Abstract
Visual functions decline with age, but how aging degrades visual functions remains controversial. In the current study, the mechanisms underlying age-related visual declines were examined psychophysically. We developed an efficient method to quickly explore contrast sensitivity as a function of nine spatial frequencies at three levels of external noise in both young and old subjects. Fifty-two young and twenty-six old subjects have been screened for ophthalmological and mental diseases and participated in the experiment. Contrast sensitivity varied significantly with spatial frequency, age, and level of external noise. By adopting a nonlinear observer model, we decomposed contrast sensitivity into inefficiencies in internal additive noise, internal multiplicative noise, perceptual template gain, and/or system non-linearity. Model analysis revealed that aging impacts both internal additive noise and perceptual template gain, and such age-related degradation is tuned to spatial frequency, which is also a good predictor to discriminate old from young. The quick characterization of contrast sensitivity functions at different noise levels and the accompanying analysis developed in the current study may have profound application in other clinical populations.
Similar content being viewed by others
Introduction
Aging is an unavoidable process in human life and affects almost all sensory and cognitive functions. As far as vision is concerned, aging impacts visual acuity1, contrast sensitivity2,3,4, motion5,6, contour perception7,8, and the useful field of view9,10, and so on. In the current study, we focused on how aging affects contrast sensitivity, one of the most fundamental visual functions11.
Contrast sensitivity, depicting creatures’ ability to detect luminance difference, is critical for daily vision. Nameda, et al.12 found that contrast sensitivity at high spatial frequencies started to decrease from 40 years old and decreased at all frequencies from 50–60 years old. Owsley, et al.13 showed that contrast sensitivity began to fall at medium and high spatial frequencies after the age of 40 to 50 years. In a later study, Sloane, et al.14 reported that contrast sensitivity decreased at all spatial frequencies and the decline was particularly prominent at high spatial frequencies. Although there were some discrepancies in the observed contrast sensitivity deficits in old observers, the declining pattern was largely consistent among published studies, i.e. contrast sensitivity began to decrease from high spatial frequencies and then extended to all frequencies after about 60 years old.
On the other hand, how aging affects contrast sensitivity remains controversial. Based on the noise titration method and linear amplification model (LAM)15,16, previous psychophysical studies attributed the decline of contrast sensitivity in the elderly to sampling inefficiency and/or internal noise elevation. Pardhan, et al.17 reported that the loss of contrast sensitivity to grating of 6 cycles per degree (c/d) in aged observers resulted from lowered calculation efficiency without any significant increase of internal noise; Bennett, et al.18 tested contrast sensitivity at the spatial frequencies of 1, 3, and 9 c/d, and found that only calculation efficiency reduced in aged observers. In another study, Pardhan19 claimed that lower calculation efficiency contributed to the declines of contrast sensitivity at 1 and 4 c/d, whereas elevated equivalent noise played a more important role at spatial frequency of 10 c/d in old subjects, which implied that different mechanism(s) were involved in the aging process. Contrary to previous studies that used local and static external noise, Allard, et al.20 adopted extended dynamic noise and concluded that age-related contrast sensitivity loss resulted from elevated internal equivalent noise at low spatial frequency (1c/d) and decreased calculation efficiency (probably combined with increased internal equivalent noise) at higher spatial frequencies (3 and 9 c/d). Arena, et al.21 investigated the sensitivity to motion direction and orientation in young and old adults and demonstrated that aging affected only the internal noise but not the calculation efficiency at low spatial frequency (1 c/d). The inconsistent results among these studies may be due to different spatial-temporal properties of the external noise patterns, the distinct stimulus attributes (e.g. spatial frequency), presentation procedures and/or the availability of feedback.
It is important to point out that almost all previous studies were adhered to the LAM model, which posited that visual signal was analyzed in a linear fashion and the only noise source was additive noise, i.e. irrespective of the input stimulus15. It’s now widely accepted that our visual system is intrinsically non-linear and/or hosts different noise sources22,23,24,25,26. Observer model that incorporates nonlinear transducer function and internal multiplicative noise, i.e. perceptual template model (PTM), has been found to provide better account for visual deficits in amblyopia27 and dyslexia28, system changes after perceptual learning29,30,31 and playing video game32, and attention modulation33,34. In the current study, we attempted to re-examine the intrinsic psychophysical mechanisms underlying age-related change(s) of contrast sensitivity at a variety of spatial frequencies in a relatively large cohort of young and aging populations. With the development of a quick characterization method of contrast sensitivity functions at multiple external noise levels and the application of a non-linear observer model analysis, we found that aging significantly lowered perceptual template gain and elevated internal additive noise in a frequency-dependent fashion.
