Abstract
Owing to the high incidence and mortality of oral squamous cell carcinoma (OSCC), knowledge of its diagnostic and prognostic factors is of significant value. The biomarkers ‘CD16, CD57, transforming growth factor beta 1 (TGF-β1), and MED15’ can play crucial roles in tumorigenesis, and hence might contribute to diagnosis, prognosis, and treatment. Since there was no previous study on MED15 in almost all cancers, and since the studies on diagnostic/prognostic values of the other three biomarkers were a few in OSCC (if any) and highly controversial, this study was conducted. Biomarker expressions in all OSCC tissues and their adjacent normal tissues available at the National Tumor Bank (n = 4 biomarkers × [48 cancers + 48 controls]) were estimated thrice using qRT-PCR. Diagnostic values of tumors were assessed using receiver-operator characteristic (ROC) curves. Factors contributing to patients’ survival over 10 years were assessed using multiple Cox regressions. ROC curves were used to estimate cut-off points for significant prognostic variables (α = 0.05). Areas under the curve pertaining to diagnostic values of all markers were non-significant (P > 0.15). Survival was associated positively with tumoral upregulation of TGF-β1 and downregulation of CD16, CD57, and MED15. It was also associated positively with younger ages, lower histological grades, milder Jacobson clinical TNM stages (and lower pathological Ns), smaller and thinner tumors, and surgery cases not treated with incisional biopsy (Cox regression, P < 0.05). The cut-off point for clinical stage –as the only variable with a significant area under the curve– was between the stages 2 and 3. Increased TGF-β1 and reduced CD16, CD57, and MED15 expressions in the tumor might independently favor the prognosis. Clinical TNM staging might be one of the most reliable prognostic factors, and stages above 2 can predict a considerably poorer prognosis.
Similar content being viewed by others
Introduction
Oral squamous cell carcinoma (OSCC) is a common oral cancer (90% of oral cancers) and has a poor prognosis1,2,3,4. It is aggressive and can modulate the immune system through evasion and direct/indirect suppression3,5,6,7. High rates of recurrence despite numerous treatments imply that current treatments and prognostic predictors are not efficient3,7,8. These call for investigating new diagnostic, prognostic, and possibly therapeutic markers for SCC. Many factors might play a role in cancer prognostication, including tobacco, alcohol, human papilloma virus, demographic/clinical/histopathological factors (such as stage, grade, or tumor budding), and biomarkers (such as Gas6)9,10,11. SCCs of head and neck might be immune-modulatory, and the prognostic effects of immune system activity have been conflicting3,5,12,13,14,15,16,17. The interaction between tumor cells and the immune system is crucial in tumorigenesis and improved knowledge of dysregulated pathways might allow identification of new targets18,19. Therefore, the assessment of diagnostic and prognostic roles of biomarkers such as transforming growth factor beta 1 (TGF-β1), CD16, CD57, and MED15 is of significant value.
Low-affinity immunoglobulin gamma Fc region receptor III (FcγRIII, CD16) is an IgG Fc receptor found on the surface of inflammatory cells20. One of the main routes of defense against tumor cells (and viral/bacterial infections) is antibody-dependent cellular cytotoxicity (ADCC) in which, immunoglobulin G antibody attaches to the target cell; the Fc domains of these antibodies then bind to Fc receptors expressed on leukocytes (such as natural killer [NK] cells), triggering the release of cytotoxic granules or upregulating the expression of death receptors on the surface of the target cell18,21,22,23,24,25. Therefore, it is anticipated to increase in tumoral tissues, and therefore probably act as a diagnostic and prognostic factor. Human studies on the prognostic role of CD16 in different cancers are a few and controversial18. In OSCC, it has not been assessed in humans except a recent immunohistochemistry survival analysis (which has studied NK cells only and has not evaluated any factors associated with its tumoral expression)18. To the best of our knowledge, its role as a diagnostic marker of OSCC has not been established either.
Mature and differentiated NK cells also express CD57 which makes them more cytotoxic and reactive to signaling via CD1618,26. CD57 (HNK-1, Leu 7) is a sulfated carbohydrate chain surface antigen containing the epitope for the antibody HNK-1, usually expressed in T-lymphocytes and NK cells18,26,27,28,29. Although its role is not yet completely understood29, heterogeneous patterns of increased and decreased expressions of CD57 have been observed in cancer29,30. Despite the importance of the interaction of immune system and tumor cells, the expression of CD57 and development/prognosis of head and neck SCC have not been adequately studied in human28,31. Additionally, the results have been controversial marking negative and positive28,32 associations between CD57 upregulation and survival. Very few studies have assessed its diagnostic role in few cancers28,29,33,34,35.
Transforming growth factor beta 1 (TGF-β1) is a pleiotropic cytokine with diverse and paradoxical effects7,36,37,38,39. It can suppress tumorigenesis via its fibrogenic and antiproliferative effects, reducing metastasis likelihood40,41. Also it might contribute to malignancy, tumor angiogenesis, tissue invasion, metastasis, and neoplastic transformation of epithelial cells, immune suppression, and epithelial hyperproliferation7,36,38,41,42,43,44. The role of TGF-β1 in SCC prognosis and diagnosis has been controversial7 and still needs further research. Disruption of TGF-β1 signaling pathways might be approached to control the tumorigenesis41, although some authors do not find it a useful prognostic factor7,45. Since it has extremely paradoxical effects even in one type of cancer depending on the stage and severity of the cancer (let alone in different cancers), and since the results have been quite controversial, the examination of its diagnostic and prognostic roles is of clinical and scientific value.
MED15 is a subunit of the tail module of the mediator multiprotein complex and is a key regulator of TGF-β signal transduction19,46,47. Mediator is a main regulator of protein coding-genes, and an integrative hub for numerous signaling pathways47,48. Mediator subunits have been recently suggested to be linked to cancer (plus metabolic, cardiovascular, and neurological disorders) but this is a very new topic and needs more evaluation47,48. Despite its importance for regulating TGF-β signaling (which plays crucial roles in SCC19), prognostic role of MED15 is not assessed except in a few recent studies on prostate and head and neck cancers19,48,49. Besides, its diagnostic roles remain unaddressed.
This study was conducted since (1) MED15 is not evaluated in any cancers except partially in very few recent studies on certain cancers, (2) reports on the other three biomarkers are controversial, non-existent (in the case of diagnostic roles), or scarce (in the case of head and neck SCCs), (3) no studies have assessed these biomarkers together, and therefore their effects on the survival have not been evaluated when controlling for the other ones; and (4) many previous studies on these cancer biomarkers have used less accurate methods such as IHC and have examined fewer markers (mostly limited to one or two). Research goals were (A) to assess the diagnostic role of each of these markers, (B) to determine their prognostic role by investigating the influences of these markers (as well as other clinicopathological factors) on patients’ 123-month survival, (C) to determine cut-off points for the identified prognostic variables, and (D) to estimate the prognostic role of other clinicopathological factors.
Materials and methods
Tissue samples
This retrospective case-control study was performed on 48 tumoral tissues and 48 genetically-matched adjacent healthy tissues as controls. The sample size was determined as All the OSCC specimens available at the National Tumor Bank (n = 384 biomarker data points = 4 markers × [48 OSCC cancer tissues + 48 control tissues]). Biological materials were provided by the National Tumor Bank which is founded by the Cancer Institute for Cancer Research. As the eligibility criteria, all patients with oral SCC who underwent surgery in the Institute were selected for this study. None of the selected patients had received any chemotherapy or radiotherapy prior to surgery. The patients were diagnosed with OSCC based on histopathological examinations at two time points by at least two pathologists. Patients’ pathological records (including the histology grade, tumor size, and Jacobson clinical TNM [tumor, node, and metastasis]) staging were recorded. Subjects with chronic or acute inflammatory diseases or any other synchronized primary tumor were also excluded from the study. The protocol ethics were approved by the Research Committee of the Alborz University of Medical Sciences, Karaj, Iran (approved as theses 1395–113 and 1395–118). All specimens were prepared with full observation of preparation and preservation processes of standard protocols in accordance with ethical permissions. Ethics of the study were approved by the research committee of the university, and written informed consents had been obtained from all patients. The data were checked for consistency and correctness for numerous times. Tumor measurements were re-performed twice by two different pathologists on all the 48 paraffin-embedded specimens to ensure a high accuracy of the recorded data.
