Abstract
The selection and combination of dose regimens for antimalarials involve complex considerations including pharmacokinetic and pharmacodynamic interactions. In this study, we use immediate ex vivo P. falciparum field isolates to evaluate the effect of cabamiquine and pyronaridine as standalone treatments and in combination therapy. We feed the data into a pharmacometrics model to generate an interaction map and simulate meaningful clinical dose ratios. We demonstrate that the pharmacometrics model of parasite growth and killing provides a detailed description of parasite kinetics against cabamiquine-susceptible and resistant parasites. Pyronaridine monotherapy provides suboptimal killing rates at doses as high as 720 mg. In contrast, the combination of a single dose of 330 mg cabamiquine and 360 mg pyronaridine provides over 90% parasite killing in most of the simulated patients. The described methodology that combines a rapid, 3R-compliant in vitro method and modelling to set meaningful doses for new antimalarials could contribute to clinical drug development.
Similar content being viewed by others
Introduction
Every year malaria continues to inflict extensive morbidity and mortality in resource-poor countries. Over the last decades, fixed-dose of artemisinin-based combination therapies (ACTs) or sulfadoxine–pyrimethamine have become available respectively as the first-line treatment for uncomplicated malaria and seasonal malaria chemoprevention (SMC) to school aged children during peak malaria transmission seasons. Despite an initial decline in malaria mortality and incidence1, malaria cases have increased recently2, indicating that malaria continues to be a major public health problem. Furthermore, the progress made in controlling the disease is threatened by the development and spread of Plasmodium (P.) falciparum resistance to artemisinins and other drugs such as mefloquine, piperaquine3,4 chloroquine or sulfadoxine–pyrimethamine5,6. Consequently, new antimalarial compounds with novel modes of action and non-artemisinin-based combination therapies are required to maintain disease decline toward elimination milestone completion. Thus, early identification of new antimalarial combinations becomes a critical priority to minimize and/or eliminate drug resistance emergence and spread following field deployment. Furthermore, this would promote long-lasting use of the novel combinations in the field by delaying emergence of the resistance. Several prerequisites contribute to the success of combination strategy, such as the choice of different pharmacological targets to minimize the development of resistance, similar pharmacokinetic (PK) profiles by matching half-lives to prevent one drug to persist as a vulnerable monotherapy and lack of reported resistance to date in P. falciparum for one of the two drugs.
Accordingly, we considered the combination of cabamiquine (M5717, DDD107498)7, an under-development antimalarial inhibiting the Plasmodium translation elongation factor 2 (PfeEF2), with pyronaridine8, an inhibitor of haemozoin formation discovered in the 1970s and used together with artesunate in an ACT (Pyramax®)9. Interestingly, both drugs have a long mean half-life (t1/2) across doses in humans, 155–193 hrs for cabamiquine and 241 hrs for pyronaridine10.
A preclinical study using a humanized mouse model (NSG, NOD/SCID/IL2rγnull) susceptible to the human P. falciparum parasite (PfalcHuEryMouse)11 had shown a favorable interaction between the two drugs10. Importantly, pyronaridine could suppress the emergence of cabamiquine-resistant mutant parasites and maintain its fast-acting profile. Based on these results and on a volunteer infection study (Phase Ib) with cabamiquine as monotherapy12, effective doses could be selected pragmatically for cabamiquine and pyronaridine to enter into a Phase II clinical trial (NCT05689047).
However, little is known about how to select dose ratios for drug combinations. In addition, the dose-response relationship and possible drug–drug-pharmacodynamic interactions may pose translational challenges due to animal model limitations and animal welfare concerns. Therefore, data obtained were not sufficient to refine the selection of a fixed-dose combination (FDC) of cabamiquine–pyronaridine in humans. In addition, as the pharmacodynamic (PD) data are based solely on laboratory strains of P. falciparum 3D7, further evidence on possible drug–drug–PD interactions in a real-world setting, i.e., field isolates of P. falciparum and endemic host factors is needed to evaluate the efficacy of the combination. Thus, as a result of a highly complex adaptation process to the in vitro environment, the parasite may integrate changes into its genome that could affect its fitness cost and drug susceptibility13,14,15,16,17. To capture these components, we opted for an in vitro testing of the combination using immediate “ex vivo” (IEV) field isolates before entering Phase IIa clinical trial. This will allow us to: (i) test the combination in a reasonable time and cost under the 3Rs principle by replacing and/or reducing the use of animals, thus providing a basis for alternative methods to reduce animal testing, (ii) improve confidence in reaching clinical efficacy by giving more precise information on the PD interactions and (ii) suggest optimal doses for a FDC.
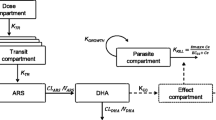
In this work, we determined the concentration and dose range for cabamiquine and pyronaridine to maximize their efficacy in combination by using IEV P. falciparum field isolates parasites processed by adapting the recently published interaction—parasite reduction ratio (PRR) assay to field settings18 and using parasite survival readout19. Using the experimental design schematized in Fig. 1, we enable rational selection of drug concentrations and ratios covering the EC50 (half maximal effective concentration) as well as the maximum drug effect as previously reported20 up to clinically observed maximum drug concentrations. Thus, our experimental design allowed (1) detection of drug–drug-PD interactions as shifts of the pharmacologically important parameters EC50, as well as (2) Emax (maximum drug effect) using a model-based approach, and (3) translated the in vitro findings into the clinical perspective using simulations.
