Abstract
To reveal waning humoral immunity after second dose BNT162b2 vaccinations in a rural Japanese community and determine factors affecting antibody titers. We aimed to report Immunoglobulin G (IgG) antibody against the SARS-CoV-2 spike (S1) protein levels and neutralizing activity in a large scale community based cohort. Methods: Participants in the observational cross-sectional study received a second dose of vaccination with BNT162b2 (Pfizer/BioNTech) and were not previously infected with COVID-19. Questionnaire-collected data on sex, age, adverse vaccine reactions, and medical history was obtained. Results: Data from 2496 participants revealed that older age groups reached a low antibody titer 90–120 days after the second vaccination. Neutralizing activity decreased with age; 35 (13.3%) of those aged ≥ 80 years had neutralizing activity under the cut-off value. Neutralizing activity > 179 days from the second vaccination was 11.6% compared to that at < 60 days from the second vaccination. Significantly lower IgG antibody titers and neutralizing activity were associated with age, male sex, increased time from second vaccination, smoking, steroids, immunosuppression, and comorbidities. Conclusions: Antibody titer decreased substantially over time. Susceptible populations, older people, men, smokers, steroid users, immunosuppression users, and people with three or more comorbidities may require a special protection strategy.
Similar content being viewed by others
Introduction
The Coronavirus disease 2019 (COVID-19) pandemic has achieved global crisis status and impact. Vaccines against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) were administered worldwide as a rapid solution. Humoral and cellar immunity markers remain high among previously infected patients1,2; thus, immunity after vaccination is expected to remain high. However, reports from USA and Israel have shown that the number of newly infected patients was increasing within a few months of vaccination, especially for delta variants of the virus3,4. Antibody titer kinetics differ between post-vaccination and post-infection populations, suggesting that humoral immunity in both needs to be examined5. Modelling studies have shown that a low antibody titer is associated with weak protection against infection6,7. Similarly, neutralizing antibody levels were lower in those who had breakthrough infections in case–control studies8. Therefore, a community survey for humoral immunity after vaccination is crucial in establishing the strategy required to protect the population from SARS-CoV-2.
Aspects of humoral immunity in the post-vaccination population have already been investigated. For instance, the peak antibody titer after two doses of vaccine is lower in susceptible populations9. Humoral immunity is reduced, especially in the geriatric population and those on immunosuppressive drugs, at 6 months after vaccination10. However, only a few of these studies assessed antibody titers after vaccination in large sample sizes.
Japan experienced a surge in COVID-19 cases in August, 2021; a total of 1,726,823 cases were reported by 27th November. BENT162b2 vaccination was offered beginning March 2021 to health care workers, older adults and people with comorbidities, and then progressively to the general population. A total of 77% of the population aged ≥ 12 years who were eligible for vaccination had received second doses by 27th November. As a result, the number of infected patients decreased in November, and deregulation was being implemented by the government.
By December, the requirement for a third vaccination dose was actively discussed in Japan, as in other countries. However, there was confusion about the population eligible for the third dose. In the beginning, only those who had a second dose over 8 months previously were eligible, but on 16th November, those who had a second dose only 6 months previously were also eligible. This was quickly reverted on 17th November, and the policy returned to the earlier conditions where the third dose was available only for those who had a second dose more than 8 months previously.
Considering these situations, humoral immunity examination after vaccination was required to best formulate a strategy for infection prevention, especially in rural communities where older adults and susceptible populations live. Several studies have attempted to describe the relationship between higher antibody titer and health status in Japan (i.e., medications, comorbidities, alcohol consumption, smoking habits, and adverse reactions after vaccination)11,13,13. However, only a few of these studies mention the kinetics of antibody titers after vaccination. In addition, antibody testing among healthcare workers has been continuously conducted in the Ken-chu District of Fukushima Prefecture since 202014,15. Therefore, this area is suitable for assessing the antibody titers after vaccinations.
