Abstract
Colorectal cancer (CRC) is known to be resistant to immunotherapy. In our phase-I clinical trial, one patient achieved a 313-day prolonged response during the combined treatment of oncolytic virotherapy and immunotherapy. To gain a deeper understanding of the potential molecular mechanisms, we performed a comprehensive multi-omics analysis on this patient and three non-responders. Our investigation unveiled that, initially, the tumor microenvironment (TME) of this responder presented minimal infiltration of T cells and natural killer cells, along with a relatively higher presence of macrophages compared to non-responders. Remarkably, during treatment, there was a progressive increase in CD4+ T cells, CD8+ T cells, and B cells in the responder’s tumor tissue. This was accompanied by a significant upregulation of transcription factors associated with T-cell activation and cytotoxicity, including GATA3, EOMES, and RUNX3. Furthermore, dynamic monitoring of peripheral blood samples from the responder revealed a rapid decrease in circulating tumor DNA (ctDNA), suggesting its potential as an early blood biomarker of treatment efficacy. Collectively, our findings demonstrate the effectiveness of combined oncolytic virotherapy and immunotherapy in certain CRC patients and provide molecular evidence that virotherapy can potentially transform a “cold” TME into a “hot” one, thereby improving sensitivity to immunotherapy.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) stands as the third leading cause of global cancer-related mortality [1], and its incidence is higher in people related to obesity, physical inactivity, or alcohol consumption and is increasing in younger patients (≤50 years) [2]. Approximately 20% of newly diagnosed CRC have synchronous metastasis, and the liver turns out to be the most common metastasis organ [3]. Colorectal liver metastasis has a poor prognosis, and the phenotype of more than 95% metastasis CRC (mCRC) is microsatellite stable (MSS) [4]. It is reported that only 20–30% CRLM patients have the opportunity of surgery [5], while the rest are mainly treated with systemic chemotherapy and often show primary resistance to immunotherapy due to the presence of an immunosuppressive microenvironment associated with MSS status and the deletion of CD8+T cells mechanisms co-opted by liver metastases to manipulate host peripheral tolerance [6].
Oncolytic viruses (OVs) exhibit the properties of selective infection, replication, and targeted propagation within tumors [7]. They have the unique ability to preferentially target and eliminate cancer cells, often mediated through dendritic cells [8]. The process of oncolysis also leads to the release of tumor-associated antigens (TAAs) and heightened cytokine expression, recognized as potential mechanisms to enhance the therapeutic effectiveness of immune checkpoint blockade (ICB) in malignancies that typically exhibit poor response rates [9, 10]. Indeed, the combination of OVs with anti-PD-1 therapy has demonstrated both safety and a potent therapeutic response in melanoma patients [11]. Preclinical studies have demonstrated promising antitumor effects of oncolytic viruses in CRC [12,13,14]. In CRC patients, Garcia-Carbonero et al. found a noteworthy occurrence of high local CD8+T-cell infiltration in ~80% of tested CRC tumor samples following OVs treatment [15]. A phase-I/II study showed tolerable toxicities and potential clinical activity of virotherapy combined immunotherapy in MSS patients [16]. These findings have paved the way for several ongoing clinical trials investigating the synergy between OVs and ICB (such as NCT03256344, NCT02636036, and others). These endeavors aim to harness the full potential of OVs as a crucial component in the treatment of various cancers, including CRC, by optimizing the interaction between virotherapy and immunotherapy.
The oncolytic Human herpes virus type 2 (OH2) is genetically engineered to encode proteins within infected cells, specifically ICP34.5 (infected cell protein 34.5), while simultaneously deleting ICP47 [17]. ICP34.5 is a neurotoxic gene that has been removed to reduce viral toxicity and enhance its tumor selectivity. ICP47 interferes with the presentation of TAA by reducing the expression of major histocompatibility complex class I (MHC I) in infected cells [18]. The deletion of ICP47, in this context, leads to the upregulation of the US11 gene, a catalyst for viral oncolytic activity [19]. Previous studies have shown that OH2 can infect most human and mouse tumor cell lines and exhibit strong oncolytic activity [19]. OH2 also showed significant antitumor activity and safety in 4T1 and CT26 tumor animal models [19, 20].
Here, we preliminarily explored the therapeutic effect of intratumorally injection of OH2 combined with LP002 (anti-PD-L1 antibody) among CRLM patients in a phase-I study and elucidated the underlying molecular mechanisms which may contribute to the sustained response. Furthermore, through ongoing dynamic monitoring and analysis of peripheral blood samples from the responding patient, we aimed to identify early biomarkers that could serve as predictive indicators for treatment effectiveness.
Results
Combined ICB and OVs therapy achieved long-term clinical efficacy in one heavily pretreated CRC patient
Between January 11, 2021 and July 7, 2021, one phase-I clinical trial (NCT04755543) enrolling heavily pretreated advanced MSS mCRC patients proceeded in our center. The treatment regimen including intratumorally injection of oncolytic virus OH2 and intravenous injection of anti-PD-L1 antibody LP002, both of them repeated every 2 weeks, and tumor assessments were performed every 6 weeks until disease progression or unbearable adverse events. The treatment process is shown in Fig. 1A. One responding patient and three non-responding patients in this study were enrolled for further mechanism exploration. The baseline characteristics, tumor burden, doses of virus, treatment response, and survival data of these four patients are shown in Supplementary Table 1. The average age of patients is 61 years, ranging from 54 to 68 years old. All enrolled patients are male. And all patients had left-side primary tumors. Enrolled patients had target liver metastases for virus injection, including two patients with peritoneal metastases, and one patient had lung metastasis. All patients had received two or more lines of systemic treatment before (Supplementary Table S1).
A Study overview, depicting the treatment protocol for patients with colorectal cancer (CRC). B CT scan at baseline, week 6 and week 12 of responded patient. C Progression-free survival (PFS) and overall survival (OS) of all enrolled patients, the responding patient achieved long progression-free survival (313 days). D Target lesions size changes in four enrolled patients during treatment, the responding patient had a 35.9% tumor remission.
The responding patient demonstrated a remarkably effective response, achieving a prolonged and substantial partial response (PR) during treatment, as prominently depicted in Fig. 1B. In contrast, the remaining three patients experienced disease progression after the initial assessment and consequently discontinued treatment. Further investigation and analysis of gene expression were focused on the responding (R) patient and three non-responding (NR) patients who participated in the study (Fig. 1C). Impressively, the patient with the partial response experienced a remarkable treatment duration of 313 days, accompanied by an extended overall survival (OS) of 499 days (Fig. 1C). In contrast, the median OS for non-responding patients was 181 days. According to RESCIST criteria, a 20% increase in the size of the tumor is considered as disease progression, and a 30% decrease is considered as partial remission. A comprehensive view of changes in tumor burden across all enrolled patients was shown in Fig. 1D, the responding patients had a 35.9% tumor remission. All four patients had fever after treatment, and the adverse events are described in Supplementary Table S2.
Genomic and transcriptomic signature correlates of treatment response in CRC tumors undergoing combined therapy
Considering that specific gene mutations can modulate tumor cells, potentially enhancing their immunogenicity or responsiveness to ICB therapies, such as mutations in the KRAS [21] and TP53 [22] genes, we conducted an analysis of the most frequently mutated driver genes in the tumor tissues of our patients through whole exome sequencing (WES), and identified top three mutated genes closely associated with CRC tumorigenesis. We found that mutations in APC were detected in all four patients’ tissue samples, and mutations in TNN occurred in 75% (3/4) of the patients. (Fig. 2A). The prevalence of these mutations highlights their potential role in the pathogenesis of CRC and provides insights into the development of targeted therapeutic strategies, including the application of ICB therapies tailored to these genetic alterations.
