Abstract
The life shortening nature of Friedreich Ataxia (FRDA) demands the search for therapies that can delay, stop or reverse its relentless trajectory. This review provides a contemporary position of drug and gene therapies for FRDA currently in phase 1 clinical trials and beyond. Despite significant scientific advances in the specificity of both compounds and targets developed and investigated, challenges remain for the advancement of treatments in a limited recruitment population. Currently therapies focus on reducing oxidative stress and improving mitochondrial function, modulating frataxin controlled metabolic pathways and gene replacement and editing. Approval of omaveloxolone, the first treatment for individuals with FRDA aged 16 years and over, has created much excitement for both those living with FRDA and those that care for them. The process of approval of omaveloxolone by the US Food and Drug Administration highlighted the importance of sensitive outcome measures and the significant role of data from natural history studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The search for therapies that could stop, delay or reverse the relentless trajectory of Friedreich ataxia continues, with new compounds currently in clinical trials or under consideration for new clinical trials. |
There is currently one approved treatment for Friedreich ataxia, (Omaveloxolone [Skyclarys™]) with a number of phase 1 and beyond drug and gene therapy clinical trials underway. |
The approval of Omaveloxolone (Skyclarys™) highlighted the importance of natural history studies in the evaluation of clinical trials. |
1 Introduction
Friedreich ataxia (FRDA) is one of the most common inherited ataxias affecting approximately 1:40,000 individuals in predominantly European populations [1, 2]. FRDA was first described by Nikolaus Friedreich, Professor of Medicine in Heidelberg, Germany, in 1863 as a distinct clinical syndrome characterised by ataxia that affected several progeny of unaffected parents [3]. Since the discovery of the genetic basis of FRDA in 1996 by Campuzano and colleagues, molecular diagnosis of affected individuals and heterozygous carriers has been possible [4].
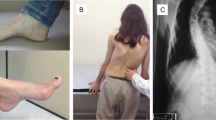
Onset of either neurological or non-neurological symptoms occurs on average between 10 and 15 years [5]. FRDA is a disease that effects multiple systems, at times in a diverse trajectory both in terms of severity and phenotype. Neurological symptoms include progressive axial and appendicular ataxia, loss of deep tendon reflexes, myopathy, spasticity, dysarthria and sensory (particularly vibration and proprioceptive) loss [6]. In addition, FRDA results in an abnormal auditory brainstem response, saccadic intrusions, optic atrophy, decreased vestibulo-ocular and vestibulospinal responses and auditory impairment [6, 7]. Non-neurological symptoms include increased rates of diabetes mellitis, depression, urinary tract morbidity, scoliosis, pes cavus, fatigue and cardiomyopathy [8]. A mixed cerebellar and sensory gait ataxia results in a broad-based ataxic gait associated with frequent falls. The relentlessly progressive nature of FRDA renders an affected person with typical onset FRDA unable to ambulate and thus dependent on a wheelchair for mobility on average 11.5 years after symptom onset [9]. Moreover, 49% of diagnosed individuals with FRDA are non-ambulant following a sequential loss of specific functions including balance and upright stability [10, 11]. Upper limb dysmetria is an early sign of FRDA and progresses well beyond loss of ambulation continuing to make a profound impact on daily activity and quality of life. FRDA is life-shortening and individuals with typical onset succumb to the disease on average at 39 years with arrhythmias, an advanced stage of neurological disability and diabetes mellitus being independent predictors of survival [12].
Herein we present a review of the available efficacy, safety and tolerability data for approved and investigational drugs and gene therapies for FRDA. We commence with an overview of the genetics of FRDA, the role of frataxin, pathophysiology, an overview of clinical outcome measures and the view of the person living with FRDA. Given the many published reviews in this area, the focus of this review will be to present a contemporary position on drug and gene therapies currently in phase 1 trials through to approval.
1.1 Overview of the Genetics of FRDA and the Role of Frataxin
FRDA is an autosomal recessive condition resulting from biallelic pathogenic variants in the FXN gene [13]. In 96% of affected individuals, FRDA results from homozygosity for an expanded GAA triplet-repeat sequence in intron 1 of the gene, ranging from 56 to 1300 repeats [1, 14]. Unaffected chromosomes contain a range of GAA repeats from 6 to 26 [15]. Carriers of one expanded allele are clinically healthy despite having lower frataxin levels than non-carriers [4]. The expanded GAA triplet-repeat sequence is responsible for reduced levels of structurally normal frataxin, considered the main protagonist in the pathology of FRDA [14]. The remaining 4% of affected individuals are heterozygous for an expanded GAA repeat and a point/insertion/deletion pathogenic variant responsible for aberrations in frataxin structure and function [14]. There is a report of three siblings homozygous for a point mutation in FXN [16].
The FXN gene encodes frataxin, a protein of 210 amino acids processed to maturity by the mitochondrial peptidase-β [17]. Frataxin is located in the mitochondria and plays a key role in the biogenesis of iron–sulfur (Fe–S) clusters, iron and heme regulation and sensitivity to oxidative stress [4, 17, 18]. Understanding the role and mode of action for frataxin continues to present challenges [19]. Frataxin is highly expressed in mitochondrial-rich tissues such as neurons (dorsal root ganglia, dentate nuclei, spinocerebellar and corticospinal tracts), muscle, heart, pancreas and liver [4, 20]. Hence, it is unsurprising that these regions are vulnerable to a reduction in functional frataxin (see Schmucker and Puccio for a review of the function of frataxin [21]).
Individuals with FRDA due to homozygous GAA expansions produce between 4% and 29% of usual levels of structurally and functionally normal frataxin [4, 22]. Carriers of one expanded allele produce between 40% and 68% of usual levels and this amount is sufficient for carriers to remain unaffected [22]. Studies of several different organisms have demonstrated the metabolic functions regulated by frataxin are fundamental to normal cellular health and development [20]. Reduced frataxin in affected individuals eventually causes cell death as evident by neural die back and cardiomyocyte mitochondrial dysfunction [23, 24]. The inverse relationship between the amount of residual frataxin and the size of the GAA repeat expansion is reflected by earlier age of onset and greater phenotypic severity associated with a larger expansion of GAA1, the smaller of the two expanded alleles [25, 26]. However, the size of GAA1 has been found to be associated with approximately only 47% of variability in age at disease onset, neurological and/or cardiac severity [20, 27,28,29]. Other factors such as environmental and genetic influences contribute, however, are yet to be fully understood [30]. For example, in a recent study, Rodden and colleagues explored the role of histone deacetylase (HDAC) and sirtuin (SIRT) variants on the expression of FRDA [31] confirming the influence of the CT SIRT6 genotype at the SNP (single nucleotide polymorphism) rs352493 locus in mitigating disease severity, despite the mechanism remaining unclear [31]. About 15% of affected individuals experience ‘delayed onset FRDA’ (late onset FRDA (LOFA) and very late onset FRDA (VLOFA) [32]. LOFA is defined as onset between 25 and 29 years, and VLOFA is defined as onset at 30 years and beyond. Such individuals have, on average, smaller GAA1 alleles than those with typical (< 25 years) onset [33] with associated phenotypical, progression and severity differences presumably related to the presence of greater residual frataxin than those with typical onset [32].
1.2 Pathology
As reflected by the clinical signs in FRDA, the major sites of pathology include the dorsal root ganglia (DRG) and posterior columns of the spinal cord, spinocerebellar tracts, corticospinal tracts, dentate nuclei of the cerebellum and the heart [34, 35]. Loss of DRG neurons is apparent as hypoplasia rather than atrophy, alluding to the neurodevelopmental impact of emerging FRDA [36] as well as progressive neuronal loss [37]. A reduction in DRG neurons and thinning of dorsal root fibres interferes with myelination of sensory nerves providing the physiological explanation for the disabling and, at times, painful sensory neuropathy associated with FRDA [38]. In addition, loss of DRG neurons and secondary gliosis contribute to impeded development of dorsal spinocerebellar tracts [37, 39]. The combined lack of fibres in the dorsal columns (DC) and dorsal spinocerebellar tracts is apparent on magnetic resonance imaging (MRI) by a progressive reduction in spinal cord cross sectional area [40].
Notwithstanding the role of DRG, spinocerebellar tract and cortical pathology, cerebellar pathology particularly that of the dentate nuclei, appears to be the main protagonist in the neurological sequalae of FRDA. Specifically, loss of neurons in the dentate nuclei coincides with the appearance of cerebellar signs and progresses in line with disease severity [41]. Death of large glutamatergic projection neurons and grumose reaction (proliferation of synaptic terminals) of Purkinje cells secondary to iron dysmetabolism appear to be the main drivers of dentate nuclei (DN) atrophy [37, 41]. Recent studies have also pointed to the role of inflammation in the pathophysiological process of neural dysfunction (see Apollini et al. 2022 for review) [42] suggesting modulating neuroinflammation as a potential therapeutic target [43]. Additional neural structures implicated in FRDA include the thalamus, brain stem and pontine nuclei (see Harding et al. for review) [38]. In terms of considering therapeutic targets, it is important to consider the changing nature of neuropathology over the course of the disease due to not only a result of primary pathophysiology but also a result of secondary compensatory mechanisms [44].
