Abstract
Introduction
This clinical trial assessed the activity of reproxalap, a novel reactive aldehyde species modulator, and estimated clinically relevant thresholds for changes in ocular itching and redness in an allergic conjunctivitis field trial.
Methods
This was a randomized, double-masked, vehicle-controlled phase 2 trial. Patients with ragweed-associated allergic conjunctivitis were assessed over 28 days in an environmental setting with approximately four doses per day of either 0.25% reproxalap, 0.5% reproxalap, or vehicle. Patients recorded ocular itching, redness, tearing, and eyelid swelling scores (each with a 0–4 scale, except for a 0–3 scale for swelling), and completed the Allergic Conjunctivitis Quality of Life Questionnaire at the beginning and end of the trial.
Results
Mixed model of repeated measures analysis demonstrated statistically lower itching and tearing scores (pooled P = 0.026 and P < 0.001, respectively) and numerically lower redness and eyelid swelling scores than vehicle on days when pollen exceeded the 95th percentile value. Using three anchor-based and three distribution-based approaches, the meaningful within-patient change and the between-group meaningful difference for patient-reported ocular itching and redness was estimated to be approximately 0.5. The most common treatment-emergent adverse event associated with reproxalap was transient irritation upon instillation.
Conclusion
In a field clinical trial, reproxalap was well tolerated and superior to vehicle in reducing ocular itching on high-pollen days. The clinical meaningfulness threshold estimates of 0.5 units are among the first such calculations generated for the standard ocular itching and redness scores, providing important context for the clinical interpretation of clinical trials in allergic conjunctivitis.
Plain Language Summary
While allergic conjunctivitis affects millions of patients worldwide, treatments with new mechanisms have not been introduced in decades. Reproxalap, a medicine being investigated as a treatment for allergic conjunctivitis, works by regulating reactive aldehyde species—molecules that are increased in a variety of inflammatory diseases. This clinical trial assessed the activity of reproxalap and estimated what amount of change in ocular itching and redness should be considered clinically important. Patients with ragweed-associated allergic conjunctivitis were assessed over 28 days and were given one of three possible eye drops at approximately four doses per day: 0.25% reproxalap; 0.5% reproxalap; or vehicle, which was composed of the same ingredients but does not contain reproxalap. Patients recorded ocular itching, redness, tearing, and eyelid swelling (all scales ranged from 0 [none] to 4 [severe] except for eyelid swelling, which ranged from 0 to 3), and completed a quality-of-life questionnaire on allergic conjunctivitis at the beginning and end of the trial. The results indicated that reproxalap was significantly better than vehicle in reducing itching and tearing scores and was better than vehicle in reducing redness and eyelid swelling scores on days when pollen counts were high. The trial also suggested that a reduction in ocular itching and redness scores of approximately 0.5 or more (scale 0–4) is likely to be clinically important. Overall, reproxalap was well tolerated and no safety concerns were noted. The most common side effect was transient ocular discomfort after eye drop administration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this clinical trial? |
This clinical trial was carried out to assess the activity of reproxalap and estimate clinically relevant thresholds for changes in ocular itching and redness in an allergic conjunctivitis field trial. |
What did the clinical trial ask/what was the hypothesis of the clinical trial? |
It was hypothesized that reproxalap would be superior to vehicle in reducing the signs and symptoms of allergic conjunctivitis. Additionally, what are the relevant thresholds for patient-reported ocular itching and redness scores? |
What was learned from the clinical trial? |
The clinical meaningfulness threshold estimates of 0.5 units were derived for the standard patient-reported ocular itching and redness scores. |
What were the clinical trial outcomes/conclusions? |
Reproxalap was well tolerated and superior to vehicle in reducing ocular itching on high-pollen days. The clinically relevant threshold for changes in ocular itching and redness scores (range 0–4) is approximately 0.5 units. |
Introduction
Allergic conjunctivitis affects millions of patients worldwide, but novel therapeutic mechanisms have not been introduced in decades. Although topical antihistamines are widely used for the treatment of allergic conjunctivitis, up to 60% of patients require additional medication, including topical corticosteroids, which can lead to ocular toxicity [1, 2]. Therefore, new drugs for ocular allergy with alternative mechanisms of action that can be combined with existing therapies are desirable [3]. One such mechanism that represents a novel approach for the treatment of ocular inflammation is the modulation of reactive aldehyde species (RASP), which are small molecule, systems-based mediators of cytokine release [4, 5]. Reproxalap, a topical ocular RASP modulator, has demonstrated activity in phase 2/3 trials in noninfectious anterior uveitis, dry eye disease, and allergic conjunctivitis [6,7,8,9,10].