A Baseline WES results of one responder (R) and three non-responders (NR1, NR2, NR3), showing the mutation frequencies across different genes. B, C The proportion of different gene mutation types in the responder patient and non-responded patient. D Missense mutation number in responded and non-responded patients. E Number of Snvs with allelic frequency greater than 10% in four enrolled patients. F–H Baseline metrics including MSI score, TMB and maximum allelic frequency in the four patients. I–L Higher gene expression in the responder patient for pathways related to virus replication and cell entry, tumor metabolism, degradation of extracellular matrix, and impaired pre-existing immunity. M KEGG pathway analysis of baseline RNA-seq data. N GO analysis of baseline RNA-seq data, providing insights into the biological processes, molecular functions, and cellular components involved.
Noteworthy is tumor suppressor gene TP53, although patients with TP53mut often have a poor prognosis [23], the role of TP53mut in response to ICB is controversial. For example, in a recent meta-analysis combining six WES data sets across cancer types, TP53mut was a negative predictor of ICB response [24]. By contrast, TP53/KRAS co-mutated non-small cell lung cancer patients tend to benefit from PD-L1 blockage, while KRAS mutation patients without additional TP53 mutation did not [25]. In TP53mut triple-negative breast cancer models, restoration of TP53 activity can sensitize the PD-L1/PD1 axis [26]. Altogether, the associations between TP53mut and ICB therapy response have not been clearly investigated. Our data showed that the TP53 mutation were both found in R and NR pretreatment tumors (Fig. 2A). Specifically, TP53 mainly showed nonsense mutation in the responder while showing missense mutation in other non-responders (Fig. 2A). The nonsense mutation of p53 mainly leads to premature termination of translation and expression of truncated unstable and non-functional p53 protein [27], while missense mutation mainly result in single amino acid substitutions in p53 and partial dysfunction [28]. Whether the nonsense mutation pattern results in more genomic instability or lead to different molecular biological features which are more associated with the beneficial effect of ICB response needs further exploration.
To further dissect whether responding and non-responding patients exhibit distinct DNA mutation profiles, we employed WES analysis and identified a total of 978 nonsynonymous somatic mutations in the tumor tissue from four pretreatment tumors, of which 399 mutations in R patient and 138 mutations,160 mutations and 281mutations in there NR patients, respectively (Fig. 2B, C). The mutation gene number for each patient was similar to a previous study in CRC patients [29]. Generally, the majority of genomic mutations observed in both responder and non-responders are missense mutations, accounting for 86.36% in responders and 92.48% in non-responders (Fig. 2D). However, it is noteworthy that responders exhibited a threefold higher frequency of nonsense mutations (5.70%) compared to non-responders (1.75%) (Fig. 2B). Furthermore, our analysis revealed that the pretreatment tumor of responders contained twofold single-nucleotide variants (SNVs) with allelic frequencies exceeding 10 compared to non-responders, suggesting that responders may generate a greater abundance of patient-specific neoantigens (Fig. 2E).
Tumor mutational burden (TMB) quantifies the total number of somatic nonsynonymous mutations within the coding region of a tumor’s genome. Tumors with high TMB are generally considered more immunogenic, increasing the likelihood of a favorable response to immune checkpoint blockade (ICB) due to the elevated presence of neoantigens [21, 22]. However, TMB is not an ideal biomarker to predict ICB response in MSS colon cancer, as these patients often exhibit a relatively low TMB [30]. In alignment with this observation, our cohort analysis employing WES with matched germline blood on pretreatment metastatic tumors, revealed that both responder and non-responders exhibited low microsatellite instability (MSI) scores (less than 0.015) (Fig. 2F) according to the previous study [31], and TMB values lower than 8 mutations per mutation/Mb (Fig. 2G). Notably, although the responder showed marginally higher TMB than the non-responders, overall TMB levels across the cohort remained modest (Fig. 2G). Furthermore, we examined another critical indicator known as Maximum Allele Frequency (MAX AF). MAX AF represents the highest observed frequency of a specific genetic variant (mutation) within the sequenced exome. MAX AF showed similarity between the R and NR group, which may not necessarily preclude the contribution of the initial genetic variant’s role in determining the response of ICB considering the sample size and specificity (Fig. 2H).
In addition to mutation patterns, we conducted a comprehensive examination of intratumoral transcriptomic alterations related to immunotherapy in CRLM patients before treatment. Through bulk RNA sequencing analysis, we identified several pathways significantly enriched in the responding patient. These include pathways related to virus replication and cellular entry (Fig. 2I), tumor metabolism (Fig. 2J), extracellular matrix degradation (Fig. 2K), and an impaired innate immune response (Fig. 2L). Notably, within the virus replication and cell entry pathway, we observed a marked upregulation of genes such as GSTA2, PRSS21, SLC10A1, GSTM, AKR1C4, and CCDC152 in the responding patient. These genes, known to be expressed as cellular entry receptors in tumor cells, appear to facilitate enhanced virus replication and penetration capacity [32,33,34]. In addition, genes including GSTA2, SRD, CYP3A7, GNMT, SLC10A1, BARX1, and AKR1C4, highly expressed in responding patients, were associated with tumor metabolism, known to enhance viral activity [32, 35]. These interactions can alter cellular phenotypes and energy utilization, impacting viral replication. Furthermore, we observed high expression of genes related to extracellular matrix (ECM) degradation such as PRSS21, SPP2, and AKR1C4 in responding patient. The ECM plays a crucial role in cellular communication, mechanical signal transduction, and adhesion substrate [36]. The degradation of ECM can facilitate oncolytic virus spread and improve their function [37]. In addition, GSTM and F13B have been found to undermine the pre-existing innate immune response, primarily mediated by B cells and NK cells. This impairment of the innate immune defense, which ordinarily acts as a barrier to viral replication in tumors, consequently, facilitates enhanced viral replication within the tumor microenvironment [38, 39].
Next, we also conducted an in-depth analysis of the molecular and biological functions of R tumor by KEGG and GO analysis. Notably, the KEGG analysis showed that R tumor encompassed the metabolism of xenobiotics by cytochrome P450, steroid hormone biosynthesis, and retinol metabolism (Fig. 2M). Concurrently, Gene Ontology (GO) analysis elucidated that R tumor was significantly enriched in lipoprotein-related cells. This enrichment bore close relevance to the fundamental biological functions and pathways associated with amino acid, carbohydrate, and lipid metabolism (Fig. 2N). Collectively, the responding CRLM patient exhibited a distinctive gene signature, which may be more conducive for the virus to enter and replicate in tumor, suggesting a potential facilitation of oncolytic virus replication and spread within the tumor milieu, thereby potentially enhancing the efficacy of ICB.
The CRC tumor responding to combined therapy exhibited an “immunologically cold” profile
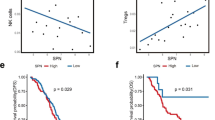
Previous clinical studies suggest that MSS CRC is insensitive to immunotherapy monotherapy and reported treatment response rate is 0% [40, 41], which may be attributed to the inherently cold immune microenvironment characterized by low T lymphocyte infiltration [42]. Consistently, by deconvolution analysis of immune cells, including the abundance of CD8+ T cells, CD4+ T cells, B cells, and myeloid cells, using RNA sequencing data, all four enrolled CRC patients exhibited a cold immune feature before treatment. Particularly noteworthy is that the sole responding patient demonstrated the lowest levels of T-cell and NK cell infiltration compared to the other three non-responding patients (Fig. 3A). Specifically, non-responding patients exhibited higher abundances of NK cells, CD8+ naive T cells, CD4+ naive T cells, and CD4+ Th1 cells than responding patient (Fig. 3B–F). Conversely, the responding patient exhibited lower infiltration of T cells and NK cell subsets, but a higher presence of macrophages, including both M1 and M2 types, compared to non-responding patients (Fig. 3G–J). This suggests that the combination therapy can be effective even in certain CRC tumors that are highly immune-cold. Overall, our findings indicate that oncolytic viruses might convert immunologically cold tumor microenvironments into hot ones, thereby increasing the responsiveness of CRC tumors to anti-PD-1 therapy.
