing controversy whether in ventilator-associated pneumonia, a severe infection that commonly affects critically ill patients [17, 18], certain microorganisms, such as P. aeruginosa, may require longer, more “traditional” courses of antimicrobial therapy [19, 20]. Finally, difficult-to-treat MDR-GNB are still underrepresented in most of these studies, impairing a wider implementation of this strategy in clinical practice [21]. Notably, recent guidelines were unable to provide recommendations for the duration of therapy for severe MDR-GNB because of the absence of studies addressing this issue [22, 23].
The combination of severe infections and MDR-GNB may be a case against shorter-duration therapies. First, because severe infections—particularly those associated with sepsis—may be associated with higher bacterial inoculum, they increase target organ damage, which may affect the pharmacokinetics of antimicrobials, and immune dysfunction, which may impair pathogen clearance [16]. Second, infections by MDR-GNB more commonly affect or immunocompromised patients or those with more comorbidities [21]. Finally, although novel antimicrobials may change this landscape [22, 23], several MDR-GNB are still treated with less potent second-line antimicrobials, such as polymyxins, aminoglycosides, and tigecycline [22, 23], for which a longer duration might be necessary.
On the other hand, there are many compelling potential benefits of shortening treatment of MDR-GNB in patients who present a favorable clinical response in the first days of therapy. First, it could avoid unnecessary exposure to novel agents, hampering the emergence of resistance to these new drugs. Second, it could reduce the incidence of adverse effects commonly associated with these second-line agents, notably the high rates of acute kidney injury (AKI) associated with polymyxins and aminoglycosides [24, 25], but also Clostridioides difficile infections, for which there is evidence that even a single day of antibiotic use may increase their incidence [26]. In addition, an overall reduction in selective pressure might potentially decrease the incidence of new infections by other MDR pathogens. Finally, avoiding unnecessary antimicrobials may decrease the length of use of intravascular catheters, potentially reducing catheter-associated bloodstream infections, and it ultimately may lead to lower lengths of hospitalization, resulting in clinical and economic benefits [27].
Therefore, in this open-label, randomized clinical trial, we address the duratiOn of theraPy in severe infecTIons by MultIdrug-reSistant gram-nEgative bacteria (OPTIMISE). Our main objective is to assess the non-inferiority of 7-day antibiotic therapy compared to 14-day therapy in the treatment of intensive care unit (ICU) patients with severe infections caused by MDR-GNB who presented clinical stability on the 7th day of antimicrobial therapy.
Methods
Study Design
This is a randomized, open-label trial, with parallel groups and 1:1 allocation ratio to assess the non-inferiority of 7 versus 14 days of antimicrobial therapy for severe infections by ICU-acquired MDR-GNB in patients who are hemodynamically stable and afebrile on the 7th day of treatment. The study intervention consists of suspending antimicrobial therapy on the 7th day in participants allocated to the intervention group versus maintaining antimicrobial therapy until the 14th day in the control group.
The study protocol and amendments have been approved by the research ethics committee (institutional review board, IRB) of the coordinating center (Hospital Moinhos de Vento), as well as IRBs from all other participant sites (Supplementary Material).
Study Setting
Participants have been recruited at ICUs of Brazilian hospitals participating in the IMPACTO MR platform [28] since 27 January 2022. In December 2022, additional centers, outside the IMPACTO MR platform, were included as participants sites, affording a total of 36 centers in October 2023, in order to increase recruitment rate. The recruitment period is expected to close on 20 December 2023.
Eligibility Criteria
Participants are eligible for the study if they are at least 18 years of age; provide written informed consent; have been admitted to the ICU for at least 48 h at the onset of infection; have a severe infection caused by an MDR-GNB; are hemodynamically stable and afebrile for at least 48 h on day 7 ± 1 of appropriate antibiotic therapy since the onset of infection (defined as the day on which the culture that yielded the growth of the isolate was collected); and the patients’ care team consents to inclusion of participant in the trial. The European Committee for Antimicrobial Susceptibility Testing (EUCAST) [29] criteria were used for interpreting antimicrobial susceptibility tests, except for ampicillin-sulbactam and A. baumannii, when Clinical Laboratory Standard Institute (CLSI) [30] breakpoint was used. Definitions of infection and infection sites were adapted from the criteria of the Brazilian Health Regulatory Agency [31] (Supplementary Material). A full description of eligibility criteria definitions is found in Table 1.