An increase in relative wall thickness (RWT) and age-normalised RWT is the hallmark cardiac abnormality in FRDA [24, 45]. Specifically, cardiac remodelling is apparent by an increase in left ventricular (LV) wall thickness and reduction in LV chamber size that may precede reduced LV ejection fraction and increased LV size [45]. Cardiac structure remodelling is a result of cellular changes including cardiomyocyte hypertrophy, focal degeneration of muscle fibres, necrosis and interstitial fibrosis [46].
1.3 Measurement of FRDA in Clinical Trials
The search for therapies that could stop, delay or reverse the relentless trajectory of FRDA continues, with new compounds currently or under consideration in clinical trials or are already commercially available and approved for other diseases. However, many questions pertinent to the design of clinical trials remain unanswered. Specifically, how to measure clinically important changes as a consequence of a therapy, how to measure the impact of FRDA in children and how to accommodate phenotypic and stage of disease diversity in FRDA in clinical trial design. Clinical trials are only as good as their measures and until these questions can be resolved, interpreting the results of clinical trials will continue to be compromised.
The central feature of the neurological phenotype of FRDA is ataxia, manifesting in a range of systems including appendicular and axial movement and speech. Ataxia is a direct result of the molecular and pathological impact of FRDA. Thus, mitigation of ataxia is seen as the surrogate measure of efficacy in clinical trials. It is important to note however that the onset of symptoms such as ataxia signifies the loss of specific cells (such as neurons) due to reduced frataxin. We still do not fully understand the events that occur prior to the onset of symptoms and in particular how much compensatory processes mask the emergence of symptoms.
Clinical rating scales such as the Friedreich’s Ataxia Rating Scale [47, 48], the modified FARS (mFARS) [49] and the Scale for the Assessment and Rating of Ataxia (SARA) [50] have been validated as clinical measures of neurological function in FRDA. These scales, usually administered in the clinic, are weighted towards gait and balance. Accordingly, they are most sensitive to change in the first 25 years of the disease trajectory while an affected person remains ambulant [9] and, importantly, depend on detecting neurological impairment to measure disease severity. On average, neurological disease progression in ambulant individuals with FRDA is reflected by an increase in the mFARS score of 3.14 per annum [10]. However, as previously noted, at any given time 33–49% of individuals with FRDA are non-ambulant. It is unsurprising that many clinical trials are focussed on individuals in the earlier stages of the disease trajectory when the sensitivity of the outcome measure is at its greatest; however, the question remains as to whether results from individuals in a specific disease stage are translatable to other stages of the disease. It is also unclear how much cerebellar dysfunction, pathological changes in DRG, spinocerebellar tracts, corticospinal tracts and secondary compensation contribute to performance on clinical rating scales. Moreover, clinical rating scales are a snapshot of one point in time and may provide limited insight into the person’s real-world capacity and function outside of the clinic. Despite their limitations, clinical rating scales continue to be the neurological outcome measure of choice for clinical trials in FRDA. Rummey and colleagues provided an excellent framework to accommodate the diversity apparent in the FRDA population, particularly with stratification of patients based on age and ambulation status [10].
In addition to clinical rating scales there are a range of performance-based and patient-reported outcome measures. Efforts to mitigate the noise of less sensitive or inconsistent measurement and to address the issue of primary deficit versus compensation have also led to the development of a range of instrumented and digital outcome measures [51, 52].
Review of the literature regarding neuroimaging markers in FRDA reveals a range of tantalising possible outcome measures using magnetic resonance imaging (MRI) including structural and diffusivity measures of brain and spinal cord, and intra-cerebral and cerebello-cerebral connectivity [44, 53,54,55,56,57], iron accumulation in the brain (using quantitative susceptibility mapping [QSM]) [58, 59] and spinal cord biochemistry (using magnetic resonance spectroscopy [MRS]) [60]. Efforts to refine and validate potential neuroimaging biomarkers of FRDA progression are currently underway via a longitudinal, multi-site and multi-modal neuroimaging natural history study [61].
Measuring the impact of FRDA on the heart also presents challenges. There is some natural history data [62, 63]; however, there are limited data about the histological changes in the LV myocardium during the early stages of the disease process to guide both choice of intervention and outcome measurement [24]. Moreover, the lack of consistency in both terminology, cardiac biomarkers and prognostic end points makes design of clinical trials challenging [24, 64]. Standard echocardiography continues to be recommended for identifying individuals with FRDA at risk of developing cardiac morbidity [51] however advances in cardiac imaging and techniques to quantify gene expression and function in the heart have assisted to improve cardiac outcomes for clinical trials.
There are four trials described in this review that include children in their cohort. Given the desire to include children in clinical trials, understanding the unique challenges of measurement of FRDA in children is a current focus of attention for the research community [65]. Specifically, performance on clinical measures such as the mFARS or SARA in children aged 12 years and under may be compounded by the normal process of maturation of the cerebellum in this age group [66] interacting with the emergence of ataxia related to FRDA. It is yet to be established if the FARS and mFARS score can accommodate the normal variability in age related motor control. Moreover, issues related to concurrent maturation of cognitive (including attentional) control as well as capacity to cooperate with a clinical exam compounds accurate assessment. These factors may affect the sensitivity in detecting ataxia and measuring its rate of change when ataxia is first emerging, reducing its value as an index of disease progression or therapeutic intervention. It is important that studies separate children and adults in analysis and that paediatric trials use outcome measures that are validated in children with FRDA [65].
Biochemical outcomes include measuring frataxin protein and frataxin mRNA in peripheral blood mononuclear cells, buccal cells, whole blood and lymphocytes; urinary 8-hydroxy-2ʹ-deoxyguanosin, dihydroxybenzoic acid serum, peroxides and plasma F2-isoprostanes (see Gavriilaki and colleagues, 2023 for a recent systematic review of clinical, cardiac, biochemical, patient-reported outcome measures, imaging and neurophysiologic biomarkers in FRDA clinical trials) [67].
1.4 What Outcomes are Important to Individuals Living with FRDA?
In recognising the importance of the patient experience and voice in the design, development and administration of clinical trials, the US Food and Drug Administration (FDA) has provided guidance on patient focussed drug development [68]. In 2017, four FRDA patient advocacy organizations hosted an externally led Patient Focused Drug Development Meeting from which a summary report of FRDA patient perspectives was developed titled, ‘The Voice of the Patient’ [69]. More recently, studies exploring the views of individuals living with FRDA have indicated their clear preference for therapies that target neurological symptoms such as speech, balance and mobility [70,71,72]. In addition, individuals with FRDA have indicated their preferences may change depending on the stage of the disease they are at [71]. It is crucial that outcome measures used in clinical trials both reflect what is important to the lived experience of FRDA but also include measures specific to varying stages of the condition (for example ambulant versus non-ambulant) [73].
The life shortening nature of FRDA demands the search for therapies that can delay, stop or reverse the relentless trajectory of FRDA, with novel compounds currently in clinical trials or under consideration in new clinical trials. Currently research is focused on novel compounds specifically for FRDA as well as those already commercially available and approved for other diseases. Given the current knowledge of FRDA and using the framework provided by the Friedreich’s Ataxia Research Alliance (FARA) Research Pipeline [74], we aim to review therapies according to status in terms of approval and thereafter their mode of action as follows: (1) compounds approved for use in FRDA, (2) compounds that reduce oxidative stress and improve mitochondrial function, (3) compounds that modulate frataxin controlled metabolic pathways and (4) gene replacement and editing.
2 Search Strategy
Rapid review was utilised using the Ovid MEDLINE and PubMed search engines. Search terms included Friedreich ataxia, Friedreich’s ataxia, antioxidants, frataxin, oxidative stress, mitochondrial function, gene editing and gene replacement. We also included previous review articles and reviewed references in these articles as well as searching https://clinicaltrials.gov. The FARA Drug Development Pipeline [74] was also accessed. Searches were limited to humans, clinical trials, reviews and meta-analyses. Only agents currently in Phase 1 trials and beyond were included. The initial search was conducted in March and again in June 2024.
3 New and Emerging Drug Therapies for FRDA
3.1 Approved Medication for FRDA
3.1.1 Omaveloxolone (Skyclarys™)
Omaveloxolone (brand name Skyclarys™) was approved by the FDA in February 2023 for the treatment of FRDA in adults and adolescents aged 16 years and older [75] and is the first and only treatment approved by the FDA for FRDA. Skyclarys has subsequently been approved by the European Commission (EC) in February 2024 [76].
Omaveloxolone was developed by Reata Pharmaceuticals (now a wholly owned subsidiary of Biogen Inc as of September 2023) and targets activation of Nrf2, which is decreased in cells in individuals with FRDA.