At the end of the 10-year study period (ending in 2017), 28 out of 48 patients were deceased. The average duration of survival since the diagnosis was 33.4 ± 35.5 months in the whole sample (minimum: 1 week, Q1: 4.5 months, median: 23.5 months, Q3: 45.5 months, maximum:123 months [i.e., the follow-up period]). Among the deceased patients, the mean survival duration was 13.7 ± 22.5 months (minimum: 1 week, Q1: 5 weeks, median:9 months, Q3:15 months, maximum:115 months).
Patients had been diagnoses with SCC between 2007 and 2015. The mean follow-up duration (from diagnosis to death or from diagnosis to the final follow-up) was 33.4 ± 35.5 months (minimum: 1 week, Q1: 4 months, median: 23 months, Q3: 45 months, maximum: 123 months). Of them, 29 were males and 19 were females. Their average age at diagnosis was 63.8 ± 15.3 years . Family history of previous cancers existed in 10 patients. Only one patient disclosed alcohol drinking. Only 7 were cigarette smokers at the time of diagnosis.
Continuous variables of the tumors are presented in Table 1. At the end of the follow-up duration, 28 patients had deceased and 20 were alive. Of tumors, 16 were in the labial mucosa and buccal mucosa, 16 were in the tongue, 7 were in the mouth floor, and the rest were in the lower gingiva (3), oropharynx (1), and not specified (or multisite OSCC) (4). Histology grades were I, II, and III in 28, 16, and 3 patients. Necrosis was present in 10 patients. Lymphatic invasion was present in 10 cases. Vascular invasion was seen in 9 cases. Perineural invasion was positive in 18 patients. Extracapsular nodal extension was present in 3 patients. Pathological T modes were T1, T2, T3, and T4 in 6, 13, 12, 16 patients, respectively. Pathological N modes were N0, N1, and N2 in 32, 4, and 11 cases, respectively. Clinical metastases were M0 in 46 cases and M1 in one case. The stages 1, 2, 3, and 4 were seen respectively in 4, 6, 11, and 26 patients. One, one, and 45 patients had undergone fine needle biopsy, incisional biopsy, and excisional biopsy, respectively.
RNA extraction and real-time quantitative polymerase chain reaction (qRT-PCR)
The qRT-PCR procedure was performed thrice for each of the 96 cancerous and benign tissues. Primer sequences were synthesized for TGF-β1 (left: AGCTGTACATTGACTTCCGC, right: GTCCAGGCTCCAAATGTAGG), MED15 (left: AGAACTTCAGTGTCCCCTCA, right: GTACTTCGACAGCTGCTTCA), CD16 (left: GTGGGTGTTCAAGGAGGAAG, right: CTGCCTTTGCCATTCTGTAA), and CD57 (left: GAACTTGTCACCCTCAACGA, right: CTTCTTGCCCTCATTCACC). The RNA was extracted using a Qiagen kit (Germantown, USA) according to the manufacturer’s instructions. After normalization of all the extracted RNAs to 1 µg, the RNA was reverse-transcribed into single-strand cDNA using a Thermo kit (Thermo Fisher Scientific, Waltham, Massachusetts, USA). The quantity and purity of extracted RNA was analyzed using Nano-Drop Technologies (ND-2000). The product was used for quantitative qRT-PCR using SYBR green/ROX (Takara, Japan) real-time PCR master mix according to the protocol of Bioneer RT-PCR thermal cycler. The amplification protocol comprised 1 cycle at 95 °C for 4 min followed by 40 cycles at 95 °C for 15 s, 60 °C for 30 s, and then 72 °C for 30 s. The relative expression of the studied genes to the housekeeping gene (β-actin) was calculated by measuring the Delta threshold cycle value (ΔCt) for each sample (i.e., Ct[Housekeeping] − Ct[Target]). The Delta Delta cycle value (ΔΔCt) as the +log2-fold-change was then calculated from the difference between the ΔCt of the tumoral tissue and the ΔCt of its normal adjacent tissue (i.e., tumor ΔCt – the ΔCt of its adjacent benign tissue). The fold-change (ratio) in the expression of the target gene in the tumoral tissue to its expression in the healthy tissue was then calculated by the 2ΔΔCt formula50. This way, a ΔΔCt above zero would indicate a logarithmic increase in the expression of the marker in the tumoral tissue compared with its adjacent tissue. Also a fold-change value above 1 would point to a tumoral overexpression compared with the control tissue.
Statistical analysis
As expression indices and log-fold-change values, ΔCts and ΔΔCts were used for analyses. According to the D’Agostino & Pearson omnibus normality test, the ΔΔCt values were normally distributed. Descriptive statistics as well as 95% confidence intervals (CI) were calculated for all continuous variables. Tumoral ΔCt values were compared with control ΔCt values using a paired-samples t-test, in order to assess if the average gene expression in the tumor was different from the average normal tissue gene expression. Correlations between ΔCt values were assessed using a Pearson coefficient. A receiver-operator characteristic (ROC) curve was used to estimate the diagnostic accuracy of ΔCts in discriminating tumoral tissues from healthy ones. A multiple Cox regression was used to assess the prognostic role of each of the biomarkers when other factors were controlled for. In order to select proper models, items such as model estimates, multiple imputation results, principal component analysis results, model significance, variance inflation factors, and the number of significant results per model were taken into account. When important variables caused multicollinearity, they would be modeled interchangeably in rather similar but separate models. A ROC curve was used to identify potential cut-off points for death prediction, through evaluating prognostic sensitivity and specificity of the variables turned significant in the Cox models. A Kaplan-Meier function was used for drawing the cumulative survival curves of dichotomized variables. The level of significance was set at 0.05.
Results
Diagnostic factors
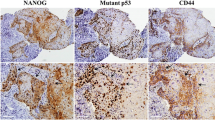
The paired-samples t-test did not detect significant differences between tumoral versus control ΔCt values of CD16 (P = 0.772), CD57 (P = 0.157), TGF-β1 (P = 0.947), and MED15 (P = 0.244): None of the relative expressions of the four evaluated genes leaned towards an overall overexpression or underexpression in the tumor compared to the adjacent healthy tissue (Fig. 1, Table 1). There was not a significant correlation between tumoral and normal ΔCt values for CD16 or TGF-β1, but the correlations between tumoral and normal ΔCt values of CD57 and MED15 were significant (Table 2).
The ROC curve did not identify significant areas under the curve (AUC) for differentiating tumoral tissues from normal controls, based on ΔCt values of CD16 (AUC [SE] = 0.530 ± 0.060, 95% CI = 0.413–0.646, P = 0.618), CD57 (AUC [SE] = 0.578 ± 0.059, 95% CI = 0.462–0.693, P = 0.190), TGF-β1 (AUC [SE] = 0.521 ± 0.059, 95% CI = 0.404–0.637, P = 0.725), and MED15 (AUC [SE] = 0.567 ± 0.059, 95% CI = 0.450–0.683, P = 0.259, Fig. 2).
