Abstract
Around 91% of migraine patients use over-the-counter medicines to treat attacks, often without further treatment or medical consultation. This therapeutic principle is established in most countries, regardless of how the healthcare system is otherwise structured or financed. Using Germany as an example, the basis for an expansion of attack therapy with rizatriptan as an over-the-counter triptan is described. To achieve the best possible tolerability and safety in the context of self-medication, the lowest possible dose should be selected to provide the most favourable tolerability and safety profile in the context of self-medication through low dosages. The lowest approved dose of rizatriptan is 5 mg. This was investigated in three randomized controlled trials with 752 patients. The results show that rizatriptan at a dose of 5 mg is more effective than the triptans naratriptan 2.5 mg, almotriptan 12.5 mg and sumatriptan 50 mg, which were previously available for self-medication in Germany. There was no significant difference in the frequency of adverse events with rizatriptan 5 mg compared to placebo. Rizatriptan 5 mg does not have a higher side effect potential than sumatriptan 50 mg, which is already exempt from the prescription requirement. The reasons given show that rizatriptan in a dose of 5 mg for the treatment of acute migraine attacks fulfils the requirements for a transfer from prescription to pharmacy-only status at least as well as sumatriptan 50 mg, naratriptan 2.5 mg and almotriptan 12.5 mg. From a clinical care perspective, it is desirable for affected patients to have other options available for self-medication. Non-responders to other substances also have a further treatment option with rizatriptan 5 mg, with the same or even better risk–benefit profile, to treat migraine attacks safely, effectively and in a tolerable manner as part of self-medication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Around 91% of migraine patients use over-the-counter medicines to treat attacks, often without further treatment or medical consultation. Using Germany as an example, the basis for an expansion of attack therapy with rizatriptan as an over-the-counter triptan is described. |
To achieve the best possible tolerability and safety in the context of self-medication, the lowest possible dose should be selected. The lowest approved dose of rizatriptan is 5 mg. This was investigated in three randomized controlled trials. |
The results show that rizatriptan at a dose of 5 mg is more effective than the triptans naratriptan 2.5 mg, almotriptan 12.5 mg and sumatriptan 50 mg, which were previously available for self-medication in Germany. |
There was no significant difference in the frequency of adverse events with rizatriptan 5 mg compared to placebo. Rizatriptan 5 mg does not have a higher side effect potential than sumatriptan 50 mg, which is already exempt from prescription. |
With rizatriptan 5 mg, non-responders to other substances have a further treatment option with the same or even better risk–benefit profile for the tolerable, safe and effective treatment of migraine attacks as part of self-medication. |
Over-the-Counter Triptans in Migraine Therapy
Headache disorders can vary greatly in severity [10, 12, 15, 25, 26, 30]. A causal treatment for primary forms of headache is not currently possible, but various symptomatic therapies are available [10, 25, 31]. These include the preventive and acute treatment of headache attacks. Seven different triptans are currently available as the drugs of choice for the acute treatment of migraine. Non-steroidal anti-inflammatory drugs (NSAIDs) including acetylsalicylic acid and other non-opioid analgesics are used in the acute treatment of both migraine and tension-type headaches [10].
Self-medication of headaches is the most common form of acute treatment [8, 10, 25]. Around 91% of migraine patients and 90% of patients with tension-type headaches use painkillers as self-medication, often without further treatment or medical consultation [8]. As a widespread disease with serious direct and indirect costs, headaches are highly relevant not only for the individual sufferer but also for society and the health insurance providers. Self-medication of migraine and headaches is established worldwide and there is a high level of satisfaction with treatment using non-prescription drugs [10, 11, 14, 24, 25].
The population's access to over-the-counter medicines in the context of self-medication is generally described as an important component of the healthcare system, as it enables patients to treat known episodic complaints or minor illnesses themselves without having to consult a doctor for a prescription. This therapeutic principle is established in most countries, regardless of how the healthcare system is otherwise structured or financed. The basis for an expansion of attack therapy with rizatriptan as an over-the-counter triptan is described below using Germany as an example. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Triptans Currently Available for Self-Medication
According to the current S1 guideline “Treatment of migraine attacks and prophylaxis of migraine” [5], triptans are the substances with the best efficacy in acute migraine attacks. They should be used for migraine attacks that do not respond to analgesics or NSAIDs. Seven different triptans are currently available: almotriptan, eletriptan, frovatriptan, naratriptan, rizatriptan, sumatriptan and zolmitriptan.
-
Naratriptan was exempted from the prescription requirement in Germany in 2006.
-
Almotriptan was exempted from the prescription requirement in Germany in 2011.
-
Sumatriptan 50 mg was exempted from the prescription requirement in Germany in 2020.
-
Rizatriptan 5 mg was exempted from the prescription requirement in Germany in 2024.
According to Annex 1 of the German Drug Prescription Ordinance (AMVV), the following rules apply to the self-medication of these four triptans in Germany:
“Subject to prescription, unless otherwise regulated in individual cases (…).
- Almotriptan::
-
Except for the acute treatment of the headache phase of migraine attacks with and without aura, after initial diagnosis of migraine by a physician, in solid preparations for oral use in concentrations of 12.5 mg in separated form and in a total quantity of 25 mg per pack.
- Naratriptan ::
-
Except for the acute treatment of the headache phase of migraine attacks with and without aura, after initial diagnosis of migraine by a physician, in solid preparations for oral use in concentrations of 2.5 mg in separated form and in a total quantity of 5 mg per pack.