A Baseline immune cells infiltration map in four patients, showing the distribution of various immune cell types. B The abundance of NK cells between the responder and non-responders. C–F The counts of different T-cell subtypes including CD4+ Th1, CD4+ naive, CD8+ naive, and CD4+ central memory T cells in responder and non-responders. G–J The abundance of macrophages (total), M1, M2, and activated myeloid dendritic cells across the responder and non-responders. K–M Baseline TCR results in tissue and blood, presenting TCR metrics including tissue TCR, blood TCR, and the overlap between tissue and blood TCR repertoires. N–P Baseline TCR clonality and max frequency, and tissue/blood ratio of clonality and max frequency, illustrating TCR diversity (Shannon index), maximum frequency, and clonality in both tissue and blood samples. Q Difference of the number of neoantigens identified in responder and non-responder patients, indicating potential differences in immunogenicity.
The T-cell receptor (TCR) serves as the key antigen receptor on T cells, determining their specificities and playing a crucial role in T-cell activation through the recognition of HLA-antigen complexes [43]. One approach to study antitumor T-cell responses involves quantifying TCR repertoire, diversity, and clonality. The high abundance of TCR in the local tumor tissue signifies host immune response and tumor prognosis [44]. while TCR levels in the blood generally be used to reflect dynamic changes and early treatment response in patients [45]. In our study, we initially observed a more than twofold increase of the total detected TCR number in both tumor tissue and peripheral blood from responding patient compared to non-responding patients, which reflect more diverse T cells are accumulated in the responding patient (Fig. 3K, L). In addition, the degree of TCR overlap between blood and tissue was higher in responding patients (Fig. 3M). This indicates that, despite the responding patient having fewer T-cell infiltrates before treatment, their more diverse T-cell population displayed a heightened potential for further activation in response to tumor antigens, thereby enhancing their ability to exert antitumor functions. Moreover, our findings revealed a consistent pattern among all non-responding patients, where each individual exhibited significantly higher TCR clonality and maximum frequency in peripheral blood compared to paired tumor tissue (TCR tissue/blood <1). In contrast, in the responding patient, this trend was inverted, with peripheral blood TCR clonality and maximum frequency being significantly lower than in paired tumor tissue (TCR tissue/blood >1, Fig. 3N–P). This observed discrepancy is likely attributable to the presence of specific immune escape mechanisms within the tumor microenvironment of non-responding patients, which hinders the expansion and infiltration of diverse T cells from blood migrating into tumors. Collectively, our findings underscore the significance of maintaining a tissue/blood TCR number ratio by greater than 1 which might predict a more effective response to therapy.
In line with the increased diversity of T-cell receptor (TCR) observed in the responding tumor, the responding patient demonstrated a higher number of detected neoantigens within the tumor tissues (Fig. 3Q). When we assessed the baseline neoantigen count in both responding and non-responding patients, it became evident that the overall neoantigen levels in the tumor tissue of all four MSS patients consistently remained below 100 (Fig. 3Q). This level of neoantigens was notably lower when compared to immunotherapy-sensitive cases in melanoma and lung cancer [46]. This finding prompts further exploration into whether neoantigens could serve as potential prognostic indicators in MSS patients.
We also conducted histological PD-L1 staining on tissue samples of the four patients before treatment and found that all patients had negative Tumor cell Proportion Score (TPS). The Combined Positive Score (CPS) in R, NR1, NR2, and NR3 was 27%, 25%, 30%, and 25%, respectively (Fig. 4).
Combining OH2 with anti-PD-L1 elicits robust immune activation in the responsive CRC patient
To further characterize the alterations in the tumor immune microenvironment (TIME) of the responding patient, we collected tumor tissue samples from the responding patient at three critical time points: before treatment, at the 6th week, and at the 12th week of post-treatment. This methodology enabled a dynamic evaluation of the TIME’s evolution throughout the therapy. RNA sequencing analysis of these samples unveiled a significant transformation in the tumor’s immune landscape. Initially, the tumor exhibited an immunologically “cold” state, characterized by scant tumor-infiltrating lymphocytes. However, as treatment progressed, there was a shift toward a “hot” immune state, marked by increased infiltration of CD4+T cells, CD8+T cells, and B cells (Fig. 5A). These findings suggest a direct link between therapeutic response and activation of the TIME, reinforcing the concept that the treatment’s efficacy might be driven by an immunomodulatory mechanism.
A Dynamic changes of infiltrated immune cells in the responder over the treatment period are shown, with the distribution of various immune cell types at baseline (R), week 6 (R W6), and week 12 (R W12) post-treatment. B–H Trends of CD8+ T cells and CD4+ T cells and their subtypes in the responder, including CD8+ effector memory, CD8+, CD8+ central memory, CD8+ naive, CD4+ naive, CD4+ effector memory, and CD4+ central memory T cells. I–L Trends of B cells and their subtypes in the responder, including class-switched memory B cells, B cells, B-cell plasma, and B-cell memory.
In detail, CD8+ naive T cell can get activated upon stimulation by cognate antigen [47]. CD8+effector memory T cell directly possesses tumor cell killing ability and produces inflammatory factors to trigger an immune response [47]. CD8+Central Memory T-cell guarantee long-lasting immune memory in response [48]. In the case of the responding patient, we noted a significant increase in various CD8+T-cell subsets associated with antitumor immunity, with over a 20-fold rise observed by the 12th week of treatment (Fig. 5B–E). This increase underscores a gradual shift in the patient’s immune environment from a “cold” to a “hot” state. This shift was accompanied by an inflammatory response, likely triggered by oncolytic virus therapy, which attracted more immune cells into the tumor microenvironment. Moreover, significant upregulation of CD4+ cells, including CD4+ naive, effector and central memory T-cell subsets were also detected during the course of treatment in responding patient TMIE. CD4+ naive T cell can differentiate into various subsets of T helper (Th) cells upon different stimulation [49], which gradually elevated during the treatment in R patient. CD4+ effector memory T cells, known for their high activation potential and capacity to produce cytokines like IFN-γ and IL-17, play a pivotal role in assisting other immune cells in tumor control [48, 50]. Meanwhile, CD4+ central memory T cells are crucial for long-term immune memory and possess self-renewal capabilities [48, 50]. These two types of cells were both elevated during the treatment in R patient (Fig. 5F–H). These results suggest that various types of CD4+ cells were increased, which is helpful in response to immunotherapy. In addition, virotherapy was reported to produce a large number of antigens after tumor cell death and trigger antibody-dependent cytotoxicity (ADCC) and antibody-associated cytotoxicity (ADCP) induced by B cells. We also observed that B cell, plasma B cell, memory B cell, and Class-switched memory B cell are all elevated due to the treatment of OH2 and anti-PD-L1 (Fig. 5I–L), indicating OV may improve ADCC and ADCP effect to enhance antitumor immune function.
Dynamic monitoring of the tumor-specific immune signature predicts response to combination therapy
To ascertain potential intratumoral immune signature for monitoring the efficacy of our combination therapy, we conducted a dynamic assessment of the expression of immune-related genes within tumor tissues. Our results demonstrated that, with the advancement of treatment and the appearance of response, a marked increase of genes associated with T-cell activation (ZAP70, GATA3, EOMES, and T-BET) and effector functions (NFKBID and TBX21) were observed (Fig. 5A). Among them, ZAP70 is essential for initiating the early events of T-cell antigen receptor (TCR) signaling cascade to ensure proper T-cell activation and function [51]. And EOMES, RUNX3, T-BET, GATA3 were killing related transcription factors that can control the follicular location of CD8+ T cells and promote the homeostasis of CD8+ T cells [52,53,54]. The above genes closely associated with T-cell activation and cytotoxicity exhibited significant upregulation after 12 weeks of treatment in the responding patient (Fig. 6A). This increase in the expression of T-cell function-related genes indicates a substantial enhancement in the antitumor capabilities of T cells following treatment and underscores the effective antitumor role of the combination therapy. At the same time, the rise in these genes not only reflects enhanced therapeutic efficacy but also underscores their potential as precise indicators of treatment response.
