Abstract
Background and Objective
Ornidazole, the third generation of nitroimidazole derivatives after metronidazole and tinidazole, it exerts both bactericidal and antiprotozoal effects. The purpose of this study was to evaluate the pharmacokinetic and bioequivalence of two ornidazole tablets manufactured by two different manufacturers based on their pharmacokinetic parameters.
Patients and Methods
Fasted and fed healthy Chinese volunteers participated in a randomized sequence, single-dose, open-label, two-period crossover trial. There were 24 participants in both the fed study and the fasted study. Following a 7-day washout period before receiving the alternative formulation, eligible research participants were randomly assigned (1:1) to receive a single dosage of either the reference formulation or the test formulation. Following tablet administration, plasma samples were obtained over 72 h and analyzed using liquid chromatography tandem mass spectrometry (LC–MS/MS) to evaluate ornidazole contents. maximum plasma concentration (Cmax), time to Cmax (Tmax), the area under the curve (AUC) from t = 0 to infinity (AUC0–∞), AUC from t = 0 to the last quantifiable concentration (AUC0–t), half-life (t1/2), and terminal elimination rate constant (z) were evaluated as pharmacokinetic (PK) parameters. The safety evaluation involved adverse events (AEs) incidence and alterations in laboratory tests (hepatic function, blood biochemistry, hematology, and urinalysis) or vital signs (temperature, pulse, and blood pressure).
Results
For the bioequivalence assessment in the fast trial, the prime PK parameters comparison between the reference and test formulation revealed that the GMR (90% CI) values for AUC0–t, Cmax, and AUC0–∞ were 100.97% (99.12–102.85%), 99.88% (90.63–110.08%), and 101.12% (99.17–103.11%), respectively. For the bioequivalence assessment in the fed trial, the key PK parameters comparison between the reference and test formulations revealed that the GMR (90% CI) values for AUC0–t, Cmax, and AUC0–∞ were 103.00% (100.94–105.11%), 101.90% (99.63–104.22%), and 102.99% (100.87–105.16%), respectively. The geometric mean ratios (GMRs) for the primary pharmacokinetic parameters (Cmax, AUC0–72, and AUC0–∞) between the two formulations and the corresponding 90% confidence intervals (CIs) were all within the range of 80.00–125.00% for both the fasting and fed states. Both treatments have comparable safety profiles.
Conclusion
The bioequivalence and tolerability of ornidazole tablet reference and test formulations were evaluated among healthy Chinese participants under both fasting and fed conditions. The results indicated that both formulations were bioequivalent and generally well tolerated; besides, the interaction between food and drug may affect drug pharmacokinetics.
Trial Registration
CTR20212873, registered on 15 November 2021; ChiCTR2300069098, registered on 7 March 2023.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Both test and reference formulations of ornidazole tablets were bioequivalent under fasting conditions in healthy Chinese subjects. |
And both were well tolerated and safe. |
The availability of this drug may help to increase access to ornidazole for patients with susceptible and anaerobe infections and reduce the burden on the health care system in China. |
1 Introduction
Ornidazole, the third generation of nitroimidazole derivatives after metronidazole and tinidazole, was developed by Roche in the 1970s. And on 11 March 1982, OrPha Swiss GmbH launched ornidazole tablets (Tiberal) in Switzerland [1]. Ornidazole exerts both bactericidal and antiprotozoal effects [2, 3], and it is commonly prescribed in China [4]. Ornidazole is effective in treating infections induced by Entamoeba histolytica, Giardia lamblia, Trichomonas vaginalis, and anaerobic bacteria. It is often used to treat infections of the mouth cavity, pelvis, and abdomen, as well as to prevent infections before and after surgery [5,6,7].
The antimicrobial mechanism of ornidazole involves the formation of a hydroxylamine intermediate in the microbe, thus damaging microbial DNA, disrupting transcription, and ultimately triggering cell death. Ornidazole is often favored in some clinical practice therapies due to its longer half-life (14.4 h against 8.4 h for metronidazole) and lower dose frequency and length of therapy in several significant clinical infections [8].
