Abstract
Child maltreatment (CM) is a widespread problem, contributing to health and societal difficulties often throughout the lifespan. Healthcare professionals (HCPs) who see potential warning signs for CM are responsible for protecting the child from future harm, which may involve alerting the authorities. The decision-making is challenging as unwarranted reporting may lead to mistrust and not benefit the child. We sought to explore what factors might influence HCPs’ decisions to report suspected CM in a Norwegian sample. Using a cross-sectional survey among HCPs in Norwegian hospitals with pediatric wards, we presented five case vignettes describing different probabilities of CM and variables assessing experience, knowledge, and confidence. A total of 382 HCPs completed the survey. Despite recognizing warning signs for CM in the case vignettes, a large proportion were reluctant to report to authorities. Recognition of CM and expressed willingness to report four or all five of the case vignettes (high reporters) was associated with the profession, knowledge, experience, and confidence in handling CM cases. Expressed confidence in performing physical examinations for physical or sexual abuse and talking with parents about abuse was significantly associated with high reporting (OR 2.3 to 17.8). Qualitative data further supported the role of self-efficacy. In summary, reporting to the authorities is an important but complex aspect in cases of suspected CM, but many HCPs relate that they fail to do so. This study indicates reporting suspicion of CM is correlated with self-efficacy and knowledge among HCPs, which should inform educational, social, and policy decisions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Child maltreatment (CM) has been established to be a major global public health problem due to its high incidence and prevalence, and its detrimental and potentially life-long health consequences (Palusci et al., 2019; World Health Organization (WHO), 2022). CM includes physical, sexual, emotional, and psychological abuse and neglect. While types of CM can be difficult to adequately define given the sometimes complex nature and societal and cultural contexts, there is an increase in consensus building around recent robust conceptual models (Mathews & Collin-Vézina, 2019; Mehta et al., 2023). Neglect consists of a child’s basic needs being unmet, whether this be a need for protection, affection, education, or physical or other emotional needs (Dubowitz et al., 2005). Physical abuse is defined by WHO and ISPCAN as “…the use of physical force against a child that results in or has a high likelihood of resulting in harm for the child’s health, survival, development or dignity” and describes the physical acts that may be inflicted (World Health Organization (WHO), 2006). Sexual abuse, though steadily becoming more multifarious with the complexities of the internet and changing norms (Laird et al., 2023), has been defined as “…the involvement of a child in sexual activity that he or she does not fully comprehend, is unable to give informed consent to, or for which the child is not developmentally prepared, or else that violates the laws or social taboos of society” (World Health Organization (WHO), 2006). Psychological abuse, a term still being developed (Hayashi, 2022; Hoffmann & Heim, 2024; Slep et al., 2022), often encompasses both neglect and emotional abuse and involves “degrading, manipulative, or neglectful behavior by caregivers,” and the failure of caregivers to provide a developmentally appropriate and supportive environment. These have a high probability of “…damaging the child’s physical or mental health, or its physical, spiritual, moral or social development”(World Health Organization (WHO), 2006), and many believe them to be the most under-reported, misunderstood, and harmful of all types of abuse (Dye, 2020; Hoffmann & Heim, 2024; Slep et al., 2022). Lastly, polyvictimization, or a child suffering more than one type of abuse, is common and has been shown to have very detrimental outcomes which are difficult to fully assess due to a lack of consensus and clarity on operationalized definitions and approaches (Finkelhor et al., 2007; Lee et al., 2023).
While the obvious risk to physical health and well-being from inflicted injuries such as burns, head and abdominal trauma, and other wounds may leave permanent scarring, disability and death (Christian, 2015), mental health disorders, criminality, physical illness, and poor school and job performance have all been linked to CM (Anda, et al. 2006; Hughes et al., 2017). Immediate and severe life and death types of outcomes are more associated with physical abuse, although all types of CM share many of the same negative consequences over time. A study from 2019 considered seven life domains life that reinforced the considerable persistent personal and societal costs from sexual abuse (Guiney et al., 2022), including “….internalizing, externalizing, and thought disorders, suicide attempts, health risk behaviors, systemic inflammation, poor oral health, sexually transmitted diseases, high-conflict relationships, benefit use, financial difficulties, antisocial behavior, and cumulative problems across multiple domains in adulthood.” Emotional abuse has been associated extensively with depression, and in one study, depression, anxiety, stress, and neuroticism personality were more highly associated with emotional abuse than the other types of CM (Dye, 2020). Neglect, also shown extensively to be associated with depression and both externalizing and internalizing behaviors (Dubowitz et al., 2005; Ogle et al., 2022), may also in the worst cases be fatal (Scott, 2020). All types of CM have long been seen as public health and economic threats (Westman & Westman, 2019).
In a web-based survey, 19% of Norwegian adolescents aged 12–16 years reported being victims of physical abuse, with 4% describing they had experienced serious abuse, “…such as being beaten up, beaten with an object, or beaten with a fist” (Hafstad et al., 2020). Furthermore, 6% reported they had experienced sexual abuse from adults (Hafstad et al., 2020). Another study from the Nordic countries showed an increased risk of sexual abuse during adolescence, with peer perpetrators being the main concern (Kloppen et al., 2016). Although quantifying the impact of CM is complex, and prevalence varies between studies, evidence suggests that many cases remain hidden and unreported. In a meta-analysis of the prevalence of child sexual abuse, rates of child sexual abuse were (Christian, 2015) more than 30 times higher in self-report studies (12.7%) than in official report investigations (0.4%) (Stoltenborgh et al., 2011).
Ensuring that exposed children receive protection and support to reduce the detrimental effects of CM is crucial and depends on professionals’ ability and willingness to detect and report CM. Effective child protection demands a team approach including judicial, welfare, health, and therapeutic intervention (Lalayants, 2008; Sedlak et al., 2006). Each of these agencies provides unique and important contributions to CM cases (Cleek et al., 2019).
Norwegian health personnel law states that reporting to Child Protection Services (CPS) is mandated in cases where there is reason to believe that a child may be experiencing CM. Health care professionals (HCPs) are also required to report to law enforcement (LE) when there is suspicion of inflicted injuries, to protect the child from further harm (see ESM Appendix 1 for a full translation of the laws). While these strong reporting laws are in place, there is no clear data on how they are interpreted and followed. In 2022, only 11% of CM reports to CPS came from HCPs (Statistics Norway, 2022).