- Sumatriptan::
-
Except for the acute treatment of the headache phase of migraine attacks with and without aura, after initial diagnosis of migraine by a physician, in solid preparations for oral use in concentrations of 50 mg in divided form and in a total quantity of 100 mg per pack.
- Rizatriptan::
-
Except for the acute treatment of the headache phase of migraine attacks with and without aura, after initial diagnosis of migraine by a physician, in solid preparations for oral use in concentrations of 5 mg in divided form and in a total quantity of 10 mg per pack.”
Migraine patients respond differently to triptans. If a triptan is not effective and/or not tolerated, a switch to another triptan may result in efficacy and/or better tolerability [5, 10, 13]. Therefore, from a clinical point of view for the appropriate care of patients, it is important that, if possible, different active substances are made available as an option. A possible choice between different triptans, also in self-medication, can thus enable improved care from the point of view of those affected and the healthcare system.
The triptans differ in terms of dosage options, efficacy and tolerability. This is due to different pharmacokinetic properties such as bioavailability, speed of onset and elimination time. If a triptan is not effective, rotation to another triptan can still achieve a clinical effect after a required waiting period.
The reliability of treatment is also variable. Even if a patient usually responds to a triptan, this is only reliably the case in up to 70% of attacks in the treatment of various migraine attacks [7]. The reliability of treatment is also variable. Even if a patient usually responds to a triptan, this is only reliably the case in up to 70% of attacks in the treatment of various migraine attacks [7]. On the other hand, there are also some migraine patients who, as non-responders, show no effect at all on the available triptans.
Triptans are selective agonists at 5HT1B/1D-Receptors. The biological receptor variability of the serotonin receptors as well as the different timing of triptan intake and the different pharmacokinetics may be responsible for the intra- and inter-individual response.
Epidemiology and Healthcare Landscape
Headaches are diagnosed according to the classification of the International Headache Society ICHD-3 [18, 23]. Tension-type headache and migraine worldwide are the second and third most common disorders of mankind, behind dental caries [21]. The 1-year prevalence in Europe for all forms of headache is 86% in women and 71.1% in men, for all forms of migraine 43.6% in women and 26.9% in men, for all forms of tension-type headache 35.7% in women and 40.7% in men, and for medication-overuse headache 4.3% in women and 1.8% in men [17]. Chronic headaches with more than 15 headache days per month are found in 9.5% of women and 4.9% of men [17].
Migraine is the most significant cause of disability in people under 50 [9, 29]. Headache disorders account for more than 75% of all years with disability due to neurological diseases, including stroke, dementia, Parkinson's disease, multiple sclerosis, epilepsy and others [9]. Migraine, one of the 367 headache disorders known today, is the second most common cause of years of disability in the population [9]. In Germany alone, around 900,000 people are affected by migraine attacks every day. Every day, 100,000 people are unable to work and are bedridden due to migraine attacks. On average, three million Germans take a headache tablet every day via self-medication, and 58,853 single doses of triptans are taken every day in Germany to treat migraine attacks [10]. Headaches are one of the most common reasons for short-term incapacity to work. The days lost per year in Germany due to migraines alone are equivalent to the annual working time of 185,000 full-time employees, at an estimated cost of 3.5 billion euros [6]. Added to this is the loss of productivity from unpaid work in the household, raising children or caring for relatives. The risk of depression, anxiety disorder and suicide is 3–7 times higher in migraine patients [32], the risk of cardiovascular disease, heart attack and stroke is 1.5–2 times higher than in healthy people. Heart attacks and strokes are 1.5–2 times more likely than in healthy people [19]. The total annual cost of headaches for 18–65 year olds in Europe is 173 billion euros [22]. Less than 20% of those affected in Europe receive medical care from a physician and less than 10% receive guideline-based prevention or acute treatment [20].
Efficacy and Safety of Rizatriptan
From a clinical perspective, the variability in the severity of migraine and the available treatment options mean that there is a need for prescription medication, but also scope for self-medication. The International Headache Classification now distinguishes 48 subtypes of migraine, which differ both qualitatively in terms of their symptoms and quantitatively in terms of their severity, frequency and symptom intensity.
Migraine attacks can occur at high frequencies. In chronic migraine, for example, headaches occur on at least 15 days a month. High-frequency attacks such as those in chronic migraine, attacks with very severe intensities of nausea, vomiting, bedriddenness and long bouts of pain through to status migraenosus require a very individualized therapeutic approach.
Complex focal neurological symptoms in the context of migraine attacks, such as migraine with brain stem aura, familial hemiplegic migraine or even migrainous infarction and epileptic seizures triggered by migraine attacks, require detailed medical diagnosis, consultation and monitoring of the course and success of the disease over time.
The monitoring of possible therapy complications, such as medication overuse headache with a frequency of intake of acute medication on 10 or more days per month, also requires accompanying medical monitoring as well as therapy adjustment in complex situations.
On the other hand, there are also courses in which the attacks only occur with low frequency, are mild and of short duration. There may be no complex or multiple neurological symptoms in the context of migraine attacks. A consistent attack phenomenology exists over years or even decades, a medical diagnosis has been made and there is a competent individual approach to acute medication for those affected. In addition, prophylactic medication is not usually necessary in such cases. In these patients, self-medication can contribute to a significant improvement in care. Direct access to acute medication in the context of self-medication can enable effective attack control.
For the latter group, self-medication of migraine is tried and tested in healthcare. For these patients, it is therefore important that the widest possible range of treatment options are available to enable a greater choice in the provision of care. For this reason, the aim should be to ensure that the established substances are available for self-medication in terms of their efficacy and, in particular, their tolerability and safety. As self-medication is aimed at easily treatable mild migraine cases, self-medication should be made available in the lower dosage range. The focus should be on a therapy that is as tolerable and safe as possible.