In both controlled and environmental settings, the typical method for assessment of activity in patients with allergic conjunctivitis includes measurement of ocular itching and redness on a 0 (none) to 4 (severe) scale [9,10,11]. Although the clinically important difference in ocular itching score between treatment groups has traditionally been set at 1 unit [12], evidence justifying 1 unit as a meaningful difference is lacking. Distribution-based techniques (e.g., effect sizes, standard deviation and, standard error of measurement) are typically used to estimate clinically meaningful between-group magnitudes, whereas anchor-based techniques, which compare changes in scores with an external indicator (anchor) as a reference, are typically used to estimate meaningful within-patient changes [13,14,15]. Remarkably, to our knowledge, clinically relevant thresholds derived from either distribution-based or anchor-based approaches for patient-reported ocular itching and redness scores have not been published.
A randomized, double-masked, parallel-group phase 2 trial in ragweed-sensitive patients with allergic conjunctivitis was performed over 28 days to assess the activity of two concentrations of reproxalap compared with vehicle in an environmental setting. In addition, the signs, symptoms, and quality-of-life (QOL) data from the trial were incorporated across three distribution-based and three anchor-based approaches to estimate clinically meaningful between-group and within-patient differences in patient-reported ocular itching and redness scores.
Methods
Trial Design
Patients with seasonal allergic conjunctivitis were enrolled in a multicenter, randomized, double-masked, vehicle-controlled, parallel-group phase 2 trial designed to evaluate the activity of two concentrations of topical ocular reproxalap (0.25% and 0.5%) relative to vehicle in an environmental setting over 28 days during ragweed pollen season. The trial consisted of five visits: two screening visits during which skin test and conjunctival challenge sensitivity to ragweed was confirmed, a visit to confirm continued eligibility after 6 days of four-times-daily plus as-needed dosing of an artificial tear, a visit 2 weeks after test article (reproxalap or vehicle) administration was initiated, and a visit 2 weeks later at the end of the trial. Patients were randomly assigned 1:1:1 according to a predetermined randomization sequence to receive either 0.25% reproxalap, 0.5% reproxalap, or vehicle four times daily and up to four more times per day as needed. All test articles were preservative-free and did not contain benzalkonium chloride. An unmasked and independent biostatistics vendor generated a randomization list for clinical sites to assign masked clinical trial drug to patients. Patients, investigators, and the sponsor were masked to treatment assignment throughout the trial.
The trial (ClinicalTrials.gov, NCT03660878) was performed in the USA in accordance with the Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Patients, the International Council for Harmonisation Guideline on Good Clinical Practice, and all applicable local regulatory requirements and laws. The trial was carried out with approval from an institutional review board (Alpha IRB, San Clemente, CA, USA), informed consent was obtained from the patients, and the research followed Health Insurance Portability and Accountability Act regulations.
Patient Selection
Adult patients aged 18 years or more were eligible to participate in the trial if they met the following criteria: history of allergic conjunctivitis, positive skin test to ragweed pollen (i.e., greater wheal size than the negative control or same wheal size as negative control with presence of itching), baseline investigator-assessed conjunctival redness and at least one patient-reported symptom (ocular itching, tearing, or eyelid swelling) scores of at least 1 (all scales ranged from 0 [none] to 4 [severe] except for eyelid swelling, which ranged from 0 to 3), and conjunctival ragweed challenge-induced ocular itching and redness scores of at least 2 for both eyes. Patients were excluded for any clinically significant slit-lamp findings or a history of inflammatory conditions, infectious diseases, or ocular surgeries that may have interfered with the conduct of the trial. Other exclusions included use of antihistamines within 3 days prior to screening, corticosteroids within 14 days prior to screening, or immunotherapeutic agents within 60 days prior to screening.
