Abstract
β-amyloid (Aβ) pathology is not always coupled with Alzheimer’s disease (AD) relevant cognitive decline. We assessed the accuracy of tau PET to identify Aβ(+) individuals who show prospective disease progression. 396 cognitively unimpaired and impaired individuals with baseline Aβ and tau PET and a follow-up of ≥ 2 years were selected from the Alzheimer’s Disease Neuroimaging Initiative dataset. The participants were dichotomously grouped based on either clinical conversion (i.e., change of diagnosis) or cognitive deterioration (fast (FDs) vs. slow decliners (SDs)) using data-driven clustering of the individual annual rates of cognitive decline. To assess cognitive decline in individuals with isolated Aβ(+) or absence of both Aβ and tau (T) pathologies, we investigated the prevalence of non-AD comorbidities and FDG PET hypometabolism patterns suggestive of AD. Baseline tau PET uptake was higher in Aβ(+)FDs than in Aβ(-)FD/SDs and Aβ(+)SDs, independently of baseline cognitive status. Baseline tau PET uptake identified MCI Aβ(+) Converters and Aβ(+)FDs with an area under the curve of 0.85 and 0.87 (composite temporal region of interest) respectively, and was linearly related to the annual rate of cognitive decline in Aβ(+) individuals. The T(+) individuals constituted largely a subgroup of those being Aβ(+) and those clustered as FDs. The most common biomarker profiles in FDs (n = 70) were Aβ(+)T(+) (n = 34, 49%) and Aβ(+)T(-) (n = 19, 27%). Baseline Aβ load was higher in Aβ(+)T(+)FDs (M = 83.03 ± 31.42CL) than in Aβ(+)T(-)FDs (M = 63.67 ± 26.75CL) (p-value = 0.038). Depression diagnosis was more prevalent in Aβ(+)T(-)FDs compared to Aβ(+)T(+)FDs (47% vs. 15%, p-value = 0.021), as were FDG PET hypometabolism pattern not suggestive of AD (86% vs. 50%, p-value = 0.039). Our findings suggest that high tau PET uptake is coupled with both Aβ pathology and accelerated cognitive decline. In cases of isolated Aβ(+), cognitive decline may be associated with changes within the AD spectrum in a multi-morbidity context, i.e., mixed AD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
β-amyloid (Aβ) positron emission tomography (PET) can accurately detect Αβ plaques in vivo [1] and has improved diagnostic confidence, refining Alzheimer’s disease (AD) patient management [2, 3]. However, the clinical utility of Αβ PET is mainly defined by its high negative predictive value (80–100%) [4, 5] i.e., a negative result can rule out AD and is significantly more meaningful than a positive one in clinical decision-making [6]. The presence of Αβ pathology is a common finding in the elderly, and it is not deterministic for prospective cognitive deterioration [7,8,9]. The relatively low positive predictive value of Aβ biomarkers [4, 10], in combination with the presence of Aβ pathology in other neurodegenerative disorders [11,12,13], challenges the interpretation of the results of ongoing clinical trials, which have focused on the recruitment of individuals in the AD spectrum based solely on Aβ positivity (Αβ(+)), even in the absence of cognitive symptoms. There is thus a warranted need for integrating novel biomarkers with higher prognostic accuracy into clinical practice for more accurate identification of clinically relevant AD pathology.
Earlier in vivo [14, 15] and autopsy studies [16] have shown a strong relationship of tau, rather than Aβ, pathology with AD neurodegeneration and cognitive performance. Further PET imaging studies have highlighted a temporal offset in this correlation, with tau deposition preceding local neuronal loss [8, 15] and being predictive of future cognitive decline [17,18,19]. In line with this temporal sequence, there is compelling evidence that T(+) individuals could be largely a subgroup of those being Aβ(+) [20]. The interplay between Aβ and tau pathology, as imaged with PET, has also been assessed [21,22,23], and the concurrent presence of both pathologies has been associated with a higher risk for fast decline relative to the presence of only Aβ [17, 20]. Nonetheless, the widespread adoption of the full characterization of an individual based on both Aβ and tau PET biomarkers appears an unrealistic clinical policy, given the associated costs and the required healthcare resources.
Despite highlighting the association between tau load and prospective cognitive decline [15, 17, 24], studies employing longitudinal cognition as a continuous variable do not allow assessment of the prognostic accuracy of the biomarker and, therefore, its ability to predict a cognitive trajectory at the individual level. Furthermore, both the use of group-level association analyses and the small sample sizes [15, 18, 25] with clinically relevant follow-up intervals do not allow elaborate assessment of the presence of other factors that could affect cognitive deterioration at an individual basis and explain concordant and discordant results between Aβ and tau biomarkers. Personalized interpretation of a biomarker result holds important clinical implications. Addressing this inquiry constitutes a crucial, yet pending, step for the establishment of tau biomarkers. To further expand the available evidence on the prognostic accuracy of tau biomarkers at an individual level, one could take advantage of the bimodal distribution of cognitive trajectories observed in both aging and clinical studies, and evaluate the accuracy of tau biomarkers to discriminate individuals declining from those remaining stable [26,27,28].
We aimed to assess the clinical utility of tau PET imaging as a standalone predictor of AD-relevant cognitive decline by testing its ability to detect the subgroup of Aβ(+) individuals who experience prospective disease progression in Alzheimer’s Disease Neuroimaging Initiative (ADNI) participants. Our study encompasses two distinct objectives: 1) clustering the individuals based on disease progression considering both change in clinical diagnosis and the rate of cognitive decline, and evaluating the accuracy of baseline tau PET for discriminating individuals with an accelerated profile of prospective cognitive decline; and 2) understanding the determinants of cognitive decline in individuals with discordant Aβ and tau biomarker status (i.e., isolated Aβ(+)) by investigating the prevalence of non-AD comorbidities and 18F-fluorodeoxyglucose (FDG) PET hypometabolism patterns suggestive of AD. We hypothesized that if tau PET is positive only in Aβ(+) individuals with AD-relevant cognitive decline, then in cases of isolated Aβ(+), cognitive decline could be associated with changes within the AD spectrum (i.e., the presence of Aβ pathology) in a mixed pathology context. The alternative hypothesis posits that if isolated Aβ(+) is solely associated with AD-relevant cognitive decline, then tau biomarkers may lack the necessary sensitivity, and would therefore have limited clinical utility.
Methods
Individuals
The data used for our analysis were obtained from the ADNI repository (https://adni.loni.usc.edu) on 21 January 2022 (Supplementary Table 1). ADNI is a multicentered study launched in 2003 and run as a public-private partnership led by Principal Investigator Michael W. Weiner. The primary aim of ADNI is to test whether imaging techniques, biological markers and clinical and neuropsychological assessment can be combined to measure the progression of mild cognitive impairment (MCI) and early AD.
We identified all participants from the latest phase of ADNI (ADNI3) who had undergone at least one tau and one Aβ PET scan within six months and had available longitudinal clinical and cognitive follow-up over a minimum of two years (Fig. 1, Table 1). Based on their clinical diagnosis at the time of the baseline tau PET scan (i.e., a priori baseline time point), the individuals were grouped into cognitively unimpaired (CU) or impaired (CI) (i.e., individuals diagnosed with MCI or dementia).
Both clinical conversion and progress in cognitive decline were studied (* number of individuals before the exclusion of three outliers/influential points). ADAS-Cog13 13-item version of the Alzheimer’s Disease Assessment Scale-Cognitive Subscale; ADNI Alzheimer’s Disease Neuroimaging Initiative, CU cognitively unimpaired, MCI mild cognitive impairment, PET positron emission tomography.
ADNI3 has been conducted in full conformity with Good Clinical Practice guidelines and Regulations for the Protection of Human Subjects of Research. The ADNI3 protocol complies with the International Conference on Harmonization, Health Insurance Portability and Accountability Act, and State and Federal regulations, and was approved by local Institutional Review Boards (IRB). Individuals provided written consent to participate with IRB-approved informed consent forms. A complete listing of ADNI investigators and participating sites can be found at the end of the article.
