Abstract
We profiled gene expression signatures to distinguish rheumatoid arthritis (RA) from non-inflammatory arthralgia (NIA), self-limiting arthritis (SLA), and undifferentiated arthritis (UA) as compared to healthy controls as novel potential biomarkers for therapeutic responsiveness. Global gene expression profiles of PBMCs from 43 drug-naïve patients presenting with joint symptoms were evaluated and differentially expressed genes identified by comparative analysis with 24 healthy volunteers. Patients were assessed at presentation with follow up at 6 and 12 months. Gene ontology and network pathway analysis were performed using DAVID Bioinformatics Resources v6.7. Gene expression profiles were also determined after disease-modifying anti-rheumatic drug (DMARD) treatment in the inflammatory arthritis groups (i.e. RA and UA) and confirmed by qRT-PCR. Receiver operating characteristic (ROC) curves analysis and Area Under the Curve (AUC) estimation were performed to assess the diagnostic value of candidate gene expression signatures. A type I interferon (IFN) gene signature distinguished DMARD-naïve patients who will subsequently develop persistent inflammatory arthritis (i.e. RA and UA) from those with NIA. In patients with RA, the IFN signature is characterised by up-regulation of SIGLEC1 (p = 0.00597) and MS4A4A (p = 0.00000904). We also identified, EPHB2 (p = 0.000542) and PDZK1IP1 (p = 0.0206) with RA-specific gene expression profiles and elevated expression of the ST6GALNAC1 (p = 0.0023) gene in UA. ROC and AUC risk score analysis suggested that MSA4A (AUC: 0.894, 0.644, 0.720), PDZK1IP1 (AUC: 0.785, 0.806, 0.977), and EPHB2 (AUC: 0.794, 0.723, 0.620) at 0, 6, and 12 months follow-up can accurately discriminate patients with RA from healthy controls and may have practical value for RA diagnosis. In patients with early inflammatory arthritis, ST6GALNAC1 is a potential biomarker for UA as compared with healthy controls whereas EPHB2, MS4A4A, and particularly PDZK1IP1 may discriminate RA patients. SIGLEC1 may also be a useful marker of disease activity in UA.
Similar content being viewed by others
Introduction
A genetic basis for rheumatoid arthritis (RA) has long been established most notably in the association of HLA-Dw4 with RA1,2. Some reports have estimated the genetic contribution to account for up to two-thirds of RA susceptibility3 with the HLA locus contributing 30 to 50%4. Recent efforts using high-density genetic mapping have identified new genetic susceptibility loci for RA5,6. A recent genome-wide association study meta-analysis identified 42 significant novel RA risk loci, bringing the total to 1016. Further in silico analysis based on functional annotation, cis-acting expression quantitative trait loci, pathway analyses and genetic overlap with human primary immunodeficiency, haematological cancer somatic mutations and knockout mouse phenotypes identified 98 biological candidate genes at these 101 risk loci. Among these new susceptibility loci, a number of which were associated with RA overall and several of which were specifically associated with disease that was anti-citrullinated peptide antibody positive5. Furthermore, many of these genes are the targets of approved therapies for RA suggesting that drugs approved for other indications may be repurposed for the treatment of RA. Although candidate gene-based and comprehensive in silico genome-wide association studies (GWAS) study meta-analysis have contributed to defining this heritability, identifying more than 98 biological candidate genes at 101 non-HLA RA susceptibility loci6,7, very little is known about how these genetic risks influence disease development or treatment response in human studies.
The 1987 American College of Rheumatology (ACR) classification criteria were developed to permit recruitment of relatively homogeneous patient phenotypes into trials but they were not designed to identify patients with early stage disease. Evidence now supports subdivision of the RA syndrome into two major subsets based on the presence or absence of autoantibodies to citrullinated protein antigen (ACPA)8. The introduction of new ACR/European League Against Rheumatism (EULAR) classification criteria permit earlier identification and treatment of persistent inflammatory arthritis [i.e. RA and undifferentiated arthritis (UA)]9,10 as there is compelling evidence for best outcomes if effective therapy is implemented early11. With the increasing range and availability of effective targeted therapies in the clinic and in development12, a contemporary challenge is to predict which patients will benefit from early intervention with drugs of particular mechanism of action.
Gene expression profiling studies in PBMC13 and validated in synovial tissue14 offer a non-biased, complementary approach to GWAS studies and may confirm risk associations at the level of gene expression associated with pathology, as well as identifying biomarkers of therapeutic response to targeted therapies15. However, there are only a few studies reported in drug-naïve early arthritis patient cohorts. In one study, Pratt et al.16 identified IL-6-mediated STAT-3 signalling in purified peripheral blood CD4 T cells of 173 patients who manifested the earliest clinical phase of RA, which is most noticeable in seronegative disease. However, the role of this pathway in disease pathogenesis awaits further clarification. In another study, Cooles et al.17 conducted phenotypic and transcriptomic profiling of peripheral blood plasmacytoid and conventional dendritic cells in early drug-naïve RA and compared findings with healthy controls; however transcriptional analysis involved a targeted immunology-related gene panel not a genome scale analysis.
Here we report the results of gene expression signatures of a longitudinal study in well-defined clinical cohorts of drug-naïve, early inflammatory arthritis patients to distinguish RA from non-inflammatory arthralgia (NIA), self-limiting arthritis (SLA, and UA as compared to healthy controls as novel potential biomarkers for therapeutic responsiveness.
Comparisons of gene expression levels from baseline to post-treatment at 6 months and at 12 months were performed. Uniquely, our study included two comparator groups which allowed us to discriminate gene expression profiles unique to drug-naïve RA and/or UA patients as distinct from those with SLA and NIA.