Results
Contrast sensitivity function (CSF)
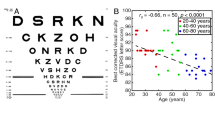
The CSFs at three external noise levels were presented in Figure 1a. An analysis of variance (ANOVA) showed that contrast sensitivity varied significantly with spatial frequency (F(8, 608) = 18.095, p = 2.247 × 10−24), external noise level (F(2, 152) = 140.082, p = 3.242 × 10−35), and age (F(1, 76) = 157.289, p = 3.420 × 10−20). There were significant interactions between spatial frequency and age (F(8, 608) = 4.199, p = 6.535×10-5), and between spatial frequency and noise level (F(16, 1216) = 46.337, p = 1.449 × 10−113), but not between noise level and age (F(2, 152) = 1.549, p = 0.216). The interaction among spatial frequency, noise level, and age was also significant (F(16,1216) = 23.933, p = 1.542 × 10−61). Our results indicated that age-related decline in contrast sensitivity was frequency-dependent, consistent with previous studies13,14,19.
(a) Contrast sensitivity functions at three external noise levels for the average observer of the young (orange) and old (green) group, respectively. (b) Schematic diagram of the AULCSF at low, medium and high noise levels. The orange and green bars denote the young and old group, respectively. Error bar represents standard error.
To index the difference in contrast sensitivity between young and old subjects, we derived the Area Under the Log CSF (AULCSF) for the two groups (Figure 1b). An ANOVA showed that AULCSF differed significantly with external noise level (F(2, 152) = 131.286, p = 7.629 × 10−34) and age (F(1, 76) = 140.003, p = 6.498 × 10−19), but not the interaction between external noise level and age (F(2, 152) = 2.247, p = 0.109). Averaged across observers, the AULCSF of old group was 87%, 78%, and 57% of that in the young group at low, medium and high noise levels, respectively.
Mechanism of contrast sensitivity declines
We fitted PTM to the CSFs for each observer in young and old groups. Averaged across subjects, the model accounted for 91.67% (±1.00%, s.e.) and 88.09% (±1.00%) of data variance in young and old groups, respectively. Although internal multiplicative noise and system non-linearity varied across subjects, they were invariant with spatial frequencies35,36. The internal multiplicative noise was 0.155 ± 0.017 and the system non-linearity was 1.459 ± 0.030 in the old group, and 0.158 ± 0.010 and 1.523 ± 0.027 in the young group, respectively. There was no significant difference in internal multiplicative noise (t(76) = 0.206, p = 0.837) and system non-linearity (t(76) = 1.489, p = 0.141) between the two groups. Average internal additive noise and template gain at the nine spatial frequencies were showed in Figure 2. An ANOVA revealed that internal additive noise varied significantly with age (F(1, 76) = 9.620, p = 0.003) and the interaction of spatial frequency and age (F(8, 608) = 11.086, p = 1.110 × 10−14), but not spatial frequency (F(8, 608) = 0.229, p = 0.986). Post-hoc comparison revealed that internal additive noise was significantly higher (by 75.58% on average) in the aged group than that in the young group at the two highest spatial frequencies, i.e. 5.33 and 8 c/d (t(76) = −2.143, p = 0.035; t(76) = −3.636, p = 0.001, respectively). Our results indicated that aging impacted internal additive noise mostly around high frequency domain.
Template gain varied significantly with spatial frequency (F(8, 608) = 6.153, p = 1.196 × 10−7) and age (F(1, 76) = 53.426, p = 2.284 × 10−10) but not the interaction of the two factors (F(8, 608) = 1.033, p = 0.410), indicating an overall down-regulation of system gain. The magnitude of gain significantly lowered by 39.44% in the aged group averaged across all spatial frequencies.
Correlation among different measures
Contrast sensitivity & internal additive noise
We employed partial correlation analysis (two-tailed) to probe the potential relationships between contrast sensitivity and internal additive noise while excluding the effect of spatial frequency. In addition, the percentile bootstrapping (2,000 bootstrap samples) was used to construct 95% confidence interval (CI) to assess the statistical significance of these correlations. The results showed that contrast sensitivity significantly correlated with internal additive noise at all three external noise levels for the old group (low noise: r = −0.658, p = 2.497 × 10−30, 95% bootstrap CI = [−0.746, −0.556]; medium noise: r = −0.637, p = 6.765 × 10−28, 95% bootstrap CI = [−0.718, −0.545]; high noise: r = −0.176, p = 0.007, 95% bootstrap CI = [−0.311, −0.046]); and in the low (r = −0.621, p = 4.014 × 10−51, 95% bootstrap CI = [−0.690, −0.542]) and medium (r = −0.539, p = 1.372 × 10−36, 95% bootstrap CI = [−0.634, −0.428]) but not high noise (r = −0.038, p = 0.409, 95% bootstrap CI = [−0.151, 0.066]) levels for the young group. Figure 3 showed the residual plus mean values of contrast sensitivity and internal additive noise at nine spatial frequencies after excluding the effect of spatial frequency.
The correlations between contrast sensitivity and internal additive noise at all spatial frequencies at the low, medium and high noise levels for young and old groups, respectively. Data from all observers were pooled. ‘Y’ denotes the young group; ‘O’ denotes the old group; ‘Low’ denotes the condition of the low noise level; ‘Medium’ denotes the condition of the medium noise level; ‘High’ denotes the condition of the high noise level. The data were the residual plus mean values after excluding the effect of spatial frequency.
