Abstract
Background
Atherosclerotic cardiovascular diseases remain the primary cause of mortality in Italy. Individuals with a history of acute coronary syndrome, peripheral arterial disease, and ischemic stroke/transient ischemic attack face an elevated risk of recurrent major adverse cardiovascular events, including mortality. The population aging, coupled with increasing risk factors such as diabetes mellitus and obesity, exacerbates the disease’s economic impact.
Objectives
This study aims to comprehensively assess the economic burden of atherosclerotic cardiovascular diseases in Italy, specifically focusing on direct healthcare costs.
Methods
We analyzed real-world data from administrative databases in the Marche region and Local Health Unit Umbria 2. The economic burden of patients discharged with acute coronary syndrome, peripheral arterial disease, and ischemic stroke/transient ischemic attack was evaluated, with a focus on direct costs associated with hospitalizations, drugs, and outpatient visits. Results were stratified by age, sex, comorbidities at baseline, and adherence to lipid-lowering therapy and antihypertensive agents.
Results
Annually, nearly 350,000 patients were hospitalized for peripheral arterial disease, acute coronary syndrome, or ischemic stroke/transient ischemic attack. Direct health costs averaged €7190 per patient over a 2-year follow-up, with hospitalizations accounting for nearly 70% of the total. Male patients incurred significantly higher costs (€7467) than female patients (€6625). Costs correlated positively with age and with the number of baseline comorbidities, with a range from €5259 (0–1 comorbidities) to €17,095 (4+ comorbidities). Costs were significantly lower in adherent subjects (€6813) compared with non-adherent subjects (€7757).
Conclusions
This study provides valuable insights into the economic implications of atherosclerotic cardiovascular diseases in Italy, emphasizing the necessity of a comprehensive approach to preventive measures, optimal medication adherence, and lifestyle modifications to mitigate its impact.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Atherosclerotic cardiovascular diseases are the primary cause of death in Italy, with a significant socioeconomic burden. |
Direct costs are higher in multimorbid patients, while treatment adherence leads to a reduction in costs. |
Addressing the economic burden of acute coronary syndrome requires a comprehensive strategy encompassing prevention, optimal medication adherence, and lifestyle modifications. |
1 Introduction
Atherosclerosis is a chronic arterial disease and a major cause of vascular mortality. The disease has a latency of many years, its major clinical manifestations include ischemic stroke or transient ischemic attack (IS/TIA), acute coronary syndrome (ACS), and peripheral arterial disease (PAD) [1]. Atherosclerotic cardiovascular disease (ASCVD) is the leading cause of mortality in Italy: even in 2020, ACS and IS were the second and third leading causes of death (after COVID-19), responsible for approximately 117,868 deaths annually (19% of total mortality) [2]. Patients with a history of myocardial infarction, IS/TIA, or peripheral artery disease (PAD) are at very high risk of facing recurrent major adverse cardiovascular (CV) events, including myocardial infarction, stroke, and death [3]. These outcomes will affect 20% of patients within 1 year from the main event, 40% within 3 years [4, 5]. An aging population further threatens to sustain these high rates of myocardial infarction and CV diseases along with their associated adverse events, especially when considering that the prevalence of diabetes mellitus and obesity (both independent risk factors for CV, which affect one out of five adults) [6], has been increasing over the last 4 decades. Low-density lipoprotein-cholesterol (LDL-C) is considered a causal factor for ASCVD, and reductions in LDL-C are associated with a proportional reduction in the risk of CV events [7]. Lipid-lowering therapy plays a key role in secondary prevention in patients affected by ASCVD, with statin therapy being the first-line treatment for lowering LDL-C [8, 9].
If the target LDL-C is not reached with statins, combination therapy with ezetimibe and/or PCSK9 has been recommended by the 2023 European Society of Cardiology/European Atherosclerosis Society guidelines [10]. Previous studies showed ezetimibe to provide a further reduction in LDL-C levels when added to statin therapy, as well as a reduction in CV events [11,12,13]. When treating patients with ASCVD, the use of antihypertensive drugs has been proven to be efficient in controlling blood pressure, thus further reducing the risk of adverse CV outcomes [14, 15]. A fixed-dose combination therapy has been suggested to improve adherence and, consequently, attain blood pressure control in a reduced amount of time [10, 16].