Methods
Subjects and study design
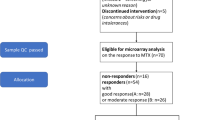
This study was performed in compliance with the Declaration of Helsinki. Consecutive, DMARD- and corticosteroid-naïve patients with peripheral joint symptoms presenting to the Charing Cross Hospital Early Arthritis Clinic were recruited with approval of the Riverside Research Ethics Committee (RREC Ref #07/H0706/127). A total of 43 subjects were enrolled and a sample of venous blood was drawn at their first clinic visit and all provided written, informed consent. Patients were assessed by a consultant rheumatologist at presentation with follow up at 6 and 12 months when additional blood samples were taken. Study subjects were assigned to prospective or retrospective classification categories based on clinical findings at presentation and follow up. Sample collection commenced before publication of the 2010 ACR/EULAR classification criteria. The classification of RA was therefore assigned prospectively to those patients fulfilling 1987 American College of Rheumatology criteria18. Where there was definite evidence of peripheral inflammatory arthritis that persisted during the first 6 months follow-up, and patients fulfilled neither criteria for RA nor other inflammatory joint disease (e.g. ankylosing spondylitis, sarcoidosis), the patient was assigned a retrospective classification of UA. Where there was definite peripheral arthritis at presentation but the patient was deemed to be in remission by 6 months follow-up without the need for DMARDs, the patient was assigned a retrospective classification of SLA. 23 patients in this analysis had persistent inflammatory arthritis [i.e. 14 RA and 9 UA. Another 7 subjects had SLA]. In addition, a fourth group of 13 patients presenting with peripheral joint pain but with no clinical, serological or imaging evidence of inflammation over 1 year of follow-up were assigned a retrospective classification of NIA.
A single blood sample was also collected from 24 healthy laboratory staff volunteers with no previous diagnosis of chronic inflammatory or autoimmune diseases and served as a reference for the clinical cohorts. Clinical characteristics of all study participants are summarised in Table 1. Disease activity scores (DAS28), serology and DMARD use for the RA patients analysed in the longitudinal arm of this study are shown in Table 2.
Blood Sampling and RNA isolation for microarray hybridization and RT-PCR
Samples of venous blood were collected in a CPT Vacutainer cell purification tube (Becton Dickinson, Franklin Lakes, NJ, USA) to isolate PBMCs for gene expression profiling. For RNA extraction PBMCs were separated from whole blood within two hours of blood draw, according to the manufacturer’s instructions and described previously13 then snap frozen and stored in liquid nitrogen until processed for analysis. Total RNA isolation was performed using QIA RNeasy mini kit (Qiagen, Valencia, CA) according to the manufacturer’s recommendations. Samples were subjected to on-column DNase treatment to remove potential contaminating DNA. Eluted RNA was quantified using a ND-8000 Spectrophotometer (Nanodrop, Wilmington, DE). RNA quality was accessed on Agilent Bioanalyzer (Agilent, Santa Clara, CA). 100 ng total RNA were used to generate biotin labelled cRNA using 3’ IVT express kit (Affymetrix, Santa Clara, CA) according to manufacturer’s instructions. The kit uses an oligo T7 primer in a reverse transcription reaction followed by in vitro transcription reaction with biotin labelled UTP and CTP.
Microarray hybridization
10 μg of cRNA were fragmented and hybridized to GeneChip(R) Human Genome U133 plus 2 array (Affymetrix, Santa Clara, CA) representing over 47, 000 RNA transcripts and variants (quality control and pre-processing of the microarray were conducted according to the manufacturers recommendation). Hybridized arrays were stained according to the manufacturers’ protocols (Affymetrix, Santa Clara, CA) on a Fluidics Station 450 and scanned on an Affymetrix scanner 3000 7 G. All array images were inspected for defects and quality via Expressionist Refiner Array (Genedata, Switzerland).
Data filtering and analysis
Cel files containing raw gene expression intensity data were imported into ArrayStar microarray analysis software (DNASTAR, Inc. Madison, WI, USA). In order to minimise the effect of technical variability, the RMT (random matrix theory) method19 was carried out to normalise across all chips using chip-included internal controls. Positively transcribed genes were selected if their mean expression levels were at least two fold increased or decreased compared to healthy controls (p < 0.05) based on the student’s test. The biological functions of candidate genes were classified using the Database for Annotation, Visualization and Integrated Discovery (DAVID) Bioinformatics Resources v6.7 (The Database for Annotation, Visualization and Intergraded Discovery) and gene ontology analysis were called significant with a false discovery rate (FDR) < 0.0520. The microarray data will be submitted to the Gene Expression Omnibus (GEO) public repository.
Statistical analysis
Differences in mean expression between groups were tested by ANOVA using ArrayStar microarray analysis software (DNASTAR, Inc. Madison, WI, USA). P-values < 0.05 were considered significant.
Quantitative real-time PCR analysis
To measure the expression level of genes of interest, we designed a 48-gene custom Taqman Low Density Array (TLDA, ThermoFisher Scientific, Waltham, MA), including multiple housekeeping genes. To perform RT-qPCR reaction, 100 ng of each RNA sample was first reverse transcribed to cDNA using High Capacity cDNA archive kit (ThermoFisher Scientific, Waltham, MA). Then each cDNA was mixed with 2x TaqMan® Fast Universal PCR Master Mix (ThermoFisher Scientific, Waltham, MA) and 100μl cDNA-PCR mix was loaded onto a TLDA card. TLDA cards were processed on ViiA7 instrument (ThermoFisher Scientific, Waltham, MA) following the manufacturer’s protocol. Normalization of RNA expression data (raw Ct) was based on the delta Ct method. The geometric mean of four housekeeping controls (PGK1, ZNF592, GUSB, and 18 S) was used as the normalizing reference. For statistical analysis the Welch test was applied to the normalized data (delta Ct) in all four clinical groups at baseline compared to healthy control. Differential expression was defined as a minimum 1.5 fold change and a Q value of <0.10 (multiple test correction). The same criteria were applied to filter significant changes in longitudinal comparisons of gene expression levels from baseline to post-treatment at 6 months and for the 6 to 12 months post-treatment interval.
Receiver Operating Characteristics
Receiver operating characteristic (ROC) curves analysis and Area Under the Curve (AUC) estimation were performed as described in the literature21,22,23,24,25. ROC analysis and AUC estimation were used to determine if baseline levels of any of the SIGLEC1, MSA4A, PDZK1IP1, EPHB2, and ST6GALNAC1 gene expression signature scores may discriminate between RA patients at Day 0, 6 months and 12 months follow-up as compared with healthy control.
We also determined if baseline levels of any of these gene expression signature scores may discriminate SLA, NIA, UA, and RA patients from healthy controls.
The sensitivity, specificity, and 95% confidence interval (CI) values were determined at the optimal cut-off value (threshold) from the ROC curve as described21,22,23,24,25. Analysis was performed using prism v8.