Oral ornidazole absorption is rapid and complete, reaching maximum plasma concentration (Tmax) in about 2 h. In most tissues, including the central nervous system, ornidazole concentrations range from 60 to 100% of plasma levels, whereas they are lower in the placenta. Ornidazole’s apparent volume of distribution in vivo is 0.87 L/kg, and the binding rate of plasma protein is less than 15% [9]. In the liver, ornidazole is primarily metabolized to 3-(2-methyl-5-nitroimidazole-l-yl)-l,2-propane-diol (M4) and a-(chloromethyl)-2-hydroxymethyl-5-nitroimidazole-l-ethanol (Ml). After oral administration of ornidazole, less than 4% of the original drug was found in the fecal matter of healthy volunteers, and within 5 days of the administration, 85% of the ornidazole dose was retrieved through urine and feces, and the predominant excretion route for ornidazole was through the urinary system, with fecal excretion representing 22.1% of the administered dose. Ornidazole has been observed to be a P-glycoprotein substrate in vivo among human volunteers, and its oral absorption was found to be affected during the intestinal absorptive phase [10].
The Pharmaceuticals and Medical Devices Agency (PMDA) and US Food and Drug Administration (FDA) have no information on the marketing of ornidazole. At present, there are seven ornidazole tablets listed in China, and the listed specifications are 0.1 and 0.5 g. For almost 30 years, ornidazole has been extensively prescribed, and prior studies have evaluated its pharmacokinetic (PK) parameters and tolerability [11, 12]. According to current regulatory requirements, the pharmacokinetic bioequivalence performance of some chemical generics can replace the therapeutic equivalence between different preparations. Therefore, our study attempted the end point of pharmacokinetic parameters instead of pharmacodynamics. The objective of this investigation was to evaluate the comparative bioavailability of two ornidazole tablets produced by two distinct manufacturers (test formulation was 0.25 g per tablet, reference formulation was 0.5 g per tablet) in adult, healthy Chinese participants under fasting and fed conditions. The purpose of this study was to lay the groundwork for the introduction of this formulation into the Chinese market, with registration under CTR20212873 on 15 November 2021, as well as ChiCTR2300069098 on 7 March 2023.
2 Patients and Methods
2.1 Formulations and Subject Selection
For bioequivalence evaluation, the test formulation was 0.25 g per tablet (lot no.: 020211001; expiration date: 7 October 2023) ornidazole manufactured by Zhejiang Aisheng Pharmaceutical Co., LTD and supplied by OrPha Swiss GmbH, whereas the reference formulation (marketed as Tiberal®) was 0.5 g per tablet (0.5 g per tablet; lot no.: 3026; expiration date: January 2025) ornidazole produced by Zhejiang Aisheng Pharmaceutical Co., LTD and supplied by Orpha Swiss GmbH.
Healthy Chinese females (weighing ≥ 45 kg) and males (weighing ≥ 50 kg) aged ≥ 18 years who had a body mass index (BMI) between 19.0 and 26.0 kg/m2 (including the cut-off value) were eligible for participation in our study. The volunteers underwent a comprehensive medical examination involving medical history review, routine physical examinations, vital signs measurements [armpit temperature, pulse, and heart rate, as well as sitting blood pressure (BP)], laboratory investigations [blood routine, blood biochemistry, hepatitis, coagulation function, human immunodeficiency virus testing, urinalysis, syphilis specificity antibody screening, human chorionic gonadotropin (HCG) test, alcohol breathalyzer test, and drug screening], chest X-ray, and 12-lead electrocardiography (ECG). Individuals who exhibited acute or chronic illnesses, clinically significant diseases, allergic reactions to any component of ornidazole tablets, allergic constitutions, needle stick or blood draw reactions, smoking or alcohol abuse, drug abuse within the past 2 years, medication intake within 14 days before the initial dosing, participation in clinical studies within the past 3 months, blood loss or donation of 200 mL or more, and female participants who were pregnant, breastfeeding, or may be likely to become pregnant were excluded from the study.
Before participating in the study, all participants were informed by the clinical investigators of the research’s objectives, methodologies, and risk–benefit evaluations. Written informed consent was obtained from each participant before their participation in the study. Subjects were allowed to withdraw at any given point in time.