A two-part, double-blind, randomised, placebo-controlled trial, MOXIe, was designed to study the safety and efficacy of omaveloxolone in FRDA. Part 1 of the study was designed to evaluate safety and potential efficacy of different doses of omaveloxolone to establish a safe dose to be used in part 2. A total of 69 individuals aged 16–40 years were enrolled and randomised 3:1 (omaveloxolone to placebo) and studied for 12 weeks. While there were no significant changes in the primary outcome measure (peak work during maximal exercise testing), omaveloxolone was found to improve neurological function as assessed by the mFARS with the maximum effect observed at the 160 mg dose [77].
Part 2 was a randomised, placebo-controlled, double-blind, parallel-group study to evaluate the safety and efficacy of 150 mg omaveloxolone with the primary endpoint being change from baseline in mFARS at week 48. A total of 103 participants received either placebo or 150 mg omaveloxolone daily. After 48 weeks of treatment, individuals who received omaveloxolone had a statistically significant, placebo-corrected mean improvement of 2.40 points in the mFARS. Omaveloxolone was found to be mostly well tolerated with minimal adverse events mostly related to upper respiratory tract infections (40%) and headache (17%). A small number of participants demonstrated increased alanine aminotransferase (ALT), aspartate aminotransferase (AST); however, these results were unrelated to liver injury [77]. Participants were invited to continue taking omaveloxolone in an ongoing open-label extension study in which additional data is being collected and safety is being monitored (NCT02255435).
Despite these promising results further work was required to achieve approval by the FDA. Additional analyses comprising propensity-matched data from a natural history study (Friedreich Ataxia Clinical Outcome Measures Study [FA-COMS]) compared with that from the open label extension study demonstrated that over a 3-year period, the progression of FRDA as measured by the mFARS was slowed by 55% in individuals treated with omaveloxolone [78]. Specifically, untreated, matched FA-COMS participants demonstrated neurological progression evident by an increase of the mFARS score by 6.6 points over three years, compared to an increase in the mFARS of 3.0 points in matched individuals treated with omaveloxelone over three years [78]. This final analysis led to the approval by the FDA for individuals aged 16 years and over. This milestone also highlighted the importance of natural history studies in the evaluation of clinical trials [78, 79].
For those clinicians considering prescribing omaveloxolone, the FDA recommend checking alanine aminotransferase (ALT), aspartate aminotransferase (AST), bilirubin, B-type natriuretic peptide (BNP), and lipid parameters prior to initiating omaveloxolone and during treatment. The recommended dosage of omaveloxolone is 150 mg (three capsules) taken orally whole once daily on an empty stomach. For individuals with moderate hepatic impairment the recommended dosage of omaveloxolone is 100 mg once daily. If adverse reactions emerge, further reduction of the dosage to 50 mg once daily is recommended. It is recommended to avoid use in individuals with FRDA with severe hepatic impairment. Clinicians prescribing omaveloxolone should consult the FDA guidelines.
3.2 Compounds that Reduce Oxidative Stress and Improve Mitochondrial Function
3.2.1 Vatiquinone (PTC-743)
Vatiquinone (or PTC-743) was previously known as EPI-743 and was developed by PTC Therapeutics. Vatiquinone is postulated to improve mitochondrial and cellular function by targeting 15-lipooxygenase, a regulator of inflammation, oxidative stress and ferroptosis [80].
MOVE-FA is a randomised, parallel-arm, double-blind, placebo-controlled trial that enrolled 146 children and young adults with FRDA (aged 7–21 years) conducted over 72 weeks, followed by a 24-week open label extension phase. Topline results demonstrated that the study did not meet its primary endpoint (change from baseline in mFARS), however, did show improvement in some secondary endpoints including fatigue and upright stability [81]. PTC Therapeutics has discussed these findings with the FDA and are exploring potential regulatory paths to approval [82]. An open-label extension study is currently ongoing, collecting additional safety and efficacy data (NCT05515536).
3.2.2 MIB-626
Β-nicotinamide mononucleotide (NMN) is a naturally occurring compound related to vitamin B3 that is being evaluated as an investigational drug. MIB-626 is a microcrystalline form of NMN. NMN is a precursor of nicotinamide adenine dinucleotide (NAD). NAD plays a key role in adenosine triphosphate (ATP synthesis), DNA repair and mitochondrial function [83]. Non-pharmaceutical grades of the compound have been available in many countries as a dietary supplement. MIB-626 has been developed by Metro International Biotech, LLC.
An open-label Phase 2 clinical trial was conducted in adults with FRDA aged 18–64 years without overt heart failure (NCT04817111). Participants were administered 1000 mg of MIB-626 daily for 14 days. The main endpoint was safety and tolerability as measured by treatment-emergent adverse events. Secondary endpoints were the effects of MIB-626 on cardiac and skeletal muscle bioenergetics as measured by phosphocreatine (PCr)/adenosine triphosphate (ATP) ratio using cardiac 31-phosphorus-magnetic resonance spectroscopy (MRS) and post-exercise creatine chemical exchange saturation transfer (CrCEST) using magnetic resonance imaging (MRI). Grip strength and the concentration of NAD+ in whole blood following treatment with MIB-626 were further secondary endpoints.
A multiple dose study was conducted in a population of older adults who were overweight or mildly obese. Two cohorts of 16 participants were enrolled—eight men and eight women per cohort were randomised in a 3:1 ratio to receive MIB-626 or placebo for 14 days. Two dose regimens of MIB-626 were studied: 1000 mg MIB-626 administrated once-daily or 1000 mg administered twice-daily. Participants treated with MIB-626 had higher levels of NMN on day 14 compared with the placebo group, with participants receiving twice-daily regimens having greater increase in mean blood NMN concentrations than those on once-daily regimens. MIB-626 was found to be well-tolerated [83].
A phase 2a double-blind placebo-controlled clinical trial studying the safety and tolerability of MIB-626 is planned in adults with FRDA.
3.2.3 Elamipretide (ELAM, SS-31, Bendavia, MTP-131)
Elamipretide (also known as ELAM, SS-31, Bendavia, MTP-131) is a peptide, developed by Stealth Therapeutics, that is reported to modulate mitochondrial function specifically by enhancing ATP synthesis and reducing reactive oxygen species production [84, 85]. It has been evaluated in a clinical trial in primary mitochondrial myopathy [86]. An investigator-initiated phase 1/2 clinical trial (ELViS-FA) is currently underway to evaluate the effect of high dose (40–60 mg) versus low dose (20–30 mg) Elamipretide on high contrast visual acuity in 18 individuals with FRDA compared with baseline at 52 weeks (NCT05168774). Results are expected at the end of 2024.
3.2.4 Resveratrol
Resveratrol is a naturally occurring polyphenol found primarily in the skin of red grapes and is reported to have numerous antioxidant and anti-inflammatory properties. An open-label trial of 24 adults with FRDA was conducted over 12 weeks, studying safety, tolerability and efficacy of two doses of resveratrol (1 g and 5 g). Participants receiving the higher dose were found to have improvement in neurological symptoms; however, they also reported significant gastrointestinal adverse events [87]. A randomised, blinded, placebo-controlled crossover trial of a micronised version of resveratrol was subsequently conducted to compare change in the mFARS score from baseline to 24 weeks following treatment with 2 g per day of micronised resveratrol compared to placebo. The primary outcome measure was the mFARS with multiple clinical and biochemical secondary outcome measures assessed. While the study has been completed, results have not yet been published (NCT03933163).
3.3 Compounds that Modulate Frataxin Controlled Metabolic Pathways
3.3.1 Leriglitazone (MIN 102)
The peroxisome proliferator-activated receptor gamma (PPARγ) is fundamental to cellular process and mitochondrial function, particularly fatty acid storage, antioxidant defence and energy metabolism [88]. In addition, PPARγ regulates the expression of coactivator 1 alpha (PGC-1α) a key component of mitochondrial biogenesis [88]. Reduced PGC-1α in the setting of reduced frataxin levels, has been observed in tissue samples from individuals with FRDA and FRDA mouse models [89] suggesting upregulating PGC-1α with PPARγ agonists such as leriglitazone (MIN 102) may increase neuronal survival and thus be beneficial for individuals with FRDA [88]. Based on promising preclinical studies in cellular and animal FRDA models [88], a 48-week double-blind, randomised controlled phase 2 trial of leriglitazone (MIN 102) was conducted at four European centres in 2019–2020 (FRAMES; NCT03917225). A total of 39 individuals with FRDA (aged 12–42 years) were randomly allocated to receive either oral leriglitazone or placebo dosed according to sex and age [90]. The primary efficacy endpoint was a change in spinal cord area at C2–C3 as measured by morphometric MRI measurement in treated versus placebo group. Secondary endpoints included further MRI measurements (including diffusivity), clinical severity as measured by the SARA and the Cerebellar Composite Functional Scale, and patient-reported outcomes. Markers of PPARγ activity and gene expression were also examined. While the primary endpoint was not met, there were encouraging changes in favour of the treatment group in measurement of iron concentration in the dentate nuclei via QSM following 48 weeks of daily leriglitazone and increases in plasma adiponectin, the latter indicating PPARγ was restored to an effective range for CNS function. Leriglitazone was generally well tolerated [90]. Overall, these results while modest, indicate further, larger studies are warranted. Since publication of these results, leriglitazone has received Orphan Drug Designation by both the FDA and the EC. Current focus is on the development and regulatory hurdles for the use of leriglitazone in adult males with X-linked adrenoleukodystrophy and thus it is unclear when future studies in FRDA are planned [91].