PET imaging biomarkers
Aβ PET (18F-florbetapir or 18F-florbetaben) scans were rated as either Aβ(+) (summary standardized uptake value ratio (SUVR) ≥ 1.11 [29, 30] or 1.08 [31], respectively) or negative (Aβ(-)), based on the uptake of tracer in a cortical summary region of interest (ROI) with previously validated tracer-specific cut-offs, relatively to the uptake in the whole cerebellum (reference region). The Aβ load measured in centiloids (CL) was also assessed [32, 33].
For tau PET, the uptake of 18F-flortaucipir (aka Tauvid, AV-1451, T807) was quantified using SUVR relative to the uptake in the inferior cerebellar grey matter for all cortical ROIs. 18F-flortaucipir is a reliable biomarker for advanced tau pathology (Braak stages V-VI) [34, 35]. To summarise the tracer uptake, we used a standard composite temporal ROI (temporal meta-ROI) (Fig. 2A) [36, 37]. Tau PET positivity (T(+)) was tested in a pilot manner with a previously suggested threshold (1.34 SUVR in the temporal meta-ROI) [38], derived from the largest independent cohort to date. A gray zone of 5% was used to compensate for the absence of postmortem validation for the definition of T(+). To assess the applicability of the published threshold in our cohort, we followed the previously reported methodology [38, 39]. A very similar cut-off value was calculated (Supplement; Methods, Supplementary Fig. 1). The ADNI pipeline was used for preprocessing the Aβ and tau PET imaging data [17]. The results after applying the correction for partial volume effects (PVC) are presented in the Supplement as detailed below.
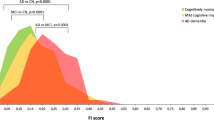
A Auxiliary legend for the rest of the analysis. The composite temporal region of interest illustrates the regions that make up the temporal meta-ROI according to the ADNI3 protocol (bilateral amygdala, entorhinal, fusiform, inferior, and middle temporal cortices). B The LME outcome for the definition of the annual rate of cognitive decline. The slope of each line represents the annual rate of cognitive decline for each individual. Longitudinal data (≥2 years after the baseline examination) for the ADAS-Cog13 were available for 338 out of the 396 individuals, but three individuals were excluded as outliers/influential points. Therefore, our analysis pipeline was completed for 335 individuals. C The GMM outcome for clustering the individuals as SDs or FDs. The distribution of the annual rates of cognitive decline can be explained by two normal distributions (blue: meanb = 0.298, StDb = 0.378; purple: meanp = 1.669, StDp = 1.005). Individuals with an annual rate of cognitive decline ≥ meanb + (2 × StDb) ≈1.05 were clustered as FDs. D, E Spaghetti plots representing all the ADAS-Cog13 scores for each individual before and after clustering respectively. F Similar to B, but after clustering. ADAS-Cog13 13-item version of the Alzheimer’s Disease Assessment Scale-Cognitive Subscale, ADNI Alzheimer’s Disease Neuroimaging Initiative, CI cognitively impaired, CU cognitively unimpaired, FD fast decliner, SD slow decliner, GMM Gaussian mixture model, LME linear mixed-effects model, ROI region of interest, StD standard deviation.
FDG PET scans were extracted from ADNI and were visually interpreted in cases of accelerated cognitive decline, by two independent nuclear medicine specialists blinded to the individual Aβ and tau biomarker status. The assessment of the FDG PET scans was assisted by the Syngo.via (Siemens Healthcare), an FDA-approved software platform [40]. The scans were dichotomously categorized as either suggestive of AD or not suggestive of AD (i.e., showing no specific neurodegeneration pattern or a pattern suggestive of another neurodegenerative disorder).
Cognitive measures
The Mini Mental State Examination (MMSE) was only used to characterize the global cognition of individuals at baseline. The 13-item version of the Alzheimer’s Disease Assessment Scale-Cognitive Subscale (ADAS-Cog13) and the Preclinical Alzheimer Cognitive Composite (PACC) score were used as measures of global cognition over the multiple time points of the follow-up interval [41, 42]. Cognitive impairment in episodic memory was measured using the ADNI episodic composite memory score (ADNI MEM) [43].
Comorbidities
Information regarding the medical history at study enrollment (i.e., cerebrovascular disease risk factors, psychiatric or neurological comorbidities) [44, 45], and the use of medications at every visit, has been recorded at the ADNI depository and was manually assessed by two independent medically trained investigators (KI, KC) (Supplementary Table 1). The vascular risk factors (VRF) burden (Table 2) was defined as previously detailed [46].
Statistical analysis
The heterogeneity of cognitive impairment trajectories was assessed over the follow-up interval in terms of both clinical conversion (i.e., change of diagnosis) and annual rate of cognitive decline (fast (FDs) vs. slow decliners (SDs)) (Fig. 1). The level of statistical significance was set at α = 0.05. Supplementary Table 2 summarizes the rationale of our analysis.
Progress in diagnosis
All CU and MCI individuals were divided into two groups according to their baseline and last follow-up diagnoses. The individuals who retained their initial diagnosis (i.e., CU to CU, MCI to MCI) were classified as Non-Converters, while those progressing in clinical severity were classified as Converters (i.e., CU to MCI, CU/MCI to dementia). Individuals with a dementia diagnosis at baseline were excluded from this analysis. The two groups were compared in terms of baseline tau PET uptake descriptively. The prognostic accuracy of both baseline Aβ and tau PET uptake in predicting clinical conversion was evaluated using receiver operating characteristic (ROC) analysis. Baseline Aβ and tau PET were also independently assessed in terms of sensitivity (Se), specificity (Sp), positive predictive value (PPV), and negative predictive value (NPV).
Progress in cognitive decline
Longitudinal cognitive performance was modelled to assess individuals’ annual rate of cognitive decline using separate linear mixed-effects (LME) models for each neuropsychological test. Akaike information criterion (AIC) was used for model selection. The time from baseline was set as a fixed and random effect to allow for the heterogeneity in cognitive trajectories across individuals. A random intercept was included to capture differences in baseline cognitive performance across individuals. Age at baseline and years of education were added as covariates to the models. The contribution of sex was not significant and did not contribute substantially to the model. Using influence plots and measures of Cook’s distance, we identified and excluded outliers and influential points as documented in the respective figure legends [47, 48].
Gaussian mixture models (GMM) were used for identifying, in a probabilistic manner, the number of underlying normal distributions that best explained the distribution of annual rates of cognitive decline for each neuropsychological test; these were extracted from the LME models of the previous step. In all neuropsychological tests, the annual rate of cognitive decline was best modelled by two normal distributions. The mean and the standard deviation (StD) of the distribution with the lower annual rates of cognitive decline were used to define a threshold (∣mean + (2 × StD)∣). Individuals with an annual rate of cognitive decline greater than or equal to the threshold value were clustered as FDs, while the others were clustered as SDs (Fig. 2). The tau PET uptake was descriptively compared across these two groups. The prognostic accuracy of both baseline Aβ and tau PET uptake in predicting fast cognitive decline (FDs) was evaluated using ROC analysis. Se, Sp, PPV, and NPV of both baseline Aβ and tau PET were also independently assessed.
Baseline tau PET uptake and rate of cognitive decline
We assessed the association between baseline tau PET uptake and the annual rate of cognitive decline with linear modelling. AIC was used for model selection. The temporal meta-ROI SUVR, the Aβ PET status (Aβ(-/+)), the baseline cognitive status (CU/CI), and the interaction between temporal meta-ROI SUVR and Aβ PET status were set as predictors of the annual rate of cognitive decline. The estimated marginal means of the linear model were used to perform post hoc comparisons on the interaction term. The existence of outliers and influential points was tested for, as detailed above. The risk ratio (RR) for being Aβ(+)FD in relation to the tau PET status (T(+) vs. T(-)) was evaluated.
Comorbidities and FDG PET hypometabolism patterns
The prevalence of non-AD comorbidities and FDG PET hypometabolism patterns in cases of accelerated cognitive decline was evaluated and compared with Fisher’s test (Aβ(+)T(–)FDs vs. Aβ(+)T(+)FDs), both including and excluding (Supplementary) the individuals located in the gray zones defined for T(–/+) and SD/FD.
Software
R version 4.1.1 was used for statistical analysis (Supplementary Table 1).
Results
We identified 396 individuals from the ADNI dataset with baseline Aβ and tau PET scans who had completed a ≥ 2-year follow-up (Table 1).
