Abstract
Purpose
This study aimed to determine whether a series of repeated maximal voluntary apnoeas is effective in improving subsequent time trial performance in competitive level track and field athletes.
Methods
Seventeen competitive runners volunteered for this study and based on their preferred competitive distance they were placed either in the 200 m (5 male, 4 female) or 1000 m group (3 male, 5 female). On two separate occasions (≤ 7 days apart), the participants performed a running time-trial that was preceded either by: (i) a standardised warm up (WO) or (ii) a standardised warm up succeeded by five repeated maximal dry static apnoeas (WA). Splenic volume, haematology and cardiovascular parameters were monitor at rest, before and after each time-trial.
Results
WA resulted in a significantly faster performance (27.51 ± 3.49 s; P = 0.009) compared with WO (27.96 ± 3.34 s) in the 200 m group, whereas no differences were observed in the 1000 m group (WA, 211.10 ± 26.18 s; WO, 215.82 ± 25.13 s, P = 0.120). No differences were noted in splenic volume between WO and WA in either group (P ≥ 0.081). Haemoglobin was significantly elevated after breath-holding in the 200 m (+ 7 g/dL, P = 0.041) but not 1000 m group.
Conclusion
This study demonstrates that five repeated maximal apnoeas are capable of significantly improving a 200 m but not a 1000 m time-trial performance in competitive track and field athletes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In elite athletics, marginal gains are a key priority for athletes and their coaches [10]. Evidence suggest that apnoea (breath-holding) might provide a method for improving performance in various activities either as a supplementary training method [19] or as a priming activity prior to exercise [16]. Acute apnoea causes a number of physiological responses that have an oxygen conserving effect within the body [7]. Collectively these responses are known as the mammalian diving reflex and include bradycardia [1], vasoconstriction of selected vascular beds [15] reduced blood flow to peripheral capillary beds [9], increased sympathetic outflow to the periphery and splenic contraction [12].
The spleen is the largest lymphoid organ in the human body and roughly contains 200–250 mL of blood [22]. During exercise and breath-holding, where the sympathetic tone is elevated, the spleen contracts, consequently releasing is stored erythrocytes into the systemic circulation [14] Notably, haemoglobin increases of up to 8 g/dL have previously been recorded in non-apnoea trained cohorts following a series of 3–5 maximal static apnoeas, with these reported to persist up to 10 min after the last apnoeic bout. Albeit transient, these increases could theoretically improve the oxygen carrying capacity of blood and the carbon dioxide clearance rate, both considered advantageous from a performance perspective. Accordingly, in the past decade several studies have explored the potential utility of breath-holding as a priming strategy prior to endurance events, with these having yielded equivocal results.
Sperlich et al. [21] was the first to investigate the effects of pre-exercise breath-holding on a 4-km cycling time-trial performance. Although splenic contractions were noted after the apnoeic intervention, these were not sufficient to invoke a strong splenic response, possibly due to the weak hypoxemic stress experienced by the participants during their maximal apnoeic attempts (pre apnoea 98% ± 1% vs. post the fourth apnoeic bout 99% ± 0%). Contrastingly, later work by Robertson et al. [19] documented a significant improvement in 400 m swim performance when the time-trial was preceded by a standardised warm-up and a series of three maximal apnoeas (275.79 ± 12.88 s) compared with control (278.66 ± 13.31 s, P = 0.035) but were comparable to the warm-up only protocol (276.01 ± 13.52 s), reiterating the importance of warming up. More recently, Bourdas and Geladas [2] demonstrated that a series of 5 maximal static apnoeic repetitions combined with face immersion in cold water (12 °C) was efficacious in improving performance (49.2 ± 4.8 s) during a time to exhaustion cycling test (i.e., intensity corresponding to 150% of peak power output) compared with control (44.8 ± 8.1 s). However, similarly to Robertson et al. [19], no differences were recorded in haemoglobin nor haematocrit concentrations following the apnoeic repetitions.
