Abstract
The study aims to undertake a rapid systematic review with meta-analysis of the interventions used to promote adherence to asthma medications in adults who have asthma. Three databases (CINAHL, Web of Science, and Medline) were searched systematically up to February 2022, to identify the factors behind the non-adherent behavior of young adults with asthma using preventer medication. Manual searching was also undertaken to detect additional research. The team screened the titles and abstracts to ensure the eligibility of included studies. The full paper was retrieved for further screening and was extracted using an extraction tool. The literature search placed nine studies with a total sample number of 74,540 that were included in the three meta-analyses. Five studies were identified for inclusion in a meta-analysis conducted to assess the effect of the intervention on adherence. The meta-analysis revealed a significant difference in adherence proportion, in favor of the intervention. Interventions delivered through technology were found to significantly enhance adults’ adherence to asthma medications. This review also revealed that there is an obvious gap in the literature that specifically examined young adults aged 18–34 years about asthma medication adherence. This demonstrates the need for robust future research to focus on this demographic (18–34 years) to develop recommendations related to enhancing young adults’ adherence to asthma inhaler medication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adherence is the primary determinant in any treatment plan that aims for success. However, a substantial barrier to an effective therapeutic plan is the failure to adhere to that plan. The World Health Organization (WHO) defines adherence as the degree to which an individual’s performance complies with the instructions of the health care provider including taking medicine [1]. Adherence to medication can be influenced by the type of disease and patients’ health beliefs [2, 3]. For example, chronic diseases (e.g., asthma) require adherence to long-term therapy, and poor adherence can potentially undermine the benefits of the treatment [4]. Furthermore, patients’ health beliefs are formulated at varying ages for each individual [2, 3]. It can positively or negatively affect their adherence [5] as it is impacted by the health knowledge which is mostly acquired in adulthood and beyond.
Asthma is often diagnosed in children and young people [6]. Examining the young adults’ population is important as this age is the time they are learning health knowledge and formulating their health beliefs. They also learn how to be responsible for their own health routines over time as they develop and mature [5]. Significant emphasis in the literature on asthma is placed on how people adhere, do not adhere, or partially adhere, to their medication [7, 8]. It is important for health care professionals to understand the health beliefs of young adults with asthma and how these can be translated to improve medication adherence. Better adherence in young adults can possibly lead to better long-term asthma management and a reduction of complications related to poorly managed asthma. A review on the most common challenges to adherence to asthma medication by George and Bender [9] supports this proposition identifying that considering the patient’s beliefs when selecting the treatment plan can potentially improve patient’s adherence to their asthma medication. Therefore, it is important for young adults to acquire the right health knowledge and formulate their health belief accurately so that the burden of the disease is lessened as they grow older [10]. For the purpose of this review, the term young adult refers to persons 18–34 years as defined by the Australian Bureau of Statistics [11].
Regardless of the effectiveness of the preventer types of asthma inhalers, most patients fail to adhere to their treatment plan [4, 12, 13]. The burden placed on healthcare systems by non-adherent behaviors is clinically significant and creates substantial economic cost to the healthcare organization and to the individual suffering [14]. It has been acknowledged that a lack of medication adherence for people with asthma may lead to disease exacerbation, reduced quality of life, lost productivity, increased health care use, and even the risk of death [15]. Alarmingly, according to the Global Initiative for Asthma GINA [13] report, adherence of adults to asthma preventer medication is commonly only achieved in 50% of this population [7, 13]. Clinically, this disadvantage would be seen through disease exacerbation and recurrent asthma attacks. Non-adherence may also cause some social restrictions for instance, absence from social activities further adding to the burden experienced by individuals [16].
Research shows that adults with asthma tend to have negative attitudes which hamper their adherence to asthma medication [17] or a belief the medication is ineffective [18]. Smoking, which is considered to be an asthma trigger, is an example of adults’ negative behavior [19, 20]. Denial of the condition was also a feature in research related to the treatment and management of asthma in adults [21].
Background
Asthma medication has an essential role in relieving and preventing asthma disease and symptoms. Adherence to the recommended management plan allows people with asthma to live a normal life with minimal restrictions from the disease. There are two main types of medications used to manage asthma: preventer medications and symptom reliever medications, each designed to meet a specific goal.