Contrast sensitivity & system template gain
Partial correlation analysis showed that contrast sensitivity (after excluding the effect of spatial frequency) positively correlated with template gain at medium and high external noise levels (r = 0.540, p = 1.223 × 10−36, 95% bootstrap confidence interval = [0.453, 0.626]; r = 0.859, p = 4.751 × 10−137, 95% bootstrap confidence interval = [0.830, 0.886], respectively), but not at the low noise level (r = 0.067, p = 0.146, 95% bootstrap confidence interval = [−0.041, 0.174]) for the young group, and at all three noise levels (low noise: r = 0.150, p = 0.022, 95% bootstrap confidence interval = [0.018, 0.281]; medium noise: r = 0.543, p = 2.989 × 10−19, 95% bootstrap confidence interval = [0.435, 0.653]; high noise: r = 0.791, p = 3.8040 × 10−51, 95% bootstrap confidence interval = [0.734, 0.857]) for the old group (Figure 4).
The correlations between contrast sensitivity and the gain of perceptual template at all spatial frequencies at low, medium and high noise levels for the young and old group, respectively. Data from all observers were pooled. ‘Y’ denotes the young group; ‘O’ denotes the old group; ‘Low’: low noise level; ‘Medium’: medium noise level; ‘High’: high noise level.
Visual acuity & CSF
We conducted Pearson correlation analysis (two-tailed) on visual acuity (logMAR) and AULCSF in the young and old groups. The results showed that visual acuity correlated significantly with AULCSF at low noise level (r = −0.274, p = 0.049) but not at medium (r = −0.106, p = 0.456) and high noise levels (r = −0.105, p = 0.460) in the young group. On the contrary, visual acuity correlated significantly with AULCSF at the high noise level (r = −0.482, p = 0.013), but not at the low (r = −0.276, p = 0.172) and medium noise levels (r = −0.349, p = 0.081) in the old group.
Classification between old and young
CSF and visual acuity as predictors
The remarkable difference of CSFs between the old and young groups prompted us to evaluate whether CSF is a good indicator of aging. We selected AULCSF, cutoff spatial frequency (cutSF) that characterizes the high spatial frequency limit of spatial vision and visual acuity as predictors. We used a logistic regression analysis to predict membership in the two groups:
where P(old) is the probability of a particular subject being recognized as an old observer, θ0 indexes the constant, θi,m indexes the coefficient corresponding to AULCSF, θj,m indexes the coefficient corresponding to cutSF, θz indexes the coefficient corresponding to visual acuity, and m indexes the noise level.
The prediction analysis revealed two predictors, i.e. AULCSF and cutSF at the middle noise level, leaded to an accuracy up to 94.9% (Hosmer and Lemeshow goodness-of fit, χ2(8) =13.991, p = 0.082). The coefficients of the two predictors and θ0 were −7.613 (p = 0.013), −2.313 (p = 0.001), and 37.597 (p = 0.001), respectively. AULCSF itself discriminated membership of age at a rate of 91.0% (Hosmer and Lemeshow goodness-of fit test, χ2(8) = 4.2423, p = 0.817). The coefficients of the predictor and θ0 were −7.179 (p = 6.267 × 10−5) and 26.392 (p = 8.220 × 10−5), respectively. In other words, AULCSF and cutSF at the middle noise level were the critical factors for discriminating the aged from the young. Moreover, the AULCSF at the middle noise level made a greater contribution tothe discrimination.
PTM parameters as predictors
The PTM characterized contrast sensitivity with internal additive noise, template gain, internal multiplicative noise, and non-linearity. We fed the four fitted parameters as predictors into a logistic regression model (similar to Eq. 1) to evaluate whether the PTM was a good indicator of age. Internal additive noise and gain were classified as the best predictors (Hosmer and Lemeshow goodness-of fit-test, χ2(8) =1.420, p = 0.994), with an accuracy of 93.60%. The coefficients of the two factors and β0 were 140.562 (p = 0.002), −13.641 (p = 4.225 × 10−4), and 8.94 (p = 0.001), respectively.
Discussion
Aging profoundly degrades contrast sensitivity and the magnitude of declines depends on spatial frequency. Our results also suggest that the increase of internal additive noise at high spatial frequencies and the decrease of template gain over a wide range of spatial frequencies underlie the age-related degradation in contrast sensitivity.