Progress in diagnosis
When analyzed separately, the accuracy (area under the curve; AUC) of baseline Aβ and tau PET uptake for predicting clinical conversion was AUC = 0.74 and AUC = 0.72, respectively (Supplementary Fig. 2A). Aβ PET showed higher Se = 0.72 and NPV = 0.94, compared to tau PET but the latter showed higher Sp = 0.92 and PPV = 0.44 (Supplementary Table 3).
MCI Aβ(+) Converters (n = 18, 39%, Table 1) were characterized by higher baseline tau PET uptake than the other groups (Fig. 3). The accuracy of tau PET uptake in predicting MCI Αβ(+) Converters was AUC = 0.85 in the temporal meta-ROI. The entorhinal and the parahippocampal cortices showed the highest AUC value (AUC = 0.89) (Fig. 3D, Supplementary Fig. 3A).
A, B Baseline tau PET uptake with respect to clinical and biomarker diagnoses, respectively. C Baseline tau PET uptake in relation to the follow-up status per diagnostic group. D The results of a ROC analysis illustrated in a brain atlas for the discrimination of MCI Aβ(+) Converters among all MCI individuals. Aβ β-amyloid, AUC area under the curve, CInt confidence interval, CU cognitively unimpaired, MCI mild cognitive impairment, PET positron emission tomography, ROC receiver operating characteristic, ROI region of interest; SUVR standardized uptake value ratio.
The accuracy of baseline tau PET uptake in predicting clinical conversion in the CU group was not evaluated separately, given that the number of CU individuals who converted to MCI or dementia (n = 9, 6% in Aβ(-) and n = 10, 14% in Aβ(+) individuals, Table 1) was not large enough to draw reliable conclusions.
Progress in cognitive decline
An annual rate of cognitive decline of 1.05 units in the ADAS-Cog13 score was set as the threshold for defining FDs (Fig. 2C). When analyzed separately, the accuracy of baseline Aβ and tau PET uptake for predicting FDs was AUC = 0.74 and AUC = 0.78, respectively (Supplementary Fig. 2B). The Se = 0.76 and NPV = 0.91 of Aβ PET were higher compared to tau PET, even though the NPV = 0.87 of tau PET was similarly high. The latter also showed higher Sp = 0.94 and PPV = 0.69 (Supplementary Table 3).
Baseline tau PET uptake was higher in Aβ(+)FDs, either CU or CI, than in Aβ(-)FD/SDs and Aβ(+)SDs in the temporal meta-ROI (Fig. 4A–B). The accuracy of tau PET uptake in predicting Aβ(+)FDs was AUC = 0.86 in the CI group separately, and AUC = 0.87 considering all individuals (Fig. 4C, D, Supplementary Fig. 3B–C) (AUC = 0.90 in the PVC data, Supplementary Fig. 4). The corresponding AUC values, for both these scenarios, for the cortical ROIs composing the temporal meta-ROI varied between 0.81 and 0.89, when analyzed separately, whereas cortical ROIs beyond them (e.g. inferior parietal cortex), showed lower AUC (Fig. 4C, D, Supplementary Fig. 5). Baseline tau PET uptake was differentially linearly related to the annual rate of cognitive decline in Aβ(+) and Aβ(-) individuals (interaction t = 4.275, p < 0.001); the association was statistically significant in Aβ(+) individuals (95% confidence interval 2.07–3.09), but not in Aβ(-) individuals (95% confidence interval -1.19–1.04) (Fig. 4E). The results for the PACC score and ADNI MEM are reported in Supplementary Fig.s 4, 6.
A Baseline tau PET uptake with respect to SD/FD profiles in both CU and CI individuals. B Average baseline tau PET uptake per group according to Aβ(-/+) and SD/FD profiles. C, D The results of a ROC analysis illustrated in brain atlases for the discrimination of Aβ(+)FDs among CI and CU + CI individuals, respectively. E Association (linear modelling) between the baseline tau PET uptake and the annual rate of cognitive decline including information about both Aβ(-/+) and SD/FD. FD was defined as ADAS-Cog13 annual rate of cognitive decline ≥ 1.05; the red/green shaded areas depict FD/SD; the gray zone for the ADAS-Cog13 annual rate of cognitive decline was obtained from meanb + [(1.65 – 2.35) × StDb] ≈ (0.92–1.19) (Fig. 2C). T(+) was defined as tau PET SUVR ≥ 1.34 in the temporal meta-ROI; the gray zone for tau PET was obtained from 1.34 ± (2.5% × 1.34) ≈ (1.31–1.37). No outliers/influential points were found. F Venn diagrams to illustrate the overlap of Aβ(+), T(+), and FDs in both CU and CI individuals. The size of each group is depicted proportional to the number of individuals it comprises. Aβ β-amyloid, ADAS-Cog13 13-item version of the Alzheimer’s Disease Assessment Scale-Cognitive Subscale, AUC area under the curve, CInt confidence interval, CI cognitively impaired, CU cognitively unimpaired, FD fast decliner, SD slow decliner, PET positron emission tomography, ROC receiver operating characteristic, ROI region of interest, SUVR standardized uptake value ratio, T tau.
Overlap of Aβ(+), T(+) and fast cognitive decline
T(+) individuals had 10 times the risk of being Aβ(+)FDs compared to T(-) individuals (RR = 10.4, p < 0.001, 95% confidence interval 6.5–16.8). Based on the group intersections, T(+) individuals constituted largely a subgroup of Aβ(+)FDs (Aβ(+)T(+)FDs). The overlap between Aβ(+), T(+) and FDs was more prominent in CI individuals. Most FDs (n = 70) were Aβ(+)T(+) (n = 34, 49%) or, less commonly, Aβ(+)T(-) (n = 19, 27%). No Aβ(-)T(+)FDs were identified. Only three CU individuals and one CI individual showed isolated tau positivity and were SDs (Aβ(-)T(+)SDs) (Fig. 4E, F).
Aβ(+)T(-)FDs vs. Aβ(+)T(+)FDs
Clinical characteristics and comorbidities
No statistically significant differences were observed between Aβ(+)T(-)FDs and Aβ(+)T(+)FDs with respect to demographics and the prevalence of APOE4 allele (Table 2, Supplementary Table 4, Supplementary Fig. 7). Baseline ADAS-Cog13 was higher in Aβ(+)T(+)FDs (M = 22.75, StD = 10.09) than in Aβ(+)T(-)FDs (M = 17.17, StD = 8.69) (p-value = 0.044), but not the annual rate of decline in the same test (p-value = 0.4). A higher baseline Aβ PET load was also detected in Aβ(+)T(+)FDs (M = 83.03CL, StD = 31.42) compared to Aβ(+)T(-)FDs (M = 63.67CL, StD = 26.75) (p-value = 0.038). The prevalence of cerebrovascular disease risk factors and psychiatric comorbidities was higher in Aβ(+)T(-)FDs than in Aβ(+)T(+)FDs, although only the prevalence of depression diagnosis reached statistical significance (47% vs. 15%, p-value = 0.021) (Table 2, Supplementary Fig. 8). The results for separate analysis of CI individuals are shown in Supplementary Fig. 9.
FDG PET hypometabolism pattern
Out of 53 Aβ(+)FDs, 38 had available baseline FDG PET scans for visual assessment. The hypometabolism pattern was different between Aβ(+)T(-)FDs and Aβ(+)T(+)FDs (p-value = 0.039). Most Aβ(+)T(-)FDs showed a hypometabolism pattern not suggestive of AD (n = 12, 86% vs. n = 2, 14%), whereas 50% of Aβ(+)T(+)FDs (n = 12) showed a hypometabolism pattern suggestive of AD (Table 2). Out of 12 (86%) Aβ(+)T(-)FDs who showed a hypometabolism pattern not suggestive of AD, 5 individuals (36% of Aβ(+)T(-)FDs) showed no specific neurodegeneration pattern in FDG PET, and 7 individuals (50% of Aβ(+)T(-)FDs) showed a pattern suggestive of another neurodegenerative disorder (Fig. 5).