Asthma Preventer Medications
Inhaled Corticosteroids (ICS) are an example of asthma preventer medication [22] which can be used alone as a preventer or in combination with other long acting bronchodilators such as Salmeterol that assists in reducing asthma exacerbations [23, 24]. ICS work as an anti-inflammatory agent to reduce inflammation, swelling, and mucus production in the lungs of asthma patients, providing a clear and open airway to reduce the likelihood of having an asthma attack [25]. Therefore, people with asthma are required to use them regularly regardless of whether they experience asthma symptoms or not [26].
Asthma Reliever Medications
Salbutamol (Ventolin) is an example of a rapid asthma reliever medication [27] that are available over the counter; therefore, patients can buy them without prescription. As asthma relievers produce immediate relief from an asthma exacerbation [28], they should always be available for the person to access in order to quickly relieve asthma symptoms [27]. It is well known needing to use a reliever inhaler more than twice a week suggests asthma is not being well managed and the person will need to start preventer medication if not previously recommended [13, 29].
Preventer and reliever inhalers should be used by following the recommended steps to get the maximum benefits of treatment. The steps to use inhalers differs depending on the device type [30] and methods of inhalation. Notably, the selection of the treatment devices (for example, Inhaler, Turbuhaler, and Diskus) should be based on person’s age, severity of disease, and the person’s functionality [31]. Specifically, the Turbuhaler device and the Diskus (which are used to deliver medicines in a powder form) may be difficult for some people to inhale, while inhalers in the form of aerosol are easier to be inhaled.
Given age is a consideration with type of asthma medication and may impact adherence; this review was aimed at examining adherence to asthma medication by young adults with asthma. In most cases, people develop asthma in childhood [32] with persistent asthma developing into adulthood; however, asthma diagnosed in people 20 years and older is known as adult asthma. In one study, the prevalence of asthma in young adults was estimated at approximately 6% [33] with only 52% (n = 1521) using medications daily. Health behaviors related to prevention and management are developed as people mature, making the young adult demographic an important population to examine to gain further insights to inform healthcare professions about strategies to promote adherence. The aim of this systematic review with meta-analysis was to examine the available evidence related to interventions that promote adherence in young adults with regard to inhaler medications (preventer) for asthma management and treatment.
Methods
A rapid systematic review with meta-analysis was undertaken examining adherence related to asthma medications in young adults who have asthma. The study was undertaken in accordance with Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) checklists [34] and has a Prospero ID No. equal to 154,740.
Types of Outcome Measures
The primary outcomes of interest were interventions that promoted adherence behaviors to asthma medications in young adults.
Types of Papers
Papers were included if they were written in English, reporting primary quantitative research, published in scientific journals, published up to February 2022, and examining asthma medication adherence in adults with asthma. Papers excluded included theses, editorials, blogs, grey literature, qualitative studies, commentaries, literature reviews, and books.
Type of Participants/Population
This review included studies reporting on young adults who had a diagnosis of asthma and were receiving asthma medication treatment.
Search Strategy
In order to do a rapid systematic review, three electronic databases (CINAHL, Web of Science, and Medline) were searched using the following search terms (Adherence, asthma, inhaler, young adults). Two different search strings were developed to broaden the search results and retrieve the maximum number of articles that discuss the same key concepts (see Boxes 1 and 2). Box 1 of the search string was assigned for CINAHL and Web of Science databases while box 2 was for Medline database. A manual search was also undertaken to locate further studies that may meet the eligibility criteria.
Box 1: Search string (1)
S1: asthma* OR "asthma* exacerbat*" |
S2: inhaler OR ventolin OR inhaled-corticosteroids OR “beta agonist” OR “B agonist” |
S3: adher* OR compliance OR concordance |
S4: "young adult*" OR "emerging adult*" |
S5: S1 AND S2 AND S3 AND S4 |
Box 2: Search string (2)
S1: asthma* OR "asthma* exacerbat*" OR ''air way inflammation*'' OR "chest tightness'' |
S2: inhaler* OR ventolin OR ‘’inhaled-corticosteroids’’ OR ''metered-dose inhaler'' OR ''asthma medication*''OR symbicort OR neubilis* ‘’B agonist’’ OR ‘’Beta agonist’’ |
S3: adher* OR compliance OR concordance |
S4: "young adult*" OR "emerging adult*"OR'' young people'' |
S5: S1 AND S2 AND S3 AND S4 |
Study Selection
The returned abstracts were initially screened by title and abstract. Following first tier screening, the remaining articles were subject to a full text read where the inclusion and exclusion criteria were applied and data from the studies that met our inclusion criteria were extracted. Consensus was sought between the three reviewers with any disagreements being discussed.