A Increased expression of T-cell activation-associated genes in the responder. B–E GSEA analysis of T-cell activation and immune response pathways, showing enrichment scores for αβ T-cell differentiation, leukocyte chemotaxis, regulation of αβ T-cell activation, and regulation of adaptive immune response. F Dynamic changes of WES data in responder. G Dynamic changes of different gene mutation types in responder.
To further understand the pathways in which the major gene enrichment differences occurred after 12 weeks of treatment, we performed GSEA analysis for genes enriched during treatment. Our GSEA analysis revealed the activation of several critical pathways, including those related to Alpha Beta T-cell differentiation, regulation of Alpha Beta T-cell activation, adaptive immune response regulation, and leukocyte chemotaxis (Fig. 6B–E). These findings are closely associated with processes such as T-cell differentiation and activation, chemotaxis release, and immune response, providing robust evidence of dynamic activation of antitumor immune response in the tumor microenvironment throughout the treatment.
Remarkably, as the treatment progressed, we also observed a substantial reduction in the total number of genomic gene mutations, including the disappearance of TP53mut. It was reduced by half by week 6 and almost undetectable by week 12 (Fig. 6F). In particular, we observed a notable decrease in missense mutations and frameshift deletions by week 6 of treatment, and this trend persisted through week 12 (Fig. 6F). In addition, nonsense mutations, in-frame deletions, and splice site mutations were no longer detectable by week 6 (Fig. 6G). In summary, these findings provide further evidence that T cell undergo dynamic activation and play a role in the antitumor response during the combination treatment. The decrease of mutation gene at genetic level after treatment can be used as a dynamic indicator of monitoring response.
Blood ctDNA as early biomarker predicting responsive during OVs+anti-PD-L1 treatment
Circulating tumor DNA (ctDNA) in bodily fluids presents a minimally invasive method for diagnosing, characterizing, and monitoring cancer in individual patients. Reflecting the actual tumor burden and specific genomic status, ctDNA has potential as a prognostic and predictive biomarker for treatment [53]. In our study, a significant early decrease in ctDNA levels was observed in the blood of the responding (R) patient (Fig. 7A). By the 6th week, over half (19/32) of the ctDNA variants had disappeared in this patient, indicating an early response, and this reduction trend continued into week 12. Regarding mutation types, the predominant decrease in ctDNA was noted in missense mutations, while nonsense and frameshift mutations remained relatively unchanged (Fig. 7B–D). Research suggests that immunotherapy may be particularly effective early on for carriers of missense mutations, even in pre-cancerous lesions [54]. We also noted a change in the types of gene variations during treatment. Single-nucleotide variations (SNVs) consistently declined, while deletions (Del) and insertions (Ins) showed no significant change (Fig. 7E–G). SNVs are linked to neoantigens and patient-specific responses, suggesting their reduction could be a result of effective treatment [55]. However, the ctDNA Microsatellite Instability (MSI) score did not show a consistent pattern of change (Fig. 6H). The ctDNA Tumor Mutational Burden (TMB) and maximum frequency consistently decreased, reflecting the reduction of mutated genes throughout the treatment (Fig. 7I, J). These observations suggest that ctDNA levels can serve as an early indicator of therapeutic effectiveness. In addition, the dynamic changes in mutation types during treatment may be intricately linked to the effects of virotherapy and immunotherapy, warranting further investigation.
A Dynamic changes in ctDNA in the responder, showing the mutation frequencies across different genes at baseline (R W0), week 6 (R W6), and week 12 (R W12). B, E Number of ctDNA mutated genes and the corresponding mutation types detected at baseline. C, F Number of ctDNA mutated genes and the corresponding mutation types detected at week 6. D, G Number of ctDNA mutated genes and the corresponding mutation types detected at week 12. H–J Dynamic changes in ctDNA MSI score, ctDNA TMB, and maximum frequency in the responder over the treatment period.
Discussion
Immune checkpoint inhibitors have acquired remarkable efficacy in metastasis CRC that is mismatch-repair-deficient (dMMR) and microsatellite instability-high (MSI-H) [55]. However, dMMR/MSI-H CRC only accounts for no more than 5% of CRC population [4]. The remaining 95% of mCRC are all MSS subtype and respond poorly to immunotherapy. Therefore, there still remains a high unmet need for the development of immunotherapy for the vast majority of mismatch-repair-proficient (pMMR) or MSS mCRC. A variety of combination therapies have been tested for potential new strategies for MSS CRC, including ICIs combined with chemotherapy, radiotherapy, anti-VEGF tyrosine kinase inhibitor and virotherapy [56]. Strikingly, REGONIVO study [57] found that the combination of regorafenib (tyrosine kinase inhibitor) plus nivolumab had a 44% overall response rate (ORR) in colorectal cancer patients, while RIN [58] study demonstrated that regorafenib combined with nivolumab and ipilimumab can achieve 27.6% ORR in MSS CRC. However, a similar North American phase 2 study [59] found that regorafenib combined with nivolumab achieved only 7% ORR. And LEAP-017 trial [60] did not show an overall survival advantage with Lenvatinib plus pembrolizumab versus chemotherapy for MSS patients. MSS CRC still exists many challenges in the strategy of immune combination therapy and new treatment option still need further exploration. Moreover, virotherapy has shown success in melanoma and lung cancer in several studies by altering the TME [61, 62], and is considered an effective partner for immunotherapy [63]. Type 1 herpes simplex virus (HSV-1) has been extensively used in past clinical studies, showing significant benefits in patients with advanced melanoma [64]. The oncolytic virus derived from OH2 demonstrates superior antitumor efficacy by removing the immune-suppressive gene ICP47, expressing the immune-enhancing gene GM-CSF, and enhancing specific antitumor immune responses. Strong oncolytic activity and safety have been demonstrated in animal models treated with OH2 [20]. Clinically, 54 patients with various tumor types participated in the phase-I clinical trial of OH2, with no dose-limiting toxicities (DLT) observed. Among these patients, in the group with a dose of 108 CCID50/mL (the dose used in our current clinical trial), only one patient experienced a grade 3 adverse event of fever, indicating the safety of our clinical trial [65]. Therefore, in this study, we attempted to adjust TME of metastasis MSS CRC patient by local injection of OH2 in the liver and aim to improve the efficacy of immunotherapy.
We developed a phase-I clinical study and include a total of four patients and obtained one sustained response patient. A limitation of our work is the relatively small number of participants in the study and the number of response patients. Despite this, by comparing the tumor microenvironment of responding and non-responding patients before treatment, and by examining the dynamic changes in the TME of the R patient through multi-omics analysis, we have gained significant insights into the molecular mechanisms and potential efficacy biomarkers underpinning the combination of oncolytic virus therapy with immune checkpoint blockade.
OVs contributes to the reprogramming of the TME and are considered as an encouraging biocarrier that could be used in both natural and genetically engineered platforms to induce oncolysis in a targeted manner [66]. A combination of OV and ICIs tend to synergize the functional effects of ICIs and overcome its primary resistant barriers in solid tumors. In our study, we revealed that OV mediate the recruitment and activation of effector immune cells, marked by increasing infiltration of CD8+ T cells, CD4+ T cells and B cells during the course of treatment. According to a previous study, this could be triggered by the release of damage-associated molecular patterns and cytokines in the TME after OVs treatment [67]. Most studies focus on cell activation and neoantigen release by OVs [68]. In our study, through further analysis of potential mechanisms, we found that the expression of T-cell activation genes and immune cell function-related genes were upregulated consistently with treatment response, which has not been reported before. Notably, the responder also high abundance of M1 and M2-type macrophages, which is consistent with the immunophenotype of “cold” tumor. The TAMs display an ability to suppress T-cell recruitment and function as well as to regulate other aspects of tumor immunity [69]. Polarization of TAM is considered to be closely related to the effect of immunotherapy [70]. Indeed, the role of macrophages in the treatment of oncolytic virus is still controversial. It is reported that macrophages can support oncolytic virus therapy by stimulating antitumor response by proinflammatory macrophages and support oncolytic virus therapy by protecting viral replication by immunosuppression [71]. Our results support that the role of TAM in virotherapy may be positive. In addition, through the analysis of ctDNA and TCR, we have a more comprehensive understanding of the spectrum of combination therapy of OV and immunotherapy.