Prognostic factors affecting the survival
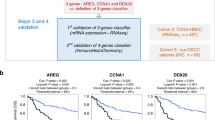
Since some of variables were considerably correlated, they were first detected by evaluating correlation matrixes, VIFs, results of multiple-imputation, and results of a component factor analysis. After detecting bivariate correlations (between independent factors and survival duration and the live/deceased status) and potentially significant variables, two Cox regression models were conducted, each with a group of the least correlated variables. Tumoral upregulation of CD16, CD57, and MED15 were associated with increased risk of mortality, while overexpression of TGF-β1 might improve prognosis. Older ages, higher stages/grades, higher Ns, as well as larger tumor volumes might deteriorate the prognosis. Incisional biopsy might as well be associated with increased mortality (Tables 3 to 5). Depth of invasion was as well associated with mortality (Table 5).
Cut-off points for death prediction
A ROC curve was used to identify which of the factors contributing to the survival can be useful for mortality prediction. The only variable with an area under the curve significantly differing from 50% was ‘stage’ (Fig. 3, Table 6). The cut-off point of the variable ‘stage’ for death prediction (as the stage yielding the greatest sum of sensitivity and specificity) was determined as between the stages 2 and 3 (sensitivity = 0.926, specificity = 0.600).
Survival plots
Gene expressions were dichotomized into upregulation (i.e., foldchanges above 1 [or ΔΔCt above 0]) and downregulation (foldchanges below 1). The Kaplan-Meier function was used to draw cumulative survival curves for the biomarkers (Fig. 4). The variable ‘clinical TNM stage’ was as well dichotomized into two modes of mild (stages 1 and 2) and severe (stages 3 and 4); its survival plot was drawn using the Kaplan-Meier estimator (Fig. 5).
Discussion
The findings of this study indicated that all the average expressions of biomarkers in the tumor were not different from their expressions in the adjacent benign tissue. Older ages, greater stages, relative tumoral upregulation of CD16, CD57, and MED15, as well as downregulation of TGF-β1 (compared to the expressions in the adjacent normal tissue), poorer histologic grades, and increases in tumor volume might predict a higher rate of mortality. In addition, it was found that cases undergone incisional biopsy might have a higher chance of mortality compared to those undergone surgical resection.
Clinicopathological predictors of survival
In this study, it was observed that an increased tumor volume could increase the risk of mortality. Few essays have mentioned tumor volume, and it should be calculated using 3D imaging systems9,51. Tumor volume is a function of its diameter and depth. Depth of invasion has been suggested as a main factor in prognosis of different cancers52,53,54,55,56,57 including SCCs57,58. It can predict recurrence, metastasis, and death9,59. In this study as well, this variable acted as a predictor of survival. Each unit of increase in TNM staging was found to be the most prominent prognostic factor for survival.
Various studies have indicated that factors including regional lymph node metastasis60,61,62,63,64, lymphatic invasion65, histological grading60,61,64, the anatomic site60, clinical TNM staging60,61,65,66 and depth of invasion60,62,63 might be key prognostic markers of OSCC60 or other cancers65. TNM staging has been recognized as a very important prognostic factor60,67,68,69. In line with our findings, a recent study34 identified both the variables staging and pathological N, but they did not indicate significant roles for age or smoking34. Associations were found in this sample between mortality with histologic grade in this sample. Some studies have estimated an increased mortality in cases with perineural and vascular invasions52,70,71,72; we could not find such roles for these variables, possibly because of methodological and sample differences. For instance, smoking, vascular invasion, or perineural invasion were themselves correlated with tumoral overexpressions of some markers, which could mask their role in multivariable models including those markers.
Although in this study, the site of cancer was not a prognostic factor, the method of treatment was. This might imply the higher efficacy of surgical resection. In this research, the expression of all the biomarkers were positively associated with each other. Almost no other studies have assessed this.
Diagnostic roles of biomarkers
Findings of this study indicated no significant overall difference between the expressions of either marker in the tumor with their expression in the benign adjacent tissue. The ROC curve as well did not point to significant diagnostic merits for any of these markers. Our findings were in line with the study of Wangerin et al.29 who did not recognize CD57 as a proper diagnostic marker for prostate cancer. According to them, this marker might not be specific to tumoral tissue but benign prostatic tissue as well29. A study on breast cancer identified CD14+–CD16+ monocytes as a proper diagnostic marker (AUC = 80.5%)33. In this study, we could not find any significant diagnostic role for TGF-β1. This was in contrast to studies showing significant diagnostic roles for this marker in different cancers (except SCC for which its diagnostic value had not been assessed)73,74 or new relevant markers such as Latent Transforming Growth Factor β Binding Protein75. Diagnostic role of MED15 has not been assessed before. The reason for disputes might be that cells expressing these markers are involved in numerous inflammatory responses, the number and complexity of which might mask their role as expected binary diagnostic factors.
Prognostic values
CD16 enables NK cells to recognize and kill target cells opsonized with antibodies through ADCC26,32. Also CD16+ monocytes are pro-inflammatory and a major source of TNF76, and their numbers are increased during infection and inflammation77,78,79,80. A positive association was observed between the overexpression of CD16 and mortality. Few human studies exist on this subject18. Taghavi et al.18 could not detect a link between survival and CD16 expression in OSCC. Similarly, Lazaris et al.81 reported a lack of significant prognostic role for CD16 in laryngeal carcinoma. Grimm et al.82 as well did not find a significant association between survival and peripheral CD16 monocytes; they also did not detect different extents of such cells in tumoral and control cells82. Russell et al.3 as well did not find a significant prognostic role for CD16 marker. On the other hand, results of Gonzalez et al.83 indicated that in laryngeal carcinoma patients, CD16 in peripheral blood mononuclear cells correlated with nodal metastases, suggesting it as a prognostic marker83. Sorskaar et al.84 found an improved prognosis of lymphoblastic leukemia with increases in CD16 cells in bone marrow. Also Millrud et al.85 reported a positive correlation between increased CD16 neutrophils in peripheral blood and a better survival. Valenzuela-Membrives et al.86 observed CD16 NK cells in peripheral blood as well as normal tissue; however, CD16 NK cells were diminished in tumor stroma (although they did not assess survival prognosis)86. Sconocchia et al.87 as well observed a significant correlation between high CD16+ cell infiltrate with long-term survival in patients with colorectal carcinoma while they detected no prognostic roles for NK cells. In vitro studies have shown reduced NK killing potential and cancer immune evasion accompanied by downregulation of CD1624,88. The dispute might be attributed to assessment of different cancers (which differ in tumor progression mechanisms, immune response/infiltration, and immune-tumor interaction86), using different methods (qPCR versus IHC, or for example some studies evaluated only certain types of cells86), and characteristics of samples in terms of demographics and cancer severities which again can affect immune response86. Moreover, it is possible for cancers to evade the immune response while evoking it simultaneously89. Therefore, perhaps in this study, the increase in CD16 expression in more severe cases was to compensate the immunosurveillance evasion mechanisms of cancer. Moreover, it is possible that severer cancers (which had higher CD16 expressions) received more aggressive treatments, improving their survival. This study found no significant difference in expression of CD16 in tumoral cells versus benign adjacent tissues; however, according to some authors, CD16 is downregulated in HNSCC90.