They are excluded if one or more of the following conditions are present: (i) Participation in other experimental trials involving antimicrobial therapy; (ii) Primary site of infection that requires longer therapy (such as endocarditis, necrotizing fasciitis, osteomyelitis, abdominal abscess, central nervous system infections, empyema, periprosthetic infections; see full description in the Supplementary Material; any other infection sites are considered eligible); (iii) Immunosuppression (see definitions in the Supplementary Material); (iv) Growth of the same bacteria under study in blood culture samples collected in the 48 h prior to randomization (if cultures requested by the care team); (v) Concomitant uncontrolled infection by another GNB (regardless of susceptibility profile); (vi) Prior participation in this trial; (vii) Known pregnancy; (viii) Patient on palliative care only for whom initiation of antimicrobials, if necessary, or hemodynamic support measures (e.g., initiation or uptitration of vasopressors) has already been decided against.
Intervention
The study intervention is the discontinuation of antibiotic therapy for the infection that prompted the participant’s enrollment in the trial. In the intervention group, antimicrobials prescribed for the MDR-GNB infection should be discontinued on day 7 of therapy (a variation of ± 1 day is acceptable for per protocol analysis). The control group consists of patients whose antimicrobial therapy prescribed for the MDR-GNB infection should be continued until day 14 (± 1 day) of therapy.
If the participant is discharged before day 28, the coordinating center will contact the participant by telephone. This evaluation can be carried out with a 7-day window (i.e., up to day 35 of follow-up). The calls will be made by investigators from the coordinating center and will be recorded.
After randomization, patients are discontinued only if consent is withdrawn. Adherence to the proposed intervention is assessed through the patient’s medical prescription. There are no other care or therapeutic interventions prohibited by this protocol. If the patient develops new signs and symptoms of active bacterial infection after randomization and (according to group allocation) discontinuation of therapy, regardless of whether this is new infection or a relapse of the infection that prompted enrollment in the trial, there is no restriction whatsoever on resumption or initiation of further antimicrobial therapy at the discretion of the care team. The protocol does not plan to discontinue patients because of the adverse effects of antimicrobial therapy, especially in the 14-day group, since this is the time considered standard for treatment. However, decisions regarding maintenance or interruption are made by the medical assistance team and all these participants will be subject to intention-to-treat analysis.
Outcomes
The primary outcome is treatment failure within 28 days of randomization, defined as death or reinfection with the same bacteria at any site. Reinfection is defined as growth of the same pathogen with the same susceptibility profile to the antimicrobials of interest (i.e., the same GNB species with the same antimicrobial resistance profile of interest), at any site of infection, in addition to meeting the diagnostic criteria of the Brazilian Health Regulatory Agency (ANVISA) [31] (see definitions in the Supplementary Material).
Secondary outcomes, which are also assessed within 28 days of participant randomization, are the following: (a) days alive and free from hospitalization; (b) days alive and free of antimicrobial therapy; (c) incidence of infections with other MDR-GNB and other bacteria; (d) length of ICU stay (assessed in survivors at 28 days); (e) acute kidney injury [32]; (f) cumulative incidence of all-cause diarrhea; (g) cumulative incidence of confirmed C. difficile infection; (h) cumulative incidence of other antimicrobial-related adverse events (hepatotoxicity; ALT > 250 U/L, AST > 200 U/L, and/or total bilirubin > 1.5 mg/dL), neutropenia (neutrophils < 1000 cells/mm3), and thrombocytopenia (platelets < 100,000 cells/mm3); and (i) cumulative incidence of hemodynamic instability lasting > 6 h (within 14 days of randomization).