A representative FDG PET scan from each category of hypometabolism pattern that we identified in this group is presented. The dashed red line encloses regions with hypometabolism. A Hypometabolism pattern not suggestive of AD (A1 + A2, n = 12 (86%)). B Hypometabolism pattern suggestive of AD (n = 2 (14%)). The analysis of the FDG PET images was made in an FDA-approved software platform i.e., Syngo.via (Siemens Healthcare) (Wilson, Selwyn, and Elojeimy 2022); 3D analysis in stereotactic surface projection. The Z-scores scale is based on the Syngo.via database that consists of healthy volunteers aged 46 to 79 years old and the whole brain has been used for intensity normalization [(statistic = (Valuepatient – Meanpopulation)/Std.Devpopulation]. The resulting images were visually assessed by two independent nuclear medicine specialists. AD Alzheimer’s disease, Aβ β-amyloid, Aβ(+) Aβ positivity, FDA food and drug administration, FDG 18F-fluorodeoxyglucose, ND neurodegenerative disorder, PET positron emission tomography, T(-) tau negativity.
Aβ(-)T(-)FDs
Aβ(-)T(-)FDs showed high prevalence of non-AD comorbidities (i.e., depression diagnosis; n = 5, 29%). Most Aβ(-)T(-)FDs (n = 9, 69%) also exhibited a hypometabolism pattern not suggestive of AD (Supplementary Table 5).
Follow-up tau PET scans in Aβ(+)T(-)FDs and Aβ(-)T(-)FDs
Nine out of 19 Aβ(+)T(-)FDs and six out of 17 Aβ(-)T(-)FDs had available follow-up tau PET scans. All individuals remained T(-) (Supplementary Table 6).
Discussion
Baseline tau PET uptake determined with high accuracy (AUC = 0.85–0.87) the subset of Aβ(+) individuals who has experienced prospective disease progression in terms of conversion of baseline diagnosis or accelerated cognitive decline. Our findings confirm the results of previous studies [19, 20] and provide further support for the ideas that: 1.) the buildup of Aβ pathology is much more prevalent among even CU elderly than that of extensive tau pathology detected with tau PET (Braak stages V-VI), which explains the suboptimal accuracy of Aβ biomarkers to predict deterioration [7,8,9, 34, 49, 50], 2.) T(+) individuals constitute largely a subset of those being Aβ(+) in AD cohorts [20], 3.) the presence of tau exceeding Braak IV – above the PET detection limit – greatly increases the risk for AD-relevant cognitive decline [15, 17, 18, 51]. We further present novel findings indicating that fast cognitive decline in individuals with isolated Aβ positivity is associated with a hypometabolism pattern not suggestive of AD and a high prevalence of depression diagnosis. This implies that in cases of isolated Aβ positivity, cognitive decline may be associated with changes within the AD spectrum in a multi-morbidity context (mixed AD) [52,53,54].
Interestingly, our study highlighted the presence of cases of Aβ(+) individuals with fast cognitive decline but a negative tau PET scan. The assessment of cognitive decline when accompanied by Aβ and tau discordance, or alternatively, of the individuals that may be overlooked if prioritizing tau over Aβ biomarkers, is a pivotal step before the clinical establishment of tau biomarkers. The interpretation of isolated Aβ positivity is quite challenging and two scenarios might explain the discordance (Aβ(+)T(-)) in the context of prospective deterioration. These individuals would either still have sufficient tau pathology to qualify for AD but we cannot detect it because of the limited sensitivity of tau PET to detect early tau pathology (i.e., false negative cases that could represent AD), or other pathologies could have been present contributing to cognitive decline by acting synergistically or additively to Aβ pathology [11, 46, 55, 56]. The first scenario cannot be excluded given the limited available postmortem data for individuals with antemortem tau PET data. The first scenario aligns with the lower baseline ADAS-Cog13 we observed in individuals exhibiting fast cognitive decline and isolated Aβ positivity (Aβ(+)T(-)FDs) compared to individuals presenting with combined evidence of Aβ and tau pathologies (Aβ(+)T(+)FDs) (Table 2). This concept implies that the former may be on the AD pathway but at an earlier stage [57]. On the other hand, the second scenario would be consistent with 1.) the high prevalence of mixed pathologies observed in autopsy studies [58, 59], where the total burden of pathology could be the determinant for cognitive decline [53, 54], and 2.) the finding that Aβ pathology has a high prevalence even in cases where a non-AD diagnosis is most likely [11, 12]. Indeed, Aβ(+)T(-)FDs in our study showed a significantly higher prevalence of depression, significantly lower average levels of Aβ pathology, and a higher prevalence of a hypometabolism pattern not suggestive of AD compared to Aβ(+)T(+)FDs (Table 2). The latter aligns with the scenario of multimorbidity in the Aβ(+)T(-)FDs and highlights the heterogeneity among Aβ(+) individuals [57, 60, 61], which reinforces the argument that cognitive decline associated with isolated Aβ positivity should be cautiously interpreted.
Taken together, our data support the hypothesis that tau positivity allows discrimination of individuals with AD-relevant cognitive decline and suggest that the consideration of incorporating tau PET in tertiary memory clinics could be advantageous since it offers both diagnostic information (45/49 (92%) of T(+) individuals were Αβ(+)) and prognostic insight (since T(+) individuals followed a fast trajectory of cognitive decline). Nevertheless, our findings cannot provide definite evidence for or against the hypothesis that when biomarker status is discordant, the underlying condition driving decline is not AD-related. The complex coincident nature of AD and non-AD comorbidities [45, 46, 62, 63] underlines the need for further research in individuals with discordant biomarker status before one suggests the prioritization of tau over Aβ biomarkers, as a standalone biomarker strategy. It is important to consider that the clinical applicability of a biomarker depends on its characteristics and different properties are required based on its desired clinical utility [64, 65].
The novelty of our study arises from the effort to understand the biomarkers discordance in the setting of multimorbidity and from the methodological approach we followed for determining clusters of individuals based on their prospective cognitive performance. The role of mixed pathologies in cognitive decline is common knowledge [52,53,54, 60, 61]. However, this is one of the few studies that took into consideration both the prevalence of non-AD comorbidities and the FDG PET hypometabolism pattern in the context of interpreting isolated Aβ positivity and establishing the clinical applicability of tau biomarkers. Our study provides proof-of-concept evidence that in the case of Aβ and tau discordance (Aβ(+)T(-)), cognitive decline could be associated with changes within the AD spectrum in a multi-morbidity context, i.e., mixed AD, while in the case of Aβ and tau positivity concordance (Aβ(+)T(+)), AD pathology is the main contributor to cognitive decline. This could facilitate the development of individualized medicine and offer novel insights into: 1) the role of comorbidities when interpreting discordant AD biomarkers and the outcomes of clinical trials; and 2) the potential of a standalone tau biomarker strategy in clinical routine. We are not aware of other previous studies testing this hypothesis.
In contrast to prior research efforts which focused solely on clinical conversion to define disease progression, i.e., change of diagnosis over time, or employed cognition as a continuous measure, we clustered the individuals based on their longitudinal cognitive performance. Although machine learning techniques and multiple cognitive scores have also been previously used to define clusters of decliners, these approaches possess inherent weaknesses and lack clinical interpretation [27, 66, 67]. To overcome these limitations, we used longitudinal modelling for assessing the annual rate of cognitive decline and a data-driven approach for clustering individuals in an unbiased manner as FDs or SDs [68]. This methodology has substantial advantages over the aforementioned approaches and provides more powerful data for detecting clinically relevant cognitive decline. A diagnosis of clinical conversion can depend on both the operator (i.e., different physicians) and the information provided by the individual’s study partner [69,70,71]. Additionally, the investigation of clinical conversion cannot assess progression in patients with dementia at baseline since they cannot progress more in terms of diagnosis. Our modelling approach for longitudinal cognitive trajectories also allows adjustment for relevant covariates and is more powerful in shorter follow-up intervals. Furthermore, the clustering of individuals into SDs and FDs rather than using cognition as a continuous variable [17] allowed us to assess the prognostic accuracy of the biomarker and, therefore, its clinical applicability to the individual level. While it is difficult to determine whether our clustering approach is optimal for defining individuals with clinically relevant cognitive decline – this construct could be controversial – similar data-driven approaches have been used previously in clinical trials [72] and they are powerful in detecting a minimal clinically important difference in longitudinal data [68]. We are confident that our findings hold since a.) the follow-up interval we employed aligns with that used in other recent pertinent studies [19, 20] and clinical trials [73] and has previously been suggested as optimal for evaluating the prognostic accuracy of AD biomarkers [74], and b.) the threshold we evaluated for defining fast cognitive decline is consistent with the existing literature [75].