3.3.2 Nomlabofusp (Previously CTI-1601)
Nomlabofusp (previously CTI-1601) is a novel recombinant fusion protein designed to deliver frataxin to the mitochondria [92]. Nomlabofusp does so by fusing a cell-penetrant peptide (CPP) with the complete human frataxin protein to facilitate delivery of mature frataxin to the mitochondria [92]. Nomlabofusp has been promoted as the first compound to address the core issue of FRDA, insufficient frataxin. Phase 1 single ascending doses (SAD) and subsequent multiple ascending doses (MAD) have recently been reported [92]. Both studies were double-blind, placebo-controlled comprising ambulant adults with FRDA. In the SAD study, participants (n = 28) were randomised to receive a single subcutaneous dose of nomlabofusp (25 mg, 50 mg, 75 mg or 100 mg) or placebo. In the MAD study, participants (n = 27) were randomly allocated to receive either seven doses of 25 mg nomlabofusp or placebo daily over the first 4 days followed by one dose every third day, or ten doses of 50 mg nomlabofusp or placebo administered daily for the first 7 days followed by one dose every other day or 13 doses of 100 mg nomlabofusp or placebo once a day for 13 days. The outcomes of the study were safety, pharmacokinetic (PK) analysis and the pharmacodynamic profile, in particular frataxin concentration in buccal cells, skin and platelets [92]. Recent reporting of the outcomes indicates frataxin concentration in buccal cells, skin and muscle biopsy increased in line with increasing dosage. A significant effect was apparent in buccal cell frataxin concentrations in those receiving 50 mg and 100 mg nomlabofusp, having a median increase of 3.89 and 4.59 pg/µg frataxin respectively by day 7 [92]. Of particular relevance was the median increase of 2.81 pg/mg in frataxin levels in skin cells from those participants in the 25 mg cohort on day 14 of dosing, an increase which translates to 33% of frataxin levels in unaffected controls [93]. No serious adverse reactions were reported with most events related to injection site reactions (in all participants), nausea and dizziness, vomiting, headache and erythema [92]. Whilst achieving some normalisation of frataxin levels by addressing frataxin deficiency is encouraging, it appears daily dosing may be required to maintain a therapeutic level of frataxin. Significant limitations of this study include a small cohort not reflective of the FRDA disease trajectory, particularly as participants in the study were ambulant. In addition, there was no indication of how increasing mitochondrial frataxin translates to improvement in clinical status such as ambulation and how sustained such improvement would be.
In March 2024, Larimar announced the first dosing of an individual with FRDA in a long term open label extension study comprising daily injections of 25 mg nomlabofusp (NCT06447025). Safety and frataxin data will support a Biologics License Application submission for accelerated approval targeted for late 2025 [94]. In addition, Larimar plans a paediatric study.
3.3.3 DT-216, DT-216P2, GeneTAC™
DT-216 was developed by Design Therapeutics using a platform known as GeneTAC™ (gene-targeted chimera small molecules) [95]. The DNA binding component of the small molecule targets the site of the repeat expansion that interferes with transcription while the linked ligand component of the molecule facilitates transcription through the repeat expansion thus increasing the expression of the frataxin protein [95]. In essence, the GeneTAC™ platform attempts to create a bypass around the repeat expansion mutation to restore frataxin expression. In December 2022, Design Therapeutics completed a Phase 1a, randomised, double-blind, placebo-controlled, SAD study of DT-216 in adults with FRDA (NCT0528554). In August 2023, Design Therapeutics announced results from a subsequent phase 1 MAD study. The primary outcome of the MAD study was safety, tolerability and the PK of three weekly doses of either 100 mg (n = 4), 200 mg (n = 11) or 300 mg (n = 14) DT-216. Frataxin levels in skeletal muscle were also examined. Participants were randomised to receive either DT-216 or placebo. There were no treatment-related serious adverse events (SAEs); however, five cases of injection site thrombophlebitis were reported raising concern about multiple injections at increasing dosages. These results are yet to be published in peer-reviewed scientific journals however a press release reported a statistically significant and dose-related increase in frataxin mRNA levels in skeletal muscle biopsies [96]. Based on concerns about ongoing injection site safety and the desire to improve the PK profile of the compound, Design Therapeutics announced on 17 March 2024, a new drug product, DT-216P2, designed to address these issues [96]. Design Therapeutics propose to complete preliminary Good Laboratory Practice studies by the end of 2024 aiming to then commence a further phase 1/2 trial of DT-216P2 in 2025.
3.3.4 Dimethyl Fumarate
Dimethyl fumarate (DMF) is an anti-inflammatory and neuro-protective compound currently approved in Europe, Australia and the USA for treatment of remitting and relapsing multiple sclerosis. The potential of DMF to increase frataxin protein levels in lymphocytes from individuals with FRDA was identified in a screening protocol for repurposed drugs [97]. Two complimentary actions for DMF were proposed: to increase FXN expression and, thus, protein levels and to induce Nrf2, thus, facilitating antioxidant defences. To test this hypothesis, Jasoliya and colleagues found that DMF increased FXN expression in FRDA cell and mouse models and in individuals with multiple sclerosis (MS) treated with DMF [98]. Importantly, it was shown that DMF increased frataxin expression by 85% in individuals with MS. These findings suggest that DMF could be an effective treatment for FRDA [98]. Based on these promising results, a Phase 2 double-blind, randomised, placebo-controlled trial has commenced to test the efficacy, safety and tolerability of DMF (EudraCT 2021-006274-23) [99]. The study comprises an initial core phase of 12 weeks in which participants are randomised to receive DMF or placebo and then a further 12 weeks of open label in which all participants receive DMF. Participants will receive 120 mg BID (total 240 mg) of DMF or placebo in week 1, thereafter increasing to 240 mg BID (total 480 mg). Participants aged ≥ 12 years, weighing ≥ 30 kg and homozygous for a GAA expansion will be eligible for screening. The primary endpoint is the change in FXN expression level from baseline to 12 weeks. Secondary clinical endpoints are changes on cardiopulmonary exercise outputs (VO2max, anaerobic threshold and peak workload) and echocardiographic measures; and changes in clinical ratings scales including the SARA, mFARS and performance outcomes being the 9HPT, PATA rate test, ADL/Instrumental ADL scales and EQ-5D. Adverse events will be reported. Secondary laboratory endpoints will compare the effect of DMF on frataxin protein and Nrf2 pathway genes. It is anticipated 40 adults and children with FRDA will be recruited to this single centre study which is expected to be completed in June 2024 [99].
3.3.5 Etravirine
Etravirine (ETR, Intelence) is a non-nucleoside reverse transcriptase inhibitor (NNRT) currently used as a lifelong treatment for HIV-1 infection [100]. ETR was identified as a potential therapy for FRDA during high throughput screening of 853 FDA-approved drugs. ETR was identified as being particularly attractive due to its established safety profile, low toxicity and capacity to increase frataxin levels in lymphoblasts and fibroblasts from individuals with FRDA [100, 101]. These promising results led to a pilot phase 2 randomised trial to assess safety and efficacy of ETR in children and adults with FRDA (NCT04273165). Thirty-five individuals with FRDA (30 adults) were randomized to receive either 200 mg or 400 mg oral ETR daily over a four-month treatment period. This period was preceded and followed by four months respectively of physical and clinical examination, thus providing comparison of disease progression pre, during and post treatment [102]. The primary endpoint was safety and tolerability and the secondary endpoints assessed efficacy. Specifically, the effect of differing dosages of ETR on peak oxygen uptake during an incremental exercise test, peak workload, the SARA score, cardiac parameters, frataxin protein levels in PBMCs and various quality of life and disability measures was assessed [102]. Preliminary results reported, though not yet peer reviewed, indicate ETR was well tolerated with minor adverse events. The one serious adverse event (symptomatic supraventricular tachycardia) was deemed unrelated to study drug, however, highlighted consideration of cardiac parameters in future studies of ETR. Potential efficacy of ETR was considered by a significant improvement in the SARA score during the treatment period followed by a significant decline on treatment cessation. There was no change in other clinical parameters though some (non-significant) changes in quality of life and disability were identified. None of these changes were dose dependent. Unfortunately, frataxin protein was unable to be analysed due to sample degradation [102]. The short duration of the trial, small sample size (and thus inability to stratify based on age or disease severity) and lack of a placebo control arm mitigate the capacity to draw robust conclusions from this trial. Future directions of this compound in FRDA are unclear.
4 New and Emerging Gene Therapies for FRDA
4.1 FRDA Gene Editing and Replacement
Gene therapies present an alternative to drugs as potential treatments for FRDA and other inherited conditions. These therapies attempt to replace or correct the underlying fault in disease-causing genes [103]. If successful, gene therapies potentially offer a revolutionary one-time, single treatment as opposed to the lifetime administration of drugs, and thus provide great hope to the one in ten people living with a currently incurable rare disease [104]. Of the more than 7000 rare diseases, 80% are monogenic disorders and are therefore the best candidates for gene therapy [103, 105].