Our results indicated different aging mechanisms of contrast sensitivity. At low to medium spatial frequency, aging affected only perceptual template gain but not internal additive noise; at high frequencies, aging impacted both template gain and internal additive noise. The finding of frequency-dependent increase of internal additive noise was similar with Pardhan19 who found the internal additive noise played an important role on contrast sensitivity at high frequency (10 c/d) but not lower frequencies (1, 4 c/d), but contrary to Pardhan, et al.17, Bennett, et al.18, Allard, et al.20, and Silvestre, et al.37. At one hand, many optical38,39,40 and neural factors41,42,43 contributed to the internal noise in visual system and internal additive noise itself may have different components (e.g. photon noise, early and late noise in Silvestre et al.,37). For example, smaller pupil size, lower optical density of the ocular media, and decreased light absorption in the aged population, may have strong influence over contrast sensitivity at high spatial frequency (Owsley, 2011), albeit the optical contribution was minimized through ophthalmological examinations. On the other hand, the characteristic of subjects (e.g. screening criterion), testing frequency (e.g. low vs high), and selected theoretical model (e.g. linear vs non-linear; single noise vs multiple noises) may also perplex the interpretation of age-related declines in contrast sensitivity. For example, subjects were included according to self-report of no known ocular diseases in the study of Bennett, Sekuler, and Ozin (1999). We performed a set of thorough ophthalmological examinations for all our subjects to minimize potential optical influence on contrast sensitivity. In addition, linear model has been reported to have difficulties in explaining several findings that related to processing inefficiency or changes of visual system44.
The down-regulation of GABAnergic inhibition in visual cortex may be the neural cause for internal additive noise elevation in old population. Leventhal, et al.42 found that the exertion of GABA or its receptor agonist rejuvenated V1 neurons of aged monkeys, exhibiting enhanced intracortical inhibition, increased signal-to-noise ratios, and reduced excitability, which suggest that GABA declines may be the basis of abnormal response properties of aging cells. Using Nissl staining and immunohistochemical techniques, Hua, et al.43 found that the density of GABA-immunoreactive neurons and the ratio of GABA-immunoreactive neurons to total V1 neurons of aged cats were significantly lower than those of young cats, which provided direct morphological evidence of decreased GABAergic inhibition in the striate visual cortex of senile animals. In human studies, with the help of magnetic resonance spectroscopy (MRS), researchers have provided some preliminary evidences that occipital GABA was significantly lower in old observers compared to the young observers45,46, and positively associated with task performance45.
The perceptual template or filters describe the observer’s overall tuning characteristics for a signal-valued stimulus, e.g., a spatial frequency filter with a center frequency of the highest gain and a bandwidth such that a range of frequencies adjacent to the center frequency passing through with smaller gains22,33. In this study, we found that aging impacted perceptual template gains over all tested spatial frequencies.
For the young group, contrast sensitivity at low noise level was negatively correlated with internal additive noise (but not perceptual template gain) and contrast sensitivity at high noise level was positively correlated with the perceptual template gain (but not internal additive noise), consistent with our previous study36. But in the old group, contrast sensitivity was negatively correlated with internal additive noise and positively correlated with the perceptual template gain at all the noise levels. We further compared the correlation strength between different measures in the two groups with Fisher z-transformation. The results indicated that the correlations between internal additive noise and contrast sensitivity of old group were significantly greater than that of young group at medium (p = 0.031, single sided test) and high noise (p = 0.041) levels; and the correlation between perceptual template gain and contrast sensitivity in the old group was significantly smaller than that in the young group at high noise level (p = 0.004). We argued that different information processing mechanisms may be involved in young subjects when exposed to different levels of external noise, and aging changed the processing mechanisms.
In this study, we used external noise titration method to quantify the psychophysical mechanism(s) underlying age-related declines in contrast sensitivity. This method and its associated noise settings have been widely used in earlier studies27,28,29,30,31,32,33,34. Allard and his colleagues proposed that the property (e.g. intensity and/or spatiotemporal characteristics) of external noise might affect subject’s information processing strategy and thus change the interpretation of some visual phenomena20,37,47,48,49. For example, with spatiotemporal extended noise, Allard, et al. (2013) found that aging lowered calculation efficiency at high spatial frequency, a finding similar to previous studies17,18, but only elevated internal additive noise at low spatial frequency, different from early studies18,19. With spatially local and temporally extended external noise, we found that aging impacted both internal additive noise and template gain across all tested frequencies, although the effects varied with spatial frequency. Since the characteristic of subjects, the way of how noise and signal integrated (spatial vs temporal), and the assumption of visual information processing (e.g. linear vs non-linear), it’s unlikely to commit to any of the conclusions presently and new studies to directly compare all relevant experimental setups and theoretical frameworks are needed in the future.
It’s worthy to note that we strictly screened our subjects for ophthalmological diseases and other diseases that may affect task fulfillment. Despite the difference of visual acuity was remarkable (t(76) = −4.752, p = 9.310 × 10−6) between the young and old groups, the correlation between visual acuity and AULCSF was inconsistent in the young and old groups at three noise levels, which was similar to the result of Yan, et al.35 at the low (zero) noise level. These results indicated that the declines in contrast sensitivity in the aged group cannot be accounted by the degradation of visual acuity. In this regard, our results may better reflect normal or physiological age-related contrast sensitivity deficits. We concluded that aging elevated internal additive noise at high spatial frequencies and weakened template gain over all spatial frequencies, leading to a reduction of contrast sensitivity across a wide range of spatial frequencies.
