Abstract
Background
To investigate the longitudinal effects of obesity on change in lung function after 1 year of follow-up in obese children and adolescents.
Methods
Obese children/adolescents aged 8–15 years with pulmonary function test (PFT) results and recorded anthropometric obesity indices from 1 year earlier for comparison were recruited. Multiple linear regression of change in each lung function parameter was applied to determine the effect of sex, change in body mass index (ΔBMI), change in chest circumference (ΔCC), change in waist circumference (ΔWC), and change in waist circumference-to-height ratio (ΔWC/Ht).
Results
Sixty-six children/adolescents (mean age: 12.5 ± 2.6 years) were recruited. Multiple linear regression analysis showed that ΔWC negatively affects the ratio of the forced expiratory volume in the first 1 s to the forced vital capacity of the lungs Δ(FEV1/FVC) (b = −0.3, p = 0.002), forced expiratory flow rate within 25–75% of vital capacity (ΔFEF25–75%) (b = −0.92, p = 0.006), and Δ(FEF25–75%/FVC) (b = −0.99, p = 0.003). When replacing ΔWC with Δ(WC/Ht) as the independent variable, Δ(WC/Ht) also negatively affects Δ(FEV1/FVC) (b = −33.71, p = 0.02), ΔFEF25–75% (b = −102.9, p = 0.03) and Δ(FEF25–75%/FVC) (b = −102.7, p = 0.03).
Conclusion
After 1 year of follow-up, change in abdominal adiposity determined by WC and WC/Ht exerted significant negative effect on lung function change specific to FEV1/FVC, FEF25–75% /FVC, and FEF25–75%.
Impact
-
Longitudinal effects of change in obesity on lung function in obese children and adolescents are evidenced.
-
Change in waist circumference or waist-to-height ratio, which indicates abdominal adiposity, was inversely correlated with a change in FEV1/FVC, FEF25–75% /FVC, and FEF25–75% in children and adolescents with obesity after 1 year of follow-up.
-
Our results suggest using waist circumference and/or waist-to-height ratio in addition to BW and/or BMI for monitoring obesity.
-
Fat loss programs, especially those focused on reducing abdominal adiposity should be encouraged to prevent late lung function impairment.
Similar content being viewed by others
Introduction
Obesity is a major global public health problem for children, adolescents, and adults, and its prevalence continues to increase. In addition to the functional impact on activities of daily living, obesity can cause significant health problems to various systems of the body.1 One of the most important systems to be adversely affected by obesity is the respiratory system with commonly observed problems that include obstructive sleep apnea, exercise intolerance, and altered lung function.2,3
Impaired lung function can also be observed in obese children and adolescents, including reductions in forced expiratory volume in 1 s/forced vital capacity (FEV1/FVC) ratio, functional residual capacity, expiratory reserve volume (ERV), and residual volume (RV).4,5 Most previous studies in the effects of obesity on lung function in children and adolescents had a cross-sectional design, and the results were often inconclusive. The long-term effects of obesity on changes in lung function were mostly studied in adults following bariatric surgery,6 which is a surgical procedure that is less commonly performed in children and adolescents. A longitudinal study in children by van de Griendt, et al.7 found a negative correlation between ERV change and both the change in waist circumference (WC) and the standard deviation score-body mass index (SDS-BMI), but no correlation with spirometric parameters. The Dutch Prevention and Incidence of Asthma and Mite Allergy (PIAMA)8 and Swedish BAMSE (Swedish abbreviation for Children, Allergy, Milieu, Stockholm, Epidemiology)9 studies found persistent obesity or high body mass index (BMI) to be associated with a lower forced expiratory volume in 1 s/forced vital capacity (FEV1/FVC) ratio.
How long-term change in weight and body composition is associated with lung function change in obese children and adolescents remains unclear, and the currently available published data on this important topic remains scarce. Accordingly, the aim of this study was to investigate the longitudinal effects of change in obesity on lung function parameters, including spirometry, respiratory muscle strength (RMS), and 6-min walk test (6-MWT), after a 1-year follow-up in obese children and adolescents. The results of this study will yield important data that will help us develop and improve strategies for managing children and adolescents with obesity.
Material and methods
Study protocol
This study was conducted at the Division of Pulmonology of the Department of Pediatrics, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand during January 2023 to January 2024. Inform consent or assent was obtained from participants and/or their legal guardian(s) before study enrollment. The study protocol was reviewed and approved by the Siriraj Institutional Review Board (approval no. Si 878/2022).