We aimed to assess the antibody titers on a large scale from Japanese communities to demonstrate the waning humoral immunity after the second BNT162b2 vaccination in a real-world rural community and to determine the factors affecting antibody titers. This survey was supported by the Japan Agency for Medical Research and Development, and this study presents the data generated from the first of five surveys which will be administered in the same cohort every 3 months.
Materials and methods
Study design and population
This was an observational cross-sectional study. The participants, recruited primarily from the rural Fukushima prefecture, included healthcare workers, frontline workers, administrative officers, general residents, and residents of long-term care facilities. Hospital groups and municipalities in Kenchu District and Soso District in Fukushima prefecture cooperated to recruit participants and perform blood sampling. Participants were mainly recruited from Ishikawa gun, Soma city, and Minami-soma city. A total of 1432 participants were recruited from Ishikawa gun, including 473 healthcare workers and 959 non-healthcare workers and general residents. A total of 500 participants were recruited from Soma city, mainly non-healthcare workers and general residents. A total of 594 participants were recruited from Minami Soma city, including 150 healthcare workers and 444 non-healthcare workers and general residents. The study was approved by the ethics committees of Hirata Central Hospital (number 2021-0611-1) and Fukushima Medical University (number 2021-116). This study conforms to The Code of Ethics of the World Medical Association (Declaration of Helsinki).
A total of 2526 participants completed the serological testing. The eligibility criteria of study participants were second dose vaccination with BNT162b2 (Pfizer/BioNTech) vaccine, no previous COVID-19 infection, and blood sampling being performed at least 10 days after the second vaccination (Fig. 1). We conducted sequential antibody surveys in 2021, and the peak titers were around 10 days from the second vaccination; thus, we conducted blood sampling after 10 days from the second vaccination16. Children ≥ 12 years were allowed to receive the COVID-19 vaccination; thus, we included 65 participants aged 12–19. The official interval between first and second doses was 21 days. A paper-based questionnaire was then conducted for all participants; data on sex, age, daily medications, medical history, date of vaccination, adverse reactions after vaccination, and type of vaccination were retrieved from the questionnaire. Written informed consent was obtained from all participants. All participants were given the serological assay results individually in writing, and authors frequently conducted seminars for medical staff and residents on how to interpret the serological results.
Study design of the serological assay
This research was supported by the Japan Agency for Medical Research and Development, a national project. All blood sampling was conducted between 8th September and 8th October in each facility in rural Fukushima prefecture. Centrifugal separation of blood samples was conducted in each facility, and serum samples were sent to Tokyo University. All serological assays were performed at Tokyo University, between 22nd September and 28th October. Levels of immunoglobulin G (IgG) antibody against the SARS-CoV-2 spike (S1) protein and the neutralizing activity were measured as the secondary immune status outcomes after second dose vaccination. IgG antibody titers against the SARS-CoV-2N-protein were used to determine the past COVID-19 infection status. We choose IgG(S) because the accuracy to measure hormonal immune response was assured in previous studies14,15.
Serological assay
All serological assays were performed using the CLIA assay with iFlash 3000 (YHLO Biotech, Shenzhen, China) and iFlash-2019-nCoV series (YHLO Biotech, Shenzhen, China) as reagents. The cut-off values for each parameter (IgG antibody against S1 protein, neutralizing activity, and IgG antibody against N protein) were 10 arbitrary units per milliliter (AU/mL), which were the official cut-off values. A neutralizing activity over > 500 AU/mL was not a guarantee of accuracy; thus, we interpreted measures of neutralizing activity > 500 AU/mL as being equal to 500 AU/mL. The testing process complied with the official guidelines. Quality assurance checks were performed every day before starting the measurement. For neutralizing activity, AU/mL × 2.4 was used to convert to International Units (IU/mL). For IgG, AU/mL × 1.0 was used to convert to binding antibody units (BAU/mL).