A Patient P. falciparum parasites were collected and cultured ex vivo to determine (B) in vitro parasite-killing kinetics of an antimalarial drugs at different concentrations either monotherapy or combinations at different timepoints using a rapid viability assay (MitoTracker™ Deep Red FM staining). From there (C), an in silico drug–drug-PD interaction map modeled and coupled with (D) individual antimalarial PK simulation obtained from previous human clinical trial to simulate (E) individual parasite-killing rate profiles per dose in monotherapy and in combination.
Results
In combination, pyronaridine suppresses the development of adaptive resistance to cabamiquine
Using an experimental design adapted from the dynamic checkerboard analysis developed for testing antibiotics combinations20,21,22, we evaluated the ex vivo susceptibility of cabamiquine and pyronaridine in monotherapy or combination on seven different P. falciparum parasites isolated directly from Malian patients (referred as IEV: EEF210, EFF211, EFF223, EEF209, EEF192, EFF204, and EFF269) in parallel with the reference laboratory 3D7 control line as displayed in Supplementary Fig. 7. Once 1% parasitemia was reached, parasites were exposed to different concentrations of cabamiquine and pyronaridine covering the EC50, concentration required to reach Emax, as well as the clinically relevant concentration range based on previous data obtained with the reference strain 3D7. This design allows to identify any PD drug–drug interaction utilizing the general pharmacodynamic interaction (GPDI) model. In addition, the longitudinal monitoring of the parasite viability using MitoTracker™ Deep Red FM staining allows to detect any time-dependent drug effects, e.g., adaptive resistance processes.
We developed a PD model describing the time course of the parasite growth and killing under monotherapy and combination therapy (Supplementary Fig. 1). The model consisted of a single compartment to describe the parasite growth and killing. As a first step, monotherapy effects for each drug were modeled. Emax, i.e., the maximum possible killing rate was derived from the reduction of the first to the second time point at the highest concentration of each drug and the growth data.
Emax was subsequently fixed in the model, as it was not estimable precisely within the model due to the reduction of the assay signal to baseline from the first to the second time point, hence representing a conservative estimate of Emax. The study showed that pyronaridine exhibited a constant EC50 of 28.3 nM and a mono-phasic killing to the baseline assay signal was observed (Supplementary Fig. 2). For cabamiquine, a biphasic killing pattern was observed i.e., initial killing followed by regrowth, which is commonly referred to as adaptive resistance23. This was modeled by a concentration and time-dependence of the EC50 of cabamiquine (Fig. 2). The typical value of the EC50 of cabamiquine was increased from 0.799 nM to a value of 5.90 nM (7.38-fold) (Fig. 2). The model accounting for a concentration-time-dependent EC50 of cabamiquine provided a superior model fit as compared to the model with a sole time-dependent EC50 (dAIC: +91.44) or a static EC50 (dAIC: +634.16). The static estimate did not consider the adaptive resistance to cabamiquine and was estimated to 5.97 nM (Fig. 2, orange dashed line). The Hill factor of cabamiquine quantifying the steepness of the concentration-effect relationship tended to a high value >20 indicating an on/off effect but could not be estimated precisely. Consequently, we fixed the Hill factor to 20 as the model was insensitive to higher values. A more detailed comparison of the model fit for scenarios that displayed adaptive resistance is provided in Supplementary Figs. 3–5. The final model also predicted the adequality of the in vitro data from a well-characterized laboratory strain parasite (P. falciparum 3D7), which helped to benchmark the model (Supplementary Fig. 7 and Supplementary Table 1).
For the analysis of the combination data several null interaction models were considered as a starting point (e.g., Loewe Additivity, Bliss Independence or Effect addition)24. These null interaction models predicted the combined effect under the assumption that both combination partners each exert their effect, but do not alter the effect of the combination partner. The Bliss Independence model24 was chosen as it predicted the additive effect of two drugs that act independently on distinct targets (cabamiquine: EF2 inhibitor, pyronaridine: involved in heme degradation). As a result of the combination, the observed regrowth in cabamiquine monotherapy at concentrations around the EC50 was suppressed when pyronaridine concentrations exceeded its EC50. No additional PD interaction was quantifiable, i.e., no synergy or antagonism was observed. A prediction-corrected visual predictive check (pcVPC) is a technique to diagnose if the model could predict the central tendency as well as the observed variability in the data25. The pcVPC for the final model indicated a good predictive performance of the model and is presented in Supplement Fig. 6. The final model parameters are presented in Table 1, which predicted the entire dataset well (Fig. 3).
Model predictions from the final model (lines) and original data (points) for each parasite (colors); each facet displays a studied scenario for cabamiquine (A1) and pyronaridine (A2). The numbers in each facet present the concentration of either cabamiquine or pyronaridine in nM in each well. Readout: total SYBR Green and MitoTracker positive parasite count.
Using the parameter estimates of the final model, the apparent parasite-killing rate was simulated for cabamiquine and pyronaridine, alone and combined, at a dense concentration grid and visualized in a heat map (Fig. 4). The simulation illustrates the cabamiquine is more active in the first 6 h with a decrease of the activity until 12 h due to the drug adaptive resistance, while it was predicted to stabilize between 48 and 72 h. If concentrations of pyronaridine exceeded its EC50 (28.3 nM) or the EC50 of cabamiquine (5.9 nM) after full adaption, the killing rate was stable.
Cabamiquine–pyronaridine combination exhibits additivity-synergy properties in induced cabamiquine-resistant field isolates
To demonstrate the efficacy of the combination and confirm the choice of pyronaridine as a partner drug in a field scenario, cabamiquine–pyronaridine PD interactions were assessed in two different cabamiquine-resistant adapted P. falciparum field isolate strains (isolate 1: parasite strain ID EFF192 with E134V mutation and isolate 2: parasite stain ID EFF209 with Y186C mutation26) using the same drugs concentrations as for the susceptible isolates26.