TCR clonality in blood and tissue reflects differences in immune cell status between the circulatory system and local tissues [72]. Previous studies have investigated peripheral TCR spectrums in patients with prostate cancer or melanoma treated with anti-CTLA-4 therapy, revealing an improved survival with T-cell clonotype stability after anti-CTLA-4 treatment [73]. Studies in melanoma patients receiving anti-PD-1 therapy have shown that patients with high levels of tumor-infiltrating lymphocytes (TIL) and high TIL clonality in tumor tissue are more likely to have radiological responses to treatment [74]. In smaller sample sizes, studies on urothelial tumors and populations receiving checkpoint blockade therapy have indicated that patients with low peripheral TCR clonality and high tumor clonality have better prognoses [75]. Based on the studies already reported above, we observed a similar correlation between TCR and immunotherapy response in our small sample study. We speculate that an increased tissue/blood TCR ratio may be used as a new indicator to predict a better immune response and may benefit more from combination therapy with oncolytic viruses and immune checkpoint inhibitors. The discrepancy between TCR number and TCR clonality can be attributed to several immune escape mechanisms that cancer cells employ to evade the immune response, such as antigen heterogeneity and variation, T-cell exhaustion and immune editing [76]. This can result in a reduction of immunogenic tumor antigens over time, causing a decline in the diversity of the TCR repertoire. We found that the abundance of exhausted T cells gradually increased as treatment continued in the responded patient, which is consistent with the evidence above.
As is well known, ctDNA has been widely utilized in the clinical exploration of tumor immunotherapy [77] and has been employed for predicting immune checkpoint blockade and distinguishing unique patterns of immune checkpoint blockade response [78], assessing response prediction in immunotherapy, and early detection of treatment resistance [79]. Up to now, there have been no large-sample clinical trials to prove whether ctDNA can predict the efficacy of ICB + OV treatment in CRC patients. However, in our clinical trial, we were surprised to find a trend of significantly decreased ctDNA mutations in the early stages of treatment in the R group of patients. This suggests that ctDNA may be applicable in evaluating the efficacy of oncolytic virus combined with immune checkpoint inhibitor therapy. We innovatively propose the predictive value of tissue/blood ratio for the complementary effects of oncolytic viruses and immune checkpoint inhibitors. The differences in TCR and clonality between circulation and tissue have been widely accepted as predictors of immunotherapy. For example, the peripheral TCR repertoire in patients with canine cancer or melanoma treated with CTLA-4 therapy predicts prognosis [73]; and the TCR repertoire in tumor tissue of melanoma patients treated with anti-PD-1 therapy predicts treatment response [74]. In conclusion, both ctDNA and TCR serve as predictive factors for treatment response.
However, the the number of patients included in this study is limited. A total of four patients underwent the multi-omics analysis. The results may be influenced by factors such as tumor genetic heterogeneity, immune microenvironment, tumor cell signaling pathways, and individual immune status of patients. Differences in genomic variations, mutations, and expression patterns within different patients may lead to differences in tumor cell sensitivity to treatment drugs; factors such as immune cell density, inflammation level, and expression levels of immune inhibitory factors in the tumor microenvironment may affect tumor response to immunotherapy.
In recent years, there is increasing evidence for the efficacy of oncolytic viruses in the treatment of glioblastoma, liver cancer and malignant pleural mesothelioma [80,81,82,83]. Clinical trial of OV in CRC patients is still rare, our findings in this phase-I study are helpful for further potential expansion of multi-omics guided phase II study for heavily treated advanced CRC patients, especially in liver metastasis disease. In the future, engineered OV, such as engineered HSV expressing GM-CSF, could further improve oncolysis activity and kill cancer cells in a targeted manner [84]. In addition, OV combined with other immunotherapy, such as CAR-T cells and cytokines, could be a new treatment strategy for solid tumor since OV-mediated reprogrammed TME can also improve function of tumor-reactive CAR-T cells [85] and be enhanced by the application of cytokines [86]. Together, OV has a promising application prospect in the treatment of CRC, and our study provides evidence for OV to improve the immune microenvironment.
Materials and methods
Clinical trial and specimens
This study was based on a phase-I clinical trial of oncolytic virus OH2 and anti-PD-L1 antibody LP002 in malignant digestive tract tumors (NCT04755543). LP002 injection was a fixed dose of 900 mg, and OH2 injection was injected as 108 CCID50/ml in all four patients. Safety and tolerability assessments in this clinical trial were conducted following the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI-CTCAE) version 4.03, including the observation of dose-limiting toxicities (DLT). We considered adverse events of grade 3 or higher non-hematologic toxicity and grade 4 or higher hematologic toxicity occurring within 2 weeks after the first dose administration to be DLTs, also known as “unbearable adverse events.” Generally, assessments were conducted every 6 weeks, and the dosage in our study referred to a previous clinical study.
OH2 was injected in liver metastases (diameter ≤1.5 cm, maximum 1 mL; >1.5 cm to ≤2.5 cm maximum injection of 2 mL; >2.5 cm to ≤5.0 cm, maximum injection of 4 mL; >5 cm was injected with a maximum of 8 mL at a concentration of 108 CCID50/mL), and LP002 (900 mg) was intravenously infused within 60 min ( ± 15 min) within 24 h after OH2 (Fig. 1A). Treatment repeated every 2 weeks until confirmed PD by immune-related Response Evaluation Criteria in Solid Tumors (irRECIST) criteria [87], adverse reaction intolerance or end of study. Imagine efficacy evaluation repeated every 6 weeks. Liver metastases biopsy was performed at baseline and every 6 weeks after imaging evaluation.
Enrolled patients were histologically confirmed patients with advanced colorectal cancer who had failed at least second-line standard therapy, had an ECOG score of 0-1, expected survival of more than 3 months, and had measurable lesions and appropriate organ function. Primary exclusion criteria were prior ICIs use, active autoimmune disease, active hepatitis, intestinal obstruction, intestinal bleeding, and symptomatic brain metastases.
WES sequencing
gDNA was extracted from fresh tissue samples and white blood cells. Fragmented DNA was used for library construction with the KAPA DNA Library Preparation Kit (Kapa Biosystems, Wilmington, MA, USA). Sequencing libraries were constructed utilizing the KAPA DNA Library Preparation Kit (Kapa Biosystems, Wilmington, MA, USA) per the manufacturer’s instructions. Barcoded libraries were subsequently hybridized to WES for the tissue gDNA. DNA sequencing was performed with the Geneplus-2000 sequencing platform (Geneplus, Beijing, China) with 2 × 100 bp paired-end reads.
TCR (T-cell receptor) sequencing
DNA from the tissue and peripheral blood lymphocyte samples was amplified using a multiplex PCR panel and sequenced on the Geneplus-2000 sequencing platform (Geneplus). The sequences were compared with the ImMunoGeneTics (IMGT) database by MIXCR software to identify the CDR3 sequence. To normalize the data volume, 106 qualified reads of were randomly selected to analysis for every sample. The diversity of the TCR repertoire was calculated on the basis of the Shannon–Wiener index (Shannon index), which scaled from 0 to 10:
where pi refers to the frequency of clonotype i for the sample with n unique clonotypes. Clonality can be considered as a normalized Shannon index over n unique clones:
RNA sequencing
RNA was extracted from fresh tissues using the TRIzol and RNeasy MinElute Cleanup Kit (Invitrogen). The libraries were prepared with the NEB Next® Ultra™ RNA Library Prep Kit (NEB, Beverly, MA, USA). The libraries were sequenced on the Geneplus-2000 sequencing platform (Geneplus, Beijing, China).