In 2015, costs related to CV disease in Europe were equal to €210 billion, with healthcare costs accounting for 53% of it [6]. Knowledge on the economic burden of ASCVD in Europe and Italy is limited, with few studies trying to quantify the impact of this pathology. The aim of this study is to estimate the economic burden of ASCVD in Italy with respect to direct healthcare costs.
2 Material and Methods
2.1 Data Sources
This study was conducted using the Hospital Information System (Scheda di Dimissione Ospedaliera, SDO) for Italy as a whole (60 million inhabitants). Additional analyses were run only for the Local Health Unit (LHU) Umbria 2 and Marche region (1.8 million inhabitants).
2.1.1 Italian SDO
The Italian SDO records all hospital discharges, both ordinary and day hospital, from public and accredited hospitals. Each record contains, together with a patient-specific anonymous code, patient’s demographic (age, sex, residence), and clinical information (primary and up to five secondary diagnoses and procedures, Diagnosis-Related Group). Data were available for the period 2010–14.
2.1.2 LHU Umbria 2 and Marche
The LHU Umbria 2 and Marche Health Information System routinely collects information on hospitalizations, drug prescriptions, outpatient care, and laboratory tests for each patient registered in the Regional Health Care Assistance Registries (approximately 97% of residents). Each patient was identified in the Health Information System by an anonymous code that allowed deterministic linkage between the databases. Data were available for the period 2010–16 for LHU Umbria 2 and 2008–14 for the Marche region.
2.2 Methods
2.2.1 National Analysis
The study population was represented by all residents in Italy of age 18–100 years with at least one hospitalization for either ACS, IS/TIA, or PAD, discharged between 2010 and 2014. Hospital admissions (HAs) were identified through a list of Diagnosis Related Groups reported in Table S1 of the Electronic supplementary material (ESM). The number of patients, hospitalizations, and the average cost by patient were estimated by year. Results were stratified by diagnosis (ACS, IS/TIA, PAD).
2.2.2 LHU Umbria 2 and Marche Region Analysis
This analysis included all patients matching the following criteria:
-
age 18–100 years;
-
at least one hospitalization for either ACS, IS/TIA, or PAD, discharged between 2009 and 2012 (for the Marche region) or between 2011 and 2014 (for LHU Umbria 2);
-
at least one prescription of statins (ATC C10AA), ezetimibe alone (ATC C10AX09) or combined (ATC C10BA02, 05, 06), or Antihypertensives (ATC C02) within 180 days from the first hospitalization for a CV event (index event).
Patients were classified as either ACS, IS, or PAD based on the diagnosis associated with the first event that occurred.
Descriptive analyses were undertaken: patients were stratified by sex, age at index event, and number of comorbidities. Five macro-categories of comorbidities were considered:
-
malignant neoplasms;
-
diabetes;
-
diseases of the circulatory system;
-
chronic obstructive pulmonary disorder;
-
diseases of the kidney, liver, or pancreas.
Comorbidities were identified by searching for HAs and drug prescriptions during the 12 months preceding the index event (baseline). International Classification of Diseases, Ninth Revision, Clinical Modification and ATC (Anatomical Therapeutic Chemical) codes used for this analysis are reported in Table S2 of the ESM. The medication possession ratio (MPR) was used to estimate adherence to treatment (statins, ezetimibe alone or combined, antihypertensive drugs), and patients were classified as:
-
adherent (MPR > 80%);
-
partially adherent (40% ≤ MPR≤ 80%);
-
non-adherent (MPR < 40%).
A 2-year follow-up was defined for each patient. The first year was used to estimate adherence, while direct costs owing to hospitalizations, drugs, and outpatient visits were estimated for both years. Only patients alive at the end of the first year of follow-up were included in this analysis. Finally, by applying these costs to the number of patients estimated at the national level, total direct costs related to ASCVD were obtained.
