Abstract
Background
The enduring presence of COVID-19 and subsequent increasing incidence of COVID-19 reinfection has prompted evaluation of associated risk factors, particularly the role of immunosuppression.
Objective
The objective of this study was to characterize cases indicative of COVID-19 reinfection with respect to their reported use of immunosuppressant/immunomodulating agents.
Methods
This cross-sectional observational study leveraged the Pfizer global safety database (SDB) containing adverse event data collected in association with use of Pfizer products between 1 October 2019, and 30 June 2022. Selected Medical Dictionary for Drug Regulatory Activities (MedDRA®) Preferred Terms were used to identify COVID-19 cases; the search was further refined to comprise cases that subsequently reported events potentially indicative of COVID-19 reinfection.
Results
Of the cumulative total of 218,242 COVID-19 cases reported into the SDB, 4590 cases (2.1%) involving potential COVID-19 reinfection were identified. Of these 4590 cases of potential Covid-19 reinfection, a total of 134 cases reported COVID-19 specifically during treatment with pharmaceutical products, of which approximately 16% (21/134) of cases reported use of immunosuppressant/immunomodulating agents. Likewise, in the overall dataset (213,652 cases; excluding the 4590 cases involving potential COVID-19 recurrence), the percentage of reported immunosuppressant/immunomodulating agents was low (12%). In applying similar parameters to a dataset that excludes COVID-19 vaccine cases, 18% of cases reported use of immunosuppressant/immunomodulating agents (similar to the aforementioned 16% of cases reported from the overall total dataset that was inclusive of vaccine cases).
Conclusion
This pharmacovigilance study provides a characterization of cases indicative of COVID-19 reinfection with respect to reported use of immunosuppressant/immunomodulating agents. The observations generated from this cross-sectional observational analysis may prompt further research into the role of immunosuppression in COVID-19 reinfection, in an effort to better inform clinical practice and patient management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This study characterized COVID-19 reinfection cases with respect to their reported use of immunosuppressant/immunomodulating agents. |
Based on our findings, immunosuppressant/immunomodulating agents are reported in a relatively low percentage of cases that involved potential COVID-19 reinfection. |
The observations generated from this cross-section observational analysis may prompt further research into the role of immunosuppression in COVID-19 reinfection, in an effort to better inform clinical practice and patient management. |
1 Introduction
Immunosuppression generally poses an increased risk of COVID-19 infection (and reinfection thereafter), given the known association between viral infection and immunosuppressant use. To this point, in our previous published research [1], immunosuppressant agents were the most frequently reported pharmaceutical products among cases of COVID-19 infection/pneumonia. However, with evolving understanding of the disease, the relationship between immunosuppressant use and COVID-19 becomes somewhat conflicting and complex. While organizations such as the Centers for Disease Control and Prevention (CDC) [2] consider immunocompromised patients (and by extension, individuals with autoimmune conditions [3]) at increased risk of severe COVID-19 illness, this risk has been somewhat debated in the literature, with several reports suggesting that immunosuppressed patients may not exhibit excess COVID-19-associated vulnerability. For example, in one analysis that compared the incidence of COVID-19 and subsequent mortality in a large cohort of patients prescribed biologic agents versus matched controls, mortality rates were similar between the two groups (after adjusting for demographics, comorbidity burden, and local infection rates) [4]. In another retrospective cohort study, chronic use of immunosuppressive drugs was associated with neither worse nor better clinical outcomes among adults hospitalized with COVID-19 [5].
While the impact of immunosuppression on COVID-19 is still being questioned, the ubiquitous and enduring presence of COVID-19, and the consequent increasing incidence of COVID-19 reinfection, has prompted the medical community to examine epidemiologic characteristics and associated risk factors related more specifically to COVID-19 reinfection. Since August 2020, individual case reports and case series of COVID-19 reinfection have been reported globally. In one recent systematic case review [6], Wang et al. found that among 17 genetically confirmed COVID-19 reinfection cases, only one patient (5.8%) was immunocompromised. Given ongoing speculation surrounding the relationship between COVID-19 reinfection and associated risk factors such as immunosuppression, it would be relevant to contemplate the role of immunosuppression on COVID-19 reinfection to better inform clinical practice and patient management.