Patient survival was associated negatively with CD57 upregulation in the tumor compared to benign adjacent tissue. This was similar to results of studies on OSCC34, renal cell carcinoma91, melanoma92, gastric carcinoma65, multiple myeloma93, lymphoma and leukemia84,94,95. Nonetheless, our finding was in contrast to the results of other studies which found better survivals in patients having a higher level of tumoral CD57 NK cells in head and neck SCC, lung SCC, breast carcinoma, esophageal carcinoma, metastatic carcinoma, gastric carcinoma, and colorectal cancer18,28,32,66,96,97,98,99. Karpathiou et al.100 reported that increases in CD57 T cells predict a better response to chemotherapy, reduced metastasis, and better prognoses. This association might be due to various factors such as diminished MHC Class I expression in some tumors which disallow T-lymphocytes immunosurveillance and make the role of NK cells more prominent32,101,102. Adachi et al.103 observed that in early stages of colorectal cancer, CD57 NK cells might increase in the lymph nodes but they might not infiltrate into the tumor; this nodal increase might positively predict survival103. Similarly, Hermann et al.104 found reduced anticancer cytotoxicity associated with reduced CD57 cells. The NK cells can improve immunosurveillance via improving the antibody production by V lymphocytes32,105, generation of antitumor cytotoxic T-lymphocytes, and upregulation of MHC molecules32,105. On the other hand, Zancope et al.106 did not detect a significant association between prognosis and NK cell count which might be due to smaller sample size and methodological differences. Also Fraga et al.28 reported no independent role for CD57 cell density in the tumor with survival although they found significant associations between high CD57+ inflammatory cell density with tumor size and more locoregional metastases; they concluded that a higher density of such cells the peritumoral stroma might lead to an ineffective locoregional antitumoral response28. Additionally, Sorbye et al.107 did not find a significant prognostic role for CD57 cells. Such results might be attributed to the method of CD57 expression evaluation, evaluated cell types, sample types and sizes, tumor types and severities, statistical methods in use, and sample demographics/ethnicities18,86. In addition, the location of infiltrating cells might be another reason for controversy as there is difference between epithelial, stromal or peritumoral CD57 positive cells107. Moreover, CD57 is expressed also on T lymphocytes which despite their cytotoxic potential are unable to undergo new cell-division107,108. Furthermore, tumor-immune system interactions are complicated: sometimes tumors act like subclinical infections evading immune response, and sometimes despite evading immonosurveillance, some of their surface antigens still trigger a progressive (yet inefficient) increase in immune response89. The latter might be the case in our study. Also as mentioned above, patients with poorer prognoses might have received stronger treatments, which could confound the results.
The findings of this study indicated a positive role for tumoral TGF-β1 upregulation in survival. Our findings were in contrast to findings of some other studies which failed to show a significant survival role for TGF-β1 in SCCs of head and neck18,45 or showed that increased TGF-β1 expression might reduce survival odds109. On the other hand, our results were in line with findings of some other studies indicating an association between increased expression of TGF-β1 in the tumor and reduced mortality (and improved survival rate)107. The controversy results might be attributed to the complex and dual role of TGF-β1 in tumorigenesis as well differences between pathogenesis of various tumors7,18,110,111. Various factors might determine the effect of TGF-β1 including TGF-β1 receptors (normal or diminished), target cell types (normal or tumoral), TGF-β1 dosage, and immune response: while it is mostly tumor suppressor in early tumors, it facilitates tumorigenesis in later stages7,18,23,36,37,38,41,44,109,110,111,112; for instance it might enhance36,41,43 or inhibit40,41 tumor cell invasion. It can facilitate metastasis through increased detachment of cancer cells, tumoral proliferation/invasion, growth stimulation, angiogenesis, MMP induction, or chemoattraction, facilitation of epithelial-to-mesenchymal transition, and increasing invasiveness and motility8,36,37,38,40,41,42,43,44,113,114,115,116,117,118; while it also can act against the cancer by maintaining the tissue architecture and genomic stability, induction of apoptosis and replicative senescence, attraction of fibroblasts and capsule synthesis, inducing the activity of inhibitors of MMPs, or inhibiting cell proliferation7,36,38,40,41,42,43,44. In certain cancers, increased expression of TGF-β1 and its pathway might reduce the production of NK cytokines and CD16 receptor18,25, increase CD16 expression77,80, downregulate the primary cytotoxicity receptor of NK cells25,90, functionally inactivate NK and cytotoxic T cells88,119,120, or decrease the suppressor effectiveness of NK cells121.
In this study, MED15 overexpression was associated positively with TGF-β1 overexpression. Although TGF-β1 was found to be associated positively with survival, the role of MED15 in survival was negative when the effects of other genes had been controlled for. This result was in contrast with the few other studies finding the opposite. Shaikhibrahim et al.48 evaluated castration-resistant prostate cancer (CRPC) and reported that MED15 was overexpressed in 76% of distant metastatic and 70% of local-recurrent CRPC versus no expression in benign prostatic tissue; they also found a significant negative association between the overexpression of MED15 and survival48. As the only study on head and neck SCC, Shaikhibrahim et al.19 found MED15 overexpressed in 35% of primary tumors, 30% of lymph node metastases, and 70% of recurrent tumors; they also observed MED15 overexpression to be associated positively with mortality19. In this study, MED15 was also positively associated with CD16 and CD57 expressions, which had effects opposite of that of TGF-β1. Based on positive associations with contradicting biomarkers, it seems that its role in survival (if existing) might have been more complicated than a log-linear one.
Conclusions
Within the limitations of this study, it might be concluded that none of these biomarkers might be suitable for diagnosis of OSCC. Tumoral overexpression of CD16, CD57, and MED15 might predict poorer prognoses, while elevated TGF-β1 levels might be associated with an improved prognosis. The prognosis might be poorer in older patients, cases with higher clinical TNM stages, greater N modes, higher histological grades, and larger/thicker tumors. Cases treated with incisional biopsy might have a poorer prognosis (compared to surgical resection) as well, but this remain inconclusive until more data are collected. Of these variables, only ‘Jacobson clinical TNM staging’ might have a cut-off point for death prediction, i.e., cases with stages above 2 might have a considerably higher risk of mortality.
Data availability
The data that support the findings of this study are available from the National Tumor Bank of Iran and the authors, but restrictions apply to the availability of a part of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the National Tumor Bank of Iran.
References
van der Waal, I., de Bree, R., Brakenhoff, R. & Coebergh, J. W. Early diagnosis in primary oral cancer: is it possible? Med. Oral Patol. Oral Cir. Bucal 16, e300–305, https://doi.org/10.4317/medoral.16.e300 (2011).
O-Charoenrat, P., Rhys-Evans, P. H. & Eccles, S. A. Expression of matrix metalloproteinases and their inhibitors correlates with invasion and metastasis in squamous cell carcinoma of the head and neck. Arch. Otolaryngol. Head Neck Surg. 127, 813–820 (2001).
Russell, S. et al. Immune cell infiltration patterns and survival in head and neck squamous cell carcinoma. Head Neck Oncol. 5, 24 (2013).
Pai, S. I. & Westra, W. H. Molecular pathology of head and neck cancer: implications for diagnosis, prognosis, and treatment. Annu. Rev. Pathol. 4, 49–70, https://doi.org/10.1146/annurev.pathol.4.110807.092158 (2009).
Duray, A., Demoulin, S., Hubert, P., Delvenne, P. & Saussez, S. Immune suppression in head and neck cancers: a review. Clin. Dev. Immunol. 2010, 701657, https://doi.org/10.1155/2010/701657 (2010).
Meissner, M. et al. Defects in the human leukocyte antigen class I antigen processing machinery in head and neck squamous cell carcinoma: association with clinical outcome. Clin. Cancer Res. 11, 2552–2560, https://doi.org/10.1158/1078-0432.CCR-04-2146 (2005).
Elahi, M., Rakhshan, V., Ghasemian, N. T. & Moshref, M. Prognostic value of transforming growth factor beta 1 [TGF-beta1] and matrix metalloproteinase 9 [MMP-9] in oral squamous cell carcinoma. Biomarkers 17, 21–27, https://doi.org/10.3109/1354750X.2011.635804 (2012).