The study also yielded unanticipated results. Firstly, the areas where tau PET uptake was most accurate in predicting disease progression were restricted to within the medial temporal lobe (i.e., entorhinal cortex) (Fig. 4C, D, Supplementary Fig. 5). Evidence from autopsy studies has suggested that isolated tau accumulation in the medial temporal lobe is a common finding in CU elderly [50] and is not associated with a neuropathological AD diagnosis even in the presence of Aβ pathology [76]. Historically, only the spread of tau pathology into more widespread brain areas has been associated with cognitive decline [51]. This contradiction between our in vivo and earlier pathological evidence could be explained by the facts that 1) 18F-flortaucipir detects only advanced tau pathology (i.e., Braak stages V-VI), while at autopsy the whole spectrum, burden, topography, and packing density of tau pathology are revealed and assessed; and 2) the burden of tau pathology in the entorhinal cortex, and therefore the tau PET tracer uptake, increases from Braak stage I to VI [34]. Secondly, regarding the clustering into SDs and FDs, while some argue that the ADAS-Cog lacks sensitivity in detecting early cognitive decline [77], we found that it yielded similar results to those based on the PACC score, and the ADNI MEM [41, 42] with respect to the evaluated prognostic accuracy of tau PET (Supplementary Fig.s 4, 6). Thirdly, cases of Aβ and tau positivity accompanied by slow cognitive decline (Aβ(+)T(+)SDs) were also observed (n = 11, 3.28%), representing individuals probably earlier in the disease course or those with high cognitive resilience (Fig. 4F, Supplementary Table 7).
The extrapolation of our findings is subject to certain limitations with respect to a.) the characteristics of ADNI participants, b.) the follow-up interval, c.) our methodological approach regarding the longitudinal modeling of cognitive decline and the clustering into groups of decliners, and d.) the interpretation of PET imaging data. ADNI has been designed as an AD cohort and individuals with clear evidence of other major comorbidities have been excluded, limiting the interpretation of our findings to this cohort. Although we consider the sample size adequate for the analysis when grouping CU and CI individuals together, it does not guarantee a high level of confidence in analyses within specific subgroups. More specifically, the power could be limited in CU individuals since the annual conversion rate in this group was low, consistent with previously reported rates (5–10%) [78,79,80], and the percentage of FDs was only 6% (14/217). This precludes any certain conclusions about the utility of the biomarker in CU highlighting the power issues that emerge when studying this population. Similarly, the small number of Aβ(+)T(-)FDs limits the confidence of our findings concerning the role of non-AD comorbidities and the prevalence of FDG PET hypometabolism patterns when cognitive decline is associated with isolated Aβ positivity. The follow-up interval was limited to an average of 33.7 months (in the case of the ADAS-Cog13, Table 1). Although clinically relevant cognitive decline is generally detected within this interval, the wide range of individual-level follow-up intervals (24–74.7 months) may also have biased the modeling of cognitive decline, especially in individuals with shorter intervals. Earlier studies have also shown that cognitive decline follows a non-linear trajectory [28, 81], and especially individuals at earlier stages of cognitive decline might need longer follow-up intervals to reach the turning point into accelerated cognitive decline [82,83,84]. However, given the limited follow-up interval and time-points, we restricted our analysis to linear models, which could have led to an underestimation of the annual rate of decline, especially in CI individuals. We should also keep in mind that while beneficial with respect to clinical applicability, clustering individuals solely based on cognitive performance may introduce some degree of generalization and overlook important idiosyncratic characteristics. The limitations pertaining to the PET data concern a.) the limited sensitivity of 18F-flortaucipir for detecting early tau pathology (i.e., Braak stages I-IV) [34, 35], and b.) the dichotomous interpretation of Aβ and FDG PET scans, which might oversimplify the information that can be obtained from these biomarkers. Briefly, although quantitative Aβ and FDG PET show associations with cognitive decline [85,86,87,88,89], we selected a dichotomous approach to align more with the interpretation of biomarkers in a clinical setting [64, 90,91,92].
Further research in other cohorts, with longer follow-up intervals, and employing different tau PET tracers [93, 94] is needed to validate our results and explore differences among cognitive tests, especially in CU individuals. Future real-world clinical data, with available postmortem evaluation, could also help us investigate the pathological correlates of the underexplored and relatively rare isolated tau positivity (Aβ(-)T(+), 1.19% of our ADNI sample) and better understand the role of comorbidities in individuals with clinically relevant cognitive decline and discordant Aβ and tau status. Finally, the visual read of tau PET scans is also needed to assess both the prevalence and the significance of atypical patterns of tau propagation that might go undetected when using thresholds and composite ROIs.
Conclusions
Tau PET imaging showed high accuracy to predict the subset of Aβ(+) individuals that will show AD-relevant cognitive decline. We provided proof-of-concept evidence that, when accelerated cognitive decline is associated with isolated Aβ positivity, the Aβ load falls within the low-positive range, the hypometabolism pattern is often not suggestive of AD, and the prevalence of depression diagnosis is high. These factors collectively suggest that cognitive decline accompanied by isolated Aβ positivity may be associated with changes within the AD spectrum in a multi-morbidity context, i.e., mixed AD. This should be investigated further before prioritizing tau over Aβ biomarkers. Overall, tau PET can predict a population of high clinical interest and should be considered as a combined diagnostic and prognostic tool with both clinical and research applications for the management of cognitively impaired individuals.
Data availability
The datasets generated during and/or analysed during the current study are available in the ADNI repository, https://ida.loni.usc.edu/login.jsp?project=ADNI.
References
Kadir A, Marutle A, Gonzalez D, Schöll M, Almkvist O, Mousavi M, et al. Positron emission tomography imaging and clinical progression in relation to molecular pathology in the first Pittsburgh Compound B positron emission tomography patient with Alzheimer’s disease. Brain. 2011;134:301–17.
de Wilde A, van der Flier WM, Pelkmans W, Bouwman F, Verwer J, Groot C, et al. Association of Amyloid Positron Emission Tomography With Changes in Diagnosis and Patient Treatment in an Unselected Memory Clinic Cohort: The ABIDE Project. JAMA Neurology. 2018;75:1062–70.
Rabinovici GD, Gatsonis C, Apgar C, Chaudhary K, Gareen I, Hanna L, et al. Association of Amyloid Positron Emission Tomography With Subsequent Change in Clinical Management Among Medicare Beneficiaries With Mild Cognitive Impairment or Dementia. JAMA. 2019;321:1286–94.
Rowe CC, Bourgeat P, Ellis KA, Brown B, Lim YY, Mulligan R, et al. Predicting Alzheimer disease with β-amyloid imaging: results from the Australian imaging, biomarkers, and lifestyle study of ageing. Ann Neurol. 2013;74:905–13.
Sabri O, Sabbagh MN, Seibyl J, Barthel H, Akatsu H, Ouchi Y, et al. Florbetaben PET imaging to detect amyloid beta plaques in Alzheimer’s disease: Phase 3 study. Alzheimer’s & Dementia. 2015;11:964–74.
Fantoni ER, Chalkidou A, O’ Brien JT, Farrar G, Hammers A. A Systematic Review and Aggregated Analysis on the Impact of Amyloid PET Brain Imaging on the Diagnosis, Diagnostic Confidence, and Management of Patients being Evaluated for Alzheimer’s Disease. Journal of Alzheimer’s Disease. 2018;63:783–96.
Jansen WJ, Ossenkoppele R, Knol DL, Tijms BM, Scheltens P, Verhey FRJ, et al. Prevalence of Cerebral Amyloid Pathology in Persons Without Dementia: A Meta-analysis. JAMA. 2015;313:1924–38.
Chiotis K, Saint-Aubert L, Boccardi M, Gietl A, Picco A, Varrone A, et al. Clinical validity of increased cortical uptake of amyloid ligands on PET as a biomarker for Alzheimer’s disease in the context of a structured 5-phase development framework. Neurobiol Aging. 2017;52:214–27.
