Abstract
Pharmacogenomic testing has emerged as an aid in clinical decision making for psychiatric providers, but more data is needed regarding its utility in clinical practice and potential impact on patient care. In this cross-sectional study, we determined the real-world prevalence of pharmacogenomic actionability in patients receiving psychiatric care. Potential actionability was based on the prevalence of CYP2C19 and CYP2D6 phenotypes, including CYP2D6 allele-specific copy number variations (CNVs). Combined actionability additionally incorporated CYP2D6 phenoconversion and the novel CYP2C-TG haplotype in patients with available medication data. Across 15,000 patients receiving clinical pharmacogenomic testing, 65% had potentially actionable CYP2D6 and CYP2C19 phenotypes, and phenotype assignment was impacted by CYP2D6 allele-specific CNVs in 2% of all patients. Of 4114 patients with medication data, 42% had CYP2D6 phenoconversion from drug interactions and 20% carried a novel CYP2C haplotype potentially altering actionability. A total of 87% had some form of potential actionability from genetic findings and/or phenoconversion. Genetic variation detected via next-generation sequencing led to phenotype reassignment in 22% of individuals overall (2% in CYP2D6 and 20% in CYP2C19). Ultimately, pharmacogenomic testing using next-generation sequencing identified potential actionability in most patients receiving psychiatric care. Early pharmacogenomic testing may provide actionable insights to aid clinicians in drug prescribing to optimize psychiatric care.
Similar content being viewed by others
Introduction
Nearly half of patients diagnosed with major depressive disorder (MDD) do not achieve adequate symptom reduction with traditional approaches to antidepressant selection [1, 2]. Treatment selection is partly trial-and-error, and unsuccessful medication trials prolong disabilities associated with depression [3]. Medication selection considerations include symptom characteristics, drug interactions, adverse event profiles, response to prior treatment(s), and other comorbidities. Genetic variation between patients has also been shown to affect responses to antidepressants [4,5,6], which can be tested with a pharmacogenetic (PGx) assay. Accordingly, several guidelines exist for evidence-based prescribing recommendations from the Food and Drug Administration (FDA) and the Clinical Pharmacogenetics Implementation Consortium (CPIC) [7,8,9,10,11,12]. One study showed that a PGx assay identified ≥1 gene-drug interactions (GDI) for a considered medication in more than half of patients [13]. Notably, gene-drug-drug interactions (GDDI), known as phenoconversion, can also exist where medications can inhibit or induce enzymes involved in drug metabolism and alter their baseline metabolizer phenotype [14]. Despite the extensive evidence-based recommendations for GDIs and GDDIs, some commercial assays report phenotypes that are not consistent with CPIC guidelines [15,16,17].
The guidelines for PGx testing and phenoconversion are supported by rigorous evidence and processes; however, updates to these guidelines do not keep pace with the emergence of new evidence [7, 8, 14, 18,19,20]. New variants can be discovered with next-generation sequencing (NGS) but need to be validated in other studies using comparable technology and methods [21]. For instance, one haplotype recently described involves two loci between CYP2C18 and CYP2C19 that affects selective serotonin reuptake inhibitor (SSRI) metabolism - called the “CYP2C haplotype” [22]. Patients may be classified as having normal CYP2C19 metabolism according to existing assays/guidelines, but carrying the CYP2C haplotype alleles rs2860840 C>T and rs11188059 G>A (“CYP2C-TG”) can increase their metabolism from normal to rapid or ultrarapid [22], changing potential actionability, although this was not reproduced in a subsequent study [23].
Copy number variations (CNVs) can lead to multiple alleles due to the variable number of copies, and when the alleles have different activity scores, the overall metabolism depends on which allele is copied. This is common for CYP2D6, and there are guidelines for assigning metabolic phenotype based on allele activity scores and assigned CNVs [24].
Most clinical PGx assays and commercial assays (targeted single-nucleotide polymorphism [SNP] assays) likely only test haplotypes described in guidelines [25,26,27] and cannot accurately assign CYP2D6 CNVs to an allele [21]. NGS provides the opportunity to interrogate CYP2D6 allele-specific CNVs and novel variations like the CYP2C haplotype.
Here, we evaluated the prevalence of guideline-based PGx actionability in a large, real-world cohort of patients receiving psychiatric care who were referred for clinical PGx testing using NGS. Secondarily, we determined the frequency of CYP2D6 CNVs in which identification of allele-specific CNVs altered phenotype assignment, the frequency of phenoconversion, and potential impact of the novel haplotype (CYP2C-TG) on CYP2C19 phenotype assignment. Based on these findings, we estimated the combined potential actionability of PGx testing in patients receiving psychiatric care.
Methods
Study design and data collection
A subset of de-identified records from patients who underwent Tempus nP PGx testing (Tempus AI, Inc, Chicago, IL) between April 2020 and November 2022 as part of their psychiatric care was selected for retrospective analysis. Patient demographics, diagnoses, and medications were obtained from order forms or attached progress notes. This study was deemed exempt from institutional review by the Advarra Institutional Review Board (Pro00072742).