Upon the World Health Organization designating COVID-19 as a global pandemic on 11 March 2020 (and declaration of a national emergency in the USA on 13 March 2020), a COVID-19 surveillance program was urgently initiated by Pfizer on 16 March 2020, using data from the Pfizer safety database and routine pharmacovigilance. In an effort to provide some insight beyond sporadic literature case reports, a real-time standing cohort of COVID-19 cases potentially indicative of reinfection was established, based on which a cross-sectional observational study was conducted to characterize those COVID-19 reinfection cases with respect to available demographic information and reported use of immunosuppressant/immunomodulating agents.
2 Methodology
2.1 Pharmacovigilance Database
The Pfizer global safety database (SDB) is a dynamic, central repository for individual case safety reports (ICSRs) collected from all sources globally, and utilized for safety monitoring activities, regulatory reporting, and responses to product-related safety queries from regulatory authorities. The SDB contains cases of adverse events (AEs) reported in association with use of all Pfizer medicinal products. Annually, approximately one million cases are reported. Multiple sources are used for data collection (i.e., ICSRs) including published literature, marketing programs including nonclinical study programs, interventional and noninterventional studies (regardless of causality), business partners, patients, and health authorities.
2.2 Case Search and Identification
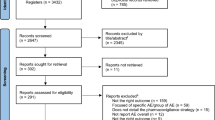
The SDB was searched retrospectively from 1 October 2019 through 30 June 2022 (based on initial safety receipt date of cases). COVID-19 cases were identified using Medical Dictionary for Regulatory Activities (MedDRA®; Version 25.0) Preferred Terms (PTs)Footnote 1,Footnote 2 specific to COVID-19 (reported as part of AEs, medical history, or indications).
Among the COVID-19 cases, the search was further refined to comprise cases that subsequently reported events potentially indicative of reinfection. To identify such cases, the following PTs were used: Disease recurrence, Symptom recurrence and Rebound effect, as well as the following MedDRA Lower Level Terms (LLTs): COVID-19 recurrent, COVID-19 reinfection and SARS-CoV-2 reinfection. As the majority of cases are spontaneously reported into the SDB, limited case details and associated lab results preclude definitive microbiological confirmation of reinfection. However, based on the employed search strategy, the relevant identified cases provided reasonable descriptive evidence of COVID-19 reinfection.
2.3 Methods and Analysis
The seriousness of each reported AE was determined by Pfizer physicians based on the International Council for Harmonisation guideline; AEs were assessed as serious if the event was considered medically important or had an adverse clinical course (e.g., death, life threatening, required hospitalization, prolonged hospitalization). Healthcare provider-reported cases were considered to be medically confirmed. The proportion of cases with reported use of immunosuppressant/immunomodulating agents is calculated by dividing the number of cases with potential COVID-19 reinfection and use of immunosuppressant/immunomodulating agents by the total number of cases of COVID-19 reinfection.Footnote 3 Furthermore, the percentage of potential COVID-19 reinfection cases reporting use of immunosuppressant/immunomodulating agents were also compared to those in the overall dataset (that excluded cases of COVID-19 reinfection). A Business Objects-based application was utilized to analyze the study data.
Immunosuppressant/immunomodulating agents were defined based on their pharmacologic activity involving targeting of any immune-related biological processes/cellular components.
Use of immunosuppressant/immunomodulating agents was further characterized by age groups and geographical regions. Additionally, subgroup analyses were conducted by limiting to cases that do not involve reporting of the COVID-19 vaccine, and those reported by healthcare professionals (known as medically confirmed cases).
