Abstract
Background
Policymakers aim to reduce C-section (CS) rates, due to well documented overtreatment. However, little is known about how hospital characteristics relate to their c-section rates on low-risk deliveries (CSR-LRD).
Methods
CSR-LRD were computed using inpatient data from all Portuguese National Health Service hospitals (2002-2011). Linear and Fractional Response Models were estimated to quantify the relationship between CSR-LRD and a set of hospital characteristics: hospital size, type (exclusively obstetrics or not), Neonatal Intensive Care Unit (NICU) availability, obstetrician-to-obstetric bed ratio, and teaching status.
Results
CSR-LRD increased from 11.7% (2002) to 14.1% (2008), declining to 12.5% in 2011. While larger hospitals and hospitals with NICU had higher CSR-LRD rates, teaching status and obstetrician-to-obstetric bed ratio had no significant effect. Adjusted estimates, controlling for those four characteristics, indicate 91% of the variation in the CSR-LRD is left unexplained.
Conclusion
Hospital characteristics do not explain variation in CSR-LRD rates. Further studies considering medical practice, financial incentives to hospitals and/or physicians, and patient education are needed.
Highlights
• Focusing on c-section rates on low-risk deliveries minimises hospitals’ risk selection biases, e.g cream skimming.
• Hospital characteristics moderately affect c-section rates in low-risk deliveries.
• Policy changes should aim to promote established best practices rather than reducing available resources.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Caesarean section (CS) is the most frequently performed surgical procedure in the world [1, 2]. In 1985, the World Health Organization (WHO) issued general recommendations on CS, stating that the minimum acceptable rate was 1% and that there was no justification for any region to have rates higher than 10–15%. In 2015, the WHO once again stated that a CS rate (CSR) above 10% was not associated with reductions in maternal and new-born mortality rates [3] corroborated by Betran et al.’ systematic review of ecologic studies [4]. Plus, exposing mothers to unnecessary risks without additional benefits should only be undertaken when deemed medically necessary [2, 5].
Most high income countries exceeded the CSR threshold in 2002, up to an average of 21% of all births [6]. A study conducted in 24 countries and 373 health facilities in Africa, the Americas, and Asia observed that 25.7% of births were by CS, although rates varied significantly across countries suggesting that a number of CS were done without medical need [7].
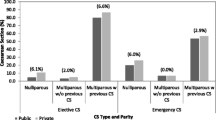
In Portugal, policy makers have tried to curtail increasing CSR. Between 2004 and 2013, NHS hospitals’ rates increased from 27.9% to 30.8%, decreasing to 28.1% in the first nine months of 2014 [8], potentially due to maternal risk factors (RF). However, if that were the case, WHO’s CSR threshold would be too low [9]. Other non-clinical justifications for the increasing trends in CSR include obstetricians’ behaviour and medical practice [10,11,12,13,14,15], provider’s financial incentives, as well as the preferences or other time related incentives for mothers requesting elective CS [5, 16,17,18,19].
Regarding obstetrician incentives to perform CS over vaginal delivery, the most obvious incentive seems to be a financial one. Evidence showed that with the right financial incentives – similar payments for CS and vaginal delivery, for example – CSR might decrease [8, 20].
Opportunity costs of prolonged deliveries, minimization of malpractice risks or defensive medicine, and the demand for leisure or regular workweeks were also identified as reasons for the increasing numbers of CS [14, 21].
Differences in hospital CSR, after adjusting for maternal RF, have been attributed to pregnancy characteristics. Nevertheless, the increasing incidence of clinical indications for CS over time did not explain the rising rates [22]. Broad variation was found in preterm CS births [23] but differences in CSR could have resulted from almost random decision making [15, 20, 24]. Variation can also be due to uncertainty in diagnosis, although recent introduction of diagnostic technology may reduce hospital variation [25].
Importantly, availability of resources might increase CSR. Previous research has showed CSR increasing for admissions taking place from Monday to Thursday and decreasing for admissions on Friday and Saturday, when fewer staff was available [5]. In contrast, CS deliveries also increase resources due to longer lengths of stay, by two to three days, higher hospital costs and higher physician fees in comparison to vaginal deliveries [21, 26, 27].