Metabolizer phenotypes and CNV allele assignment
Patients’ saliva specimens were assayed with the Tempus nP laboratory-developed test, which combines NGS whole-exome sequencing (WES) and Agena MassARRAY® in a College of American Pathologists/Clinical Laboratory Improvement Amendments-accredited laboratory (Tempus AI, Inc., Chicago, IL, USA) [19]. Detailed methodology describing sequencing equipment, bioinformatic processing, and validation are provided in the supplementary methods. Star alleles and metabolizer phenotypes were based on clinical guidelines from CPIC, the Dutch Pharmacogenomics Working Group (DPWG), and the Association for Molecular Pathology (AMP). Genetic results were reviewed and finalized by a board-certified clinical geneticist.
Genomic DNA was used for analysis of CYP2D6 single-nucleotide variations (SNVs) and small insertions/deletions (indels) by NGS. Data synthesized from NGS and MassARRAY® were used in combination to assign CYP2D6 CNVs to a specific allele. The impact of CYP2D6 CNV allele assignment on metabolism phenotype was assessed based on activity scores as described in CPIC and DPWG consensus recommendations [24] and is referred to as “allele-specific CNV-actionability” when allele copy number assignment disambiguates patients among metabolism phenotypes with different therapy guidance (see section “PGx Actionability” below). Tempus’ system for personalized psychiatric disorder treatment is described in U.S. patent 10978196 [28].
PGx actionability: potential and clinical
CYP2D6 and CYP2C19 phenotypes were defined as “actionable” based on CPIC guidelines [7, 8, 11] (regardless of classification of recommendation) and the FDA Table of Pharmacogenetic Associations [12] for which the Data Support Therapeutic Management Recommendations (Section 1) (hereafter referred to as the “FDA Table”; Supplementary Table S1). Two levels of actionability were defined:
-
“Potentially actionable”: presence of CYP2D6 or CYP2C19 phenotypes associated with GDIs in the FDA Table or CPIC guidelines (regardless of medication(s) prescribed or considered), including potentially actionable CYP2D6 or CYP2C19 phenotypes.
-
“Clinically actionable”: presence of a GDI (Supplementary Table S1) based on prescribed or considered medications in patients with medication data available at time of testing.
Genetic ancestry and race/ethnicity imputation
Continental genetic ancestry proportions were predicted from WES data using a supervised version of the ADMIXTURE algorithm [29]. After conditioning variants on having adequate sequencing coverage on the Tempus xE and nP assays, data from the 1000 Genomes Project [30] and the Simons Genome Diversity Project [31] were used to identify a set of 6711 ancestry-informative markers (AIMs) varying in frequency among individuals from five continental regions: Africa (AFR), the Americas (AMR), Europe (EUR), East Asia (EAS), and South Asia (SAS). For each exome sequence input, the model yields estimates of the proportions of ancestry arising from each of the five continental regions.
Many patients have a mixture of continental genetic ancestries representing the genetic similarities shared between different groups. In contrast, race and ethnicity are not biological, but rather social/cultural categorizations that patients are assigned to and/or identify with [32]. We imputed race/ethnicity groups from genetic admixtures using proportions observed in patients with solid-tumor sequencing and stated race/ethnicity labels at Tempus AI [33], which are consistent with those reported for African American/Black and Hispanic/Latino groups in the United States [34]. Race/ethnicity imputation cutoffs were selected heuristically by creating mutually exclusive groups. Imputed race/ethnicity cutoffs are as follows: >20% AFR, <10% AMR, and >70% combined AFR and EUR ancestry were classified as Non-Hispanic Black (hereafter referred to as “Black”), >10% AMR and >70% combined AMR, EUR, and AFR ancestry were classified as Hispanic/Latino, >70% combined EAS and SAS ancestry were classified as Asian, >80% EUR and <10% AMR ancestry were classified as Non-Hispanic White (hereafter called “White”), and all others were classified as Complex Admixture (hereafter called “Admixed”) [35].
Phenoconversion
Phenoconversion indicates that the patient’s metabolism phenotype after accounting for interacting medications is different from that assigned by genotype alone [36]. The Indiana University Flockhart Table [37] (Supplementary Table S2) was utilized to estimate CYP2D6 phenoconversion in patients with medication data where medications were categorized as strong or moderate inhibitors [36]. CYP2D6 activity score was defined as 0 or multiplied by 0.5 for strong or moderate inhibitors, respectively.
Genotype imputation of a novel CYP2C haplotype
Only 1 of 2 loci that comprise the CYP2C-TG haplotype is targeted by the nP NGS-enhanced assay, therefore patients’ genotypes were imputed and phased at these loci using off-target sequencing reads and a reference panel of haplotypes. The imputation algorithm, GLIMPSE [38], is described in the supplementary methods. Haplotype imputation methods and software commands are provided in the “Haplotype Imputation Commands” section. Imputation performance was evaluated using the HG001 reference sample from the National Institute of Standards and Technology (NIST) (described in the supplementary methods and results).
Statistical analysis
Confidence intervals for frequency estimates were computed using bootstrap analysis. For each patient group, we randomly sampled with replacement the number of patients originally in the group 1000 times, computed the 1000-sample frequencies of a phenotype or actionability, and then reported (or plotted) 2.5th and 97.5th percentiles.