On one hand, HCPs who see potential warning signs for CM are responsible for protecting the child from future harm, which may involve alerting the authorities. On the other hand, there is always a possibility that the concern for CM is mistaken. Unwarranted reporting may cause difficulties for the parents, lead to mistrust, and thus not benefit the child. The complexity of the different factors involved, including child, family, and injury characteristics, as well as HCP personal and previous experiences have all been discussed in previous research (Flaherty et al., 2008). International studies have addressed various reporting barriers for professionals and found that there is often a large degree of hesitancy, even when there is a high degree of suspicion of CM. These involve fear of negative consequences for the child and families, fear of negative consequences for oneself (including loss of positive clinical relationship to the family and child), and feelings of uncertainty (Albaek et al., 2019a; Berkowitz, 2008; Flaherty et al., 2006, 2008; Kuruppu et al., 2020; Tiyyagura et al., 2015). Conversely, self-efficacy has been shown to improve decision-making and increase adopting behaviors (Bandura & Watts, 1996; Lee et al., 2012). Bandura describes confidence as assurance in one’s own ability to perform a task or behavior, while self-efficacy is the belief that this behavior will influence outcomes (Finch et al., 2008). In our questionnaire, we used the term “confidence” in order to determine the participants’ belief in their specific abilities, but in the discussion, we applied this confidence to the broader clinical decision-making process using the term “self-efficacy.”
The impact of the cultural context in decision-making seems to be important to understanding the reporting behaviors of HCPs specific to their country (Hartmann & McLaughlin, 2018; Hussain & Oestreicher, 2018; Yates & de Oliveira, 2016). To date, we could not find any studies in Northern Europe that examined barriers to reporting CM in hospital-based HCPs. Therefore, our aim was to explore which factors influence whether or not HCPs report suspicion of CM to CPS or LE in a Norwegian context.
We performed a two-tiered survey of Norwegian HCP knowledge, attitudes, and management of CM cases. The first analysis of the data involved pediatrician participants only. We found little agreement among the participants on the management of CM, and most worryingly a hesitancy to report recognized cases of maltreatment to the authorities (Vollmer-Sandholm et al., 2021). In this second part of the study, we also included other HCPs involved in the examination of children as participants and explored their knowledge, attitudes, and reporting of CM.
Methods
Data Collection
We performed a cross-sectional national survey between May 2019 and January 2020 at 17 of the 22 hospitals in Norway with children’s wards. We arranged on-site seminars at the hospitals. At the beginning of the seminar, the attending HCPs were asked to complete a questionnaire. For a full description of our research project, see our previous article (Vollmer-Sandholm et al., 2021).
A total of 486 HCPs participated in the study, of which 104 were excluded because they did not complete the questionnaire. Participation in the study was anonymous and voluntary. The study was reviewed and approved by the Regional Committee for Medical and Health Research Ethics (reference number 31839).
Questionnaire
The questionnaire had 170 items with a mix of dichotomous, semantic differential, and Likert-type scale response options split into sections: (I) vignettes, (II) barriers/challenges, (III) knowledge and confidence, (IV) work experience with CM cases, and (V) demographics (see ESM Appendix 2.) Under the vignette questions, we included open-ended questions for participants to explain why they suspected CM or why they did not.
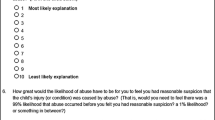
Including all types of CM under a single umbrella can lead to over-simplification and a too-nebulous consideration of the topics at hand. Our vignettes focused primarily on physical abuse, followed by one case of sexual abuse (#2) and two that bore elements of psychological abuse (#4) and neglect (#6) in addition to possible physical abuse. Based on six potential CM vignettes (see Table 1), the questionnaire assessed the following: (a) Whether the participants suspected CM and their assessed need for further evaluation, (b) the reason for such, (c) if they felt confident that they had the competence to handle this case, and (d) whether or not they would report to the authorities. An open-ended question offered the possibility to include other management alternatives that we had not mentioned. Five of these vignettes had previously been used in a European study, three of which were published (Naughton et al. 2018). The sixth, vignette 3, was a control case the study authors developed based on an actual event. An advisory group to the research project consisting of eight experts from LE, CPS, and healthcare determined the five patient vignettes (minus the control vignette) to be suspicious for CM and qualified for a report to either CPS or LE. After the control case established that the HCP participants recognized the non-abuse case and that they would not report this to the authorities, we eliminated it from further analysis.
In addition to demographic information, the questionnaire assessed various aspects of the participants’ knowledge and experience, including confidence, previously researched perceived barriers to engaging in cases of CM, and whether or not they had access to expert advice and guidelines (see ESM Appendix 2.) These questions and answers were developed by the authors and research team from a broad sweep of the literature of previously reported findings in order to assess if there was relevance for our population. We summarized and categorized participant responses, collectively refining categories out of the coding, which were then stratified into quartiles according to normal distribution.
Data Analysis
All data were coded from the printed questionnaire into the statistics program SPSS (version 29.00, IBM Corporation, Armonk, NY) database. A conventional significance level of 5% was used. An initial analysis involved assessing the frequency distributions of the responses. Following this, the participants were split into groups based on their responses as to whether or not they would report to CPS and/or LE in the five case vignettes. Those who stated readiness to report in four or all five vignettes were designated high reporters. Reporting two or less were labeled low reporters. Those reporting three vignettes were labeled medium reporters.
Logistical regression analysis was done with high/low reporters as the outcome variable. We used multivariate logistical regression analysis in which the independent variables that were significant in univariate analysis were included in the model. Moreover, the gender and years of experience of the participants were included. Non-significant variables were removed stepwise, and in the final multivariate analysis, only significant variables were included.
The HCP free text explanations for suspicion were analyzed by the first and second authors using content analysis (Graneheim & Lundman, 2004) and team-based qualitative data analysis (Binder et al., 2012). After familiarizing ourselves with the qualitative data, we compared responses of high and low reporters to see if there was a difference in their reasons for suspicion of abuse and or neglect (see Supplement Table 1.) Next, the responses to each open-ended question were systematically coded and grouped (Braun & Clarke, 2023). This analysis was later, together with the descriptive statistics, discussed with the research team. Thus, our findings were derived from a combination of descriptive statistics, correlation analysis, and qualitative content analysis, as presented below.
Ethical Considerations
The participants were informed prior to the questionnaire administration that it would be used for research purposes. Participation was anonymous and voluntary.
Results
A total of 382 participants were included in the study, consisting of 150 pediatricians, 50 physicians working in other pediatric specialties such as orthopedics, gynecology, and radiology, 147 nurses, and 35 ancillary care providers (i.e., physical therapists). Among the 147 nurses, 74 (50%) reported being trained in pediatric nursing. The participants consisted of 81% females and 68% of the participants were between 30 and 50 years of age (see Table 2).
While 63% of the participants answered that they at some point in their career had suspected physical abuse in a patient, only 38% answered they had ever reported suspicion of physical abuse to CPS. The participants’ experience with reporting other forms of CM is presented in Table 2.
Recognition of CM in Vignettes
The participants’ reported suspicion of CM and their readiness to report after reading the vignettes is illustrated in Fig. 1.