Statistical analysis
The median and mean antibody titer values were determined for both ‘age’ and ‘duration since second vaccination’ groups to identify groups with low antibody titers. The number of individuals with antibody titers under the cut-off values was shown group-wise. The mean titer for the ‘duration since second vaccination’ group was adjusted using a country-wide population age distribution based on the Japanese population in 1985. Violin plots were used to show the distribution of natural log-transformed antibody titer. Neutralizing activity > 500 AU/mL was taken as 500 AU/mL in all statistical methods.
Log transformed anti-S1 IgG antibody and neutralizing activity were analyzed as dependent variables with multiple linear regression to determine their association with the antibody titers and the participants’ characteristics. Age, sex, duration since second vaccination, the interval between vaccinations, smoking habits, alcohol consumption, daily medications, comorbidities, and the number of adverse reactions after the second vaccination dose were included in the multiple linear regression as dependent variables. We included comorbidities that are associated with low antibody titers in the literature: hypertension9, diabetes9, heart disease9, kidney disease17, cancer18,19, connective tissue disease20, and immune deficiency9,21. We considered the interaction between age and duration since vaccination; however, a relationship was not established. Individuals with missing data on dependent variables were excluded from the regression analysis.. STATA IC (Lightstone, Texas, USA, version 15) was used for all analyses.
Results
Between 8th September and 8th October, 2526 individuals in a rural area of Fukushima Prefecture completed blood sampling. Single blood sampling was performed on all participants. Of these, 21 individuals were over cut-off values of Anti-N antibody and thus excluded from participating in the study. Finally, 2496 participants were eligible for this study (Fig. 1). There were no missing data for anti-S1 IgG antibody, neutralizing activity, IgG antibody titers against N protein, age, and sex. Of these, 2358 participants (94.5%) without missing data were included in the multiple regression analysis.
The median age was 51 years (IQR; 37–67 years). Demographic characteristics and coexisting conditions are provided in Table 1. A total of 58 individuals were on regular steroids, and 24 were on immunosuppressive therapy (Table 1). The median of the interval between first dose and second dose was 21 days (IQR 21–22) among the whole cohort; of these 98 (3.9%) were < 21 days, 1,722 (69.0%) were 21 days, 464 (18.6%) were 22–28 days, and 212 (8.5%) were > 22 days. The relationships between the age group and the duration since the second vaccination are shown in Fig. S1. A total of 89% of participants who were ≥ 80 years had blood sampled in the period of 90–120 days after the second vaccination dose. The interquartile range and median for both anti-S1 IgG antibody and neutralizing activity titers for each age group are shown using a box plot (Fig. S1). The peak antibody titers were lower among the older age group; older participants reached a low antibody titer, 90–120 days after the second vaccination (Fig. S1).
Antibody titers were analyzed based on age groups to assess the differences in antibody titers across the demographic characteristics. The median anti-S1 IgG antibody and neutralizing activity titers decreased with age (Fig. 2). The median value of anti-S1 IgG antibody in participants aged ≥ 80 years was 10.9% of the median titer of those aged ≤ 19 years. The number of people with an antibody titer under cut-off value was 16; of these, 14 were aged ≥ 80 years. The median neutralizing activity decreased with age; 35 (13.3%) of those aged ≥ 80 years had neutralizing activity under the cut-off value, which is remarkably higher than in the other age groups. A total of 50 participants had antibody titers below the cut-off; of these, 15 were on steroids, four on immunosuppressants, seven on non-steroidal anti-inflammatory drugs, two on acetaminophen, and nine on antihistamines. Also, among these 50 participants, 28 had hypertension, 13 had heart disease, eight had rheumatism, and eight had diabetes.