The previously developed model structure was used to model the in vitro data of cabamiquine combined with pyronaridine against induced cabamiquine-resistant field isolates strains26. As the strains were already cabamiquine-resistant, no adaptation model was used to describe the EC50 of cabamiquine, but a static EC50 was used instead. While the EC50 of pyronaridine was even slightly lower as compared to the cabamiquine-susceptible isolates (12.9 or 7.62 nM vs. 28.3 nM), the EC50 of cabamiquine was estimated to 961 nM (resistant isolate 1) or was so high that it was not precisely estimable (5E + 15 nM, resistant isolate 2) (Table 2). Hence, the effect of cabamiquine against the resistant isolates could be described by a slope model; nonetheless the EC50 model was kept for comparability with the susceptible strain. In summary, the drug effect of cabamiquine alone was marginal, even at the highest concentration studied, while pyronaridine retained its effect against cabamiquine-resistant parasites.
Modeling revealed a synergistic interaction for the resistant isolate 1, where inactive cabamiquine seemed to potentiate the effect of pyronaridine. A model considering the synergistic interaction provided a highly superior fit compared to a model assuming an additive interaction according to Bliss Independence (dAIC: −689.87). At 5 nM, pyronaridine alone was inactive but became effective at killing cabamiquine-resistant parasites when placed in combination with cabamiquine (Supplement Fig. 8, column with 5 nM pyronaridine and increasing cabamiquine concentrations). For the resistant isolate 2, no synergistic interaction was quantifiable, and the data was best described assuming Bliss Independence as an additivity model, as for the susceptible field isolates. The model predictions and data are presented in Supplementary Fig. 9. The final parameter estimates of both resistant isolates is presented in Supplementary Table 2.
Model-based simulations support cabamiquine and pyronaridine clinical dose selection
We used the PD model derived from the cabamiquine-susceptible IEV P. falciparum field isolates as well as the model developed on the induce cabamiquine-resistant field isolate strains26 to perform clinical trial simulations and translate the in vitro findings into the clinical setting. Therefore, the PD models were coupled to published population PK models for cabamiquine27 and pyronaridine (Supplementary Fig. 10)28. The single dose PK/PD profiles of cabamiquine (0–660 mg, free base) or pyronaridine (0–720 mg, tetraphosphate), alone or combined, were simulated in 40,000 patients (1000 virtual patients for each dosing scenario) considering the demographics (body weight, ideal body weight, sex) from an African population older than 18 years.
The extracted killing rates at 24 and 96 h, stratified per dosing level are presented in Fig. 5. The clinical trial simulations indicate that 200 mg cabamiquine alone led to >90% killing rate in >95% of the virtual patients at 24 and 96 h, which was further increased to >99% when combined with pyronaridine at doses higher than 360 mg. For pyronaridine alone, differences between 24 and 96 h were more marked. For example, 720 mg pyronaridine monotherapy resulted in >90% killing rate in 86.6% of the patients at 24 h while showed it showed a significant decrease (34.5%) at 96 h. Overall, even at the highest dose of pyronaridine, the maximum killing rate was not obtained when used alone.
Distribution of the apparent killing rate against susceptible field isolates of P. falciparum at 24 h (upper panel) and 96 h (lower panel) from clinical trial simulations using a single dose of cabamiquine (free base) and pyronaridine (tetraphosphate); percentage in label: virtual patients exceeding a killing rate of 90% (dashed line); box: 25th to 75th percentile (interquartile range) with median (black horizontal line); whiskers: 1.5 times interquartile range below 25th or above 75th percentile, respectively; dots: values outside whiskers’ range; n = 1000 simulations for each dosing scenario.
The apparent killing rates against the cabamiquine-resistant isolate are presented in Fig. 6. Since the EC50 of pyronaridine was quantified to be lower in the cabamiquine-resistant strain compared to the field isolate (12.9 vs. 28.3 nM) overall higher killing rates were observed for pyronaridine alone as compared to the susceptible isolates. Due to the quantified synergistic interaction, although almost inactive itself, cabamiquine enhanced the observed killing rate of pyronaridine. For example, a dose of 400 mg cabamiquine combined with 360 mg of pyronaridine resulted in >90% killing rate in 97.1% of the patients at 96 h while cabamiquine alone was inactive and 360 mg of pyronaridine alone solely showed a >90% killing rate in 67% of the patients at 96 h.
Distribution of the apparent killing rate against a cabamiquine-resistant P. falciparum strain at 24 h (upper panel) and 96 h (lower panel) from clinical trial simulations using a single dose of cabamiquine and pyronaridine; percentage in label: virtual patients exceeding a killing rate of 90% (dashed line); box: 25th to 75th percentile (interquartile range) with median (black horizontal line); whiskers: 1.5 times interquartile range below 25th or above 75th percentile, respectively; dots: values outside whiskers’ range; n = 1000 simulations for each dosing scenario.
Furthermore, to simulate the worst-case scenario, clinical trial simulations (wild-type and cabamiquine-resistant parasites) were conducted using pyronaridine PK values obtained from patients given that pyronaridine exposure may vary between patients and healthy volunteers (Supplementary Figs. 11 and 12). Compared to the previous results using the model in healthy volunteers, the model predicted a slower killing rate for pyronaridine in patients because of the reduced exposure. However, the difference was only visible when pyronaridine was given in monotherapy or at 96 h. When combined with 400 mg of cabamiquine, the results were similar in both scenarios for doses of pyronaridine ≥360 mg, also at 96 h.