In four of five case vignettes (#1, 2, 4, and 6), 74% or more of the HCPs recognized and were concerned about potential CM (Fig. 1). Despite their suspicion, a large proportion indicated they would not have contacted the authorities, even when they gave clear, detailed, and warranted reasons for their suspicion in the free-text answers, “Worried because this is a high-energy injury. Requires rapid physician evaluation and is suspicious” (see Table 4). In the final vignette (#5) which described a femur fracture in a 2-year-old, only 42% were worried about CM, and 29% stated they would report. In all of the vignettes, the respondents were more willing to report to CPS than LE, often by large percentages (Fig. 1). They were most willing to report vignette #2 to LE, a case of child sexual abuse where the suspect was not a family member.
In summary, 136 (36%) of the participants were designated low reporters as they stated they would only report two or fewer of the five cases to either LE or CPS. There were 116 (30%) medium and 130 (34%) high reporters, the latter stating they would report four or all five of the cases.
Compared to nurses, pediatricians were more likely (OR 2.5, p < 0.001) and other HCPs less likely (OR 0.2, p = 0.01) to be high reporters (Fig. 2).
There was no significant difference between nurses and non-pediatric physicians. When adjusting for other factors in multivariate analysis, no significant difference between pediatricians and nurses was observed (Table 3). Neither age, gender, years of experience, nor affiliation to a university clinic or regional/local hospital had a significant influence on reporting. All variables significantly associated with reporting are shown in Supplement Table 1.
Confidence
HCP level of confidence was shown repeatedly to be a primary factor correlated with willingness to report to the authorities (Fig. 3), and the theme of uncertainty arose frequently in the qualitative answers. When stating their reason for concern for abuse after a vignette, many participants ended their statements with a question mark. For example, “The baby must have cried as the injury occurred?” and “The explanation from the father that he was awakened by the baby crying, but how could the baby have done that to him/herself?” “Is someone abusing this child or do the parents need education and support?” or from the spiral fracture case, “Unusual injury from the reported mechanism?” and; “I have never seen/heard of this.”
Interestingly, two of the significant determinants of being a high reporter according to multivariate analysis support this: Those that were confident in performing a sexual abuse exam were almost 25 times (AOR 24.7, p = 0.01) more likely to be in the high reporters group, and those that reported being confident in managing the vignette cases were almost three times more likely to be in the high reporters group (AOR 2.7, p = 0.008).
Univariate analysis also reflected the relationship between confidence, experience, career, and reporting choices. Those who reported feeling confident performing a CM exam and those that reported being confident talking to parents and children about abuse were more likely to be high reporters (OR 2.8, p < 0.001 and OR 2.3, p = 0.006, respectively). Those who felt confident in their knowledge and ability to report to the authorities were two times more likely (p = 0.005) to be in the high reporter category.
Reported experience with performing CM exams and previous reporting to the authorities was associated with being high reporters (see Supplement Table 1). Sixty-eight percent of those who stated they examined a child for CM > 1 time per month were high reporters (OR 3.0, p = 0.01).
Reasons for Suspicion?
On all five vignettes, we analyzed the HCP free-text explanations as to why they suspected abuse or not; however, we could find no difference in the reasoning between those that said they would report and those that would not. For example, in vignette 5, an HCP who would report to the authorities wrote: “A fall in the sandbox shouldn’t cause a spiral fracture, unless the child has an underlying sickness such as brittle bones” and another HCP who would report wrote: “The fracture is not consistent with the history of injury.” On the other hand, an HCP who chose not to report wrote the following: “Femur fracture is a high-energy trauma and should require more than a stumble in the sandbox” and another non-reporter wrote: “Worried because this is a high-energy injury. Requires rapid physician evaluation and is suspicious” (Table 4).
Barriers
We analyzed and categorized the quantitative Likert scale perceived barrier questions into four categories: (1) lack of knowledge, (2) personal barriers, (3) feeling powerless, and (4) situational barriers. Only knowledge (OR 2.3) and personal barriers (OR 2.7) were measured as statistically significant for being a high or low reporter, with particularly strong results on the statement: “I don’t know how to manage this case” (Supplement Table 1 and ESM Appendix 3). After splitting the individual barriers into groups and spreading them over a normal distribution, we saw that among those participants that were affected by barriers, lack of knowledge and conversely, personal barriers, such as “What if I am wrong?” (OR 2.3) were those that bore significance (Supplement Table 1.)
Overall, 81% (297/365) answered that they would have asked about abuse more often if they were convinced that they could make things better by doing so. Stating awareness of a CM consultant and organizational CM guidelines was associated with being a high reporter (OR 2.0, p = 0.04) (Supplement Table 1). Strangely, in vignette #6 some of the participants who denied being concerned about CM stated that they would regardless report a refugee child to LE (7%) or CPS (20%).
Discussion
Does Recognition of CM Lead to Reporting?
CM is documented to affect a substantial proportion of children in Norway (Hafstad et al., 2020), and many victims of CM never tell or do not disclose until adulthood (Bottoms et al., 2016; Brattfjell & Flåm, 2019). Therefore, it is concerning that little more than half of HCPs had ever suspected physical abuse or neglect during their career, and under half had suspected sexual abuse (see Table 2.)
It is interesting that although they had not suspected CM in their clinical practice, our participants were skilled at recognizing abuse in most (four out of five) of our vignettes. However, our participants’ recognition of CM in the vignettes did not cause most of them to convey intent to report to LE or CPS.
Uncertainties and Fear of Consequences
Funambulism, or a mental tightrope walking, plays a noticeable role in the field of CM when it comes to all aspects of these sensitive cases, including reporting. In an article by Cleek and colleagues (2019), the HCPs conveyed suffering a pervasive uncertainty when they faced potential or factual CM (Cleek et al., 2019). In our vignette about sexual abuse, the caregivers themselves were not implicated, and this allowed the HCP to stay in the supportive role of the family even as they reported the abuse. One might wonder if this helps to explain why they were so much more willing than in the other vignettes. Other research has shown that there is a reluctance on the part of HCPs to address abuse (Albaek et al., 2018), and this is often accompanied by a lack of confidence in their own abilities as well as that of the outside agencies with which they collaborate (Foster et al., 2017). This confidence has also been shown to be a determinant in other clinical areas, such as violence prevention and domestic violence patient counseling (Finch et al., 2008).
The HCPs’ experience of reporting to authorities may be important, as for most HCPs, there is a lack of understanding about how LE and CPS approach these cases, as well as what the process and outcomes may be for the family, child, and HCPs themselves. A lack of trust in LE and CPS has previously been cited as a reason for HCPs not to report (Albaek et al., 2019b; Foster et al., 2017). In our study, however, it was interesting that those who had reported previously were more likely to do so. It may be that they had good experiences of reporting, or they could have the conviction that reporting is the right thing to do. Experiences where reporting was perceived to have detrimental effects on the child or where the HCP did not receive updates from LE or CPS have been shown to negatively affect future reporting (Albaek et al., 2018; Hartmann & McLaughlin, 2018; Hussain & Oestreicher, 2018; Keenan et al. 2017b). Additionally, the process of reporting involves a paradox for HCPs, because it requires both letting go and becoming responsible: they must relinquish some control over their patient’s case, and at the same time, they become accountable to other non-medical professionals. This involves letting people into their professional world and becoming vulnerable to others’ scrutiny of their work and their decisions. The uncertainty exposed by most of our participants could explain their reluctance to the risk of making rash decisions open to second-guessing.
