Abstract
This review explores methodological considerations in estimating racial disparities in mortality among very preterm infants (VPIs). Significant methodological variations are evident across studies, potentially affecting the estimated mortality rates of VPIs across racial groups and influencing the perceived direction and magnitude of racial disparities. Key methodological approaches include the birth-based approach versus the fetuses-at-risk approach, with each offering distinct insights depending on the specific research questions posed. Cohort selection and the decision for crude versus adjusted comparison are also critical elements that shape the outcomes and interpretations of these studies. This review underscores the importance of careful methodological planning and highlights that no single approach is definitively superior; rather, each has its strengths and limitations depending on the research objectives. The findings suggest that adjusting the methodological approach to align with specific research questions and contexts is essential for accurately assessing and addressing racial disparities in neonatal mortality.
Impact
-
Elucidates the impact of methodological choices on perceived racial disparities in neonatal mortality.
-
Offers a comprehensive comparison of birth-based vs. fetuses-at-risk approaches in the context of racial disparity research.
-
Provides guidance on the cohort selection and adjustment criteria critical for interpreting studies on racial disparities in very preterm infant mortality.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Racial and ethnic disparities in newborn health outcomes arise from a complex interplay of socioeconomic and healthcare-related factors across different levels.1,2,3 Maternal health status, fetal and neonatal factors, hospital resources, provider attitudes, and social and neighborhood environments all contribute significantly to these disparities. Accurately measuring these disparities is challenging and heavily influenced by the methodological choices made in study design, which can significantly impact the findings.1,2,3,4,5 Currently, there is variability in methodological approaches used to estimate racial disparities in preterm infant mortality, with the chosen approach potentially altering the observed direction and extent of disparities.1 Selection of the source population also has implications on mortality rates and requires careful consideration. In this review, we highlight differences in common methodological approaches to estimating racial disparities in mortality of very preterm infants and discuss how particular methods might be suitable for various research goals. We consider the very preterm infant (VPI) as those born prior to 32 weeks gestational age and the extremely preterm infant (EPI) as those born prior to 28 weeks.
Birth-based approach vs. fetuses-at-risk approach
The examination of racial disparities in VPI mortality is underpinned by two methodological approaches: the birth-based approach and the fetuses-at-risk (FAR) approach.6,7,8,9,10 The birth-based method calculates mortality rates exclusively based on births, which are predominantly live births. In contrast, the FAR approach considers all fetuses beyond a specified gestational age as at risk.6 This distinction has led to seemingly contradictory findings. Table 1 shows results from several recent studies using US national vital statistics data: the birth-based approach typically shows lower mortality rates among Black VPIs/EPIs compared to White infants, with a rate ratio approximately between 0.8–0.9; while under the FAR approach, this trend reverses, revealing Black very preterm or extremely preterm fetuses experiencing 2–3 times the mortality rate of White fetuses.8,9,10
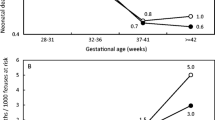
This divergence raises controversy regarding which approach more effectively illuminates the racial disparities in VPI outcomes.7,11,12 Both the birth-based and FAR approaches contribute valuable perspectives, with the choice between them hinging on the specific research questions and aspects of care under consideration. The FAR approach, by including a broader at-risk population, allows for an analysis of the total impact of racial and ethnic disparities on VPI outcomes. This includes the racial influence of very preterm birth rates and the direct racial effects on VPI outcomes, spanning both before and after birth (Fig. 1).7 The comprehensive nature of disparities uncovered by the FAR method may carry broader implications for public health and obstetric practices. However, the results of this approach are highly driven by the differences in very or extremely preterm birth rates, so it may not be suitable to capture the nuances of postnatal care practices’ impact.
This figure highlights the fundamental distinctions between the fetuses-at-risk approach and the birth-based approach, focusing on differences in source populations and the timing of racial exposure. These distinctions define how each approach addresses unique research questions, illustrating that the racial disparities observed by each method reveal different facets of the impact of racial exposure on mortality among very preterm infants.