Discussion
Following WHO guidelines and intending to mitigate the selection of cabamiquine-resistant parasites, the early identification and evaluation of potential cabamiquine combination partners, such as pyronaridine, with relevant data on their respective contribution to the overall effect, are crucial to progress in Phase II clinical trials. To ensure good translatability from bench to bedside, we used an in vitro/ex vivo assay based on real-world data (IEV P. falciparum field isolate parasites), combining ex vivo and in silico-based approaches to provide quantitative insights into potential PD interactions between two drugs and facilitate translation into a clinical setting. This in vitro combination assay represents a further adaptation of the previously described interaction-PRR assay18. To retain the genotype/phenotype information of the original clinical isolates14, we used non-adapted field isolates. As non-adapted field isolates do not survive multiple blood stage cycles, we leveraged on the MitoTracker technique19 instead of the PRR29,30,31 to inform parasite viability at different timepoints and evaluate the maximum parasite-killing rate after drug exposure.
Using a pharmacometric modeling approach, we characterized the time-kill kinetics of cabamiquine and pyronaridine, alone and combined, respectively, and the model allowed to characterize the typical pharmacodynamics as well as interparasite variability. Parasite killing was quantified in relation to parasite growth. The quantified growth rates ex vivo were very similar compared to those in volunteer infection studies32. Thereby, the utilized modeling approach was superior over the isobologram which is a conventional non-model-based PD interaction assessment solely evaluating the combined PD response at a defined effect (usually the EC50) that can only be interpreted graphically33. In contrast, a model-based approach allows the in vitro data to be represented by a mathematical model, which enables vitro experiments to be translated into dosing regimens by linking the in vitro PD model to clinically derived population PK model. A minor limitation is that the experimental design did not allow to precisely estimate Emax. Nonetheless, the here determined value quantifies the full reduction of the assay signal until 12 h and hence represents a conservative estimate of maximum effect, as the maximum effect may have occurred even earlier. Moreover, since the dosing simulations were evaluated relative to Emax, the same conclusion would have been drawn even for a higher value of Emax. For the field isolates, the model quantified a neutral interaction, i.e., no deviation from an additive response using Bliss Independence as a null interaction model. Interestingly, for one of the resistant isolates (isolates 1), a synergistic effect was found were inactive cabamiquine potentiated the effect of pyronaridine (Table 2), a phenomenon referred to as collateral sensitivity for antibiotics34. Also, available data indicated that cabamiquine-resistant Plasmodium parasites are limited by fitness costs that may accompany resistance26,35. Thus, increasing cabamiquine pressure results in the selection of mutations with the highest-cost mutation (higher EC50 shifts) that have the lowest parasite fitness7. Consequently, the selection of resistant parasites with a lower growth rate than wild-type parasites would facilitate their clearance by the partner drug. This could explain why cabamiquine-resistant strains are more susceptible to pyronaridine than wild-type parasites. Thus, these data support previous results obtained with the PfalcHuEryMouse model in which neither compound negatively impacted the killing rate of the partner drug, and pyronaridine demonstrated the ability to control and kill cabamiquine-resistant mutants10.
Model-based simulations of cabamiquine and pyronarindine alone and in combination in were conducted using the in vitro-derived interaction parameters integrated with PK parameters obtained from monotherapy clinical trials in humans. Results indicate that cabamiquine alone reached a maximum killing rate in >99% of the simulated patients if the dose exceeded 200 mg until 96 h Pyronaridine alone showed a substantially lower killing rate, even at the highest dose studied (720 mg) in line with clinical data36. Instead, in combination even low doses of pyronaridine (360 mg) enhanced the combined effect. Of note, doses of 360–540 mg of pyronaridine showed high killing rates against the cabamiquine-resistant isolate indicating that the observed synergy in vitro seems clinically useful. This is qualitatively in line with observed in PfalcHuEryMouse10 model where the combination of the two compounds increased the parasite-killing rate.
The simulations performed in this study were largely consistent with the observed drug response of clinical trials12. Indeed, the observed Phase I clinical data from volunteer infection studies where cure was observed in 3 of the 6 subjects (50% with one wild-type and two drug-resistant recrudescences) in the 120 mg group and 6 of the 8 subjects (75% with two drug-resistant recrudescences) in the 320 mg group26. All participants were cured in the 630 mg dose group. Although, not directly comparable, the difference between the outcome of Phase I study and model-based simulations, where the EC50 values of susceptible field isolates were used, can be partially explained by the drug-resistant mutants detected in clinic. The efficacy and lack of cross-resistance to pyronaridine makes it useful in combination with other antimalarial drugs with resistance issues. In fact, our prediction suggests that pyronaridine is only active above 5 nM as monotherapy, whereas it becomes active at 5 nM below the EC50 in combination with cabamiquine. In this way, cabamiquine considerably enhances the effect of pyronaridine in combination, and pyronaridine in turn suppresses adaptive resistance to cabamiquine.
In light of these results (Fig. 7) and considering the characteristics (e.g., safety and resistance) of both drugs, it would be appropriate to use pyronaridine at the lowest possible dose with cabamiquine doses as high as possible, possibly fitting into a 1 g tablet. Indeed, a high dose of cabamiquine (e.g., 400 or 600 mg) will maximize its properties and potentially select the highest-grade mutants that are least fit. While a low dose of pyronaridine (e.g., 180 or 360 mg) will minimize any potential safety concerns, it will still provide the PD contribution to the combination. In addition, low concentrations of pyronaridine in combination with cabamiquine were found to be effective in controlling and killing parasites that were resistant to cabamiquine. However, further clinical studies are needed to confirm this hypothesis. In addition, to ensure the universality of the observed outcomes, field isolates from various countries and continents should be used. As a result of this broader approach, we will be able to determine whether the findings are applicable across different geographical and demographic contexts.