Complexities around legal ramifications such as regarding what constitutes “reasonable suspicion” and confidentiality concerns should also be a consideration in this discussion. In a study from the US and Germany, there were different thresholds for what constituted reasonable suspicion within the respective pediatrician groups (Berthold et al., 2022), and stringent confidentiality laws are often interpreted in a way which hinders both reporting and communication between professionals who wish to share information in order to protect children. Fear of prosecution or ethical compromise creates a difficult dilemma when implementing reporting laws (Lines et al., 2020).
In our findings, the vignette where the parents were not the suspects, but their 7-year-old disclosed molestation by a neighbor boy (vignette 2) registered the most willingness to report among the participants. Previous literature concurs that when parents were not the suspects, HCPs found it easier to report (Stige et al., 2022). The case of the immigrant child the participants wanted to report despite lack of suspicion may illustrate, as previous studies have shown, that it is easier to recognize and report parents who are not like us or to whom it is more difficult to identify (Halvorsen et al., 2013). This tendency of immigrant children to be overrepresented in CPS has previously been revealed in Norway and elsewhere (Fauske et al., 2018; Keenan et al., 2017a, 2017b; Kojan and Storhaug 2021; Palusci & Botash, 2021).
Uncertainty of the Best Interest of the Child
Although Norway has ratified the United Nations’ Convention on the Rights of the Child, our judicial determinations tend to rely on the penal code as the more decisive factor. The participants in our study expressed doubt as to whether reporting could make the situation better for the child, and 81% answered they would have asked about abuse more often if they knew it would make a positive difference. Handling CM is complex, and sometimes it may not be in the child’s best interest to convict one of the parents. Other times, reporting may put on hold support and treatment for the child from CPS or child mental health services pending investigation. Reporting may also damage the child’s relationships and cause the child to lose valuable allies (Devries et al., 2015; McTavish et al., 2017). All of these factors may create reluctance to report among HCPs.
Low Self-Efficacy
Self-efficacy has previously been associated with child abuse reporting (Lawrence & Brannen, 2000), and in our participants, low self-efficacy became evident in four main areas of care: responding to the vignette cases, communicating with patients and caregivers regarding issues of CM, performing the exams, and reporting to the authorities.
The participants’ lack of confidence may be well founded. Norway does not currently have a CM subspecialty nor other formalized education for HCPs working with these cases. Several studies over the last two decades have demonstrated the efficacy of education and training on reporting patterns, tolerance of uncertainty, and sense of confidence (Carson, 2018; Doran and Mortel 2022; Harris et al., 2002; Lawrence & Brannen, 2000; Stephens et al., 2022). However, a recent article indicated that further research in this area is needed (Walsh et al., 2022). Moreover, as both previous research (Boroon et al., 2023; Carson, 2018) and our study have demonstrated, having the knowledge and even skill may influence but not necessarily correlate with action. Not only did our participants have the knowledge and skill to recognize abuse in the vignettes, but both high and low reporters expressed the same reasons for suspicions in their open-ended answers.
We need to investigate further why many HCPs choose not to report suspected CM. How much does their reported emotional discomfort talking about CM, the ambiguity of assessing cases, or possible detrimental consequences from reporting CM impact their decisions? Perhaps education, integrated with Bandura’s four primary sources of self-efficacy, may be a key (Bandura & Watts, 1996; Pfitzner-Eden, 2016). He suggested that education may not be pivotal to self-efficacy. Rather, it is influenced by four primary sources: mastery experiences, vicarious experiences, verbal persuasion, and physiological and affective states (Bandura & Watts, 1996). These sources include the wide range of experiences that build true confidence in a specific area; learning to navigate both success and failure in the tasks involved; sharing the comparison, mentoring, and inspiration of others who are accomplished in the field; positive verbal reinforcement, especially from credible sources; and lastly, experiencing and enduring the physiological and emotional aspects that are inherent in these interactions (Albaek et al., 2019a, 2019b).
Disagreement with Barriers
Why so few participants seemed to agree with the barriers that we presented in our study is puzzling. One explanation could be that they answered in light of the previous vignettes, and it is less complex and stressful to assess vignettes than real-life clinical cases. Or they could have been under the influence of social desirability, where people answer in accordance with a desired self-image rather than realistic scrutiny of themselves (Bell & Bishai, 2021; Dovran et al., 2019; Weijters et al., 2013). Acquiescence may also affect validity, and it is unclear whether the participants’ answers reflect confusion around what they feel and think or their experienced barriers.
The barriers that correlated most with reporting in our study were related to personal barriers, such as “What if I am wrong?” Those participants who reported being unaffected by this were over two times more likely to be a high reporter. This may reflect the impact of self-efficacy which participants conveyed in the other portions of the survey.
Case-by-Case Considerations
In case 1, featuring physical abuse in an infant, a very young child, unable to ambulate or generate enough force to cause their own injuries, presents with an unexplained trauma to the face (oral cavity). While the injury in itself may not be considered life-threatening, most seasoned child abuse pediatricians will recognize that they are common red flags for other abusive injuries, and the lack of history further reinforces a need for a multidisciplinary approach (Christian, 2015, 2019). Infants are extremely vulnerable to severe injury and death, and unexplained injuries necessitate quick and steady reactions. The fact that 26% of HCPs were not suspicious and around 67% would not report should awaken concern and motivation for better education and recognition of physical abuse.
Case 2, featuring sexual abuse, is interesting for several reasons, not the least of which is that it had the most consensus regarding suspicion as well as reporting it was the only vignette presenting sexual abuse, and the abusers were unrelated to the child, therefore negating, at least in part, the barrier of potential consequences of reporting for the family and provider. In addition, it was also the only vignette where a child themselves disclosed what had occurred. While sexual abuse is generally not life-threatening, in some studies, it has been shown to be the most influential in mental health outcomes (Gardner et al., 2019; Stewart et al., 2023) and HCP need to be skilled at recognizing and reporting the subtle signs regardless of who the perpetrator might be.
Case 3 was the control case involving a waffle-iron burn and was reassuring in terms of illustrating that the HCP respondents were alert to cases that could, while potentially indicative of abuse, also be more suggestive of accidental injury. The complexity and seriousness of the injury were less than some of the others, which may also have helped the HCP to recognize it as more likely to be non-abusive. At the same time, the smaller injuries may also be harbingers of other underlying concerns and should be noticed.
Case 4 (primarily focused on physical abuse, but also included neglect and emotional abuse) involved many potential facets, with perhaps the most unique being that of previous repeated family violence, yet many HCPs remained reticent to report. In addition, the parents’ apparent lack of communication and the concerning placement of the injuries should have been further red flags that there was concern for abuse. Injuries to the head and neck are always concerning (Boos et al., 2022; Christian, 2019), particularly in the context of previous family violence. In this case, some may have considered the mom’s explanation plausible, despite the facial and ear bruises.