To compare frequencies of actionability among race/ethnicities, we performed chi-squared 5-sample, 2-sided proportion tests. If found to be significant (P < 0.05), then pairwise 2-sided proportion-tests between each pair of imputed race/ethnicities were applied and corrected for multiple hypotheses with Holm using the R stats package [39].
Combined actionability of PGx results, phenoconversion, and novel haplotype
We prioritized and combined actionability sources according to assay features for patients with medication and NGS data to determine initial actionability of each patient. Initial actionability was summed to determine the combined actionability of the cohort, where “initial actionability” was defined in the following order:
-
1.
Did the patient have CYP2C19 or CYP2D6 potential actionability (accounting for allele-specific CNV-actionability)?
-
a.
NGS was required to identify the initial actionability when:
-
i.
CYP2D6 was actionable with allele-specific CNV-actionability, and CYP2C19 was not actionable; or
-
ii.
There was no PGx actionability and ruling out CYP2D6 actionability required allele-specific CNV (e.g., a *1/*4 patient whose CNV was assigned to *1 resulting in a normal metabolizer phenotype).
-
i.
-
a.
-
2.
Did the remaining patients carry CYP2C-TG?
-
a.
NGS was required to identify the CYP2C-TG haplotype and identify patients that were initially CYP2C19 normal metabolizers but found to carry the CYP2C-TG actionable haplotype.
-
a.
-
3.
Did the remaining patients have CYP2D6 phenoconversion from non-actionable to actionable?
Results
Patient characteristics
Across 15,000 PGx-tested patients (median age=30 years, interquartile range 18–44 years, 63% female), the most common diagnoses were MDD (44%), generalized anxiety disorder (38%), and attention-deficit hyperactivity disorder (19%) (Table 1). Fifty-two percent of patients previously tried ≥1 prior medication. Analyses on clinical PGx testing were done in the overall cohort of 15,000 patients, whereas Research Use-Only analyses of phenoconversion and CYP2C haplotypes were conducted in the 4,114-patient subset with available medication and NGS data (Fig. 1).
Patients with clinical PGx results were assessed for potential actionability of results and CYP2D6 allele-specific copy number variation actionability. Patients with clinical PGx results and medication data were assesed for clinical actionability of results, CYP2D6 phenoconversion, presenence of a novel CYP2C-TG haplotype. The presence of clinical actionability, CYP2C-TG haplotype, or phenoconversion was assessed to determine the combined actionability of the cohort with PGx results and medication data.
Potential actionability from CYP2C19 and CYP2D6 phenotypes
Sixty-five percent of patients had a potentially actionable CYP2C19 and/or CYP2D6 phenotype associated with decreased efficacy or increased risk of toxicity for ≥1 psychiatric medication according to CPIC and/or the FDA Table (Supplementary Table S1).
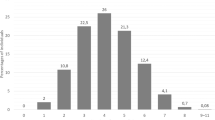
Clinical actionability based on the ordering clinician’s medications
Across 15,000 patients, 2215 had prior or current psychiatric medication information available at the time of PGx testing. Of these, 1663 patients (74%) attempted medications metabolized by CYP2D6 and/or CYP2C19 enzymes, where 360 (22%) had ≥1 clinically actionable phenotype. Medication data was also available on 2478 patients for whom the clinician was considering a new psychiatric medication. Of 1674 patients considering medications metabolized by CYP2D6 and/or CYP2C19 enzymes (68%), 295 (18%) had ≥1 clinically actionable phenotype. SSRIs were the most common attempted (n = 1,594) or considered (n = 1,334) medication class (Supplementary Table S3, Supplementary Table S4), with citalopram and escitalopram having the most frequent GDIs (32% and 30% of patients reporting medications, respectively), and sertraline being the least frequent with FDA/CPIC guidance (3%) (Fig. 2). Although tricyclic antidepressants (TCAs) were not commonly attempted (n = 132) or considered (n = 123), they were most likely to interact (59%) with the CYP2D6 and/or CYP2C19 phenotypes (Supplementary Table S5, Supplementary Table S6). Aripiprazole, dextroamphetamine/amphetamine, and venlafaxine had similar actionability rates (5%, 6%, and 5% of patients, respectively).
Each point represents a psychiatric medication with PGx prescribing guidance. The x-axis represents how many patients had the medication, and the y-axis shows how frequently those patients had clinically actionable PGx results. amit amitriptyline, arip aripiprazole, atom atomoxetine, brex brexpiprazole, cita citalopram, clom clomipramine, cloz clozapine, desi desipramine, deut deutetrabenazine, dext dextroamphetamine, doxe doxepin, esci escitalopram, fluv fluvoxamine, ilop iloperidone, imip imipramine, nort nortriptyline, paro paroxetine, sert sertraline, valb valbenazine, venl venlafaxine, vort vortioxetine.
Imputed race and ethnicity
Among the cohort, 82% were imputed as White, 7% Hispanic/Latino, 6% Black, 2% Asian, and 2% complex admixed (Supplementary Fig. 1). Potential actionability rates were highest for Whites (CYP2D6 = 50%, CYP2C19 = 34%) and Blacks (CYP2D6 = 43%, CYP2C19 = 33%), and lowest for Asians (CYP2D6 = 39%, CYP2C19 = 22%) (Fig. 3). CYP2C19 potential actionability was significantly higher for Whites than Hispanic/Latinos, Asians, and complex admixed (P ≤ 0.02); CYP2D6 potential actionability was significantly higher for Whites than Hispanic/Latinos, Blacks, and Asians (P ≤ 6e-4). Overall, Whites had significantly higher actionability rates than all other groups (P ≤ 9e-4) and Blacks had higher actionability rates than Hispanic/Latino and Asian groups (P = 0.05).