Roberts RO, Aakre JA, Kremers WK, Vassilaki M, Knopman DS, Mielke MM, et al. Prevalence and Outcomes of Amyloid Positivity Among Persons Without Dementia in a Longitudinal, Population-Based Setting. JAMA Neurology. 2018;75:970–9.
Hatashita S, Yamasaki H. Diagnosed Mild Cognitive Impairment Due to Alzheimer’s Disease with PET Biomarkers of Beta Amyloid and Neuronal Dysfunction. PLoS One. 2013;8:e66877.
Farid K, Carter SF, Rodriguez-Vieitez E, Almkvist O, Andersen P, Wall A, et al. Case Report of Complex Amyotrophic Lateral Sclerosis with Cognitive Impairment and Cortical Amyloid Deposition. J Alzheimers Dis. 2015;47:661–7.
Bergeron D, Gorno-Tempini ML, Rabinovici GD, Santos-Santos MA, Seeley W, Miller BL, et al. Prevalence of amyloid-β pathology in distinct variants of primary progressive aphasia. Ann Neurol. 2018;84:729–40.
Diaz-Galvan P, Przybelski SA, Lesnick TG, Schwarz CG, Senjem ML, Gunter JL, et al. β-Amyloid Load on PET Along the Continuum of Dementia With Lewy Bodies. Neurology. 2023;101:e178–e188.
Pontecorvo MJ, Devous MD, Navitsky M, Lu M, Salloway S, Schaerf FW, et al. Relationships between flortaucipir PET tau binding and amyloid burden, clinical diagnosis, age and cognition. Brain. 2017;140:748–63.
La Joie R, Visani AV, Baker SL, Brown JA, Bourakova V, Cha J, et al. Prospective longitudinal atrophy in Alzheimer’s disease correlates with the intensity and topography of baseline tau-PET. Sci Transl Med. 2020;12:eaau5732.
Arriagada PV, Growdon JH, Hedley-Whyte ET, Hyman BT. Neurofibrillary tangles but not senile plaques parallel duration and severity of Alzheimer’s disease. Neurology. 1992;42:631–9.
Bucci M, Chiotis K, Nordberg A, Alzheimer’s Disease Neuroimaging Initiative. Alzheimer’s disease profiled by fluid and imaging markers: tau PET best predicts cognitive decline. Mol Psychiatry. 2021;26:5888–98.
Chiotis K, Savitcheva I, Poulakis K, Saint-Aubert L, Wall A, Antoni G, et al. 18F]THK5317 imaging as a tool for predicting prospective cognitive decline in Alzheimer’s disease. Mol Psychiatry. 2021;26:5875–87.
Ossenkoppele R, Smith R, Mattsson-Carlgren N, Groot C, Leuzy A, Strandberg O, et al. Accuracy of Tau Positron Emission Tomography as a Prognostic Marker in Preclinical and Prodromal Alzheimer Disease: A Head-to-Head Comparison Against Amyloid Positron Emission Tomography and Magnetic Resonance Imaging. JAMA Neurol. 2021;78:961–71.
Ossenkoppele R, Pichet Binette A, Groot C, Smith R, Strandberg O, Palmqvist S, et al. Amyloid and tau PET-positive cognitively unimpaired individuals are at high risk for future cognitive decline. Nat Med. 2022;28:2381–7.
Hanseeuw BJ, Betensky RA, Jacobs HIL, Schultz AP, Sepulcre J, Becker JA, et al. Association of Amyloid and Tau With Cognition in Preclinical Alzheimer Disease: A Longitudinal Study. JAMA Neurology. 2019;76:915–24.
Pascoal TA, Mathotaarachchi S, Mohades S, Benedet AL, Chung C-O, Shin M, et al. Amyloid-β and hyperphosphorylated tau synergy drives metabolic decline in preclinical Alzheimer’s disease. Mol Psychiatry. 2017;22:306–11.
Wang L, Benzinger TL, Su Y, Christensen J, Friedrichsen K, Aldea P, et al. Evaluation of Tau Imaging in Staging Alzheimer Disease and Revealing Interactions Between β-Amyloid and Tauopathy. JAMA Neurol. 2016;73:1070–7.
Ossenkoppele R, Schonhaut DR, Schöll M, Lockhart SN, Ayakta N, Baker SL, et al. Tau PET patterns mirror clinical and neuroanatomical variability in Alzheimer’s disease. Brain. 2016;139:1551–67.
Colato E, Chiotis K, Ferreira D, Mazrina MS, Lemoine L, Mohanty R, et al. Assessment of Tau Pathology as Measured by 18F-THK5317 and 18F-Flortaucipir PET and Their Relation to Brain Atrophy and Cognition in Alzheimer’s Disease. JAD. 2021;84:103–17.
Soldan A, Pettigrew C, Cai Q, Wang J, Wang M-C, Moghekar A, et al. Cognitive reserve and long-term change in cognition in aging and preclinical Alzheimer’s disease. Neurobiol Aging. 2017;60:164–72.
Gamberger D, Lavrač N, Srivatsa S, Tanzi RE, Doraiswamy PM. Identification of clusters of rapid and slow decliners among subjects at risk for Alzheimer’s disease. Sci Rep. 2017;7:6763.
Cho SH, Woo S, Kim C, Kim HJ, Jang H, Kim BC, et al. Disease progression modelling from preclinical Alzheimer’s disease (AD) to AD dementia. Sci Rep. 2021;11:4168.
Landau SM, Mintun MA, Joshi AD, Koeppe RA, Petersen RC, Aisen PS, et al. Amyloid deposition, hypometabolism, and longitudinal cognitive decline. Ann Neurol. 2012;72:578–86.
Landau SM, Lu M, Joshi AD, Pontecorvo M, Mintun MA, Trojanowski JQ, et al. Comparing positron emission tomography imaging and cerebrospinal fluid measurements of β-amyloid. Ann Neurol. 2013;74:826–36.
Royse SK, Minhas DS, Lopresti BJ, Murphy A, Ward T, Koeppe RA, et al. Validation of amyloid PET positivity thresholds in centiloids: a multisite PET study approach. Alzheimer’s. Res Ther. 2021;13:99.
Navitsky M, Joshi AD, Kennedy I, Klunk WE, Rowe CC, Wong DF, et al. Standardization of amyloid quantitation with florbetapir standardized uptake value ratios to the Centiloid scale. Alzheimers Dement. 2018;14:1565–71.
Rowe CC, Doré V, Jones G, Baxendale D, Mulligan RS, Bullich S, et al. 18F-Florbetaben PET beta-amyloid binding expressed in Centiloids. Eur J Nucl Med Mol Imaging. 2017;44:2053–9.
Fleisher AS, Pontecorvo MJ, Devous MD Sr, Lu M, Arora AK, Truocchio SP, et al. Positron Emission Tomography Imaging With [18F]flortaucipir and Postmortem Assessment of Alzheimer Disease Neuropathologic Changes. JAMA Neurology. 2020;77:829–39.
Soleimani-Meigooni DN, Iaccarino L, La Joie R, Baker S, Bourakova V, Boxer AL, et al. 18F-flortaucipir PET to autopsy comparisons in Alzheimer’s disease and other neurodegenerative diseases. Brain. 2020;143:3477–94.
Cho H, Choi JY, Hwang MS, Kim YJ, Lee HM, Lee HS, et al. In vivo cortical spreading pattern of tau and amyloid in the Alzheimer disease spectrum. Ann Neurol. 2016;80:247–58.
Schwarz AJ, Yu P, Miller BB, Shcherbinin S, Dickson J, Navitsky M, et al. Regional profiles of the candidate tau PET ligand 18F-AV-1451 recapitulate key features of Braak histopathological stages. Brain. 2016;139:1539–50.
Ossenkoppele R, Rabinovici GD, Smith R, Cho H, Schöll M, Strandberg O, et al. Discriminative Accuracy of [18F]flortaucipir Positron Emission Tomography for Alzheimer Disease vs Other Neurodegenerative Disorders. JAMA. 2018;320:1151–62.