3 Results
3.1 Overall Summary of Cases
Of the cumulative total of 218,242 COVID-19 cases reported into the SDB as of 30 June 2022, 4590 cases (2.1%) involving potential COVID-19 reinfection were identified. The 4590 cases involving potential COVID-19 reinfection retrieved from our SDB were reported from the USA (4147), the European Union (EU; 198), the UK (154), Namibia (88), UK-Northern Ireland (2), and European Economic Area (1). Within the EU, cases were reported from France (94), Germany (22), Italy (14), Netherlands (13), Greece (10), Spain (9), Sweden (8), Czech Republic (6), Austria, Belgium, Denmark, Estonia, Hungary (3 each), Poland, Romania (2 each), Finland, Portugal and Slovakia (1 each). Among cases where age was reported, the majority involved adults; pediatric cases (ages ≤ 17 years) and elderly cases (ages ≥ 65 years) represented < 1% (n = 11) and 29% (n = 1344) of all cases, respectively. The reported age ranges included 31–50 years (1443), 51–64 years (1218), 65–74 years (1056), ≥75 years (288), 18–30 years (227) and ≤ 17 years (11). In 347 cases, age was not provided. Of the 4590 cases, 56% (n = 2600) and 39% (n = 1783) involved female and male patients, respectively; sex was not reported in 207 cases.
Of these 4590 cases, 4032 cases reported COVID-19 PTs as part of events (AEs), while the remaining 558 cases reported COVID-19 PTs as part of other fields (e.g., indications, medical history). Among the 4032 cases that reported COVID-19 PTs as part of AEs, the vast majority (3913) of cases reported nonserious COVID-19-related events and the remaining 120 cases reported serious eventsFootnote 4 (with < 1% (N = 8) of cases reporting fatal COVID-19-associated outcomes). The eight fatal cases involved elderly patient (aged ≥ 65 years) who experienced fatal COVID-19 events, along with concurrent fatal complications (e.g., pneumonia/respiratory failure, cerebrovascular accident, coma, pulmonary embolism, renal insufficiency/failure). Of these eight cases, seven cases involved at-risk medical history (e.g., hypertension, cardiac disorders, diabetes mellitus, cerebrovascular infarction/accident, chronic obstructive pulmonary disease, obesity).
3.2 Use of Immunosuppressant/Immunomodulating Agents
Of the 4,590 cases of potential Covid-19 reinfection, a total of 134 cases reported COVID-19 reinfection (as part of AEs) specifically during treatment with pharmaceutical products for various indications. Within this dataset, the reported products were not utilized for COVID-19 treatment, but rather for concurrent conditions. Overall, approximately 16% (21/134) of these cases reported use of immunosuppressant/immunomodulating agents, generally employed for underlying autoimmune-related conditions or malignancies. The reported immunosuppressant/immunomodulating agents include adalimumab, arsenic trioxide, ciclosporin, cyclophosphamide, dexamethasone, etanercept, idarubicin, infliximab, methotrexate, ocrelizumab, risankizumab, rituximab, tofacitinib, upadacitinib and corticosteroids (e.g., prednisone, methylprednisolone, dexamethasone). Notably, while some of these agents (particularly corticosteroids) may also be utilized for treatment of COVID-19 and associated complications, the 134 cases referenced in this section exclude those agents that report COVID-19-specific indications.
Also of note, among cases that reported COVID-19 indications, the utilized treatments that were reported included Paxlovid, corticosteroids (excluding the aforementioned cases where these agents were used for other autoimmune-related indications), remdesivir, hydroxychloroquine, heparin, and antibiotics (e.g., azithromycin, amoxicillin, ceftriaxone, linezolid, piperacillin-tazobactam).
In comparison, within the overall dataset (of 213,652 COVID-19 cases) that excludes the 4590 cases involving potential Covid-19 reinfection, a total of 123,056 cases reported COVID-19 during treatment with pharmaceutical products, of which approximately 12% (14,408/123,056) reported use of immunosuppressant/immunomodulating agents.
When limiting the datasets to medically confirmed (MC) cases, of the cumulative total of 218,242 COVID-19 cases reported into the SDB, 119,604 were MC cases. Of the 4590 cases involving potential COVID-19 reinfection, 1293 were MC cases, of which a total of 50 MC cases reported COVID-19 specifically during treatment with pharmaceutical products. Of these 50 MC cases, 12% (6/50) reported use of immunosuppressant/immunomodulating agents. Additionally, in comparison, within the overall dataset that excludes the cases involving potential COVID-19 reinfection (118,311 MC cases/213,652 total cases), 90,064 MC cases reported COVID-19 during treatment with pharmaceutical products, of which approximately 8% (6879/90,064) reported use of immunosuppressant/immunomodulating agents.