Data Extraction
Data extraction was completed independently by the research team using a standardized data extraction form created for the purpose of this project and devised from details in the Critical Appraisal Skills Program [35] checklists. The extraction form contained sections for data extraction related to the following: publication, title, journal name, inclusion criteria, aim of the study, location of the study, description of participants and study, type of intervention, blinding, comparison, outcomes measured, limitations and strengths of the study, and key findings. Data were extracted and the final inclusion of articles was determined by inclusion criteria and through discussion and consensus by all reviewers.
Assessment of Methodological Quality
The quality assessment of the research was critiqued using the CASP [35] methodological checklists. These checklists provide well-accepted standards for research methodological quality assessment.
Assessment of Bias in Included Studies
The assessment of risk of bias in the included studies was based on the risk of bias principles by Cochrane undertaken during the meta-analysis [36]. Bias risks were considered in relation to selection, performance, detection, and attrition, using the team judgment (see Table 1 below).
Statistical Methods
Comparative meta-analyses were constructed for randomized controlled trials and other comparative studies. All comparative meta-analyses derived comprised studies with continuous outcome measurements measured on the same scale. Hence, in all cases, the unstandardized difference in means (between intervention and treatment groups) was used as a summary statistic. Due to observed levels of clinical and content heterogeneity, random effects models were derived for all comparative meta-analyses, using the method of DerSimonian and Laird [37]. Following standard procedures, treatment groups in included studies with 2 or more treatment groups were combined to facilitate a single pairwise analysis. Sub-group analyses and meta-regressions were not planned a priori or subsequently undertaken.
For all meta-analyses, statistical heterogeneity was assessed using Cochran’s Q statistic, which approximately follows a χ2 distribution on n-1 degrees of freedom. The corresponding I2 statistic and the between-study variance of the intervention effect (τ2) were also derived. A Z-test for overall effect was also conducted in all cases. Results were summarized using forest plots. Funnel plots were not constructed due to the limited number of studies included in the meta-analyses. All meta-analyses were conducted using the Stata statistical software (Version 14 I/C) (33).
Results
There were no studies that separated the age groups to delineate the young adults and therefore, the focus adjusted to include all adults and young adults were included within these samples.
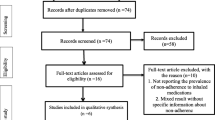
Records identified through database searching were n = 291, and additional records identified through other sources were n = 40. Records after removing duplicates were n = 299 (see Fig. 1). The titles and abstracts of the final number of studies were screened based on the inclusion criteria. The number of records excluded were n = 209 due to several reasons such as not written in English, could not get the full text, and not related to the topic. After screening, n = 90 papers were eligible for full text screening. After screening against the inclusion criteria and eligibility for meta-analysis, n = 9 articles were included in the analysis. A table with the details of the included articles is provided in Table 2.
PRISMA flow chart for screening [34]
Results of Studies Included in Meta-analysis
Five studies considered the effect of an intervention to improve adherence in randomized controlled trials, measuring adherence based on the proportion of prescribed inhaler doses taken over the duration of the study period.
-
Bender, Apter [38] tested the effectiveness of a theory-based interactive voice response in 50 adult patients (aged 18 to 65 years) over 10 weeks.
-
Foden and Hand [39] tested the effectiveness of the use of combination of ICS/LABA inhalers compared with ICS inhalers alone in 82 adult patients over 1 year.
-
Petrie, Perry [40] tested the effectiveness of a text messaging program on 147 older children and young adult (aged 16 to 45 years) patients over 18 weeks.
-
Strandbygaard, Thomsen [41] tested the effectiveness of a text messaging program on 26 young adult patients (aged 18 to 45 years) over 60 days (8.5 weeks).
-
Vollmer, Feldstein [42] tested the effectiveness of a health-information technology-based intervention using the speech recognition software on 3171 adult patients (aged 18 to 98 years) over 18 months.