Methods
Observers
Fifty-two young, aged 18 to 29 years (22.6 ± 2.6 yrs, mean ± s.d.), and twenty-six old subjects, aged 60 to 80 years (67.3 ± 6.1 yrs), participated in the experiment. The observers were recruited from nearby universities and/or communities (education> 9 yrs) and examined by an ophthalmologist (the third author). The inclusion criteria were: normal or corrected-to-normal visual acuity in both eyes (≥20/25), normal ocular media, free of retinal disease (e.g., strabismus, glaucoma, cataract, and macular degeneration), normal trichromatic vision, normal stereo vision, and free from history of mental diseases and cognitive deficits (MMSE score> 24). The average visual acuity was −0.201 ± 0.073 (logMAR, mean ± s.d.) in the young group and −0.117 ± 0.071 in the old group. Written informed consent was obtained from each observer after the nature of the study was explained. The experimental protocol was approved by the ethics review committee of Institute of Psychology, Chinese Academy of Sciences and all research activities were adhered to the tenets of the Declaration of Helsinki.
Apparatus and stimuli
Stimuli were controlled by a computer running Matlab and PsychToolBox extensions50,51 and presented on DELL color monitor with a spatial resolution of 1600 × 1200 pixels, a refresh rate of 85 Hz, a mean luminance of 40.4 cd/m2, and a circuit-enabled and Gamma-corrected 14-bit gray resolution52. A chin rest was used to minimize head movements during the experiment. The observers viewed the display binocularly in a dimly lit room at a distance of 1.14 meters.
Stimuli were oriented gratings (45° or 135°) of nine spatial frequencies (0.5, 0.67, 1, 1.33, 2, 2.67, 4, 5.33, 8 c/d) at three levels of external noise (white noise, μ =0 and σ ∈ [0 0.08 0.24]). The size of signal gratings was inversely proportional to its frequencies, i.e., 6°, 4.5°, 3°, 2.25°, 1.5°, 1.125°, 0.75°, 0.563°, 0.375°, respectively. They had constant cycles (N = 3). A truncated-Gaussian envelope, whose size was 1:6 to the gratings, blended the image into background. External noise, with same size as the signal, was generated randomly in each trial and the size of noise elements also varied with spatial frequency of the masked grating such that the number of noise elements in each grating cycle was same across all spatial frequencies36,53,54.
Procedure
A grating orientation identification task was used in the experiment (Figure5). Each trial started with a 250-ms fixation cross in the screen center with a brief tone signaling each trial’s onset, which was followed by 125-ms blank screen, two 35-ms frames of external noises, one 35-ms frame of signal grating with random orientation (45° or 135°), and two 35-ms additive frames of external noises. Observers reported the grating orientation with keyboard press. No feedback was provided. Inter-trial interval was 500 ms.
Design
A quick procedure was used to evaluate CSFs at different noise levels35,55. Briefly, the quick method characterized CSF with a four-parameter log-parabola function, e.g. peak gain (or maximum contrast sensitivity), spatial frequency that corresponds to peak gain, low-frequency truncation, and bandwidth that defines the parabolic function’s full-width at half-height (in octaves). Different combinations of parameter values were assigned a prior as a four-dimensional probability density function (i.e. parameter space). The stimuli space consisted of the possible grating contrast ranged from 0.1% to 100% in 1 dB steps and nine spatial frequencies (0.5, 0.67, 1, 1.33, 2, 2.67, 4, 5.33, and 8 c/d). Based on observer’s response (correct or incorrect) on a grating of a certain spatial frequency and contrast, the parameter probability density function was updated using Bayes’ rule (i.e. posterior). The contrast and spatial frequency of the signal grating in next trial was chosen such that the expected entropy of the probability density function after that trial was the lowest (i.e. maximal information gain). The experiment consisted of 300 trials, with 100 trials per external noise level.
Analysis
To obtain CSF at each noise level, we sampled 1,000 sets of CSF parameters from the posterior distribution of CSF parameters, constructed 1,000 corresponding CSF curves, and obtained the empirical distribution of the CSF. This re-sampling procedure automatically takes into account the covariance structure in the posterior distribution of the CSF parameters and allows us to assess the precision of the estimated CSF curve35,56.
The AULCSF, a summary metric of the CSF function35,55,57,58, was calculated as the integration of the area under the log CSF curve from 0.5 to 8 c/d. The cutSF was defined as the spatial frequency at which contrast sensitivity is 1.0.
The perceptual template model (PTM, Figure6; Lu & Dosher, 1999) described an observer’s perceptual sensitivity as a function of performance level (d’) and external noise level with four free parameters, i.e. the signal non-linearity (γ), gain of the perceptual template (β) that expressed relative to the external noise, the internal additive noise whose intensity was invariant to input stimulus energy (Na), and internal multiplicative noise whose intensity co-varied with the input stimulus energy (Nm):
where c is contrast threshold, Next is the external noise, d’ is the performance level (80.3% percent correct for qCSF method or d’ = 1.705), and γ, β, Nm, Na are the four free parameters used to characterize system inefficiency.