Cortesina, G. & Martone, T. Molecular metastases markers in head and neck squamous cell carcinoma: review of the literature. Acta Otorhinolaryngol Ital 26, 317–325 (2006).
Jadhav, K. B. & Gupta, N. Clinicopathological prognostic implicators of oral squamous cell carcinoma: need to understand and revise. N. Am. J. Med. Sci. 5, 671–679, https://doi.org/10.4103/1947-2714.123239 (2013).
Shimizu, S. et al. Tumor budding is an independent prognostic marker in early stage oral squamous cell carcinoma: with special reference to the mode of invasion and worst pattern of invasion. PloS one 13, e0195451 (2018).
Jiang, T., Liu, G., Wang, L. & Liu, H. Elevated serum Gas6 is a novel prognostic biomarker in patients with oral squamous cell carcinoma. PLoS One 10, e0133940 (2015).
Jochems, C. & Schlom, J. Tumor-infiltrating immune cells and prognosis: the potential link between conventional cancer therapy and immunity. Exp. Biol. Med. (Maywood) 236, 567–579, https://doi.org/10.1258/ebm.2011.011007 (2011).
Distel, L. V. et al. Tumour infiltrating lymphocytes in squamous cell carcinoma of the oro- and hypopharynx: prognostic impact may depend on type of treatment and stage of disease. Oral Oncol. 45, e167–174, https://doi.org/10.1016/j.oraloncology.2009.05.640 (2009).
Pretscher, D. et al. Distribution of immune cells in head and neck cancer: CD8+ T-cells and CD20+ B-cells in metastatic lymph nodes are associated with favourable outcome in patients with oro- and hypopharyngeal carcinoma. BMC Cancer 9, 292, https://doi.org/10.1186/1471-2407-9-292 (2009).
Badoual, C. et al. Prognostic value of tumor-infiltrating CD4+ T-cell subpopulations in head and neck cancers. Clin. Cancer Res. 12, 465–472, https://doi.org/10.1158/1078-0432.CCR-05-1886 (2006).
Gooden, M. J., de Bock, G. H., Leffers, N., Daemen, T. & Nijman, H. W. The prognostic influence of tumour-infiltrating lymphocytes in cancer: a systematic review with meta-analysis. Br. J. Cancer 105, 93–103, https://doi.org/10.1038/bjc.2011.189 (2011).
Allen, C. T., Judd, N. P., Bui, J. D. & Uppaluri, R. The clinical implications of antitumor immunity in head and neck cancer. Laryngoscope 122, 144–157, https://doi.org/10.1002/lary.21913 (2012).
Taghavi, N., Bagheri, S. & Akbarzadeh, A. Prognostic implication of CD57, CD16, and TGF-beta expression in oral squamous cell carcinoma. J Oral Pathol Med 45, 58–62, https://doi.org/10.1111/jop.12320 (2016).
Shaikhibrahim, Z. et al. Clinical and molecular implications of MED15 in head and neck squamous cell carcinoma. Am. J. Pathol. 185, 1114–1122, https://doi.org/10.1016/j.ajpath.2014.12.010 (2015).
Murphy, K. & Weaver, C. Janeway’s immunobiology. (Garland Science, 2016).
Yeap, W. H. et al. CD16 is indispensable for antibody-dependent cellular cytotoxicity by human monocytes. Sci. Rep. 6 (2016).
Scott, A. M., Wolchok, J. D. & Old, L. J. Antibody therapy of cancer. Nat. Rev. Cancer 12, 278–287, https://doi.org/10.1038/nrc3236 (2012).
Wilson, E. B. et al. Human tumour immune evasion via TGF-beta blocks NK cell activation but not survival allowing therapeutic restoration of anti-tumour activity. PLoS One 6, e22842, https://doi.org/10.1371/journal.pone.0022842 (2011).
Trotta, R. et al. TGF-beta utilizes SMAD3 to inhibit CD16-mediated IFN-gamma production and antibody-dependent cellular cytotoxicity in human NK cells. J. Immunol. 181, 3784–3792, https://doi.org/10.4049/jimmunol.181.6.3784 (2008).
Dasgupta, S., Bhattacharya-Chatterjee, M., O’Malley, B. W. Jr. & Chatterjee, S. K. Inhibition of NK cell activity through TGF-beta 1 by down-regulation of NKG2D in a murine model of head and neck cancer. J. Immunol. 175, 5541–5550, https://doi.org/10.4049/jimmunol.175.8.5541 (2005).
Topham, N. J. & Hewitt, E. W. Natural killer cell cytotoxicity: how do they pull the trigger? Immunology 128, 7–15, https://doi.org/10.1111/j.1365-2567.2009.03123.x (2009).
Longworth, M. S. & Laimins, L. A. The binding of histone deacetylases and the integrity of zinc finger-like motifs of the E7 protein are essential for the life cycle of human papillomavirus type 31. J Virol 78, 3533–3541, https://doi.org/10.1128/jvi.78.7.3533-3541.2004 (2004).
Fraga, C. A. et al. Infiltrating CD57+ inflammatory cells in head and neck squamous cell carcinoma: clinicopathological analysis and prognostic significance. Appl. Immunohistochem. Mol. Morphol. 20, 285–290, https://doi.org/10.1097/PAI.0b013e318228357b (2012).
Wangerin, H. et al. CD57 expression in incidental, clinically manifest, and metastatic carcinoma of the prostate. Biomed Res Int 2014, 356427, https://doi.org/10.1155/2014/356427 (2014).
Serrano, D. et al. Clonal expansion within the CD4+ CD57+ and CD8+ CD57+ T cell subsets in chronic lymphocytic leukemia. J. Immunol. 158, 1482–1489 (1997).
Chang, C. C. & Ferrone, S. NK cell activating ligands on human malignant cells: molecular and functional defects and potential clinical relevance. Semin. Cancer Biol. 16, 383–392, https://doi.org/10.1016/j.semcancer.2006.07.001 (2006).
Agarwal, R., Chaudhary, M., Bohra, S. & Bajaj, S. Evaluation of natural killer cell (CD57) as a prognostic marker in oral squamous cell carcinoma: An immunohistochemistry study. J. Oral Maxillofac. Pathol. 20, 173–177, https://doi.org/10.4103/0973-029X.185933 (2016).
Feng, A. L. et al. CD16+ monocytes in breast cancer patients: expanded by monocyte chemoattractant protein-1 and may be useful for early diagnosis. Clin Exp Immunol 164, 57–65, https://doi.org/10.1111/j.1365-2249.2011.04321.x (2011).
Fang, J. et al. Prognostic significance of tumor infiltrating immune cells in oral squamous cell carcinoma. BMC Cancer 17, 375, https://doi.org/10.1186/s12885-017-3317-2 (2017).
de Sousa Lopes, M. L. D. et al. Evaluation of CD57+ cells in oral squamous cells carcinoma and their relationship with clinicopathological parameters. Journal of Oral Diagnosis 2, 1–7 (2017).
Yang, L. TGFbeta and cancer metastasis: an inflammation link. Cancer Metastasis Rev 29, 263–271, https://doi.org/10.1007/s10555-010-9226-3 (2010).
Chen, Y., Zhang, W., Geng, N., Tian, K. & Jack Windsor, L. MMPs, TIMP-2, and TGF-beta1 in the cancerization of oral lichen planus. Head Neck 30, 1237–1245, https://doi.org/10.1002/hed.20869 (2008).
Tian, M. & Schiemann, W. P. The TGF-beta paradox in human cancer: an update. Future Oncol. 5, 259–271, https://doi.org/10.2217/14796694.5.2.259 (2009).