The same approach was taken in the previous procedures for exempting naratriptan 2.5 mg, almotriptan 12.5 mg and sumatriptan 50 mg from the prescription requirement. These active substances are characterized by good tolerability. Triptans display inter- and intra-individual variations in efficacy and tolerability. It is therefore desirable that as wide a selection of active substances as possible is available for self-medication of migraine attacks.
There is now almost 27 years of experience in the use of rizatriptan. In the following, the safety and efficacy of rizatriptan 5 mg will be discussed from a clinical perspective. Based on the available evidence, the use of rizatriptan in the self-medication of migraine will also be discussed.
The indication for rizatriptan is the acute treatment of the headache phase of migraine attacks with or without aura in adults. Rizatriptan is approved in two different strengths and in two different pharmaceutical forms:
-
Maxalt Lingua® 5 mg orodispersible tablets contain 5 mg rizatriptan and Maxalt Lingua® 10 mg orodispersible tablets contain 10 mg rizatriptan. The marketing authorization was granted in Germany on September 25, 1998.
-
Maxalt® 5 mg tablets contain 5 mg rizatriptan and Maxalt® 10 mg tablets contain 10 mg rizatriptan. Approval for this dose was also granted in Germany on September 25, 1998.
Risk–Benefit Profile of Rizatriptan Compared to Other Triptans
Efficacy: The systematic network meta-analysis by Cameron et al. (2015) provides an analysis of triptans in the acute treatment of migraine attacks [1]. A total of 133 randomized controlled trials were used for this analysis. According to this analysis, triptans in standard doses (eletriptan 40 mg, sumatriptan 50 mg, rizatriptan 10 mg, frovatriptan 2.5 mg, almotriptan 12.5 mg, zolmitriptan 5 mg, naratriptan 2.5 mg) significantly reduce headaches within 2 h in 42–76% of patients. In 18–50% of patients, persistent pain relief was achieved after 2 h. With a standard dose of triptans, 29–50% of patients achieved sustained headache relief after 24 h and 18–33% of patients achieved sustained freedom from pain. The use of escape medication for lack of efficacy was between 20% and 34%. With regard to the parameter “headache relief after 2 h”, the standard doses of triptans achieved better results (42–76%) than ergot alkaloids (38%). They also achieved the same or better results than NSAIDs, ASA and paracetamol (46–52%).
If the aim is to achieve the best possible tolerability and safety in the context of self-medication, the lowest possible dose should be selected in order to provide the most favourable tolerability and safety profile in the context of self-medication through low dosages. The lowest approved dose of rizatriptan is 5 mg. This was investigated in three randomized controlled trials with 752 patients (low dose, LD) [1]:
-
Rizatriptan 5 mg showed a higher efficacy of 51.2% with regard to the target parameter “2-h headache relief” compared to almotriptan in the standard dose (48.3%) and the low dose (43.3%), naratriptan in the standard dose (44.5%) and sumatriptan in the standard dose (49.7%) and sumatriptan in the low dosage (44.2%).
-
For the target parameter “2-h freedom from pain”, rizatriptan 5 mg also showed higher responder rates of 27.5% in the low dose compared to naratriptan in the standard dose (17.5%), almotriptan in the standard dose (24.5%) and the low dosage (18.5%) and compared to sumatriptan in the low dosage (24.9%).
The results show that rizatriptan at a dose of 5 mg (low dose, LD) is more effective than the triptans naratriptan 2.5 mg, almotriptan 12.5 mg and sumatriptan 50 mg, which were previously available for self-medication in Germany.
Tolerability: Ferrari et al. (2002) [7] analyzed in detail the results of 53 randomized clinical trials on the efficacy and tolerability of triptans in the acute treatment of migraine in the most comprehensive meta-analysis to date. The percentages below show the placebo-subtracted frequency rates of adverse events for the various triptans. According to these figures, the most common adverse event rate is 24.5% for the use of zolmitriptan 5 mg. Adverse events in the area of the CNS were found most frequently at 14.6% with the use of eletriptan 80 mg. At 2.9%, chest symptoms were the most common adverse event associated with the use of zolmitriptan 5 mg.
Rizatriptan 5 mg showed a similar frequency of any adverse event as sumatriptan 50 mg (7.9 vs. 7.8%), CNS adverse events were observed numerically more frequently than with sumatriptan 50 mg (6.1 vs. 3.7%) and chest symptoms less frequently than with sumatriptan 50 mg (0.9 vs. 1.9%).
When comparing the efficacy and tolerability parameters for the oral triptans in the meta-analysis by Ferrari et al. 2002 [7], there were no significant differences compared to sumatriptan 100 mg and rizatriptan 5 mg. The efficacy parameters of the standard dose of rizatriptan 10 mg are significantly better compared to sumatriptan 100 mg.
Effect of Beta-Adrenoceptor Antagonists on the Pharmacokinetics of Rizatriptan
Goldberg et al. 2001 [16] investigated potential pharmacokinetic and pharmacodynamic interactions between beta-adrenoceptor blockers and rizatriptan in several studies. In four double-blind, placebo-controlled, randomized, cross-over studies, the possible interaction was analyzed in 51 healthy volunteers. A single dose of 10 mg rizatriptan was administered after 7 days of propranolol (60 or 120 mg twice daily), nadolol (80 mg twice daily), metoprolol (100 mg twice daily) or placebo. The pharmacokinetics of rizatriptan were investigated.