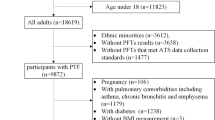
This follow-up study recruited non-syndromic obese children and adolescents aged 8–15 years who had acceptable and reproducible pulmonary function test (PFT) and recorded anthropometric obesity indices 1 year (±3 months) earlier for comparison. For this study, PFT and obesity indices were remeasured on the appointed study date so that the new measurement data could be compared with the measurement data collected one year prior. Obesity was defined as BMI z-score ≥2 according to World Health Organization (WHO) criteria.10 We excluded patients with a history of cardiac, neuromuscular, or pulmonary diseases; respiratory infections within the preceding 4 weeks; history of active or passive smoke; and/or, inability or unwillingness to perform the proposed study tests. All enrolled study patients were given standard treatment for obesity, including nutritional consultation for dietary control, recommendation for exercise and lifestyle modification, and evaluation of comorbidities. They may receive treatment for other specific diseases such as positive airway pressure for obstructive sleep apnea, intranasal steroid/ antihistamine for allergic rhinitis, or antihypertensive medications for hypertension.
Collected data included age, sex, height, and obesity indices, including body weight (BW), BMI, BMI z-score, chest circumference (CC), WC, and waist-to-height ratio (WC/Ht). PFTs, including spirometry, 6-MWT, and RMS, were performed by the same technician during the follow-up remeasurement period (i.e., the current study).
Anthropometric evaluation
Standardized measurement tools (TANITA Corporation, Tokyo, Japan) were used to measure BW and height. BMI was calculated as BW (kg) divided by the square of height (m2). BMI was also expressed as z-score (BMI z-score), which is the BMI adjusted for age and sex according to WHO growth reference data.11 CC was measured at nipple level, and WC was measured between the lower margin of the last rib and the iliac crest (Fig. 1)– both measured using a tape measure.
Spirometry
A VyntusTM BODY Plethysmograph (Vyaire Medical, Mettawa, IL) was used for spirometry according to American Thoracic Society (ATS)/European Respiratory Society (ERS) recommendations.12 The collected spirometry data included forced expiratory volume in 1 s (FEV1), forced vital capacity (FVC), FEV1/FVC ratio, forced expiratory flow rate within 25–75% of vital capacity (FEF25–75%). Except for FEV1/FVC ratio, all parameters were reported as percentage of predicted value (%predicted) calculated from multiethnic global lung function 2012 equations.13
6-min walk test (6-MWT)
The 6-MWT, which is a recommended performance-based tool for functional fitness assessment in accordance with the ATS guideline, was performed.14 Participants were instructed to walk as fast as possible without running for 6 min on a flat and straight surface. The length of the walking course was 30 meters with a clearly visible cone placed at the end of the course. During the test, participants were encouraged to walk, and the time remaining was announced at different timepoints. This test was immediately stopped if participants had shortness of breath, chest pain, heart palpitations, or leg cramps. The total distance walked was measured after 6 min of walking. The 6-MWT distance were reported as absolute and z-score value according to reference equation.15
Respiratory muscle strength (RMS)
Inspiratory and expiratory muscle strength was assessed via maximal inspiratory pressure (MIP) and maximal expiratory pressure (MEP), respectively, using a VyntusTM BODY Plethysmograph (Vyaire Medical) according to ATS/ERS recommendations.16 MIP was measured with the subject breathing in from RV to total lung capacity (TLC), and MEP was measured during forced expiration from TLC to RV. The measurement considered for data analysis was the highest value among 3 acceptable maneuvers (without leakage and lasting for at least 1 s), and at least two were reproducible (not different more than 10% from the second highest value). MIP and MEP values were expressed as absolute value and %predicted value based on reference equation.17
Statistical analysis
The data are presented as mean plus/minus (±) standard deviation (SD) for normally distributed continuous data, and as number and percentage for categorical data. Student’s t-test was used to compare baseline and follow-up data. Multiple linear regression was used to identify the effects of the independent variables, including sex, change in body mass index (ΔBMI), change in chest circumference (ΔCC), change in waist circumference (ΔWC), and change in waist circumference-to-height ratio (ΔWC/Ht), on each lung function parameter. Those results are shown as correlation coefficient (b) and p-value. Multicollinearity between independent variables was checked using variance inflation factor. SPSS Statistics for Windows version 26.0 (SPSS, Inc., Chicago, IL) was used to analyze the data. A p < 0.05 was considered statistically significant for all tests.