At an aggregate level, supply factors played a critical role: the greater the hospital capacity of the health system, the greater the number of CS performed [28]. Moreover, obstetricians had a substantial influence on the delivery mode [28]. At the same time, hospital characteristics also seem to affect the CSR. It decreased when more specialized resources were available, including facilities with a neonatal intensive care unit (ICU) and maternal foetal medicine subspecialists [29]. The rates also decreased with the availability of obstetricians–gynaecologists specialists as opposed to family physicians only, higher delivery volume, urban location, and 24-hour in-house anaesthesiology. No differences were found between types of hospital ownership or by teaching status [5, 30, 31].
There is no evidence on the relationship between hospital characteristics and maternal risk profile, namely low-risk deliveries. This work aims to understand how hospital characteristics relate to c-section rates on low-risk deliveries, at the hospital level. By focusing our research on low-risk deliveries, biases related to hospitals’ case-mix and potential cream skimming are minimised and it singles out the effects of hospital resources on c-section rates.
Our study period is between 2002 and 2011. Due to changes in coding practices, data from more recent years would not be comparable with the data used in this work and the current percentage of c-sections observed in NHS hospitals is similar to one observed in 2010. Looking at data up to 2020, most recent data available, we can observe the following (Table 1):
The number of deliveries has been decreasing and CS were around 33% between 2015 and 2017, its lowest number. However, since 2018, an upward trend is being observed and we are now at the same values we had in 2010. This information strikingly shows that the situation has not changed much.
Methods
Our database combined anonymized data on discharges in Portuguese NHS hospitals between 2002 and 2011 collected by the Central Administration of the Health System (Administração Central do Sistema de Saúde) and a dataset on the resources available at each NHS hospital for the same period collected by the Directorate General of Health (Direcção Geral de Saúde). Women aged between 15 and 55 years old grouped in Diagnosis Related Groups 370-373 (AP-DRG 21) were selected. To single out potential effects of risk factors from the analysis only low-risk deliveries were considered. The subset of low-risk deliveries was created by excluding all deliveries with registered conditions deemed as risk factors (RF) for CS (Table 2). The selection of conditions followed the definition of low-risk deliveries provided by García-Armesto et al. [32] When hospitals’ budgets are set based on DRGs, they are influenced by coding practices, therefore all hospitals in our dataset were faced with the same incentives to maximize their revenue. Furthermore, internal and external audits were carried out on a regular basis to assess the quality and accuracy of the coding standards [33].
A C-section rate in low-risk deliveries (CSR-LR) was calculated for each hospital in each year.
Hospital characteristics considered in this analysis included: hospital size (number of beds per hospital), hospital specialization in obstetrics (availability of neonatal ICU, binary variable: yes/no), availability of obstetric resources (ratio of obstetricians to obstetric beds) and teaching status (binary variable: yes/no). Summary statistics can be found in Table 3.
The reduction in the number of hospitals between 2002 and 2011 was due to hospital mergers taking place over the period. That organizational fact influenced not only the number of institutions analysed in each year but also the resources of each hospital which were combined as a new institution was created. As a consequence, the average number of beds available at hospitals increased over the years as well as the percentage of hospitals with a neonatal ICU and the number of teaching hospitals. No more than three hospitals nationwide had no teaching activities, nevertheless, it was decided that the variable should be controlled for to understand whether the differences appeared to be systematic.
Fractional Response Models (FRM) are used when the response variable is a proportion and is bounded between 0 and 1. These models accommodate this boundness and avoid estimation of nonsensical predictions (out of bounds of the standard unit interval) by assuming that the effects of explanatory variables are not linear (not constant through all of its range as the variance tends to decrease when the mean gets closer to the boundaries) [34, 35]. Both cross-sectional and panel data models were estimated in the present study. FRMs (cross-sectional and panel data) required the correct specification of the conditional expectation of the fractional response variable, i.e., a functional form for the distribution of the CSR-LRD must be assumed. This functional form imposed constraints on the conditional mean of this variable. Frequent choices for the functional form include logistic, probit, loglog, cloglog and cauchit functions. Details about these functions may be found in Ramalho et al. [35]. A cloglog distribution was selected for the functional form (both for cross-sectional and panel data) as CSR-LRD tended to be closer to 0. In the panel data model, the pooled fixed-effects estimator described in Ramalho et al. [36] was used. This estimator was chosen because it captured individual hospital characteristics that may not have been reflected in the explanatory variables related to hospital characteristics, but that could have been correlated with this set of variables. In both cross-sectional and panel data models, year-dummies were included among the explanatory variables.