In applying similar search parameters to a dataset that excluded cases involving the COVID-19 vaccine, a total of 34,076 COVID-19 cases were reported as of 30 June 2022, of which 17,152 cases reported COVID-19 during treatment with pharmaceutical products. Overall, 75% (12,851/17,152) of these cases reported use of immunosuppressant/immunomodulating agents. Of this cumulative total of 34,076 COVID-19 cases (excluding vaccine cases), 4225 cases involving potential COVID-19 reinfection were reported, of which a total of 83 cases reported COVID-19 during treatment with pharmaceutical products. Overall, 18% (15/83) of these cases reported use of immunosuppressant/immunomodulating agents (similar to the aforementioned 16% of cases reported from the overall total dataset that was inclusive of vaccine cases).
4 Discussion
Based on our findings, 2.1% of the cumulative total COVID-19 cases reported into the SDB involved potential COVID-19 reinfection. As a way of comparison, one retrospective cohort analysis of an entire population in an Italian region followed 1,293,941 subjects from the beginning of the pandemic to the current scenario of Omicron predominance (up to mid-February 2022) [7]. After an average of 277 days, 729 reinfections among 119,266 previously infected subjects (overall rate: 6.1%) were recorded.
Accordingly with our findings, immunosuppressant/immunomodulating agents are reported in a relatively low percentage (16%) of cases that involved potential COVID-19 reinfection. Likewise, in the overall dataset (213,652 COVID-19 cases; excluding the 4590 cases involving potential COVID-19 reinfection), the percentage of reported immunosuppressant/immunomodulating agents was also low (12%). However, it is possible that, since this dataset is inclusive of cases within the SDB that involved all Pfizer products (including the COVID-19 vaccine), reporting proportions of various products (including immunosuppressant/immunomodulating agents) are somewhat diluted by the high number of retrieved vaccine cases (given the proportionately high global rates of vaccine utilization).
Interestingly, in our previous published research [1], 65% of cases involved use of immunosuppressant/immunomodulating agents among cases that reported COVID-19 during treatment with pharmaceutical products. However, that dataset was significantly smaller (based on a total of 1508 cases reported as of 25 June 2020) and was exclusive of cases involving the COVID-19 vaccine. As detailed in our results, when applying similar parameters (excluding vaccine cases) to the more current dataset, 75% of these cases reported use of immunosuppressant/immunomodulating agents and, of those cases involving potential COVID-19 reinfection, 18% reported use of immunosuppressant/immunomodulating agents (similar to the aforementioned 16% of cases reported from the overall total dataset that was inclusive of vaccine cases).
The relatively low reporting of immunosuppressant/immunomodulating agents among cases involving potential COVID-19 reinfection appears to counter the general consideration of immunosuppression as a risk factor for increased susceptibility to infection (and by extension, reinfection). This finding is also contradictory to currently published literature, such as one systemic review [8] that identified immunosuppressive drugs as one of the commonly reported factors among cases of COVID-19 reinfection, and another review [9] that implicated non-selective immunosuppressive drugs (i.e., prednisolone) as a potential cause of COVID-19 recurrence (even upon initial clinical improvement).
Perhaps COVID-19 uniquely differs with respect to the currently known risk factors for viral reinfection, as earlier published case studies (albeit small in sample size) have already challenged [10,11,12,13,14] the notion of baseline immunosuppressive therapy worsening COVID-19 severity. In general, however, literature examining the impact of immunosuppressant use specifically on COVID-19 reinfection is relatively scarce. While our research may provide some insight into this issue, several limitations are inherent to spontaneous post-marketing AE reporting, including: under-reporting, particularly of non-serious cases; missing/lack of robust clinical information such as COVID-19 severity and associated lab results to confirm reinfection versus extension or relapse of the previous infection; unknown temporality between immunosuppressant use and reporting of COVID-19 reinfection; and limited information regarding treatment history prior to COVID-19 reinfection. Given these boundaries, it is beyond the scope of this cross-sectional observational study to draw correlations and appropriate conclusions. Nevertheless, perhaps our findings may encourage further research to better characterize the risks of COVID-19 reinfection, particularly given the increasingly endemic presence of this pathogen.