Overall, under this framework allows the selection of combination therapy partners by simulating the clinical effect of various combination regimens in a real-world setting. Identifying novel effective combinations of malaria chemotherapies that maximize inhibitory effects on parasites and suppress resistance is key to future deployments of malaria chemotherapies. In conclusion, this framework could accelerate and refine the selection early in the drug development process of compounds and potential drug combinations while reducing the number of animals used in the preclinical phase under the 3Rs principle.
Methods
Ethics statements
The human biological samples were sourced ethically, and their research use was in accord with the terms of the informed consents. The study was approved by the ethical committee of the Université des Sciences, des Techniques et des Technologies de Bamako (USTTB) under the reference: N°2020/296/CE/FMOS/FAPH renewed N°2022/03/USTTB and then N°2023/03/USTTB.
Human blood
Donations of 0+ human red blood cell (hRBCs) concentrate of malaria-negative donors, but non-naïve malaria individuals were obtained from the Malian blood bank in Bamako (Mali). Prior to use, hRBCs were washed three times with RPMI 1640 culture medium (25 mM HEPES, 30 mM NaHCO3 supplemented with 50 mg/ml gentamicin) and processed immediately ex vivo (IEV) culture. Finally, leukocyte-free hRBCs were stored in RPMI 1640 culture medium (at 50% hematocrit) and kept at 4 °C for further use no more than 3 weeks.
Parasites
All IEV P. falciparum field isolate parasites used in this study were collected from microscopically diagnosed P. falciparum positive individuals in Faladjè’s site (Kati, Mali) that were PCR confirmed as P. falciparum mono-infection as reported earlier37. Blood was collected after obtaining the consent of the patient or guardian in case of children. P. falciparum 3D7 strain was obtained from the National Institutes of Health (NIH) and kept under culture condition in the laboratory. To note that the parasites used in this study were not sequenced, and therefore, the genetic diversity among the strains was not assessed.
P. falciparum field isolates parasites processed immediately ex vivo (IEV) culture
IEV P. falciparum field isolate parasites (EEF210, EFF211, EFF223, EEF209, EEF192, EFF204 and EFF269) were collected in ACD vacutainers (BD Biosciences, ref# 364606) and transported to the laboratory for processing within 2 h after collection. IEV culture was performed using standard protocols38. Briefly, after plasma removal, to deplete leukocytes the red blood cell (RBC) pellet was washed three times in RPMI 1640 culture medium (Gibco-Life Technologies SAS, France) and placed in RPMI 1640 culture medium supplemented with 0.5% AlbuMAX II (Gibco-Life Technologies SAS, France) and 200 mM hypoxanthine, at 2% hematocrit and 1% parasitemia for immediately drug assays, without prior culture adaptation, at 37 °C in 5% O2, 5% CO2, rest of N2 atmosphere.
Cabamiquine-sensitive adapted P. falciparum field isolate parasites
IEV P. falciparum field isolate parasites were collected and cultivated in human erythrocytes using supplemented RPMI 1640 culture medium as previously described26. Briefly, cultures were maintained in a total volume of 6 mL of complete medium containing uninfected hRBCs from the Malian blood bank (Bamako) at 4% hematocrit at 37 °C under 5% CO2, 5% O2, and 90% N2 atmosphere. Adaptation of the culture was considered successful after 3 weeks of uninterrupted culture. The adapted field isolates parasites were cryopreserved in liquid nitrogen when parasitemia reached 5–6%.
Cabamiquine-resistant adapted P. falciparum field isolate parasites
Mutant parasites resistant to cabamiquine were selected as previously descripted26. Briefly, sensitive P. falciparum adapted field isolate parasites were synchronized by three 5% sorbitol treatments39 and cultured in supplemented RPMI 1640 culture medium. Parasites at the ring stage (>95%) at ~5% parasitemia and 4% hematocrit were exposed to 7.5 nM (15xEC50) of cabamiquine (Merck KGaA, Darmstadt, Germany) for 6 days. After drug exposure, cultures were washed to remove cabamiquine from the cultures, and resuspended in supplemented RPMI 1640 culture medium. Parasites growth was monitored by microscopy every 2 days until the appearance of recrudescent parasites. Recrudescent parasites susceptibility to cabamiquine was assessed by determining the EC50 pre- and post drug exposure. Moreover, recrudescent parasites were sequenced using SeqStudio Genetic Analyzer from Applied Biosystems to identify possible PfeEF2 mutations responsible for the decreased cabamiquine susceptibility.
Cabamiquine–pyronaridine interaction assay
IEV P. falciparum field isolate parasites sensitive to cabamiquine and adapted field isolate cabamiquine-resistant parasites along with P. falciparum laboratory 3D7 strain were cultured in supplemented RPMI 1640 culture medium in 96 well plates in the presence and absence of the drug. To initiate the assay, the parasite culture was adjusted to 1% parasitemia and 2% hematocrit. Compounds powders were dissolved in dimethyl sulfoxide (DMSO) to obtain 10 mM stocks. Thereafter, monotherapies and combinations stocks were prepared in supplemented RPMI 1640 culture medium and added to the corresponding well to achieve the desired concentrations and tested on biological replicates (one for Pf3D7, two for cabamiquine-resistant parasites, and eight for IEV P. falciparum field isolate parasites) in two independents experimental for monotherapies and combination for each concentration. Parasites were exposed to drugs for desired defined timing starting from time 0 h until the completion of the first two in vitro cycles40 at 37 °C and under 5% CO2 atmosphere. Untreated and parasite free culture well controls were included at time zero to monitor parasite growth. The parasites viability was assessed at different timepoints (12, 24, 48, and 72 h post drug exposure) using flow cytometry (BD Accuri™ C6 Flow Cytometer®) after staining of parasites with SYBR™ Green (ThermoFisher Scientific, Cat# M22426) combined with MitoTracker™ Deep Red FM (ThermoFisher Scientific, Cat# S7563) as previously reported19.