The presence of statistically significant differences in log-costs between two groups was evaluated by the Z-score [17], while analysis of variance was used to compare differences between more than two populations [18]. All analyses were performed using R software version 4.1.
3 Results
3.1 National Analysis
During 2010–14, on average, every year almost 360,000 patients in Italy had at least one HA for PAD, ACS, or IS/TIA. The annual number of subjects with an HA related to PAD was 121,191, 142,494 patients experienced an HA for ACS, and 109,353 for IS/TIA (Fig. 1). Overall, a reduction in the number of patients was observed across time, equal to − 3.9% for PAD, − 1.8% for ACS, and − 20.6% for IS/TIA. The rate of re-hospitalization per patient within the year was constant across time (1.2 for PAD, 1.1 for both ACS and IS/TIA).
The annual cost related to HAs was around €2.2 billion (€5169 per hospitalization). The acute coronary syndrome cohort accounted for 47.8% (€7310 per patient) of it, followed by PAD (36.4%, €6546 per patient) and IS/TIA (15.8%, €3147 per patient, Fig. 2).
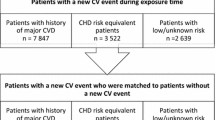
3.2 LHU Umbria 2 and Marche Region Analysis
A cohort of 20,898 patients with a history of PAD (19.5%), ACS (55.6%), or IS/TIA (24.9%) was included in the analysis. Two out of three patients were men, one out of three was in the 71–80 years of age group (Table 1). While in the PAD and ACS cohorts, subjects of age 71+ years represented half of the population, 70.8% of patients with IS/TIA belonged to this age category. Half of the subjects experienced one comorbidity, while only 1.6% of patients had four or more comorbidities, with values being consistent regardless of the diagnosis. Adherence rates were quite heterogeneous across groups: the highest proportion of adherent patients was found in the ACS population (64.8%), followed by PAD (52.8%) and IS/TIA (40.9%). The same was true for non-adherent patients, from 12.0% in the ACS group to 23.6% in the IS/TIA group.
From the regional analysis, direct health costs equal to €7190 per patient were estimated during 2 years of follow-up (index HA excluded). Expense was higher in patients with PAD (€8532), followed by ACS (€7623) and IS/TIA (€5172, Fig. 3). Hospitalizations accounted for almost 70% of the costs, the second most relevant voice being drugs (19%, with statins and antihypertensives representing around 40% of it), followed by outpatient visits. These percentages were quite consistent regardless of the pathology group.
Costs stratified by sex, age category, and number of comorbidities during baseline are reported in Fig. 4. A significantly higher cost was associated with male patients (€7467) with respect to female patients (€6625 Z-score = 6.574, p < 0.001). The difference was mainly explained by costs related to HAs (75.6%, p = 0.001), followed by outpatient visits (10.8%, p < 0.001). A positive correlation was observed between costs and age up until the age group 71–80 years, with a major reduction in expense in patients aged over 80 years: the same trend was observed for HAs, other drugs, and outpatient visits, while costs related to statins and antihypertensives decreased steadily with increasing age (€612 in age group 18–60 years, €380 in age group 81+ years). Differences in costs by age category were statistically significant (F-score 68.21, p < 0.001), the result was confirmed when considering specific voices of expense, with the exception of outpatient visits (F-score = 1.22, p = 0.269). The main driver of this difference was the expense related to HAs: costs literally doubled up from patients with 0–1 comorbidities (€3363) to patients with 2–3 comorbidities (€6562) and those with 4+ comorbidities (€13,974). A similar trend was observed for outpatient visits, while costs related to drugs were quite similar. When considering the number of comorbidities, all differences were statistically significant. Presence of comorbidities at baseline was associated with higher costs. Finally, lower costs were estimated in subjects who were adherent to treatment. The average expense along the 2-year follow-up was equal to €7757 in non-adherent patients, €7635 in partially adherent patients, and €6814 in fully adherent patients (p < 0.001). Costs stratified by two factors at a time are reported in Tables S3–S8 of the ESM. The increase in costs with the number of comorbidities was much steeper when considering young people, while almost no difference was observed in patients aged over 80 years. Apart from that, results were consistent with univariate distributions.