Weigand AJ, Maass A, Eglit GL, Bondi MW. What’s the cut-point?: a systematic investigation of tau PET thresholding methods. Alzheimers Res Ther. 2022;14:49.
Wilson CM, Selwyn RG, Elojeimy S. Comparison of PET/CT SUV metrics across different clinical software platforms. Clin Imaging. 2022;89:104–8.
Donohue MC, Sperling RA, Salmon DP, Rentz DM, Raman R, Thomas RG, et al. The preclinical Alzheimer cognitive composite: measuring amyloid-related decline. JAMA Neurol. 2014;71:961–70.
Kueper JK, Speechley M, Montero-Odasso M. The Alzheimer’s Disease Assessment Scale-Cognitive Subscale (ADAS-Cog): Modifications and Responsiveness in Pre-Dementia Populations. A Narrative Review. J Alzheimers Dis. 2018;63:423–44.
Crane PK, Carle A, Gibbons LE, Insel P, Mackin RS, Gross A, et al. Development and assessment of a composite score for memory in the Alzheimer’s Disease Neuroimaging Initiative (ADNI). Brain Imaging Behav. 2012;6:502–16.
Bangen KJ, Nation DA, Delano-Wood L, Weissberger GH, Hansen LA, Galasko DR, et al. Aggregate effects of vascular risk factors on cerebrovascular changes in autopsy-confirmed Alzheimer’s disease. Alzheimers Dement. 2015;11:394–403.e1.
Zahodne LB, Gongvatana A, Cohen RA, Ott BR, Tremont G, Alzheimer’s Disease Neuroimaging Initiative. Are apathy and depression independently associated with longitudinal trajectories of cortical atrophy in mild cognitive impairment? Am J Geriatr Psychiatry. 2013;21:1098–106.
Ferrari-Souza JP, Brum WS, Hauschild LA, Da Ros LU, Ferreira PCL, Bellaver B, et al. Vascular risk burden is a key player in the early progression of Alzheimer’s disease. Neurobiol Aging. 2024;136:88–98.
Cook RD. Detection of Influential Observation in Linear Regression. Technometrics. 1977;19:15–18.
Demidenko E, Stukel TA. Influence analysis for linear mixed-effects models. Stat Med. 2005;24:893–909.
Villemagne VL, Burnham S, Bourgeat P, Brown B, Ellis KA, Salvado O, et al. Amyloid β deposition, neurodegeneration, and cognitive decline in sporadic Alzheimer’s disease: a prospective cohort study. Lancet Neurol. 2013;12:357–67.
Braak H, Thal DR, Ghebremedhin E, Del Tredici K. Stages of the pathologic process in Alzheimer disease: age categories from 1 to 100 years. J Neuropathol Exp Neurol. 2011;70:960–9.
Braak H, Del Tredici K. The preclinical phase of the pathological process underlying sporadic Alzheimer’s disease. Brain. 2015;138:2814–33.
Botha H, Mantyh WG, Murray ME, Knopman DS, Przybelski SA, Wiste HJ, et al. FDG-PET in tau-negative amnestic dementia resembles that of autopsy-proven hippocampal sclerosis. Brain. 2018;141:1201–17.
White LR, Edland SD, Hemmy LS, Montine KS, Zarow C, Sonnen JA, et al. Neuropathologic comorbidity and cognitive impairment in the Nun and Honolulu-Asia Aging Studies. Neurology. 2016;86:1000–8.
Kapasi A, DeCarli C, Schneider JA. Impact of multiple pathologies on the threshold for clinically overt dementia. Acta Neuropathol. 2017;134:171–86.
Lo RY, Jagust WJ, Alzheimer’s Disease Neuroimaging Initiative. Vascular burden and Alzheimer disease pathologic progression. Neurology. 2012;79:1349–55.
Goukasian N, Hwang KS, Romero T, Grotts J, Do TM, Groh JR, et al. Association of brain amyloidosis with the incidence and frequency of neuropsychiatric symptoms in ADNI: a multisite observational cohort study. BMJ Open. 2019;9:e031947.
Landau SM, Lee J, Murphy A, Ward TJ, Harrison TM, Baker SL, et al. Individuals with Alzheimer’s disease and low tau burden: Characteristics and implications. Alzheimers Dement. 2024. 19 January 2024. https://doi.org/10.1002/alz.13609.
Schneider JA, Arvanitakis Z, Leurgans SE, Bennett DA. The neuropathology of probable Alzheimer disease and mild cognitive impairment. Ann Neurol. 2009;66:200–8.
Rahimi J, Kovacs GG. Prevalence of mixed pathologies in the aging brain. Alzheimers Res Ther. 2014;6:82.
Wennberg AM, Whitwell JL, Tosakulwong N, Weigand SD, Murray ME, Machulda MM, et al. The influence of tau, amyloid, alpha-synuclein, TDP-43, and vascular pathology in clinically normal elderly individuals. Neurobiol Aging. 2019;77:26–36.
Josephs KA, Weigand SD, Whitwell JL. Characterizing Amyloid-Positive Individuals With Normal Tau PET Levels After 5 Years. Neurology. 2022;98:e2282–e2292.
van der Flier WM, Skoog I, Schneider JA, Pantoni L, Mok V, Chen CLH, et al. Vascular cognitive impairment. Nat Rev Dis Primers. 2018;4:1–16.
Lyketsos CG, Carrillo MC, Ryan JM, Khachaturian AS, Trzepacz P, Amatniek J, et al. Neuropsychiatric symptoms in Alzheimer’s disease. Alzheimers Dement. 2011;7:532–9.
Califf RM. Biomarker definitions and their applications. Exp Biol Med. 2018;243:213–21.
Trevethan R. Sensitivity, Specificity, and Predictive Values: Foundations, Pliabilities, and Pitfalls in Research and Practice. Front Public Health. 2017;5:307.
Wang X, Ye T, Zhou W, Zhang J. for the Alzheimer’s Disease Neuroimaging Initiative. Uncovering heterogeneous cognitive trajectories in mild cognitive impairment: a data-driven approach. Alzheimer’s. Res Ther. 2023;15:57.
Phillips ML, Stage EC Jr., Lane KA, Gao S, Risacher SL, Goukasian N, et al. Neurodegenerative Patterns of Cognitive Clusters of Early-Onset Alzheimer’s Disease Subjects: Evidence for Disease Heterogeneity. Dement Geriatr Cogn Disord. 2019;48:131–42.
Rentz DM, Wessels AM, Annapragada AV, Berger A-K, Edgar CJ, Gold M, et al. Building clinically relevant outcomes across the Alzheimer’s disease spectrum. Alzheimers Dement. 2021;7:e12181.
Zaleta AK, Carpenter BD, Porensky EK, Xiong C, Morris JC. Agreement about diagnosis among patients, companions, and professionals following a dementia evaluation. Alzheimer Dis Assoc Disord. 2012;26:232–7.
Sugarman MA, Alosco ML, Tripodis Y, Steinberg EG, Stern RA. Neuropsychiatric Symptoms and the Diagnostic Stability of Mild Cognitive Impairment. J Alzheimers Dis. 2018;62:1841–55.
Han JW, Kim TH, Lee SB, Park JH, Lee JJ, Huh Y, et al. Predictive validity and diagnostic stability of mild cognitive impairment subtypes. Alzheimer’s & Dementia. 2012;8:553–9.
Ostrowitzki S, Lasser RA, Dorflinger E, Scheltens P, Barkhof F, Nikolcheva T, et al. A phase III randomized trial of gantenerumab in prodromal Alzheimer’s disease. Alzheimers Res Ther. 2017;9:95.
van Dyck CH, Swanson CJ, Aisen P, Bateman RJ, Chen C, Gee M, et al. Lecanemab in Early Alzheimer’s Disease. N Engl J Med. 2023;388:9–21.
Boccardi M, Gallo V, Yasui Y, Vineis P, Padovani A, Mosimann U, et al. The biomarker-based diagnosis of Alzheimer’s disease. 2-lessons from oncology. Neurobiol Aging. 2017;52:141–52.
Borland E, Edgar C, Stomrud E, Cullen N, Hansson O, Palmqvist S. Clinically Relevant Changes for Cognitive Outcomes in Preclinical and Prodromal Cognitive Stages. Neurology. 2022;99:e1142–e1153.