Ordinary Least Squares (OLS) and Fixed-Effects linear panel data model (PLM-FE) were also estimated for comparison. R2 were studied when available. For the cross-sectional estimation of the FRM, RESET-type tests and the generalised goodness-of-functional form (GGOFF) tests were performed. Both tested if the functional form assumed corresponded to the conditional mean and could be interpreted as a test for the omission of other explanatory variables in the model. If the functional form was correctly specified, the null hypothesis should be accepted. The choice of the cloglog for the functional form turned out to be supported by specification tests GGOFF and RESET. There were no tests available for panel data estimation in FRM.
SPSS and R were used for the summary statistics and econometric model estimation.
Results
Table 4 presents general information of the evolution of deliveries, low-risk deliveries, CSR-LRD and CSR-LRD at hospital level. Deliveries were continuously decreasing until 2010 when a slight increase occurred. CSR steadily increased from 26% in 2002 to 31.6% in 2009, when the rate started to slightly decline to 29% in 2011. These values were still much higher than the widely quoted 15% threshold recommended by the WHO.
Low-risk deliveries accounted for 55.4% of total deliveries and followed the same tendency decreasing in total until 2010 and slightly increasing in 2011. CSR-LRD were much lower than CSR as was anticipated. The trend nevertheless was similar; CSR-LRD increased between 2002 and 2008 from 11.7% to 14.1% and then decreased to 12.5% in 2011.
At hospital level, CSR-LRD varied from 1% to 45.8%. The coefficient of variation ranged from 45.2% to 65.3% over the years of analysis presenting a large dispersion of CSR-LR across hospitals.
Linear vs Fractional response models
Model estimations are presented in Table 5. The sign and statistical significance of cross sectional estimates were consistent across linear and FRM. For panel data, this statement was true for hospital characteristics except “teaching” but not true for year-dummies which assumed some significance in the linear model but not on the FRM model.
For cross-sectional FRM estimates, GGOFF and RESET tests were not rejected indicating that the cloglog functional form was adequately selected to estimate the models. These tests were not available for panel data FRM. Nevertheless, standard errors of the parameters from linear models were smaller than those from FRMs. Using linear models to predict fractional response variables may be more efficient when the analysis is not concentrated on extreme values of 0 and 1 as happened in this situation.
Cross-Sectional vs Panel data analysis
Although R2 was higher for cross-sectional models, in both linear and FRM when panel data models were estimated hospital characteristics lost significance and even reversed sign. In the panel data of linear model, some year-dummies were significant. This suggested that hospital previous results, past practice and year may have been more relevant than the hospital characteristics considered in the analysis.
Hospital characteristics
Availability of Neonatal ICU was the only variable with consistent positive effect on CSR-LRD across the four models, although the estimates were significant only in cross-sectional models. In the cross-sectional models availability of Neonatal ICU was significant and the rate of CSR-LRD significantly increased with number of beds per hospital.
Teaching hospitals were associated with lower levels of CSR-LRD in cross-sectional models and these results were statistically significant. However, when extending the analysis to a panel data model this relation became positive.
The effect of ratio of obstetricians to obstetric beds was not significant in any model, being positive for cross-sectional and negative for panel data models.
For all the models estimated, the R2 was small and thus, the selected hospital characteristics and year only explain a small part of the variations observed in the CSR-LRD of hospitals.
Discussion
In this study, we aim to understand the relationship between hospital characteristics and c-section rates, focusing on low-risk deliveries, at the hospital level. This approach is especially relevant when working at hospital level since it minimises biases related to hospitals’ case-mix.
So far, the literature has justified the variability in CSR with differences in medical practice, physicians’ behaviours, patients’ risk profile or preferences, hospitals’ characteristics and availability of resources [10,11,12,13, 15, 16, 20, 22,23,24,25,26,27,28,29]. Availability of resources has been suggested to increase activity regardless of its need, but specialized resources have been linked to lower clinically unnecessary CSR [29].