Conversely, the birth-based approach provides a more focused lens on the postnatal period, examining the direct influence of racial factors on the outcomes of infants who have been born. This specificity makes it especially relevant to neonatal healthcare professionals. By offering a targeted view of racial disparities that emerge after birth, the birth-based method underscores the importance of postnatal care in addressing these disparities.2,13,14
Therefore, the decision to employ the birth-based versus FAR approach should be informed by the research aim and the domain of care being investigated. Recognizing the distinct advantages and limitations of each method is essential for a thorough understanding of racial disparities in VPI mortality. Based on the current data, it appears that during the very preterm period, because 2 to 3 times as many Black than white fetuses will be born during the very preterm period, Black fetuses face a 2–3 times higher risk of mortality compared to white fetuses; however, postnatally, among liveborn VPIs, Black infants exhibit a lower risk of death compared with white infants.8,9,10 The exact reasons for the relatively low mortality risk among Black VPIs require further investigation. This postnatal “advantage” for Black infants may partly be a reflection of the disproportionately high number of Black VPIs1. It should be kept in mind that despite the relative risk, the absolute number of Black VPIs that die is still higher than that of white VPIs in almost all contexts in the United States. In addition to mortality, morbidities such as bronchopulmonary dysplasia also show conflicting results under different approaches. Bronchopulmonary dysplasia seems to be less frequently observed in Black VPIs when using the birth-based approach.15,16,17 However, the FAR approach yields differing estimates of risk showing disadvantage rather than advantage for Black infants.7
Cohort selection
In studies examining mortality among very or extremely live preterm infants, the process of cohort selection (inclusion and exclusion) also introduces variations that influence the results (Table 2, Fig. 2).1,2,13,14,18,19 A notable example is a comprehensive assessment using population-based data from California, which highlighted that cohort selection could lead to nearly a threefold difference in estimated mortality rates of EPIs (Fig. 3).1 Studies employing various inclusion and exclusion criteria also found varying extent and direction of racial disparities (Table 2). The key aspects influencing cohort selection and their implications are as follows:
The main variations in cohort selection include gestational age and birth weight criteria, and the inclusion and exclusion of early deaths, delivery room deaths, and congenital anomalies (Table 2). The distribution of infants is not uniform across different gestational age or birth weight categories. Additionally, the incidence rates of neonatal death, early or delivery room death, and congenital anomalies vary significantly among these groups. Therefore, the cohort selection criteria can profoundly influence the estimated mortality rates and the perceived racial disparities in mortality among very preterm infants.
Data from reference.1 DR delivery room.
Lower gestational age cut-off
The practice of initiating active treatment for infants at 22–23 weeks’ gestation varies across hospitals and regions, leading to inconsistent inclusion of these infants in research. Their notably high mortality rates mean that their inclusion or exclusion can significantly affect mortality estimates. For instance, overall mortality estimates, including delivery room and early deaths, vary significantly between cohorts with lower gestational age cut-offs at 22 weeks versus those starting at 24 weeks (16% vs. 9%, Fig. 3).1 It is also worth noting that the analysis of racial disparities shows a potential reversal in the direction of absolute mortality difference when extending the lower gestational age cut-off from 24 to 22 weeks, albeit without statistical significance. Such reversal does not imply that Black infants at 22–23 weeks have higher mortality than White infants. On the contrary, Black infants at 22–23 weeks exhibit significantly lower mortality compared to white infants, but the higher proportion of birth at 22–23 weeks among Black EPIs causes this reversal.
Upper gestational age cut-off
The upper gestational age cut-off also varied from 27 to 31 weeks across studies (Table 2). Expanding the upper gestational age limit can dilute the representation of overall mortality for infants with smaller gestational age. Moreover, racial effects also differ across gestational age groups. The seeming survival advantage for Black infants diminishes and eventually reverses in favor of white infants around 32–34 weeks.18 Thus, varying the upper gestational age cut-off can alter the perceived direction and magnitude of racial disparities.
Birth weight criteria
Birth weight criteria have also been applied parallel or serial to gestational age. Compared with serial criteria (“and”) of gestational age and birth weight, the parallel criteria (“or”) generate more significant effect on mortality. Specifically, including infants with a birth weight of 401–1500 g alongside those at 22–29 weeks generally results in the inclusion of infants with a gestational age ≥ 30 weeks, affecting mortality similarly to adjustments in the upper gestational age cut-off. As shown in Fig. 3, the overall mortality decreases from 16 to 12% after adding the birthweight criteria.1 What’s more, after applying birth weight criteria, there is a trend toward an increase in the overall mortality disparity between Black and white infants, with the direction of differences in mortality, excluding early death, being reversed. This change is primarily due to the higher mortality among Black infants with a birth weight of 401–1500 g and gestational age ≥ 30 weeks. The relatively lower proportion of Black infants with a higher gestational age further contributes to the increase in disparity.