Bierie, B. & Moses, H. L. Tumour microenvironment: TGFbeta: the molecular Jekyll and Hyde of cancer. Nat. Rev. Cancer 6, 506–520, https://doi.org/10.1038/nrc1926 (2006).
Takiuchi, H. et al. Particular types of tumor cells have the capacity to convert transforming growth factor beta from a latent to an active form. Cancer Res. 52, 5641–5646 (1992).
Wakefield, L. M. & Roberts, A. B. TGF-beta signaling: positive and negative effects on tumorigenesis. Curr. Opin. Genet. Dev. 12, 22–29, https://doi.org/10.1016/s0959-437X(01)00259-3 (2002).
Sinpitaksakul, S. N., Pimkhaokham, A., Sanchavanakit, N. & Pavasant, P. TGF-beta1 induced MMP-9 expression in HNSCC cell lines via Smad/MLCK pathway. Biochem. Biophys. Res. Commun. 371, 713–718, https://doi.org/10.1016/j.bbrc.2008.04.128 (2008).
Lewis, M. P. et al. Tumour-derived TGF-beta1 modulates myofibroblast differentiation and promotes HGF/SF-dependent invasion of squamous carcinoma cells. Br J Cancer 90, 822–832, https://doi.org/10.1038/sj.bjc.6601611 (2004).
Yang, L. & Moses, H. L. Transforming growth factor beta: tumor suppressor or promoter? Are host immune cells the answer? Cancer Res. 68, 9107–9111, https://doi.org/10.1158/0008-5472.CAN-08-2556 (2008).
Logullo, A. F. et al. Transforming growth factor beta1 (TGFbeta1) expression in head and neck squamous cell carcinoma patients as related to prognosis. J Oral Pathol Med 32, 139–145, https://doi.org/10.1034/j.1600-0714.2003.00012.x (2003).
Kato, Y., Habas, R., Katsuyama, Y., Naar, A. M. & He, X. A component of the ARC/Mediator complex required for TGF beta/Nodal signalling. Nature 418, 641–646, https://doi.org/10.1038/nature00969 (2002).
Malik, S. & Roeder, R. G. The metazoan Mediator co-activator complex as an integrative hub for transcriptional regulation. Nat. Rev. Genet. 11, 761–772, https://doi.org/10.1038/nrg2901 (2010).
Shaikhibrahim, Z. et al. MED15, encoding a subunit of the mediator complex, is overexpressed at high frequency in castration-resistant prostate cancer. Int. J. Cancer 135, 19–26, https://doi.org/10.1002/ijc.28647 (2014).
Offermann, A. et al. MED15 overexpression in prostate cancer arises during androgen deprivation therapy via PI3K/mTOR signaling. Oncotarget 8, 7964–7976, https://doi.org/10.18632/oncotarget.13860 (2017).
Baghaei, F. et al. PTEN and miR-26b: Promising prognostic biomarkers in initiation and progression of Oral Squamous Cell Carcinoma. J Oral Pathol Med 48, 31–35, https://doi.org/10.1111/jop.12794 (2019).
Massano, J., Regateiro, F. S., Januario, G. & Ferreira, A. Oral squamous cell carcinoma: review of prognostic and predictive factors. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 102, 67–76, https://doi.org/10.1016/j.tripleo.2005.07.038 (2006).
Hong, S. M. et al. Depth of tumor invasion better predicts prognosis than the current American Joint Committee on Cancer T classification for distal bile duct carcinoma. Surgery 146, 250–257, https://doi.org/10.1016/j.surg.2009.02.023 (2009).
Hong, S. M., Cho, H., Moskaluk, C. A. & Yu, E. Measurement of the invasion depth of extrahepatic bile duct carcinoma: An alternative method overcoming the current T classification problems of the AJCC staging system. Am. J. Surg. Pathol. 31, 199–206, https://doi.org/10.1097/01.pas.0000213384.25042.86 (2007).
Hong, S. M. et al. Analysis of extrahepatic bile duct carcinomas according to the New American Joint Committee on Cancer staging system focused on tumor classification problems in 222 patients. Cancer 104, 802–810, https://doi.org/10.1002/cncr.21236 (2005).
Nakanishi, Y. et al. Extrahepatic bile duct carcinoma with extensive intraepithelial spread: a clinicopathological study of 21 cases. Mod. Pathol. 21, 807–816, https://doi.org/10.1038/modpathol.2008.65 (2008).
Paik, K. Y., Heo, J. S., Choi, S. H. & Choi, D. W. Intraductal papillary neoplasm of the bile ducts: the clinical features and surgical outcome of 25 cases. J. Surg. Oncol. 97, 508–512, https://doi.org/10.1002/jso.20994 (2008).
Tarsitano, A., Del Corso, G., Tardio, M. L. & Marchetti, C. Tumor Infiltration Depth as Predictor of Nodal Metastasis in Early Tongue Squamous Cell Carcinoma. J. Oral Maxillofac. Surg. 74, 523–527, https://doi.org/10.1016/j.joms.2015.09.015 (2016).
Chao, Y. K. et al. Using pretreatment tumor depth and length to select esophageal squamous cell carcinoma patients for nonoperative treatment after neoadjuvant chemoradiotherapy. Ann. Surg. Oncol. 20, 3000–3008, https://doi.org/10.1245/s10434-013-2962-1 (2013).
Thompson, A. K., Kelley, B. F., Prokop, L. J., Murad, M. H. & Baum, C. L. Risk Factors for Cutaneous Squamous Cell Carcinoma Recurrence, Metastasis, and Disease-Specific Death: A Systematic Review and Meta-analysis. JAMA Dermatol 152, 419–428, https://doi.org/10.1001/jamadermatol.2015.4994 (2016).
Vasconcelos, M. G., Mafra, R. P., Vasconcelos, R. G., Medeiros, A. M. Cd & Queiroz, L. M. G. Squamous cell carcinoma of the tongue: clinical and morphological analysis of 57 cases and correlation with prognosis. Jornal Brasileiro de Patologia e Medicina Laboratorial 50, 359–363 (2014).
Rodrigues, P. C. et al. Clinicopathological prognostic factors of oral tongue squamous cell carcinoma: a retrospective study of 202 cases. Int. J. Oral Maxillofac. Surg. 43, 795–801, https://doi.org/10.1016/j.ijom.2014.01.014 (2014).
Suslu, N., Hosal, A. S., Aslan, T., Sozeri, B. & Dolgun, A. Carcinoma of the oral tongue: a case series analysis of prognostic factors and surgical outcomes. J. Oral Maxillofac. Surg. 71, 1283–1290, https://doi.org/10.1016/j.joms.2013.01.018 (2013).
Thiagarajan, S. et al. Predictors of prognosis for squamous cell carcinoma of oral tongue. J. Surg. Oncol. 109, 639–644, https://doi.org/10.1002/jso.23583 (2014).
Alves, P. M. et al. Significance of galectins-1, -3, -4 and -7 in the progression of squamous cell carcinoma of the tongue. Pathol. Res. Pract. 207, 236–240, https://doi.org/10.1016/j.prp.2011.02.004 (2011).
Akagi, J. & Baba, H. Prognostic value of CD57(+) T lymphocytes in the peripheral blood of patients with advanced gastric cancer. Int. J. Clin. Oncol. 13, 528–535, https://doi.org/10.1007/s10147-008-0789-8 (2008).
Menon, A. G. et al. Immune system and prognosis in colorectal cancer: a detailed immunohistochemical analysis. Lab. Invest. 84, 493–501, https://doi.org/10.1038/labinvest.3700055 (2004).
Lee, B. E. et al. TNM stage is the most important determinant of survival in metachronous lung cancer. Ann. Thorac. Surg. 88, 1100–1105, https://doi.org/10.1016/j.athoracsur.2009.06.098 (2009).