The component of primary outcome, relapse of the infection, will be adjudicated by two independent infectious diseases physicians, who will be blinded to the intervention. They will receive the specific medical records and laboratory and radiological examination results which have been used to fulfill the criteria for infection. If the physicians’ adjudications do not agree, a third infectious diseases specialist will review the case.
Participant Timeline
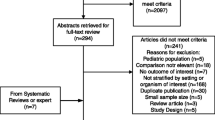
Screening, evaluation for eligibility and follow-up is detailed in Fig. 1. Each participant will be voluntarily invited to participate in the study and must provide their consent by signing an informed consent form (ICF)—see the ICF in the Supplementary Material. If the participant is unable to provide consent, the invitation will be made to their legal guardian or proxy. The consent can be obtained between the 5th and 8th day of antimicrobial treatment once they are identified as eligible for the study.
Assignment of Interventions
The randomized patient allocation sequence was created using the R studio program [33] by a statistician, respecting an individual randomization in blocks of 2 and 4, in a 1:1 ratio and stratified by sites and by risk for mortality due to infection (high versus low risk). For the purposes of this study, urinary tract infections and central line-associated bloodstream infections are defined as low risk. All other infections are considered high risk. Randomization is performed by the investigator of each participating hospital through the REDCap data collection platform ensuring concealment of the randomization list.
This is an open-label randomized clinical trial and, as such, investigators and patients are not blinded to group allocation. However, outcomes will be assessed by a blinded evaluation committee.
Data Collection
The information will be recorded on electronic Case Report Forms (eCRFs) using REDCap. After randomization, information will be evaluated daily regarding development of hemodynamic instability, clinical variables (antimicrobials administered, diarrhea, urinary output), adverse events related to antimicrobial therapy, and laboratory variables (new cultures, creatinine) (Table S1 in the Supplementary Material).
All staff members involved in data collection will receive training in utilizing the REDCap tool, as well as training in Good Clinical Practice guidelines. Quality assessment and consent forms and eCRFs will be checked by the coordinator center monitors.
Data Management
Several procedures have been adopted to ensure data quality and protocol standardization. These procedures include (i) Online training with all investigators; (ii) A detailed investigator brochure describing each step of the protocol; (iii) Contacting participating centers to review the protocol and offer new training sessions; (iv) Real-time data assessment by a team of investigators from the coordinating center; and (v) Monthly reports on patient screening, recruitment, and randomization.
No patient data will be disclosed to the study or data management teams. In the eCRFs, patients and sites are identified by numbers. Data from printed medical records are kept confidential (stored in locked files) by all participating sites. The identity of all patients will be anonymized in all interim and final reports.
Considering the profile of patients who will be included in the research and the 28-day follow-up period, it is unlikely that these participants will be lost to follow-up. However, participants who are discharged and with whom the research team is unable to make contact will be considered as “missing”.
Sample Size
The sample size was calculated considering a clinical failure of 30% in both groups, a randomization ratio of 1:1, a non-inferiority margin of 10%, an alpha of 0.05, and a beta of 0.20. A total of 520 participants will be needed. The sample size will be monitored throughout the study, through interim analyses, for adjustment if necessary.
Data Analysis
All statistical analyses will be performed in R. A non-inferiority analysis of the 7-day course of treatment compared to the conventional 14-day course of treatment will be performed. The primary analysis will be conducted by intention to treat. Secondarily, a per protocol analysis will also be performed. Non-inferiority will be achieved if the upper edge of the two-tailed 95% confidence interval (CI) of the difference between the failure rate in the intervention group and the control group is not higher than 10%.
A superiority analysis will also be performed for the secondary outcomes, as the shorter duration of antimicrobial therapy is expected to yield a lower incidence of toxicity, reduce length of hospital stay and use of antimicrobials, and reduce the incidence of superinfections, such as C. difficile-associated diarrhea. For this purpose, chi-square or Fisher’s exact test will be used for categorical outcomes and Student’s t test for independent samples or nonparametric tests for continuous outcomes, depending on the nature of the variable (see full description of statistical analysis for secondary outcomes in the Supplementary Material). All tests will be two-tailed and a p ≤ 0.05 will be considered statistically significant.