Results
Study group
This study enrolled 66 obese children and adolescents (50 boys, and 16 girls) with a mean age of 12.5 ± 2.6 years at follow-up. BMI was reduced in 35 participants, and increased in 31 participants with the mean change of 1.78 ± 1.28 kg/m2 and 1.28 ± 1.10 kg/m2 respectively, after a mean follow-up duration of 1.01 ± 0.14 years. Obesity indices that were statistically significantly different from baseline to follow-up included bodyweight (77.4 vs. 80.5 kg, p < 0.001), BMI z-score (3.56 vs. 3.20 kg/m2, p < 0.001), CC (98.1 vs. 99.6 cm, p = 0.049), and WC/Ht (0.66 vs. 0.65, p = 0.029) (Table 1).
A comparison of lung function between baseline and the follow-up showed a significant increase in MIP (106.2 vs. 118.1 cmH2O, p < 0.001, and 115.7 vs. 126.8%predicted, p < 0.001), MEP (100.6 vs. 110.0 cmH2O, p < 0.001, and 100.0 vs. 108.4%predicted, p < 0.001), and 6-MWT distance (533.9 vs. 554.2 meters, p = 0.004). The spirometry parameters that were significantly decreased at follow-up included FEV1/FVC (84.1 vs. 82.5%, p = 0.008) and FEF25–75%/FVC (92.7 vs. 87.2%, p = 0.007) (Table 2).
No participants received weight loss pharmacotherapy or underwent surgery for the treatment of obesity.
Factors related to change in PFTs
Table 3 shows the results of multiple linear regression analysis of changes in lung function on two different sets of independent variables. Model 1 included sex, ΔBMI, ΔCC, and ΔWC. Model 2 included sex, ΔBMI, ΔCC, and Δ(WC/Ht).
In Model 1, ΔWC showed a negative correlation with change in FEV1/FVC [Δ(FEV1/FVC)] (b = −0.3; p = 0.002), FEF25–75% (ΔFEF25–75%) (b = −0.92; p = 0.006), and FEF25–75%/FVC [Δ(FEF25–75%/FVC)] (b = −0.99; p = 0.003). Male sex was shown to significantly influence ΔFEF25–75% (b = −9.76; p = 0.04) and Δ(FEF25–75%/FVC) (b = −11.17; p = 0.02) (Table 3a).
In Model 2, Δ(WC/Ht) showed a negative correlation with Δ(FEV1/FVC) (b = −33.71; p = 0.02), ΔFEF25–75% (b = −102.9; p = 0.04), and Δ(FEF25–75%/FVC) (b = −102.7; p = 0.03). Male sex was found to significantly affect ΔFEF25–75% (b = −8.84; p = 0.04) and Δ(FEF25–75%/FVC) (b = −10.04; p = 0.03) (Table 3b).
Discussion
The present study found that the overall BMI z-score and WC/Ht among obese children and adolescents were significantly reduced at the 1-year follow-up; however, only minor changes were observed. These minor changes in obesity indices are within normal expectations, as achieving weight control through lifestyle modifications or dietary changes—without a specific weight loss program—can be quite challenging for obese individuals. The individual differences in adherence to recommendations, as well as variations in physical activity, dietary changes, and lifestyle modifications, can also introduce confounding effects on the study results.
In terms of lung function, we observed significant increases in both the absolute and %predicted values of RMS, along with a reduction in the FEV1/FVC and FEF25–75/FVC at follow-up. A possible explanation for the increased RMS could be the heightened workload on respiratory muscles due to the excess weight carried by obese individuals. This heightened workload may elicit an adaptive response, prompting the respiratory muscles to strengthen as a compensatory mechanism to meet the increased oxygen demand.18,19,20 The present study indicated a decrease in the BMI z-score but the reduction was minimal and BMI z-score remained within the obesity range. Consequently, this compensatory mechanism may continue and contribute to the increased RMS. Despite the improvements in BMI z-score and WC/Ht, the FEV1/FVC and FEF25–75/FVC values were found to be reduced at follow-up. This decline may be explained by ongoing dysanapsis process, which refers to the disproportionate overgrowth of lung tissue relative to airway development in obese children and adolescents21 due to persistent obesity.