Clinical Trial Assessments and Endpoints
Patient-reported ocular itching, ocular redness, ocular tearing, and eyelid swelling scores were recorded three times daily for 28 days. All scores, which were averaged by day, were derived from Ora Calibra® scale (Ora, Inc., Andover, MA, USA) scores ranging from 0 (none) to 4 (severe) except eyelid swelling, which ranged from 0 (none) to 3 (severe). Half-unit increments were possible for the ocular itching scale. The Allergic Conjunctivitis Quality of Life Questionnaire (ACQLQ©; Ora, Inc.), a 17-item assessment scale (each item rated on a 0 [not bothered] to 6 [extremely bothered]) was performed on the first and last days of test article administration concurrent with assessment of symptom scores [16, 17]. The itching and redness ACQLQ items were used to assess the QOL impact relative to itching and redness scores. Safety assessments included visual acuity, slit-lamp biomicroscopy, undilated fundoscopy, intraocular pressure, and adverse events (AEs).
Statistical Analysis
The trial was exploratory and not formally powered. Given that reproxalap had not been previously tested in an allergen chamber, no primary or secondary endpoints were designated. Mixed-effect models for repeated measures (MMRM) were used to assess change from baseline (the first day of treatment) of symptom scores over all time points in aggregate, with treatment group and day as factors. Subset MMRM analyses were performed on high-pollen days, defined as days when pollen counts met or exceeded the 95th percentile for weed pollens (i.e., 325 grains per cubic meter) for individual and pooled reproxalap groups, according to the American Academy of Allergy, Asthma, and Immunology’s National Allergy Bureau [18]. Rank-based nonparametric testing for longitudinal data was used as a sensitivity analysis for the pooled-group MMRM subset results [19]. Ocular itching and redness symptom scores were regressed versus the respective ACQLQ items with the y intercept set at 0. Safety assessments were evaluated with summary statistics.
Three anchor-based techniques (comparison of the ACQLQ as a QOL anchor to itching and redness scores) were performed to assess the meaningful within-patient change in patient-reported ocular itching and redness scores: slope of the relationship between scores and the respective ACQLQ item, upper limit of the 95th percentile confidence interval of the change in scores for patients with no change in the respective ACQLQ item [15, 20], and the subtraction method (i.e., change in scores for patients with 1-point improvement in the respective ACQLQ item minus change in scores for patients with no improvement in the respective ACQLQ item) [21]. Three distribution-based techniques were performed on the itching and redness scores to estimate a relevant between-group difference: 10% of the range of the scoring scales (0–4) [22], half of the baseline standard deviation [23], and standard error of the mean using Cronbach’s alpha across all symptom scores in aggregate as the test reliability [24, 25].
Results
Patient Disposition, Baseline Characteristics, Dosing, and Pollen Exposure
Patient disposition is diagrammed in Fig. 1. A total of 196 patients with allergic conjunctivitis were screened, and 52 were randomized and treated between September 9, 2018 and December 20, 2019 at three clinical sites in the USA. Most screen failures were due to insufficient ocular itching and redness either at baseline or after conjunctival challenge. There were three discontinuations among the randomized patients: one in the 0.25% reproxalap group discontinued for voluntary reasons not otherwise specified and two in the 0.5% reproxalap group were withdrawn because of AEs (ocular irritation in one patient considered related to drug and development of brain lesions in one patient deemed unrelated to drug).
Baseline demographic characteristics were generally comparable across groups (Table 1). Compliance with drug administration was high; the average eye drops per day for all patients in the 0.25% reproxalap, 0.5% reproxalap, and vehicle groups were 3.9, 3.6, and 3.9 drops, respectively. As-needed dosing was minimal; two, four, and three patients required more than four eye drops during any single day in the 0.25% reproxalap, 0.5% reproxalap, and vehicle groups, respectively. Pollen exposure was significantly lower than expected, and the most common daily pollen count was 0 grains per cubic meter (Fig. 2). Five patients in each reproxalap group and four patients in the vehicle group were exposed to American Academy of Allergy Asthma, and Immunology’s National Allergy Bureau weed pollen levels at the 95th or higher percentile (325 grains per cubic meter) for an average of 7 days, and were therefore designated high-pollen patients [18].