To date, no study has investigated the effect of a serial apnoeas on running performance in competitive athletes. Furthermore, to the best of our knowledge no study exists that has evaluated whether the efficacy of breath-holding on endurance performance could be affected by the total duration of the exercise intervention. In this regard, retrospective comparison of the currently available studies suggests that pre-exercise apnoeas may be more beneficial in shorter than longer duration endurance activities [2, 3, 21], with only Robertson et al. [19] demonstrating a significant positive effect of pre-exercise apnoea in comparatively longer trials.
The contradictory nature of previous studies and the lack of studies related to running identify the need for further research into the application of pre-performance apnoeas. As such the aim of this study was to identify whether a series of maximal apnoeas prior to a running time trial is effective in improving performance. Furthermore, this study attempts to determine whether the distance of the time trial impacts upon the results.
Methods
Experimental Design
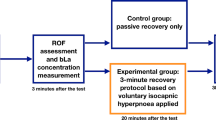
A randomized, repeated measure cross-over design was used for this study. All testing took place on the Leeds Beckett University 400 m running track. Participants attended the track on two separate occasions performing two conditions. During one visit participants performed a warm-up only (WO) (control condition) and on the other occasion a warm-up with apnoeas (WA) with the order of the testing based on a counterbalance of participants at each testing session to minimise the effect of environmental conditions and order effects. Testing was scheduled to take place at a similar time of day for both conditions no more than seven days apart and in similar weather conditions. Participants were requested to follow similar training and dietary patterns on the days before the testing with no food (2 h) and caffeine (that day) prior to testing [8]. The testing took place during the competitive season. A distance of 200–1000 m was selected for the trial by participants based on their preferred competitive distance of 100 m, 200–1500 m respectively. These distances were selected to allow comparison between sprint (200 m) and middle distance (1500 m) runners and to allow participants who specialised in 1500 m to run an “under distance” time trial– giving maximum effort but not causing the degree of fatigue associated with full distance trials that might affect subsequent training or competition as the testing was performed “in season”.
Subjects
Seventeen participants volunteered for this study and were stratified into two groups based on preferred competitive distance, 200 m [9 participants (5 males, 4 females)] and 1000 m [8 participants (3 males, 5 females)]. All participants were competitive athletes of a minimum of county (regional) standard. The study was approved by the Leeds Beckett Carnegie School of Sport Ethics Committee (ethics number: 36549) and all participants completed written informed consent prior to testing. Participants were free from injury and identified as low risk using the ACSM 2017 screening guidelines.
Procedures
On arrival the participants’ stature (Harpenden Stadiometer, Holtain Ltd, Pembrokeshire, UK) and body mass (Seca 709, Seca Ltd, Birmingham, UK) were assessed. Thereafter, the participants underwent a 20 min resting period following baseline measurements of heart rate (HR) (Polar FT1, Polar Electro, OY, Finland) and peripheral oxygen saturation (SpO2) (Nonin 8500 Hand Held Digital Oximeter, Plymouth, USA) along with fingertip blood samples for the analysis of blood lactate (BL) (YSI2300 stat plus, Yellow Springs Instruments, USA), haemoglobin (Hb) (HemoCue, Radiometer Group, Sweden) and haematocrit (Hct) (Hawksley Microcentrifuge Nottingham, United Kingdom). Finally, splenic volume was determined by measuring the spleen’s length (L), width (W) and thickness (T) (MindRay DP-50, Shenzhen MindRay Bio-Medical Electronics Co., Ltd., Shenzhen, China) and calculated using the Pilström formula [Lπ(WT-T2)/3] [6].
Following resting measurements, the participants then performed either the WO or WA protocol. During both protocols the participants performed their own pre-race warm up and were instructed to use the same routine for both testing conditions. Following completion of their warm-up, cardiovascular parameters, haematology and spleen volume were evaluated. Thereafter, over a 20-min period the participants: (i) remained seated for the entirety of this period whilst breathing normally to simulate a pre-competition holding period (WO protocol) or (ii) completed a series of five, dry, static apnoeas in a seated position, each separated by a two minutes resting period [5, 19], whilst wearing a nose clip to avoid micro breathing protocol (WA protocol). This apnoeic modality was used to provide a more practicable technique that could potentially be adapted by athletes in a competition setting, such as during a “call room” scenario [19].At the end of WO and immediately after each successive maximal apnoeic attempt splenic volume was assessed, a fingertip blood sample (haemoglobin, haematocrit and blood lactate) was collected; heart rate and SpO2 were noted.