Results
Gene microarray analysis in patients presenting to the early arthritis clinic
In the NIA cohort as a whole a total of 617 transcripts, representing 508 genes, displayed a 2-fold change compared to the healthy control group, with comparable numbers of more highly-expressed (51%) and under-expressed (49%) transcripts (p < 0.05). The distribution of differentially expressed (DE) transcripts was similar within the UA (100 up, 87 down) and SLA (28 up, 38 down) cohorts, whereas in RA most (241 were up-regulated and just 53 down-regulated. Conversely, in the NIA cohort most DE transcripts (262) were down-regulated and 17 up-regulated (Fig. 1).
Differentially expressed genes unique to persistent arthritis patient groups
To determine DE gene expression profiles unique to persistent arthritis we removed transcripts from the RA and UA groups which were also up co-regulated in the SLA and NIA groups. This identified 277 transcripts (231 annotated genes, 14 uncharacterized) which are potentially uniquely up-regulated in persistent arthritis. Of the 277 DE up-regulated transcripts in the persistent arthritis group, 194 transcripts representing 164 genes (156 annotated, 8 uncharacterized), were only elevated in RA (Additional File 2A), and 62 transcripts representing 61 genes (55 annotated, 6 uncharacterized), were unique to UA (Additional File 2B). One gene, protein S (alpha) (PROS1), displayed elevated expression in RA but a down-regulated expression pattern in UA (Additional File 2A). A further group of 21 transcripts, representing 17 genes, were elevated in both groups (Additional File 2C).
Of the total 111 transcripts down-regulated in the persistent arthritis group, only 8 transcripts representing 8 genes, were uniquely down in RA (Additional File 2A) compared to 27 genes only down-regulated in the UA (Additional File 2E) group.
Ontology enrichment analysis of genes differentially expressed in persistent inflammatory arthritis groups
DE genes unique to the RA and UA cohorts were annotated and categorised according to biological function using gene clustering with DAVID bioinformatics software against a background of all human genes. Gene set enrichment analysis of up-regulated RA-specific genes revealed 151 genes associated with GO terms in 6 clusters of biological processes with an FDR < 0.05. These included secretion via cytoplasmic membrane-bounded vesicles; haemostasis, blood coagulation and the regulation of body fluid levels; response to infection; chemotaxis; active membrane transport and regulation of protein kinase activity (Table 3). A single cluster comprising 13 genes involved in an active immune response was associated with genes up-regulated specifically in the UA group (data not shown). No significant clusters were associated with down-regulated genes in either of the persistent arthritis groups.
RA and UA microarray gene signature responses to treatment regime
To assess the effect of DMARD treatment in RA and UA cohorts, we performed a ratio analysis based on our microarray data. This was expressed as fold-decrease and we considered greater than 2 fold reductions in transcript levels, at either 6 months and/or 12 months after the initiation of treatment with conventional synthetic DMARDs (csDMARDs) +/− steroids, or with steroids alone as detailed in Table 2, to be indicative of a treatment response. By this calculation, a small number of transcripts were found to be lower in RA and UA than in healthy controls or in response to csDMARD therapy. This could be due to the small sample size and/or a small number of transcripts were found to be lower in RA and UA than in healthy controls. Among the few transcripts that were found to be downregulated in RA and UA in response to csDMARD therapy, 25/164 unique RA genes (15%) exhibited at minimum two-fold down regulation post treatment (methotrexate) including 7 of the 8 RA-specific type I interferon response (IFN) genes namely, sialic acid binding Ig-like lectin 1 (SIGLEC1), epithelial stromal interaction 1 (breast) (EPSTI1), 2′-5′-oligoadenylate synthetase-like (OASL), interferon-induced protein 44 (IFI44), ISG15 ubiquitin-like modifier (ISG15) and membrane-spanning 4-domains, subfamily A, member 4 (MS4A4A) and receptor (chemosensory) transporter protein 4 (RTP4)(Fig. 2 and Additional File 3A). In the UA cohort, 38/64 (60%) of the uniquely elevated genes demonstrated a treatment response (corticosteroids) (Fig. 2 and Additional File 3B). Among the 17 genes commonly elevated in UA and RA, 10 were attenuated by DMARDs. This category included potassium inwardly-rectifying channel, subfamily J, member 2 (KCNJ2) and all 7 of the IFN genes that were only reduced following the RA treatment regimen. Two genes, tumour necrosis factor receptor superfamily, member 10c, decoy without an intracellular domain (TNFRSF10C) and membrane metallo-endopeptidase (MME) responded specifically to treatment in the UA group (Fig. 2 and Additional File 3C).
RA and UA gene signature responses to treatment regimes. A heat map representing colour-coded expression levels of differentially expressed (normalised, log2 fold changes) responsive genes in rheumatoid arthritis (RA) and undifferentiated arthritis (UA) patients following baseline (T0), 6 months (T6) and 12 months (T12) of methotrexate or corticosteroid therapy.
Quantitative validation of selected gene expression profiles
The expression profiles of 20 genes of biological interest identified by microarray analysis were confirmed by quantitative polymerase chain reaction analysis (qPCR) (Table 4). This panel of genes was chosen on the basis of evidence from the microarray data for disease group-discriminating expression profiles at baseline and/or DMARD-responsiveness (DR) longitudinally with minimum 2 fold change and p- value <0.05. Additionally, we also included ST6 (alpha-N-acetyl-neuraminyl-2,3-beta-galactosyl-1,3)-N-acetylgalactosaminide alpha-2,6-sialyltransferase 1) (ST6GALNAC1) within our qPCR panel because, while it did not reach significance, it showed a strong > 2 fold regulation. Therefore, profiles indicating gene expression patterns (a) unique to RA (n = 8), including caspase recruitment domain family, member 6 (CARD6), C-type lectin domain family 4, member D (CLECD4), chemokine (C-X-C motif) ligand 5 (CXCL5), EPH receptor B2 (EPHB2), interferon regulatory factor 5 (IRF5), membrane-spanning 4-domains, subfamily A, member 4 (MS4A4A), PDZK1 interacting protein 1 (PDZK1IP1), sialic acid binding Ig-like lectin 1 (SIGLEC1); (b) unique to UA (n = 8), calmodulin binding transcription activator 1 (CAMTA1), cut-like homeobox 1 (CUX1), lysine (K)-specific demethylase 6A (KDM6A), KIAA0922 (KIAA0922), sema domain, immunoglobulin domain (Ig), transmembrane domain (TM) and short cytoplasmic domain, (semaphorin) 4D (SEMA4D), SET domain containing 5 (SETD5), ST6GALNAC1, zinc finger protein 91 (ZNF91); and (c) those common all inflammatory arthritis groups including interferon-induced protein with tetratricopeptide repeats 1 (IFIT1), interferon, alpha-inducible protein 27 (IFI27), interferon-induced protein 44-like (IFI44L) were chosen for validation. We also included the protein S alpha (PROS1) gene, which exhibited divergent patterns of expression in RA versus UA on the microarray. The data for this gene panel is shown in Table 4 and Fig. 3.