Gene transfer involves the use of vectors, viral and non-viral, for in vivo delivery to the cell’s nucleus of a working gene, containing the instructions needed for the cell to function properly. Viral vectors are commonly used in gene transfer delivery due to their high transduction efficiency, and they include adenoviruses (AV), adeno-associated virus (AAV), herpes simplex virus (HSV), retroviruses and lentiviruses [106]. Of these viral vectors, AAVs are most commonly used due to their long-term gene expression, low immune responses and their ability to cross the blood–brain barrier (BBB). As such they are favoured in neurodegenerative disease clinical trials [106]. While there is a limitation on the size of gene that can be introduced by AAVs, FXN produces a small protein of 210 amino acids and therefore this is not a consideration for FRDA gene therapy.
FRDA gene transfer involves the use of a vector to deliver frataxin systemically or targeted to affected tissues. FRDA is a good candidate for AAV delivery because most cases are due to a homozygous GAA repeat expansion, which means the level of frataxin is significantly reduced but the protein is normal [43]. Heterozygous carriers also have lower levels of frataxin but are asymptomatic, indicating that relatively modest increases of frataxin in individuals with FRDA should be beneficial [43]. The first demonstration of gene delivery efficacy occurred in a conditional cardiac and skeletal muscle FXN knockout mouse model. Intravenous delivery of human FXN via an AAV rh10 vector resulted in the prevention of cardiac disease onset when the vector was delivered early and a complete reversal of cardiomyopathy when given post symptom onset [107]. Subsequently, a complete reversal of sensory ataxia was observed when an AAV9 vector was used to deliver FXN to a parvalbumin-conditional FXN knockout mouse model that mimics the neuropathophysiology in individuals with FRDA [108]. Since these encouraging mouse studies, international gene therapy research efforts have concentrated on the development and optimisation of AAV vectors for both targeted and systemic FXN delivery. Challenges that still need to be overcome include potentially toxic frataxin overexpression, acquired immunity in the population preventing the administration and re-administration of AAVs, complicated localised delivery to target sites potentially resulting in tissue-specific rescue only and systematic delivery requiring a high vector load [109]. Non-viral approaches such as nanoparticles are also being explored for FXN delivery.
Gene editing involves adding, removing or altering DNA sequences in the genome. It originated with the discovery of endonucleases that could recognise and cut DNA, with the main classes of endonucleases being meganucleases, zinc-finger nucleases (ZFN), transcription activator-like effector nucleases (TALEN) and clustered regularly interspaced short palindromic repeats-associated nucleases (CRISPR-Cas9) [110].
Gene editing approaches have been explored in FRDA [111,112,113,114,115]. Gene editing in FRDA involves removing the GAA expansion within the first intron of the FXN gene; it has been shown to lead to increased frataxin expression using ZFNs and CRISPR-Cas9 in pre-clinical studies [116, 117]. Ex vivo gene editing and gene therapy using autologous transplantation of haematopoietic stem and progenitor cells (HSPCs) is currently being explored [118]. Advantages are that gene editing does not affect the coding sequence, potentially only one allele needs to be corrected to restore the frataxin protein to carrier levels, and using HSPC autologous transplantation is likely to avoid immune reactions [109]. Challenges of gene editing include that the efficiency can be limited, and there are potential off target effects [109].
4.2 Current Investigational Gene Therapies
4.2.1 Phase 1A study of Gene Therapy for FRDA Cardiomyopathy—AAVrh.10hFXN, Weill Medical College of Cornell University
The first demonstration of successful gene transfer and FRDA cardiac phenotype rescue in a mouse model with cardiomyopathy similar to individuals with FRDA was seen with the one-time intravenous administration of 1011 genome copies of AAVrh.10hFXN, an AAV serotype rh10 gene transfer vector expressing human frataxin. This cardiac-specific mouse model was developed using a cardiac promoter (αMyhc) and gene transfer corrected the stress induced FRDA cardiac phenotypes [119]. In further studies, AAVrh.10hFXN was administered to determine the safe and effective intravenous doses required to treat the cardiac manifestations in FRDA using a cardiac and skeletal FXN knockout model [120].
Following these studies, and in a significant milestone for FRDA research, the first gene therapy to be investigated for FRDA in humans commenced in 2022 in a study titled ‘Phase IA Study of AAVrh.10hFXN Gene Therapy for the Cardiomyopathy of Friedreich's Ataxia’ (NCT05302271). This non-randomised, sequential assignment, and dose-escalation study aims to recruit 10 individuals with FRDA, with five subjects in each of the first and second dose cohorts. It involves the intravenous delivery of a single dose of AAVrh.10hFXN, serotype rh.10 adeno-associated virus (AAV) gene transfer vector expressing the cDNA coding for human frataxin in addition to immunosuppression therapy with prednisone for a total of 14 weeks. The primary outcome measure is safety, as measured by the number of subjects with any treatment-related adverse events for 5 years. Secondary outcome measures include changes in cardiopulmonary exercise testing, cardiac-related parameters in cardiac-magnetic resonance scans and echocardiograms and changes in arrhythmias with 24-h monitoring. Outcome measures will continue to be assessed for 5 years post administration. Adults with FRDA aged 18 to 50 years with a left ventricle ejection fraction (EF) as measured by cardiac MRI of > 45–70%, a left ventricular mass index on cardiac MRI > 2 standard deviations above the normal range and < 5% fibrosis in the left ventricular wall on late gadolinium enhancement cardiac MRI are being included.
Outcome measures and inclusion criteria selected for this study restrict the participant profile to those who can both participate in cardiopulmonary arm crank testing and have a left ventricle EF of > 45%. By definition this includes those with less advanced symptoms and excludes those with reduced cardiac function or with more advanced neurological symptoms. Understanding contributors to participation in gene therapy trials, particularly in terms of risk taking is important in the design of such trials [71].
4.2.2 Phase 1/2 Study of Gene Therapy for FRDA Cardiomyopathy—LX2006, LEXEO
Following this phase 1A study, a multi-site phase 1/2 study commenced in 2022. The study titled, ‘A Phase 1/2 Study of the Safety and Efficacy of LX2006 Gene Therapy in Participants With Cardiomyopathy Associated With Friedreich's Ataxia’ (NCT05445323) involves the single intravenous administration of one of three doses (low, mid and high) of LX2006 (AAVrh.10hFXN) to an estimated cohort of n = 9. The gene therapy is designed to deliver the human FXN gene to cardiac cells over a 52 week period. The sequential assignment, open label trial seeks to study the safety and efficacy of LX2006 for participants with FRDA and evidence of cardiomyopathy with long-term safety and efficacy data evaluated for an additional 4 years.
Primary outcome measures include safety determined by documentation of treatment-emergent adverse events (TEAEs) and treatment-emergent serious adverse events (TESAEs). Secondary outcome measures include change from baseline in LVMi, LVEF, cardiac fibrosis as measured by cardiac MRI, measures of cardiopulmonary exercise tolerance and presence and severity of cardiac arrythmias. Adults with FRDA will be recruited to this study if they have an onset of FRDA < 25 years of age and meet protocol specified ranges for antibodies and measures of cardiomyopathy. Exclusion criteria include those with contraindications to cardiac MRI and cardiac biopsies, a history of significant coronary artery disease or any structural heart of vascular disease and the presence of clinically significant, hemodynamically unstable arrhythmias. Similar to the phase 1A study, the outcome measures, inclusion and exclusion criteria for this phase 1/2 study restricts participation to those adults with a typical onset and in the early stages of FRDA cardiomyopathy.
In June 2023, LEXEO announced it had completed the first dose cohort and had begun treatment with a larger frataxin dose in the second cohort; the gene therapy had been well tolerated and no unexpected events have been observed. An interim update in March 2024 announced that the first ever cardiac biopsies evaluating frataxin levels had been successfully conducted in three participants, and frataxin expression levels were increased relative to the pre-treatment baseline levels [121]. Promisingly, a dose-dependent response was observed with frataxin expression increased approximately fivefold on average in the second cohort relative to the first cohort.
4.2.3 Phase 1 study of Gene Therapy for FRDA Cardiomyopathy—ASP2016, Astellas
Preclinical animal studies conducted by Astellas Gene Therapies using the cardiac and skeletal muscle conditional knockout FRDA mouse model (FXN-MCK) showed that a single intravenous injection of an AAV8 vector containing either the human or mouse FXN gene improved cardiac function in this mouse and increased survival [122]. In an April 2024 communication with FARA and the FRDA community, Astellas announced that the FDA has granted Fast Track designation for their investigational new AAV8 gene therapy drug, ASP2016, to treat cardiomyopathy in individuals with FRDA [123]. ASP2016 is designed to restore functional frataxin to levels necessary for normal cellular function. It is administered via intravenous infusion and delivers a full length functional copy of the FXN gene to the heart. Preparation for a phase 1 clinical trial of ASP2016 is underway and is expected to begin in the second half of 2024 [124].