The 95% confidence limits for each race/ethnicity and gene’s potential actionability are indicated with error bars and were estimated with nonparametric bootstrapping. Proportion tests between pairs of race/ethnicity are displayed as horizontal lines with stars “*” above pairs that are significantly different (P < 0.05) and sorted from most significant to least significant top to bottom.
CYP2D6 copy number variations
Of 15,000 patients tested, 1,104 (7%) harbored CYP2D6 CNVs, and 338 (30%, or 2% of the total population) had a genotype where knowledge of allele-specific CYP2D6 CNVs would change the phenotype and corresponding actionability. The most common CYP2D6 genotypes requiring allele-specific CNVs to assign correct phenotype were *1/*4, *2/*4, *2/*41, *4/*35, *35/*41, *10/*41, *1/*41, and *1/*6 (Table 2). The rate of CYP2D6 CNVs and allele-specific CNV-actionability were significantly different among imputed races (5-sample chi-square P = 2e-16 and 2e-5, respectively). CYP2D6 CNV rate was highest in Asians and lowest in Whites, while the rate of allele-specific CNV actionability was highest in Blacks (4%) (Supplementary Table S7).
Phenoconversion
Among 4114 patients with any reported medications, 1980 (48%) were reported to receive medications that were moderate or strong CYP2D6 inhibitors, most commonly bupropion (n = 1002 patients) and fluoxetine (n = 952). Of those receiving moderate or strong CYP2D6 inhibitors, the CYP2D6 metabolism phenotype and potential actionability changed in 1734 patients (87%) – or 42% of all patients with reported medications (relative to the genotype-based phenotype) (Supplementary Table S8).
CYP2C haplotypes
Genotype imputation at individual CYP2C loci in the 4,114 patients with medication data predicted alternative frequencies matching the National Institutes of Health (NIH) dbSNP database: 33% rs2860840 C>T [40] and 13% rs11188059 G>A [41]. On average, there were NGS results at 1,436 (standard deviation (SD) = 196) of the 7220 linked SNPs in the region (region = chr10:96375267-98547144; mean effective coverage = 0.2×; SD = 0.03x).
The overall frequency of the CYP2C-TG haplotype was 36%. Of patients with a CYP2C19 *1/*1 diplotype (40%), 51% were expected to have at least one CYP2C-TG allele. Therefore, should the CYP2C haplotype be validated and considered actionable in future guidelines, then approximately 21% of all patients could experience a change in CYP2C19 actionability from normal metabolizer to rapid or ultrarapid metabolizer when this variant is interrogated. Additionally, CYP2C-TG frequencies differed significantly among imputed race/ethnicities. Black patients had the lowest frequency (14%) compared to Asian (34%), White (37%), and Hispanic/Latino (46%) (Supplementary Table S9, Supplementary Table S10). Hispanics had a higher frequency of altered phenotypes (30%) than Whites (21%) and Blacks (9%) (Supplementary Table S11).
Combined actionability in patients with medication data
Considering the 4,114 patients with medication and WES data available, 66% had a potentially actionable CYP2D6 or CYP2C19 phenotype with 2% requiring NGS to confirm allele-specific CYP2D6 CNVs (Table 3). Of the remaining 34% of patients, an additional 10% did not have a potentially actionable CYP2D6 or CYP2C19 phenotype but were expected to carry the CYP2C-TG allele (based on WES), increasing the total potential actionability to 76%. Further, an additional 11% of patients had a drug interaction resulting in CYP2D6 phenoconversion, culminating in a final combined actionability of 87%. Overall, 11% of patients had initial actionability, and 22% had some actionability that was detected with the NGS-enhanced PGx platform.
Discussion
To our knowledge, this is the first study to evaluate PGx actionability of CYP2D6 and CYP2C19 variants in a large real-world cohort of patients receiving NGS-based clinical PGx testing in the US. In this study of 15,000 patients, the majority (65%) had a potentially actionable CYP2D6 or CYP2C19 phenotype which corresponded to a GDI based on CPIC guidelines and the FDA Table Section 1. Roughly half of the patients who had medication data available reported taking a strong or moderate CYP2D6-inhibiting medication resulting in phenoconversion and altered metabolism phenotype from baseline. CYP2D6 CNVs were observed in 7% of patients and the NGS-based PGx test allowed for allele-specific CNV assignment, leading to a change in CYP2D6 phenotype assignment in almost one-third of these patients. Using NGS to also impute a novel CYP2C haplotype demonstrated that half of the patients currently assigned a CYP2C19 normal metabolizer phenotype carry this novel haplotype and may be predicted to metabolize certain antidepressant medications faster than normal, if validated in subsequent studies.