Our study also revealed differences in the absolute value of the 6-MWT distance between baseline and follow-up. The increase in absolute value can be attributed to somatic growth, particularly an increase in height, as the 6-MWT distance is significantly correlated with height.22 However, the z-score value for the 6-MWT distance, which is adjusted for height, did not show a significant difference. This lack of change in the z-score value may be caused by the marginal changes in BMI z-score and WC/Ht at follow-up, which likely had no impact on the z-score for the 6-MWT distance.
Alterations in lung function may result in shortness of breath or exercise intolerance.2,3 In our study, although notable changes in lung function were observed at the follow-up assessment, these changes were not considered clinically significant. This lack of clinical impacts may be attributed to the minor changes in both lung function and obesity indices, as well as the fact that lung function remained within normal ranges at the beginning of the study and at the 1-year follow-up.
The present study provides important data specific to the longitudinal effects of a change in obesity on lung function in obese children and adolescents. We found a change in WC or WC/Ht, which indicates abdominal adiposity, to be inversely correlated with a change in FEV1/FVC, FEF25–75% /FVC, and FEF25–75% in children and adolescents with obesity after 1 year of follow-up. In contrast, a change in BMI did not significantly affect any spirometry parameters, RMS, or 6-MWT distance.
Our results indicate that abdominal fat deposition influences lung function change more profoundly than total adiposity, as reflected by BMI. Consistent with the findings of our study, a recent large longitudinal study in middle-aged Asian population by Park, et al.23 reported increased WC/Ht to be significantly associated with long-term impairment of lung function. A long-term study in children and adolescents with obesity found that a change in WC had more effect on lung function than change in BMI.7 Many previous cross-sectional studies in children24,25 and adults26,27,28 also reported abdominal adiposity to be a predictor of altered lung function. The main mechanism of abdominal obesity on altered lung function is excessive fat deposition in the diaphragm and abdominal visceral organs, which exerts an adverse mechanical effect on diaphragmatic movement and lung expansion.29,30 In our study, a change in BMI after 1 year follow-up was not significantly related to lung function change. The reason might be that BMI indicates overall fat and non-fat components of the body, but BMI does not reflect specific body fat distribution like WC or WC/Ht. Our results seem to strongly suggest WC and WC/Ht as important markers for lung function change in obesity. Accordingly, these two obesity parameters should be measured and monitored (in addition to BW and BMI) in routine clinical practice for obese individuals. Ideally, distribution of body fat and muscle mass as measured by direct methods, such as dual-energy X-ray absorptiometry or bioelectrical impedance analysis, should be used for monitoring obese individuals. However, these measurement modalities are expensive and often not available, which makes their use often impractical in routine clinical practice.
The present study included FEF25–75% /FVC, which was rarely investigated in previous studies, and found that change in WC and WC/Ht had negative association with change in FEV1/FVC, FEF25–75% /FVC, and FEF25–75%, but no association with FEV1 or FVC.
FEV1/FVC and FEF25–75%/FVC are surrogate markers for dysanapsis, which is defined as disproportionate scaling of airway dimensions to lung volume, which in turn leads to low FEV1/FVC and FEF25–75%/FVC.21,31 Our 1-year follow-up study supports dysanapsis growth, which can occur in obese children and adolescents.21 Most studies that found negative association between FEF25–75%/FVC32 or FEV1/FVC4,5,25,32 and obesity indices had a cross-sectional design. The longitudinal Dutch PIAMA study8 and Swedish BAMSE cohort study9 also found persistent high BMI or obesity in children to be associated with lower FEV1/FVC, but neither of those studies evaluated FEF25–75%/FVC.
We also found that change in WC and WC/Ht significantly inversely affects FEF25–75%, which reflects small airway function. This supports the findings of recent meta-analyses that found negative association between FEF25–75% and obesity status in obese children and adolescents.4,5 The greater effect of both WC and WC/Ht on FEF25–75%/FVC compared to their effect on FEV1/FVC, as indicated by a greater b-value for FEF25–75%/FVC, may reflect that obesity has more focused adverse effect on small airways. Lung function measurement that is more sensitive than spirometry for detecting impairment of small airways, such as oscillation technique, should be used to evaluate and clarify respiratory function change in obese individuals. In contrast to these findings, a longitudinal study in obese children and adolescents by van de Griendt, et al.7 reported no effect of change in obesity on any spirometric parameters. The actual long-term effects of fat deposition on the respiratory system and the pathophysiology of respiratory symptoms in obesity are still being investigated and debated. Further study is, therefore, needed to improve our understanding of this issue so that we can develop and improve prevention and treatment strategies.