Four additional FRDA gene editing and gene replacement programs are included in the FARA FRDA Drug Development Pipeline [74]. These preclinical programs are being developed by Solid Biosciences [125], Neurocrine Biosciences/Voyager Therapeutics [126], Prime Medicine [127] and Papillon Therapeutics [118, 128, 129].
5 Conclusion/Future Directions
Facilitated by our understanding of the prevalence, pathophysiology and natural history of FRDA, there is a great breadth and depth of compounds under investigation that address each of the different modes of action. The process of approval by the US FDA of a treatment for individuals with FRDA aged 16 years and over highlighted to the research community the importance of sensitive outcome measures and the significant role of data from natural history studies [78]. The quest continues to identify compounds that will augment mitochondrial function and/or increase frataxin expression. At the time of this review there were five compounds that reduce oxidative stress and improve mitochondrial function currently approved, either in trial or just completed (Table 1). Our understanding of FRDA has increased exponentially since the identification of the causative mutation in FXN [4]. Given the understanding that frataxin deficiency is the main source of pathology in FRDA, it is unsurprising that there are five compounds currently under investigation that modulate frataxin controlled metabolic pathways. Moreover, given the promise of gene replacement and editing, there are currently two trials in progress. Importantly, the cardiac gene therapy programs have been designed to target one of the major sites of pathology and therefore hold great potential for addressing the leading cause of premature death in FRDA [46].
It is plausible that a combination of therapies may achieve both symptom reduction, slowing of progression, improvements in mitochondrial function and expression of frataxin [130]. Despite significant scientific advances in the specificity of both compounds and targets developed and investigated, challenges remain for the advancement of treatments in a limited recruitment population. This includes designing clinical trials that align inclusion criteria with patient cohorts at different disease stages so that meaningful outcomes will be achieved.
For individuals with FRDA and for researchers working in this area these are exciting times. While the numbers of current trials have varied over the past few years, the specificity of both the compounds and targets has increased. That we have an approved treatment for FRDA is to be celebrated and heralds a bright future for ongoing therapeutic development in FRDA.
References
Cossée M, et al. Evolution of the Friedreich’s ataxia trinucleotide repeat expansion: founder effect and premutations. Proc Natl Acad Sci USA. 1997;94(14):7452–7.
Labuda M, et al. Unique origin and specific ethnic distribution of the Friedreich ataxia GAA expansion. Neurology. 2000;54(12):2322–4.
Friedreich N. Uber degenerative Atrophie der spinalen Hinterstrange. Virchow’s Archiv Pathological Anatomy. 1863;26:291–419.
Campuzano V, et al. Friedreich’s ataxia: autosomal recessive disease caused by an intronic GAA triplet repeat expansion. Science. 1996;271(5254):1423–7.
Delatycki MB, Corben LA. Clinical features of Friedreich ataxia. J Child Neurol. 2012;27(9):1133–7.
Keita M, et al. Friedreich ataxia: clinical features and new developments. Neurodegener Dis Manag. 2022;12(5):267–83.
Maudoux A, et al. Vestibular impact of Friedreich ataxia in early onset patients. Cerebellum Ataxias. 2020;7:6.
Reetz K, et al. Protocol of a randomized, double-blind, placebo-controlled, parallel-group, multicentre study of the efficacy and safety of nicotinamide in patients with Friedreich ataxia (NICOFA). Neurol Res Pract. 2019;1:33.
Rummey C, Farmer JM, Lynch DR. Predictors of loss of ambulation in Friedreich’s ataxia. EClinicalMedicine. 2020;18: 100213.
Rummey C, et al. Natural history of Friedreich Ataxia: heterogeneity of neurologic progression and consequences for clinical trial design. Neurology. 2022;99(14):e1499–510.
Reetz K, et al. Progression characteristics of the European Friedreich’s Ataxia Consortium for Translational Studies (EFACTS): a 4-year cohort study. Lancet Neurol. 2021;20(5):362–72.
Indelicato E, et al. Predictors of survival in Friedreich’s Ataxia: a prospective cohort study. Mov Disord. 2024;39(3):510–8.
Campuzano V, et al. Frataxin is reduced in Friedreich ataxia patients and is associated with mitochondrial membranes. Hum Mol Genet. 1997;6(11):1771–80.
Evans-Galea MV, et al. Beyond loss of frataxin: the complex molecular pathology of Friedreich ataxia. Discov Med. 2014;17(91):25–35.
Boehm T, et al. Variations of frataxin protein levels in normal individuals. Neurol Sci. 2011;32(2):327–30.
Candayan A, et al. The first biallelic missense mutation in the FXN gene in a consanguineous Turkish family with Charcot-Marie-Tooth-like phenotype. Neurogenetics. 2020;21(1):73–8.
Smith FM, Kosman DJ. Molecular defects in Friedreich’s Ataxia: convergence of oxidative stress and cytoskeletal abnormalities. Front Mol Biosci. 2020;7: 569293.
Monfort B, et al. Recent advances in the elucidation of Frataxin biochemical function open novel perspectives for the treatment of Friedreich’s Ataxia. Front Neurosci. 2022;16: 838335.
Maio N, Rouault TA. Iron-sulfur cluster biogenesis in mammalian cells: New insights into the molecular mechanisms of cluster delivery. Biochim Biophys Acta. 2015;1853(6):1493–512.
Santos R, et al. Friedreich ataxia: molecular mechanisms, redox considerations, and therapeutic opportunities. Antioxid Redox Signal. 2010;13(5):651–90.
Schmucker S, Puccio H. Understanding the molecular mechanisms of Friedreich’s ataxia to develop therapeutic approaches. Hum Mol Genet. 2010;19(R1):R103–10.
Saccà F, et al. A combined nucleic acid and protein analysis in Friedreich ataxia: implications for diagnosis, pathogenesis and clinical trial design. PLoS ONE. 2011;6(3): e17627.
Calabrese V, et al. Oxidative stress, mitochondrial dysfunction and cellular stress response in Friedreich’s ataxia. J Neurol Sci. 2005;233(1–2):145–62.
Payne RM. Cardiovascular research in Friedreich Ataxia: unmet needs and opportunities. JACC Basic Transl Sci. 2022;7(12):1267–83.
Chutake YK, et al. Epigenetic promoter silencing in Friedreich ataxia is dependent on repeat length. Ann Neurol. 2014;76(4):522–8.
Reetz K, et al. Biological and clinical characteristics of the European Friedreich’s Ataxia Consortium for Translational Studies (EFACTS) cohort: a cross-sectional analysis of baseline data. Lancet Neurol. 2015;14(2):174–82.
Mateo I, et al. Expanded GAA repeats and clinical variation in Friedreich’s ataxia. Acta Neurol Scand. 2004;109(1):75–8.
Montermini L, et al. Phenotypic variability in Friedreich ataxia: role of the associated GAA triplet repeat expansion. Ann Neurol. 1997;41(5):675–82.
Pandolfo M. Friedreich ataxia. Arch Neurol. 2008;65(10):1296–303.
Kelly M, et al. A polymorphic miR-155 binding site in AGTR1 is associated with cardiac hypertrophy in Friedreich ataxia. J Mol Cell Cardiol. 2011;51(5):848–54.
Rodden LN, et al. A non-synonymous single nucleotide polymorphism in SIRT6 predicts neurological severity in Friedreich ataxia. Front Mol Biosci. 2022;9: 933788.
Lecocq C, et al. Delayed-onset Friedreich’s ataxia revisited. Mov Disord. 2016;31(1):62–9.
Bhidayasiri R, et al. Late-onset Friedreich ataxia: phenotypic analysis, magnetic resonance imaging findings, and review of the literature. Arch Neurol. 2005;62(12):1865–9.
Junck L, et al. Structural and functional brain imaging in Friedreich’s ataxia. Arch Neurol. 1994;51(4):349–55.
Parkinson MH, et al. Clinical features of Friedreich’s ataxia: classical and atypical phenotypes. J Neurochem. 2013;126(Suppl 1):103–17.
Koeppen AH, et al. The dorsal root ganglion in Friedreich’s ataxia. Acta Neuropathol. 2009;118(6):763–76.
Koeppen AH. Tissue Iron in Friedreich Ataxia. J Integr Neurosci. 2024;23(1):4.
Harding IH, et al. Central nervous system therapeutic targets in friedreich ataxia. Hum Gene Ther. 2020;31(23–24):1226–36.
Koeppen AH, et al. Dorsal root ganglia in Friedreich ataxia: satellite cell proliferation and inflammation. Acta Neuropathol Commun. 2016;4(1):46.
Rezende TJR, et al. Progressive spinal cord degeneration in Friedreich’s Ataxia: results from ENIGMA-Ataxia. Mov Disord. 2023;38(1):45–56.
Koeppen AH, et al. Friedreich ataxia: failure of GABA-ergic and glycinergic synaptic transmission in the dentate nucleus. J Neuropathol Exp Neurol. 2015;74(2):166–76.
Apolloni, S., M. Milani, and N. D'Ambrosi, Neuroinflammation in Friedreich's Ataxia. Int J Mol Sci, 2022. 23(11).