The index HA cost on average was €6176, with a high heterogeneity between population subgroups: costs were lower in female patients, in elderly patients, and in patients with a higher number of comorbidities, while a positive relationship was observed with MPR levels (Table 2). During the 2-year follow-up, the expense was equal to €7190, with the first year accounting for 64% of the amount (this result was consistent regardless of population strata). Furthermore, the differences in costs previously described were constant across the years of follow-up. Overall, when considering both the index event and follow-up, mean costs per patient reached €13,366.
3.3 National Extrapolation
The estimate of direct costs obtained at the regional level was multiplied by the mean annual number of incident patients estimated across Italy. Total direct health costs amounted to €4.9 billion, with the ACS cohort accounting for 2.1 billion, followed by PAD (€1.9 billion) and IS/TIA (€0.9 billion, Fig. 5). Costs associated with the index event were €2.2 billion, while follow-up related costs represented 61.1% of the total. Hospital admissions (both index event and during the follow-up) accounted for 83.6% of total costs, followed by drugs (9.8%) and outpatient visits (6.6%).
4 Discussion
The present study aimed to estimate the economic burden of ASCVD in Italy, specifically focusing on the direct healthcare costs associated with the disease. The findings of the study revealed important insights into the economic burden of ASCVD in Italy. The national analysis showed that, on average, nearly 350,000 patients had at least one hospitalization related to ACS, IS/TIA, or PAD each year. Although there was a decrease in the number of patients over time, the annual costs associated with hospitalizations remained substantial, amounting to approximately €2.1 billion per year. Acute coronary syndrome accounted for the highest proportion of costs (47.6%), followed by PAD (37.3%) and IS/TIA (15.1%). These results highlight the significant financial impact of ASCVD on the healthcare system in Italy. The negative trend in the number of HAs is consistent with results from other studies on CV diseases [19].
In addition to the national analysis, a regional analysis was conducted to provide a more detailed understanding of the economic burden within specific areas. Direct healthcare costs per patient during a 2-year follow-up period were estimated to be around €7190. Peripheral arterial disease was associated with the highest costs per patient (€8532), followed by ACS (€7623) and IS/TIA (€5172). Hospitalizations accounted for the majority of costs (approximately 70%), followed by drug expenses and outpatient visits. A similar study conducted in Europe in 2012 estimated average annual direct costs of €2772 over a 5-year follow-up period [20]. Consistently with our results, hospitalizations accounted for 74.2% of the costs, followed by drugs (15.2%) and outpatient visits (10.7%).
The study also examined the influence of demographic and clinical factors on costs. Male patients were found to have significantly higher costs compared with female patients, primarily driven by expenses related to hospitalizations and outpatient visits. Age was positively correlated with costs up until the 71–80 years of age group, after which there was a reduction in expenses. Comorbidities were associated with higher costs, primarily driven by hospitalization expenses. The presence of multiple comorbidities significantly increased the costs of managing ASCVD. Additionally, adherence to treatment was associated with lower costs, highlighting the importance of medication adherence in reducing healthcare expenditures. An average cost of €7635 was estimated in non-adherent patients, +10.7% with respect to adherent patients. Other studies proved that adherence to antihypertensive treatment was associated with a lower healthcare utilization [21, 22]. The same pattern has been observed with statins: a study based on a large cohort of US citizens reported a reduction in total costs per patient during a 1-year period equal to almost $2000 [23].
The extrapolation of regional-level cost estimates to the national level revealed a staggering economic burden of ASCVD in Italy, with total direct healthcare costs amounting to approximately €4.8 billion. Acute coronary syndrome accounted for the highest proportion of costs (€2.1 billion), followed by PAD (€1.9 billion) and IS/TIA (€0.8 billion). Hospitalizations, including both index events and follow-up hospitalizations, represented the largest component of total costs (83.6%), underscoring the significant financial impact of ASCVD-related hospital admissions.