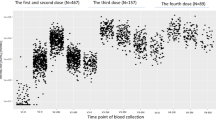
Antibody titers and neutralizing activity were assessed relative to the duration since the second vaccine dose (Fig. 3). The median anti-S1 IgG antibody and neutralizing activity decreased as the duration from the second vaccine dose increased. The median anti-S1 IgG antibody levels of participants who had the second dose > 179 days before testing was 18.3% lower than the median in participants who had the second dose < 60 days before testing. The adjusted mean value of anti-S1 IgG antibody levels of participants who had the second dose > 179 days before testing was 21.9% lower than the adjusted mean in participants who had the second dose < 60 days before testing. The adjusted mean value with the Japanese population age structure of 1985 tended to be slightly higher than the actual data. The frequency of levels under the cut-off value was the highest in participants who had the second dose > 4 months before testing (15 participants).
Distribution of (a) IgG antibody titer against S1 protein and (b) neutralizing activity by groups based on duration from second vaccination. Anti-S1 IgG antibody and neutralizing activity were log-transformed. The cut-off values of each antibody were 10 arbitrary units per milliliter (AU/mL). The adjusted mean titer was calculated using the age distribution of the whole country’s population based on the Japanese model population in 1985 (we do not have the new version of the model population).
Similarly, neutralizing activity decreased as the duration since the second vaccination increased. The median value of neutralizing activity in participants who had the second dose > 179 days before testing was 11.6% lower than that of participants who had the second dose < 60 days before testing. The adjusted mean value for neutralizing activity for those who had the second dose > 179 days before testing was 26.7% lower than the mean in those who had the second dose < 60 days before testing. The frequency of neutralizing activity under the cut-off value was the highest in participants who had the second dose > 4 months before testing (41 participants).
We used multivariate linear regression analysis to predict the variables that affect the log anti-S1 IgG antibody (Table 2). Significantly lower IgG antibody titer was associated with older age, male sex, longer time since second vaccination, smoking, regular use of steroids and immunosuppressants, and comorbidities (i.e., diabetes, heart disease, and connective tissue disease). Conversely, significantly higher IgG antibody titer was associated with female sex, 22–28 days interval between vaccinations, increased number of adverse reactions at second vaccination (such as > 37.5 ℃ fever, fatigue, headache, joint pain, diarrhea, nausea, and dizziness; Table 2), and hypertension.
Linear regression analysis was performed to predict the variables that affect the log-transformed neutralizing activity. The results were almost identical to those of the anti-S1 IgG antibody; however, heart disease and hypertension were not significantly associated with the neutralizing activity titer. An interval between vaccinations of > 28 days was significantly associated with higher neutralizing activity (Table 3).
Discussion
Understanding humoral immunity after vaccination in communities is crucial for COVID-19 infection control. This study revealed the waning of antibody titers after the second dose of BNT162b2 in real-world rural communities in Japan and determined the factors associated with decreased antibody titer.
Antibody titers decreased substantially over time in a rural community in Japan. In particular, both anti-S1 IgG antibody and neutralizing activity declined significantly within 3 months and declined slowly thereafter. A similar trend was observed in other cohort studies10. This speedy decline in humoral immunity after vaccination is faster than in vaccines for other diseases. Reports from Israel and the USA have shown an increase of infected patients a few months after vaccination3,4. For those > 4 months away from vaccination, humoral immunity has decreased notably from its peak.
Antibody titers showed a marked sharp decline among those aged ≥ 80 years. Low levels of both humoral and cellular immunity have been reported among older age groups, especially in people > 80 years22,24,24. Medical literature also reports the efficacy of the third vaccination in the elderly25. Stringent infection prevention strategies should be implemented for people ≥ 80 years and people who frequently come into contact with them.
In addition to the older adult population and the population with a relatively long interval since the last vaccination, male sex, smokers, steroid users, immunosuppressant users, individuals with diabetes, and individuals with connective tissue disease had lower antibody titers and neutralizing activities. Those with heart disease had significantly lower IgG titers but not neutralizing activity. Among these multi-risk susceptible populations, long-lasting infection and multi-mutation of virus genes were reported because of the impossibility of virus elimination26,28,28. In addition, patients who suffer breakthrough infections are often immunocompromised29. In high-risk populations such as these, monitoring humoral and cellular immunity after vaccination might be required.