Our results were aligned with the literature. The availability of specialised resources is linked to higher CSR, measured by the positive correlation between neonatal ICU and number of beds with CSR-LRD.
When other variables were considered in the models, the ratio of obstetricians to obstetric beds was not significant suggesting that the relationship between obstetric resources availability did not explain the differences found in CSR-LRD.
When panel data models were estimated, accommodating for time fixed effects, hospital characteristics became not significant. This suggested that, apart from hospital characteristics, there may have been other factors explaining the differences between the CSR-LRD at hospital level. Moreover, even when statistically significant, marginal effects of hospital characteristics were small and changes in resources would only affect CSR-LRD slightly. The R2 was small conveying that the selected hospital characteristics were not very relevant in justifying variations across hospitals.
Auditing and feedback on all CS, second opinions, training of doctors on caesarean delivery guidelines and implementation of health education and behaviour change strategies, have all been hailed as crucial measures to reduce CSR, without affecting patient outcomes. However, the literature is inconclusive. Some authors have found positive results [37,38,39], while others have found modest results [40,41,42]. The findings of Epstein and Nicholson [41], for example, suggested that experience sharing did not lead to physicians’ prior belief or practice change. Other suggestions for reducing rates include annual publication of the CSR per hospital and the inpatient rate due to hypoxic-ischemic new-borns, equalizing the payment of CS and vaginal delivery, financial incentives to hospitals that present lower CSR, implementation of an operating theatre next to a delivery room and the implementation of a rule of non-induction of labour with no medical reason before 41 weeks gestation [8]. In Portugal, the implementation of these measures seems to have led to a decrease in NHS hospitals CSR, to 28.1%, in 2014 [8].
There were some discrepancies between the results found in this work and the results from other authors. This work focus was on low-risk deliveries as opposed to using the general CSR or the common nulliparous, term, singleton and vertex births (NTSV) and thus results were not truly comparable. Nevertheless, CSR did not account for CS that were clinical justifiable and the NTSV definition has proven not to be sufficient to eliminate potential clinical justification for CS. This lack of comparison also happened when using other metrics and comparing results across countries since there have been international discrepancies in the classification of deliveries without complications [43].
Strengths and limitations
This paper has an innovative modelling approach. So far different models were used in the literature with some authors modelling the probability of CS delivery and not CSR-LRD at hospital level. The choice of FRM to model the research question was technically the most appropriate given the fractionary nature of the response variable. As for the choice of the panel-data model, this estimator could accommodate individual characteristics of hospitals beyond hospital characteristics already included.
The small explanatory power of the models revealed that much of the variation in the CSR-LR was still to be explained, but further variables relating to medical practice and organizational settings were not available, as weren’t mothers’ preferences or economic incentives to the physicians. However, at the time of the analysis, economic incentives to change physicians’ behaviours had not been implemented in Portugal therefore their impact could not have been assessed.
Additional limitations relate to aggregated information on merged hospitals which made us lose additional insights on individual hospitals, data unavailability of other potential explanatory variables such as anaesthesiologists who are required to perform CS and the role of hospitals’ financial incentives on performance.
Conclusion
Policies aiming at reducing CSR, namely CSR-LRD, should not focus on increasing efficiency by reducing available resources. In fact, policies targeting practice change may be more effective, as reported in literature [37,38,39]. This can be achieved not only by introducing economic incentives, but also by investing in continuous training of doctors, through the development of shared obstetric protocols and monitoring adherence to standardized clinical guidelines, and by promoting trial of labour after caesarean (TOLAC) where appropriate. Possible interventions include performing peer reviews, obtaining second opinions on adequacy for all CS, and auditing representative samples of CS cases, as suggested by different authors [8, 15, 20, 37,38,39]. Further, raising awareness of staff/patients by opinion leaders and prenatal counselling for women and partners would be important. Public health campaigns aimed at the general population on the risks associated with CS could also be given a careful thought. We expect that our findings contribute to policy makers designing effective policies to reduce c-section rates at the hospital and national level.
Availability of data and materials
Data is not available to be shared with other researchers.
References
Althabe, F. and J.M. Belizán, Caesarean section: the paradox, in Lancet. 2006: England. p. 1472-3.