The PTM model was fitted directly to the estimated CSF for each observer in the young and old groups by a weighted least-square method, which was used to minimize \({\sum }^{}{(C{S}_{predicted}-C{S}_{measured})}^{2}\). CSpredicted is the model-predicted contrast sensitivity (i.e. log(1/contrast threshold)) at the tested spatial frequencies and noise levels, and CSmeasured is the measured contrast sensitivity. Our recent studies have demonstrated that the slope of contrast psychometric function was invariant to spatial frequencies and external noises35,36, which rules out the possibility that non-linearity (γ) and multiplicative noise (Nm) change along with spatial frequency and external noise22. The goodness-of-fit was evaluated by r2:
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Elliott, D. B., Yang, K. C. & Whitaker, D. Visual acuity changes throughout adulthood in normal, healthy eyes: seeing beyond 6/6. Optometry and vision science: official publication of the American Academy of Optometry 72, 186–191, https://doi.org/10.1097/00006324-199503000-00006 (1995).
Crassini, B., Brown, B. & Bowman, K. Age-related changes in contrast sensitivity in central and peripheral retina. Perception 17, 315–332, https://doi.org/10.1068/p170315 (1988).
Elliott, D. B., Whitaker, D. & MacVeigh, D. Neural contribution to spatiotemporal contrast sensitivity decline in healthy ageing eyes. Vision research 30, 541–547, https://doi.org/10.1016/0042-6989(90)90066-T (1990).
Burton, K. B., Owsley, C. & Sloane, M. E. Aging and neural spatial contrast sensitivity: photopic vision. Vision research 33, 939–946, https://doi.org/10.1016/0042-6989(93)90077-A (1993).
Andersen, G. J. & Enriquez, A. Aging and the detection of observer and moving object collisions. Psychology and aging 21, 74–85, https://doi.org/10.1037/0882-7974.21.1.74 (2006).
Roudaia, E., Bennett, P. J., Sekuler, A. B. & Pilz, K. S. Spatiotemporal properties of apparent motion perception and aging. Journal of vision 10, 5, https://doi.org/10.1167/10.14.5 (2010).
Roudaia, E., Bennett, P. J. & Sekuler, A. B. The effect of aging on contour integration. Vision research 48, 2767–2774, https://doi.org/10.1016/j.visres.2008.07.026 (2008).
Casco, C., Robol, V., Barollo, M. & Cansino, S. Effects of aging on visual contour integration and segmentation. Investigative ophthalmology & visual science 52, 3955–3961, https://doi.org/10.1167/iovs.10-5439 (2011).
Ball, K. K., Beard, B. L., Roenker, D. L., Miller, R. L. & Griggs, D. S. Age and visual search: expanding the useful field of view. Journal of the Optical Society of America. A, Optics and image science 5, 2210–2219, https://doi.org/10.1364/JOSAA.5.002210 (1988).
Sekuler, A. B., Bennett, P. J. & Mamelak, M. Effects of aging on the useful field of view. Experimental aging research 26, 103–120, https://doi.org/10.1080/036107300243588 (2000).
Nicholas, J. J., Heywood, C. A. & Cowey, A. Contrast sensitivity in one-eyed subjects. Vision research 36, 175–180, https://doi.org/10.1016/0042-6989(95)00119-K (1996).
Nameda, N., Kawara, T. & Ohzu, H. Human visual spatio-temporal frequency performance as a function of age. Optometry and vision science: official publication of the American Academy of Optometry 66, 760–765, https://doi.org/10.1097/00006324-198911000-00007 (1989).
Owsley, C., Sekuler, R. & Siemsen, D. Contrast sensitivity throughout adulthood. Vision research 23, 689–699, https://doi.org/10.1016/0042-6989(83)90210-9 (1983).
Sloane, M. E., Owsley, C. & Alvarez, S. L. Aging, senile miosis and spatial contrast sensitivity at low luminance. Vision research 28, 1235–1246, https://doi.org/10.1016/0042-6989(88)90039-9 (1988).
Pelli, D. G. Effects of visual noise. Ph.D. disseration, University of Cambridge, Cambridge, UK (1981).
Pelli, D. G. The quantum efficiency of vision. C. Blakemore(Ed.) Vision: Coding and Efficiency, pp. 3-24. Cambridge: Cambridge University Press, https://doi.org/10.1017/CBO9780511626197.003 (1990).
Pardhan, S., Gilchrist, J., Elliott, D. B. & Beh, G. K. A comparison of sampling efficiency and internal noise level in young and old subjects. Vision research 36, 1641–1648, https://doi.org/10.1016/0042-6989(95)00214-6 (1996).
Bennett, P. J., Sekuler, A. B. & Ozin, L. Effects of aging on calculation efficiency and equivalent noise. Journal of the Optical Society of America. A, Optics, image science, and vision 16, 654–668, https://doi.org/10.1364/JOSAA.16.000654 (1999).
Pardhan, S. Contrast sensitivity loss with aging: sampling efficiency and equivalent noise at different spatial frequencies. Journal of the Optical Society of America. A, Optics, image science, and vision 21, 169–175, https://doi.org/10.1364/JOSAA.21.000169 (2004).
Allard, R., Renaud, J., Molinatti, S. & Faubert, J. Contrast sensitivity, healthy aging and noise. Vision research 92, 47–52, https://doi.org/10.1016/j.visres.2013.09.004 (2013).