The IgG and neutralizing activity titers were higher among those vaccinated with 22 to 28 days intervals between doses than those vaccinated with ≤ 21 days intervals. IgG and neutralizing activity were also higher among those who had experienced a systemic adverse reaction at the second dose. The results are consistent with previous reports that higher antibody titers are associated with longer intervals between vaccinations11. A vaccination interval of 22–28 days is the most efficacious in terms of antibody titer in the Japanese population.
Limitations of our study include the fact that the study design was a cross-sectional study with various demographic characteristics within participants, while the purpose of this study was to observe the kinetics of humoral immunity. The sample size was too small for findings to be generalized to the general population. The proportion of females was high. Data on comorbidities and medications were self-reported. Neutralizing activity titers > 500 AU/mL were not accurate and were taken as 500 AU/mL. Cellular immunity was not investigated. Hypertension was significantly associated with higher anti-S1 IgG antibody, but this result was inconsistent with those of other published works. Finally, the blood samples were not obtained from the participants at a fixed time point following the second dose. Therefore, variations between anti-S1 IgG antibody titers are expected. Humoral immunity was lower among older age groups and those with a long duration between vaccination and testing. The kinetics of individual humoral immunity and the factors associated with immunity need to be studied for a more extended period. To clarify these issues, we will continue to survey humoral immunity in the same cohort as a national project.
Conclusion
This study shows the waning of humoral immunity after the second vaccination. Neutralizing activity under the cut-off value is mainly found among those > 80 years old and > 4 months after the second vaccination. Susceptible populations, older age, males, smokers, steroid users, immunosuppressant users, and people with three or more comorbidities may require a special protective strategy and perhaps monitoring for immunity after vaccination.
Data availability
The data that support the findings of this study are available from Fukushima Medical University School of Medicine but restrictions apply to the availability of these data, which were used under license for the current study, and are not publicly available. Data are however available from the corresponding author upon reasonable request and with permission of Fukushima Medical University School of Medicine.
References
Alfano, G. et al. One-year persistence of neutralizing anti-SARS-CoV-2 antibodies in dialysis patients recovered from COVID-19. Hemodial. Int. 25, E53–E56. https://doi.org/10.1111/hdi.12963 (2021).
Le Bert, N. et al. SARS-CoV-2-specific T cell immunity in cases of COVID-19 and SARS, and uninfected controls. Nature 584, 457–462. https://doi.org/10.1038/s41586-020-2550-z (2020).
Goldberg, Y. et al. Waning immunity after the BNT162b2 vaccine in Israel. N. Engl. J. Med. 385, e85. https://doi.org/10.1056/NEJMoa2114228 (2021).
Tartof, S. Y. et al. Effectiveness of mRNA BNT162b2 COVID-19 vaccine up to 6 months in a large integrated health system in the USA: A retrospective cohort study. Lancet 398, 1407–1416. https://doi.org/10.1016/S0140-6736(21)02183-8 (2021).
Israel, A. et al. Large-scale study of antibody titer decay following BNT162b2 mRNA vaccine or SARS-CoV-2 infection. medRxiv https://doi.org/10.1101/2021.08.19.21262111 (2021).
Khoury, D. S. et al. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat. Med. 27, 1205–1211. https://doi.org/10.1038/s41591-021-01377-8 (2021).
Cromer, D. et al. Neutralising antibody titres as predictors of protection against SARS-CoV-2 variants and the impact of boosting: A meta-analysis. Lancet Microbe 3, e52–e61. https://doi.org/10.1016/S2666-5247(21)00267-6 (2022).
Bergwerk, M. et al. Covid-19 breakthrough infections in vaccinated health care workers. N. Engl. J. Med. 385, 1474–1484. https://doi.org/10.1056/NEJMoa2109072 (2021).