The prevalence of actionable phenotypes observed in our predominantly European ancestry cohort is similar to previous studies of individuals of European ancestry [42], and marked differences in CYP2D6 CNV rates (~2-fold) have previously been observed between geographic cohorts [43, 44]. The predominance of White patients in this cohort may be exacerbated by racial disparities in the U.S. in receiving PGx testing to guide their care [45, 46]. Actionable phenotypes were observed across all race and ethnicity categories in this cohort, albeit at lower frequencies in minority groups. Notably, most alleles associated with drug response have been discovered primarily in patients of European ancestries [47], which may inform the alleles included on various panels, thus limiting their actionability to cohorts of other ancestries [48].
In the subset of patients with medication data, 22% and 18% of patients had a GDI with their attempted and considered medications, respectively. SSRIs, specifically citalopram and escitalopram, were the most common medications affected by PGx, as these are commonly prescribed medications with prescribing guidance for all non-normal CYP2C19 metabolizers [7, 12, 20]. The most prescribed SSRI, sertraline, had 10x lower rates of actionability than (es)citalopram because there is only guidance for CYP2C19 poor metabolizers. Although TCAs are not frequently prescribed, this class of medications is most likely to be clinically actionable since many TCAs are impacted by both CYP2C19 and CYP2D6 metabolism [8]. Due to marked differences in actionability rates between medications, healthcare providers and systems may consider PGx testing more strongly when patients are eligible for medications with high actionability rates.
We were able to assign CNVs to a specific CYP2D6 allele to improve accuracy in assigning genotype and phenotype. In this study, nearly one-third of patients with CNVs would have been assigned a phenotype range, assigned a potentially inaccurate phenotype, or marked as indeterminant in the absence of allele-specific CNV assignment. Precise genotypic and phenotypic assignment are crucial to identify patients with actionable results and optimize PGx-guided medication prescribing for the more than 20 psychiatric-related medications metabolized by CYP2D6.
Based on the CPIC guideline for SSRIs published in 2015, sertraline should be initiated at standard dose except for CYP2C19 poor metabolizers; however, there is emerging evidence that additional haplotypes and genes can impact the metabolism of sertraline and other SSRIs. The CYP2C-TG haplotype was reported in patients previously identified as CYP2C19 normal metabolizers to be associated with decreased sertraline and escitalopram levels similar to CYP2C19 rapid/ultrarapid metabolizers, therefore potentially requiring higher doses or alternative medications [22]. To our knowledge, inclusion of this novel haplotype is not available on commercial clinical PGx tests and still requires further clinical validation. However, NGS-based genotype imputation found that more than half of CYP2C19 normal metabolizers in this cohort carry the CYP2C-TG haplotype and may benefit from higher dosing or an alternative medication, if validated in subsequent studies. Additional studies are needed to confirm the clinical impact of this novel haplotype on two of the most prescribed antidepressants in this cohort. Additionally, there is emerging evidence for variations in other CYP450 genes including CYP2B6 affecting antidepressant concentrations [20, 49]. Incorporating emerging biomarkers into PGx testing guidelines and clinical care in the future will identify more patients with actionable results to guide drug prescribing.
When patients are taking multiple medications, it is important to consider GDDIs which can change the predicted phenotype and medication metabolism. In this cohort, nearly half of patients with medication data were prescribed or being considered for a medication that inhibits CYP2D6, and most (87%) would result in an alternate phenotype due to phenoconversion. Of all patients with medication data, 42% had phenoconversion, which is slightly greater than the 10–30% prevalence seen in other clinical cohorts [50, 51]. This is likely due to this cohort being a psychiatric population where strong CYP2D6-inhibiting medications such as bupropion and fluoxetine are more commonly prescribed. Notably, while patients receiving fluoxetine or paroxetine can experience phenoconversion due to strong CYP2D6 inhibition, the impact of autoinhibition (since these drugs are also metabolized by CYP2D6) is unclear and is likely to be dose-dependent and greater at steady-state concentrations [52]. Nonetheless, these drugs were included in the calculation of proportion with phenoconversion since patients could be on other CYP2D6-metabolized drugs and the overall goal was to determine the proportion experiencing phenoconversion regardless of which drug is causing the inhibition or if autoinhibition is present.
Many laboratory platforms exist for interrogating pharmacogenes, ranging from single-gene assays (e.g., TaqMan) to targeted or WES. While targeted assays are informative for the SNPs of interest, relatively easier to perform with faster turnaround time, and less expensive, the inherent limitations are the inability to accurately detect novel or rare variants not included on the reported panel and inability to disambiguate certain alleles or structural variation within complex genes like CYP2D6.
NGS generates data on novel haplotypes which are not measured in most PGx assays. In the largest dataset tested for the CYP2C-TG haplotype thus far, we reproduced the overall prevalence and showed that Black patients have a significantly lower frequency of this haplotype compared to Hispanics/Latinos and Whites. Generating data on novel variants across genetic ancestries is important for organizations like the AMP and National Human Genomics Research Institute to expand non-White associations and bring equity to personalized medicine.