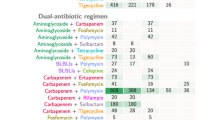
Six subgroups analysis are defined for the primary outcome, considering the variables infecting bacteria (Enterobacterales, A. baumannii, or P. aeruginosa); susceptibility profile (resistant vs. susceptible to carbapenems); criteria defining infection severity (SOFA score ≥ 2 [sepsis or septic shock] [34], bloodstream infection, or pneumonia); empirical therapy (appropriate vs. initially inappropriate); antimicrobial therapy (monotherapy vs. combination therapy); risk of infection (low risk vs. high risk).
Missing Data
We anticipate minimal missing values for outcomes, given that the study procedures involve both training of site research staff and independent remote data monitoring by the study coordinator. Nevertheless, the coordinating center will contact site investigators to retrieve any missing data values. Analyses for primary and secondary outcomes will be based on participants for whom outcome data are available, i.e., available case analysis.
Statistical Interim Analysis and Stopping Guidance
A statistical interim analysis is planned when 25% (130 participants), 50% (260 participants), and 75% (390 participants) are recruited. In these analyses, the safety of the study participants will be evaluated on the basis of data related to the primary outcome “clinical failure”, the components of the main outcome separately (death and relapse of infection), and the secondary outcome “new hemodynamic instability in the first 14 days of study follow-up”. We defined as a stopping rule a statistical significance with p < 0.001 (Peto’s rule) in any of these analyses. The interim analysis will be carried out by an external committee (data monitoring and safety board, DMSB) composed of three independent members (one infectious diseases specialist, one statistician, and one specialist in clinical research bioethics) and it will provide guidance on how to proceed with the study, and may guide the interruption of the study if the level of significance described above is found in the analyzed variables, or if the committee decides that the study should be interrupted for other reasons, such as the high rate of serious adverse events.
The Brazilian Ministry of Health will be notified of the DMSB decision and, if any change is identified as necessary, such as a change in the sample size or interruption of the study, it will be involved in these discussions. In addition, at each interim analysis, the sample size will be reassessed for possible readjustment if the overall event rates are different from those initially estimated. As this is a non-inferiority study, there is no provision for early stoppage due to superiority of the treatment of interest, and no theoretical rationale to support this hypothesis.
Adverse Events
Severe adverse events (SAE) must be reported to the coordinating center within 24 h of becoming aware of the event. The principal investigator at each participating center will be responsible for informing the Research Ethics Committees of any SAE, as required by local regulations.
This study will not test any experimental medication or treatment other than the standard of care already implemented by the participating hospitals. The sole intervention of the study concerns the duration of antibiotic therapy. Therefore, the expected risk is recurrence of infection, which could lead to sepsis or death. However, as previously described, the medical team is free to resume or initiate treatment in case of recurrence or new infection.
Protocol Amendments
The second to fourth versions of the protocol amendments were done before the initiation of the study. The major amendments to the protocol are presented in Table S2 in the Supplementary Material.
Strengths and Limitations
Recommendations of antimicrobial therapy duration for severe HCAIs have been mostly based on expert opinion rather than on solid evidenced-based data. There have been few completed studies addressing the effectiveness of shorter durations in severe HCAIs, all of them in ventilator-associated pneumonia [35,36,37]. In two, there was no MDG-GNB included [35, 36], while in the other there was no description of the susceptibility profile [37]. There were also two randomized clinical trials comparing duration of therapy for GNB bloodstream infections [38, 39]. However, one included both community-acquired and HCAIs, excluded non-fermentative-GNB, and did not report the number of MDR isolates [39]; while in the other study, less than 20% were considered MDR-GNB [38], using a less restrictive WHO definition when defining critical priority pathogens [1, 38]. Therefore, none of the currently published trials has been designed to assess MDR-GNB infections, which have limited therapeutic options, often with less reliable agents [1]. OPTIMISE is the first randomized clinical trial specifically designed to evaluate the non-inferiority of shorter durations in two scarcely investigated conditions, i.e., severe infections caused by WHO critical priority MDR-GNB.