CIBERSORT was applied to quantify the percentage of different types of tumor-infiltrating cells (TICs) with RNA-seq data. We estimated the immune infiltration of each sample with the LM22 signature file, which can define 22 subtypes of immune cells. ssGSEA was used to estimate the activity score of the T-cell exhaustion (TEX) in each patient with a previously reported TEX-related gene set.
ctDNA sequencing
Circulating free DNA (cfDNA) was extracted using a DNeasy Blood Kit (Qiagen, Hilden, Germany) and QIAamp Circulating Nucleic Acid Kit (Qiagen). Sequencing libraries were constructed utilizing the KAPA DNA Library Preparation Kit (Kapa Biosystems, Wilmington, MA, USA) per the manufacturer’s instructions. Barcoded libraries were subsequently hybridized to a customized panel of 1021 genes for cfDNA.
Mutation calling
The initial sequencing data underwent a dual-step cleaning process, first by removing terminal adapter sequences with NCrealSeq (version 1.2.0), followed by the selection of high-quality reads using NCfilter (version 2.0.0). Subsequently, these cleaned reads were aligned to the reference human genome (GRCh37) utilizing the Burrows-Wheeler Aligner (BWA, version 0.7.15-r1140). Duplicate reads were flagged using realSeq, and normal samples were identified with Picard tools (version 2.6.0). Single-nucleotide variants (SNVs) and small insertions and deletions (indels) were detected by TNSCOPE (version 201808) and realDcaller (version 1.7.1), an in-house software for reviewing hotspot variants. The findings from these analyses were consolidated using NChot (version 2.7.2) and then annotated with reference to various public databases through NCanno (version 1.1.3). Copy number variations (CNVs) were identified with CNVKIT (version 0.9.2). In addition, an in-house algorithm, NCSV (version 0.2.3), was employed to pinpoint split-read and discordant read-pair signatures indicative of structural variations (SVs).
Data availability
Raw sequencing data generated in this study are deposited in the Genome Sequence Archive for Human (https://ngdc.cncb.ac.cn/gsa-human/) with accession number subHRA008991.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7–33.
Done JZ, Fang SH. Young-onset colorectal cancer: a review. World J Gastrointest Oncol. 2021;13:856–66.
Argiles G, Tabernero J, Labianca R, Hochhauser D, Salazar R, Iveson T, et al. Localised colon cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;31:1291–305.
Overman MJ, Ernstoff MS, Morse MA. Where we stand with immunotherapy in colorectal cancer: deficient mismatch repair, proficient mismatch repair, and toxicity management. Am Soc Clin Oncol Educ Book. 2018;38:239–47.
Creasy JM, Sadot E, Koerkamp BG, Chou JF, Gonen M, Kemeny NE, et al. Actual 10-year survival after hepatic resection of colorectal liver metastases: what factors preclude cure? Surgery. 2018;163:1238–44.
Yu J, Green MD, Li S, Sun Y, Journey SN, Choi JE, et al. Liver metastasis restrains immunotherapy efficacy via macrophage-mediated T cell elimination. Nat Med. 2021;27:152–64.
Engeland CE, Bell JC. Introduction to oncolytic virotherapy. Methods Mol Biol. 2020;2058:1–6.
Kim Y, Clements DR, Sterea AM, Jang HW, Gujar SA, Lee PW. Dendritic cells in oncolytic virus-based anti-cancer therapy. Viruses. 2015;7:6506–25.
Berkey SE, Thorne SH, Bartlett DL. Oncolytic virotherapy and the tumor microenvironment. Adv Exp Med Biol. 2017;1036:157–72.
Harrington K, Freeman DJ, Kelly B, Harper J, Soria JC. Optimizing oncolytic virotherapy in cancer treatment. Nat Rev Drug Discov. 2019;18:689–706.
Ribas A, Dummer R, Puzanov I, VanderWalde A, Andtbacka RHI, Michielin O, et al. Oncolytic virotherapy promotes intratumoral T cell infiltration and improves anti-PD-1 immunotherapy. Cell. 2018;174:1031–2.
Crupi MJF, Taha Z, Janssen TJA, Petryk J, Boulton S, Alluqmani N, et al. Oncolytic virus driven T-cell-based combination immunotherapy platform for colorectal cancer. Front Immunol. 2022;13:1029269.
Luo Q, Song H, Deng X, Li J, Jian W, Zhao J, et al. A triple-regulated oncolytic adenovirus carrying microRNA-143 exhibits potent antitumor efficacy in colorectal cancer. Mol Ther Oncolytics. 2020;16:219–29.
Ren Y, Miao JM, Wang YY, Fan Z, Kong XB, Yang L, et al. Oncolytic viruses combined with immune checkpoint therapy for colorectal cancer is a promising treatment option. Front Immunol. 2022;13:961796.
Garcia-Carbonero R, Salazar R, Duran I, Osman-Garcia I, Paz-Ares L, Bozada JM, et al. Phase 1 study of intravenous administration of the chimeric adenovirus enadenotucirev in patients undergoing primary tumor resection. J Immunother Cancer. 2017;5:71.
Monge C, Xie C, Myojin Y, Coffman K, Hrones DM, Wang S, et al. Phase I/II study of PexaVec in combination with immune checkpoint inhibition in refractory metastatic colorectal cancer. J Immunother Cancer. 2023;11, https://doi.org/10.1136/jitc-2022-005640.
Hu H, Zhang S, Cai L, Duan H, Li Y, Yang J, et al. A novel cocktail therapy based on quintuplet combination of oncolytic herpes simplex virus-2 vectors armed with interleukin-12, interleukin-15, GM-CSF, PD1v, and IL-7 x CCL19 results in enhanced antitumor efficacy. Virol J. 2022;19:74.
Sethumadhavan S, Barth M, Spaapen RM, Schmidt C, Trowitzsch S, Tampe R. Viral immune evasins impact antigen presentation by allele-specific trapping of MHC I at the peptide-loading complex. Sci Rep. 2022;12:1516.
Zhao Q, Zhang W, Ning Z, Zhuang X, Lu H, Liang J, et al. A novel oncolytic herpes simplex virus type 2 has potent anti-tumor activity. PLoS ONE. 2014;9:e93103.
Zhang W, Hu X, Liang J, Zhu Y, Zeng B, Feng L, et al. oHSV2 can target murine colon carcinoma by altering the immune status of the tumor microenvironment and inducing antitumor immunity. Mol Ther Oncolytics. 2020;16:158–71.
Edin S, Gylling B, Li X, Stenberg A, Lofgren-Burstrom A, Zingmark C, et al. Opposing roles by KRAS and BRAF mutation on immune cell infiltration in colorectal cancer—possible implications for immunotherapy. Br J Cancer. 2023. https://doi.org/10.1038/s41416-023-02483-9.
Sacconi A, Muti P, Pulito C, Urbani G, Allegretti M, Pellini R, et al. Immunosignatures associated with TP53 status and co-mutations classify prognostically head and neck cancer patients. Mol Cancer. 2023;22:192.
Toshida K, Itoh S, Iseda N, Izumi T, Yoshiya S, Toshima T, et al. Impact of TP53-induced glycolysis and apoptosis regulator on malignant activity and resistance to ferroptosis in intrahepatic cholangiocarcinoma. Cancer Sci. 2023. https://doi.org/10.1111/cas.15981.
Gajic ZZ, Deshpande A, Legut M, Imielinski M, Sanjana NE. Recurrent somatic mutations as predictors of immunotherapy response. Nat Commun. 2022;13:3938.
Zhang C, Wang K, Lin J, Wang H. Non-small-cell lung cancer patients harboring TP53/KRAS co-mutation could benefit from a PD-L1 inhibitor. Future Oncol. 2022;18:3031–41.
Yang Z, Sun JK, Lee MM, Chan MK. Restoration of p53 activity via intracellular protein delivery sensitizes triple negative breast cancer to anti-PD-1 immunotherapy. J Immunother Cancer. 2022;10. https://doi.org/10.1136/jitc-2022-005068.
Albers S, Allen EC, Bharti N, Davyt M, Joshi D, Perez-Garcia CG, et al. Engineered tRNAs suppress nonsense mutations in cells and in vivo. Nature. 2023;618:842–8.