Lustig, Y. et al. BNT162b2 COVID-19 vaccine and correlates of humoral immune responses and dynamics: A prospective, single-centre, longitudinal cohort study in health-care workers. Lancet Respir. Med. 9, 999–1009. https://doi.org/10.1016/S2213-2600(21)00220-4 (2021).
Levin, E. G. et al. Waning immune humoral response to BNT162b2 Covid-19 vaccine over 6 months. N. Engl. J. Med. 385, e84. https://doi.org/10.1056/NEJMoa2114583 (2021).
Kageyama, T. et al. Antibody responses to BNT162b2 mRNA COVID-19 vaccine and their predictors among healthcare workers in a tertiary referral hospital in Japan. Clin. Microbiol. Infect. 27(1861), e1-1861.e5. https://doi.org/10.1016/j.cmi.2021.07.042 (2021).
Nomura, Y. et al. Age and smoking predict antibody titres at 3 months after the second dose of the BNT162b2 COVID-19 vaccine. Vaccines (Basel) 2021, 9. https://doi.org/10.3390/vaccines9091042 (2021).
Yamamoto, S. et al. Association between reactogenicity and SARS-CoV-2 antibodies after the second dose of the BNT162b2 COVID-19 vaccine. Vaccine https://doi.org/10.1101/2021.07.19.21260744 (2022).
Kobashi, Y. et al. Seroprevalence of SARS-CoV-2 antibodies among hospital staff in rural Central Fukushima, Japan: A historical cohort study. Int. Immunopharmacol. 98, 107884. https://doi.org/10.1016/j.intimp.2021.107884 (2021).
Kobashi, Y. et al. The difference between IgM and IgG antibody prevalence in different serological assays for COVID-19; lessons from the examination of healthcare workers. Int. Immunopharmacol. 92, 107360. https://doi.org/10.1016/j.intimp.2020.107360 (2021).
Kobashi, Y. et al. Peak IgG antibody titers against SARS-CoV-2 spike protein followingimmunization with the Pfizer/BioNTech BNT162b2 vaccine. Fukushima J. Med. Sci. 8, 67–70. https://doi.org/10.5387/fms.2021-28 (2022).
Hou, Y. C., Lu, K. C. & Kuo, K. L. The efficacy of COVID-19 vaccines in chronic kidney disease and kidney transplantation patients: A narrative review. Vaccines (Basel) 2021, 9. https://doi.org/10.3390/vaccines9080885 (2021).
Guven, D. C., Sahin, T. K., Kilickap, S. & Uckun, F. M. Antibody responses to COVID-19 vaccination in cancer: A systematic review. Front. Oncol. 11, 759108. https://doi.org/10.3389/fonc.2021.759108 (2021).
Tran, S., Truong, T. H. & Narendran, A. Evaluation of COVID-19 vaccine response in patients with cancer: An interim analysis. Eur. J. Cancer 159, 259–274. https://doi.org/10.1016/j.ejca.2021.10.013 (2021).
Furer, V. et al. Immunogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine in adult patients with autoimmune inflammatory rheumatic diseases and in the general population: A multicentre study. Ann. Rheum. Dis. 80, 1330–1338. https://doi.org/10.1136/annrheumdis-2021-220647 (2021).
Barrière, J., Re, D., Peyrade, F. & Carles, M. Current perspectives for SARS-CoV-2 vaccination efficacy improvement in patients with active treatment against cancer. Eur. J. Cancer 154, 66–72. https://doi.org/10.1016/j.ejca.2021.06.008 (2021).
Müller, L. et al. Age-dependent immune response to the Biontech/Pfizer BNT162b2 Coronavirous Disease 2019 Vaccination. Clin. Infect. Dis. 73, 2065–2072. https://doi.org/10.1093/cid/ciab381 (2021).
Parry, H. et al. mRNA vaccination in people over 80 years of age induces strong humoral immune responses against SARS-CoV-2 with cross neutralization of P.1 Brazilian variant. Elife 2021, 10. https://doi.org/10.7554/eLife.69375 (2021).