Efficacy
No statistically significant changes were observed across treatment groups for any patient-reported ocular symptom. For high-pollen patients, however, all patient-reported symptoms diminished over the course of the trial in patients treated with reproxalap (Fig. 3). Improvement (i.e., decreases) from baseline in ocular tearing was statistically superior to that of vehicle for each reproxalap group (P = 0.005 and P < 0.001 for 0.25% reproxalap and 0.5% reproxalap, respectively) and for pooled reproxalap groups (P < 0.001) (Fig. 3a). Improvement in ocular itching over that of vehicle was numerically superior for both reproxalap groups (P = 0.058 for each) and achieved statistical significance when reproxalap groups were pooled (P = 0.026) (Fig. 3b). Improvement in ocular redness (Fig. 3c) and eyelid swelling (Fig. 3d) was not statistically significant for either reproxalap group in comparison to vehicle, although improvement in ocular redness approached statistical significance for 0.25% reproxalap (P = 0.071). Nonparametric statistics were consistent with the MMRM findings for the high-pollen patients.
Patient-reported symptom scores for a ocular tearing, b ocular itching, c ocular redness, and d eyelid swelling during high-pollen days. The range of each scale is 0 (none) to 4 (severe) except for eyelid swelling, which is 0–3. P values were derived from mixed-effect models for repeated measures analysis of change from baseline (the first day of treatment) over all time points in aggregate through the end of the trial (day 28). High pollen was defined as > 95th percentile weed pollen count (325 g/m3) [16]. SEM, standard error of the mean
Estimation of Ocular Itching and Ocular Redness Clinical Relevance Thresholds
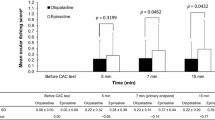
A high degree of correlation between patient-reported ocular itching (r = 0.87) and redness (r = 0.88) scores and the corresponding itching and redness items of the ACQLQ was demonstrated (P < 0.001 for each) (Fig. 4). The regression slopes for itching and redness were 0.46 and 0.59, respectively, indicating symptom score change per unit change on the appropriate ACQLQ item. During the 28 days of the trial, mean itching and redness score changes (upper 95th percentile confidence interval) for patients with no change on the appropriate ACQLQ item were 0.03 (0.41) and 0.39 (0.66), respectively. Similarly, mean itching and redness score changes for patients with a 1-unit improvement on the respective ACQLQ item were 0.81 and 0.80, respectively, resulting in subtraction method differences of 0.78 for itching and 0.41 for redness (Fig. 5a). Distribution-based approaches yielded results similar to those of the anchor-based methods. Ten percent of the scale range (0–4) is 0.4 for the symptom scores. The standard errors of the means for itching and redness scores were 0.38 and 0.41, respectively. Half of the baseline standard deviation was 0.43 for itching and 0.46 for redness scores (Fig. 5b).
Relationship of a ocular itching and b ocular redness scores to quality-of-life scores. For all randomized participants, patient-reported ocular itching and redness scores were plotted relative to Allergic Conjunctivitis Quality of Life Questionnaire (ACQLQ) items for itching and redness, respectively
Threshold estimates for a meaningful within-patient change, as assessed by anchor-based analyses, and b between-group meaningful difference, as assessed by distribution-based analyses. Squares indicate ocular itching score estimates, and circles indicate ocular redness score estimates. Both ocular itching and redness scores were reported by patients over a range of 0 (none) to 4 (severe). ACQLQ Allergic Conjunctivitis Quality of Life Questionnaire, SD standard deviation, SEM standard error of the mean
Safety and Tolerability
Both concentrations of reproxalap were well tolerated. Treatment-emergent AEs (TEAEs) related to test article were observed in 13 patients (25%) following exposure to 0.25% reproxalap, 16 patients (31%) following exposure to 0.5% reproxalap, and one patient (2%) following exposure to vehicle. Approximately 42% of patients experienced no TEAEs, and no patients experienced a serious AE related to therapy. Overall, the most common TEAEs were transient irritation upon instillation of the drug. Changes from baseline in best-corrected visual acuity, slit-lamp biomicroscopy, dilated fundoscopy, and intraocular pressure assessments did not reveal any clinically significant findings, as assessed by the site investigators.