Following the 20-min period (WO & WA), the participants transitioned immediately from the testing area to the start line, with the time-trial commencing within five minutes from completing the WO or WA protocol. The time was recorded by two timekeepers with the average time of the two measurements being used for analysis. Following completion of their respective time-trial cardiovascular parameters, haematology and splenic volumes measurements were performed.
Statistical Analysis
Statistical analysis was performed using SPSS Statistics (version 26: SPSS Inc, Chicago, IL), with significance set at P < 0.05. The Shapiro-Wilk test was used to assess normality, whereas homogeneity was assessed using Levene’s test. Sphericity was evaluated using Mauchly’s test of sphericity; for instances where the assumption of sphericity was violated, the Greenhouse-Geisser correction was applied. Repeated measures ANOVAs with Tukey’s post-hoc tests were used to assess within-group differences for baseline measurements and other timepoints for breath-hold duration, HR, SpO2, haemoglobin, haematocrit, blood lactate and splenic volume. Two-way ANOVAs were used to assess temporal differences in collection time points between conditions. Pair-sample t-tests were used to compare the time-trial performances between conditions (i.e., WO vs. WA) two conditions were being compared. All graphs were produced using GraphPad Prism (GraphPad Software, Prism 9.0, San Diego, CA 92,108). Unless otherwise stated, data are reported as mean ± SD, with significance accepted at P < 0.05. Raw data for this study are not publicly available to preserve individuals’ privacy under the European General Data Protection Regulation and in accordance with the data management plan that was outlined in the participant information sheet at the point of consent.
Results
Performance
During the 200 m time-trial, WA resulted in a significantly faster performance (27.51 ± 3.49 s; P = 0.009) compared with WO (27.96 ± 3.34 s), whereas no differences were observed in the 1000 m running trials (WA, 211.10 ± 26.18 s; WO, 215.82 ± 25.13 s, P = 0.120) (Figs. 1 and 2). Across both conditions the average 200 m TT was 25.32 ± 1.33 s for males and 30.75 ± 1.53 s for females, 1000 m TT was 197.03 ± 18.24 s for males and 222.34 ± 21.09 s for females (Fig. 1).
Apnoea Duration
There was a significant increase in apnoea duration throughout the apnoea protocol with each apnoea being significantly (P < 0.05) longer than the proceeding apnoea in both groups (Table 1).
Heart Rate
Significant differences in heart rate were recorded during both groups (200 m; 1000 m) and protocols (WO, P ≤ 0.0001 and WA, P ≤ 0.0001) (Table 2), whereas no differences were documented between the two interventions in either group (P ≥ 0.069).
In the 200 m group, heart rate was significantly higher than baseline compared with the warm-up (WO, P < 0.001; WA, P < 0.002) and post-trial (WO, P < 0.001; WA, P < 0.001) (Table 1). In the 1000 m group, heart rate was significantly elevated from baseline compared with warm up (P = 0.016) and post-trial (P < 0.001) in the WA protocol and compared with pre- and post-trial (P = 0.023; P < 0.001, respectively) in the WO protocol.
During apnoeic protocol, a significant increase in heart rate was an overall affect observed in the 1000 m group (P = 0.013) but not the 200 m (P = 0.138), with post hoc analyses identifying no significant differences. No differences were recorded in the post-apnoeic heart rate levels between the two groups (P = 0.737) (Table 2).
Peripheral Oxygen Saturation
SpO2 was lower than baseline in the 1000 m (WO, P = 0.306; WA, P = 0.013) but not the 200 m group (WO, P = 0.06; WA, P = 0.277). Specifically, during the WA protocol, pre-trial SpO2 was significantly lower than baseline (P = 0.016) (Table 2). Moreover, in the 1000 m but not the 200 m (P = 0.183) group there was a significant difference between the two protocols (P = 0.002), with a lower SpO2 being documented pre-trial in WA (P = 0.043) than the WO protocol (Table 2). There was no significant difference between groups (P = 0.950).