-
Administration of rizatriptan during propranolol treatment (120 mg twice daily for 7.5 days) increased the AUC for rizatriptan by about 67% and the c-Max by about 75%.
-
A reduction in the dose of propranolol (60 mg twice daily) and/or a delay of 1 or 2 h between propranolol and rizatriptan did not result in a statistically significant change in the efficacy of propranolol on the pharmacokinetics of rizatriptan.
-
Administration of rizatriptan together with nadolol (80 mg twice daily) or metoprolol (100 mg twice daily) for 7 days had no effect on the pharmacokinetics of rizatriptan.
-
The study showed that no adverse events attributable to the pharmacokinetic interaction between propranolol and rizatriptan occurred.
-
None of the subjects experienced severe clinical, laboratory or other significant adverse effects during concomitant administration of rizatriptan with an adrenoceptor blocker.
-
In vitro incubations showed that propranolol, but not other beta-adrenoceptor blockers, inhibited the production of the indole acetic acid metabolite of rizatriptan and sumatriptan.
-
The results suggest that propranolol increases the plasma concentration of rizatriptan by inhibiting monoamine oxidase A.
The authors conclude from this study that, when prescribing rizatriptan to patients receiving propranolol for migraine prophylaxis, a dose of 5 mg of rizatriptan should be recommended. No dose adjustment is required when administered with other beta-adrenoceptor antagonists.
This study documents that propranolol can lead to an increase in plasma concentrations when taken concomitantly with rizatriptan. However, clinical effects, in particular an increased incidence of adverse events, have not been described or known to date.
The recommendation to use rizatriptan at a dose of 5 mg with concomitant treatment with propranolol is based on the theoretical possibility that increased plasma concentrations in clinical use could lead to an increased potential for side effects. However, to the best of our knowledge, no adverse events resulting from a potential interaction have been reported to date, despite over 20 years of use of rizatriptan in the treatment of migraine patients.
Possible safety concerns in self-medication with simultaneous use or intake of propranolol are relativized when using 5 mg rizatriptan. If the lower dose of 5 mg is used for self-medication, this issue is taken into account ex ante.
Efficacy and Tolerability of Rizatriptan in Sumatriptan Non-Responders
The response to the different triptans varies from patient to patient, both inter-individually and intra-individually. For example, while patients respond to one triptan, they may be non-responders to another triptan or triptans. The care of migraine patients has improved significantly thanks to the availability of seven different triptans. It is possible to rotate from one triptan to another if a patient does not respond to a particular triptan. In order to find an effective migraine treatment as quickly as possible, it is common practice to initially prescribe two or three triptans when migraine patients are first prescribed a triptan, so that the patient can gain experience with the effectiveness of different triptans.
Seeburger et al. (2010) [28] analyzed the effectiveness of rizatriptan in the treatment of acute migraine attacks in sumatriptan non-responders. The study included patients who did not respond adequately to sumatriptan 100 mg. Unsatisfactory response was defined as at least 50% of the attacks could not be treated effectively. In the baseline phase, the subjects treated migraine attacks with sumatriptan 100 mg, which is available as an OTC version in the USA. In a double-blind treatment phase, they were able to treat three further migraine attacks in a cross-over design with either rizatriptan 10 mg or placebo. The primary endpoint was pain relief after 2 h. A total of 102 patients took part in the study.
In the sumatriptan non-responders, taking rizatriptan 10 mg resulted in significant pain relief after 2 h compared to placebo (51% vs. 20%). Rizatriptan was also shown to be significantly superior in terms of pain relief after 2 h and sustained pain relief after 24 h. This study demonstrates the benefit of having several options to choose from, even in the context of self-medication, so that patients can achieve an effective therapy in this area.
Safety and Tolerability of Rizatriptan 5 mg, Rizatriptan 10 mg and Sumatriptan 100 mg
Since three triptans are now available for self-medication without a prescription, it is relevant for the decision of a switch to evaluate the efficacy, tolerability and safety of rizatriptan 5 mg in comparison with these substances. Several studies are available for this purpose.
In study protocol 030 [3], the safety, tolerability and efficacy of a single dose of rizatriptan 5 mg or 10 mg with sumatriptan 100 mg for the acute treatment of migraine attacks were analyzed in a randomized, placebo-controlled, parallel-group design. The main outcome measures were the time to onset of headache relief, the efficacy of the substances 2 h after dose administration and the comparison of the efficacy of rizatriptan 2 h after administration with the efficacy of placebo. The study was randomized and double-blind, triple-dummy and placebo-controlled in a parallel-group design. 164 patients were treated with rizatriptan 5 mg, 387 patients with rizatriptan 10 mg, 388 patients with sumatriptan 100 mg and 160 patients with placebo.
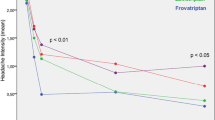
The results showed that rizatriptan 5 mg, rizatriptan 10 mg and sumatriptan are effective in relieving moderate and severe migraine attacks. Rizatriptan 5 mg was found to provide earlier or comparable pain relief compared to sumatriptan 100 mg. Rizatriptan 10 mg provided earlier pain relief than sumatriptan 100 mg and showed a significant effect just 1 h after ingestion. Rizatriptan 5 mg, rizatriptan 10 mg and sumatriptan 100 mg are effective in terms of pain relief and reduction of functional impairment in patients with migraine. Rizatriptan 10 mg is superior to sumatriptan 100 mg with regard to these criteria. Rizatriptan 5 mg, rizatriptan 10 mg and sumatriptan 100 mg are all effective in reducing concomitant symptoms of migraine attacks. Rizatriptan 5 mg, rizatriptan 10 mg are both superior to sumatriptan 100 mg in reducing the accompanying symptom of nausea. Rizatriptan 5 mg and Rizatriptan 10 mg are well tolerated. Both rizatriptan doses lead to fewer drug-related adverse effects than sumatriptan 100 mg. Figure 1 shows the percentage of patients with pain relief within 2 h.