There is a correlation between partner violence and CM. In addition, a child being witness to violence in the home, whether or not they themselves are targets, is considered by most literature to be either neglect or emotional abuse, or both (psychological maltreatment) (Gardner et al., 2019; Pearson et al., 2023), and one might suppose that a family that has already demonstrated this characteristic should be reported to the authorities when there is any further concern. HCP education should familiarize them with the complexities of partner violence and its effect on children, in some cases both physically and emotionally.
Case 5 features possible physical abuse in a toddler who presents with a spiral femur fracture. The fact that it was a witnessed injury (albeit only reportedly by another young child) in a mobile toddler may help to explain why so few HCPs were concerned and even fewer wanted to report. While it is true that the literature is not as clear regarding the seriousness of this injury in this age group, particularly in regard to a witnessed spiral fracture, the low rates of suspicion and response are concerning as there should still be consideration regarding possible CM and other occult injuries (de Marco et al., 2023; Kemp et al., 2008; Mitchell et al., 2021) and an exploration of other possible red flags.
Finally, case 6 involves the case of an immigrant child with concern for several types of CM, including repeated injuries, delay in seeking care, inappropriate response to and care of injuries, and indications of lack of supervision which might constitute neglect or a child’s needs being unmet. This case has the extra complexity of social and cultural implications in an immigrant family who may themselves have suffered trauma and be significantly lacking in resources. Hesitancy to report in this instance might be an example of depriving a family of support that may benefit the child. HCPs need to be skilled at understanding and sorting through cases of polyvictimization in order to see clearly where the most significant concerns lie and to ensure that the details in the report and subsequent interventions will encompass the child and family’s needs (Finkelhor et al., 2007; Lee et al., 2023). Though our data does not clearly explain the reason, it may be that the few respondents in this vignette who stated they were not concerned about CM but reported anyway were seeing this potential for neglect and responding in kind.
Strengths and Limitations of the Study
We collected data from HCPs from all over the country, thus ensuring a representative participant sample. A multi-disciplinary consulting team of experts endorsed the validity of our previously published vignettes, and we composed the research team with researchers with various expertise within the field of CM. The survey applied a mixed-method approach and included variables from previous research on facilitators and barriers for reporting CM.
While our mixed method approach did add depth to the study, we collected a limited amount of qualitative data. Qualitative focus group interviews or in-depth individual interviews could have given us more insight and understanding of why HCPs choose to report suspected CM or not. Furthermore, reactions towards vignettes, while useful, may deviate from how HCPs would react in “real-life” scenarios.
Clinical Implications
In some ways, our study led to more questions than answers. The medical profession is steeped in the Hippocratic Oath “First do no harm,” and it is reasonable to believe that for HCPs to feel they are morally and ethically obligated to report all cases of suspicion, they need to be convinced it is in the best interest of the child. Moreover, experience with successful protection and care for children who are reported for suspected CM might motivate HCPs to report. Reporting is inherently difficult, and HCPs need to have reassurance that the actions they take will more likely be of benefit than unnecessary cost to their patients and their families.
There also remains obscurity around how the reporting laws and confidentiality laws are to be interpreted and adhered to. The ability to understand and recognize the different types of CM and the dynamics they might represent for the child, their trajectory, and their family over time are also important. A restructured system of evidence-based, child-centered, multi-disciplinary CM training and shared teamwork should be implemented going forward.
Conclusion
Despite several challenges, the literature remains clear that inter-agency collaboration is the most effective means of protecting children from CM (Cleek et al., 2019; Lalayants, 2008; Okato et al., 2020; Sedlak et al., 2006). This study indicates that many children suspected of CM in the Norwegian healthcare system are not being reported to the authorities and therefore do not receive a comprehensive investigation and multi-agency response. This may leave children exposed to CM without the help they require, to great personal and societal costs (Mathews et al., 2008). We hope our study will motivate all agencies to acknowledge areas where they could contribute to a more joint protocol and team to facilitate better recognition of the needs of children (Nouman et al., 2020). An approach where HCPs and the other agencies have the CM education and tools they need and equal yet shared responsibility to work in coordination with reciprocal exchange of information should be considered. One example of this would be reciprocal regional multi-disciplinary team meetings on a regular basis.
We hope that the findings in this study can further our understanding and inspire empowerment in overcoming the barriers and challenges that HCPs face in reporting suspected CM.
Data Availability
The data that support the findings of this study are not openly available but are available from the corresponding author upon reasonable request. Data are located in controlled access data storage at Oslo University Hospital.
References
Albaek, A. U., Binder, P. E., & Milde, A. M. (2019b). Plunging into a dark sea of emotions: Professionals’ emotional experiences addressing child abuse in interviews with children. Qual Health Res, 1049732318825145. https://doi.org/10.1177/1049732318825145
Albaek, A. U., Binder, P. E., & Milde, A. M. (2019a). Entering an emotional minefield: Professionals’ experiences with facilitators to address abuse in child interviews. BMC Health Services Research, 19(1), 302. https://doi.org/10.1186/s12913-019-4128-8
Albaek, A. U., Kinn, L. G., & Milde, A. M. (2018). Walking children through a minefield: How professionals experience exploring adverse childhood experiences. Qualitative Health Research, 28(2), 231–244. https://doi.org/10.1177/1049732317734828
Anda, R. F., Felitti, V. J., Bremner, J. D., et al. (2006). The enduring effects of abuse and related adverse experiences of abuse and related adverse experiences in childhood. Eur Arch Psichiatry Clin Neurosci, 256, 174–186.