There are limitations of this study. First, attempted or considered medication data was only available for a subset of patients, and data may have been missing or affected by reporting bias. This study did not evaluate outcomes related to potential medication changes based on the PGx results and therefore conclusions of clinical utility cannot be made. Only two genes, CYP2D6 and CYP2C19, were evaluated in this study and actionability was limited to CPIC guidelines (2015) [7] and the FDA Table that were available at the time when patients were tested; therefore, more recent CPIC guidelines (2023) [20] or updates to the FDA table could affect the results of this study. Inclusion of additional alleles and GDIs would likely capture additional patients with actionable results to guide medication prescribing. Additionally, the data herein may not be generalizable to PGx tests other than the one used in this study. The alleles evaluated in this study were based on CPIC and AMP guidelines and may report undetected variants as *1, potentially missing unknown actionable phenotypes. Lastly, the combined actionability, including the CYP2C haplotype may be overestimated since the clinical utility of this variant has yet to be confirmed.
Conclusion
This evaluation of a large real-world psychiatric patient population receiving clinical PGx testing identified a high proportion of patients with potential actionability for medication prescribing decisions. While this analysis focused on two genes (CYP2D6 and CYP2C19), other emerging genes may also play a role and further increase the potential actionability of PGx testing. This study underscores the potential value of using NGS to detect CYP2D6 allele-specific CNV allele assignment in CYP2D6 genotype/phenotype calling and the novel CYP2C haplotype. When accounting for these variations, as well as phenoconversion, most patients displayed some level of actionability. This information is critical for clinicians, laboratories, and researchers to consider when applying PGx in psychiatric care.
Data availability
Deidentified data used in the research was collected in a real-world healthcare setting and is subject to controlled access for privacy and proprietary reasons. When possible, derived data supporting the findings of this study have been made available within the paper and its Supplementary figures/tables.
References
Thase ME, Entsuah AR, Rudolph RL. Remission rates during treatment with venlafaxine or selective serotonin reuptake inhibitors. Br J Psychiatry. 2001;178:234–41.
Trivedi MH, John Rush A, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163:28–40.
Andersen BL, DeRubeis RJ, Berman BS, Gruman J, Champion VL, Massie MJ, et al. Screening, assessment, and care of anxiety and depressive symptoms in adults with cancer: an American Society of Clinical Oncology guideline adaptation. J Clin Oncol. 2014;32:1605–19.
Arnone D, Omar O, Arora T, Östlundh L, Ramaraj R, Javaid S, et al. Effectiveness of pharmacogenomic tests including CYP2D6 and CYP2C19 genomic variants for guiding the treatment of depressive disorders: systematic review and meta-analysis of randomised controlled trials. Neurosci Biobehav Rev. 2023;144:104965.
Bousman CA, Arandjelovic K, Mancuso SG, Eyre HA, Dunlop BW. Pharmacogenetic tests and depressive symptom remission: a meta-analysis of randomized controlled trials. Pharmacogenomics. 2019;20:37–47.
Brown LC, Stanton JD, Bharthi K, Maruf AA, Müller DJ, Bousman CA. Pharmacogenomic testing and depressive symptom remission: a systematic review and meta-analysis of prospective, controlled clinical trials. Clin Pharmacol Ther. 2022;112:1303–17.
Hicks JK, Bishop JR, Sangkuhl K, Müller DJ, Ji Y, Leckband SG, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for CYP2D6 and CYP2C19 Genotypes and Dosing of Selective Serotonin Reuptake Inhibitors. Clin Pharmacol Ther. 2015;98:127–34.
Hicks JK, Sangkuhl K, Swen JJ, Ellingrod VL, Müller DJ, Shimoda K, et al. Clinical Pharmacogenetics Implementation Consortium guideline (CPIC) for CYP2D6 and CYP2C19 genotypes and dosing of tricyclic antidepressants: 2016 update. Clin Pharmacol Ther. 2017;102:37–44.
Karnes JH, Rettie AE, Somogyi AA, Huddart R, Fohner AE, Formea CM, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline for CYP2C9 and HLA‐B genotypes and phenytoin dosing: 2020 update. Clin Pharmacol Ther. 2021;109:302–9.
Phillips EJ, Sukasem C, Whirl-Carrillo M, Müller DJ, Dunnenberger HM, Chantratita W, et al. Clinical Pharmacogenetics Implementation Consortium Guideline for HLA genotype and use of carbamazepine and oxcarbazepine: 2017 update. Clin Pharmacol Ther. 2018;103:574–81.
Brown JT, Bishop JR, Sangkuhl K, Nurmi EL, Mueller DJ, Dinh JC, et al. Clinical Pharmacogenetics Implementation Consortium guideline for cytochrome P450 (CYP)2D6 genotype and atomoxetine therapy. Clin Pharmacol Ther. 2019;106:94–102.
Center for Devices, Radiological Health. Table of Pharmacogenetic Associations. US Food and Drug Administration. https://www.fda.gov/medical-devices/precision-medicine/table-pharmacogenetic-associations. Accessed 20 March 2023.
Ramsey CM, Lynch KG, Thase ME, Gelernter J, Kranzler HR, Pyne JM, et al. Prevalence of predicted gene-drug interactions for antidepressants in the treatment of major depressive disorder in the Precision Medicine in Mental Health Care Study. J Affect Disord. 2021;282:1272–7.
Center for Drug Evaluation, Research. Drug development and drug interactions. US Food and Drug Administration; 2022. https://www.fda.gov/drugs/drug-interactions-labeling/drug-development-and-drug-interactions-table-substrates-inhibitors-and-inducers. Accessed 29 Jan 2023.