Cheng J, Novati G, Pan J, Bycroft C, Zemgulyte A, Applebaum T, et al. Accurate proteome-wide missense variant effect prediction with AlphaMissense. Science. 2023;381:eadg7492.
Srivastava AK, Wang Y, Huang R, Skinner C, Thompson T, Pollard L, et al. Human genome meeting 2016 : Houston, TX, USA. 28 February - 2 March 2016. Hum Genomics. 2016;10:12.
Westcott PMK, Sacks NJ, Schenkel JM, Ely ZA, Smith O, Hauck H, et al. Low neoantigen expression and poor T-cell priming underlie early immune escape in colorectal cancer. Nat Cancer. 2021;2:1071–85.
Middha S, Zhang L, Nafa K, Jayakumaran G, Wong D, Kim HR, et al. Reliable Pan-cancer microsatellite instability assessment by using targeted next-generation sequencing data. JCO Precis Oncol. 2017. https://doi.org/10.1200/PO.17.00084.
Cho IJ, Ki SH, Brooks C 3rd, Kim SG. Role of hepatitis B virus X repression of C/EBPbeta activity in the down-regulation of glutathione S-transferase A2 gene: implications in other phase II detoxifying enzyme expression. Xenobiotica. 2009;39:182–92.
Yamashita M, Honda A, Ogura A, Kashiwabara S, Fukami K, Baba T. Reduced fertility of mouse epididymal sperm lacking Prss21/Tesp5 is rescued by sperm exposure to uterine microenvironment. Genes Cells. 2008;13:1001–13.
Jakovljevic A, Nikolic N, Carkic J, Beljic-Ivanovic K, Soldatovic I, Miletic M, et al. Association of polymorphisms in TNF-alpha, IL-1beta, GSTM and GSTT genes with apical periodontitis: is there a link with herpesviral infection? Int Endod J. 2020;53:895–904.
Johnson N, De Ieso P, Migliorini G, Orr N, Broderick P, Catovsky D, et al. Cytochrome P450 allele CYP3A7*1C associates with adverse outcomes in chronic lymphocytic leukemia, breast, and lung cancer. Cancer Res. 2016;76:1485–93.
Rozario T, DeSimone DW. The extracellular matrix in development and morphogenesis: a dynamic view. Dev Biol. 2010;341:126–40.
Alsisi A, Eftimie R, Trucu D. Nonlocal multiscale modelling of tumour-oncolytic viruses interactions within a heterogeneous fibrous/non-fibrous extracellular matrix. Math Biosci Eng. 2022;19:6157–85.
Lee M, Chang Y, Ahmadinejad N, Johnson-Agbakwu C, Bailey C, Liu L. COVID-19 mortality is associated with pre-existing impaired innate immunity in health conditions. PeerJ. 2022;10:e13227.
Saalbach A, Tremel J, Herbert D, Schwede K, Wandel E, Schirmer C, et al. Anti-inflammatory action of keratinocyte-derived vaspin: relevance for the pathogenesis of psoriasis. Am J Pathol. 2016;186:639–51.
Le DT, Uram JN, Wang H, Bartlett BR, Kemberling H, Eyring AD, et al. PD-1 blockade in tumors with mismatch-repair deficiency. New Engl J Med. 2015;372:2509–20.
O’Neil BH, Wallmark JM, Lorente D, Elez E, Raimbourg J, Gomez-Roca C, et al. Safety and antitumor activity of the anti-PD-1 antibody pembrolizumab in patients with advanced colorectal carcinoma. PLoS ONE. 2017;12:e0189848.
Moretto R, Rossini D, Catteau A, Antoniotti C, Giordano M, Boccaccino A, et al. Dissecting tumor lymphocyte infiltration to predict benefit from immune-checkpoint inhibitors in metastatic colorectal cancer: lessons from the AtezoT RIBE study. J Immunother Cancer. 2023;11. https://doi.org/10.1136/jitc-2022-006633.
Szeto C, Lobos CA, Nguyen AT, Gras S. TCR Recognition of peptide-MHC-I: rule makers and breakers. Int J Mol Sci. 2020;22. https://doi.org/10.3390/ijms22010068.
Li R, Wang J, Li X, Liang Y, Jiang Y, Zhang Y, et al. T-cell receptor sequencing reveals hepatocellular carcinoma immune characteristics according to Barcelona Clinic liver cancer stages within liver tissue and peripheral blood. Cancer Sci. 2023. https://doi.org/10.1111/cas.16013.
Chen YT, Hsu HC, Lee YS, Liu H, Tan BC, Chin CY, et al. Longitudinal high-throughput sequencing of the T-cell receptor repertoire reveals dynamic change and prognostic significance of peripheral blood TCR diversity in metastatic colorectal cancer during chemotherapy. Front Immunol. 2021;12:743448.
Schumacher TN, Scheper W, Kvistborg P. Cancer neoantigens. Annu Rev Immunol. 2019;37:173–200.
Gerritsen B, Pandit A. The memory of a killer T cell: models of CD8(+) T cell differentiation. Immunol Cell Biol. 2016;94:236–41.
Ando M, Ito M, Srirat T, Kondo T, Yoshimura A. Memory T cell, exhaustion, and tumor immunity. Immunol Med. 2020;43:1–9.
Moon JJ, Chu HH, Pepper M, McSorley SJ, Jameson SC, Kedl RM, et al. Naive CD4(+) T cell frequency varies for different epitopes and predicts repertoire diversity and response magnitude. Immunity. 2007;27:203–13.
Kunzli M, Masopust D. CD4(+) T cell memory. Nat Immunol. 2023;24:903–14.
Li J, Liang W, Li K, Jiao X, Ai K, Zhang Y, et al. ZAP70 activation is an early event of T cell immunity that involved in the anti-bacterial adaptive immune response of Nile tilapia. Dev Comp Immunol. 2021;124:104177.
Mishra S, Liao W, Liu Y, Yang M, Ma C, Wu H, et al. TGF-beta and Eomes control the homeostasis of CD8+ regulatory T cells. J Exp Med. 2021;218. https://doi.org/10.1084/jem.20200030.
Boto P, Csuth TI, Szatmari I. RUNX3-mediated immune cell development and maturation. Crit Rev Immunol. 2018;38:63–78.
Szabo SJ, Kim ST, Costa GL, Zhang X, Fathman CG, Glimcher LH. A novel transcription factor, T-bet, directs Th1 lineage commitment. Cell. 2000;100:655–69.
Diaz LA Jr., Shiu KK, Kim TW, Jensen BV, Jensen LH, Punt C, et al. Pembrolizumab versus chemotherapy for microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer (KEYNOTE-177): final analysis of a randomised, open-label, phase 3 study. Lancet Oncol. 2022;23:659–70.
Wang D, Zhang H, Xiang T, Wang G. Clinical application of adaptive immune therapy in mss colorectal cancer patients. Front Immunol. 2021;12:762341.
Fukuoka S, Hara H, Takahashi N, Kojima T, Kawazoe A, Asayama M, et al. Regorafenib plus nivolumab in patients with advanced gastric or colorectal cancer: an open-label, dose-escalation, and dose-expansion phase Ib trial (REGONIVO, EPOC1603). J Clin Oncol. 2020;38:2053–61.
Fakih M, Sandhu J, Lim D, Li X, Li S, Wang C. Regorafenib, ipilimumab, and nivolumab for patients with microsatellite stable colorectal cancer and disease progression with prior chemotherapy: a phase 1 nonrandomized clinical trial. JAMA Oncol. 2023;9:627–34.
Fakih M, Raghav KPS, Chang DZ, Larson T, Cohn AL, Huyck TK, et al. Regorafenib plus nivolumab in patients with mismatch repair-proficient/microsatellite stable metastatic colorectal cancer: a single-arm, open-label, multicentre phase 2 study. EClinicalMedicine. 2023;58:101917.
Kawazoe A, Xu RH, Garcia-Alfonso P, Passhak M, Teng HW, Shergill A, et al. Lenvatinib Plus Pembrolizumab Versus Standard of Care for Previously Treated Metastatic Colorectal Cancer: Final Analysis of the Randomized, Open-Label, Phase III LEAP-017 Study. J Clin Oncol. 2024. https://doi.org/10.1200/JCO.23.02736.