2.2 Study Design and Treatment
The present investigation was subjected to approval by the ethics committee of the Cangzhou Central Hospital (approval number 2021-061-01) and was conducted at Phase I Clinical Research Center of the Cangzhou Central Hospital from December 2021 to April 2022 following the International Conference on Harmonisation Good Clinical Practice Guideline [13] and the Guideline for Good Clinical Practice suggested by the National Medical Products Administration (NMPA) [14]. Before participating in this investigation, every participant provided written informed consent.
The primary objective of this single-center, randomized, open-label, two-period, two-sequence crossover, and single-dose bioavailability study for fasting or fed participants was to determine bioequivalence. There was a 7-day washout period between each administration. The participants in the study were randomly classified into either the test/reference (T/R) or reference/test (R/T) group in a 1:1 ratio for both the fed and fasted trials. Each participant was administered a single oral dose of either test or reference tablets, consisting of test tablets (two tablets × 0.25 g) or reference tablets (one tablet × 0.5 g), followed by 240 mL of warm water. The recruited participants in the fasting trial were subjected to a minimum of 10 h of overnight fasting. Additionally, the enlisted participants in the fed trial were administered a standard high-fat, high-calorie breakfast (800–1000 kcal) consisting of 52.1% fat, 17.7% protein, and 30.2% carbohydrate, 30 min before the ingestion of the medications. Participants were not allowed to drink additional water for 2 h after drug administration. In addition, 4 and 10 h following drug administration, each participant received a standardized meal during the study, participants were not allowed to consume alcoholic drinks, engage in vigorous exercise, or smoke.
2.3 Sampling of Blood
Blood samples were collected to the EDTA-K2 vacuum tube by inserting a cannula into the forearm vein prior to administration. In the fasted trial, pre-dose 4 mL blood samples were at baseline (0 h), and 0.25, 0.5, 1, 1.5, 2, 2.5, 3, 4, 5, 6, 8, 12, 24, 36, 48, and 72 h after the dose. Similarly, in the fed trial, pre-dose 4 mL blood samples were taken at baseline (0 h), and 0.25, 0.5, 1, 1.5, 2, 2.5, 3, 4, 5, 6, 8, 12, 24, 36, 48, and 72 h after the dose. Blood samples were centrifuged at 1700g at 4 °C for 10 min within 1 h of collection and kept at − 70 ± 10 °C within 2 h of collection until they were utilized for subsequent analysis purposes.
2.4 Analytical Method
The plasma concentrations of ornidazole were determined by a validated liquid chromatography tandem mass spectrometry (LC–MS/MS) method. The method involved protein precipitation and the quantitation of the target compounds, which was performed using a positive ion mode and multiple reaction monitoring (MRM). The lower limit of quantification (LLOQ) for the plasma assay was 0.100 μg/mL and the linear calibration range was 0.100–15.0 μg/mL. The overall precision of the ornidazole assay ≤ 2.9% coefficient of variation (CV).
2.5 Safety Evaluation
The safety evaluation approach involved tracking alterations in vital signs, physical examination results, and adverse events (AEs) incidence. Physical examination, 12-lead ECG, routine blood test, liver function, blood glucose, renal function, urinalysis, and female HCG test were performed in the laboratory at baseline and 72 h after the second dose administration. The study recorded the vital signs, including temperature, pulse rate, and blood pressure, of the participants at several timepoints. These timepoints included 1 day and 1 h before administration, and 2, 24, 48, and 72 h after each administration. Medical observations and spontaneous reports from individual participants were used to collect AEs that occurred during the study. According to the Medical Dictionary for Regulatory Activities, v20.0, all AEs were preferred terms and systemic organ classes.
2.6 Pharmacokinetic and Statistical Analysis
The PK analysis set included participants who completed all clinical trials without any substantial protocol deviations. The area under the curve from t = 0 to infinity (AUC0–∞); AUC from t = 0 to the final measurable concentration (AUC0–t); and maximum plasma concentration (Cmax) were the primary assessment indices. Time to Cmax (Tmax), terminal elimination rate constant (z), and half-life (t1/2) were the secondary assessment indices.