Delatycki MB, Bidichandani SI. Friedreich ataxia- pathogenesis and implications for therapies. Neurobiol Dis. 2019;132: 104606.
Harding IH, et al. Brain structure and degeneration staging in Friedreich Ataxia: magnetic resonance imaging volumetrics from the ENIGMA-Ataxia working group. Ann Neurol. 2021;90(4):570–83.
Peverill RE, et al. Left ventricular structural and functional changes in Friedreich ataxia - Relationship with body size, sex, age and genetic severity. PLoS ONE. 2019;14(11): e0225147.
Lees JG, et al. Cellular pathophysiology of Friedreich’s ataxia cardiomyopathy. Int J Cardiol. 2022;346:71–8.
Subramony SH, et al. Measuring Friedreich ataxia: interrater reliability of a neurologic rating scale. Neurology. 2005;64(7):1261–2.
Zesiewicz, T.A., Susan Perlman, Kelly L. Sullivan, Yangxin Huang, Jason L. Salemi, Matthew Klein, Charles Isaacs, Clifton Gooch, Jessica Shaw, David Lynch 88 (S16): S17.005 EPI-743 (alpha-tocotrienol quinone) demonstrates long-term improvement in neurological function and disease progression in Friedreich’s ataxia. Neurology, 2017. 88(S17.005).
Rummey C, et al. Psychometric properties of the Friedreich Ataxia Rating Scale. Neurol Genet. 2019;5(6):371.
Schmitz-Hübsch T, et al. Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology. 2006;66(11):1717–20.
Corben LA, et al. Developing an instrumented measure of upper limb function in Friedreich ataxia. Cerebellum. 2021;20(3):430–8.
Nguyen KD, et al. The assessment of upper limb functionality in Friedreich ataxia via self-feeding activity. IEEE Trans Neural Syst Rehabil Eng. 2020;28(4):924–33.
Akhlaghi H, et al. Superior cerebellar peduncle atrophy in Friedreich’s ataxia correlates with disease symptoms. Cerebellum. 2011;10(1):81–7.
Selvadurai LP, et al. Cerebral and cerebellar grey matter atrophy in Friedreich ataxia: the IMAGE-FRDA study. J Neurol. 2016;263(11):2215–23.
Corben LA, et al. Myelin paucity of the superior cerebellar peduncle in individuals with Friedreich ataxia: an MRI magnetization transfer imaging study. J Neurol Sci. 2014;343(1–2):138–43.
Rezende TJ, et al. Longitudinal magnetic resonance imaging study shows progressive pyramidal and callosal damage in Friedreich’s ataxia. Mov Disord. 2016;31(1):70–8.
Vavla M, et al. Sensitivity of neuroimaging indicators in monitoring the effects of interferon gamma treatment in Friedreich’s ataxia. Front Neurosci. 2020;14:872.
Ward PGD, et al. Longitudinal evaluation of iron concentration and atrophy in the dentate nuclei in friedreich ataxia. Mov Disord. 2019;34(3):335–43.
Straub S, et al. Toward quantitative neuroimaging biomarkers for Friedreich’s ataxia at 7 Tesla: susceptibility mapping, diffusion imaging, R(2) and R(1) relaxometry. J Neurosci Res. 2020;98(11):2219–31.
Joers, J.M., et al., Spinal cord magnetic resonance imaging and spectroscopy detect early-stage alterations and disease progression in Friedreich ataxia. Brain Commun, 2022. 4(5): p. fcac246.
Georgiou-Karistianis N, et al. A natural history study to track brain and spinal cord changes in individuals with Friedreich’s ataxia: TRACK-FA study protocol. PLoS ONE. 2022;17(11): e0269649.
Legrand L, et al. Predictors of left ventricular dysfunction in Friedreich’s ataxia in a 16-year observational study. Am J Cardiovasc Drugs. 2020;20(2):209–16.
Ribaï P, et al. Neurological, cardiological, and oculomotor progression in 104 patients with Friedreich ataxia during long-term follow-up. Arch Neurol. 2007;64(4):558–64.
Peverill RE. Letter by Peverill regarding article, “The heart in Friedreich ataxia: definition of cardiomyopathy, disease severity, and correlation with neurological symptoms.” Circulation. 2012;126(17): e272.
Rummey, C., et al., Evaluating mFARS in pediatric Friedreich's ataxia: Insights from the FACHILD study. Ann Clin Transl Neurol, 2024.
Tiemeier H, et al. Cerebellum development during childhood and adolescence: a longitudinal morphometric MRI study. Neuroimage. 2010;49(1):63–70.
Gavriilaki, M., et al., Therapeutic biomarkers in Friedreich's ataxia: a systematic review and meta-analysis. Cerebellum, 2023.
U.S. Food and Drug Administration. Patient-focused drug development: selecting, developing, or modifying fit for purpose clinical outcome assessments 2022 [cited 2024 9 April 2024]; Available from: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/patient-focused-drug-development-selecting-developing-or-modifying-fit-purpose-clinical-outcome.
Friedreich’s Ataxia Research Alliance, The voice of the patient. 2017: https://www.curefa.org/pdf/news/FA-Voice-of-the-Patient.pdf.
Thomas-Black G, et al. The attitude of patients with progressive ataxias towards clinical trials. Orphanet J Rare Dis. 2022;17(1):1.
Lieschke K, et al. How great a risk do you take? A qualitative study exploring attitudes of individuals with Friedreich ataxia toward gene therapy. Hum Gene Ther. 2023;34(19–20):1041–8.
Trantham SJ, et al. Perspectives of the Friedreich ataxia community on gene therapy clinical trials. Mol Ther Methods Clin Dev. 2024;32(1): 101179.
Rummey C, K.E., Lynch DR, Clinical trial design for Friedreich ataxia - Where are we now and what do we need? OrphDrugs, 2018. 6(3): p. 219-230.
Friedreich’s Ataxia Research Alliance. Drug development pipeline. 2024 [cited 2024 25 June, 2024]; Available from: https://www.curefa.org/wp-content/uploads/2024/06/Pipeline-June-18-2024.pdf.
Lee A. Omaveloxolone: first approval. Drugs. 2023;83(8):725–9.
Biogen, Biogen received european commission approval for SKYCLARYS® (omaveloxolone), the first therapy to treat Friedreich’s ataxia. 2024.
Lynch DR, et al. Safety and efficacy of omaveloxolone in Friedreich ataxia (MOXIe Study). Ann Neurol. 2021;89(2):212–25.
Lynch DR, et al. Propensity matched comparison of omaveloxolone treatment to Friedreich ataxia natural history data. Ann Clin Transl Neurol. 2024;11(1):4–16.
Subramony SH, Lynch DL. A milestone in the treatment of ataxias: approval of omaveloxolone for Friedreich ataxia. Cerebellum. 2024;23(2):775–7.
Shrader WD, et al. α-Tocotrienol quinone modulates oxidative stress response and the biochemistry of aging. Bioorg Med Chem Lett. 2011;21(12):3693–8.
PTC Therapeutics, PTC Therapeutics announces topline results from vatiquinone MOVE-FA Registration-Directed Trial. 2023.
PTC Therapeutics, PTC Therapeutics provides corporate update and reports fourth quarter and full year 2023 financial results. 2024.
Pencina KM, et al. MIB-626, an oral formulation of a microcrystalline unique polymorph of β-nicotinamide mononucleotide, increases circulating nicotinamide adenine dinucleotide and its metabolome in middle-aged and older adults. J Gerontol A Biol Sci Med Sci. 2023;78(1):90–6.
Edzeamey FJ, et al. Emerging antioxidant therapies in Friedreich’s ataxia. Front Pharmacol. 2024;15:1359618.
Pharaoh G, et al. The mitochondrially targeted peptide elamipretide (SS-31) improves ADP sensitivity in aged mitochondria by increasing uptake through the adenine nucleotide translocator (ANT). Geroscience. 2023;45(6):3529–48.
Karaa A, et al. Efficacy and safety of elamipretide in individuals with primary mitochondrial myopathy: The MMPOWER-3 randomized clinical trial. Neurology. 2023;101(3):e238–52.
Yiu EM, et al. An open-label trial in Friedreich ataxia suggests clinical benefit with high-dose resveratrol, without effect on frataxin levels. J Neurol. 2015;262(5):1344–53.
Rodríguez-Pascau L, et al. PPAR gamma agonist leriglitazone improves frataxin-loss impairments in cellular and animal models of Friedreich Ataxia. Neurobiol Dis. 2021;148: 105162.
Coppola G, et al. Functional genomic analysis of frataxin deficiency reveals tissue-specific alterations and identifies the PPARgamma pathway as a therapeutic target in Friedreich’s ataxia. Hum Mol Genet. 2009;18(13):2452–61.
Pandolfo M, et al. Efficacy and safety of leriglitazone in patients with Friedreich ataxia: a phase 2 double-blind, randomized controlled trial (FRAMES). Neurol Genet. 2022;8(6): e200034.
Friedreich’s Ataxia Research Alliance. Research pipeline. 2024 [cited 2024 9 April, 2024]; Available from: https://www.curefa.org/research/research-pipeline.