Okuyemi, O. T., Piccirillo, J. F. & Spitznagel, E. TNM staging compared with a new clinicopathological model in predicting oral tongue squamous cell carcinoma survival. Head Neck 36, 1481–1489, https://doi.org/10.1002/hed.23486 (2014).
Le Campion, A. et al. Low Survival Rates of Oral and Oropharyngeal Squamous Cell Carcinoma. Int J Dent 2017, 5815493, https://doi.org/10.1155/2017/5815493 (2017).
Murakami, Y. et al. Prognostic significance of lymph node metastasis and surgical margin status for distal cholangiocarcinoma. J. Surg. Oncol. 95, 207–212, https://doi.org/10.1002/jso.20668 (2007).
Yoshida, T. et al. Prognostic factors after pancreatoduodenectomy with extended lymphadenectomy for distal bile duct cancer. Arch. Surg. 137, 69–73, https://doi.org/10.1001/archsurg.137.1.69 (2002).
Oida, Y. et al. Laparoscopic-assisted resection of gastrointestinal stromal tumor in small intestine. Hepatogastroenterology 55, 146–149 (2008).
Duysinx, B. C. et al. Diagnostic value of interleukine-6, transforming growth factor-beta 1 and vascular endothelial growth factor in malignant pleural effusions. Respir. Med. 102, 1708–1714, https://doi.org/10.1016/j.rmed.2008.07.008 (2008).
Song, B. C. et al. Transforming growth factor-beta1 as a useful serologic marker of small hepatocellular carcinoma. Cancer 94, 175–180, https://doi.org/10.1002/cncr.10170 (2002).
Wang, C., Wang, G., Zhang, L., Pan, J. & Wei, Y. Latent Transforming Growth Factor beta Binding Protein 2 (LTBP2) as a Novel Biomarker for the Diagnosis and Prognosis of Pancreatic Carcinoma. Med. Sci. Monit. 23, 3232–3239, https://doi.org/10.12659/msm.905284 (2017).
Belge, K. U. et al. The proinflammatory CD14+ CD16+ DR++ monocytes are a major source of TNF. J. Immunol. 168, 3536–3542, https://doi.org/10.4049/jimmunol.168.7.3536 (2002).
Todd, I. et al. Elevated CD16 expression by monocytes from patients with tumor necrosis factor receptor-associated periodic syndrome. Arthritis Rheum. 56, 4182–4188, https://doi.org/10.1002/art.23133 (2007).
Horelt, A., Belge, K. U., Steppich, B., Prinz, J. & Ziegler-Heitbrock, L. The CD14+ CD16+ monocytes in erysipelas are expanded and show reduced cytokine production. Eur. J. Immunol. 32, 1319–1327 10.1002/1521-4141(200205)32:5<1319::AID-IMMU1319>3.0.CO;2-2 (2002).
Fernandez, G. C. et al. Differential expression of function-related antigens on blood monocytes in children with hemolytic uremic syndrome. J Leukoc Biol 78, 853–861, https://doi.org/10.1189/jlb.0505251 (2005).
Kawanaka, N. et al. CD14+,CD16+ blood monocytes and joint inflammation in rheumatoid arthritis. Arthritis Rheum. 46, 2578–2586, https://doi.org/10.1002/art.10545 (2002).
Lazaris, A. C., Segas, J. V., Nikolopoulos, T. P. & Patsouris, E. S. Tissue detection of natural killer cells in laryngeal carcinoma. Neoplasma 54, 379–382 (2007).
Grimm, M. et al. Analysis of circulating CD14+/CD16+ monocyte-derived macrophages (MDMs) in the peripheral blood of patients with oral squamous cell carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol 121, 301–306, https://doi.org/10.1016/j.oooo.2015.10.024 (2016).
Gonzalez, F. M. et al. Natural killer cell activity in laryngeal carcinoma. Arch. Otolaryngol. Head Neck Surg. 119, 69–72, https://doi.org/10.1001/archotol.1993.01880130071010 (1993).
Sorskaar, D., Forre, O. & Lie, S. O. Increased natural killer cell activity and numbers of Leu-7 and Leu-11b (CD 16)-positive cells in bone marrow of children in remission from acute lymphoblastic leukaemia. Scand. J. Immunol. 29, 65–72, https://doi.org/10.1111/j.1365-3083.1989.tb01100.x (1989).
Millrud, C. R. et al. NET-producing CD16(high) CD62L(dim) neutrophils migrate to tumor sites and predict improved survival in patients with HNSCC. Int. J. Cancer 140, 2557–2567, https://doi.org/10.1002/ijc.30671 (2017).
Del Mar Valenzuela-Membrives, M. et al. Progressive changes in composition of lymphocytes in lung tissues from patients with non-small-cell lung cancer. Oncotarget 7, 71608–71619, https://doi.org/10.18632/oncotarget.12264 (2016).
Sconocchia, G. et al. Tumor infiltration by FcgammaRIII (CD16)+ myeloid cells is associated with improved survival in patients with colorectal carcinoma. Int. J. Cancer 128, 2663–2672, https://doi.org/10.1002/ijc.25609 (2011).
Jewett, A., Teruel, A., Romero, M., Head, C. & Cacalano, N. Rapid and potent induction of cell death and loss of NK cell cytotoxicity against oral tumors by F(ab’)2 fragment of anti-CD16 antibody. Cancer Immunol. Immunother. 57, 1053–1066, https://doi.org/10.1007/s00262-007-0437-6 (2008).
Balkwill, F., Charles, K. A. & Mantovani, A. Smoldering and polarized inflammation in the initiation and promotion of malignant disease. Cancer Cell 7, 211–217, https://doi.org/10.1016/j.ccr.2005.02.013 (2005).
Gildener-Leapman, N., Ferris, R. L. & Bauman, J. E. Promising systemic immunotherapies in head and neck squamous cell carcinoma. Oral Oncol. 49, 1089–1096, https://doi.org/10.1016/j.oraloncology.2013.09.009 (2013).
Characiejus, D. et al. Predictive value of CD8highCD57+ lymphocyte subset in interferon therapy of patients with renal cell carcinoma. Anticancer Res. 22, 3679–3683 (2002).
Characiejus, D. et al. Peripheral blood CD8highCD57+ lymphocyte levels may predict outcome in melanoma patients treated with adjuvant interferon-α. Anticancer Res. 28, 1139–1142 (2008).
Sze, D. M. et al. Clonal cytotoxic T cells in myeloma. Leuk. Lymphoma 44, 1667–1674, https://doi.org/10.1080/1042819031000097438 (2003).
Van den Hove, L. E. et al. Peripheral blood lymphocyte subset shifts in patients with untreated hematological tumors: evidence for systemic activation of the T cell compartment. Leuk. Res. 22, 175–184, https://doi.org/10.1016/s0145-2126(97)00152-5 (1998).
Atayar, C., Poppema, S., Visser, L. & van den Berg, A. Cytokine gene expression profile distinguishes CD4+ /CD57+ T cells of the nodular lymphocyte predominance type of Hodgkin’s lymphoma from their tonsillar counterparts. J. Pathol. 208, 423–430, https://doi.org/10.1002/path.1894 (2006).
Park, M. H., Lee, J. S. & Yoon, J. H. High expression of CX3CL1 by tumor cells correlates with a good prognosis and increased tumor-infiltrating CD8+ T cells, natural killer cells, and dendritic cells in breast carcinoma. J. Surg. Oncol. 106, 386–392, https://doi.org/10.1002/jso.23095 (2012).
Ishigami, S. et al. Prognostic value of intratumoral natural killer cells in gastric carcinoma. Cancer 88, 577–583 10.1002/(sici)1097-0142(20000201)88:3<577::aid-cncr13>3.0.co;2-v (2000).