Analyst 1.6.3 workstation (Sciex, USA) was used to collect data and chromatogram integration, and regression analysis was performed to calculate the original concentration. Blood concentration analysis was conducted using Phoenix WinNonlin Software, v8.3, and the non-compartmental model using PKCS. Cmax and Tmax were calculated using the data obtained. AUC0–t was calculated using the linear trapezoidal rule. The terminal log-linear phase slope (Ke) was divided by the final measurable concentration (Ct) to determine the extrapolated area, which was added to the AUC0–t to get the AUC0–∞. The terminal log-linear phase slope was used to compute the t1/2 value, which was 0.693/Ke. The tested formulation’s relative bioavailability (F) was calculated based on the equation below: F = AUC0–t (test)/AUC0–t (reference) × 100%. To ascertain the effects of therapy, sequence, time, and individuals nested in sequence, the logarithm (ln)-transformed PK parameters (AUC0–t, Cmax, and AUC0–∞) were evaluated using a one-way analysis of variance following the NMPA regulatory standards. Tmax values were compared across groups using the Wilcoxon signed-rank test. The general linear model (GLM) approach was used to conduct the statistical analysis using SAS, V9.4 (SAS Institute Inc, Cary, North Carolina, license number 000063317058). The geometric mean ratio (GMR) AUC0–∞, AUC0–t, and Cmax of the two formulations were regarded to be bioequivalent when the disparities between the measured parameters were found to be negligible (P > 0.05) and the 90% confidence interval (CI) for these measurements ranged between 80.00 and 125.00%.
Parametric 90% CIs for the GMR between the two formulations (test–reference) were determined using the Schuirmann method.
3 Results
3.1 Participants
In total, 148 healthy Chinese participants were evaluated (Fig. 1). Both the fed and fasted trials involved 24 patients (17 men and 7 women and 16 men and 8 women, respectively). No participant included was excluded thereafter. Table 1 displays the demographic information for all the included participants.
3.2 Pharmacokinetic Properties
In the fed and fasted trials, all 24 participants completed both phases and were analyzed for pharmacokinetics.
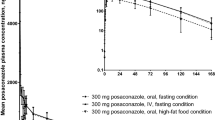
In the fed and fasted phases after an oral single dose of the reference and test ornidazole formulations, respectively, Figs. 2 and 3 depict ornidazole’s mean plasma concentration–time profiles. The PK characteristics for ornidazole are presented in Table 2.
For the bioequivalence assessment in the fast trial, the prime PK parameters comparison between the reference and test formulation revealed that the GMR (90% CI) values for AUC0–t, Cmax, and AUC 0–∞ were 100.97% (99.12–102.85%), 99.88% (90.63–110.08%), and 101.12% (99.17–103.11%), respectively. The defined equivalency margin of 80.00–125.00% included all the estimated 90% CIs. For the bioequivalence assessment in the fed trial, the key PK parameters comparison between the reference and test formulations revealed that the GMR (90% CI) values for AUC0–t, Cmax, and AUC0–∞ were 103.00% (100.94–105.11%), 101.90% (99.63–104.22%), and 102.99% (100.87–105.16%), respectively. The fed trial’s 90% CIs, similar to those of the fast trial, fell within the anticipated range of 80.00 to 125.00%. Tables 3, 4 and 5 provide the average bioequivalence assessments for ornidazole plasma PK parameters under fasting or fed settings, as well as the variance analyses for AUC0–∞, AUC0–t, and Cmax after logarithmic transformation.
3.3 Safety Assessment
The incidence rate of AEs during the fasting trial was 33.33%, with nine AEs recorded in eight participants. Laboratory testing detected 100% of these AEs, which were mild and did not need treatment. No SAEs occurred and no participants withdrew from the trial due to adverse events. Among them, the relationship between two AEs in two participants and the experimental drug was determined to be “possibly related” and recorded as adverse reactions. Table 6 summarizes the AE incidence during the fasted trial.
The AE incidence during the fed trial was 58.33%, with 23 AEs recorded in 14 patients. Laboratory examinations revealed that all these AEs were mild. Except for two cases of AEs, subjects were instructed to drink more warm water and keep warm, and no measures were taken for the other AEs. Among all the AEs, the relationship between five AEs in four subjects and the experimental drug was determined to be “possibly related” and recorded as adverse reactions. Table 7 summarizes the AE incidence in the fed trial.
4 Discussion
The PK characteristics of a test ornidazole tablet and a reference ornidazole tablet were compared in this research between fasting and fed healthy Chinese adult volunteers. All recruited participants engaged in the fed and fasted trials completed in the experiment, no participants withdrew or were excluded from the research. Both the bioequivalence analysis set and the pharmacokinetic analysis set comprised all of the participants.