Adherence proportions in treatment groups ranged from 40.0 [42] to 81.5% [41]. Adherence proportions in control groups ranged from 38.0 [42] to 70.1% [41]. All studies reported higher levels of adherence in their intervention groups.
In this meta-analysis, a random effect was chosen due to the assumption that individual effects were uncorrelated with the independent variables. A random effects meta-analysis conducted on study data revealed that the synthesized estimate for the unstandardized difference in means between intervention and control groups was 0.14 (95% confidence interval 0.04 to 0.24), with the higher estimate for intervention groups. A Z-test for overall effect revealed evidence that this difference was statistically significant at the 5% significance level (Z = 2.64, p = 0.008).
Cochran’s Q test revealed strong evidence for statistical heterogeneity (χ2(4) = 26.1; p < 0.001). The I2 statistic was 84.7%, indicating substantial statistical heterogeneity. The τ2 statistic (between-study variance) was 0.0102. Results are summarized in a forest plot (Fig. 2).
Two studies considered the effect of an intervention to improve adherence in randomized controlled trials, measuring adherence based on the Morisky medication adherence scale (MMAS-4) score reported by study participants; with scores reported objectively rather than converted to proportions of patients deemed to be adherent.
-
Giraud, Allaert [43] tested the effectiveness of pharmacist inhaler training in adult patients (aged 18 to 94 years) over 1 month.
-
Guenette, Breton [44] tested the effectiveness of an integrated care program in adult and child patients (aged 12 to 45 years) over 12 months.
A random effects meta-analysis conducted on study data revealed that the synthesized estimate for the unstandardized difference in means between intervention and control groups was -0.16 (95% confidence interval -0.54 to 0.21). A Z-test for overall effect revealed no evidence that this difference was statistically significant at the 5% significance level (Z = 0.86, p = 0.392).
Cochran’s Q test revealed evidence for statistical heterogeneity (χ2(1) = 5.48; p = 0.019). The I2 statistic was 81.8%, indicating high statistical heterogeneity. The τ2 statistic (between-study variance) was 0.059. Results are summarized in a forest plot (Fig. 3).
Two studies considered the effect of an intervention to improve adherence in randomized controlled trials, measuring adherence based on the proportion of patients deemed to be adherent.
-
Garcia-Cardenas, Sabater-Hernandez [45] tested the effectiveness of a protocol-based intervention in 336 adult patients (aged 18 to 78 + years) over 6 months; reporting the proportion of patients considered adherent according to the MMAS-4 scale.
-
Wu, Butler [46] tested the effectiveness of controller medications in 69,652 adult and child patients (aged 0 to 65 + years); reporting the proportion of patients considered “primary adherent” according to whether the first prescription was filled within 30 days.
A random effect meta-analyses conducted on study data revealed that the synthesized estimate for the unstandardized difference in means between intervention and control groups was 0.15 (95% confidence interval − 0.06 to 0.36), with the higher estimate for intervention groups. A Z-test for overall effect revealed no evidence that this difference was statistically significant at the 5% significance level (Z = 1.39, p = 0.164).
Cochran’s Q test revealed strong evidence for statistical heterogeneity (χ2(1) = 17.5; p < 0.001). The I2 statistic was 94.3%, indicating substantial statistical heterogeneity. The τ2 statistic (between-study variance) was calculated to be 0.0222, reflecting a high proportion of variance between studies compared to within studies. Results are summarized in a forest plot (Fig. 4).
Discussion
This systematic review included three meta-analyses with a total combined sample of n = 74,540. We are presuming that our target population was represented in the samples of the included studies; however, the papers did not differentiate between age categories. Due to this low specificity, the results will be discussed as an adult demographic rather than young adults 18–34 years old. Also, due to heterogeneity among studies, caution is recommended with interpreting the results. The results of the meta-analysis provide evidence regarding the improvements to adherence through various interventions. Specifically, the first meta-analysis (see Fig. 2) revealed statistical significance in five studies [38,39,40,41,42]. These studies examined the effect of two different types of interventions (health technologies and medications) used to improve adherence to asthma inhaler medication. Four of these studies used various health technologies to improve adherence to adult patients with asthma [38, 40,41,42]. These interventions included a theory-based interactive voice response, a text messaging program, and health information technology. Most interventions permitted individuals to self-monitor medication use and encouraged adherence behavior. Participants involved in studies with the health technological intervention [38, 40,41,42] had significantly higher adherence compared with the control groups. One study, Foden and Hand [39], used medications as an intervention and tested the effectiveness of the use of the combination of inhaled Corticosteroids/Long Acting Beta 2 agonist (ICS/LABA) inhalers compared with inhaled Corticosteroids (ICS) inhalers alone.