Park, B. G. et al. The extended leukocyte differential count using the Cytodiff flow cytometric system reveals that higher CD16+ cytotoxic NK+ T lymphocyte levels predict superior survival outcomes in patients with metastatic carcinoma. Cytometry B Clin. Cytom. 84, 202–204, https://doi.org/10.1002/cyto.b.21063 (2013).
Villegas, F. R. et al. Prognostic significance of tumor infiltrating natural killer cells subset CD57 in patients with squamous cell lung cancer. Lung Cancer 35, 23–28, https://doi.org/10.1016/s0169-5002(01)00292-6 (2002).
Karpathiou, G. et al. Prognostic impact of immune microenvironment in laryngeal and pharyngeal squamous cell carcinoma: Immune cell subtypes, immuno-suppressive pathways and clinicopathologic characteristics. Oncotarget 8, 19310–19322, https://doi.org/10.18632/oncotarget.14242 (2017).
Cruz, I., Meijer, C. J., Walboomers, J. M., Snijders, P. J. & Van der Waal, I. Lack of MHC class I surface expression on neoplastic cells and poor activation of the secretory pathway of cytotoxic cells in oral squamous cell carcinomas. Br J Cancer 81, 881–889, https://doi.org/10.1038/sj.bjc.6690780 (1999).
Paul, P. et al. HLA-G expression in melanoma: a way for tumor cells to escape from immunosurveillance. Proc Natl Acad Sci USA 95, 4510–4515, https://doi.org/10.1073/pnas.95.8.4510 (1998).
Adachi, W., Sugenoya, A. & Iida, F. Immune competent cells of regional lymph nodes in colorectal cancer patients: I. Flow cytometric analysis of lymphocyte subpopulation. J. Surg. Oncol. 46, 110–116, https://doi.org/10.1002/jso.2930460209 (1991).
Hermann, G. G., Petersen, K. R., Steven, K. & Zeuthen, J. Reduced LAK cytotoxicity of peripheral blood mononuclear cells in patients with bladder cancer: decreased LAK cytotoxicity caused by a low incidence of CD56+ and CD57+ mononuclear blood cells. J. Clin. Immunol. 10, 311–320, https://doi.org/10.1007/bf00917476 (1990).
Kurosawa, S. et al. Early-appearing tumour-infiltrating natural killer cells play a crucial role in the generation of anti-tumour T lymphocytes. Immunology 85, 338–346 (1995).
Zancope, E. et al. Differential infiltration of CD8+ and NK cells in lip and oral cavity squamous cell carcinoma. J Oral Pathol Med 39, 162–167, https://doi.org/10.1111/j.1600-0714.2009.00792.x (2010).
Sorbye, S. W. et al. Prognostic impact of CD57, CD68, M-CSF, CSF-1R, Ki67 and TGF-beta in soft tissue sarcomas. BMC Clin Pathol 12, 7, https://doi.org/10.1186/1472-6890-12-7 (2012).
Focosi, D., Bestagno, M., Burrone, O. & Petrini, M. CD57+ T lymphocytes and functional immune deficiency. J Leukoc Biol 87, 107–116, https://doi.org/10.1189/jlb.0809566 (2010).
Sterlacci, W. et al. High transforming growth factor beta expression represents an important prognostic parameter for surgically resected non-small cell lung cancer. Hum. Pathol. 43, 339–349, https://doi.org/10.1016/j.humpath.2011.05.017 (2012).
Tang, R. G. et al. Polymorphisms of transforming growth factor beta 1 (RS#1800468 and RS#1800471) and esophageal squamous cell carcinoma among Zhuangese population, China. Gene 512, 1–5, https://doi.org/10.1016/j.gene.2012.10.009 (2013).
Bennett, K. L., Romigh, T. & Eng, C. Disruption of transforming growth factor-beta signaling by five frequently methylated genes leads to head and neck squamous cell carcinoma pathogenesis. Cancer Res. 69, 9301–9305, https://doi.org/10.1158/0008-5472.CAN-09-3073 (2009).
Arteaga, C. L. et al. Anti-transforming growth factor (TGF)-beta antibodies inhibit breast cancer cell tumorigenicity and increase mouse spleen natural killer cell activity. Implications for a possible role of tumor cell/host TGF-beta interactions in human breast cancer progression. J. Clin. Invest. 92, 2569–2576, https://doi.org/10.1172/JCI116871 (1993).
Dranoff, G. Cytokines in cancer pathogenesis and cancer therapy. Nat. Rev. Cancer 4, 11–22, https://doi.org/10.1038/nrc1252 (2004).
Verstappen, J. & Von den Hoff, J. W. Tissue inhibitors of metalloproteinases (TIMPs): their biological functions and involvement in oral disease. J. Dent. Res. 85, 1074–1084 (2006).
Cooper, C. R. et al. Stromal factors involved in prostate carcinoma metastasis to bone. Cancer 97, 739–747, https://doi.org/10.1002/cncr.11181 (2003).
Johansson, N. et al. Expression of collagenase-3 (matrix metalloproteinase-13) in squamous cell carcinomas of the head and neck. Am. J. Pathol. 151, 499–508 (1997).
Salo, T., Lyons, J. G., Rahemtulla, F., Birkedal-Hansen, H. & Larjava, H. Transforming growth factor-beta 1 up-regulates type IV collagenase expression in cultured human keratinocytes. J. Biol. Chem. 266, 11436–11441 (1991).
Overall, C. M., Wrana, J. L. & Sodek, J. Transcriptional and post-transcriptional regulation of 72-kDa gelatinase/type IV collagenase by transforming growth factor-beta 1 in human fibroblasts. Comparisons with collagenase and tissue inhibitor of matrix metalloproteinase gene expression. J. Biol. Chem. 266, 14064–14071 (1991).
Molinolo, A. A. et al. Dysregulated molecular networks in head and neck carcinogenesis. Oral Oncol. 45, 324–334, https://doi.org/10.1016/j.oraloncology.2008.07.011 (2009).
Moutsopoulos, N. M., Wen, J. & Wahl, S. M. TGF-beta and tumors–an ill-fated alliance. Curr. Opin. Immunol. 20, 234–240, https://doi.org/10.1016/j.coi.2008.04.003 (2008).
Crane, C. A. et al. TGF-beta downregulates the activating receptor NKG2D on NK cells and CD8+ T cells in glioma patients. Neuro Oncol 12, 7–13, https://doi.org/10.1093/neuonc/nop009 (2010).
Acknowledgements
The authors would like to thank Prof. Amir Nader Emami Razavi, Dr Ali Abdollahi, Dr Hadis Mohamadpour, and Dr Mohammadreza Parmar for their valuable assistance in providing the patients, genetic assessments/consultations, pathological assessments, and data collection for this research. This report is prepared in accordance with the REMARK criteria for cancer prognostic biomarkers and STARD criteria for diagnostic factors. The study was self-funded by the authors and their institution.
Author information
Authors and Affiliations
Contributions
Maryam Elahi searched the literature, conceived the study, designed it, performed the experiments, collected/verified the data, mentored the theses and wrote most of the theses, and participated in drafting the methods part of the article. Vahid Rakhshan searched the literature, conceived the study, designed it, supervised the theses, verified the data, designed and performed the statistical analyses, prepared the figures and tables, and drafted the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elahi, M., Rakhshan, V. MED15, transforming growth factor beta 1 (TGF-β1), FcγRIII (CD16), and HNK-1 (CD57) are prognostic biomarkers of oral squamous cell carcinoma. Sci Rep 10, 8475 (2020). https://doi.org/10.1038/s41598-020-65145-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-65145-3
- Springer Nature Limited