The analysis, which was based on AUC0–t, Cmax, and AUC0–∞, showed that the PK characteristics of the two ornidazole formulations in healthy Chinese participants were comparable. The 90% CIs for the GMR values of AUC0–t, AUC0-∞, and Cmax were all within the NMPA bioequivalence acceptable range of 80.00 to 125.00% [15].
Furthermore, we examined the PK data from the fasting and fed trials and discovered that food affected Tmax but not AUC0–t or AUC0–∞ values for ornidazole (reference and test) formulations. Both the test and reference ornidazole formulations performed well after a conventional high-fat, high-calorie breakfast and increased Tmax by approximately 100 and 125%, respectively, but neither demonstrated a significant rise in AUC0–t and AUC0–∞ values. Thus, food seemed to reduce the rate of ornidazole absorption but not to enhance the extent of ornidazole absorption.
All AEs in this study were mild. We found the same number of AEs in both the test and reference ornidazole formulations. As a result, both the reference and test formulations were well tolerated by the participants in our research. Our study population tolerated both test and reference formulations. We further found seven AEs may relate to drugs in the fasting and fed trial. Among these cases, four AEs were liver function-related medical events such as alanine aminotransferase increased. This situation may be related to ornidazole metabolism mainly through the liver, suggesting that long-term use of ornidazole may lead to liver injury and appropriate adjustment of the dosage of ornidazole in liver patients. Early studies have confirmed that ornidazole is a substrate for P-gp [16], and long-term use of ornidazole has also been reported to cause severe hepatitis (severe hepatotoxicity as a result of extended use of rnidazole), so it is suggested that long-term administration of ornidazole should pay attention to monitoring liver function to prevent liver damage, and it suggests that we can further study the liver metabolism mechanism of ornidazole and the pharmacokinetic characteristics in people with liver damage.
5 Conclusion
Following the oral administration of 0.5 g preparation (two test tablets × 0.25 g or one reference tablet × 0.5g) under both fasted and fed conditions, no participants withdrew from the study due to AEs, and no serious AEs occurred, suggesting that both formulations were well tolerated and safe enough. The PK investigation revealed that the primary PK parameters (Cmax, AUC0–t, and AUC0–∞,) satisfied the People’s Republic of China regulatory standards, regardless of whether the medication was delivered fasting or fed. Furthermore, these parameters were found to be within the predefined equivalence margin of 80.00 to 125.00%. Consequently, it was established that the reference and test formulations exhibited bioequivalence. The 0.25 g ornidazole tablets produced by Zhejiang Aisheng Pharmaceutical Co., LTD. could serve as a viable and cost-effective substitute for the existing reference formulation in Chinese patients, offering comparable benefits.
References
Singh P, Mittal R, Sharma GC, et al. Ornidazole: comprehensive profile. Profiles Drug Subst Excip Relat Methodol. 2003;30:123–84. https://doi.org/10.1016/S0099-5428(03)30007-3.
Wei TT, Sun JH, Han LW, et al. Effects of the ornidazole enantiomers on the central nervous system: involvement of the GABAA receptor. Chem Biol Interact. 2015;242:163–9. https://doi.org/10.1016/j.cbi.2015.09.019.
Wang Y, Zhang P, Jiang N, et al. Simultaneous quantification of metronidazole, tinidazole, ornidazole and morinidazole in human saliva. J Chromatogr B. 2012;899:27–30. https://doi.org/10.1016/j.jchromb.2012.04.032.
http://www.medsafe.govt.nz. Available: July 17, 2014. http://www.medsafe.govt.nz/profs/datasheet/a/arrowornidazoletab.pdf.
Rajesh P, Gunasekaran S, Gnanasambandan T, et al. Experimental and theoretical study of ornidazole. Spectrochim Acta A Mol Biomol Spectrosc. 2016;153:496–504. https://doi.org/10.1016/j.saa.2015.08.032.
Buisson A, Chevaux JB, Bommelaer G, et al. Diagnosis, prevention and treatment of postoperative Crohn’s disease recurrence. Dig Liver Dis. 2012;44(6):453–60. https://doi.org/10.1016/j.dld.2011.12.018.