Bandura, A., & Watts, R. E. (1996). Self-efficacy in changing societies. Journal of Cognitive Psychotherapy, 10(4), 313–315. https://doi.org/10.1891/0889-8391.10.4.313
Bell, S. O., & Bishai, D. (2021). Can you repeat the question? Paradata as a lens to understand respondent experience answering cognitively demanding, sensitive questions. PLoS ONE, 16(6), e0252512. https://doi.org/10.1371/journal.pone.0252512
Berkowitz, C. D. (2008). Child abuse recognition and reporting: Supports and resources for changing the paradigm. Pediatrics, 122(Suppl 1), S10-12. https://doi.org/10.1542/peds.2008-0715e
Berthold, O., Clemens, V., Levi, B. H., Jarczok, M., Fegert, J. M., & Jud, A. (2022). Survey on reporting of child abuse by pediatricians: Intrapersonal inconsistencies influence reporting behavior more than legislation. Int J Environ Res Public Health, 19(23). https://doi.org/10.3390/ijerph192315568
Binder, P.-E., Holgersen, H., & Moltu, C. (2012). Staying close and reflexive: An explorative and reflexive approach to qualitative research on psychotherapy. Nordic Psychology, 64(2), 103–117. https://doi.org/10.1080/19012276.2012.726815
Boos, S. C., Wang, M., Karst, W. A., & Hymel, K. P. (2022). Traumatic head injury and the diagnosis of abuse: A cluster analysis. Pediatrics, 149(1). https://doi.org/10.1542/peds.2021-051742
Boroon, M., Mokhtari, S., Nojomi, M., Hadi, F., Soraya, S., & Shalbafan, M. (2023). Knowledge, attitude, and practice regarding child maltreatment amongst Iranian medical students through internship course: An 18-month longitudinal study. BMC Primary Care, 24(1), 37. https://doi.org/10.1186/s12875-023-01988-9
Bottoms, B. L., Peter-Hagene, L. C., Epstein, M. A., Wiley, T. R., Reynolds, C. E., & Rudnicki, A. G. (2016). Abuse characteristics and individual differences related to disclosing childhood sexual, physical, and emotional abuse and witnessed domestic violence. Journal of Interpersonal Violence, 31(7), 1308–1339. https://doi.org/10.1177/0886260514564155
Brattfjell, M. L., & Flåm, A. M. (2019). “They were the ones that saw me and listened”. From child sexual abuse to disclosure: Adults’ recalls of the process towards final disclosure. Child Abuse and Neglect, 89, 225–236. https://doi.org/10.1016/j.chiabu.2018.11.022
Braun, V., & Clarke, V. (2023). Toward good practice in thematic analysis: Avoiding common problems and be(com)ing a knowing researcher. International Journal of Transgender Health, 24(1), 1–6. https://doi.org/10.1080/26895269.2022.2129597
Carson, S. M. (2018). Implementation of a comprehensive program to improve child physical abuse screening and detection in the emergency department. Journal of Emergency Nursing, 44(6), 576–581. https://doi.org/10.1016/j.jen.2018.04.003
Christian, C. (2019). Child abuse: Evaluation and diagnosis of abusive head trauma in infants and children. UpToDate. Retrieved March 19, 2020, from https://www.uptodate.com/contents/child-abuse-evaluation-and-diagnosis-of-abusive-head-trauma-in-infants-and-children
Christian, C. W. (2015). The evaluation of suspected child physical abuse. Pediatrics, 135(5), e1337-1354. https://doi.org/10.1542/peds.2015-0356
Cleek, E. A., Johnson, N. L., & Sheets, L. K. (2019). Interdisciplinary collaboration needed in obtaining high-quality medical information in child abuse investigations. Child Abuse and Neglect, 92, 167–178. https://doi.org/10.1016/j.chiabu.2019.02.012
Devries, K. M., Child, J. C., Elbourne, D., Naker, D., & Heise, L. (2015). “I never expected that it would happen, coming to ask me such questions”: Ethical aspects of asking children about violence in resource poor settings. Trials, 16, 516. https://doi.org/10.1186/s13063-015-1004-7
Doran, F., & van de Mortel, T. (2022). The influence of an educational intervention on nursing students’ domestic violence knowledge and attitudes: A pre and post intervention study. BMC Nursing, 21(1), 109–109. https://doi.org/10.1186/s12912-022-00884-4
Dovran, A., Winje, D., Arefjord, K., Tobiassen, S., Stokke, K., Skogen, J. C., & Øverland, S. (2019). Associations between adverse childhood experiences and adversities later in life. Survey data from a high-risk Norwegian sample. Child Abuse Negl, 98, 104234. https://doi.org/10.1016/j.chiabu.2019.104234
Dubowitz, H., Newton, R. R., Litrownik, A. J., Lewis, T., Briggs, E. C., Thompson, R.,…Feerick, M. M. (2005). Examination of a conceptual model of child neglect. Child Maltreat, 10(2), 173-189. https://doi.org/10.1177/1077559505275014
Dye, H. L. (2020). Is emotional abuse as harmful as physical and/or sexual abuse? Journal of Child & Adolescent Trauma, 13(4), 399–407. https://doi.org/10.1007/s40653-019-00292-y
Fauske, H., Kojan, B., & Storhaug, A. (2018). Social class and child welfare: Intertwining issues of redistribution and recognition. Social Sciences. https://doi.org/10.3390/socsci7090143
Finch, S. A., Weiley, V., Ip, E. H., & Barkin, S. (2008). Impact of pediatricians’ perceived self-efficacy and confidence on violence prevention counseling: A national study. Maternal and Child Health Journal, 12(1), 75–82. https://doi.org/10.1007/s10995-007-0223-2
Finkelhor, D., Ormrod, R. K., & Turner, H. A. (2007). Poly-victimization: A neglected component in child victimization. Child Abuse and Neglect, 31(1), 7–26. https://doi.org/10.1016/j.chiabu.2006.06.008
Flaherty, E. G., Sege, R. D., Griffith, J., Price, L. L., Wasserman, R., Slora, E.,…Binns, H. J. (2008). From suspicion of physical child abuse to reporting: Primary care clinician decision-making. Pediatrics, 122(3), 611-619. https://doi.org/10.1542/peds.2007-2311
Flaherty, E. G., Sege, R., Price, L. L., Christoffel, K. K., Norton, D. P., & O’Connor, K. G. (2006). Pediatrician characteristics associated with child abuse identification and reporting: Results from a national survey of pediatricians. Child Maltreatment, 11(4), 361–369. https://doi.org/10.1177/1077559506292287
Foster, R. H., Olson-Dorff, D., Reiland, H. M., & Budzak-Garza, A. (2017). Commitment, confidence, and concerns: Assessing health care professionals’ child maltreatment reporting attitudes. Child Abuse and Neglect, 67, 54–63. https://doi.org/10.1016/j.chiabu.2017.01.024
Gardner, M. J., Thomas, H. J., & Erskine, H. E. (2019). The association between five forms of child maltreatment and depressive and anxiety disorders: A systematic review and meta-analysis. Child Abuse and Neglect, 96, 104082. https://doi.org/10.1016/j.chiabu.2019.104082
Graneheim, U. H., & Lundman, B. (2004). Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Education Today, 24(2), 105–112. https://doi.org/10.1016/j.nedt.2003.10.001
Guiney, H., Caspi, A., Ambler, A., Belsky, J., Kokaua, J., Broadbent, J.,…Poulton, R. (2022). Childhood sexual abuse and pervasive problems across multiple life domains: Findings from a five-decade study. Development and psychopathology, 36, 1-17. https://doi.org/10.1017/S0954579422001146
Hafstad, G. S., Sætren, S. S., Myhre, M. C., Bergerud-Wichstrøm, M., & Augusti, E. M. (2020). Cohort profile: Norwegian youth study on child maltreatment (the UEVO study). British Medical Journal Open, 10(8), e038655. https://doi.org/10.1136/bmjopen-2020-038655
Halvorsen, S., Killén, K., & Grøgaard, J. (2013). Why do we overlook child abuse? Tidsskrift for Den Norske Laegeforening, 133(1), 16–17. https://doi.org/10.4045/tidsskr.12.0801
Harris, J. M., Jr., Kutob, R. M., Surprenant, Z. J., Maiuro, R. D., & Delate, T. A. (2002). Can Internet-based education improve physician confidence in dealing with domestic violence? Family Medicine, 34(4), 287–292.