The studies in the first analysis (see Fig. 2) that used health technologies as an intervention to improve adherence in adults with asthma were found to be significant. Bender, Apter [38] examined the efficacy of theory-based interactive voice response (IVR) in 50 adult patients using asthma preventer medication over 10 weeks. The IVR system comprised of multiple technologies working as one system to plan, make, collect, and record programmed phone calls. The system could also make and receive phone calls, ask participants questions, and provide information based on each individual query. The IVR intervention was based on the benefit-risk model of health behavior that considers it is essential to address the patient’s belief related to the benefits of asthma preventer inhaler before any alteration in adherence behavior occurs. Hence, to change patient’s beliefs about why asthma preventer medication is beneficial, content within IVR intervention was developed to deliver educational messages. Adherence was higher among patients in the IVR group. Likewise, Vollmer, Feldstein [42] tested the effectiveness of a health-information technology-based intervention using phone messages, specifically, the speech recognition software in 3171 adult patients (aged 18 to 98 years) over 18 months. Interactive voice recognition (IVR) was used to enhance medication top-ups and improve ICS adherence. It included three types of IVR calls that were about 2–3 min in duration. Each call planned to be either a reminder or delayed refill or initiator. Scanning the electronic medical record (EMR) monthly allowed the researchers to ascertain which participant needed which type of IVR calls. For example, the refill reminder went to the participant who ran out of stock of ICS by calculating the number of doses the participant had been supplied divided by the number of days needed to finish the doses assuming that the patient was using the medication appropriately. Using this intervention, ICS adherence increased significantly for the intervention group. Adherence interventions based on health information technology demonstrate substantial support for medication adherence predominantly in chronic diseases such as asthma. Additionally, the successful application of technology-based interventions endorses further functioning of individuals’ self-management and accordingly better control of the disease.
Petrie, Perry [40] tested the effectiveness of a text messaging program as an intervention to improve adherence in 147 older children and adults (aged 16 to 45 years) patients over 18 weeks. In their study, participants received a personalized text message that was tailored to their previous disease and medication beliefs. A bank of 166 messages was created and participants’ beliefs were assessed at the beginning of the study while the adherence rate was at 6, 12, and 18 weeks as well as after 6 and 9 months. Participants received text message twice a day for the first 6 weeks and one text message for the next 6 weeks. While from week 13 to 18, the participants received text message three times a week. At the end of week 18, intervention group significantly improved adherence compared to control group. Strandbygaard, Thomsen [41] also tested the effectiveness of text messaging reminders to take medication in n = 26 adult patients (aged 18 to 45 years) over 60 days. Adherence improved among the intervention group with an absolute difference between the two groups. The technology field has been developed significantly to become a tool for improving adherence to long-term treatment regimens. For future research, it is recommended to focus on improving the adherence using technology devices that proved to be effective and accepted by most people.
Foden and Hand [39] tested the effectiveness of the use of a combination of ICS/LABA inhalers compared with ICS inhalers alone in 82 adult patients over 1 year. The participants had either ICS or combination ICS/LABA and were within the age group of 18–45 years. The study was retrospective so participants’ data about the number of inhalers during the last year was extracted from their medical records. The number of inhalations taken per year was divided by the yearly number of prescribed inhalations and multiplied by 100 to calculate the adherence as a percentage. Their results showed participants with a combination of ICS/LABA had substantially higher adherence scores in comparison to those on ICS alone.
Interventions like a theory-based interactive voice response, a text messaging program, and health information technology delivered through technology were found to be effective in enhancing medication adherence in adults with asthma. The first meta-analysis provided some evidence that health technology was a good intervention for the adult demographic and could help improve adherence with asthma inhaler medication.
The second meta-analysis only included two studies (see Fig. 3) where the researchers measured adherence using the Morisky medication adherence scale. Although meta-analysis was undertaken, there were differences in the studies that could account for a lack of statistical significance in the analysis. Specifically, Guenette, Breton [44] conducted the study over a period of 12 months while the duration of the study of Giraud, Allaert [43] was only for 1 month. In addition, adherence was measured using 2 measures in Guenette et al. study (Morisky & medication possession ratio) while in Giraud, Allaert [43] study, adherence was measured by Morisky scale only. Therefore, these differences between the two studies imply that the second meta-analysis did not present any significant evidence.
