Abstract
Background: Markedly elevated D-dimer levels can occur in emergency patients with various clinical situations, and is likely to indicate the presence of coagulopathy, rapid differential diagnosis was crucial for them. Methods: D-dimer was detected in consecutive 813 patients entering the emergency department of our hospital, for the patients with D-dimer levels above 5.0 µg/mL, the final diagnoses and 28-day mortality were confirmed, and the levels of thrombomodulin (TM), thrombin-antithrombin complex (TAT) and plasmin-antiplasmin complex (PAP) on admission were detected. Results: There were 148 emergency patients with D-dimer levels higher than 5.0 µg/mL mainly due to sepsis, malignancy, trauma, venous thromboembolism (VTE), cerebrovascular accident, and so on. Both of the TM and TAT levels among these diagnoses were significantly different (p < 0.001). The elevated TM (>13.3 TU/mL) had a predictive value of 96.0% for excluding VTE, and the normal TM had a predictive value of 90.4% for excluding sepsis. The overall 28-day mortality of these patients with D-dimer >5.0 ug/mL was 14.2%, the TAT level on admission was independently associated with 28-day mortality (odds ratio 1.014, 95% CI 1.001–1.027, P = 0.030). Conclusions: The medical emergencies associated with markedly elevated D-dimer levels were revealed, specific markers of endothelial dysfunction and thrombin generation measured by automatic analyzer have the potential to distinguish diagnoses and predict outcomes in these patients.
Similar content being viewed by others
Introduction
D-dimer is a biomarker of fibrin formation and degradation and has been used routinely for variety of diagnostic purposes, including excluding venous thromboembolism (VTE), determining the optimal duration of anticoagulation in VTE patients, and diagnosing disseminated intravascular coagulation (DIC) et al.1,2. Emergency patients who present with markedly elevated D-dimer levels are a concern, as they were more likely to have associated coagulopathy3. However, markedly elevated D-dimer levels can occur in various clinical situations and is commonly hard to distinguish rapidly1, this may due to that as an indirect marker of activation of coagulation as well as fibrinolysis, D-dimer alone can’t indicate the specific state. For instance, with similarly high D-dimer, hyperfibrinolysis is considered to be the major manifestation and therapeutic target of trauma-induced coagulopathy, meanwhile, endothelial dysfunction, excess thrombin generation and fibrinolysis shutdown are the feature of sepsis-induced coagulopathy4,5. Hence, more specific coagulation markers may be needed for distinction of these conditions.
In this study, we aimed to investigate the clinical features, diagnoses and outcomes of emergency patients with markedly elevated D-dimer levels on admission; Meanwhile, markers of endothelium, thrombin and plasmin in these patients were detected and evaluated, we assumed that some of these markers might has discriminatory or prognosis value in patients with markedly elevated D-dimer level, i.e. a high possibility of coagulopathy.
Methods
Patients
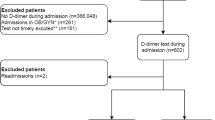
D-dimer was detected in consecutive 813 patients entering the emergency department of our hospital from July 2019 to October 2019. As 3.0–7.0 ug/mL of D-dimer levels had been used as the cutoff of item in several DIC criterias, or to define high risk of VTE5,6,7, we selected the average value of 5.0 µg/mL to define a markedly elevated of D-dimer. A total of 166 (20.4%) patients had D-dimer levels above 5.0 µg/mL (fibrinogen equivalent units, 10 times of the upper normal limit), within 24 hours after admission, and the samples were reserved for further detection.
This study was approved by the Ethics Committee of Tongji Hospital (Wuhan, China), and written informed consent was obtained from all patients or their family members. All methods were carried out in accordance with relevant guidelines and regulations.
Eighteen of the 166 patients were lost to follow-up or died before a diagnosis was confirmed, and were excluded from the study. The remaining 148 patients were all hospitalized, and a retrospective review of their characteristics and outcomes was performed using the hospital’s electronic medical records system, the results of breathing rate, mean arterial pressure, bilirubin and creatinine on admission were recorded to describe multiple organ dysfunctions of each enrolled patient8. In addition, in the other 647 patients with D-dimer ≤5.0 ug/mL, 338 (52.2%) were hospitalized, and there were no further investigation on them due to the high rate of lost to follow-up.