During the apnoeic protocol, a significant reduction in SpO2 was only documented in the 200 m group (P = 0.015) while no differences were observed in the 1000 m group (P = 0.078) (Table 2). Notably, SpO2 was significantly lower than baseline during the fourth apnoeic repetition (P = 0.021) (Table 2). Moreover, there were no between-group differences (P = 0.433).
Splenic Volume
Splenic contractions were evident in both groups [200 m(WO, P < 0.001; WA, P < 0.001); 1000 m (WO, P = 0.012; WA, P = 0.035)]. Notably, a significant reduction was observed from baseline (200 m, WO, 250 ± 83 mL, WA, 219 ± 78 mL; 1000 m, WO, 228 ± 77 mL, WA, 234 ± 93 mL) to post time-trials across both distances [200 m (WO, 224 ± 58 mL, P < 0.001; WA, 196 ± 65 mL, P < 0.001); 1000 m (WO, 204 ± 79 mL, P = 0.048; WA, 149 ± 41 mL, P = 0.014)] and protocols, with the only exception of a significant decrease (149 ± 41 mL; P = 0.045) also being denoted after the apnoeic intervention (Pre-Trial) in the 1000 m group. Furthermore, there were no between-protocols (200 m, P = 0.165; 1000 m, P = 0.081) nor group (P = 0.307) differences.
Haemoglobin
Haemoglobin was significantly elevated from baseline (200 m, WO, 146 ± 15 g/dL, WA, 144 ± 20 g/dL; 1000 m, WO, 138 ± 15 g/dL, WA, 143 ± 8 g/dL) during both protocols in the 1000 m (WO, P = 0.018; WA, P = 0.035) but only in the WA protocol (P = 0.003) in the 200 m group. In the 1000 m group, haemoglobin was significantly higher than baseline compared with pre-trial (145 ± 12 g/dL, P = 0.039) and post-trial concentrations (149 ± 17 g/dL, P = 0.028) during the WO protocol, while in the WA protocol haemoglobin was only higher than baseline compared with the post-trial concentrations (154 ± 11 g/dL, P = 0.011). Moreover, in the 200 m WA protocol, haemoglobin concentrations were significantly higher than baseline after the apnoeic intervention (151 ± 11 g/dL, P = 0.041) and post-trial (159 ± 14 g/dL, P < 0.001). No differences were denoted between-protocols (200 m, P = 0.105; 1000 m, P = 0.236) nor groups (P = 0.633).
Haematocrit
Haematocrit was only significantly higher than baseline (43% ± 3%, P < 0.001) during the WO protocol in the 200 m group. Notably, haematocrit post-trial concentrations (47% ± 4%, P = 0.001) were significantly higher than baseline. However, there were no between-group (P = 0.667) nor protocol (200 m, P = 0.145; 1000 m, P = 0.845) differences in haematocrit concentrations.
Lactate
Blood lactate was significantly elevated from baseline during both groups and protocols (P < 0.001). In the 200 m group, blood lactate concentrations were significantly higher than baseline following the run-trials in both protocols (WO, P = 0.001; WA, P < 0.001) as well as compared with post-warm up in the WA (P = 0.006) (Table 1). Moreover, during the 1000 m group, blood lactate concentrations were significantly higher than baseline following the run-trials in both protocols (WO, P = 0.002; WA, P = 0.004) (Table 1). There were no between-protocol (200 m, P = 0.933; 1000 m, P = 0.683) nor group (P = 0.713) differences.
Discussion
This study aimed to examine whether a series of maximal apnoeas prior to a running time trial is effective in improving performance. The key finding of this research is that five repeated maximal apnoeas significantly improved running performance in 200 m but not in 1000 m in a sample of competitive runners.
The improvement in the 200 m time-trial adds to the growing body of evidence that pre-exercise apnoeas can impact performance, as highlighted by Robertson et al. [19] and Bourdas & Geladas [2], yet the 1000 m findings supports the perspectives of Sperlich et al. [21] and Bouten et al. [4], who found no performance advantage from pre-exercise apnoea. It is interesting to note that the exercise duration of our 200 m trial (27.51 ± 3.49 s) and that of Bourdas and Geladas [2] (44.8 ± 8.1 s), were substantially shorter than our 1000 m trial (211.10 ± 26.18 s) and those of Robertson et al. [19] (275.79 ± 12.88 s), Sperlich et al. [21] (342 ± 34 s) and Bouten et al. [20] (264.8 ± 14.1 s); with only Robertson et al. [19] demonstrating a significant positive effect of pre-exercise apnoea in comparatively longer trials. This potentially suggests that pre-exercise apnoeas may be more beneficial in shorter than longer duration endurance activities. However, further research is necessary to ascertain or refute this supposition.