Two studies [45, 46] in the third meta-analysis considered the effect of an intervention to improve adherence by measuring adherence based on the proportion of patients deemed to be adherent. Since only 2 studies measured adherence grounded in this concept, the meta-analysis (see Fig. 4) did not produce a significant result. Garcia-Cardenas, Sabater-Hernandez [45] conducted a randomized control trial to examine the effectiveness of a protocol-based intervention in n = 336 adult patients (aged 18 to 78 + years) divided into two groups (control and intervention). The study used one type of preventer medication Symbicort which is a combination of Budesonide (ICS) and Formoterol (LABA) over 6 months; reporting the proportion of patients considered adherent according to Morisky scale which classifies patient as adherent or non-adherent [45]. In contrast, the intervention in the Wu, Butler [46] study was educational, as it aimed to educate patients with asthma on how to use their inhaler with different strategies based on the type of non-adherence. Education about inhaler technique was provided through verbal and written as well as a physical demonstration. Wu, Butler [46] tested the effectiveness of 3 types of controller medications (ICS, Leukotriene antagonists (LA), ICS/LABA) in n = 69,652 adult and pediatric patients (aged 0 to 65 + years) over 12 months; reporting the proportion of patients considered “primary adherent” according to whether the first prescription was filled within 30 days. However, the meta-analysis of the combination of these two studies did not offer any significant results.
Clinical Implications
The results of the meta-analyses in this review provides evidence for the use of technology-based interventions to improve adult’s adherence with asthma medications. In the health technology space, other authors have found similar types of technologies such as mobile and internet-based initiatives, which have worked with adults with regards to smoking cessation, adherence to antiretroviral medications, and promoting mental health [47,48,49] demonstrating the broad efficacy of this type of intervention. The use of technology to improve health could extend to the young adult demographic as they are known heavy users of technology, especially for entertainment, connecting with friends, and in searching for information related to their health [47]. Drawing on previous examples of using technology for health with success, and in light of our results of this systematic review, using technology to promote asthma medication adherence is recommended to improve management of this chronic condition.
Limitation of the Systematic Review and Meta-analysis
The systematic review with meta-analysis has several limitations. First, the inclusion criteria were limited to studies written in English potentially reducing the returned articles from the search. Secondly, since meta-analysis was undertaken, some articles were excluded on the basis of being unsuitable/not comparable for the purposes of meta-analysis. Another important limitation was the low specificity in the returned studies which did not delineate in age categories that directed us to discuss the results as an adult demographic rather than young adults (18–34 years). However, this limitation also presents as a gap in the evidence base related to the young adult demographic and asthma medication adherence.
Conclusions
This systematic review identified an obvious gap in the literature; that there are no studies that specifically examined young adults aged 18–34 years regarding asthma medication adherence. This demonstrates that future research needs to focus on this demographic to develop recommendations related to enhancing young adult’s adherence to asthma inhaler medication. Also, the findings of the meta-analysis provide some evidence that technological interventions could enhance the adherence of adults to asthma medication. However, there appeared an obvious gap in the evidence related to young adults and adherence to asthma medication where future research addressing the causes of non-adherence in this demographic could open new insights into how to develop effective interventions accepted by this demographic.
Data Availability
Not applicable.
Code availability
Not applicable.
References
WHO. World Health Organization. 2003 [cited 2019 22/5/2019]; Available from: https://www.who.int/chp/knowledge/publications/adherence_full_report.pdf?ua=1.
Soones TN, et al. Pathways linking health literacy, health beliefs, and cognition to medication adherence in older adults with asthma. J Allergy Clin Immunol. 2017;139(3):804–9.
Sweileh WM, et al. Influence of patients’ disease knowledge and beliefs about medicines on medication adherence: findings from a cross-sectional survey among patients with type 2 diabetes mellitus in Palestine. BMC Public Health. 2014;14(1):94.
Boulet L-P, et al. Adherence: the goal to control asthma. Clin Chest Med. 2012;33(3):405–17.