Discussion
The results of the present trial highlight the challenge of controlling pollen exposure during field-based assessments of allergic conjunctivitis. Figure 2 illustrates the striking numerical skew toward a pollen count of 0 (grains per cubic meter) during the trial, indicating that most patients were not exposed to target levels of pollen (at least 95th percentile). Compounding the problem of variability in allergen exposure, many patients monitor pollen counts to avoid exposure during high-pollen days. The variability of pollen exposure in field trials suggests that conjunctival challenge trials and real-world allergen chamber exposures may be more efficient designs for the assessment of drug activity in allergic conjunctivitis [9, 10]. Nonetheless, consistent with prior clinical results, the activity of reproxalap over vehicle across all four symptom scores, which were statistically significant for pooled itching (P = 0.026) and tearing (P < 0.001) scores, during high-pollen days (Fig. 3) suggests activity of reproxalap in ameliorating allergic conjunctivitis symptoms [9, 10]. Because the exposure to high-pollen days in the clinical trial was limited, both parametric and nonparametric statistics were employed, yielding similar outcomes. Larger field trials of reproxalap are needed to confirm the results.
Notwithstanding the longtime use of patient-reported symptom scores in allergic conjunctivitis trials, the determination of clinically important thresholds for such scores has not been previously described [11]. In the present trial, the ACQLQ was used as an allergic conjunctivitis-specific QOL assessment to anchor the utility of itching and redness symptom scores [16, 17]. A statistically significant correlation was observed between ACQLQ itching and redness items and the symptom scores (0.88 and 0.87, respectively; each P < 0.0001), and the slopes of the correlations were 0.46 and 0.59, respectively (Fig. 4). The slopes imply that for each measurable change in QOL, itching and redness scores changed by approximately 0.5 units, an estimate of the meaningful within-patient change. Two other anchor-based assessments, the subtraction method and the 95th percentile confidence interval upper limit for patients with no change in ACQLQ scores, were consistent with the regression results for both itching and redness scores (Fig. 5b) [20, 21]. Distribution-based assessments used to estimate between-group meaningful differences also yielded a 0.5-unit threshold (Fig. 5a). Thus, for the 0–4 ocular itching and redness patient-reported scales, thresholds for clinically meaningful within-patient change, which could be used for responder analyses, and between-group difference, which could be used to compare treatment groups, were deemed to be approximately 0.5 units.
Although the estimation of meaningful clinical thresholds is influenced by response options, patient population, number of items, assessment type, frequency of test administration, and other factors, the 0.5-unit value suggested for meaningful within-patient change by the anchor-based techniques described is consistent with that of other scales. Using anchor-based techniques, Zisapel and Nir noted that a 1-point change on a 5-point scale for sleep quality likely overestimates within-patient relevance thresholds [26]. Meaningful within-patient improvement as a percentage of scale across a variety of ranges was reviewed and prospectively tested using anchor-based techniques with two functional scales, two utility scales, and a performance scale in patients with cancer and was 4.5% on average, which is equivalent to less than 0.25 points for the ocular itching and redness scales [22].
Meaningful within-patient change estimates the difference that is relevant to individual patients, and is generally larger than clinically relevant between-group differences [21]. With respect to ocular itching, therefore, the within-patient estimate of approximately 0.5 points suggests that the 1-point between-group threshold of clinical relevance that has been typically employed is overly conservative and may substantially underestimate the clinical relevance of drug activity in allergic conjunctivitis trials [12]. Similarly, the 2-point responder analysis demonstrating the clinical relevance of reproxalap in the ALLEVIATE allergic conjunctivitis trial suggests that the average between-group difference in ALLEVIATE during the time frame of the responder analysis (0.4 points) is clinically meaningful and consistent with the data summarized above [9]. Finally, the clinical utility estimates derived from the present trial suggest that the reduction in itching and redness scores presented in Fig. 3 are clinically meaningful.
Conclusions
This clinical trial found reproxalap to be well tolerated and superior to vehicle in reducing ocular itching on high-pollen days. Additionally, relative to the patient-reported ocular itching and redness scales typically used in allergic conjunctivitis clinical trials, the results from the present trial suggest a new threshold for responder analyses and imply that the typical between-group threshold for clinical relevance in future clinical trials could be reasonably lowered. Larger trials correlating changes in QOL with changes in patient-reported ocular itching and redness scores are warranted to confirm the clinical relevance threshold findings reported herein.
References
Leonardi A, Piliego F, Castegnaro A, et al. Allergic conjunctivitis: a cross-sectional study. Clin Exp Allergy. 2015;45(6):1118–25.
McGhee CN, Dean S, Danesh-Meyer H. Locally administered ocular corticosteroids: benefits and risks. Drug Saf. 2002;25(1):33–55.