Pratt VM, Everts RE, Aggarwal P, Beyer BN, Broeckel U, Epstein-Baak R, et al. Characterization of 137 genomic DNA reference materials for 28 pharmacogenetic genes: a GeT-RM collaborative project. J Mol Diagn. 2016;18:109–23.
Bousman CA, Dunlop BW. Genotype, phenotype, and medication recommendation agreement among commercial pharmacogenetic-based decision support tools. Pharmacogenomics J. 2018;18:613–22.
Blazy C, Ellingrod V, Ward K. Variability Between Clinical Pharmacogenetics Implementation Consortium (CPIC®) guidelines and a commercial pharmacogenetics laboratory in genotype to phenotype interpretations for patients utilizing psychotropics. Front Pharmacol. 2022;13:939313.
Hahn M, Roll SC. The role of phenoconversion in the pharmacogenetics of psychiatric medication. Pharmacogenomics. 2023;24:485–7.
Nahid NA, Johnson JA. CYP2D6 pharmacogenetics and phenoconversion in personalized medicine. Expert Opin Drug Metab Toxicol. 2022;18:769–85.
Bousman CA, Stevenson JM, Ramsey LB, Sangkuhl K, Hicks JK, Strawn JR, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline for CYP2D6, CYP2C19, CYP2B6, SLC6A4, and HTR2A genotypes and serotonin reuptake inhibitor antidepressants. Clin Pharmacol Ther. 2023;114:51–68.
Enko D, Michaelis S, Schneider C, Schaflinger E, Baranyi A, Schnedl WJ, et al. The use of next-generation sequencing in pharmacogenomics. Clin Lab. 2023;69 https://doi.org/10.7754/Clin.Lab.2023.230103.
Bråten LS, Haslemo T, Jukic MM, Ivanov M, Ingelman-Sundberg M, Molden E, et al. A novel CYP2C-haplotype associated with ultrarapid metabolism of escitalopram. Clin Pharmacol Ther. 2021;110:786–93.
Zubiaur P, Soria-Chacartegui P, Boone EC, Prasad B, Dinh J, Wang WY, et al. Impact of CYP2C:TG Haplotype on CYP2C19 substrates clearance in vivo, protein content, and in vitro activity. Clin Pharmacol Ther. 2023. https://doi.org/10.1002/cpt.3012.
Caudle KE, Sangkuhl K, Whirl-Carrillo M, Swen JJ, Haidar CE, Klein TE, et al. Standardizing CYP2D6 genotype to phenotype translation: consensus recommendations from the Clinical Pharmacogenetics Implementation Consortium and Dutch Pharmacogenetics Working Group. Clin Transl Sci. 2020;13:116–24.
Pratt VM, Cavallari LH, Del Tredici AL, Gaedigk A, Hachad H, Ji Y, et al. Recommendations for clinical CYP2D6 genotyping allele selection: a joint consensus recommendation of the Association for Molecular Pathology, College of American Pathologists, Dutch Pharmacogenetics Working Group of the Royal Dutch Pharmacists Association, and the European Society for Pharmacogenomics and Personalized Therapy. J Mol Diagn. 2021;23:1047–64.
Pratt VM, Del Tredici AL, Hachad H, Ji Y, Kalman LV, Scott SA, et al. Recommendations for clinical CYP2C19 genotyping allele selection: a report of the association for molecular pathology. J Mol Diagn. 2018;20:269–76.
NIH National Library of Medicine. Genetic Testing Registry. National Library of Medicine Genetic Testing Registry. https://www.ncbi.nlm.nih.gov/gtr/. Accessed 13 Mar 2024.
Data-based mental disorder research and treatment systems and methods. USPTOReport. https://uspto.report/patent/grant/10,978,196. Accessed 10 Aug 2023.
Alexander DH, Novembre J, Lange K. Fast model-based estimation of ancestry in unrelated individuals. Genome Res. 2009;19:1655–64.
1000 Genomes Project Consortium, Auton A, Brooks LD, Durbin RM, Garrison EP, Kang HM, et al. A global reference for human genetic variation. Nature. 2015;526:68–74.
Mallick S, Li H, Lipson M, Mathieson I, Gymrek M, Racimo F, et al. The Simons Genome Diversity Project: 300 genomes from 142 diverse populations. Nature. 2016;538:201–6.
National Academies of Sciences, Engineering, and Medicine, Division of Behavioral and Social Sciences and Education, Health and Medicine Division, Committee on Population, Board on Health Sciences Policy, Committee on the Use of Race, Ethnicity, and Ancestry as Population Descriptors in Genomics Research. Using population descriptors in genetics and genomics research: a new framework for an evolving field. Washington DC: National Academies Press; 2023.
Rhead B, Haffener PE, Pouliot Y, De La Vega FM. Imputation of race and ethnicity categories using genetic ancestry from real-world genomic testing data. Biocomputing. 2024;2023:433–45.
Bryc K, Durand EY, Michael Macpherson J, Reich D, Mountain JL. The genetic ancestry of African Americans, Latinos, and European Americans across the United States. Am J Hum Genet. 2015;96:37–53.
Hein DM, Deng W, Bleile M, Kazmi SA, Rhead B, De La Vega FM, et al. Racial and ethnic differences in genomic profiling of early onset colorectal cancer. J Natl Cancer Inst. 2022;114:775–8.
