Abstract
Endometriosis-associated intestinal tumors represent malignant transformation of gastrointestinal endometriosis. Clinical features are similar to colon tumor with abdominal or pelvic pain, dyschezia, or bloody stools. Intestinal occlusion or perforation has also been described as a first presentation. The diagnosis is often postoperative, and it is based on specific immunohistochemical patterns (CK7+/CK20−). We present a rare case of a woman with a malignant transformation of an endometriotic lesion of the sigmoid colon, who underwent emergency surgery for intestinal occlusion. She underwent an exploratory laparotomy and Hartmann resection. The immunophenotypic analysis of the specimens revealed the following pattern: CK20−, CK7+, compatible with the diagnosis of endometrioid adenocarcinoma. Endometrioid carcinoma is a rare tumor, difficult to diagnose preoperatively because of similar symptoms of sigmoid carcinoma. A high index of suspicion in conjunction with careful histological and immunohistochemical examination (CK7, CK20, CDX2, CD10, ER, and PR) is important for establishing a correct diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endometriosis represents a common gynecologic condition. It is defined as the presence of endometrial glands in extrauterine sites [1], like ovary, fallopian tubes, cervix, pouch of Douglas, small and large intestines, recto vaginal septum, and the appendix [2]. 5–15% of women with endometriosis could suffer intestinal endometriosis. Bowel endometriosis is located especially in the sigmoid colon and the rectum (90%) [3], and it can rarely turn into intestinal tumors [4,5,6]. In literature, we found no more than 50 cases [7]. Hyperestrogenism is a possible risk factor for the development of cancer from endometriosis [8]. Endometriosis-associated intestinal tumors (EAITs) may present with non-specific symptoms or manifest with bowel obstruction, intussusception, or perforation [4, 5]. The differential diagnosis includes any neoformation that invades the intestinal wall as well as colorectal carcinoma, especially in the presence of mucosal disruption. The definitive diagnosis is established by immunohistochemical analysis, which distinguishes between endometrial adenocarcinoma (CK7+/CK20−) and intestinal adenocarcinoma (CK20+/CK7−) [9]. Five-year overall survival reaches 82—100% [10]. In this article, we present a rare case of a woman with a malignant transformation of an endometriotic lesion of the sigmoid colon, who underwent emergency surgery for intestinal occlusion.
Case Report
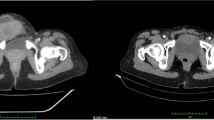
A 54-year-old nulliparous postmenopausal woman was admitted to our emergency room with acute and persistent abdominal pain, vomiting, and intestinal blockage lasting two days. The patient had a past medical history of asymptomatic endometriosis ovarian cyst and fibromatous uterus discovered only 2 months before the presented acute event. She had no past familiar history of malignancies. Clinical examination revealed diffuse abdominal tenderness mainly situated in the left iliac fossa. An urgent contrast enhanced-CT (Fig. 1) showed intestinal obstruction with concentric thickening of the sigma and severe proximal distention of the colon with air-fluid levels. A colonoscopy was performed and revealed an edematous sigmoidal mucosa, situated above 35–40 cm from the anal margin without macroscopic lesions (Fig. 2). Endoscopic biopsies of this tract were negative for neoplastic cells. The patient was treated without surgery initially; after two days, the clinical conditions worsened with an increase in abdominal pain. Exploratory laparotomy was performed. It showed severe intestinal distention due to a stenosis of sigma, which appeared edematous and ischemic. No further lesions were observed in the uterine wall or in the left ovary. Left hemicolectomy and colostomy were performed, and the surgical resected specimens were sent to histological examination. Pathological specimens consisted of a stenosis lesion occupying about 2/3 of the lumen, extended for 3.5 cm. The histological specimens revealed the presence of a lesion, which microscopically involved the muscularis propria and the pericolic adipose tissue. In addition, in the surrounding pericolic adipose tissue, foci of endometriosis were observed. The immunophenotypic analysis revealed the following pattern: CK20−, CDX2−, PAX8+, CK7+, ER +/−, Vim+ (Fig. 3). These findings were compatible with endometrioid adenocarcinoma. Two of the 19 examined pericolic lymph nodes were metastatic. The patient received adjuvant chemotherapy consisting of paclitaxel 175 mg/mq + AUC5 carboplatin. A staging CT was performed after 6 months, and it was negative for neoplastic lesions; therefore, the patient underwent Hartmann reversal and bilateral hysteroannessectomy, in order to remove any possible residual endometriosis focus. The final histological diagnosis after surgery was clear cells ovarian cancer, without uterine repetitions and foci of endometriosis, unlike the histological analysis performed on the first surgery and with the immunohistochemical pattern: PAX ì8N, CK7+, CK20−, and CDX2−. Therefore, the two tumors were considered as two different primary tumors: the first one was an EAIT and the second one was an ovarian cancer.