Singh K, Axelrod S, Bielory L. The epidemiology of ocular and nasal allergy in the United States, 1988–1994. J Allergy Clin Immunol. 2010;126(4):778–83.e6.
Higdon A, Diers AR, Oh JY, Landar A, Darley-Usmar VM. Cell signalling by reactive lipid species: new concepts and molecular mechanisms. Biochem J. 2012;442(3):453–64.
Raghavan S, Subramaniyam G, Shanmugam N. Proinflammatory effects of malondialdehyde in lymphocytes. J Leukoc Biol. 2012;92(5):1055–67.
Mandell KJ, Clark D, Chu DS, Foster CS, Sheppard J, Brady TC. Randomized phase 2 trial of reproxalap, a novel reactive aldehyde species inhibitor, in patients with noninfectious anterior uveitis: model for corticosteroid replacement. J Ocul Pharmacol Ther. 2020;36(10):732–9.
Clark D, Sheppard J, Brady TC. A randomized double-masked phase 2a trial to evaluate activity and safety of topical ocular reproxalap, a novel RASP inhibitor, in dry eye disease. J Ocul Pharmacol Ther. 2021;37(4):193–9.
Clark D, Tauber J, Sheppard J, Brady TC. Early onset and broad activity of reproxalap in a randomized, double-masked, vehicle-controlled phase 2b trial in dry eye disease. Am J Ophthalmol. 2021;226:22–31.
Clark D, Cavanagh B, Shields AL, Karpecki P, Sheppard J, Brady TC. Clinically relevant activity of the novel RASP inhibitor reproxalap in allergic conjunctivitis: the phase 3 ALLEVIATE trial. Am J Ophthalmol. 2021;230:60–7.
Clark D, Karpecki P, Salapatek AM, Sheppard JD, Brady TC. Reproxalap improves signs and symptoms of allergic conjunctivitis in an allergen chamber: a real-world model of allergen exposure. Clin Ophthalmol. 2022;16:15–23.
Abelson MB, Gomes PJ, Vogelson CT, et al. Clinical efficacy of olopatadine hydrochloride ophthalmic solution 0.2% compared with placebo in patients with allergic conjunctivitis or rhinoconjunctivitis: a randomized, double-masked environmental study. Clin Ther. 2004;26(8):1237–48.
Torkildsen G, Narvekar A, Bergmann M. Efficacy and safety of olopatadine hydrochloride 0.77% in patients with allergic conjunctivitis using a conjunctival allergen-challenge model. Clin Ophthalmol. 2015;9:1703–13.
Shields A, Coon C, Hao Y, et al. Patient-reported outcomes for US oncology labeling: review and discussion of score interpretation and analysis methods. Expert Rev Pharmacoecon Outcomes Res. 2015;15(6):951–9.
US Food and Drug Administration. Guidance for Industry—Patient-reported outcome measures: use in medical product development to support labeling claims. Published 2009. https://www.fda.gov/media/77832/download. Accessed April 27, 2022.
US Food and Drug Administration. Patient-Focused Drug Development Guidance Public Workshop: Incorporating clinical outcome assessments into endpoints for regulatory decision-making. Held December 6, 2019. https://www.fda.gov/media/132505/download. Accessed April 27, 2022.
Berger W, Abelson MB, Gomes PJ, et al. Effects of adjuvant therapy with 0.1% olopatadine hydrochloride ophthalmic solution on quality of life in patients with allergic rhinitis using systemic or nasal therapy. Ann Allergy Asthma Immunol. 2005;95(4):361–71.
Mroz M, Shapiro SA, Abelson MB. Development of the Allergic Conjunctivitis Quality of Life Questionnaire (ACQLQ). Presented at DIA 9th Annual Symposium for Quality of Life Evaluations. Hilton Head, SC, USA; 2002.
American Academy of Allergy, Asthma and Immunology. Reading the levels. https://pollen.aaaai.org/#/pages/reading-the-levels. Accessed February 23, 2022.
Noguchi K, Gel YR, Brunner E, Konietschke F. nparLD: an R Software package for the nonparametric analysis of longitudinal data in factorial experiments. J Stat Softw. 2012;50(12):1–23.
Conijn AP, Bipat S, Reekers JA, Koelemay MJ. Determining the minimally important difference for the VascuQol Sumscore and its domains in patients with intermittent claudication. Eur J Vasc Endovasc Surg. 2016;51(4):550–6.