Gibbons, L., et al., Inequities in the use of cesarean section deliveries in the world, in Am J Obstet Gynecol. 2012, © 2012 Mosby, Inc: United States. p. 331 e1-19.
WHO Statement on caesarean section rates, in Reprod Health Matters. 2015: England. p. 149-50.
Betran AP et al (2015) What is the optimal rate of caesarean section at population level? A systematic review of ecologic studies. Reprod Health 12(1):57
Aelvoet W et al (2008) Screening for inter-hospital differences in cesarean section rates in low-risk deliveries using administrative data: an initiative to improve the quality of care. BMC Health Serv Res 8:3
Betrán, A.P., et al., Rates of caesarean section: analysis of global, regional and national estimates, in Paediatr Perinat Epidemiol. 2007: England. p. 98-113.
Souza JP et al (2010) Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: the 2004-2008 WHO Global Survey on Maternal and Perinatal Health. BMC Med 8(1):71
Ayres-De-Campos D et al (2015) Lowered national cesarean section rates after a concerted action. Acta Obstet Gynecol Scand 94(4):391–398
Gibbons, L., et al., The global numbers and costs of additionally needed and unnecessary caesarean sections performed per year: overuse as a barrier to universal coverage. 2010, World Health Report.
Bailit, J.L., T.E. Love, and B. Mercer, Rising cesarean rates: are patients sicker?, in Am J Obstet Gynecol. 2004: United States. p. 800-3.
Finsen, V., A.H. Storeheier, and O.G. Aasland, Cesarean section: Norwegian women do as obstetricians do--not as obstetricians say, in Birth. 2008: United States. p. 117-20.
Habiba, M., et al., Caesarean section on request: a comparison of obstetricians' attitudes in eight European countries, in BJOG. 2006: England. p. 647-56.
Lehmann, S., et al., Norwegian midwives and doctors have increased cesarean section rates, in Acta Obstet Gynecol Scand. 2007: United States. p. 1087-9.
Costa-Ramón, A.M., et al., It's about time: Cesarean sections and neonatal health, in J Health Econ. 2018, © 2018 Elsevier B.V: Netherlands. p. 46-59.
Cegolon L et al (2020) Understanding Factors Leading to Primary Cesarean Section and Vaginal Birth After Cesarean Delivery in the Friuli-Venezia Giulia Region (North-Eastern Italy), 2005-2015. Sci Rep 10(1):380
Baicker K, Buckles KS, Chandra A (2006) Geographic variation in the appropriate use of cesarean delivery. Health Aff (Millwood) 25(5):w355–w367
Ma KZ, Norton EC, Lee SY (2010) Declining fertility and the use of cesarean delivery: evidence from a population-based study in Taiwan. Health Serv Res 45(5 Pt 1):1360–1375
McCourt C et al (2007) Elective cesarean section and decision making: a critical review of the literature. Birth 34(1):65–79
Schulkind L, Shapiro TM (2014) What a difference a day makes: quantifying the effects of birth timing manipulation on infant health. J Health Econ 33:139–158
Cegolon L et al (2019) A systematic evaluation of hospital performance of childbirth delivery modes and associated factors in the friuli venezia giulia region (North-Eastern Italy), 2005-2015. Sci Rep 9(1):19442
Brown HS (1996) Physician demand for leisure: implications for cesarean section rates. J Health Econ 15(2):233–242
Kozhimannil KB, Law MR, Virnig BA (2013) Cesarean delivery rates vary tenfold among US hospitals; reducing variation may address quality and cost issues. Health Aff (Millwood) 32(3):527–535
Zeitlin J et al (2010) Variability in caesarean section rates for very preterm births at 28-31 weeks of gestation in 10 European regions: results of the MOSAIC project. Eur J Obstet Gynecol Reprod Biol 149(2):147–152
Clark SL et al (2007) Variation in the rates of operative delivery in the United States. Am J Obstet Gynecol 196(6):526.e1–526.e5
Grytten J, Monkerud L, Sørensen R (2012) Adoption of diagnostic technology and variation in caesarean section rates: a test of the practice style hypothesis in Norway. Health Serv Res 47(6):2169–2189
Cegolon L et al (2020) Determinants of length of stay after cesarean sections in the Friuli Venezia Giulia Region (North-Eastern Italy), 2005-2015. Sci Rep 10(1):19238
Cegolon L et al (2019) Length of stay following cesarean sections: A population based study in the Friuli Venezia Giulia region (North-Eastern Italy), 2005-2015. PLoS One 14(2):e0210753
Lauer JA et al (2010) Determinants of caesarean section rates in developed countries: supply, demand and opportunities for control in World Health Report (2010). World Health Organization, p 22
Clark SL et al (1998) Institutional influences on the primary cesarean section rate in Utah, 1992 to 1995. Am J Obstet Gynecol 179(4):841–845
Snyder CC et al (2011) The influence of hospital type on induction of labor and mode of delivery. Am J Obstet Gynecol 205(4):346.e1–346.e4
Han KT et al (2017) Do hospital characteristics influence Cesarean delivery? Analysis of National Health Insurance claim data. Eur J Public Health 27(5):801–807
García-Armesto, S., et al., Potential of geographical variation analysis for realigning providers to value-based care. ECHO case study on lower-value indications of C-section in five European countries, in Eur J Public Health. 2015, © The Author 2015. Published by Oxford University Press on behalf of the European Public Health Association: England. p. 44–51.