Modeling of in vitro data of the combination of pyronaridine and cabamiquine in susceptible IEV P. falciparum field isolates
The model was built from the in vitro assay data from seven field isolates. These data were analyzed simultaneously using nonlinear mixed effects modeling in the NONMEM® software (ICON development service, Gaithersburg, MD, version 7.5), while assuming constant concentrations of cabamiquine and pyronaridine.
In the first step, the parasite growth parameters were estimated with an exponential growth model. The growth model is defined as follows:
Where \(N\left(t\right)\) represents the model-predicted parasites at time \(t\) and \({k}_{{growth}}\) the first-order growth rate and \({N}_{0}\) the initial condition (assay readout at t = 0 h).
The raw assay readout \(Y\) was related to \(N\) by a proportional residual error model and a \({Baseline}\) (remaining assay signal after elimination of the parasites), as follows:
with \(\varepsilon\) quantifying the deviation from \(Y\) from \(N\) at each time point of the assay readout.
Subsequently, the mono drug effects were estimated from the wells containing only single drugs using a sigmoidal maximum effect model:
where \({E}_{\max }\) represents the maximum kill rate, \(E{C}_{50}\) the concentration stimulating half-maximum kill and the hill coefficient \(h\) the steepness of the concentration-effect relationship.
For cabamiquine, adaptive resistance development, i.e., parasite growth after initial killing was observed in the raw data. This was modeled by a concentration- and time-dependent \(E{C}_{50}\) for cabamiquine using an adaptive resistance compartment41,42:
where \({k}_{{adapt}}\) describes the second-order delay rate constant of the onset of the adaptive resistance, \({{MAX}}_{{adapt}}\) the maximum fractional change of the EC50of cabamiquine, \({{AR}}_{{on}}\) describes the concentration- and time-dependent addition to the EC50 of cabamiquine by adaptive resistance at each time point and concentration of cabamiquine, and IC: the initial condition of the differential equation. Simpler models with a sole time-dependent and a static EC50 were evaluated as well for comparison.
Thereafter, the combined drug effects for both cabamiquine and pyronaridine were modeled assuming Bliss Independence:
where:
Interparasite variability was evaluated on all model parameters assuming a log-normal distribution.
Potential pharmacodynamic interactions were quantified as deviation from Bliss Independence and quantified using the general pharmacodynamic interaction (GPDI) model22. Drug effects were scaled by the highest Emax as a prerequisite for Bliss Independence24. Since Emax was not quantifiable precisely due to the rapid decline of the assay readout to baseline from the first to the second time point, we focused on interactions on the EC50 level. In the GPDI model, the EC50 of a victim drug is shifted by the perpetrator drug. The interaction is thereby characterized by the maximum fractional shift of the EC50 (INT) and the potency of the perpetrator drug in the interaction (EC50,INT), and the sigmoidicity (HillINT, set to 1 in the present analysis). The EC50 of the perpetrator in combination (EC50comb) is calculated by:
while each drug was evaluated as perpetrator and/or victim. Model fit was assessed by goodness of fit plots, inspection of the individual model fits per each experimental scenario, and prediction-corrected visual predictive checks25. In the case of competing models, the likelihood ratio test (alpha = 0.05, df=1) was used to select amongst nested models, whereas the Akaike Information Criterion (AIC, lower value indicates superior model) was used for non-nested models.
The developed model was used to predict the in vitro data from a combination experiment with a reference parasite (3D7) and thereby externally evaluated (Supplementary Fig. 6).
To illustrate the concentration-response surface of cabamiquine and pyronaridine, a simulation was performed using the final parameter estimates and the apparent kill rate was visualized in a heat map.
Modeling of in vitro data of the combination of cabamiquine and pyronaridine in cabamiquine-resistant adapted P. falciparum field isolates
The same model structure as outlined above was used to model the in vitro data of two cabamiquine -resistant field isolates. As these two strains were already highly cabamiquine-resistant, the adaptive resistance development component of the model was removed and a static \(E{C}_{50}\) of cabamiquine was estimated. Potential PD interactions were evaluated using the GPDI model quantified as shifts of EC50 or Emax as outlined above22.
Dose simulations for translation of preclinical model to the clinical setting
The final in vitro-based PD models described above were linked to PK models of cabamiquine27 and pyronaridine28 developed in humans in healthy volunteers and/or patients. Due to the lack of cabamiquine PK information in the target malaria population at the time of the analysis, the population PK (popPK) model developed in healthy volunteers was utilized. For pyronaridine, different popPK models have been reported to characterize PK profile in healthy volunteer’s vs malaria patients. Due to the lack of understanding of these differences and the absence of pyronaridine PK data in our target population receiving a combination of cabamiquine and pyronaridine, the two popPK models have been utilized in clinical trial simulations. The main manuscript presents results based on the popPK model in healthy volunteers, while results based on the popPK model in malaria patients are included in the supplementary material. A simulation dataset was developed in which single doses of 0–660 mg or 0–720 mg of cabamiquine or pyronaridine tetraphosphate, alone or combined, respectively, were administered to a virtual patient population of 40,000 patients (1000 virtual patients for each dosing scenario). Doses were selected to offer a comprehensive view of the dose-exposure-response relationship, and to cover clinically relevant doses. In the model, pyronaridine was dosed as free base as in the utilized population PK model28. Since the PK models contained the covariates total body weight (WT) as well as lean body weight (LBW), the covariates WT, height, and sex were sampled from a provided database containing these covariates from an African population. Only values from subjects ≥18 years were sampled.