Montine TJ, Phelps CH, Beach TG, Bigio EH, Cairns NJ, Dickson DW, et al. National Institute on Aging-Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease: a practical approach. Acta Neuropathol. 2012;123:1–11.
Cano SJ, Posner HB, Moline ML, Hurt SW, Swartz J, Hsu T, et al. The ADAS-cog in Alzheimer’s disease clinical trials: psychometric evaluation of the sum and its parts. J Neurol Neurosurg Psychiatry. 2010;81:1363–8.
Edmonds EC, Delano-Wood L, Galasko DR, Salmon DP, Bondi MW, Alzheimer’s Disease Neuroimaging Initiative. Subtle Cognitive Decline and Biomarker Staging in Preclinical Alzheimer’s Disease. J Alzheimers Dis. 2015;47:231–42.
Knopman DS, Jack CR, Wiste HJ, Weigand SD, Vemuri P, Lowe V, et al. Short-term clinical outcomes for stages of NIA-AA preclinical Alzheimer disease. Neurology. 2012;78:1576–82.
Parnetti L, Chipi E, Salvadori N, D’Andrea K, Eusebi P. Prevalence and risk of progression of preclinical Alzheimer’s disease stages: a systematic review and meta-analysis. Alzheimers Res Ther. 2019;11:7.
Raket LL. Statistical Disease Progression Modeling in Alzheimer Disease. Front Big Data. 2020;3:24.
Wilson RS, Segawa E, Boyle PA, Anagnos SE, Hizel LP, Bennett DA. The Natural History of Cognitive Decline in Alzheimer’s Disease. Psychol Aging. 2012;27:1008–17.
Rajan KB, Wilson RS, Barnes LL, Aggarwal NT, Weuve J, Evans DA. A Cognitive Turning Point in Development of Clinical Alzheimer’s Disease Dementia and Mild Cognitive Impairment: A Biracial Population Study. J Gerontol A Biol Sci Med Sci. 2017;72:424–30.
Yu L, Boyle P, Wilson RS, Segawa E, Leurgans S, De Jager PL, et al. A random change point model for cognitive decline in Alzheimer’s disease and mild cognitive impairment. Neuroepidemiology. 2012;39:73–83.
Joie RL, Ayakta N, Seeley WW, Borys E, Boxer AL, DeCarli C, et al. Multi-site study of the relationships between ante mortem [11C]PIB-PET Centiloid values and post mortem measures of Alzheimer’s disease neuropathology. Alzheimers Dement. 2019;15:205–16.
Pemberton HG, Collij LE, Heeman F, Bollack A, Shekari M, Salvadó G, et al. Quantification of amyloid PET for future clinical use: a state-of-the-art review. Eur J Nucl Med Mol Imaging. 2022;49:3508–28.
Hanseeuw BJ, Malotaux V, Dricot L, Quenon L, Sznajer Y, Cerman J, et al. Defining a Centiloid scale threshold predicting long-term progression to dementia in patients attending the memory clinic: an [18F] flutemetamol amyloid PET study. Eur J Nucl Med Mol Imaging. 2021;48:302–10.
Ng S, Villemagne VL, Berlangieri S, Lee S-T, Cherk M, Gong SJ, et al. Visual Assessment Versus Quantitative Assessment of 11C-PIB PET and 18F-FDG PET for Detection of Alzheimer’s Disease. J Nucl Med. 2007;48:547–52.
Levin F, Ferreira D, Lange C, Dyrba M, Westman E, Buchert R, et al. Data-driven FDG-PET subtypes of Alzheimer’s disease-related neurodegeneration. Alzheimers Res Ther. 2021;13:49.
Schwarz AJ. The Use, Standardization, and Interpretation of Brain Imaging Data in Clinical Trials of Neurodegenerative Disorders. Neurotherapeutics. 2021;18:686–708.
Pauker SG, Kassirer JP. The Threshold Approach to Clinical Decision Making. N Engl J Med. 1980;302:1109–17.
Pletcher MJ, Pignone M. Evaluating the clinical utility of a biomarker: a review of methods for estimating health impact. Circulation. 2011;123:1116–24.
Leuzy A, Chiotis K, Lemoine L, Gillberg P-G, Almkvist O, Rodriguez-Vieitez E, et al. Tau PET imaging in neurodegenerative tauopathies-still a challenge. Mol Psychiatry. 2019;24:1112–34.
Malarte M-L, Gillberg P-G, Kumar A, Bogdanovic N, Lemoine L, Nordberg A. Discriminative binding of tau PET tracers PI2620, MK6240 and RO948 in Alzheimer’s disease, corticobasal degeneration and progressive supranuclear palsy brains. Mol Psychiatry. 2023;28:1272–83.
Acknowledgements
Data collection and sharing for the Alzheimer’s Disease Neuroimaging Initiative (ADNI) is funded by the National Institute on Aging (National Institutes of Health Grant U19 AG024904). The grantee organization is the Northern California Institute for Research and Education. In the past, ADNI has also received funding from the National Institute of Biomedical Imaging and Bioengineering, the Canadian Institutes of Health Research, and private sector contributions through the Foundation for the National Institutes of Health (FNIH) including generous contributions from the following: AbbVie, Alzheimer’s Association; Alzheimer’s Drug Discovery Foundation; Araclon Biotech; BioClinica, Inc.; Biogen; Bristol-Myers Squibb Company; CereSpir, Inc.; Cogstate; Eisai Inc.; Elan Pharmaceuticals, Inc.; Eli Lilly and Company; EuroImmun; F. Hoffmann-La Roche Ltd and its affiliated company Genentech, Inc.; Fujirebio; GE Healthcare; IXICO Ltd.; Janssen Alzheimer Immunotherapy Research & Development, LLC.; Johnson & Johnson Pharmaceutical Research &Development LLC.; Lumosity; Lundbeck; Merck & Co., Inc.; Meso Scale Diagnostics, LLC.; NeuroRx Research; Neurotrack Technologies; Novartis Pharmaceuticals Corporation; Pfizer Inc.; Piramal Imaging; Servier; Takeda Pharmaceutical Company; and Transition Therapeutics.
Funding
This study was financially supported by the Center for Innovative Medicine (CIMED) at Region Stockholm and Karolinska Institutet, the KID funding at Karolinska Institutet, the Swedish Alzheimer’s Foundation, the Swedish Society for Medical Research, the Foundation for Geriatric Diseases and the Loo and Hans Osterman Foundation for Medical Research at Karolinska Institutet, the Swedish Dementia Association, the Gun and Bertil Stohne Foundation, the Åke Wiberg Foundation, the Foundation for Old Servants, the Eva and Oscar Ahrén Research Foundation Stockholm, the Åhlen Foundation, the Magnus Bergvall Foundation and the Tore Nilssons Foundation for Medical Research. Work in the Norberg lab is also supported by the Swedish Research Council (2017-02965, 2017-06086, 2020-01990), the Swedish Foundation for Strategic Research (SSF), and the Region Stockholm and Karolinska Institutet regional agreement on medical training and clinical research (ALF). An Erasmus+ fellowship grant supported Konstantinos Ioannou. Konstantinos Chiotis was supported by Region Stockholm (clinical postdoctoral appointment). Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Consortia
Contributions
KI and KC made substantial contributions to the conception and design of the analysis. KI also made substantial contributions to the acquisition of data from the ADNI repository, analysis, visualization of the data, and drafting the manuscript. MB, AT, and IS made substantial contributions to the data analysis. KI, MB, AT, IS, AN, and KC revised the manuscript critically for important intellectual content, approved the final version to be published, and have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consortia
Data used in preparation of this article were obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu). As such, the investigators within the ADNI contributed to the design and implementation of ADNI and/or provided data but did not participate in analysis or writing of this report. A complete listing of ADNI investigators can be found at: https://adni.loni.usc.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A list of authors and their affiliations appears at http://adni.loni.usc.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ioannou, K., Bucci, M., Tzortzakakis, A. et al. Tau PET positivity predicts clinically relevant cognitive decline driven by Alzheimer’s disease compared to comorbid cases; proof of concept in the ADNI study. Mol Psychiatry (2024). https://doi.org/10.1038/s41380-024-02672-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41380-024-02672-9
- Springer Nature Limited