Wang C, Lu N, Yan L, Li Y. The efficacy and safety assessment of oncolytic virotherapies in the treatment of advanced melanoma: a systematic review and meta-analysis. Virol J. 2023;20:252.
Li Z, Feiyue Z, Gaofeng L, Haifeng L. Lung cancer and oncolytic virotherapy–enemy’s enemy. Transl Oncol. 2023;27:101563.
Wang Z, Sun P, Li Z, Xiao S. Clinical advances and future directions of oncolytic virotherapy for head and neck cancer. Cancers. 2023;15. https://doi.org/10.3390/cancers15215291.
Andtbacka RH, Kaufman HL, Collichio F, Amatruda T, Senzer N, Chesney J, et al. Talimogene laherparepvec improves durable response rate in patients with advanced melanoma. J Clin Oncol. 2015;33:2780–8.
Zhang B, Huang J, Tang J, Hu S, Luo S, Luo Z, et al. Intratumoral OH2, an oncolytic herpes simplex virus 2, in patients with advanced solid tumors: a multicenter, phase I/II clinical trial. J Immunother Cancer. 2021;9. https://doi.org/10.1136/jitc-2020-002224.
Zhang L, Pakmehr SA, Shahhosseini R, Hariri M, Fakhrioliaei A, Karkon Shayan F, et al. Oncolytic viruses improve cancer immunotherapy by reprogramming solid tumor microenvironment. Med Oncol. 2023;41:8.
Ma J, Ramachandran M, Jin C, Quijano-Rubio C, Martikainen M, Yu D, et al. Characterization of virus-mediated immunogenic cancer cell death and the consequences for oncolytic virus-based immunotherapy of cancer. Cell Death Dis. 2020;11:48.
Packiriswamy N, Upreti D, Zhou Y, Khan R, Miller A, Diaz RM, et al. Oncolytic measles virus therapy enhances tumor antigen-specific T-cell responses in patients with multiple myeloma. Leukemia. 2020;34:3310–22.
DeNardo DG, Ruffell B. Macrophages as regulators of tumour immunity and immunotherapy. Nat Rev Immunol. 2019;19:369–82.
Wei B, Pan J, Yuan R, Shao B, Wang Y, Guo X, et al. Polarization of tumor-associated macrophages by nanoparticle-loaded Escherichia coli combined with immunogenic cell death for cancer immunotherapy. Nano Lett. 2021;21:4231–40.
Denton NL, Chen CY, Scott TR, Cripe TP. Tumor-associated macrophages in oncolytic virotherapy: friend or foe? Biomedicines. 2016;4. https://doi.org/10.3390/biomedicines4030013.
Zheng C, Zheng L, Yoo JK, Guo H, Zhang Y, Guo X, et al. Landscape of infiltrating T cells in liver cancer revealed by single-cell sequencing. Cell. 2017;169:1342–56.e1316.
Cha E, Klinger M, Hou Y, Cummings C, Ribas A, Faham M, et al. Improved survival with T cell clonotype stability after anti-CTLA-4 treatment in cancer patients. Sci Transl Med. 2014;6:238ra270.
Tumeh PC, Harview CL, Yearley JH, Shintaku IP, Taylor EJ, Robert L, et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature. 2014;515:568–71.
Snyder A, Nathanson T, Funt SA, Ahuja A, Buros Novik J, Hellmann MD, et al. Contribution of systemic and somatic factors to clinical response and resistance to PD-L1 blockade in urothelial cancer: an exploratory multi-omic analysis. PLoS Med. 2017;14:e1002309.
Dong LQ, Peng LH, Ma LJ, Liu DB, Zhang S, Luo SZ, et al. Heterogeneous immunogenomic features and distinct escape mechanisms in multifocal hepatocellular carcinoma. J Hepatol. 2020;72:896–908.
Nikanjam M, Kato S, Kurzrock R. Liquid biopsy: current technology and clinical applications. J Hematol Oncol. 2022;15:131.
Zhang Q, Luo J, Wu S, Si H, Gao C, Xu W, et al. Prognostic and predictive impact of circulating tumor DNA in patients with advanced cancers treated with immune checkpoint blockade. Cancer Discov. 2020;10:1842–53.
Razavi P, Dickler MN, Shah PD, Toy W, Brown DN, Won HH, et al. Alterations in PTEN and ESR1 promote clinical resistance to alpelisib plus aromatase inhibitors. Nat Cancer. 2020;1:382–93.
Ling AL, Solomon IH, Landivar AM, Nakashima H, Woods JK, Santos A, et al. Clinical trial links oncolytic immunoactivation to survival in glioblastoma. Nature. 2023;623:157–66.
Ponce S, Cedres S, Ricordel C, Isambert N, Viteri S, Herrera-Juarez M, et al. ONCOS-102 plus pemetrexed and platinum chemotherapy in malignant pleural mesothelioma: a randomized phase 2 study investigating clinical outcomes and the tumor microenvironment. J Immunother Cancer. 2023;11. https://doi.org/10.1136/jitc-2023-007552.
Nassiri F, Patil V, Yefet LS, Singh O, Liu J, Dang RMA, et al. Oncolytic DNX-2401 virotherapy plus pembrolizumab in recurrent glioblastoma: a phase 1/2 trial. Nat Med. 2023;29:1370–8.
Heo J, Liang JD, Kim CW, Woo HY, Shih IL, Su TH, et al. Safety and dose escalation of the targeted oncolytic adenovirus OBP-301 for refractory advanced liver cancer: Phase I clinical trial. Mol Ther. 2023;31:2077–88.
Keshavarz M, Mohammad Miri S, Behboudi E, Arjeini Y, Dianat-Moghadam H, Ghaemi A. Oncolytic virus delivery modulated immune responses toward cancer therapy: challenges and perspectives. Int Immunopharmacol. 2022;108:108882.
Moon EK, Wang LS, Bekdache K, Lynn RC, Lo A, Thorne SH, et al. Intra-tumoral delivery of CXCL11 via a vaccinia virus, but not by modified T cells, enhances the efficacy of adoptive T cell therapy and vaccines. Oncoimmunology. 2018;7:e1395997.
Rosewell Shaw A, Porter CE, Watanabe N, Tanoue K, Sikora A, Gottschalk S, et al. Adenovirotherapy delivering cytokine and checkpoint inhibitor augments CAR T cells against metastatic head and neck cancer. Mol Ther. 2017;25:2440–51.
Chiou VL, Burotto M. Pseudoprogression and immune-related response in solid tumors. J Clin Oncol. 2015;33:3541–3.
Acknowledgements
This study would like to appreciate every participant enrolled in this study. This work was supported by the 2023 Hangzhou West Lake Pearl Project Leading Innovative Youth Team Project (TD2023017); Fundamental Research Funds for the Central Universities (226-2022-00214); Zhejiang Provincial Natural Science Foundation Key Project (LZ24C080001); National Natural Science Foundation of China (82203186), National Natural Science Foundation of China (81602128) and Natural Science Foundation of Zhejiang Province (LQ23H160041).
Author information
Authors and Affiliations
Contributions
XL and LL conceived of the study and carried out its design. XT, YR, and FW performed the experiments. ZT and YZ provided materials. JC did pathological immunohistochemistry. HZ, PZ, JL, and WF analyzed the data. HZ and YR wrote and revised the manuscript with input from all authors. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
The study followed the Declaration of Helsinki principles and was approved by the Medical Ethics Committee of the First Affiliated Hospital, Zhejiang University, Hangzhou, China. The informed consent was obtained from all subjects.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, H., Ren, Y., Wang, F. et al. The long-term effectiveness and mechanism of oncolytic virotherapy combined with anti-PD-L1 antibody in colorectal cancer patient. Cancer Gene Ther 31, 1412–1426 (2024). https://doi.org/10.1038/s41417-024-00807-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41417-024-00807-2
- Springer Nature America, Inc.