Quantitative baseline expression of 20 selected genes in arthritis cohorts with respect to expression in healthy control. Relative expression of selected gene expression in non-inflammatory arthralgia (NIA), self-limiting arthritis (SLA), undifferentiated arthritis (UA) and rheumatoid arthritis (RA) clinical groups at baseline compared to healthy control, as determined by quantitative RT-PCR. Gene expression profiles identified by microarray analysis as uniquely elevated in RA (A) UA (B) or co-regulated in both UA and RA (C) are shown. Genes with Welch test p-value < 0.05 and a Q value of <0.10 were considered statistically significant and are indicated, n = 6 independent donors and bars represent standard error of mean. *P < 0.05, **P < 0.005, ***P < 0.0005.
Subgroup discriminating genes at first presentation
Quantitative PCR confirmed preferential expression of many genes in RA over UA and SLA. These included SIGLEC1 (x 2.28 FC, p = 0.00597), EPHB2 (2.1 × FC, p = 0.000542), MS4A4A (2.19 × FC, p = 0.00000904), CXCL5 (x 1.94 FC, p = 0.0103) and PDZK1IP1 (x 1.67 FC, p = 0.0206). However, although PROS1 distinguished RA (1.86 × FC, p = 0.0191) from UA and SLA, significant level of this gene were also detected in the NIA cohort (1.75 × FC, p = 0.00846). Only one gene, ST6GALNAC1 distinguished UA (2.79 FC, p = 0.0023) from the RA and SLA groups (Table 4).
An interferon gene signature is common to all inflammatory arthritis groups
A feature of the microarray gene signature in the persistent arthritis groups was the presence of an IFN gene signature. This was more prominent in the RA cohort where 8 IFN genes, including EPSITI1, IFI44, ISG15, MS4A4A, OASL, RTP4, serpin peptidase inhibitor, clade G (C1 inhibitor), member 1 (SERPING1) and SIGLEC1, were uniquely overexpressed (Additional File 2A). A further 8 DE genes in this category, including DEAD (Asp-Glu-Ala-Asp) box polypeptide 58 (RIG-I) (DDX58), IFI27, IFI44L, interferon-induced protein with tetratricopeptide repeats 1, 2 and 3 (IFIT1, IFIT2, IFIT3), radical S-adenosyl methionine domain containing 2 (RSAD2) and XIAP associated factor 1 (XAF1), were elevated in both RA and UA cohorts (Additional File 2C). We also noted the expression of several prototypical IFN genes which approached the cut-off in SLA but not NIA, including IFIT1 (x1.88 FC), IFI27 (x1.64 FC) and IFI44L (x 1.76 FC) (Additional File 2C). This suggested that an interferon response might also be a feature of self-limiting arthritis patients. qPCR validation confirmed elevated IFI27 expression (x 4.11 FC, p = 0.0198) in SLA and persistent arthritis groups. However, the profiles of other IFN response genes tested displayed a more disease-specific pattern such that IFIT1 only reached statistical significance in RA (x 1.93 FC, p = 0.00435) and UA (x 1.98 FC, p = 0.0180) and significant levels of SIGLEC1 (x 2.28 FC, p = 0.00597) and MS4A4A (x 2.19 FC, p = 0.00000904) were restricted to the RA cohort (Fig. 3 and Table 4).
Genes responding to conventional synthetic DMARDs (csDMARD) treatment
Validation of gene profiles longitudinally using the same 2-fold filter criteria for qPCR revealed that only a modest effect of csDMARD treatment. This was indicated by significant trends in the reduction in the expression of IFN genes MS4A4A and IFIT1 at 6 months in the RA treatment regimen that did not pass the filter. Similar reductions in IFI27 and SIGLEC1 levels approached the filter cut-off, but these changes were not significant. In the UA treatment group, a non-significant trend to reduced expression was observed at 12 months for IFI27, SIGLEC1, IFI44L and PDZK1IP1 (Additional File 4).
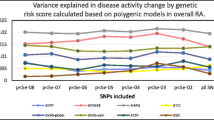
Diagnostic value for five genes for RA Identification
To further evaluate the ability of PBMC five gene expression signatures to distinguish RA patients at baseline and 6 and 12 month follow up and healthy controls (Fig. 4) and SLA, NIA, and UA from healthy controls (Fig. 5), we performed ROC curve analysis. As described in the literature25, we used the following guide for classifying the accuracy of our genes. An AUC value of 0.5 provides no information for classification, while a value of 1 indicates correct classification. A test with AUC between 0.90 and 1.00 has excellent discrimination ability, AUC from 0.80 to 0.90 has decent discrimination ability, AUC from 0.70 to 0.80 has fair discrimination ability, AUC from 0.60 to 0.70 has poor discrimination ability, and AUC from 0.50 to 0.60 has fail discrimination ability25. ROC analysis and AUC estimation showed that baseline levels of any of MSA4A, PDZK1IP1, and EPHB2 gene expression signature scores may discriminate between RA patients at Day 0, 6 months and 12 months follow-up as compared with healthy controls.
Receiver operating characteristics showing the average predictive performance for Rheumatoid Arthritis. The specificity and sensitivity rate for 5 genes showing the Area Under the Curve (AUC) for patients presenting to the clinic with a diagnosis of RA at Day 0, 6 Months and 12 months follow-up, when compared to healthy individuals. Receiver operating characteristic curves of (A) SIGLEC1, (B) MSA4A, (C) PDZK1IP1, (D) EPHB2 and (E) ST6GALNAC1 are presented.