Cicali EJ, Smith DM, Duong BQ, Kovar LG, Cavallari LH, Johnson JA. A scoping review of the evidence behind cytochrome P450 2D6 isoenzyme inhibitor classifications. Clin Pharmacol Ther. 2020;108:116–25.
Indiana University. Drug Interactions Flockhart Table. 2024. https://drug-interactions.medicine.iu.edu/MainTable.aspx. Accessed 6 Feb 2024.
Rubinacci S, Ribeiro DM, Hofmeister RJ, Delaneau O. Efficient phasing and imputation of low-coverage sequencing data using large reference panels. Nat Genet. 2021;53:120–6.
R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2013.
NIH National Library of Medicine. rs2860840. rs2860840 Reference SNP (Rs) Report. 2022. https://www.ncbi.nlm.nih.gov/snp/rs2860840. 20 Accessed Mar 2023.
NIH National Library of Medicine. rs11188059. Rs11188059 Reference SNP (Rs) Report. 2022. https://www.ncbi.nlm.nih.gov/snp/rs11188059. Accessed 20 Mar 2023.
Koopmans AB, Braakman MH, Vinkers DJ, Hoek HW, van Harten PN. Meta-analysis of probability estimates of worldwide variation of CYP2D6 and CYP2C19. Transl Psychiatry. 2021;11:141.
Ivanov HY, Grigorova D, Lauschke VM, Velinov B, Stoychev K, Kyosovska G, et al. CYP2C19 and CYP2D6 genotypes and metabolizer status distribution in a Bulgarian psychiatric cohort. J Pers Med. 2022;12:1187.
Häkkinen K, Kiiski JI, Lähteenvuo M, Jukuri T, Suokas K, Niemi-Pynttäri J, et al. Implementation of CYP2D6 copy-number imputation panel and frequency of key pharmacogenetic variants in Finnish individuals with a psychotic disorder. Pharmacogenomics J. 2022;22:166–72.
Knerr S, Wayman D, Bonham VL. Inclusion of racial and ethnic minorities in genetic research: advance the spirit by changing the rules? J Law Med Ethics. 2011;39:502–12.
Adiukwu F, Essien EA, Adesokun O, Ofori S. Psychiatry pharmacogenomics: Africans are not at the table. Lancet Psychiatry. 2023;10:80.
Uffelmann E, Huang QQ, Munung NS, de Vries J, Okada Y, Martin AR, et al. Genome-wide association studies. Nat Rev Methods Primers. 2021;1:1–21.
Kimmel SE, French B, Kasner SE, Johnson JA, Anderson JL, Gage BF, et al. A pharmacogenetic versus a clinical algorithm for warfarin dosing. N Engl J Med. 2013;369:2283–93.
Bråten LS, Ingelman-Sundberg M, Jukic MM, Molden E, Kringen MK. Impact of the novel CYP2C:TG haplotype and CYP2B6 variants on sertraline exposure in a large patient population. Clin Transl Sci. 2022;15:2135–45.
Cicali EJ, Weitzel KW, Elsey AR, Orlando FA, Vinson M, Mosley S, et al. Challenges and lessons learned from clinical pharmacogenetic implementation of multiple gene-drug pairs across ambulatory care settings. Genet Med. 2019;21:2264–74.
Smith DM, Weitzel KW, Elsey AR, Langaee T, Gong Y, Wake DT, et al. CYP2D6-guided opioid therapy improves pain control in CYP2D6 intermediate and poor metabolizers: a pragmatic clinical trial. Genet Med. 2019;21:1842–50.
CPIC. CPIC® Guideline for serotonin reuptake inhibitor antidepressants and CYP2D6, CYP2C19, CYP2B6, SLC6A4, and HTR2A. CPIC PGx guidelines. https://cpicpgx.org/guidelines/cpic-guideline-for-ssri-and-snri-antidepressants/. Accessed 13 Mar 2024.
Acknowledgements
We would like to express our sincere gratitude to Matthew Kase for his invaluable contribution in refining and improving the quality of this manuscript.
Author information
Authors and Affiliations
Contributions
Acquisition and analysis of data: MB, JS, RT, BR. Interpretation of data: JS, MB, JNP, SAM, RT and BR. Conception and design: JS, MB, JNP, SAM, RT and BR. Drafting the article or revising the article: JS, MB, JNP, SAM, RT, BR, CV, LB, AZ, KB and FMDLV. Final approval of the version to be published: All authors.
Corresponding authors
Ethics declarations
Competing interests
RT, BR, CV, HL, MA, FDV, KCB, JS, and MB are employees of Tempus AI. LCB is an employee of Nestle Health Science, receives consulting fees from Tempus AI, Sherlock Bioscience, and Headlamp Health, and performs unpaid consulting for Sequence2Script. MA is a contracted physician with Amen Clinics Inc.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Patel, J.N., Morris, S.A., Torres, R. et al. Pharmacogenomic insights in psychiatric care: uncovering novel actionability, allele-specific CYP2D6 copy number variation, and phenoconversion in 15,000 patients. Mol Psychiatry (2024). https://doi.org/10.1038/s41380-024-02588-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41380-024-02588-4
- Springer Nature Limited