It is important to acknowledge certain limitations of this study. The analysis focused solely on direct healthcare costs and did not consider indirect costs, such as productivity losses or the impact on the broader economy. Furthermore, the study relied on administrative healthcare databases, which may have limitations in terms of data accuracy and completeness. Administrative data sources are designed for accounting and billing purposes. Therefore, this dataset only includes data considered relevant for accounting purposes, while information relevant to our scope could be missing. However, to date, there are no specific epidemiological registries for measuring clinical outcomes and costs of patients with CV disease in Italy; thus, administrative sources remain the best possible alternative for tracking patients’ health care resource utilization within the Italian setting. Second, the Marche and Umbria 2 regions account for 3.1% of the total population of Italy and so the results described here may not be representative of event rates for the entire country. Yet, representativeness of this dataset has already been proven elsewhere [24].
5 Conclusions
The findings of this study provide valuable insights into the economic burden of ASCVD in Italy and underscore the need for effective management and prevention strategies to mitigate the financial impact of the disease. Given the high costs associated with hospitalizations, efforts should be directed towards implementing preventive measures, optimizing medication adherence, and promoting lifestyle modifications to reduce the occurrence of ASCVD-related events. Additionally, targeted interventions to address comorbidities and promote better disease management may help alleviate the economic burden associated with ASCVD.
References
Herrington W, Lacey B, Sherliker P, Armitage J, Lewington S. Epidemiology of atherosclerosis and the potential to reduce the global burden of atherothrombotic disease. Circ Res. 2016;118(4):535–46.
OECD/European Observatory on Health Systems and Policies (2023), Italy: Country Health Profile 2023, State of Health in the EU, OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels.
Tangri N, Ferguson TW, Whitlock RH, Rigatto C, Jassal DS, Kass M, et al. Long term health outcomes in patients with a history of myocardial infarction: a population based cohort study. PLoS One. 2017;12(7):e0180010.
Jokhadar M, Jacobsen SJ, Reeder GS, Weston SA, Roger VL. Sudden death and recurrent ischemic events after myocardial infarction in the community. Am J Epidemiol. 2004;159(11):1040–6.
Bhatt DL, Eagle KA, Ohman EM, Hirsch AT, Goto S, Mahoney EM, et al. Comparative determinants of 4-year cardiovascular event rates in stable outpatients at risk of or with atherothrombosis. JAMA. 2010;304(12):1350–7.
Timmis A, Vardas P, Townsend N, Torbica A, Katus H, De Smedt D, et al. European Society of Cardiology: cardiovascular disease statistics 2021. Eur Heart J. 2022;43(8):716–99.
Silverman MG, Ference BA, Im K, Wiviott SD, Giugliano RP, Grundy SM, et al. Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: a systematic review and meta-analysis. JAMA. 2016;316(12):1289–97.
Nordestgaard BG, Chapman MJ, Humphries SE, Ginsberg HN, Masana L, Descamps OS, et al. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease. Eur Heart J. 2013;34(45):3478-90a.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111–88.
Marx N, Federici M, Schütt K, Müller-Wieland D, Ajjan RA, Antunes MJ, et al. 2023 ESC guidelines for the management of cardiovascular disease in patients with diabetes. Eur Heart J. 2023;44(39):4043–140.
Cannon CP, Blazing MA, Giugliano RP, McCagg A, White JA, Theroux P, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015;372(25):2387–97.
Morrone D, Weintraub WS, Toth PP, Hanson ME, Lowe RS, Lin J, et al. Lipid-altering efficacy of ezetimibe plus statin and statin monotherapy and identification of factors associated with treatment response: a pooled analysis of over 21,000 subjects from 27 clinical trials. Atherosclerosis. 2012;223(2):251–61.
Catapano A, Toth PP, Tomassini JE, Tershakovec AM. The efficacy and safety of ezetimibe coadministered with statin therapy in various patient groups. Clin Lipidol. 2013;58(8):746–55.
Lamprea-Montealegre JA, Zelnick LR, Hall YN, Bansal N, De Boer IH. Prevalence of hypertension and cardiovascular risk according to blood pressure thresholds used for diagnosis. Hypertension. 2018;72(3):602–9.