Receiver operating characteristics showing the average predictive performance for self-limiting arthritis (SLA), Non-inflammatory arthritis (NIA) and Undifferentiated arthritis (UA). This figure is similar to Fig. 4 and shows the specificity and sensitivity rate for 5 genes showing the Area Under the Curve (AUC) for patients presenting the clinic with Self Limiting Arthritis, Non-inflammatory arthritis and Undifferentiated arthritis, when compared to healthy individuals. Receiver operating characteristic curves of (A) SIGLEC1, (B) MSA4A, (C) PDZK1IP1, (D) EPHB2 and (E) ST6GALNAC1 are presented.
As shown in (Fig. 4), ROC analysis performed using signature scores of these five genes showed AUC values as discriminatory ability for SIGLEC1 (Day 0, 0.677, poor score; 6 Months, 0.56, fail score; 12 months, 0.503, fail score); MSA4A (Day 0, 0.8944, good score; 6 Months, 0.644, poor score; 12 months, 0.720, fair score); PDZK1IP1 (Day 0, 0.785, fair score; 6 Months, 0.806, good score; 12 months, 0.977, excellent score); EPHB2 (Day 0, 0.794, fair score; 6 Months, 0.723, fair score; 12 months, 0.620, poor score); and finally ST6GALNAC1 (Day 0.507, fail score; 6 Months, 0.560, fail score; 12 months, 0.580, fail score).
On the other hand, ROC analysis performed using signature scores of these five genes showed no significant discriminatory ability for SIGLEC1, MSA4A, and PDZK1IP1, EPHB2 between SLA, NIA, and UA as compared with healthy control (Fig. 5). Only PDZK1IP1 showed a fair score (0.701) between SLA and healthy control and EPHB2 showed poor score (0.670) between NIA and healthy control and ST6GALNAC1 signature scores were fair (0.787) for discriminating UA from healthy control and poor (0.640) for discriminating SLA from healthy control (Fig. 5).
Discussion
Our study compared gene expression profiles in patient cohorts who were drug-naïve at presentation, subsequently developing either persistent arthritis or SLA, with reference to controls with arthralgia [i.e. NIA] but no evidence of inflammatory joint disease, and with healthy individuals. Two subgroups were defined with persistent disease; those with inflammatory arthritis remaining undifferentiated [i.e. UA] over the observation period that received steroid treatment and those fulfilling 1987 classification for RA where 10 of 12 patients were prescribed methotrexate. Microarray analysis at baseline revealed distinct and overlapping gene expression patterns in both arthritis subgroups that were unique to the persistent inflammatory arthritis group as a whole. The UA group exhibited signs of an active adaptive immune response and was characterised by a cluster of immunoglobulin genes with raised expression. In the RA group, cellular and biological processes including protein kinase activity, secretion, chemotaxis, response to infection, haemostasis and blood coagulation were elevated.
Using quantitative PCR analysis, we validated disease subset-specific expression patterns of several candidate genes identified by microarray analysis. Only one gene, ST6GALNAC1, with a minimum 1.5-fold change and a Q value of <0.1, met our criteria in the undifferentiated arthritis cohort. ST6GALNAC1 codes for a sialic acid transferase, and has not previously been associated with UA. Sialyltransferases add sialic acid to the terminal portions of glycolipids or to the N- or O-linked sugar chains of glycoproteins. Glycosylation of proteins affects cell-cell interaction, interactions with the matrix, and the functions of many plasma proteins. Micro heterogeneity in glycosylation of IgG, ACPA and many other plasma proteins have been widely studied and are implicated in the pathogenesis of RA26,27,28. However a definitive role of ST6GALNAC1 has still to be elucidated, although it has been shown to negatively regulate P-selectin function by modification of the glycosylation status of the O-linked glycans at the N-terminus of the leukocyte cell-surface molecule P-selectin glycoprotein ligand-129. Clearly given ST6GALNAC1 met our strict criterion its role in arthritis clearly warrants further biochemical analysis.
When patients present to an early arthritis clinic, if they do not meet classification criteria for RA, it can be a challenge to confidently identify patients who will eventually follow the disease course of RA, and therefore benefit from prompt intervention with csDMARDs. In this study, ROC and AUC risk score analysis suggested that MSA4A, PDZK1IP1 and EPHB2 at first presentation can discriminate patients with RA from healthy controls and may therefore have practical value for RA diagnosis.
In contrast, ROC analysis performed using signature AUC scores showed no significant discriminatory ability for SIGLEC1, MSA4A, and PDZK1IP1, EPHB2 between SLA, NIA, and UA as compared with healthy control (Fig. 5). However, PDZK1IP1 showed a fair AUC score (0.701) between SLA and healthy control and EPHB2 showed poor AUC score (0.670) between NIA and healthy control. ST6GALNAC1 signature AUC scores were fair (0.787) for discriminating UA from healthy control and poor (0.640) for discriminating SLA from healthy control.
Our data suggest that baseline MSA4A, PDZK1IP1, EPHB2 levels may help to identify RA patients at risk for future progression (Fig. 4). However, since ROC analysis was conducted using the same and relatively limited sample group that was used to construct the gene signatures, an overfitting problem might occur. Therefore, it is warranted to validate our results in sufficiently powered independent cohorts in the future.
We also identified PDZK1IP1, MS4A4A, and EPHB2 as genes that have not previously been linked to RA. The plasma membrane protein PDZK1IP1 (MAP17) gene is also expressed in human carcinoma lines, although the role it plays in resistance to TNF-induced apoptosis30 may be of relevance to RA. A more promising RA-discriminating candidate may be the IFNβ-induced gene, MS4A4A31. This is a member of a large family of structurally similar cell-surface proteins with putative signal transduction functions that includes functionally important B lymphocyte (B cell) marker, CD2032. MS4A4A was also found to be to be up-regulated in a cohort of DMARD-naïve recent onset juvenile idiopathic arthritis patients33 and is absent on normal B lymphocytes22. We also identified ephrin B2 receptor with an RA-discriminating profile. A role for erythropoietin-producing human hepatocellular receptors (ephrin receptors) in the aetiology of systemic inflammatory diseases such as RAhas previously been postulated34; although evidence to support this speculation has been lacking, high levels of ephrin B1 ligand were reported in peripheral and synovial T lymphocytes (T cells) in a small study with RA patients35. Our data demonstrating that EPHB2 is also elevated in early RA further supports the notion that this system is active once RA becomes established, as opposed to UA.