Lean body weight (LBW) was calculated according to the formula used for the development of pyronaridine popPK model28, as follows:
The apparent kill rate constants at 24 and 96 h were extracted from simulations using the PK/PD model and were visualized using boxplots, stratified per dosing level. A killing rate of >90% was deemed adequate. Since no standard approach is in place to define the probability of target attainment for antimalarial combinations, the probability threshold of >95% was used in accordance with the probability of target attainment assessment for antibiotics43.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All data to replicate th in vitro PD model are available on Figshare capusle (https://doi.org/10.6084/m9.figshare.26088031).
Code availability
All codes to replicate the in vitro-based PKPD model are available on CodeOcean capsule (https://doi.org/10.24433/CO.9928592.v1).
References
World Health Organization. WHO Malaria Report 2019. Malaria Report 2019 (WHO, 2019).
World Health Organization. WHO Malaria Report 2022 (WHO, 2022).
Uwimana, A. et al. Emergence and clonal expansion of in vitro artemisinin-resistant Plasmodium falciparum kelch13 R561H mutant parasites in Rwanda. Nat. Med. 26, 1602–1608 (2020).
van der Pluijm, R. W. et al. Determinants of dihydroartemisinin-piperaquine treatment failure in Plasmodium falciparum malaria in Cambodia, Thailand, and Vietnam: a prospective clinical, pharmacological, and genetic study. Lancet Infect. Dis. 19, 952–961 (2019).
Flegg, J. A. et al. Spatiotemporal spread of Plasmodium falciparum mutations for resistance to sulfadoxine-pyrimethamine across Africa, 1990–2020. PLoS Comput. Biol. 18, e1010317 (2022).
Singh Sidhu, A. B., Verdier-Pinard, D. & Fidock, D. A. Chloroquine resistance in Plasmodium falciparum malaria parasites conferred by pfcrt mutations. Science 298, 210–213 (2002).
Baragaña, B. et al. A novel multiple-stage antimalarial agent that inhibits protein synthesis. Nature 522, 315–320 (2015).
Chu, W.-Y. & Dorlo, T. P. C. Pyronaridine: a review of its clinical pharmacology in the treatment of malaria. J. Antimicrob. Chemother. 78, 2406–2418 (2023).
Kurth, F., Bélard, S., Basra, A. & Ramharter, M. Pyronaridine-artesunate combination therapy for the treatment of malaria. Curr. Opin. Infect. Dis. 24, 564–569 (2011).
Rottmann, M. et al. Preclinical antimalarial combination study of M5717, a Plasmodium falciparum elongation factor 2 inhibitor, and pyronaridine, a hemozoin formation inhibitor. Antimicrob. Agents Chemother. 64, 10–1128 (2020).
Jiménez-Díaz, M. B. et al. Improved murine model of malaria using Plasmodium falciparum competent strains and non-myelodepleted NOD-scid IL2Rgammanull mice engrafted with human erythrocytes. Antimicrob. Agents Chemother. 53, 4533–4536 (2009).
McCarthy, J. S. et al. Safety, pharmacokinetics, and antimalarial activity of the novel Plasmodium eukaryotic translation elongation factor 2 inhibitor M5717: a first-in-human, randomised, placebo-controlled, double-blind, single ascending dose study and volunteer infection stu. Lancet Infect. Dis. 21, 1713–1724 (2021).
White, J. et al. In vitro adaptation of Plasmodium falciparum reveal variations in cultivability. Malar. J. 15, 33 (2016).
Chaorattanakawee, S. et al. Attenuation of Plasmodium falciparum in vitro drug resistance phenotype following culture adaptation compared to fresh clinical isolates in Cambodia. Malar. J. 14, 486 (2015).
Brown, A. C. & Guler, J. L. From circulation to cultivation: Plasmodium in vivo versus in vitro. Trends Parasitol. 36, 914–926 (2020).
Piel, L. et al. Experimental evolution links posttranscriptional regulation to Leishmania fitness gain. PLoS Pathog. 18, e1010375 (2022).
Lee, H. J. et al. Transcriptomic studies of malaria: a paradigm for investigation of systemic host-pathogen interactions. Microbiol. Mol. Biol. Rev. 82, 10–1128 (2018).
Wicha, S. G. et al. New in vitro interaction-parasite reduction ratio assay for early derisk in clinical development of antimalarial combinations. Antimicrob. Agents Chemother. 66, e00556-22 (2022).
Dembele, L. et al. The Plasmodium PI(4)K inhibitor KDU691 selectively inhibits dihydroartemisinin-pretreated Plasmodium falciparum ring-stage parasites. Sci. Rep. 7, 2325 (2017).
Chen, C., Wicha, S. G., Nordgren, R. & Simonsson, U. S. H. Comparisons of analysis methods for assessment of pharmacodynamic interactions including design recommendations. AAPS J. 20, 77 (2018).
Wicha, S. G., Kees, M. G., Kuss, J. & Kloft, C. Pharmacodynamic and response surface analysis of linezolid or vancomycin combined with meropenem against Staphylococcus aureus. Pharm. Res. 32, 2410–2418 (2015).
Wicha, S. G., Chen, C., Clewe, O. & Simonsson, U. S. H. A general pharmacodynamic interaction model identifies perpetrators and victims in drug interactions. Nat. Commun. 8, 2129 (2017).