Source: MRL clinical study report: a randomized, placebo-controlled, parallel-groups, outpatient study to examine the safety, tolerability, and efficacy of single oral doses of MK–0462 5 mg, MK–0462 10 mg, and Sumatriptan 100 mg for acute treatment of migraine (protocol 030) [3]
Number of patients with freedom from pain after 2 h with a single dose of rizatriptan 5 or 10 mg or sumatriptan 100 mg for the acute treatment of migraine attacks. The study was randomized and double-blind, triple-dummy and placebo-controlled in a parallel group design. Totals of 164 patients were treated with rizatriptan 5 mg, 387 patients with rizatriptan 10 mg, 388 patients with sumatriptan 100 mg and 160 patients with placebo.
All 1099 patients were included in the safety analysis. The following frequencies of adverse events were observed: rizatriptan 5 mg, 39%; rizatriptan 10 mg, 46.5%; sumatriptan 100 mg, 52.1%; and placebo, 31.9%. A higher percentage of patients reported higher frequencies of adverse events in the rizatriptan 10 mg treatment group compared to the placebo treatment group (p < 0.010). In contrast, the frequency of adverse events in the rizatriptan 5 mg group did not differ significantly from the frequency of adverse events in the placebo group. This study illustrated that the frequency of adverse events of rizatriptan 5 mg does not differ significantly compared to placebo.
In contrast, the sumatriptan 100 mg group had a higher incidence of adverse events compared to the placebo group (p < 0.010). Furthermore, the incidence of adverse events was significantly higher in the sumatriptan 100 mg group than in the rizatriptan 5 mg group (p < 0.010). The percentage of adverse events that were possibly, probably or definitely related to the drugs was higher in the sumatriptan 100 mg than in the rizatriptan 10 mg group (41.2% vs. 32.6%, p = 0.014).
Comparison of the Efficacy and Safety of Rizatriptan 5 mg and Sumatriptan 50 mg
As sumatriptan 50 mg has already been released from the prescription requirement and transferred to self-medication, the comparison of the efficacy and safety of rizatriptan 5 mg with that of sumatriptan 50 mg is of particular relevance. A corresponding analysis was carried out with study protocol 029 [2].
Rizatriptan 5 mg and sumatriptan 50 mg were significantly superior to placebo for both target parameters. Rizatriptan 5 mg and sumatriptan 50 mg were comparable for the parameters pain relief after 2 h and onset of pain relief within 2 h (see Figs. 2, 3, 4 [2]).

Source: MRL Clinical study report, multicenter: a randomized, placebo-controlled, parallel-groups, outpatient study to compare the efficacy and safety of MK–0462 5 mg and Sumatriptan 50 mg for the acute treatment of migraine (protocol 029) [2]
Percent of patients reporting pain relief at 2 h after treatment-by-baseline severity (all-patients-treated).

Source: MRL clinical study report, multicenter.: a randomized, placebo-controlled, parallel-groups, outpatient study to compare the efficacy and safety of MK–0462 5 mg and Sumatriptan 50 mg for the acute treatment of migraine (protocol 029) [2]
Cumulative percentage (life-table estimate) of patients with first report of pain relief within 2 h and 95% confidence intervals (all-patients-treated).

Source: MRL clinical study report, multicenter: a randomized, placebo-controlled, parallel-groups, outpatient study to compare the efficacy and safety of MK–0462 5 mg and Sumatriptan 50 mg for the acute treatment of migraine (protocol 029) [2]
Percent of patients reporting pain relief within 2 h of treatment dose (all-patients-treated).
The frequency of adverse events is listed in Table 1. At 37.3%, sumatriptan 50 mg showed significantly more clinical adverse events than placebo. At 33%, the frequency of clinical adverse events was significantly higher in the rizatriptan 5 mg group than in the placebo group.
-
Adverse events related to the drug were higher in the sumatriptan 50 mg group (28.9%) than in the placebo group (15%).
-
In contrast, the drug-related adverse events in the rizatriptan 5 mg group (23.7%) did not differ significantly from the corresponding frequency in the placebo group.
All 792 patients who received study medication were included in the safety analysis. The primary target parameter was the safety and tolerability of rizatriptan 5 mg in the treatment of acute migraine attacks. In addition, the safety and tolerability of rizatriptan 5 mg and sumatriptan 50 mg were evaluated comparatively. Adverse events, laboratory values and vital signs were included in the safety analysis. Clinical adverse events occurred with the following frequency: rizatriptan 5 mg, 33.0%; sumatriptan 50 mg, 37.3%; and placebo:20%. The rizatriptan 5 mg and sumatriptan 50 mg groups had higher incidences of adverse events than the placebo group (p = 0.023 and p < 0.010, respectively). The incidence of adverse events in the rizatriptan 5 mg and sumatriptan 50 mg groups did not differ significantly (p > 0.10).