Unlike most previous studies addressing 7–8 versus 14–15 days of therapy, in which randomization happens soon after the infection diagnosis, before any clinical indication of improvement, and ultimately is interrupted at day 7–8 regardless of the patient’s clinical status, in the OPTIMISE trial, eligible patients are those with severe infections, who have been treated with appropriate antimicrobials for at least 7 ± 1 days and present clinical signs of improvement for at least 48 h. In addition, to protect patients from a potential early interruption when the clinical condition might indicate a poor response in the first 7 days of treatment, we believe it better represents clinical practice, in which clinicians consider stopping antimicrobial therapy after some consistent evidence that the patients have improved their clinical condition and additional therapy may not be necessary. Finally, in previous trials, the events accounting for the outcomes may occur before day 7 of therapy, i.e., when groups have not yet become differentiated in relation to the intervention. The design of OPTIMISE is similar to that used in the trial by Yahav et al. [38], addressing duration of therapy for GNB bloodstream infection.
Another strength of this trial is that randomization has been stratified for important factors that might affect the outcome. The stratification by site diminishes the effect that local protocols and other differences in patients’ care provided at each hospital may have on the outcomes of interest. We also stratified by risk of infection (high vs. low risk) so that infections of lower severity, potentially associated with lower bacterial inoculum and/or ease control with device removal, would be homogeneously distributed between the two groups.
The major limitation of this trial is its open design. As previously commented [20], the treating physician could tend to seek a new infection diagnosis in patients without antimicrobial therapy, in this case in the 7-day therapy group. Since relapse of the infection is part of the composite outcome, it could imply more clinical failures in the 7-day group, simply because of asymmetric (longer) time exposure to develop relapse compared to the 14-day group. To mitigate this issue, two independent and blinded infectious diseases physicians are adjudicating any reported relapses of infection.
Another limitation of the study is the definition of adequate antimicrobial treatment since this concept only takes into account in vitro susceptibility to the antimicrobial and does not consider the class of the antimicrobial. For example, polymyxins and aminoglycosides are no longer recommended therapy for carbapenem-resistant Enterobacterales [22, 23], but they are still used in some resource-limited centers. Currently, neither has a breakpoint that could be recommended for monotherapy [29, 40]; nonetheless, assuming that the patient infected by a MDR-GNB with a susceptible result for any of these antimicrobials received any of them in monotherapy and presents the eligibility criteria of clinical stability, it is considered as adequate. It does not mean that the investigators recommend any of these agents in monotherapy for severe infections, but since it has been demonstrated that it might have acted positively in a given case, it is assumed that it was appropriate. No antimicrobial with in vitro results showing resistance may be considered as adequate. In addition, doses are also not considered in the evaluation of appropriateness of therapy, with the exception of tigecycline, where an adapted breakpoint considering the minimal inhibitory concentration and dose was considered in this evaluation, based on data from previous studies [41,42,43,44].
Ethics
This study has been conducted in accordance with the Brazilian and international regulations set forth in the following documents: Declaration of Helsinki; Brazilian National Health Council Resolution CNS 466/2012 and related Brazilian Ministry of Health publications; and1996 ICH Harmonized Tripartite Guideline for Good Clinical Practice.
The study protocol and amendments have been approved by the research ethics committee (IRB) of the coordinating center (Hospital Moinhos de Vento), as well as IRBs from all other participant sites.
Each patient or legal representative is asked to sign an ICF consenting to participate in the study. The ICF (see Supplementary Material) can be administered between day 5 and day 8 of antimicrobial treatment.
Dissemination Plans
The principal investigator and co-investigators that fulfill the authorship criteria (see Supplementary Material) will prepare a manuscript that will be submitted for publication in an international peer-reviewed journal that is made available free of charge, so that the information can be accessible to all interested parties in the matter, such as health professionals located in the centers where the study is being carried out. The results will also be made available to the Ministry of Health of Brazil and disseminated in international scientific conferences and events in the area.