Nielsen, E. I. & Friberg, L. E. Pharmacokinetic-pharmacodynamic modeling of antibacterial drugs. Pharmacol. Rev. 65, 1053–1090 (2013).
Pearson, R. A., Wicha, S. G. & Okour, M. Drug combination modeling: methods and applications in drug development. J. Clin. Pharmacol. 63, 151–165 (2023).
Bergstrand, M., Hooker, A. C., Wallin, J. E. & Karlsson, M. O. Prediction-corrected visual predictive checks for diagnosing nonlinear mixed-effects models. AAPS J. 13, 143–151 (2011).
Stadler, E. et al. Propensity of selecting mutant parasites for the antimalarial drug cabamiquine. Nat. Commun. 14, 5205 (2023).
Courlet, P., Wilkins, J. J., Oeuvray, C., Gao, W. & Khandelwal, A. Semi-mechanistic population pharmacokinetic/pharmacodynamic modeling of a Plasmodium elongation factor 2 inhibitor cabamiquine for prevention and cure of malaria. Antimicrob. Agents Chemother. 67, e0089123 (2023).
Wattanavijitkul, T. Population Pharmacokinetics of Pyronaridine in the Treatment of Malaria (University of Iowa, 2010).
Linares, M. et al. Identifying rapidly parasiticidal anti-malarial drugs using a simple and reliable in vitro parasite viability fast assay. Malar. J. 14, 441 (2015).
Sanz, L. M. et al. P. falciparum in vitro killing rates allow to discriminate between different antimalarial mode-of-action. PLoS ONE 7, e30949 (2012).
Walz, A. et al. The parasite reduction ratio (PRR) assay version 2: standardized assessment of Plasmodium falciparum viability after antimalarial treatment in vitro. Pharmaceuticals 16, 163 (2023).
Wockner, L. F. et al. Growth rate of Plasmodium falciparum: analysis of parasite growth data from malaria volunteer infection studies. J. Infect. Dis. 221, 963–972 (2020).
Gavigan, C. S., Machado, S. G., Dalton, J. P. & Bell, A. Analysis of antimalarial synergy between bestatin and endoprotease inhibitors using statistical response-surface modelling. Antimicrob. Agents Chemother. 45, 3175–3181 (2001).
Roemhild, R. & Andersson, D. I. Mechanisms and therapeutic potential of collateral sensitivity to antibiotics. PLoS Pathog. 17, e1009172 (2021).
Walliker, D., Hunt, P. & Babiker, H. Fitness of drug-resistant malaria parasites. Acta Trop. 94, 251–259 (2005).
Croft, S. L. et al. Review of pyronaridine anti-malarial properties and product characteristics. Malar. J. 11, 270 (2012).
Dembele, L. et al. Ex vivo Plasmodium malariae culture method for antimalarial drugs screen in the field. ACS Infect. Dis. 7, 3025–3033 (2021).
Trager, W. & Jensen, J. B. Human malaria parasites in continuous culture. Science 193, 673–675 (1976).
Lambros, C. & Vanderberg, J. P. Synchronization of Plasmodium falciparum erythrocytic stages in culture. J. Parasitol. 65, 418 (1979).
Thiam, L. G., Ansah, F., Niang, M., Awandare, G. A. & Aniweh, Y. Short-term cryopreservation and thawing have minimal effects on Plasmodium falciparum ex vivo invasion profile. Front. Cell. Infect. Microbiol. 12, 997418 (2022).
Mohamed, A. F. et al. Dynamic interaction of colistin and meropenem on a WT and a resistant strain of Pseudomonas aeruginosa as quantified in a PK/PD model. J. Antimicrob. Chemother. 71, 1279–1290 (2016).
Wicha, S. G., Huisinga, W. & Kloft, C. Translational pharmacometric evaluation of typical antibiotic broad-spectrum combination therapies against Staphylococcus aureus exploiting in vitro information. CPT Pharmacomet. Syst. Pharmacol. 6, 512–522 (2017).
Mouton, J. W. et al. The role of pharmacokinetics/pharmacodynamics in setting clinical MIC breakpoints: the EUCAST approach. Clin. Microbiol. Infect. 18, E37–E45 (2012).
Acknowledgements
This research was financially supported by the healthcare business of Merck KGaA, Darmstadt, Germany (CrossRef Funder ID: 10.13039/100009945).
Author information
Authors and Affiliations
Contributions
L.D., S.W. and C.D.G. conceived and designed the study. M.M., L.D., A.D., F.S., F.O.M., Y.B. and S.G. performed research, acquired and analyzed the in vitro data. S.W. modeled and visualized the data. P.C. and A.K. reviewed the model outputs. A.D., F.S., O.D., F.O.M., F.D., S.S., M.D., A.A.D., and S.A.S.D. assisted research. S.W. and C.D.G. wrote and edited the original draft. M.M., L.D., P.C., C.O., and T.S. reviewed and edited the article.
Corresponding authors
Ethics declarations
Competing interests
C.D.G., C.O., P.C., and T.S. are employed by Ares Trading S.A., Switzerland, an affiliate of the healthcare business of Merck KGaA, Darmstadt, Germany. S.W. consultancy was funded by the healthcare business of Merck KGaA, Darmstadt, Germany. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Linda Aulin, Gavin Koh and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Maiga, M., Dembele, L., Courlet, P. et al. Towards clinically relevant dose ratios for Cabamiquine and Pyronaridine combination using P. falciparum field isolate data. Nat Commun 15, 7659 (2024). https://doi.org/10.1038/s41467-024-51994-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-024-51994-3
- Springer Nature Limited