With regard to the parameter study drug-related adverse events, the following results were obtained: rizatriptan 5 mg, 23.7%; sumatriptan 50 mg, 28.9%; and placebo,15.0%. In the sumatriptan 50 mg group, study medication-related adverse events were significantly more frequent than in the placebo group. Rizatriptan 5 mg showed no statistically significant differences with regard to the study drug-related adverse events parameter compared to placebo.
Comparison of Rizatriptan 5 mg, Rizatriptan 10 mg with Sumatriptan 25 mg and Sumatriptan 50 mg
In study protocol 46 [4], the efficacy, tolerability and safety of rizatriptan 5 mg and 10 mg were compared with those of sumatriptan 25 mg and sumatriptan 50 mg in a double-blind, placebo-controlled, cross-over design.
Table 2 shows a comparison of various target parameters between the four study groups. The efficacy of sumatriptan 50 mg did not differ significantly from the efficacy of rizatriptan 5 mg.
The adverse events for the first and for both treated attacks showed the following frequencies:
-
The incidence of any type of clinical adverse event in the rizatriptan 5 mg group and in the placebo group did not differ significantly (43.5% vs. 34.5%).
-
However, sumatriptan 50 mg had significantly more adverse events than treatment with placebo (45.7% vs. 34.5%, p < 0.05).
In all study groups, there were significantly more drug-related adverse events compared to placebo: rizatriptan 5 mg, 33.7%; rizatriptan 10 mg, 36.4%; sumatriptan 25 mg, 34.0%; sumatriptan 50 mg, 32.3%,; and placebo, 18.3%.
-
The efficacy of rizatriptan 5 mg is comparable to that of sumatriptan 50 mg.
-
Rizatriptan 5 mg is superior to sumatriptan 50 mg in terms of reducing the accompanying symptom of nausea.
-
Rizatriptan 5 and 10 mg as well as sumatriptan 25 and 50 mg are safe and well tolerated.
-
The frequency of adverse events for rizatriptan 5 mg does not differ significantly from the frequency of adverse events in the placebo group.
-
In contrast, however, the frequency of adverse events in the sumatriptan 50 mg group was significantly higher than in the placebo group.
Tolerability, Safety and Efficacy of Rizatriptan 5 mg from a Clinical Perspective
The studies allow the following conclusions:
-
Rizatriptan 5 mg is effective in the acute treatment of migraine attacks.
-
Compared to sumatriptan 50 mg, rizatriptan 5 mg displays comparable or greater efficacy with regard to the main target parameter of headache reduction after 2 h.
-
Nevertheless, drug-related adverse events are less frequent for rizatriptan 5 mg compared to sumatriptan 50 mg.
-
The frequency of drug-related adverse events when taking rizatriptan 5 mg does not differ significantly from placebo.
-
In contrast, the frequency of drug-related adverse events was significantly higher in the group treated for migraine with sumatriptan 50 mg compared to placebo.
The study results show that rizatriptan 5 mg does not have a higher side effect potential than sumatriptan 50 mg, which is already exempt from prescription. Nevertheless, rizatriptan 5 mg has a comparable or higher efficacy than sumatriptan 50 mg. Overall, there is therefore a better risk–benefit ratio for rizatriptan 5 mg compared to sumatriptan 50 mg.
As a switch from prescription-only to pharmacy-only status has already been implemented for sumatriptan 50 mg, it is appropriate to also implement this switch for rizatriptan 5 mg on the basis of the study and clinical experience.
Rizatriptan may also be effective in patients who do not respond to sumatriptan. This means that an active substance with a superior risk–benefit profile compared to sumatriptan 50 mg would also be available for self-medication in this group.
Intended Patient Group for Self-Medication with Rizatriptan 5 mg
In the area of self-medication, it is not necessary for patients to be treated with maximum dose and maximum efficacy. Patients who self-medicate with drugs from the pharmacy are characterized by the fact that the symptoms of their migraine attacks are in the mild or moderate range. It is therefore appropriate that the lowest effective dose is made available for self-medication and that the focus is on tolerability and safety.
Naratriptan 5 mg is also more effective than the 2.5-mg dose. However, only the dose of 2.5 mg was authorised from the onset. This means that the efficacy of naratriptan 2.5 mg is in the lower range compared to the other triptans. On the other hand, this results in better tolerability. From a clinical point of view, it therefore seems appropriate that this substance in the dose of 2.5 mg was the first to be made available in pharmacies for self-medication.
With regard to long-term clinical experience and clinical studies, it is also evident for rizatriptan 5 mg that this dose has no increased side effect potential compared to placebo. It is therefore justified that rizatriptan 5 mg should also be made available in pharmacies for self-medication and that patients should be provided with a further treatment option.
It follows on from this, that for patients with severe migraine attacks who do not respond to treatment with rizatriptan 5 mg as part of self-medication, physician consultation will be arranged and here it may be considered whether a higher dose of 10 mg is required. In the clinical context of migraine treatment, but also regarding development of medication overuse headache, early and higher doses are suggested to achieve effective attack therapy [27]. Therefore, if 5 mg is not sufficiently effective, 10 mg should be used.
The finding of altered pharmacokinetics of rizatriptan 5 mg when pretreated with propranolol is of no further clinical relevance in the event of a switch of rizatriptan 5 mg from prescription to pharmacy-only status. As rizatriptan 5 mg is provided as a single dose, concomitant prophylactic treatment of migraine with propranolol and the altered pharmacokinetics are already taken into account ex ante. This also applies to the group of patients with renal or hepatic disease.