Conclusions
The OPTIMISE trial is the first randomized clinical trial specifically designed to assess the optimal duration of antimicrobial therapy in patients with severe infections by MDR-GNB. We expect to demonstrate that 7-day therapy is not inferior to 14-day therapy, in patients who present signs of clinical stability on the seventh day of appropriate antimicrobial therapy, and might be superior in reducing length of ICU, decreasing the use of antimicrobials and the incidence of adverse events.
Data Availability
The anonymous stored data will be available on reasonable request after all analyzes are done.
References
Tacconelli E, Carrara E, Savoldi A, et al. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis. 2018;18(3):318–27.
Review on antimicrobial resistance. Tackling drug-resistant infections globally: final report and recommendations (2016). https://amr-review.org/sites/default/files/160518_Final%20paper_with%20cover.pdf. Accessed 9 Sept 2023.
WHO. Antimicrobial resistance. https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance. Accessed 29 Sep 2023.
Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399(10325):629–55.
Stewardson AJ, Marimuthu K, Sengupta S, et al. Effect of carbapenem resistance on outcomes of bloodstream infection caused by Enterobacteriaceae in low-income and middle-income countries (PANORAMA): a multinational prospective cohort study. Lancet Infect Dis. 2019;19(6):601–10.
Falcone M, Tiseo G, Carbonara S, et al. Mortality attributable to bloodstream infections caused by different carbapenem-resistant Gram-negative bacilli: results from a nationwide study in Italy (ALARICO Network). Clin Infect Dis. 2023;76(12):2059–69.
Reyes J, Komarow L, Chen L, et al. Global epidemiology and clinical outcomes of carbapenem-resistant Pseudomonas aeruginosa and associated carbapenemases (POP): a prospective cohort study. Lancet Microbe. 2023;4(3):e159–70.
Wang M, Ge L, Chen L, et al. Clinical outcomes and bacterial characteristics of carbapenem-resistant Acinetobacter baumannii among patients from different global regions. Clin Infect Dis. 2023. https://doi.org/10.1093/cid/ciad556.
Wang M, Earley M, Chen L, et al. Clinical outcomes and bacterial characteristics of carbapenem-resistant Klebsiella pneumoniae complex among patients from different global regions (CRACKLE-2): a prospective, multicentre, cohort study. Lancet Infect Dis. 2022;22(3):401–12.
Allegranzi B, Bagheri Nejad S, Combescure C, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet. 2011;377(9761):228–41.
Allel K, Stone J, Undurraga EA, et al. The impact of inpatient bloodstream infections caused by antibiotic-resistant bacteria in low- and middle-income countries: a systematic review and meta-analysis. PLoS Med. 2023;20(6):e1004199.
Aiken AM, Rehman AM, de Kraker MEA, et al. Mortality associated with third-generation cephalosporin resistance in Enterobacterales bloodstream infections at eight sub-Saharan African hospitals (MBIRA): a prospective cohort study. Lancet Infect Dis. 2023. https://doi.org/10.1016/S1473-3099(23)00233-5.
Lee RA, Stripling JT, Spellberg B, Centor RM. Short-course antibiotics for common infections: what do we know and where do we go from here? Clin Microbiol Infect. 2023;29(2):150–9.
Spellberg B, Rice LB. The shorter is better movement: past, present, future. Clin Microbiol Infect. 2023;29(2):141–2.
Wald-Dickler N, Spellberg B. Short-course antibiotic therapy-replacing Constantine units with “shorter is better.” Clin Infect Dis. 2019;69(9):1476–9.
Yek C, Lawandi A, Evans SR, Kadri SS. Which trial do we need? Optimal antibiotic duration for patients with sepsis. Clin Microbiol Infect. 2023;29(10):1232–6.
Zaragoza R, Vidal-Cortés P, Aguilar G, et al. Update of the treatment of nosocomial pneumonia in the ICU. Crit Care. 2020;24(1):383.
Papazian L, Klompas M, Luyt CE. Ventilator-associated pneumonia in adults: a narrative review. Intensive Care Med. 2020;46(5):888–906.
Albin OR, Kaye KS, McCreary EK, Pogue JM. Less is more? Antibiotic treatment duration in Pseudomonas aeruginosa ventilator-associated pneumonia. Clin Infect Dis. 2023;76(4):745–9.