Schwarzer R, Lippke S, Luszczynska A. Mechanisms of health behavior change in persons with chronic illness or disability: the Health Action Process Approach (HAPA). Rehabil Psychol. 2011;56(3):161.
Dharmage SC, Perret J, Custovic A. Epidemiology of asthma in children and adults. Front Pediatr. 2019;7:246.
Engelkes M, et al. Medication adherence and the risk of severe asthma exacerbations: a systematic review. Eur Respir J. 2015;45(2):396–407.
Allegra L, et al. Real-life prospective study on asthma control in Italy: cross-sectional phase results. Respir Med. 2012;106(2):205–14.
George M, Bender B. New insights to improve treatment adherence in asthma and COPD. Patient Prefer Adherence. 2019;13:1325.
Roberts, G., et al., EAACI Guideline on the effective transition of adolescents and young adults with allergy and asthma. J Allergy, Asthma, 2020.
ABS. Australian Bureau of Statistics. 2013 [cited 2019 1 / 9 / 2019]; Available from: http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/4102.0Main+Features40April+2013
Price D, et al. Establishing the relationship of inhaler satisfaction, treatment adherence, and patient outcomes: a prospective, real-world, cross-sectional survey of US adult asthma patients and physicians. World Allergy Organ J. 2015;8(1):1.
GINA. Global strategy for asthma managment and prevention. 2017 [cited 2019 1/10]; Available from: https://ginasthma.org/.
Cutler, R.L., et al., Economic impact of medication non-adherence by disease groups: a systematic review. BMJ open, 2018. 8(1): p. e016982.
Zeiger, R.S., et al., Utilization and costs of severe uncontrolled asthma in a managed-care setting. The Journal of Allergy and Clinical Immunology: In Practice, 2016. 4(1): p. 120–129. e3.
Cole, S., C. Seale, and C. Griffiths, ‘The blue one takes a battering’ why do young adults with asthma overuse bronchodilator inhalers? A qualitative study. BMJ open, 2013. 3(2): p. e002247.
Lee SJ, Pincus KJ, Williams AA. Behavioral influences on prescription inhaler acquisition for persistent asthma in a patient-centered medical home. Res Social Adm Pharm. 2016;12(5):789–93.
De Simoni, A., et al., What do adolescents with asthma really think about adherence to inhalers? Insights from a qualitative analysis of a UK online forum. BMJ open, 2017. 7(6): p. e015245.
Desai M, Oppenheimer JJ. Medication adherence in the asthmatic child and adolescent. Curr Allergy Asthma Rep. 2011;11(6):454.
Ahmed AE, et al. Factors associated with poor asthma control among asthmatic patient visiting emergency department. Clin Respir J. 2014;8(4):431–6.
Bitsko MJ, Everhart RS, Rubin BK. The adolescent with asthma. Paediatr Respir Rev. 2014;15(2):146–53.
Barnes PJ. Corticosteroid resistance in patients with asthma and chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2013;131(3):636–45.
Gershon AS, et al. Combination long-acting β-agonists and inhaled corticosteroids compared with long-acting β-agonists alone in older adults with chronic obstructive pulmonary disease. JAMA. 2014;312(11):1114–21.
Stempel DA, et al. Serious asthma events with fluticasone plus salmeterol versus fluticasone alone. J New England J Med. 2016;374(19):1822–30.
Barnes PJ. Inhaled corticosteroids. Pharmaceuticals. 2010;3(3):514–40.
O’Byrne PM, Jenkins C, Bateman ED. The paradoxes of asthma management: time for a new approach? Eur Respir J. 2017;50(3):1701103.
Reddel H. Rational prescribing for asthma in adults–written asthma action plans. Aust Prescr. 2012;35:78–81.
Albertson TE, Sutter ME, Chan AL. The acute management of asthma. Clin Rev Allergy Immunol. 2015;48(1):114–25.
Beasley R, et al. Combination corticosteroid/β-agonist inhaler as reliever therapy: a solution for intermittent and mild asthma? J Allergy Clin Immunol. 2014;133(1):39–41.
Sanchis J, et al. Inhaler devices–from theory to practice. Respir Med. 2013;107(4):495–502.
Scichilone N, et al. Patient perspectives in the management of asthma: improving patient outcomes through critical selection of treatment options. Patient Prefer Adherence. 2010;4:17.