To date, there is no known clinical relevance for the increase in plasma concentrations of rizatriptan with concomitant use of propranolol. In other countries, such as the United States, a corresponding restriction on the use of rizatriptan 10 mg with concomitant pre-treatment with propranolol is not listed in the prescribing information. There is no indication in the literature regarding a clinical relevance for the safety and tolerability of pretreatment with propranolol during treatment with rizatriptan 5 or 10 mg. These are studies in healthy subjects and theoretical precautionary measures in the context of initial drug approval. However, after more than 20 years of experience, no clinically relevant effects on the tolerability or safety of rizatriptan 5 mg or rizatriptan 10 mg were found in the clinical use in the acute treatment of migraine attacks.
On average, migraine patients suffer 1.6 attacks per month [10]. From a clinical point of view, it is appropriate for migraine patients with an average or even lower frequency of migraine attacks per month to self-medicate from the pharmacy. This applies all the more if patients can thereby achieve effective treatment. It is appropriate for this group of patients to have various treatment options from different groups of active ingredients at their disposal. It is therefore necessary that further substances with a comparable or even better risk–benefit profile are transferred from the prescription-only to the pharmacy-only status. As the study situation proves this for rizatriptan 5 mg, it is appropriate from a clinical standpoint that rizatriptan 5 mg should be transferred from prescription-only to pharmacy-only status.
When headaches occur for the very first time, there is always diagnostic uncertainty as to which type of headache is present. As a result, patients experiencing headaches for the first time with a relevant degree of suffering should always be examined and advised by a doctor. The requirement for self-medication should therefore be that this should only take place after an initial diagnosis of the headache by a doctor.
As primary headache disorders such as migraine can persist for several decades of life, self-medication can then be carried out responsibly in the further course of the disease if the headache phenotype remains constant and the occurrence of attacks is known, and if it is effective and well tolerated. However, if the medication is not effective, if adverse events occur or if the headache phenotype changes, patients should be informed that they should be seen by a doctor again during the course of the disease.
Patients should be informed at the pharmacy about what to do if a recurrent headache occurs. Patients should also be told what to do if rizatriptan 5 mg is not initially effective during an acute migraine attack.
-
If there is a significant improvement in the migraine attack after taking Rizatriptan 5 mg (reduction from severe or moderate headache to mild or no headache) and the headache recurs after this reduction, this is referred to as a recurrence headache. In this case, it is appropriate to take a second dose. A renewed improvement in the headache is then to be expected according to the clinical study situation. It is therefore also appropriate that two tablets are available in one packaging unit for self-medication.
-
However, if there is no initial improvement after taking Rizatriptan 5 mg, there is a primary inefficacy in the context of this attack. This does not necessarily mean that there will be no efficacy in the event of another attack at a different time. In the current attack, however, it is not practical to take the second dose. According to study data, it cannot be expected that a repeated dose will be effective during this attack in the event of primary inefficacy. Instead, a backup medication with a different active ingredient should be used.
Conclusion
-
The data presented show that rizatriptan in a dose of 5 mg for the treatment of acute migraine attacks fulfils the requirements for a transfer from prescription-only to pharmacy-only status at least as well as sumatriptan 50 mg, naratriptan 2.5 mg and almotriptan 12.5 mg.
-
From a clinical standpoint, it is desirable for migraine patients to have additional options available for self-medication.
-
Non-responders to other substances have a further treatment option with rizatriptan 5 mg with the same or even a better risk–benefit profile for a tolerable, safe and effective treatment of migraine attacks as part of self-medication.
References
Cameron C, Kelly S, Hsieh SC, et al. Triptans in the acute treatment of migraine: a systematic review and network meta-analysis. Headache. 2015;55(Suppl 4):221–35.
Clinical study report: a randomized, placebo-controlled, parallel-groups, outpatient study to compare the efficacy and safety of mk–0462 5 mg and sumatriptan 50 mg for the acute treatment of migraine (Protocol 029). https://classic.clinicaltrials.gov/ct2/show/NCT00897104 Accessed 12 May 2024.
Clinical study report: a randomized, placebo-controlled, parallel-groups, outpatient study to examine the safety, tolerability, and efficacy of single oral doses of MK–0462 5 mg, MK–0462 10 mg, and sumatriptan 100 mg for acute treatment of migraine protocol 030). https://classic.clinicaltrials.gov/ct2/show/NCT00898677. Accessed 12 May 12 2024.
Goldstein J, Ryan R, Jiang K et al. Crossover comparison of rizatriptan 5 mg and 10 mg versus sumatriptan 25 mg and 50 mg in migraine. Rizatriptan Protocol 046 Study Group. Headache 1998;38:737–747
Diener H-C, Förderreuther S, Kropp P et al (2018) Therapie der Migräneattacke und Prophylaxe der Migräne, S1-Leitlinie. Deutsche Gesellschaft für Neurologie (Hrsg.), Leitlinien für Diagnostik und Therapie in der Neurologie. www.dgn.org/leitlinien. Accessed 12 May 2024.
Evers S, Frese A, Marziniak M. Differenzialdiagnose von Kopfschmerzen. Dtsch Arztebl Int. 2006;103:3040.
Ferrari MD, Goadsby PJ, Roon KI, et al. Triptans (serotonin, 5-HT1B/1D agonists) in migraine: detailed results and methods of a meta-analysis of 53 trials. Cephalalgia. 2002;22:633–58.
Forward SP, Mcgrath PJ, Mackinnon D, et al. Medication patterns of recurrent headache sufferers: a community study. Cephalalgia. 1998;18:146–51.
Gbd 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1211–59.
Göbel H. Die Kopfschmerzen. Berlin, Heidelberg: Springer; 2012.