Blood sampling and detection
Blood samples were collected from each patient within 24 hours after admission. Samples were collected into vacuum tubes (BD Vacutainer; Becton Dickinson and Company, Devon, UK) with 3.2% sodium citrate for coagulation tests. The samples for coagulation tests were centrifuged at 2700 × g for 10 minutes to obtain platelet-poor plasma, and D-dimer was detected using a STA-R analyzer and STA-Liatest D-Di reagent (Diagnostica Stago, Saint-Denis, France) based on the latex immune turbidimetric assay (reference interval <0.5 µg/mL). As markers of endothelium, thrombin and plasmin, the levels of thrombomodulin (TM), thrombin-antithrombin complex (TAT) and plasmin-antiplasmin complex (PAP) were detected using a HISCL 5000 analyser and original chemiluminescence reagents (SYSMEX, Kobe, Japan), the reference intervals of these three markers were suggested by the manufacturer and had been validated before application in our hospital.
All cases of VTE, aortic dissection, and cerebrovascular accident were confirmed by Doppler ultrasound, computed tomography or magnetic resonance imaging. The diagnosis of sepsis was based on the sepsis 3.0 definition9, the presence of infection was confirmed by pathogen detection or comprehensive judgment of our clinician (Dengju Li). Cases of malignancy were confirmed by necessary pathological and imaging examinations.
Statistical analysis
Quantitative variables are presented as median (interquartile range). Multiple comparisons among biomarkers of each diagnosises were performed using Kruskal-Wallis H test. Between survivors and non-survivors, comparisons of continuous variables were performed using the Mann-Whitney test, and categorical variables were evaluated using Fisher’s exact test or Pearson’s Chi-squared test, where appropriate. Categorical and consecutive variables were evaluated by logistic regression analysis for their ability to predict 28-day mortality. A P-value of <0.05 was considered statistically significant. Data were analyzed using SPSS 21.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
The 148 consecutive emergency patients with D-dimer levels >5.0 µg/mL included 89 men and 59 women, with a mean age of 56.5 years (range 12–88 years). The primary diagnoses and levels of coagulation biomarkers on admission of these patients are shown in Table 1. Both of the TM and TAT levels among these diagnoses were significantly different (p < 0.001).
Due to the patients with diagnoses of sepsis and VTE had the highest and lowest TM levels, respectively, diagnostic values of TM for sepsis and VTE were evaluated (Table 2). In these emergency patients with D-dimer levels >5.0 µg/mL, the high TM (>13.3 TU/mL) had a sensitivity of 77.8% and a specificity of 58.0% for sepsis diagnosis, and the low TM (<13.3 TU/mL) had a sensitivity of 82.4% and a specificity of 55.0% for VTE diagnosis. Although TAT had the highest levels in trauma patients, and the lowest levels in patients with Liver cirrhosis, these patients commonly had definite medical history, hence the differential value of TAT between trauma and liver cirrhosis didn’t be evaluated. In addition, higher TAT level in patients with artery dissection comparing to those with VTE has been found (P = 0.012).
Correlation analysis showed that D-dimer levels had significant correlations to TAT (P = 0.004) and PAP (P < 0.001) levels in these emergency patients, the correlation coefficients were 0.236 and 0.558, respectively. No significant correlation was found between D-dimer and TM levels (P = 0.570).
The overall 28-day mortality of emergency patients with D-dimer >5.0 ug/mL was 14.2% (21/148 patients). The comparison of age, sex ratio, biomarkers of coagulation and organ function between survivals and non-survivals were showed in Table 3. The non-survivors had significantly higher TM, TAT, total bilirubin and creatinine levels and lower mean arterial pressure on admission than the survivors (P < 0.05), these parameters were further evaluated by the multivariable logistic regression analysis (Table 4), and the levels of TAT, mean arterial pressure and total bilirubin were independently associated with 28-day mortality.