5 Conclusion
Of the cumulative total of 218,242 COVID-19 cases reported into the SDB, 4,590 cases (2.1%) involving potential COVID-19 reinfection were identified. Of these 4,590 cases of potential COVID-19 reinfection, a total of 134 cases reported COVID-19 specifically during treatment with pharmaceutical products, of which approximately 16% (21/134) of cases reported use of immunosuppressant/immunomodulating agents. Likewise, in the overall dataset (213,652 cases; excluding the 4590 cases involving potential COVID-19 reinfection), the percentage of reported immunosuppressant/immunomodulating agents was also low (12%). Albeit with several aforementioned limitations, this study is the first to utilize a spontaneous reporting safety database to document use of immunosuppressant/immunomodulating agents among cases of potential COVID-19 reinfection, and to perhaps challenge our understanding of expected risk factors for COVID-19 reinfection. Evidence-based clinical data associated with COVID-19-related reporting patterns and trends gathered via pharmacovigilance is paramount in contributing to patient treatment and safety. In this context, the additional information provided (beyond sporadically reported cases in the literature), as well as the hypothesis generated from this cross-sectional observational analysis, may prompt further research questions and activity into the role of immunosuppression in COVID-19 reinfection, in an effort to better inform clinical practice and patient management.
Notes
PTs Asymptomatic COVID-19, Coronavirus infection, Coronavirus test, Coronavirus test positive, COVID-19, COVID-19 pneumonia, COVID-19 prophylaxis, COVID-19 treatment, Exposure to SARS-CoV-2, Occupational exposure to SARS-CoV-2, SARS-CoV-2 antibody test, SARS-CoV-2 antibody test positive, SARS-CoV-2 carrier, SARS-CoV-2 sepsis, SARS-CoV-2 test, SARS-CoV-2 test false negative, SARS-CoV-2 test positive, SARS-CoV-2 viraemia, Suspected COVID-19, Congenital COVID-19, Post-acute COVID-19 syndrome, SARS-CoV-2 RNA decreased, SARS-CoV-2 RNA fluctuation, SARS-CoV-2 RNA increased, Vaccine derived SARS-CoV-2 infection and SARS-CoV-2 RNA.
In 2019 and partly in 2020, prior to implementation of an updated MedDRA® rerelease, historical cases were retrieved primarily using a text string search. These historical cases were continuously reviewed for follow-up information relevant to COVID-19 infections. Additionally, case-processing efforts to update the coding of cases that were reported to the safety database prior to the MedDRA® update (on 4 May 2020) were undertaken; as such, these historical cases currently include relevant COVID-19 terms, based on the currently updated MedDRA® version.
Among those cases reporting COVID-19 during treatment with pharmaceutical products and not involving COVID-19 treatment indications.
One case reported both serious and nonserious COVID-19 events.
References
Beyzarov E, Chen Y, Julg R, Naim K, Shah J, Gregory WW, Ayoub A, Caubel P. Global safety database summary of COVID-19-related drug utilization-safety surveillance: a sponsor’s perspective. Drug Saf. 2021;44(1):95–105. https://doi.org/10.1007/s40264-020-01035-x.
Centers for Disease Control and Prevention. CDC coronavirus disease 2019 (COVID-19): people with certain medical conditions. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html#:~:text=Like%20adults%2C%20children%20with%20obesity,very%20sick%20from%20COVID%2D19. Accessed 18 Jul 2022.
Tan EH, Sena AG, Prats-Uribe A, et al. COVID-19 in patients with autoimmune diseases: characteristics and outcomes in a multinational network of cohorts across three countries. Rheumatology (Oxford). 2021;60(SI):SI37–50.
Pahalyants V, Murphy WS, Klebanov N, et al. Immunosuppressive biologics did not increase the risk of COVID-19 or subsequent mortality: a retrospective matched cohort study from Massachusetts. J Am Acad Dermatol. 2022;86(1):252–5. https://doi.org/10.1016/j.jaad.2021.08.065.
Andersen KM, Mehta HB, Palamuttam N, et al. Association between chronic use of immunosuppresive drugs and clinical outcomes from coronavirus disease 2019 (COVID-19) hospitalization: a retrospective cohort study in a large US health system. Clin Infect Dis. 2021;73(11):e4124–30.