Metersky ML, Klompas M, Kalil AC. Less is more: a 7-day course of antibiotics is the evidence-based treatment for Pseudomonas aeruginosa ventilator-associated pneumonia. Clin Infect Dis. 2023;76(4):750–2.
Haddad SF, Allaw F, Kanj SS. Duration of antibiotic therapy in Gram-negative infections with a particular focus on multidrug-resistant pathogens. Curr Opin Infect Dis. 2022;35(6):614–20.
Paul M, Carrara E, Retamar P, et al. European Society of Clinical Microbiology and Infectious Diseases (ESCMID) guidelines for the treatment of infections caused by multidrug-resistant Gram-negative bacilli (endorsed by European Society of Intensive Care Medicine). Clin Microbiol Infect. 2022;28(4):521–47.
Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ. Infectious Diseases Society of America 2023 guidance on the treatment of antimicrobial resistant gram-negative infections. Clin Infect Dis. 2023. https://doi.org/10.1093/cid/ciad428.
Wagenlehner F, Lucenteforte E, Pea F, et al. Systematic review on estimated rates of nephrotoxicity and neurotoxicity in patients treated with polymyxins. Clin Microbiol Infect. 2021. https://doi.org/10.1016/j.cmi.2020.12.009.
Marcus R, Paul M, Elphick H, Leibovici L. Clinical implications of β-lactam-aminoglycoside synergism: systematic review of randomised trials. Int J Antimicrob Agents. 2011;37(6):491–503.
Branch-Elliman W, O’Brien W, Strymish J, Itani K, Wyatt C, Gupta K. Association of duration and type of surgical prophylaxis with antimicrobial-associated adverse events. JAMA Surg. 2019;154(7):590–8.
Bauer KA, Kullar R, Gilchrist M, File TM Jr. Antibiotics and adverse events: the role of antimicrobial stewardship programs in “doing no harm.” Curr Opin Infect Dis. 2019;32(6):553–8.
Tomazini BM, Nassar AP Jr, Lisboa TC, et al. IMPACTO-MR: a Brazilian nationwide platform study to assess infections and multidrug resistance in intensive care units. Rev Bras Ter Intensiva. 2022;34(4):418–25.
ESCMID-European Society of Clinical Microbiology, Diseases I. eucast: EUCAST. https://www.eucast.org/. Accessed 18 Oct 2023.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. 30th ed. CLSI supplement M100. Wayne: Clinical and Laboratory Standards Institute; 2020.
Caderno 2—Critérios Diagnósticos de Infecção Relacionada à Assistência à Saúde.pdf. https://www.gov.br/anvisa. Accessed 13 Oct 2023.
Fujii T, Uchino S, Takinami M, Bellomo R. Validation of the Kidney Disease Improving Global Outcomes criteria for AKI and comparison of three criteria in hospitalized patients. Clin J Am Soc Nephrol. 2014;9(5):848–54.
The R Project for Statistical Computing. https://www.R-project.org/. Accessed 13 Oct 2023.
Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–10.
Chastre J, Wolff M, Fagon JY, et al. Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: a randomized trial. JAMA. 2003;290(19):2588–98.
Capellier G, Mockly H, Charpentier C, et al. Early-onset ventilator-associated pneumonia in adults randomized clinical trial: comparison of 8 versus 15 days of antibiotic treatment. PLoS One. 2012;7(8):e41290.
Bouglé A, Tuffet S, Federici L, et al. Comparison of 8 versus 15 days of antibiotic therapy for Pseudomonas aeruginosa ventilator-associated pneumonia in adults: a randomized, controlled, open-label trial. Intensive Care Med. 2022;48(7):841–9.