Hartmann, D. J., & McLaughlin, O. (2018). Heuristic patterns of ethical decision making. Journal of Empirical Research on Human Research Ethics, 13(5), 561–572. https://doi.org/10.1177/1556264618800208
Hayashi, M. (2022). Child psychological/emotional abuse and neglect: A definitional conceptual framework. Journal of Child & Adolescent Trauma, 15(4), 999–1010. https://doi.org/10.1007/s40653-022-00448-3
Hoffmann, F., & Heim, C. (2024). Emotional abuse in childhood and adolescence: Biological embedding and clinical implications. Prax Kinderpsychol Kinderpsychiatr, 73(1), 4–27. https://doi.org/10.13109/prkk.2024.73.1.4 (Emotionaler Missbrauch in Kindheit und Jugend – Biologische Einbettung und klinische Implikationen.)
Hughes, K., Bellis, M. A., Hardcastle, K. A., Sethi, D., Butchart, A., Mikton, C.,…Dunne, M. P. (2017). The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Health, 2(8), e356-e366. https://doi.org/10.1016/s2468-2667(17)30118-4
Hussain, A., & Oestreicher, J. (2018). Clinical decision-making: Heuristics and cognitive biases for the ophthalmologist. Survey of Ophthalmology, 63(1), 119–124. https://doi.org/10.1016/j.survophthal.2017.08.007
Keenan, H. T., Cook, L. J., Olson, L. M., Bardsley, T., & Campbell, K. A. (2017b). Social intuition and social information in physical child abuse evaluation and diagnosis. Pediatrics, 140(5). https://doi.org/10.1542/peds.2017-1188
Keenan, H. T., Campbell, K. A., Page, K., Cook, L. J., Bardsley, T., & Olson, L. M. (2017a). Perceived social risk in medical decision-making for physical child abuse: A mixed-methods study. BMC Pediatrics, 17(1), 214. https://doi.org/10.1186/s12887-017-0969-7
Kemp, A. M., Dunstan, F., Harrison, S., Morris, S., Mann, M., Rolfe, K.,…Maguire, S. (2008). Patterns of skeletal fractures in child abuse: Systematic review. BMJ, 337, a1518. https://doi.org/10.1136/bmj.a1518
Kloppen, K., Haugland, S., Svedin, C. G., Mæhle, M., & Breivik, K. (2016). Prevalence of child sexual abuse in the Nordic countries: A literature review. Journal of Child Sexual Abuse, 25(1), 37–55. https://doi.org/10.1080/10538712.2015.1108944
Kojan, B. H., & Storhaug, A. S. (2021). Barnevern og sosioøkonomisk ulikhet - sammenhenger, forståelser og ansvar (Rapportserie for sosialt arbeid, Issue. S. K. AS. https://www.ntnu.no/documents/1272526675/1281525946/101471_NTNU_Barnevernsrapport_dig.pdf/89919b9f-da71-13e1-cdaa-48e6cd2a01de?t=1636551839182
Kuruppu, J., McKibbin, G., Humphreys, C., & Hegarty, K. (2020). Tipping the scales: Factors influencing the decision to report child maltreatment in primary care. Trauma Violence Abuse, 1524838020915581. https://doi.org/10.1177/1524838020915581
Laird, J. J., Klettke, B., Hall, K., & Hallford, D. (2023). Toward a global definition and understanding of child sexual exploitation: The development of a conceptual model. Trauma, Violence, & Abuse, 24(4), 2243–2264. https://doi.org/10.1177/15248380221090980
Lalayants, M. (2008). Interagency collaboration approach to service delivery in child abuse and neglect: Perceptions of professionals. International Journal of Interdisciplinary Social Sciences, 3, 225–236. https://doi.org/10.18848/1833-1882/CGP/v03i01/52493
Lawrence, L. L., & Brannen, S. J. (2000). The impact of physician training on child maltreatment reporting: A multi-specialty study. Military Medicine, 165(8), 607–611.
Lee, N., Pigott, T. D., Watson, A., Reuben, K., O'Hara, K., Massetti, G.,…Self-Brown, S. (2023). Childhood polyvictimization and associated health outcomes: A systematic scoping review. Trauma Violence Abuse, 24(3), 1579-1592. https://doi.org/10.1177/15248380211073847
Lee, P. Y., Dunne, M. P., Chou, F. H., & Fraser, J. A. (2012). Development of the child abuse and neglect reporting self-efficacy questionnaire for nurses. Kaohsiung Journal of Medical Sciences, 28(1), 44–53. https://doi.org/10.1016/j.kjms.2011.10.032
Lines, L. E., Grant, J. M., & Hutton, A. (2020). Nurses’ perceptions of systems and hierarchies shaping their responses to child abuse and neglect. Nursing Inquiry, 27(2), e12342. https://doi.org/10.1111/nin.12342
de Marco, G., Valaikaite, R., Chargui, M., Coulin, B., Vazquez, O., Tabard-Fougère, A.,…Ceroni, D. (2023). Femoral fractures and abuse in children under 36 months old: A Swiss case series. J Pediatr Orthop B. https://doi.org/10.1097/bpb.0000000000001140
Mathews, B., & Collin-Vézina, D. (2019). Child sexual abuse: Toward a conceptual model and definition. Trauma, Violence & Abuse, 20(2), 131–148. https://doi.org/10.1177/1524838017738726
Mathews, B., Fraser, J., Walsh, K., Dunne, M., Kilby, S., & Chen, L. (2008). Queensland nurses’ attitudes towards and knowledge of the legislative duty to report child abuse and neglect: Results of a state-wide survey. Journal of Law and Medicine, 16(2), 288–304.
McTavish, J. R., Kimber, M., Devries, K., Colombini, M., MacGregor, J. C. D., Wathen, C. N.,…MacMillan, H. L. (2017). Mandated reporters’ experiences with reporting child maltreatment: A meta-synthesis of qualitative studies. BMJ Open, 7(10), e013942. https://doi.org/10.1136/bmjopen-2016-013942
Mehta, D., Kelly, A. B., Laurens, K. R., Haslam, D., Williams, K. E., Walsh, K.,…Mathews, B. (2023). Child maltreatment and long-term physical and mental health outcomes: An exploration of biopsychosocial determinants and implications for prevention. Child Psychiatry Hum Dev, 54(2), 421-435. https://doi.org/10.1007/s10578-021-01258-8
Mitchell, I. C., Norat, B. J., Auerbach, M., Bressler, C. J., Como, J. J., Escobar, M. A., Jr.,…Maguire, S. (2021). Identifying maltreatment in infants and young children presenting with fractures: Does age matter? Acad Emerg Med, 28(1), 5-18. https://doi.org/10.1111/acem.14122
Naughton, A., Nurmatov, U., Van Konijnenburg, E. H., Watkins, J. W., Otterman, G., Nelson, J., & Kemp, A. (2018). Variability in child protection medical evaluations of suspected physical abuse in four European countries: A vignette study. Child Abuse Review, 27, 404–418.