Arena, A., Hutchinson, C. V., Shimozaki, S. S. & Long, M. D. Visual discrimination in noise: behavioural correlates of age-related cortical decline. Behavioural brain research 243, 102–108, https://doi.org/10.1016/j.bbr.2012.12.039 (2013).
Lu, Z. L. & Dosher, B. A. Characterizing human perceptual inefficiencies with equivalent internal noise. Journal of the Optical Society of America. A, Optics, image science, and vision 16, 764–778, https://doi.org/10.1364/JOSAA.16.000764 (1999).
Burgess, A. E. & Colborne, B. Visual signal detection. IV. Observer inconsistency. Journal of the Optical Society of America. A, Optics and image science 5, 617–627, https://doi.org/10.1364/JOSAA.5.000617 (1988).
Eckstein, M. P., Ahumada, A. J. Jr. & Watson, A. B. Visual signal detection in structured backgrounds. II. Effects of contrast gain control, background variations, and white noise. Journal of the Optical Society of America. A, Optics, image science, and vision 14, 2406–2419, https://doi.org/10.1364/JOSAA.14.002406 (1997).
Lu, Z. L. & Dosher, B. A. Visual psychophysics: From laboratory to theory, https://doi.org/10.7551/mitpress/9780262019453.001.0001 (Cambridge, MA, 2014).
Lu, Z. L. & Dosher, B. A. Characterizing observers using external noise and observer models: assessing internal representations with external noise. Psychol Rev 115, 44–82, https://doi.org/10.1037/0033-295X.115.1.44 (2008).
Xu, P., Lu, Z. L., Qiu, Z. & Zhou, Y. Identify mechanisms of amblyopia in Gabor orientation identification with external noise. Vision research 46, 3748–3760, https://doi.org/10.1016/j.visres.2006.06.013 (2006).
Sperling, A. J., Lu, Z. L., Manis, F. R. & Seidenberg, M. S. Deficits in perceptual noise exclusion in developmental dyslexia. Nature neuroscience 8, 862–863, https://doi.org/10.1038/nn1474 (2005).
Dosher, B. A. & Lu, Z. L. Perceptual learning reflects external noise filtering and internal noise reduction through channel reweighting. Proceedings of the National Academy of Sciences of the United States of America 95, 13988–13993, https://doi.org/10.1073/pnas.95.23.13988 (1998).
Bower, J. D. & Andersen, G. J. Aging, perceptual learning, and changes in efficiency of motion processing. Vision research 61, 144–156, https://doi.org/10.1016/j.visres.2011.07.016 (2012).
Zhang, P. et al. High reward enhances perceptual learning. Journal of vision 18, 11, https://doi.org/10.1167/18.8.11 (2018).
Bejjanki, V. R. et al. Action video game play facilitates the development of better perceptual templates. Proceedings of the National Academy of Sciences of the United States of America 111, 16961–16966, https://doi.org/10.1073/pnas.1417056111 (2014).
Lu, Z. L. & Dosher, B. A. External noise distinguishes attention mechanisms. Vision research 38, 1183–1198, https://doi.org/10.1016/S0042-6989(97)00273-3 (1998).
Dosher, B. A. & Lu, Z. L. Mechanisms of perceptual attention in precuing of location. Vision research 40, 1269–1292, https://doi.org/10.1016/S0042-6989(00)00019-5 (2000).
Yan, F. F., Hou, F., Lu, Z. L., Hu, X. P. & Huang, C. B. Efficient Characterization and Classification of Contrast Sensitivity Functions in Aging. Scientific reports 7, https://doi.org/10.1038/s41598-017-05294-0 (2017).
Chen, G. et al. Noise provides new insights on contrast sensitivity function. PloS one 9, e90579, https://doi.org/10.1371/journal.pone.0090579 (2014).
Daphné Silvestre, Angelo Arleo, Rémy Allard, Internal noise sources limiting contrast sensitivity. Scientific Reports 8 (1) https://doi.org/10.1038/s41598-018-20619-3 (2018).
Campbell, F. W. & Green, D. G. Optical and retinal factors affecting visual resolution. J Physiol 181, 576–593, https://doi.org/10.1113/jphysiol.1965.sp007784 (1965).
Pokorny, J., Smith, V. C. & Lutze, M. Aging of the human lens. Appl Opt 26, 1437–1440, https://doi.org/10.1364/AO.26.001437 (1987).
van de Kraats, J. & van Norren, D. Optical density of the aging human ocular media in the visible and the UV. Journal of the Optical Society of America. A, Optics, image science, and vision 24, 1842–1857, https://doi.org/10.1364/JOSAA.24.001842 (2007).
Schmolesky, M. T., Wang, Y., Pu, M. & Leventhal, A. G. Degradation of stimulus selectivity of visual cortical cells in senescent rhesus monkeys. Nature neuroscience 3, 384–390, https://doi.org/10.1038/73957 (2000).