McLeod LD, Cappelleri JC, Hays RD. Best (but oft-forgotten) practices: expressing and interpreting associations and effect sizes in clinical outcome assessments. Am J Clin Nutr. 2016;103(3):685–93.
Ringash J, O’Sullivan B, Bezjak A, Redelmeier DA. Interpreting clinically significant changes in patient-reported outcomes. Cancer. 2007;110(1):196–202.
Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(5):582–92.
Wyrwich KW, Nienaber NA, Tierney WM, Wolinsky FD. Linking clinical relevance and statistical significance in evaluating intra-individual changes in health-related quality of life. Med Care. 1999;37(5):469–78.
Jelovsek JE, Chen Z, Markland AD, et al. Minimum important differences for scales assessing symptom severity and quality of life in patients with fecal incontinence. Female Pelvic Med Reconstr Surg. 2014;20(6):342–8.
Zisapel N, Nir T. Determination of the minimal clinically significant difference on a patient visual analog sleep quality scale. J Sleep Res. 2003;12(4):291–8.
Acknowledgements
Funding
This clinical trial was sponsored by Aldeyra Therapeutics, Inc. (Lexington, MA, USA). Aldeyra Therapeutics is also funding the journal Rapid Service Fee.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Bill Cavanagh: data curation, investigation, project administration, and supervision and writing—original draft. Paul J. Gomes: data curation, investigation, project administration, and supervision, formal analysis and methodology, and validation. Christopher E. Starr: visualization. Kelly K. Nichols: visualization. Todd C. Brady: conceptualization, provision of resources, and funding acquisition, formal analysis and methodology, visualization, writing—original draft.
Medical Writing, Editorial, and Other Assistance
Editorial and medical writing support under the guidance of the authors was provided by Ricky Sidhu, PharmD (ApotheCom, San Francisco, CA, USA), and funded by Aldeyra Therapeutics, Inc. (Lexington, MA, USA), in accordance with Good Publication Practice (GPP3) guidelines (Ann Intern Med 2015;163:461–464). The authors also thank the participants of this clinical trial.
Disclosures
Bill Cavanagh reports employment with and stock ownership in Aldeyra Therapeutics. Paul J. Gomes reports employment with Ora, Inc. Christopher E. Starr reports consulting fees from Novartis, Allergan, TearLab, Sun Pharma, Bruder, BlephEx, Kala Pharmaceuticals, Eyevance, Quidel, Dompe, Johnson & Johnson Vision, Essiri Labs, Tarsus Pharmaceuticals, Oyster Point Pharma, Visionology, CSI Dry Eye, Aerie, and Aldeyra Therapeutics; and reports stock ownership in Essiri Labs and Visionology. Kelly K. Nichols reports consulting fees from Allergan/AbbVie, Axim, Bruder, Bausch + Lomb, Dompe, HanAll Biopharma, Kala Pharmaceuticals, Novartis, Osmotica/RVL, Oyster Point Pharma, Sight Sciences, Sun Pharma, Thea, Tarsus Pharmaceuticals, Topivert, and Visionology; reports grants from Allergan, Kala Pharmaceuticals, NIH, and TearScience; and has stock ownership in Alcon Vision/Tear Film Innovations, Axim, and Visionology. Todd C. Brady reports employment with, patent interests in, and stock ownership in Aldeyra Therapeutics, and reports stock ownership in F-Star Therapeutics and Evoke Pharma.
Compliance with Ethics Guidelines
The trial (ClinicalTrials.gov, NCT03660878) was performed in the USA in accordance with the Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Patients, the International Council for Harmonisation Guideline on Good Clinical Practice, and all applicable local regulatory requirements and laws. The trial was carried out with approval from an Institutional Review Board (Alpha IRB, San Clemente, CA, USA), informed consent was obtained from the patients, and the research followed Health Insurance Portability and Accountability Act regulations.
Data Availability
The datasets generated during and/or analyzed during the current clinical trial are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Cavanagh, B., Gomes, P.J., Starr, C.E. et al. Reproxalap Activity and Estimation of Clinically Relevant Thresholds for Ocular Itching and Redness in a Randomized Allergic Conjunctivitis Field Trial. Ophthalmol Ther 11, 1449–1461 (2022). https://doi.org/10.1007/s40123-022-00520-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00520-z