The present study also found sex difference in small airway growth. Boys demonstrated more negative effect on FEF25–75% and FEF25–75%/FVC. This result is consistent with those reported from previous studies that demonstrated airway growth of boys to be slower than that observed in girls.21,33,34
Strengths and limitations
The strength of our study is its longitudinal design, which facilitated observation of change in the same patients over time. This is in contrast to a cross-sectional design which observes different patients at a single time point. Another strength is that we included WC and WC/Ht as obesity status variables, and FEF25–75%/FVC, RMS, and 6-MWT as lung function variables.
This study also has some mentionable limitations. First, data specific to other variables, such as physical activity, diet, and other environmental exposures, were not collected. Second, subgroup analysis of sex and pubertal stage was not be performed because the small size of many subgroups would need yield the statistical power needed to provide reliable statistical results. Future multicenter study in a much larger patient population is needed to confirm and expand upon the results of this study.
Conclusions
The present longitudinal study in children and adolescents with obesity demonstrated that change in abdominal adiposity, as determined by WC and WC/Ht, significantly influences lung function change in FEV1/FVC, FEF25–75% /FVC, and FEF25–75% after 1 year of follow-up. Our results indicate that change in WC and WC/Ht adversely impacts airflow, and with likely more pronounced effect on small airways. These results permit us to suggest using WC and/or WC/Ht in addition to BW and/or BMI for monitoring obesity. Fat loss programs, especially those focused on reducing abdominal adiposity should be encouraged to prevent late lung function impairment.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request and with approval of the IRB.
References
Hampl, S. E. et al. Clinical practice guideline for the evaluation and treatment of children and adolescents with obesity. Pediatrics 151, e2022060640 (2023).
Dixon, A. E. & Peters, U. The effect of obesity on lung function. Expert Rev. Respir. Med. 12, 755–767 (2018).
Shah, N. M. & Kaltsakas, G. Respiratory complications of obesity: from early changes to respiratory failure. Breathe 19, 220263 (2023).
Forno, E., Han, Y. Y., Mullen, J. & Celedón, J. C. Overweight, obesity, and lung function in children and adults-a meta-analysis. J. Allergy Clin. Immunol. Pract. 6, 570–581 (2018).
Ferreira, M. S., Marson, F. A. L., Wolf, V. L. W., Ribeiro, J. D. & Mendes, R. T. Lung function in obese children and adolescents without respiratory disease: a systematic review. BMC Pulm. Med. 20, 281 (2020).
Alsumali, A., Al-Hawag, A., Bairdain, S. & Eguale, T. The impact of bariatric surgery on pulmonary function: a meta-analysis. Surg. Obes. Relat. Dis. 14, 225–236 (2018).
van de Griendt, E. J. et al. Gain in lung function after weight reduction in severely obese children. Arch. Dis. Child 97, 1039–1042 (2012).
Bekkers, M. B. et al. BMI, waist circumference at 8 and 12 years of age and FVC and FEV1 at 12 years of age; the PIAMA birth cohort study. BMC Pulm. Med. 15, 39 (2015).
Ekström, S. et al. Body mass index status and peripheral airway obstruction in school-age children: a population-based cohort study. Thorax 73, 538–545 (2018).
de Onis, M. et al. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 85, 660–667 (2007).
WHO AnthroPlus for personal computers Manual: Software for assessing growth of the world’s children and adolescents. Geneva: WHO, 2009. https://www.who.int/tools/growth-reference-data-for-5to19-years.
Graham, B. L. et al. Standardization of spirometry 2019 update. an official American Thoracic Society and European Respiratory Society technical statement. Am. J. Respir. Crit. Care Med. 200, e70–e88 (2019).
Quanjer, P. H. et al. Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur. Respir. J. 40, 1324–1343 (2012).
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 166, 111–117 (2002).
Chen, C. A. et al. Six-minute walking test: normal reference values for Taiwanese children and adolescents. Acta Cardiol. Sin. 31, 193–201 (2015).
American Thoracic Society/European Respiratory Society. ATS/ERS Statement on respiratory muscle testing. Am. J. Respir. Crit. Care Med. 166, 518–624 (2002).
Verma, R., Chiang, J., Qian, H. & Amin, R. Maximal static respiratory and sniff pressures in healthy children. a systematic review and meta-analysis. Ann. Am. Thorac. Soc. 16, 478–487 (2019).