Over the series of the repeated breath-holds, participants achieved progressively longer apnoeic durations, a response that is well documented across the literature [6, 11, 20]. Importantly, the gradual increases in breath-hold durations over the repeated attempts were of similar magnitude between the two groups (Table 1). This suggests that the performance gains noted in the 200 m time-trial were not attributable to differences in sustained breath-hold durations nor the hypoxaemic-dose encountered by the participants during their respective maximal attempts. In addition, although in both groups the warm-up routines elevated haemoglobin levels, these increases were only maintained following the succeeding apnoeic intervention in the 200 m group. Importantly, these increases did not concur with changes in splenic volume (Fig. 3); suggesting that factors beyond the splenic response might have also played a role in these haematological undulations. Taking into consideration that haemoglobin concentrations are prone to plasma volume changes [17, 18], it is reasonable to assume that these may have emanated from a combination of haemoconcentration and splenic contraction. While it is unclear what proportion of the documented increases reflect a genuine enhancement in haemoglobin content, it is tempting to speculate that these may, at least partially, have contributed to the observed improvements in performance in the 200 m group.
Serial breath-holding has been shown to transiently elevate arterial carbon dioxide levels and disrupt redox balance. These fluctuations are known to prompt vasodilation, enhance oxygen delivery to working muscles and accelerate oxygen consumption [13]; all considered advantageous from a performance perspective. Supporting this notion is that when a series of five maximal breath-holds preceded a time-to-exhaustion test as opposed to normal breathing, a greater contribution from aerobic metabolism was noted, consequently improving performance [2]. Thus, present findings might have also stem from blood gas and/or redox fluctuations, exerting a greater influence on the performance of shorter rather than longer duration endurance activities. A measure of blood gases and/or parameters related to redox balance would have certainly provided additional insights to the mechanistic basis of our findings.
In conclusion, this study demonstrates that five repeated maximal apnoeas are capable of significantly improving a 200 m but not a 1000 m time-trial performance in competitive runners. The results suggest that the 1000 m time-trial was of sufficient duration and intensity to invoke a significant splenic contraction and the associated haematological responses, but the inclusion of pre-exercise apnoea conveyed no physiological advantage. This study suggests that pre-exercise apnoea might be beneficial as a priming activity for short duration activities and could be employed by athletes seeking marginal gains, specifically where athletes may be confined within a ‘holding area’ before the performance or incorporated into warm-up activities.
References
Asmussen E, Kristiansson NG. The diving bradycardia in exercising man. Acta Physiol Scand. 1968;73(4):527–35.
Bourdas DI, Geladas ND. Five repeated maximal efforts of apneas increase the time to exhaustion in subsequent high-intensity exercise. Respir Physiol Neurobiol. 2021;292:103703.
Bouten J, Bourgois JG, Lootens L, Boone J. Acute apnea and white blood cell count: a biphasic response formal comment on ‘Hematologic changes after short term hypoxia in non-elite apnea divers under voluntary dry apnea conditions’. PLoS ONE. 2021;16(7):e0253584.
Bouten J, Colosio AL, Bourgois G, Leen L, Van Eenoo P, Bourjois j, Boone J. Acute apnea does not improve 3-km cycling time trial performance. Med Sci Sports Exerc. 2020;52(5):1116–25.
Elia A, Barlow MJ, Deighton K, Wilson OJ, O’Hara JP. Erythropoietic responses to a series of repeated maximal dynamic and static apnoeas in elite and non-breath-hold divers. Eur J Appl Physiol. 2019;119(11):2557–65.
Elia A, Barlow MJ, Wilson OJ, O’Hara JP. Splenic responses to a series of repeated maximal static and dynamic apnoeas with whole-body immersion in water. Exp Physiol. 2021;106(1):338–49.