Mateus C (2011) Portugal: Results of 25 years of experience with DRGs. In: Busse R et al (eds) Diagnosis-Related Groups in Europe Moving towards transparency, efficiency and quality in hospitals. McGraw Hill
Papke LE, Wooldridge JM (1996) Econometric methods for fractional response variables with an application to 401(k) plan participation rates. J Appl Economet 11(6):619–632
Ramalho EA, Ramalho JJS, Murteira JMR (2011) Alternative estimating and testing empirical strategies for fractional regression models. J Econ Surveys 25(1):19–68
Ramalho EA, Ramalho JJS, Coelho LMS (2018) Exponential regression of fractional-response fixed-effects models with an application to firm capital structure. J Econom Methods 7(1):20150019. https://doi.org/10.1515/jem-2015-0019
Althabe F et al (2004) Mandatory second opinion to reduce rates of unnecessary caesarean sections in Latin America: a cluster randomised controlled trial. Lancet 363(9425):1934–1940
Poma PA (1998) Effect of departmental policies on cesarean delivery rates: a community hospital experience. Obstet Gynecol 91(6):1013–1018
Socol, M.L., et al., Reducing cesarean births at a primarily private university hospital. Am J Obstet Gynecol, 1993. 168(6 Pt 1): p. 1748–54; discussion 1754-8.
Bickell NA et al (1996) Effect of external peer review on cesarean delivery rates: a statewide program. Obstet Gynecol 87(5 Pt 1):664–667
Epstein AJ, Nicholson S (2009) The formation and evolution of physician treatment styles: an application to cesarean sections. J Health Econ 28(6):1126–1140
Frigoletto FD Jr et al (1995) A clinical trial of active management of labor. N Engl J Med 333(12):745–750
Or Z et al (2012) Diagnosis related groups and variations in resource use for child delivery across 10 European countries. Health Econ 21(Suppl 2):55–65
Acknowledgments
The authors would like to thank the Administration of the Health System (Administração Central do Sistema de Saúde) and the Directorate General of Health (Direcção Geral de Saúde) for the data made available through the European Collaboration for Healthcare Optimization project, to which special thanks should also be addressed. We also thank Pedro Pita Barros and Sara Machado for their feedback and comments on previous versions of this paper. The authors thank the Editor and the referees for their valuable suggestions and comments that have much improved this paper.
Funding
The research leading to these results has received funding from the European Community's Seventh Framework Programme (FP7/2007-2013) under grant agreement n°242189. Sole responsibility lies with the authors, and the European Commission is not responsible for any use that may be made of the information contained therein.
Author information
Authors and Affiliations
Contributions
IJ conceived the original idea, was responsible for the statistical analysis and took the lead in writing the manuscript. CM was responsible for gathering the data, supervising the study, and revising the manuscript. All authors provided critical feedback and contributed to the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests or financial conflicts.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Joaquim, I., Pereira, L.N., Nunes, C. et al. C-sections and hospital characteristics: a long term analysis on low-risk deliveries. Res Health Serv Reg 1, 15 (2022). https://doi.org/10.1007/s43999-022-00014-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43999-022-00014-2