In agreement with earlier studies we observed an IFN signature in PBMCs in RA36,37 where eight genes detected by microarray analysis in our cohort, namely, IFIT1, IFIT2, IFI44L, RSAD2, SERPING1, EPSTI1, RTP4, and ISG15 were identified in an earlier RA gene expression profiling study38. However, our study is also the first to report SIGLEC1 (CD169) expression in the peripheral IFN signature of drug-naïve patients with early RA, which we also confirmed by qPCR. Peripheral expression of SIGLEC1 is consistent with an earlier report describing co-expression of SIGLEC1 or Siglec-1 protein in synovial tissue CD68+ cells39 and a more recent report that demonstrated elevated numbers of Siglec-1+ inflammatory monocytes in the periphery of established RA patients32.
Activation of an IFN gene signature is a molecular feature shared by many autoimmune diseases including a subset of RA37 and is already detectable in the periphery during the preclinical disease phase38. Although the clinical relevance of IFN activity remains unclear, it may be that a predominance of TNF over IFN activity or vice versa may promote the development of autoimmune diseases where excess of one cytokine plays a dominant role such as in RA and SLA respectively. Alternatively, IFNs may play a more prominent role in the initiation phase of disease while TNF predominates in the effector phase40.
We speculate that differences in the number and magnitude of IFN gene profiles observed between our drug-naïve inflammatory arthritis cohorts may suggest that the spectrum of early inflammatory arthritis from SLA to UA through RA is characterised by progressive escalations in IFN activity whereby SIGLEC1 expression in particular appears to distinguish persistent arthritis from SLA patients. This hypothesis is supported by studies using SIGLEC1 knockout animals in experimental models of autoimmune uveoretinitis (EAU) and autoimmune encephalomyelitis (EAE) suggesting a role for SIGLEC1 in promoting disease development41. In this scenario, the capacity of Siglec-1+ macrophages to inhibit the proliferation of regulatory T cells (Tregs)42 and to induce cell death in Tregs and/or CD4+Foxp3- T effector cells (Teffs) has been documented43. It is tempting to speculate therefore that increased SIGLEC1 expression and/or the numbers of circulating Siglec-1+ monocyte/macrophages in UA and RA may reflect a homeostatic feedback mechanism engaged to limit increased Treg numbers and/or to regulate the Treg: Teff balance at a critical point in the progression from acute to chronic inflammatory disease status. The notion that Tregs control the transition from acute to chronic inflammation but fail to regulate an established chronic inflammation is supported by evidence in an animal model of self-remitting arthritis44. We have also shown in a human ex vivo model of RA that Tregs are unable to inhibit proinflammatory cytokine production from more active synovial tissues45. However, to understand the role of IFN in inflammatory arthritis and its potential contribution to the pathogenesis of RA, it will be necessary to define the function IFN response genes such as SIGLEC1 in both disease stage and subtype-specific contexts.
Clinical studies addressing the predictive power of the IFN signature have established the responsiveness of IFN-inducible genes to anti-TNF treatment38. While such studies have not defined a consistent response across different therapeutics, the concept of monitoring the IFN response as a predictor of therapeutic response is supported by a recent study which measured IFN activity in RA plasma pre- and post- anti-TNF biologic therapy and reported better EULAR outcomes in patients with a high baseline IFNβ/α ratio46. Longitudinal gene microarray profiling in our patient cohorts confirmed DMARD responsiveness of IFN genes, albeit delayed in the undifferentiated arthritis (UA compared to the RA treatment group. Perhaps due the small sample sizes, the reduction in RA-specific IFN genes SIGLEC1 and MS4A4A while significant did not pass the filter stringency in confirmatory qPCR. However, the recent report of Xiong et al.43, showing a positive correlation for Siglec-1 protein expression on PBMCs with disease activity in established RA, and the parallel decrease in SIGLEC1 expression with DAS28 after DMARD treatment, suggests that SIGLEC1 and the more RA-restricted MS4A4A identified are both potential biomarkers of disease activity in persistent arthritis. However, SIGLEC1 has been reported to be a feature of the IFN signature in systemic lupus erythematous47, suggesting that its expression alone may not be sufficient to define RA, therefore a combination of SIGLEC1 and MS4A4A expression is more likely to discriminate RA from other inflammatory diseases.
Nevertheless, our study has a number of limitations. First, due to the small sample size for the four subgroups, the large variability of early arthritis, and heterogeneous treatment regimens are the challenges for meaningful analysis and generalizability of our findings to other populations and disease stages. These findings are at best hypotheses generating; therefore, validating these findings in sufficiently powered independent cohorts of each disease subgroup with multiple testing (i.e. the Bonferroni adjustment) correction procedure to adjust our statistical confidence measures based on the number of tests performed is warranted to strengthen our finding.
Second, our proposed biomarkers are only at the mRNA level are not validated at the protein level and mechanistic insight into the putative biomarkers is lacking and thus these are obvious limitations of our study. However, for some of these mRNAs, the respective protein products may not be present or detectable in blood; hence quantification of transcript levels may be the better option. Third, because gene expression profiling was carried out in whole PBMCs, there is, therefore, significant chance that differences in the composition of cellular subsets either adds to or diminishes the biomarker potential of these signatures. However, for liquid biopsy to be practical in the clinical setting, expression profiling in whole PBMCs is the best choice, due to its simplicity, high turnaround, and relatively lower cost; not the peripheral blood lymphocyte subsets.
Fourth, the mechanistic insight into the putative biomarkers in relation to the history of disease progression and response to therapies is unknown; therefore, longer-term treatment and follow-up studies to understand mechanisms of action and to better gauge, the clinical utility of these potential biomarkers is warranted.
Nevertheless, results of our pilot and feasibility longitudinal study in well-defined clinical cohorts of drug-naïve, early inflammatory arthritis patients provide some key but yet to be validated potentially useful biomarkers as classifiers to discriminate drug-naïve RA and/or UA patients from those with SLA and NIA as compared to healthy control as well as potential DMARD responsive biomarkers in RA and UA.