Elia A, Gennser M, Harlow P, Lees MJ. Physiology, pathophysiology and (mal) adaptations to chronic apnoeic training: a state-of-the-art review. Eur J Appl Physiol. 2021;121:1543–66.
Elia A, Johannesson B, Gottschalk F, Gennser M. The effect of dietary intake on apneic performance, cardiovascular and splenic responses during repeated breath holds. Am J Physiology-Regulatory Integr Comp Physiol. 2022;323(6):R839–48.
Elsner R, Gooden B. Diving and asphyxia. A comparative study of animals and man. Monogr Physiol Soc. 1983;40:1–168.
Hall D, James D, Marsden N. Marginal gains: olympic lessons in high performance for organisations. HR Bulletin: Res Pract. 2012;7(2):9–13.
Heath J, Irwin C. An increase in breath-hold time appearing after breath-holding. Respir Physiol. 1968;4(1):73–7.
Hurford WE, Hong SK, Park YS, Ahn DW, Shiraki K, Mohri M, Zapol WM. Splenic contraction during breath-hold diving in the Korean ama. J Appl Physiol (1985). 1990;69(3):932–6.
Jones AM, Koppo K, Burnley M. Effects of prior exercise on metabolic and gas exchange responses to exercise. Sports Med. 2003;33(13):949–71.
Laub M, Hvid-Jacobsen K, Hovind P, Kanstrup IL, Christensen NJ, Nielsen SL. Spleen emptying and venous hematocrit in humans during exercise. J Appl Physiol (1985). 1993;74(3):1024–6.
Leuenberger UA, Hardy JC, Herr MD, Gray KS, Sinoway LI. Hypoxia augments apnea-induced peripheral vasoconstriction in humans. J Appl Physiol (1985). 2001;90(4):1516–22.
Bourdas DI, Tsakiris TS, Pavlakis KI, Triantafillou DV, Geladas ND. Repeated apneas and hypercapnic ventilatory response before and after apnea training. Aerosp Med Hum Perform. 2015;86(1):27–33.
Otto JM, Montgomery HE, Richards T. Haemoglobin concentration and mass as determinants of exercise performance and of surgical outcome. Extrem Physiol Med. 2013;2:1–8.
Otto JM, Plumb JO, Clissold E, Kumar SB, Wakeham DJ, Schmidt W, Grocott MPW, Richards T, Montgomery HE.Hemoglobin concentration, total hemoglobin mass and plasma volume in patients: implications for anemia. Haematologica. 2017;102(9):1477.
Robertson C, Lodin-Sundström A, O’Hara J, King R, Wainwright B, Barlow M. Effects of pre-race apneas on 400-m freestyle swimming performance. J Strength Cond Res. 2020;34(3):828–37.
Schagatay E, van Kampen M, Emanuelsson S, Holm B. Effects of physical and apnea training on apneic time and the diving response in humans. Eur J Appl Physiol. 2000;82(3):161–9.
Sperlich B, Zinner C, Pfister R, Holmberg HC, Michels G. Repeated apnea-induced contraction of the spleen in cyclists does not enhance performance in a subsequent time-trial. Eur J Appl Physiol. 2015;115(1):205–12.
Stewart IB, McKenzie DC. The human spleen during physiological stress. Sports Med. 2002;32(6):361–9.
Funding
The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception, design and material preparation. Data collection was performed by MB, CR, RC, MR, HC, and AE. Analyses were performed by MB and AE. The first draft of the manuscript was written by MB and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
This study was performed in line with the principles of the Declaration of Helsinki. The study was approved by the Leeds Beckett Carnegie School of Sport Ethics Committee (ethics number: 36549).
Consent to Participate
All participants completed written informed consent prior to testing.
Consent to Publish
All participants completed written informed consent prior to testing including consent to publish.
Competing Interests
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Barlow, M.J., Ross, C., Cockrell, R. et al. Effects of Five Serial Apnoeas Prior to a Running Time Trial in Competitive Athletes. J. of SCI. IN SPORT AND EXERCISE (2024). https://doi.org/10.1007/s42978-024-00296-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s42978-024-00296-7