Magnani, K. L. & Cataneo, A. J. Respiratory muscle strength in obese individuals and influence of upper-body fat distribution. Sao Paulo Med. J. 125, 215–219 (2007).
Pazzianotto-Forti, E. M., Peixoto-Souza, F. S., Piconi-Mendes, C., Rasera-Junior, I. & Barbalho-Moulim, M. Behavior of respiratory muscle strength in morbidly obese women by using different predictive equations. Rev. Bras. Fisioter. 16, 479–486 (2012).
Shinde, B. V., Phatale, S. R., Shinde, P. U. & Waghmare, S. N. The impact of obesity on respiratory muscle strength in adults. Int. J. Contemp. Med. Res. 4, 1879–1882 (2017).
Forno, E. et al. Obesity and airway dysanapsis in children with and without asthma. Am. J. Respir. Crit. Care Med. 195, 314–323 (2017).
Mylius, C. F., Paap, D. & Takken, T. Reference value for the 6-min walk test in children and adolescents: a systematic review. Expert Rev. Respir. Med 10, 1335–1352 (2016).
Park, Y. et al. Longitudinal association between adiposity changes and lung function deterioration. Respir. Res. 24, 44 (2023).
Druce Axley, J. & Werk, L. N. Relationship between abdominal adiposity and exercise tolerance in children with obesity. Pediatr. Phys. Ther. 28, 386–391 (2016).
Udomittipong, K. et al. Obesity indices for predicting functional fitness in children and adolescents with obesity. Front. Pediatr. 9, 789290 (2021).
Ochs-Balcom, H. M. et al. Pulmonary function and abdominal adiposity in the general population. Chest 129, 853–862 (2006).
Sutherland, T. J., McLachlan, C. R., Sears, M. R., Poulton, R. & Hancox, R. J. The relationship between body fat and respiratory function in young adults. Eur. Respir. J. 48, 734–747 (2016).
Yang, M. S., Choi, S., Choi, Y. & Jin, K. N. Association between airway parameters and abdominal fat measured via computed tomography in asthmatic patients. Allergy Asthma Immunol. Res. 10, 503–515 (2018).
Choe, E. K. et al. The longitudinal association between changes in lung function and changes in abdominal visceral obesity in Korean non-smokers. PLoS ONE 13, e0193516 (2018).
Molani Gol, R. & Rafraf, M. Association between abdominal obesity and pulmonary function in apparently healthy adults: a systematic review. Obes. Res Clin. Pract. 15, 415–424 (2021).
Litonjua, A. A., Sparrow, D. & Weiss, S. T. The FEF25-75/FVC ratio is associated with methacholine airway responsiveness. the normative aging study. Am. J. Respir. Crit. Care Med. 159, 1574–1579 (1999).
Cibella, F. et al. An elevated body mass index increases lung volume but reduces airflow in Italian schoolchildren. PLoS ONE 10, e0127154 (2015).
Hibbert, M., Lannigan, A., Raven, J., Landau, L. & Phelan, P. Gender differences in lung growth. Pediatr. Pulmonol. 19, 129–134 (1995).
Becklake, M. R. & Kauffmann, F. Gender differences in airway behaviour over the human life span. Thorax 54, 1119–1138 (1999).
Acknowledgements
The authors gratefully acknowledge the study children/adolescents and their parents for generously agreeing to participate in this study. We would also like to thank Asst. Prof. Dr. Chulaluk Komoltri for her assistance with statistical analysis.
Funding
This study was supported by the Siriraj Research Development Fund (managed by Routine to Research: R2R) of the Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand [grant no. (IO) R016635036]. Open access funding provided by Mahidol University.
Author information
Authors and Affiliations
Contributions
K.U. conceived and designed the study, analyzed and interpreted the data, prepared the manuscript, and is the corresponding author. P.C. conceived and designed the study, recruited study participants, conducted fieldwork and statistical analysis, and wrote the first draft of the manuscript. A.P. recruited study participants and conducted fieldwork. K.M. conducted fieldwork and performed data collection. All authors reviewed, critically revised, and are in agreement with the version of the manuscript submitted for journal publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
Inform consent or assent was obtained from participants and/or their legal guardian(s) before study enrollment.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Charoensittisup, P., Udomittipong, K., Mahoran, K. et al. Longitudinal effects of obesity on pulmonary function in obese children and adolescents. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03544-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03544-2
- Springer Nature America, Inc.