Discussion
Any extragonadal site of endometriosis can turn into malignancies. EAITs (endometriosis-associated intestinal tumor) are most commonly found among women aged 30–60 years, earlier than most colorectal cancers [7]. Hyperestrogenism is considered a risk factor for the development of cancer from endometriosis [8]. The pelvic peritoneum, rectovaginal septum, vagina, and colorectal serosa are the most common site. Among the EAITs, the rectosigmoid colon is the most common site, particularly in the anti-mesocolic border of the rectosigmoid colon [7]. The initial symptoms or signs are abdominal and/or pelvic pain, pelvic mass, and vaginal bleeding [11]. It can also begin acutely with small or large bowel obstruction due to a mass or acute abdomen due to intussusception or perforation, as occurred in our case [7].
Endometrioid adenocarcinoma can simulate a colorectal carcinoma, as in the case of our patient. Analyzing the preoperative CT images (Fig. 1), it is very difficult distinguishing endometrioid carcinoma from adenocarcinoma. The diagnosis is based on histological and immunohistochemical analysis. In fact, primary colonic adenocarcinomas involved the mucosal layer and may be associated with precancerous lesions, like adenomatous changes or a neoplastic polyp. On the contrary, endometrioid adenocarcinomas usually show initial involvement of the outer layers of the colon; the mucosa is frequently normal or shows only minimal changes endoscopically [12]. In this case, the mucosa of the sigmoid was edematous, without macroscopic lesions. Microscopically, squamous differentiation within a glandular neoplasm of the colon is a characteristic strongly suggesting the endometriotic origin of a tumor. Immunohistochemical staining for CK7 and CK20 is also useful in the differential diagnosis of some carcinomas of epithelial origin. Among primary colonic adenocarcinomas, 75–95% have a CK7-negative and CK20-positive phenotype, whereas 80–100% of endometrioid adenocarcinomas have a CK7-positive and CK20-negative phenotype [9]. Occasional cases of endometrioid adenocarcinoma of the ovary could be positive to CD 2. [13]. Regarding treatment, there are no precise guidelines, and it is highly individualized. Patients who do not manifest metastases can undergo surgery with a complete resection of macroscopic disease. This was also the treatment selected in this case, because dissemination of the tumor was not revealed during laparotomy. The therapeutic value of chemoradiation for metastatic EAIT is of unclear value. The situation is similar in the adjuvant setting after complete resection of disease because of only sporadic reports [14]. The prognosis of EAITs is associated with the stage of endometriosis. A 100% 5-year survival rate has been noted for malignant transformation in extragonadal endometriosis, confined to the site of origin. Disseminated intraperitoneal disease has a poor prognosis; the 5-year survival rate is only 12.5% [15].
Conclusions
In this article, we report a case of EAIT with clinical features simulating a primary colonic carcinoma, including occlusion and bowel perforation. These tumors can be diagnostically challenging because they can resemble common primary neoplasms of the gastrointestinal tract clinically and pathologically. A high index of suspicion in conjunction with careful histological and immunohistochemical examination (CK7, CK20, CDX2, CD10, ER, and PR) is important for establishing a correct diagnosis.
Data Availability
The original contributions presented in the study are included in the supplementary material; further inquiries can be directed to the corresponding author.
Code Availability
Not applicable.
References
Sanchez Cifuentes A, Candel Arenas MF, Albarracín M-BA. Intestinal endometriosis. Our experience. Rev Esp Enferm Dig. 2016;108:524–5. https://doi.org/10.17235/reed.2016.4292/2016.