Alborzi A, Attar A, Sayadi M, Nouri F. The effects of intensive blood pressure control on cardiovascular outcomes based on 10-year ASCVD risk score: an analysis of a clinical trial. Cardiol Res Pract. 2021;2021:6635345.
Bahiru E, de Cates AN, Farr MRB, Jarvis MC, Palla M, Rees K, et al. Fixed-dose combination therapy for the prevention of atherosclerotic cardiovascular diseases. Cochrane Database Syst Rev. 2017;3(3):CD009868.
Zhou XH, Melfi CA, Hui SL. Methods for comparison of cost data. Ann Intern Med. 1997;127(8 Pt 2):752–6.
Chambers JM, Freeny AE, Heiberger RM. Analysis of variance; designed experiments. Statistical Models in S. 2017.
Cortesi PA, Fornari C, Madotto F, Conti S, Naghavi M, Bikbov B, et al. Trends in cardiovascular diseases burden and vascular risk factors in Italy: the Global Burden of Disease study 1990–2017. Eur J Prev Cardiol. 2021;28(4):385–96.
Carlsson K, Nilsson K, Wolden ML, Faurby M. Economic burden of atherosclerotic cardiovascular disease: costs related to healthcare and loss of productivity; a matched case-control study in more than 450,000 Swedish individuals. BMC Cardiovasc Disord. 2023;23(1):483.
Bailey JE, Wan JY, Tang J, Ghani MA, Cushman WC. Antihypertensive medication adherence, ambulatory visits, and risk of stroke and death. J Gen Intern Med. 2010;25(6):495–503.
Osterberg L, Blaschke T. Drug therapy: adherence to medication. N Engl J Med. 2005;353(5):487–97.
Axon DR, Vaffis S, Chinthammit C, Lott BE, Taylor AM, Pickering M, et al. Assessing the association between medication adherence, as defined in quality measures, and disease-state control, health care utilization, and costs in a retrospective database analysis of Medicare supplemental beneficiaries using statin medications. J Manag Care Spec Pharm. 2020;26(12):1529–37.
Sciattella P, Maggioni AP, Arcangeli E, Sidelnikov E, Kahangire DA, Mennini FS. Healthcare resource utilization, cardiovascular event rate and use of lipid-lowering therapies in secondary prevention of ASCVD in hospitalized patients in Italy. Adv Ther. 2022;39(1):314–27.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open access funding provided by Università degli Studi di Roma Tor Vergata within the CRUI-CARE Agreement. This study was funded by Servier Group Italy. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflicts of Interest
Francesco S. Mennini, Matteo Scortichini, Paolo Sciattella, and Furio Colivicchi have no relevant financial or non-financial interests to disclose. Aldo P. Maggioni received personal fees for participating in committees of studies supported by Bayer, AstraZeneca, Novartis, and Sanofi outside the present work.
Ethics Approval
According to the rules from the Italian Medicines Agency (available at https://www.aifa.gov.it/documents/20142/0/DETERMINAZ_AIFA_20_Marzo_2008_ST_OSS.pdf), retrospective studies using administrative databases do not require Ethics Committee protocol approval.
Consent to Participate
According to the General Authorization for the Processing of Personal Data for Scientific Research Purposes issued by the Italian Privacy Authority on 10 August, 2018 (available at www.garanteprivacy.it/web/guest/home/docweb/-/docweb-display/docweb/9124510), this study was exempt from informed consent.
Consent for Publication
Not applicable.
Availability of Data and Material
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request and with permission of the Marche region and LHU Umbria 2.
Code Availability
The R code is available from the corresponding author on reasonable request.
Authors’ Contributions
All authors contributed to the study conception. PS and FSM developed the study design, PS and MS conducted the statistical analysis and derived the analytical results. The first draft of the manuscript was written by MS and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Mennini, F.S., Scortichini, M., Colivicchi, F. et al. The Economic Burden of Atherosclerotic Cardiovascular Disease in Italy. Clin Drug Investig (2024). https://doi.org/10.1007/s40261-024-01365-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s40261-024-01365-z