Conclusions
Despite the need for replicating the findings in an independent dataset, this study has potentially identified a type I IFN gene signature in the periphery of drug naïve patients with persistent arthritis and SLA as a promising biomarker. The expression of the immunoregulatory receptor SIGLEC1 and MSA4A is a novel feature which characterizes this IFN signature in persistent arthritis. Finally, we identify ST6GALNAC1 as a marker of undifferentiated arthritis and MSA4A, PDZK1IP1 and EPHB2 whose expression profiles may potentially discriminate untreated early RA from UA and SLA.
Data availability
The datasets supporting the conclusions of this article are included within the article (and its additional files).
References
McMichael, A. J., Sasazuki, T., McDevitt, H. O. & Payne, R. O. Increased frequency of HLA-Cw3 and HLA-Dw4 in rheumatoid arthritis. Arthritis Rheum 20, 1037–42 (1977).
Stastny, P. Association of the B-cell alloantigen DRw4 with rheumatoid arthritis. N Engl J Med 298, 869–71 (1978).
MacGregor, A. J. et al. Characterizing the quantitative genetic contribution to rheumatoid arthritis using data from twins. Arthritis Rheum 43, 30–7 (2000).
Imboden, J. B. The immunopathogenesis of rheumatoid arthritis. Annu Rev Pathol 4, 417–34 (2009).
Eyre, S. et al. High-density genetic mapping identifies new susceptibility loci for rheumatoid arthritis. Nat Genet 44, 1336–40 (2012).
Okada, Y. et al. Genetics of rheumatoid arthritis contributes to biology and drug discovery. Nature 506, 376–81 (2014).
Gregersen, P. K. Susceptibility genes for rheumatoid arthritis - a rapidly expanding harvest. Bull NYU Hosp Jt Dis 68, 179–82 (2010).
Nielen, M. M. et al. Specific autoantibodies precede the symptoms of rheumatoid arthritis: a study of serial measurements in blood donors. Arthritis Rheum 50, 380–6 (2004).
Aletaha, D. et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis 69, 1580–8 (2010).
Smolen, J. S. et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs. Ann Rheum Dis 69, 964–75 (2010).
van Dongen, H. et al. Efficacy of methotrexate treatment in patients with probable rheumatoid arthritis: a double-blind, randomized, placebo-controlled trial. Arthritis Rheum 56, 1424–32 (2007).
Tak, P. P. & Kalden, J. R. Advances in rheumatology: new targeted therapeutics. Arthritis Res Ther 13(Suppl 1), S5 (2011).
Edwards, C. J. et al. Molecular profile of peripheral blood mononuclear cells from patients with rheumatoid arthritis. Mol Med 13, 40–58 (2007).
Kuai, J. et al. TREM-1 expression is increased in the synovium of rheumatoid arthritis patients and induces the expression of pro-inflammatory cytokines. Rheumatology (Oxford) 48, 1352–8 (2009).
Koczan, D. et al. Molecular discrimination of responders and nonresponders to anti-TNF alpha therapy in rheumatoid arthritis by etanercept. Arthritis Res Ther 10, R50 (2008).
Pratt, A. G. et al. A CD4 T cell gene signature for early rheumatoid arthritis implicates interleukin 6-mediated STAT3 signalling, particularly in anti-citrullinated peptide antibody-negative disease. Ann Rheum Dis 71, 1374–81 (2012).
Cooles, F. A. H. et al. Phenotypic and Transcriptomic Analysis of Peripheral Blood Plasmacytoid and Conventional Dendritic Cells in Early Drug Naive Rheumatoid Arthritis. Front Immunol 9, 755 (2018).
Arnett, F. C. et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31, 315–24 (1988).
Luo, F., Zhong, J., Yang, Y. & Zhou, J. Application of random matrix theory to microarray data for discovering functional gene modules. Phys Rev E Stat Nonlin Soft Matter Phys 73, 031924 (2006).
Huang da, W., Sherman, B. T. & Lempicki, R. A. Bioinformatics enrichment tools: paths toward the comprehensive functional analysis of large gene lists. Nucleic Acids Res 37, 1–13 (2009).
Nakamura, S. et al. Identification of baseline gene expression signatures predicting therapeutic responses to three biologic agents in rheumatoid arthritis: a retrospective observational study. Arthritis Res Ther 18, 159 (2016).
Nunez Lopez, Y. O., Retnakaran, R., Zinman, B., Pratley, R. E. & Seyhan, A. A. Predicting and understanding the response to short-term intensive insulin therapy in people with early type 2 diabetes. Mol Metab 20, 63–78 (2019).
Chalan, P. et al. Analysis of serum immune markers in seropositive and seronegative rheumatoid arthritis and in high-risk seropositive arthralgia patients. Sci Rep 6, 26021 (2016).
Myngbay, A. et al. CTHRC1: A New Candidate Biomarker for Improved Rheumatoid Arthritis Diagnosis. Frontiers in Immunology 10 (2019).
Li, F. & He, H. Assessing the Accuracy of Diagnostic Tests. Shanghai Arch Psychiatry 30, 207–212 (2018).
Raghav, S. K. et al. Altered expression and glycosylation of plasma proteins in rheumatoid arthritis. Glycoconj J 23, 167–73 (2006).
Rombouts, Y. et al. Extensive glycosylation of ACPA-IgG variable domains modulates binding to citrullinated antigens in rheumatoid arthritis. Ann Rheum Dis (2015).
Saroha, A., Biswas, S., Chatterjee, B. P. & Das, H. R. Altered glycosylation and expression of plasma alpha-1-acid glycoprotein and haptoglobin in rheumatoid arthritis. J Chromatogr B Analyt Technol Biomed Life Sci 879, 1839–43 (2011).
Lo, C. Y. et al. Competition between core-2 GlcNAc-transferase and ST6GalNAc-transferase regulates the synthesis of the leukocyte selectin ligand on human P-selectin glycoprotein ligand-1. J Biol Chem 288, 13974–87 (2013).
Guijarro, M. V., Castro, M. E., Romero, L., Moneo, V. & Carnero, A. Large scale genetic screen identifies MAP17 as protein bypassing TNF-induced growth arrest. J Cell Biochem 101, 112–21 (2007).
Sellebjerg, F. et al. Identification of new sensitive biomarkers for the in vivo response to interferon-beta treatment in multiple sclerosis using DNA-array evaluation. Eur J Neurol 16, 1291–8 (2009).