Discussion
Clinicians routinely use D-dimer levels as part of a diagnostic algorithm to exclude a diagnosis of VTE10, and the ISTH has also endorsed the role of D-dimer testing in the diagnostic algorithm for DIC11. In our study, the emergency patients with D-dimer levels higher than 10 times of the upper normal limit mainly due to sepsis, malignancy, trauma, venous thromboembolism, cerebrovascular accident, and so on. A higher hospitalization rate in these patients were found, comparing to patients with D-dimer ≤5.0 ug/mL (89.2% vs 52.2%). The good correlation between D-dimer and TAT or PAP in our study confirmed the large generations of thrombin and plasmin in these patients, and indicated the existence of coagulopathy.
TM, also called CD141, is an anticoagulant protein constitutively distributed on the surface of vascular endothelial cells. TM binds to thrombin, then this complex activates protein C and forms the major physiological anticoagulant pathway12. In sepsis, release of TM from the surface of vascular endothelial cells into the blood circulation partly through proteolytic cleavage by neutrophil elastase13,14. Hence, it’s considered to be a biomarker for endothelial cell damage, and that plasma TM levels are elevated in patients with sepsis has been described previously15. On the other hand, no association of TM with venous thromboembolism has been found in a former study16, also as shown in our study, this may be explained as when VTE is the primary or only diagnosis of a patient rather than being secondary to trauma or infection et al., endothelial dysfunction commonly is not the major factor. Hence, it’s reasonable that in our emergency patients with markedly elevated D-dimer, a low or high TM level could be helpful to exclude sepsis or VTE, respectively. In addition, TM had higher on-admission levels in non-survivors compared with survivors, which is consistent with previous studies17,18, however, it’s not independently associated with the outcome according to the logistic regression analysis.
As a biomarker related to thrombin generation, TAT had the highest level in trauma patients of our study, that has also been described in previous reports19,20. Although it’s not needed to distinguish trauma patient from others by blood testing, TAT might be used for prognosis as it was associated with the outcome and independent of other organ dysfunctions in this study. In addition, as both of VTE and artery dissection could present markedly elevated D-dimer and similar symptoms21, patients with artery dissection showed higher TAT level, this indicates more obvious coagulation activation in artery dissection than in VTE and the potential of differential diagnose, and also can be used to explain that why patients with artery dissection often show a DIC-like coagulopathy22. However, a study with larger sample size is needed to confirm it. Relatively, as a biomarker of plasmin generation, PAP seemed to be of little differential or prognosis value in patients with markedly elevated D-dimer.
According to these results, it seemed that detection of these specific coagulation markers could support a further explanation of elevated D-dimer mechanistically, moreover, unlike most previous studies, the TM, TAT, and PAP levels were all measured by an automatic analyzer in our study, the shorter turn-around time and simpler methodology ensure that these biomarkers can be used for emergency case.
This study had some limitations. The TM, TAT and PAP levels of patients with D-dimer less than 5.0 ug/mL had not been detected and evaluated. In addition, we defined the markedly elevated D-dimer as higher than 10 times of the upper normal limit (5.0 ug/mL) according to previous studies5,6,7, this definition might still be arbitrary.
Nevertheless, the current results revealed that medical emergencies commonly associated with markedly elevated D-dimer levels, which were correlated with more productions of thrombin and plasmin, and indicated the risk of coagulopathy. Plasma TM and TAT levels measured by automatic analyzer have the potential to distinguish diagnoses and predict outcomes in these emergency patients.
References
Linkins, L. A. & Takach Lapner, S. Review of D-dimer testing: Good, Bad, and Ugly. Int. J. Lab. Hematol. 39, 98–103 (2017).
Taylor, F. B. Jr., Toh, C. H., Hoots, W. K., Wada, H. & Levi, M. Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb. Haemost. 86, 1327–1330 (2001).
Olson, J. D. D-dimer: An Overview of Hemostasis and Fibrinolysis, Assays, and Clinical Applications. Adv. Clin. Chem. 69, 1–46 (2015).