ALA, A.L.A. Asthma and children fact sheet. 2020 [cited 2020 23/8]; Available from: https://www.lung.org/lung-health-and-diseases/lung-disease-lookup/asthma/learn-about-asthma/asthma-children-facts-sheet.html.
Arias SJ, et al. Prevalence and features of asthma in young adults in urban areas of Argentina. Archivos de Bronconeumología (English Edition). 2018;54(3):134–9.
Moher D, L.A., Tetzlaff J, Altman DG, The PRISMA Group (2009). PRISMA 2009 Checklist. 2009 25/10/2019]; Available from: http://prisma-statement.org/documents/PRISMA%202009%20checklist.pdf.
CASP, C.A.S.P. Critical Appraisal Skills Programme. 2018 22/9/2019]; Available from: https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist-2018.pdf.
Higgins, J.P. and D.G. Altman, Assessing risk of bias in included studies. Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series, 2008: p. 187–241.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Bender BG, et al. Test of an interactive voice response intervention to improve adherence to controller medications in adults with asthma. J Am Board Family Med. 2010;23(2):159–65.
Foden J, Hand CH. Does use of a corticosteroid/long-acting beta-agonist combination inhaler increase adherence to inhaled corticosteroids? Primary Care Resp J J Gen Pract Airways Group. 2008;17(4):246–7.
Petrie KJ, et al. A text message programme designed to modify patients’ illness and treatment beliefs improves self-reported adherence to asthma preventer medication. Br J Health Psychol. 2012;17(1):74–84.
Strandbygaard U, Thomsen SF, Backer V. A daily SMS reminder increases adherence to asthma treatment: a three-month follow-up study. Respir Med. 2010;104(2):166–71.
Vollmer, W.M., et al., Use of health information technology to improve medication adherence. Am J Managed Care, 2011. 17(12 Spec No.): p. SP79-SP87.
Giraud V, Allaert F-A, Roche N. Inhaler technique and asthma: feasability and acceptability of training by pharmacists. Respir Med. 2011;105(12):1815–22.
Guenette L, et al. Effectiveness of an asthma integrated care program on asthma control and adherence to inhaled corticosteroids. J Asthma Off J Assoc Care Asthma. 2015;52(6):638–45.
Garcia-Cardenas V, et al. Effect of a pharmacist intervention on asthma control. Cluster Random Trial Resp Med. 2013;107(9):1346–55.
Wu AC, et al. Primary adherence to controller medications for asthma is poor. Ann Am Thorac Soc. 2015;12(2):161–6.
Ellis LA, et al. Young men’s attitudes and behaviour in relation to mental health and technology: implications for the development of online mental health services. BMC Psychiatry. 2013;13(1):119.
Free, C., et al., The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Medicine, 2013. 10(1): p. e1001362.
Nicholas J. The role of internet technology and social branding in improving the mental health and wellbeing of young people. Perspect Public Health. 2010;130(2):86–90.
Acknowledgements
This paper and the research behind it would not have been possible without the exceptional support of my supervisors Karen-Leigh Edward and Loretta Garvey. Their knowledge and exacting attention to detail have been an inspiration and kept my work always on track. Also, I would like to express my special thanks of gratitude to Dr. John Stephenson who has a great role in doing the meta-analysis.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Contributions
First author.
Name: Amal Al Wadhahi.
Percentage of contribution: 80%
Second author.
Name: Loretta Garvey.
Percentage of contribution: 5%
Third author.
Name: John Stephenson.
Percentage of contribution: 5%
Forth author.
Name: Karen-Leigh Edward.
Percentage of contribution: 10%
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Messages
1. There is an obvious gap in the literature that specifically examined young adults aged 18–34 years with regard to asthma medication adherence.
2. Future research needs to focus on this demographic (18–34 years) to develop recommendations related to enhancing young adult’s adherence to asthma inhaler medication.
3. The study presents good evidence for the use of technology-based interventions to improve adherence of adults with asthma.
4. The use of technology to improve health can be well accepted in the young adult demographic as they are usually heavy users of technology.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alwadhahi, A., Garvey, L., Stephenson, J. et al. Asthma Inhaler Adherence in Adults: a Rapid Systematic Review with Meta-analysis. SN Compr. Clin. Med. 4, 84 (2022). https://doi.org/10.1007/s42399-022-01161-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-022-01161-w