Verma R, Osborn S, Horgan K. Endometrioid adenocarcinoma of caecum causing intussusception. Case Rep Surg. 2013;2013:1–3. http://www.hindawi.com/journals/cris/2013/714126/
Rodriguez-Lopez M, Bailon-Cuadrado M, Tejero-Pintor F, Choolani E, Fernandez-Perez G, Tapia-Herrero A. Ileocecal intussusception extending to left colon due to endometriosis. Ann R Coll Surg Engl. 2018;100(3):e62–3.
Hoang CD, Boettcher AK, Jessurun J, Pambuccian SE, Bullard KM. An unusual rectosigmoid mass: Endometrioid adenocarcinoma arising in colonic endometriosis: Case report and literature review. Am Surg. 2005;71(8):694–7.
Li N, Zhou W, Zhao L, Zhou J. Endometriosis-associated recto-sigmoid cancer: A case report. BMC Cancer. 2018;18(1):905.
García-Marín JA, Pellicer-Franco EM, Soria-Aledo V, Mengual-Ballester M, Valero-Navarro G, Aguayo-Albasini JL. Malignant degeneration of rectal endometriosis. Rev Esp Enferm Dig. 2015;107(12):761–4.
Palla V-V, Karaolanis G, Bliona T, Katafigiotis I, Anastasiou I, Hassiakos D. Endometrioid adenocarcinoma arising from colon endometriosis. SAGE Open Med Case Rep. 2017;5:2050313X1774520.
Zanetta GM, Webb MJ, Li H, Keeney GL. Hyperestrogenism: A relevant risk factor for the development of cancer from endometriosis. Gynecol Oncol. 2000;79(1):18–22. https://linkinghub.elsevier.com/retrieve/pii/S0090825800959055
Chu P, Wu E, Weiss LM. Cytokeratin 7 and cytokeratin 20 expression in epithelial neoplasms: A survey of 435 cases. Mod Pathol. 2000;13(9):962–72.
Benoit L, Arnould L, Cheynel N, Diane B, Causeret S, Machado A, et al. Malignant extraovarian endometriosis: A review. Eur J Surg Oncol. 2006;32(1):6–11.
Slavin RE, Krum R, Van DT. Endometriosis-associated intestinal tumors: A clinical and pathological study of 6 cases with a review of the literature. Hum Pathol. 2000 Apr;31(4):456–63. https://linkinghub.elsevier.com/retrieve/pii/S0046817705800310
Chen KTK. Endometrioid adenocarcinoma arising from colonic endometriosis mimicking primary colonic carcinoma. Int J Gynecol Pathol. 2002;21(3):285–8. http://journals.lww.com/00004347-200207000-00014
Kaimaktchiev V, Terracciano L, Tornillo L, Spichtin H, Stoios D, Bundi M, et al. The homeobox intestinal differentiation factor CDX2 is selectively expressed in gastrointestinal adenocarcinomas. Mod Pathol. 2004;17(11):1392–9. https://linkinghub.elsevier.com/retrieve/pii/S0893395222042491
Yantiss RK, Clement PB, Young RH. Neoplastic and pre-neoplastic changes in gastrointestinal endometriosis. Am J Surg Pathol. 2000;24(4):513–24. http://journals.lww.com/00000478-200004000-00005
Heaps JM, Nieberg RK, Berek JS. Malignant neoplasms arising in endometriosis. Obstet Gynecol. 1990;75(6):1023–8. http://www.ncbi.nlm.nih.gov/pubmed/2188180
Funding
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by G.C., M.D.G.P., and F.S. The first draft of the manuscript was written by M.P., and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Procedures performed in the studies involving human participants were carried out in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to Participate
Not applicable.
Consent for Publication
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Surgery
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pace, M., Carillo, G., Paolo, M.D.G. et al. A Rare Histopathological Diagnosis: Endometrioid Adenocarcinoma Localized in the Rectum: a Case Report. SN Compr. Clin. Med. 5, 254 (2023). https://doi.org/10.1007/s42399-023-01589-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-023-01589-8