Clayton R, et al. Safety, pharmacokinetics, and pharmacodynamics of nomlabofusp (CTI-1601) in Friedreich’s ataxia. Ann Clin Transl Neurol. 2024;11(3):540–53.
Larimar Therapeutics, Larimar therapeutics reports positive top-line data from phase 2 dose exploration study from 25 mg and 50 mg cohorts of nomlabofusp in patients with Friedreich’s ataxia. 2024.
Larimar Therapeutics, Larimar therapeutics announces the dosing of the first patient in long-term open label extension study for nomlabofusp in patients with Friedreich’s ataxia. 2024.
Khorkova O, et al. Amplifying gene expression with RNA-targeted therapeutics. Nat Rev Drug Discov. 2023;22(7):539–61.
Design Therapeutics, Design therapeutics outlines progress across GeneTAC™ platform and announces fourth quarter and full year 2023 financial results. 2024.
Sahdeo S, et al. Dyclonine rescues frataxin deficiency in animal models and buccal cells of patients with Friedreich’s ataxia. Hum Mol Genet. 2014;23(25):6848–62.
Jasoliya M, et al. Dimethyl fumarate dosing in humans increases frataxin expression: a potential therapy for Friedreich’s ataxia. PLoS ONE. 2019;14(6): e0217776.
Pane C, et al. Rationale and protocol of a double-blind, randomized, placebo-controlled trial to test the efficacy, safety, and tolerability of dimethyl fumarate in Friedreich Ataxia (DMF-FA-201). Front Neurosci. 2023;17:1260977.
Rufini A, et al. Drug repositioning in Friedreich ataxia. Front Neurosci. 2022;16: 814445.
Alfedi G, et al. Drug repositioning screening identifies etravirine as a potential therapeutic for friedreich’s ataxia. Mov Disord. 2019;34(3):323–34.
Paparella, G., et al., A pilot phase 2 randomized trial to evaluate the safety and potential efficacy of etravirine in Friedreich ataxia patients, in Preprints. 2024, Preprints.
Landhuis, E., The definition of gene therapy has changed, in Nature 2021: https://www.nature.com/articles/d41586-021-02736-8.
Mendell JR, et al. Current clinical applications of in vivo gene therapy with AAVs. Mol Ther. 2021;29(2):464–88.
Neurology L. Rare advances for rare diseases. Lancet Neurol. 2016;16(1):1.
Ocana-Santero, G., J. Díaz-Nido, and S. Herranz-Martín, Future prospects of gene therapy for Friedreich's ataxia. Int J Mol Sci, 2021. 22(4).
Perdomini M, et al. Prevention and reversal of severe mitochondrial cardiomyopathy by gene therapy in a mouse model of Friedreich’s ataxia. Nat Med. 2014;20(5):542–7.
Piguet F, et al. Rapid and complete reversal of sensory ataxia by gene therapy in a novel model of Friedreich ataxia. Mol Ther. 2018;26(8):1940–52.
Sivakumar A, Cherqui S. Advantages and limitations of gene therapy and gene editing for Friedreich’s ataxia. Front Genome Ed. 2022;4: 903139.
Popovitz J, et al. Gene editing therapeutics based on mRNA delivery. Adv Drug Deliv Rev. 2023;200: 115026.
Li J, et al. Defining transcription regulatory elements in the human frataxin gene: implications for gene therapy. Hum Gene Ther. 2020;31(15–16):839–51.
Maheshwari S, Vilema-Enríquez G, Wade-Martins R. Patient-derived iPSC models of Friedreich ataxia: a new frontier for understanding disease mechanisms and therapeutic application. Transl Neurodegener. 2023;12(1):45.
Li J, et al. Excision of the expanded GAA repeats corrects cardiomyopathy phenotypes of iPSC-derived Friedreich’s ataxia cardiomyocytes. Stem Cell Res. 2019;40: 101529.
Shen X, et al. Efficient electroporation of neuronal cells using synthetic oligonucleotides: identifying duplex RNA and antisense oligonucleotide activators of human frataxin expression. RNA. 2019;25(9):1118–29.
Mazzara PG, et al. Frataxin gene editing rescues Friedreich’s ataxia pathology in dorsal root ganglia organoid-derived sensory neurons. Nat Commun. 2020;11(1):4178.
Li Y, et al. Excision of expanded GAA repeats alleviates the molecular phenotype of Friedreich’s ataxia. Mol Ther. 2015;23(6):1055–65.
Ouellet DL, et al. Deletion of the GAA repeats from the human frataxin gene using the CRISPR-Cas9 system in YG8R-derived cells and mouse models of Friedreich ataxia. Gene Ther. 2017;24(5):265–74.
Mishra, P., et al., Gene editing improves endoplasmic reticulum-mitochondrial contacts and unfolded protein response in Friedreich’s ataxia iPSC-derived neurons. Frontiers in Pharmacology, 2024. 15.
Salami CO, et al. Stress-induced mouse model of the cardiac manifestations of Friedreich’s ataxia corrected by AAV-mediated gene therapy. Hum Gene Ther. 2020;31(15–16):819–27.
Munoz-Zuluaga, C., et al., Identification of safe and effective intravenous dose of AAVrh.10hFXN to treat the cardiac manifestations of Friedreich's ataxia. Hum Gene Ther, 2023. 34(13-14): p. 605-615.
LEXEO Therapeutics, LEXEO THERAPEUTICS REPORTS FOURTH QUARTER AND FULL YEAR 2023 FINANCIAL RESULTS AND OPERATIONAL HIGHLIGHTS. 2024.
Chang JC, et al. AAV8 gene therapy reverses cardiac pathology and prevents early mortality in a mouse model of Friedreich’s ataxia. Mol Ther Methods Clin Dev. 2024;32(1): 101193.
Friedreich Ataxia Research Alliance. Astellas shares that US FDA cleared their IND with Fast Track designation for Phase 1 trial of their investigational gene therapy for the treatment of cardiomyopathy in FA. 2024 [cited 2024 24 June 2024]; Available from: https://www.curefa.org/astellas-shares-that-us-fda-cleared-their-ind-with-fast-track-designation-for-phase-1-trial-of-their-investigational-gene-therapy-for-the-treatment-of-cardiomyopathy-in-fa/.
Okamura, N., FY2023 Financial Results Ended March 31, 2024. 2024, Astellas.
Pavlath, G.K. Efficacy and safety of a novel AAV FXN gene therapy (AVB-202) for the treatment of Friedreich’s ataxia. In American Society for Cell and Gene Therapy. 2023. Los Angeles, CA.
Voyager Therapeutics, I., Voyager Therapeutics Announces Selection of Gene Therapy Development Candidate for Friedreich’s Ataxia in Collaboration with Neurocrine Biosciences, Triggering Milestone Payment. 2024, Voyager Therapeutics: www.voyagertherapeutics.com
Anzalone, A., Developing Prime Editors to Treat Repeat Expansion Diseases, in 6th International Conference on CRISPR Technologies. 2023: Boston, MA.
Papillon Therapeutics. FXN corrected HSPC. 2024 [cited 2024 2 July 2024]; https://www.papillon-tx.com/science.
Rocca CJ, et al. Transplantation of wild-type mouse hematopoietic stem and progenitor cells ameliorates deficits in a mouse model of Friedreich's ataxia. Sci Transl Med. 2017;9(413).
Clay A, et al. New developments in pharmacotherapy for Friedreich ataxia. Expert Opin Pharmacother. 2019;20(15):1855–67.
Acknowledgements
The authors are grateful to Professor Bronya Keats in the critical review and editing of this manuscript. The authors also thank the Friedreich Ataxia Research Alliance and the Australian Friedreich Ataxia Stem Cell and Gene Therapy Consortium for ongoing support of their research endeavours.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open access funding enabled and organized by CAUL and its Member Institutions. V.S. and L.A.C. receive funding support from the Friedreich Ataxia Research Alliance (USA) via the Australian Friedreich Ataxia Stem Cell and Gene Therapy Consortium.
Conflict of interest
V.S. and G.T. do not report any conflicts of interest. M.B.D. and L.A.C. were the Principal Investigator and Co-Investigator respectively for the clinical trial for Resveratrol (funded by the National Health and Medical Research Council (NHMRC) project grant 1102207). M.B.D. receives funding from PTC Therapeutics and Biogen to conduct clinical trials. L.A.C. provides consultancy services to Biogen Inc.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
All data generated or analysed during this study are included in this published article.
Code availability
Not applicable.
Author contribution
V.S. and L.A.C. conceived and designed the work, completed the literature review and analysis and prepared the first manuscript draft. G.T. and M.B.D. contributed to literature review and analysis and provided critical review of manuscript drafts. All authors have read and approve the final version of the manuscript and agree to be accountable for the work.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Scott, V., Delatycki, M.B., Tai, G. et al. New and Emerging Drug and Gene Therapies for Friedreich Ataxia. CNS Drugs 38, 791–805 (2024). https://doi.org/10.1007/s40263-024-01113-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-024-01113-z