Exclusion of delivery room and early neonatal death
Several considerations must be weighed when deciding whether to exclude early neonatal deaths from analyses. Firstly, delivery room or early neonatal deaths are closely linked with the status at birth, decisions regarding active care, and delivery room management practices. Therefore, excluding these early deaths from analyses makes the resulting population more suitable for evaluating racial disparities influenced by variations in practices post-NICU admission. Secondly, early neonatal mortality is disproportionately high among infants at 22–23 weeks (Fig. 2); excluding these early deaths can lead to a significant reduction in the overall mortality estimation.1,20 For instance, with a 46% delivery room mortality rate for infants born at 22–23 weeks, excluding delivery room deaths resulted in a one-third reduction of the overall mortality from 16.1% to 10.9% in California (Fig. 3).1 Thirdly, in cases where universal active resuscitation is provided, such as ≥ 24 or 25 weeks, both the absolute delivery room mortality and the proportion of delivery room deaths relative to overall deaths are relatively low. This suggests that the inclusion or exclusion of these deaths may not significantly affect the extent or direction of comparisons across different groups, such as by location or race.1,21 Lastly, potential racial disparities in the rates of active management and death rates in the delivery room for periviable infants may offer additional insights into the impact of racial factors on perinatal decision making, and deserve targeted and independent investigation.1,22,23
Exclusion of congenital anomaly
Most studies investigating racial disparities exclude infants with congenital anomalies (Table 2). This selection strategy aims to create a “healthier” preterm population that allows for a more unambiguous evaluation of the association between postnatal exposures and outcomes, by minimizing confounding from potentially varying rates and severities of congenital anomalies across different exposure groups. Very or extremely preterm infants generally have a higher incidence of congenital anomalies with high mortality. For example, in California, 6.7% of infants at 22–29 weeks’ gestation or weighing 401–1500 g were noted to have congenital anomalies, with an overall mortality of 17.5%.1 Consequently, the exclusion of infants with congenital anomalies resulted in a 12% reduction in the absolute overall mortality rate, from 13.6% to 12.0% (Fig. 3). However, the exclusion of infants with congenital anomaly did not appear to significantly affect the direction and extent of racial disparity (Fig. 3). Notably, Black infants exhibited a lower incidence of congenital anomaly (5.1% vs. 7.3%) compared to white infants, but showed a significantly higher mortality (34.5% vs. 14.1%) from such conditions. This discrepancy may be explained by increased severity of congenital abnormalities in Black compared to White infants, differences in maternal risk status such as comorbidities that also impact neonatal outcomes, or racial differences in treatment for congenital anomalies.24 For example, the Black: White mortality disparity among infants with congenital heart disease was found to be wider in the post-neonatal period than the neonatal period, even after adjusting for maternal risk status, implying that timing of surgical procedures may differ in Black compared with white infants.25 The differential distribution and outcomes of infants with congenital anomalies across racial groups may necessitate independent investigation and verification to fully understand the implication of these findings.
In summary, cohort selection is another important methodology issue in shaping the outcomes and interpretations of research into racial disparities in VPI mortality. Variations in selection criteria may alter perceptions of the disparities’ magnitude and direction. Therefore, it is essential to exercise meticulous care in the cohort selection process, ensuring the study population accurately represents the source population and is aptly chosen to address the research question at hand.
Crude vs. adjusted comparisons
Risk adjustments are frequently applied in studies evaluating racial disparity of VPI mortality, while variations exist in the adoption of adjustments and the selection of adjustment variables. Results should be interpreted in context of the specific research question, with attention to appropriateness of the risk adjustment strategy.
To adjust or not to adjust
Most studies adjust for factors including maternal socioeconomic status, maternal health condition, antenatal care practices, and infant birth characteristics (Table 2). Some investigators argue that adjusting for such variables related to medical care will mask the effects of race as well as related factors and therefore mask disparities.13 The purpose of adjustment is to identify the independent association between race and neonatal mortality, by controlling for other variables that could confound the association. So, the decision to adjust is determined by what race represents in a specific study context. In studies assessing the overall antenatal and postnatal effect of race on neonatal mortality, all the aforementioned factors may lie within the causal pathway from race to neonatal mortality (Fig. 4a), and act as mediators; thus, the adjustment of these factors could diminish the race-mortality association. Conversely, in studies focusing on postnatal or neonatal periods, race serves as a proxy for the impact of postnatal care practice (Fig. 4b, c). Factors occurring before and at birth may influence both the exposure (racial-related postnatal care practice) and the outcome and may be adjusted as confounders. The interpretation of such analysis assumes that any adjusted racial effect on neonatal mortality is due to postnatal or post-admission events.