Göbel H, Gessner U, Petersen-Braun M, et al. Acetylsalicylsäure bei der Selbstmedikation von Migranekopfschmerzen. Eine apothekenbasierte Analyse. Schmerz. 2007;21:49–54.
Göbel H, Heinze-Kuhn K, Petersen I, et al. Sektorenübergreifende schmerzmedizinische Versorgung. Schmerzklinik Kiel und bundesweites Kopfschmerzbehandlungsnetz. Schmerz. 2013;27:149–65.
Göbel H, Heinze A, Heinze-Kuhn K, et al. Efficacy and tolerability of rizatriptan 10 mg in migraine: experience with 70 527 patient episodes. Headache. 2001;41:264–70.
Göbel H, Petersen-Braun M. Why patients with primary headache illnesses do not consult a doctor. In: Olesen J, editor. Epidemiology and classification of headache. New York: Raven Press; 1994. p. 267–72.
Göbel H, Petersen-Braun M, Soyka D. The epidemiology of headache in Germany: a nationwide survey of a representative sample on the basis of the headache classification of the International Headache Society. Cephalalgia. 1994;14:97–106.
Goldberg MR, Sciberras D, De Smet M, et al. Influence of beta-adrenoceptor antagonists on the pharmacokinetics of rizatriptan, a 5-HT1B/1D agonist: differential effects of propranolol, nadolol and metoprolol. Br J Clin Pharmacol. 2001;52:69–76.
Hagen K, Stordal E, Linde M, et al. Headache as a risk factor for dementia: a prospective population-based study. Cephalalgia. 2014;34:327–35.
Headache Classification Committee of the International Headache Society. The international classification of headache disorders, 3rd edition. Cephalalgia. 2018;38:1–211.
Hu X, Zhou Y, Zhao H, et al. Migraine and the risk of stroke: an updated meta-analysis of prospective cohort studies. Neurol Sci. 2017;38:33–40.
Katsarava Z, Mania M, Lampl C, et al. Poor medical care for people with migraine in Europe—evidence from the Eurolight study. J Headache Pain. 2018;19:10.
Lebedeva ER, Olesen J, Osipova VV, et al. The Yekaterinburg headache initiative: an interventional project, within the global campaign against headache, to reduce the burden of headache in Russia. J Headache Pain. 2013;14:101.
Linde M, Gustavsson A, Stovner LJ, et al. The cost of headache disorders in Europe: the Eurolight project. Eur J Neurol. 2012;19:703–11.
Olesen J. International classification of headache disorders. Lancet Neurol. 2018;17:396–7.
Petersen-Braun M, Göbel H. Names and classification patients with primary headache illnesses find for their headaches. In: Olesen J, editor. Epidemiology and classification of headache. New York: Raven Press; 1994. p. 51–4.
Porst M, Wengler A, Leddin J, et al. Migraine and tension-type headache in Germany. Prevalence and disease severity from the BURDEN 2020 Burden of Disease Study. J Health Monit. 2020;5:2–24.
Radtke A, Neuhauser H. Prevalence and burden of headache and migraine in Germany. Headache. 2009;49:79–89.
Ruscheweyh R, Gossrau G, Dresler T, et al. Triptan non-response in specialized headache care: cross-sectional data from the DMKG Headache Registry. J Headache Pain. 2023;24:135.
Seeburger JL, Taylor FR, Friedman D, et al. Efficacy and tolerability of rizatriptan for the treatment of acute migraine in sumatriptan non-responders. Cephalalgia Int J Headache. 2011;31:786–96.
Steiner TJ, Stovner LJ, Vos T, et al. Migraine is first cause of disability in under 50s: will health politicians now take notice? J Headache Pain. 2018;19:17.
Stovner LJ, Zwart JA, Hagen K, et al. Epidemiology of headache in Europe. Eur J Neurol. 2006;13:333–45.
Straube A, Gaul C, Forderreuther S, et al. Therapie und Versorgung bei chronischer Migrane : Expertenempfehlung der Deutschen Migrane- und Kopfschmerzgesellschaft/Deutsche Gesellschaft fur Neurologie sowie der Osterreichischen Kopfschmerzgesellschaft/Schweizerischen Kopfwehgesellschaft. Nervenarzt. 2012;83:1600–8.
Wang SJ, Chen PK, Fuh JL. Comorbidities of migraine. Front Neurol. 2010;1:16.
Funding
This journal’s Rapid Service Fee and Open Access Fee were supported by Organon Healthcare GmbH.
Author information
Authors and Affiliations
Contributions
PD Dr. Carl Göbel—conceptualization, interpretation of the results, writing of the first draft of the manuscript. Dr. Axel Heinze—contribution to interpretation and analysis. PD Dr. Anna Cirkel—contribution to interpretation and analysis. Prof. Dr. Hartmut Göbel—conceptualization, co-writing of the manuscript, interpretation and analysis.
Corresponding author
Ethics declarations
Conflict of Interest
Carl Göbel has received research and/or consulting funding from Novartis and Teva. Axel Heinze has received research and/or consulting funding from Novartis and Teva. Anna Cirkel declares no conflicts of interest. Hartmut Göbel has received research and/or consulting funding from Amgen, Abbvie, Allergan, Biohaven, Elli Lilly, Hormosan, Lundbeck, Novartis, Organon, Teva.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Göbel, C.H., Heinze, A., Cirkel, A. et al. Rizatriptan as an Over-the-Counter Triptan in the Treatment of Migraine Attacks. Pain Ther 13, 813–827 (2024). https://doi.org/10.1007/s40122-024-00625-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-024-00625-2