Wang J, Kaperak C, Sato T, Sakuraba A. COVID-19 reinfection: a rapid systematic review of case reports and case series. J Investig Med. 2021;69(6):1253–5.
Flacco ME, Soldato G, Acuti Martellucci C, Di Martino G, Carota R, Caponetti A, Manzoli L. Risk of SARS-CoV-2 reinfection 18 months after primary infection: population-level observational study. Front Public Health. 2022;2(10): 884121.
Sotoodeh Ghorbani S, Taherpour N, Bayat S, Ghajari H, Mohseni P, Hashemi Nazari SS. Epidemiologic characteristics of cases with reinfection, recurrence, and hospital readmission due to COVID-19: a systematic review and meta-analysis. J Med Virol. 2022;94(1):44–53. https://doi.org/10.1002/jmv.27281.
Piri SM, Edalatfar M, Shool S, Jalalian MN, Tavakolpour S. A systematic review on the recurrence of SARS-CoV-2 virus: frequency, risk factors, and possible explanations. Infect Dis (Lond). 2021;53(5):315–24.
Hsu JJ, Gaynor P, Kamath M, Fan A, Al-Saffar F, et al. COVID-19 in a high-risk dual heart and kidney transplant recipient. Am J Transplant. 2020;20:1911–5.
Jacobs J, Clark-Snustad K, Lee S. Case report of a SARS-CoV-2 infection in a patient with ulcerative colitis on tofacitinib. Inflamm Bowel Dis. 2020;26: e64.
Sharmeen S, Elghawy A, Zarlasht F, Yao Q. COVID-19 in rheumatic disease patients on immunosuppressive agents. Semin Arthritis Rheum. 2020;50:680–6.
Ning L, Liu L, Li W, Liu H, Wang J, Yao Z, et al. Novel coronavirus (SARS-CoV-2) infection in a renal transplant recipient: case report. Am J Transplant. 2020;20:1864–8.
Haberman R, Axelrad J, Chen A, Castillo R, Yan D, Izmirly P, et al. Covid-19 in immune-mediated inflammatory diseases: case series from New York. N Engl J Med. 2020;383:85–8.
Acknowledgements
The authors acknowledge the additional associated analyses provided by Rob F. Julg, Director Business Analyst, Pfizer Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by Pfizer Inc.
Conflicts of Interest
All authors are employees of Pfizer Inc and may hold stock or stock options.
Ethics Statement
The analyses for this study were conducted retrospectively using deidentified patient data; as such, this study was deemed exempt by the institutional review board and informed consent was not required.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Materials
Upon request, and subject to certain criteria, conditions and exceptions (see https://www.pfizer.com/science/clinical-trials/trial-data-and-results for more information), Pfizer will provide access to individual de-identified participant data from Pfizer-sponsored global interventional clinical studies conducted for medicines, vaccines and medical devices (1) for indications that have been approved in the US and/or EU or (2) in programs that have been terminated (i.e., development for all indications has been discontinued). Pfizer will also consider requests for the protocol, data dictionary, and statistical analysis plan. Data may be requested from Pfizer trials 24 months after study completion. The de-identified participant data will be made available to researchers whose proposals meet the research criteria and other conditions, and for which an exception does not apply, via a secure portal. To gain access, data requestors must enter into a data access agreement with Pfizer.
Code availability
No specific custom code was created for the study. We utilized an SAP Business Objects (Desktop Intelligence Version 12.6.2.1782) based application to analyze the study data. For more details, please contact the corresponding author.
Authors' contributions
All authors met the below criteria for authorship: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; and, drafting the work or revising it critically for important intellectual content; and, final approval of the version to be published; and, agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Beyzarov, E., Chen, Y. & Caubel, P. Reporting of COVID-19 Reinfection and Potential Role of Immunosuppressant/Immunomodulating Agents: A Cross-Sectional Observational Analysis Based on a Spontaneous Reporting Database. Clin Drug Investig 42, 807–812 (2022). https://doi.org/10.1007/s40261-022-01200-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-022-01200-3