Davenport, R. A. & Brohi, K. Cause of trauma-induced coagulopathy. Curr. Opin. Anaesthesiol. 29, 212–219 (2016).
Iba, T. et al. Diagnosis of sepsis-induced disseminated intravascular coagulation and coagulopathy. Acute Med. Surg. 6, 223–232 (2019).
Suzuki, K. et al. A re-evaluation of the D-dimer cut-off value for making a diagnosis according to the ISTH overt-DIC diagnostic criteria: communication from the SSC of the ISTH. J. Thromb. Haemost. 16, 1442–1444 (2018).
Samuelson Bannow, B. T. & Konkle, B. A. Laboratory biomarkers for venous thromboembolism risk in patients with hematologic malignancies: A review. Thromb. Res. 163, 138–145 (2018).
Vincent, J. L. et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 22, 707–710 (1996).
Singer, M. et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 315, 801–810 (2016).
Righini, M., Perrier, A., De Moerloose, P. & Bounameaux, H. D-Dimer for venous thromboembolism diagnosis: 20 years later. J. Thromb. Haemost. 6, 1059–1071 (2008).
Wada, H. et al. The Scientific Standardization Committee on DIC of the International Society on Thrombosis Haemostasis. Guidance for diagnosis and treatment of DIC from harmonization of the recommendations from three guidelines. J. Thromb. Haemost. 11, 761–767 (2013).
Conway, E. M. Thrombomodulin and its role in inflammation. Semin. Immunopathol. 34, 107–125 (2012).
Furuno, T., Mitsuyama, T., Hidaka, K., Tanaka, T. & Hara, N. The role of neutrophil elastase inhuman pulmonary artery endothelial cell injury. Int. Arch. Allergy Immunol. 112, 262–269 (1997).
Iba, T. et al. Potential diagnostic markers for disseminated intravascular coagulation of sepsis. Blood reviews. 30, 149–155 (2016).
Wada, H. et al. Plasmathrombomodulin as a marker of vascular disorders in thrombotic thrombocytopenic purpura and disseminated intravascular coagulation. Am. J. Hematol. 39, 20–24 (1992).
Aleksic, N. et al. Prospective study of the A455V polymorphism in the thrombomodulin gene, plasma thrombomodulin, and incidence of venous thromboembolism: the LITE Study. J. Thromb. Haemost. 1, 88–94 (2003).
Kinasewitz, G. T. et al. Universal changes in biomarkers of coagulation and inflammation occur in patients with severe sepsis, regardless of causative micro-organism. Crit. Care. 8, R82–R90 (2004).
Boehme, M. W. et al. Release of thrombomodulin from endothelial cells by concerted action of TNF-alpha and neutrophils: in vivo and in vitro studies. Immunology. 87, 134–140 (1996).
Helling, H., Stephan, B. & Pindur, G. Coagulation and complement system in critically ill patients. Clin. Hemorheol. Microcirc. 61, 185–193 (2015).
Gando, S., Nanzaki, S., Sasaki, S. & Kemmotsu, O. Significant correlations between tissue factor and thrombin markers in trauma and septic patients with disseminated intravascular coagulation. Thromb. Haemost. 79, 1111–1115 (1998).
Jo, Y. et al. Re-elevation of D-dimer as a predictor of re-dissection and venous thromboembolism after Stanford type B acute aortic dissection. Heart Vessels. 25, 509–514 (2010).
Guan, X., Li, J., Gong, M., Lan, F. & Zhang, H. The hemostatic disturbance in patients with acute aortic dissection: A prospective observational study. Med. 95, e4710 (2016).
Author information
Authors and Affiliations
Contributions
N.T. performed research and wrote the paper. Y.P. and C.X. collected and analyzed the data. D.L. confirmed the diagnosis of included patients and designed the study. All the authors have accepted responsibility for the entire content of this submitted manuscript and approved submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tang, N., Pan, Y., Xu, C. et al. Characteristics of emergency patients with markedly elevated D-dimer levels. Sci Rep 10, 7784 (2020). https://doi.org/10.1038/s41598-020-64853-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-64853-0
- Springer Nature Limited