This figure maps out the different adjusting factors considered when evaluating the racial disparities in neonatal mortality. a Evaluating the overall antenatal and postnatal effects of racial exposure on neonatal mortality: In this scenario, maternal socioeconomic status, health conditions, antenatal care, infant birth characteristics, and postnatal care are viewed as mediators in the causal pathway from race to neonatal mortality. b Evaluating the overall postnatal effect of race on neonatal mortality: In this scenario, antenatal factors such as maternal health condition, antenatal care and infant birth characteristics act as confounders. The postnatal effect of race could be mediated by, or independent of, maternal social economic status. c Evaluating the postnatal effect of race on neonatal mortality independent of maternal socioeconomic status: In this scenario, maternal socioeconomic status is treated as a confounder. The analysis seeks to isolate the postnatal effects of race on neonatal mortality from the influences of socioeconomic factors.
There is often a contradiction between unadjusted and adjusted associations between race and VPI mortality. Despite higher or similar mortality of observed mortality among the Black VPI/EPIs, the adjusted analyses show better outcomes among Black VPI/ EPIs compared to white infants.1,2 This may indicate that factors such as gestational age and clinical status at birth have the most significant impact on the observed racial disparity.1 Some of these factors may be outside the direct control of healthcare providers, while others may depend on the approach of the combined obstetric and neonatal teams. Mortality by gestational age stratification also replicates this finding.18 Successful interventions aimed at addressing social determinants of health to improve maternal and neonatal health outcomes would decrease the discrepancy between unadjusted and adjusted analyses.
What to adjust
There are also variations in the factors adjusted for when evaluating the postnatal association between race and neonatal mortality (Table 2). A common point of contention is whether to adjust for maternal socioeconomic status. Again, the decision to include these factors in multivariable models depends on the specific research question. The postnatal racial effect may arise from two sources: effects mediated by socioeconomic status and those unrelated to socioeconomic status (Fig. 4b). For example, racial disparities in breast milk or human milk feeding for VPIs may be mediated by socioeconomic factors, which influence cultural norms, parental leave policies, visitation opportunities, and availability of lactation support.26,27 In addition to these factors, hospital practices and quality improvement efforts can also significantly influence the provision of breast milk for VPIs.28 Therefore, when the objective is to evaluate the overall postnatal racial effect, maternal socioeconomic status may have mediation effect and generally should not be adjusted. In contrast, when the study aims to ascertain racial disparity irrespective of socioeconomic status, this status acts as a confounder (Fig. 4c). This approach may have significance in guiding quality improvement in NICUs, as effects unrelated to socioeconomic status may be more closely related with NICU care practice and could be modified in the NICU environment.
Another decision point in methodology is adjustment for treating hospitals. Both between-hospital and within-hospital racial variation exist in care practice and outcomes for VPIs.14,19 When centers are not accounted for in adjustment, the association between race and neonatal mortality reflect the combined effect of both between- and within- hospital care variations. For example, Black and Hispanic infants may be more likely to receive care in NICUs with worse quality measures. They may also receive lower quality of care compared to white infants within the same NICU. When adjusting for the hospital as a cluster, the between-NICU disparity may be obscured, and the associations observed may reflect more the effect of within-hospital practice variations. In situations where a hospital or group of hospitals do not provide optimal care to Black infants or other minoritized populations, incorporating the hospital as an adjustment factor may mask such disparities.
Conclusion
In conclusion, significant methodological variations exist in studies that assess racial disparities in mortality among VPIs. These methodological differences can substantially affect the estimated mortality rates of VPIs across different racial groups and potentially alter the perceived direction and magnitude of racial disparities. There is no singular “best” or “correct” methodology for studying racial disparities; each approach offers valuable insights and implications. The selection of the source population, as well as the careful definition of inclusion and exclusion criteria and the choice of analysis model, requires meticulous consideration. These decisions must align closely with the specific objectives of the research question to ensure that the findings are both robust and relevant.
References
Gould, J. B., Bennett, M. V., Profit, J. & Lee, H. C. Cohort selection and the estimation of racial disparity in mortality of extremely preterm neonates. Pediatr. Res. 95, 792–801 (2024).
Travers, C. P. et al. Racial/ethnic disparities among extremely preterm infants in the United States from 2002 to 2016. JAMA Netw. Open 3, e206757 (2020).
Profit, J., Edwards, E. M. & Pursley, D. Getting to health equity in NICU care in the USA and beyond. Arch. Dis. Child Fetal. Neonatal. Ed. 108, 326–331 (2023).
Brumberg, H. L., Dozor, D. & Golombek, S. G. History of the birth certificate: from inception to the future of electronic data. J. Perinatol. 32, 407–411 (2012).