Yahav D, Franceschini E, Koppel F, et al. Seven versus 14 days of antibiotic therapy for uncomplicated Gram-negative bacteremia: a noninferiority randomized controlled trial. Clin Infect Dis. 2019;69(7):1091–8.
von Dach E, Albrich WC, Brunel AS, et al. Effect of C-reactive protein-guided antibiotic treatment duration, 7-day treatment, or 14-day treatment on 30-day clinical failure rate in patients with uncomplicated Gram-negative bacteremia: a randomized clinical trial. JAMA. 2020;323(21):2160–9.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. 33rd ed. CLSI supplement M100. Wayne: Clinical and Laboratory Standards Institute; 2023.
Kispal B, Walker SAN. Monte Carlo simulation evaluation of tigecycline dosing for bacteria with raised minimum inhibitory concentrations in non-critically ill adults. Eur J Clin Pharmacol. 2021;77(2):197–205.
Bhavnani SM, Rubino CM, Hammel JP, et al. Pharmacological and patient-specific response determinants in patients with hospital-acquired pneumonia treated with tigecycline. Antimicrob Agents Chemother. 2012;56(2):1065–72.
Qin X, Kong L, Wu C, Zhang X, Xie M, Wu X. Pharmacokinetic/pharmacodynamic analysis of high-dose tigecycline, by Monte Carlo simulation, in plasma and sputum of patients with hospital-acquired pneumonia. J Clin Pharm Ther. 2022;47(12):2312–9.
De Pascale G, Lisi L, Ciotti GMP, et al. Pharmacokinetics of high-dose tigecycline in critically ill patients with severe infections. Ann Intensive Care. 2020;10(1):94.
Medical Writing Assistance
An English review has been performed by the Scientific Linguagem company and was funded by the authors.
Funding
This work and the journal’s Rapid Service fee are funded by the Ministry of Health (MH) of Brazil through the Support Program for Institutional Development of the Unified Health System (PROADI-SUS). MH members have reviewed and provided suggestions to the first version of the protocol and reviewed and approved all protocol modifications. The funding source is not involved in collection, analysis, and interpretation of data, nor in writing the manuscript.
Author information
Authors and Affiliations
Contributions
Beatriz Arns and Alexandre P. Zavascki conceived of the study; Beatriz Arns, Guilhermo Prates Sesin and Alexandre P. Zavascki wrote the first draft of the first manuscript; Beatriz Arns, Jaqueline Driemeyer C. Horvath, Guilhermo Prates Sesin, Crepin Aziz Jose Oluwafoumi Agani, Tiago Marcon dos Santos, Liliane Spencer Bittencourt Brochier, Alexandre Biasi Cavalcanti, Bruno Martins Tomazini, Adriano Jose Pereira, Viviane Cordeiro Veiga, Giovana Marssola Nascimento, Andre C. Kalil and Alexandre P. Zavascki made significant contributions to the final study design; Gabriela Soares Rech and Bruna Silveira da Rosa provided statistical help; Alexandre Biasi Cavalcanti, Bruno Martins Tomazini, Adriano Jose Pereira, Viviane Cordeiro Veiga, Giovana Marssola Nascimento, and Andre C. Kalil provided critical review of the manuscript for important intellectual content. All authors contributed and agreed with the content and conclusions of this manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
All authors confirm that they have no conflicts of interest to declare. Alexandre P. Zavascki is a research fellow of the National Council for Scientific and Technological Development (CNPq), Ministry of Science and Technology, Brazil.
Ethical Approval
This study has been conducted in accordance with the Brazilian and international regulations set forth in the following documents: Declaration of Helsinki; Brazilian National Health Council Resolution CNS 466/2012 and related Brazilian Ministry of Health publications; and 1996 ICH Harmonized Tripartite Guideline for Good Clinical Practice. The study protocol and amendments have been approved by the research ethics committee (IRB) of the coordinating center (Hospital Moinhos de Vento), as well as IRBs from all other participant sites.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Arns, B., Horvath, J.D.C., Rech, G.S. et al. A Randomized, Open-Label, Non-inferiority Clinical Trial Assessing 7 Versus 14 Days of Antimicrobial Therapy for Severe Multidrug-Resistant Gram-Negative Bacterial Infections: The OPTIMISE Trial Protocol. Infect Dis Ther 13, 237–250 (2024). https://doi.org/10.1007/s40121-023-00897-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-023-00897-9