Emre S, Ahsen H, Aktaş A. Ornidazole-induced fixed drug reaction on sole: case report and review of the literature. Cutan Ocul Toxicol. 2017;36(3):294–6. https://doi.org/10.1080/15569527.2016.1249796.
Du J, Ma Z, Zhang Y, Wang T, Chen X, Zhong D. Enantioselective determination of ornidazole in human plasma by liquid chromatography–tandem mass spectrometry on a Chiral-AGP column. J Pharm Biomed Anal. 2013;12–01(86):182–8. https://doi.org/10.1016/j.jpba.2013.07.048.
Wei T, Sun J, Han L, Chen Ke, Wang Z, Ji H. Effects of the ornidazole enantiomers on the central nervous system: involvement of the GABAA receptor. Chem Biol Interact. 2015;5(242):163–9. https://doi.org/10.1016/j.cbi.2015.09.019.
Ramesh S, Kumar YS, Rao YM. Effect of ketoconazole on the pharmacokinetics of ornidazole—a possible role of P-glycoprotein and CYP3A. Drug Metab Drug Interact. 2006;22(1):67–77. https://doi.org/10.1515/dmdi.2006.22.1.67.
Ramamurthy L, Kulkarni RD, Chauhan BL, Singh A. Relative bioavailability of two brands of ornidazole in twelve healthy volunteers. J Assoc Physicians India. 2002;9(50):1149–52.
Wei M, Li T, Zhao CY, Zhang P, Sheng K, Liu Y, Yuan L. Bioequivalence of ornidazole tablets in Chinese healthy volunteers. Chin J Clin PharmacoI. 2010;26(11):822–5 (Serial No. 133).
The International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH). Guideline for good clinical practice. Available from: https://www.ich.org/products/guidelines/efficacy/efficacy-single/article/integrated-addendum.good-clinical-practice.html. Accessed 1 Mar 2019.
National Medical Products Administration. Guideline for good clinical practice. Available from: http://www.nmpa.gov.cn/WS04/CL2101/329583.html. Accessed 18 June 2020.
National Medical Products Administration. Center for Drug Evaluation. Guideline for bioavailability and bioequivalence studies of generic drug products. Available from: http://www.nmpa.gov.cn/WS04/CL2093/331454.html. Accessed 18 June 2020.
Ramesh S, Kumar YS, Rao YM, et al. Effect of ketoconazole on the pharmacokinetics of ornidazole—a possible role of P-glycoprotein and CYP3A. Drug Metabol Drug Interact. 2006;22(1):67–77.
Acknowledgements
We thank Zhejiang Aisheng Pharmaceutical Co., LTD and Beijing Fuyuan Pharmaceutical Co., Ltd. for their financial support and all the healthy volunteers in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Zhejiang Aisheng Pharmaceutical Co. Ltd, and Beijing Fuyuan Pharmaceutical Co. Ltd.
Conflicts of Interest/Competing Interests
Lijing Gao and Yingzi Pei are affiliated with Beijing Fuyuan Pharmaceutical Co., Ltd. The authors disclose no further conflicts of interest in this study. Zhejiang Aisheng Pharmaceutical Co., Ltd. is a subsidiary of Beijing Fuyuan Pharmaceutical Co. Ltd. This article was related to the 2020 Hebei Province medical science research project (no. 20200340).
Ethics approval
This study was approved by the ethics committee of the Cangzhou Central Hospital (approval number 2021-061-01).
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
Author contributions
Y.R.W. was principal investigator and contributed to all aspects of this study. Y.Y.H. and W.H.L. participated in conducting the study as a sub-investigator. Y.Z.P. and L.J.G. participated as an investigator and wrote the manuscript. L.Y.T. participated as a study assistant and contributed to manuscript drafting. X.Y.D., W.H.L., H.M.L., and L.Y.T. conducted the study as study assistants. H.M.L. contributed to study design and pharmacokinetic analysis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wang, Y., He, Y., Li, W. et al. Evaluation of Ornidazole Tablets Bioequivalence in Chinese Healthy Participants Under Fasted and Fed Conditions Using Pharmacokinetic Parameters. Drugs R D 24, 145–154 (2024). https://doi.org/10.1007/s40268-024-00457-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40268-024-00457-7