Weikel, B. W. et al. Defining an infant’s race and ethnicity: a systematic review. Pediatrics 151, e2022058756 (2023).
Joseph, K. S. & Kramer, M. S. The fetuses-at-risk approach: survival analysis from a fetal perspective. Acta Obstet. Gynecol. Scand. 97, 454–465 (2018).
Janevic, T. et al. Association of race/ethnicity with very preterm neonatal morbidities. JAMA Pediatr. 172, 1061–1069 (2018).
Wu, B., Taylor, S., Shabanova, V. & Hawley, N. L. Birth-based vs. fetuses-at-risk approaches for assessing neonatal mortality rate by race. JAMA Pediatr. 177, 633–635 (2023).
Boutin, A. et al. Bias in comparisons of mortality among very preterm births: a cohort study. PLoS ONE 16, e0253931 (2021).
Shukla, V. V., Youngblood, E. M., Tindal, R. R., Carlo, W. A. & Travers, C. P. Persistent disparities in black infant mortality across gestational ages in the United States. J. Perinatol. 44, 584–586 (2024).
Basso, O. Implications of using a fetuses-at-risk approach when fetuses are not at risk. Paediatr. Perinat. Epidemiol. 30, 3–10 (2016).
Schisterman, E. F. & Sjaarda, L. A. No right answers without knowing your question. Paediatr. Perinat. Epidemiol. 30, 20–22 (2016).
Boghossian, N. S. et al. Racial and ethnic differences over time in outcomes of infants born less than 30 weeks’ gestation. Pediatrics 144, e20191106 (2019).
Profit, J. et al. Racial/ethnic disparity in NICU quality of care delivery. Pediatrics 140, e20170918 (2017).
Lapcharoensap, W. et al. Hospital variation and risk factors for bronchopulmonary dysplasia in a population-based cohort. JAMA Pediatr. 169, e143676 (2015).
Ryan, R. M. et al. Black race is associated with a lower risk of bronchopulmonary dysplasia. J. Pediatr. 207, 130–135 (2019).
Lewis, T. R. et al. Association of racial disparities with in-hospital outcomes in severe bronchopulmonary dysplasia. JAMA Pediatr. 176, 852–859 (2022).
Venkatesan, T. et al. National trends in preterm infant mortality in the United States by race and socioeconomic status, 1995–2020. JAMA Pediatr. 177, 1085–1095 (2023).
Howell, E. A. et al. Differences in morbidity and mortality rates in black, white, and Hispanic very preterm infants among New York City Hospitals. JAMA Pediatr. 172, 269–277 (2018).
Forner, O. et al. Extremely premature infants: how does death in the delivery room influence mortality rates in two level 3 centers in France? Arch. Pediatr. 25, 383–388 (2018).
Profit, J. et al. Variations in definitions of mortality have little influence on neonatal intensive care unit performance ratings. J. Pediatr. 162, 50–55 (2013).
Venkatesh, K. K. et al. Trends in active treatment of live-born neonates between 22 weeks 0 Days and 25 weeks 6 days by gestational age and maternal race and ethnicity in the US, 2014 to 2020. JAMA 328, 652–662 (2022).
Chen, X. et al. Active treatment of infants born at 22–25 weeks of Gestation in California, 2011–2018. J. Pediatr. 249, 67–74 (2022).
Ely, D. M. & Driscoll, A. K. Infant mortality in the United States, 2020: data from the period linked birth/infant death file. Natl. Vital. Stat. Rep. 71, 1–18 (2022).
Collins, J. W. Jr., Soskolne, G., Rankin, K. M., Ibrahim, A. & Matoba, N. African-American:white disparity in infant mortality due to congenital heart disease. J. Pediatr. 181, 131–136 (2017).
Quintero, S. M. et al. Race/ethnicity-specific associations between breastfeeding information source and breastfeeding rates among U.S. Women. BMC Public Health 23, 520 (2023).
Parker, M. G. et al. National trends in the provision of human milk at hospital discharge among very low-birth-weight infants. JAMA Pediatr. 173, 961–968 (2019).
Lee, H. C. et al. A quality improvement project to increase breast milk use in very low birth weight infants. Pediatrics 130, e1679–e1687 (2012).
Funding
The research reported in this article was supported by the National Institutes of Health (Grant R01 HD098287). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Contributions
SJ, LAR, JBG, MVB, JP, and HCL contributed to conception and design, drafted the article and revised it critically for important intellectual content; and give final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jiang, S., Rose, L.A., Gould, J.B. et al. Methodologic considerations in estimating racial disparity of mortality among very preterm infants. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03485-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03485-w
- Springer Nature America, Inc.