Nouman, H., Alfandari, R., Enosh, G., Dolev, L., & Daskal-Weichhendler, H. (2020). Mandatory reporting between legal requirements and personal interpretations: Community healthcare professionals’ reporting of child maltreatment. Child Abuse and Neglect, 101, 104261. https://doi.org/10.1016/j.chiabu.2019.104261
Ogle, C. M., Miller, T. L., Fisher, J. E., Zhou, J., & Cozza, S. J. (2022). Latent classes of child neglect types and associated characteristics. Child Abuse and Neglect, 134, 105909. https://doi.org/10.1016/j.chiabu.2022.105909
Okato, A., Hashimoto, T., Tanaka, M., Saito, N., Endo, M., Okayama, J.,…Iyo, M. (2020). Inter-agency collaboration factors affecting multidisciplinary workers’ ability to identify child maltreatment. BMC Research Notes, 13(1), 323. https://doi.org/10.1186/s13104-020-05162-7
Palusci, V. J., Council on Child, A., Neglect, Kay, A. J., Batra, E., Section on Child Death, R.,…Graham, M. (2019). Identifying child abuse fatalities during infancy. Pediatrics, 144(3). https://doi.org/10.1542/peds.2019-2076
Palusci, V. J., & Botash, A. S. (2021). Race and bias in child maltreatment diagnosis and reporting. Pediatrics, 148(1). https://doi.org/10.1542/peds.2020-049625
Pearson, I., Page, S., Zimmerman, C., Meinck, F., Gennari, F., Guedes, A., & Stöckl, H. (2023). The co-occurrence of intimate partner violence and violence against children: A systematic review on associated factors in low- and middle-income countries. Trauma, Violence & Abuse, 24(4), 2097–2114. https://doi.org/10.1177/15248380221082943
Pfitzner-Eden, F. (2016). Why do I feel more confident? Bandura’s sources predict preservice teachers’ latent changes in teacher self-efficacy. Frontiers in Psychology, 7, 1486. https://doi.org/10.3389/fpsyg.2016.01486
Scott, D. (2020). Reporting fatal neglect in child death review. Trauma, Violence & Abuse, 21(2), 382–392. https://doi.org/10.1177/1524838018770416
Sedlak, A. J., Schultz, D., Wells, S. J., Lyons, P., Doueck, H. J., & Gragg, F. (2006). Child protection and justice systems processing of serious child abuse and neglect cases. Child Abuse and Neglect, 30(6), 657–677. https://doi.org/10.1016/j.chiabu.2005.11.010
Slep, A. M. S., Glaser, D., & Manly, J. T. (2022). Psychological maltreatment: An operationalized definition and path toward application. Child Abuse and Neglect, 134, 105882. https://doi.org/10.1016/j.chiabu.2022.105882
Statistics Norway. (2022). 10674: Meldingar til barnevernet, etter konklusjon, innhald i meldinga, kven som melde saka og alder 2013 - 2023. Retrieved 01 Jan from https://www.ssb.no/statbank/table/10674/tableViewLayout1/
Stephens, G. C., Sarkar, M., & Lazarus, M. D. (2022). Medical student experiences of uncertainty tolerance moderators: A longitudinal qualitative study. Front Med (lausanne), 9, 864141. https://doi.org/10.3389/fmed.2022.864141
Stewart, S. L., Vasudeva, A. S., Mistry, D., & Poss, J. W. (2023). The impact of child maltreatment on mental health outcome improvements among children and youth accessing community mental health care. Child Abuse and Neglect, 139, 106066. https://doi.org/10.1016/j.chiabu.2023.106066
Stige, S. H., Andersen, A. C., Halvorsen, J. E., Halvorsen, M. S., Binder, P. E., Måkestad, E., & Albæk, A. U. (2022). Possible paths to increase detection of child sexual abuse in child and adolescent psychiatry: A meta-synthesis of survivors’ and health professionals’ experiences of addressing child sexual abuse. Int J Qual Stud Health Well-Being, 17(1), 2103934. https://doi.org/10.1080/17482631.2022.2103934
Stoltenborgh, M., van Ijzendoorn, M. H., Euser, E. M., & Bakermans-Kranenburg, M. J. (2011). A global perspective on child sexual abuse: Meta-analysis of prevalence around the world. Child Maltreatment, 16(2), 79–101. https://doi.org/10.1177/1077559511403920
Tiyyagura, G., Gawel, M., Koziel, J. R., Asnes, A., & Bechtel, K. (2015). Barriers and facilitators to detecting child abuse and neglect in general emergency departments. Annals of Emergency Medicine, 66(5), 447–454. https://doi.org/10.1016/j.annemergmed.2015.06.020
Vollmer-Sandholm, M. J., Myhre, A. K., Otterman, G., Lydersen, S., & Stray-Pedersen, A. (2021). Amongst Norwegian paediatricians there is little agreement in management of cases of suspected child maltreatment. Acta Paediatrica, 110(10), 2865–2872. https://doi.org/10.1111/apa.16017
Walsh, K., Eggins, E., Hine, L., Mathews, B., Kenny, M. C., Howard, S.,…Vagenas, D. (2022). Child protection training for professionals to improve reporting of child abuse and neglect. Cochrane Database of Systematic Reviews(7). https://doi.org/10.1002/14651858.CD011775.pub2
Weijters, B., Baumgartner, H., & Schillewaert, N. (2013). Reversed item bias: An integrative model. Psychological Methods, 18(3), 320–334. https://doi.org/10.1037/a0032121
Westman, J. C., & Westman. (2019). Dealing with child abuse and neglect as public health problems. Springer.
World Health Organization (WHO). (2006). Preventing child maltreatment: A guide to taking action and generating evidence. World Health Organization and International Society for Prevention of Child Abuse and Neglect. https://iris.who.int/handle/10665/43499
World Health Organization. (WHO). (2022). Child maltreatment. World Health Organization. Retrieved August 9, 2023, from https://www.who.int/news-room/fact-sheets/detail/child-maltreatment
Yates, J. F., & de Oliveira, S. (2016). Culture and decision making. Organizational Behavior and Human Decision Processes, 136, 106–118. https://doi.org/10.1016/j.obhdp.2016.05.003
Funding
Open access funding provided by University of Oslo (incl Oslo University Hospital). This work was supported by grants from Stine Sofie Stiftelsen (Foundation).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vollmer-Sandholm, M.J., Myhre, A.K., Albæk, A.U. et al. Child Maltreatment: To Report or Not to Report? It’s More Complex than That. Int. Journal on Child Malt. (2024). https://doi.org/10.1007/s42448-024-00212-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s42448-024-00212-0