Leventhal, A. G., Wang, Y., Pu, M., Zhou, Y. & Ma, Y. GABA and its agonists improved visual cortical function in senescent monkeys. Science 300, 812–815, https://doi.org/10.1126/science.1082874 (2003).
Hua, T., Kao, C., Sun, Q., Li, X. & Zhou, Y. Decreased proportion of GABA neurons accompanies age-related degradation of neuronal function in cat striate cortex. Brain research bulletin 75, 119–125, https://doi.org/10.1016/j.brainresbull.2007.08.001 (2008).
Lu, Z. L. & Dosher, B. A. Perceptual learning retunes the perceptual template in foveal orientation identification. Journal of vision 4, 44–56, https://doi.org/10.1167/4.1.5 (2004).
Simmonite, M. et al. Age-Related Declines in Occipital GABA are Associated with Reduced Fluid Processing Ability. Acad Radiol, https://doi.org/10.1016/j.acra.2018.07.024 (2018).
Hermans, L. et al. Brain GABA Levels Are Associated with Inhibitory Control Deficits in Older Adults. The Journal of neuroscience: the official journal of the Society for Neuroscience 38, 7844–7851, https://doi.org/10.1523/JNEUROSCI.0760-18.2018 (2018).
Silvestre, D., Cavanagh, P., Arleo, A. & Allard, R. Adding temporally localized noise can enhance the contribution of target knowledge on contrast detection. Journal of vision 17, https://doi.org/10.1167/17.2.5 (2017).
Allard, R. & Faubert, J. To characterize contrast detection, noise should be extended, not localized. Frontiers in psychology 5, https://doi.org/10.3389/fpsyg.2014.00749 (2014).
Allard, R. & Cavanagh, P. Crowding in a detection task: external noise triggers change in processing strategy. Vision research 51, 408–416, https://doi.org/10.1016/j.visres.2010.12.008 (2011).
Brainard, D. H. The Psychophysics Toolbox. Spatial vision 10, 433–436, https://doi.org/10.1163/156856897X00357 (1997).
Pelli, D. G. The VideoToolbox software for visual psychophysics: transforming numbers into movies. Spatial vision 10, 437–442, https://doi.org/10.1163/156856897X00366 (1997).
Li, X., Lu, Z. L., Xu, P., Jin, J. & Zhou, Y. Generating high gray-level resolution monochrome displays with conventional computer graphics cards and color monitors. J Neurosci Methods 130, 9–18, https://doi.org/10.1016/S0165-0270(03)00174-2 (2003).
Hou, F., Lu, Z. L. & Huang, C. B. The external noise normalized gain profile of spatial vision. Journal of vision 14, 9, https://doi.org/10.1167/14.13.9 (2014).
Rovamo, J., Franssila, R. & Nasanen, R. Contrast sensitivity as a function of spatial frequency, viewing distance and eccentricity with and without spatial noise. Vision research 32, 631–637, https://doi.org/10.1016/0042-6989(92)90179-M (1992).
Lesmes, L. A., Lu, Z. L., Baek, J. & Albright, T. D. Bayesian adaptive estimation of the contrast sensitivity function: the quick CSF method. Journal of vision 10(17), 11–21, https://doi.org/10.1167/10.3.17 (2010).
Hou, F., Lesmes, L., Bex, P., Dorr, M. & Lu, Z. L. Using 10AFC to further improve the efficiency of the quick CSF method. Journal of vision 15, 2, https://doi.org/10.1167/15.9.2 (2015).
Oshika, T., Okamoto, C., Samejima, T., Tokunaga, T. & Miyata, K. Contrast sensitivity function and ocular higher-order wavefront aberrations in normal human eyes. Ophthalmology 113, 1807–1812, https://doi.org/10.1016/j.ophtha.2006.03.061 (2006).
Hou, F. et al. qCSF in clinical application: efficient characterization and classification of contrast sensitivity functions in amblyopia. Investigative ophthalmology & visual science 51, 5365–5377, https://doi.org/10.1167/iovs.10-5468 (2010).
Acknowledgements
This work was supported by National Key Research and Development Program of China (2018YFC0705100 to CBH); National Natural Science Foundation of China (NSFC 31230032, 31470983 to CBH); the Department of Human Resources and Social Security of Zhejiang Province (Qianjiang Talent Project, QJD1803028 to FH); the Scientific Foundation of Institute of Psychology, Chinese Academy of Sciences (Y7CX332008 to FFY); Chinese Post-doctoral Research Foundation (2018M641514 to FFY); and Medical science and technology project of health commission of Hebei province (HYL 152777134 to HYL).
Author information
Authors and Affiliations
Contributions
F.-F.Y., F.H. and C.-B.H. designed research; F.-F.Y., H.L., J.Y., L.C., Y.W. and G.C. performed research; F.-F.Y., F.H. and C.-B.H. analyzed data; and F.-F.Y., F.H. and C.-B.H. wrote the paper. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yan, FF., Hou, F., Lu, H. et al. Aging affects gain and internal noise in the visual system. Sci Rep 10, 6768 (2020). https://doi.org/10.1038/s41598-020-63053-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-63053-0
- Springer Nature Limited