Liang, Y. & Tedder, T. F. Identification of a CD20-, FcepsilonRIbeta-, and HTm4-related gene family: sixteen new MS4A family members expressed in human and mouse. Genomics 72, 119–27 (2001).
Griffin, T. A. et al. Gene expression signatures in polyarticular juvenile idiopathic arthritis demonstrate disease heterogeneity and offer a molecular classification of disease subsets. Arthritis Rheum 60, 2113–23 (2009).
Romanovsky, A. A., Ivanov, A. I. & Petersen, S. R. Microsomal prostaglandin E synthase-1, ephrins, and ephrin kinases as suspected therapeutic targets in arthritis: exposed by “criminal profiling”. Ann N Y Acad Sci 1069, 183–94 (2006).
Kitamura, T. et al. Enhancement of lymphocyte migration and cytokine production by ephrinB1 system in rheumatoid arthritis. Am J Physiol Cell Physiol 294, C189–96 (2008).
Olsen, N. et al. A gene expression signature for recent onset rheumatoid arthritis in peripheral blood mononuclear cells. Ann Rheum Dis 63, 1387–92 (2004).
van der Pouw Kraan, T. C. et al. Rheumatoid arthritis subtypes identified by genomic profiling of peripheral blood cells: assignment of a type I interferon signature in a subpopulation of patients. Ann Rheum Dis 66, 1008–14 (2007).
van Baarsen, L. G. et al. Regulation of IFN response gene activity during infliximab treatment in rheumatoid arthritis is associated with clinical response to treatment. Arthritis Res Ther 12, R11 (2010).
Hartnell, A. et al. Characterization of human sialoadhesin, a sialic acid binding receptor expressed by resident and inflammatory macrophage populations. Blood 97, 288–96 (2001).
Cantaert, T., Baeten, D., Tak, P. P. & van Baarsen, L. G. Type I IFN and TNFalpha cross-regulation in immune-mediated inflammatory disease: basic concepts and clinical relevance. Arthritis Res Ther 12, 219 (2010).
Jiang, H. R. et al. Sialoadhesin promotes the inflammatory response in experimental autoimmune uveoretinitis. J Immunol 177, 2258–64 (2006).
Wu, C. et al. Sialoadhesin-positive macrophages bind regulatory T cells, negatively controlling their expansion and autoimmune disease progression. J Immunol 182, 6508–16 (2009).
Xiong, Y. S. et al. Increased expression of Siglec-1 on peripheral blood monocytes and its role in mononuclear cell reactivity to autoantigen in rheumatoid arthritis. Rheumatology (Oxford) 53, 250–9 (2014).
Frey, O. et al. Regulatory T cells control the transition from acute into chronic inflammation in glucose-6-phosphate isomerase-induced arthritis. Ann Rheum Dis 69, 1511-8 (2010).
Beavis, P. A. et al. Resistance to regulatory T cell-mediated suppression in rheumatoid arthritis can be bypassed by ectopic foxp3 expression in pathogenic synovial T cells. Proc Natl Acad Sci USA 108, 16717–22 (2011).
Mavragani, C. P., La, D. T., Stohl, W. & Crow, M. K. Association of the response to tumor necrosis factor antagonists with plasma type I interferon activity and interferon-beta/alpha ratios in rheumatoid arthritis patients: a post hoc analysis of a predominantly Hispanic cohort. Arthritis Rheum 62, 392–401 (2010).
Rose, T. et al. IFNalpha and its response proteins, IP-10 and SIGLEC-1, are biomarkers of disease activity in systemic lupus erythematosus. Ann Rheum Dis 72, 1639–45 (2013).
Acknowledgements
Written informed consent was obtained from the patients for publication of their anonymised data and accompanying images in this manuscript. The consent form is held by the authors’ institution and is available for review by the Editor-in-Chief. We would like to especially acknowledge the valuable contribution made to this work by Professor Fionula M. Brennan who passed away prior to its completion. Her guidance, mentorship and enthusiasm for scientific research will be remembered with gratitude by her many friends and students. Our special thank also go to Margot O’Toole, Maryann Whitley, and Ching Li for their contribution to this work. We also thank Marek Honczarenko for his support of the qPCR assays and we are grateful to tissue procurers Renee Best and Darren Ennis. Professor Taylor thanks Arthritis Research UK and the National Institute of Health Research for their funding of The NIHR Biomedical Research Centre in Musculoskeletal Disease at Oxford University Hospitals NHS Trust and the University of Oxford. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. This study was supported by Wyeth, now part of Pfizer Inc.
Author information
Authors and Affiliations
Contributions
B.G. participated in the design and coordination of the study, analysis and interpretation of data, and drafted the manuscript. A.C. performed analysis tools, interpretation of data and helped in drafting the manuscript. SB conceived of the study and participated in study design, patient inclusion, disease activity measurement, clinical laboratory analyses and critically reviewed the manuscript. C.L. and Y.Z. participated in data acquisition, analysis and interpretation and critically reviewed the manuscript. L.W., Y.L. and Y.G. contributed to data analysis and interpretation and critical review of the manuscript. A.S. participated in the study concept and design, acquisition and interpretation of data and critical review of the manuscript. L.-L.L., M.F. and F.B. contributed to study concept and design and helped to draft and critically review the manuscript. P.T. contributed to study concept and design, patient inclusion, data acquisition and interpretation and helped to draft and critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Attila A Seyhan, Christine Loreth, Yizheng Li, Ying Zhang, Yongjing Guo, and Lih-Ling Lin are or have been employees of Pfizer and have stock shares or ownership options. Bernard Gregory, Adam Cribbs, Sundeep Bhalara, Marc Feldmann, Adam Cribbs, Lynn Williams, Fionula Brennan declare no competing interests. Peter C. Taylor has acted as a consultant to Pfizer.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seyhan, A.A., Gregory, B., Cribbs, A.P. et al. Novel biomarkers of a peripheral blood interferon signature associated with drug-naïve early arthritis patients distinguish persistent from self-limiting disease course. Sci Rep 10, 8830 (2020). https://doi.org/10.1038/s41598-020-63757-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-020-63757-3
- Springer Nature Limited
This article is cited by
-
Role of IFN-α in Rheumatoid Arthritis
Current Rheumatology Reports (2024)
-
Serum level of IFNβ distinguishes early from late relapses after biologics withdrawal in rheumatoid arthritis
Scientific Reports (2022)