Collier, D. A. et al. Age-related immune response heterogeneity to SARS-CoV-2 vaccine BNT162b2. Nature 596, 417–422. https://doi.org/10.1038/s41586-021-03739-1 (2021).
Eliakim-Raz, N. et al. Antibody titers before and after a third dose of the SARS-CoV-2 BNT162b2 vaccine in adults aged ≥60 years. JAMA 326, 2203–2204. https://doi.org/10.1001/jama.2021.19885 (2021).
Moelling, K. Within-host and between-host evolution in SARS-CoV-2-New variant’s source. Viruses 13, 5. https://doi.org/10.3390/v13050751 (2021).
Avanzato, V. A. et al. Case study: Prolonged infectious SARS-CoV-2 shedding from an asymptomatic immunocompromised individual with. Cancer Cell 183, 1901–12.e9 (2020).
Choi, B. et al. Persistence and evolution of SARS-CoV-2 in an immunocompromised Host. N. Engl. J. Med. 383, 2291–2293. https://doi.org/10.1056/NEJMc2031364 (2020).
Brosh-Nissimov, T. et al. BNT162b2 vaccine breakthrough: Clinical characteristics of 152 fully vaccinated hospitalized COVID-19 patients in Israel. Clin. Microbiol. Infect. 27, 1652–1657. https://doi.org/10.1016/j.cmi.2021.06.036 (2021).
Acknowledgements
We would like to thank all the staff from Fukushima Medical University, Seireikai health care group, Hirata Village office, Soma City office, Soma Central Hospital, Soma General Hospital, Minamisoma City office, Minamisoma City Medical Association, Minamisoma Municipal General Hospital, and Medical Governance Institute, who contributed significantly to the accomplishment of this research, especially Ms. Yuka Harada, Ms. Naomi Ito, Ms. Serina Noji, Mr. Masahiko Nihei, Mr. Hideo Sato, Ms. Rie Yanai, Ms. Yasuko Suzuki, Ms. Keiko Abe, Dr. Hidekiyo Tachiya, Mr. Kouki Nakatsuka, Dr. Ryuzaburo Shineha, Ms. Miki Sato, Dr. Masahiko Sato, Mr. Naoharu Tadano, Mr. Kazuo Momma, Mr. Shu-ichi Mori, Ms. Saori Yoshisato, Ms. Katsuko Onoda, Mr. Satoshi Kowata, Mr. Masatsugu Tanaki, Ms. Xujin Zhu, and Ms. Tomoyo Nishimura.
Funding
This research was supported by AMED under Grant Number JP21nf0101638, and by Medical & Biological Laboratories Co., Ltd. and Shenzhen YHLO Biotech Co., Ltd., the distributor and manufacturer of the antibody measurement system (iFlash 3000). This research also was supported by grants from the Kowa Co. and Research Center for Advanced Science and Technology in the University of Tokyo.
Author information
Authors and Affiliations
Contributions
Conception of the work: Y.K., T.Ka., Y.N., F.O., M.T., K.S., T.Ko., M.Ts. Data collection: Y.K., Y.S., S.S., J.S., T.O., K.S. Investigation: T.Ka., A.S., A.N., Y.K., T.Ko. Data analysis and interpretation: Y.K., T.Ka., Y.S., Y.N., F.O., K.S., M.Ts. Data curation: Y.K., T.Z., C.Y., M.Y., M.Ko., A.M., S.S., M.Tan., M.Ka., Y.U. Drafting of the article: Y.K., T.Ka., M.Ts. Critical revision of the article: Y.K., T.Ka., M.Tak., T.Ko., M.Ts. Final approval of the version to be published: all authors.
Corresponding author
Ethics declarations
Competing interests
Kaneko is employed by Medical & Biological Laboratories, Co., (MBL, Tokyo, Japan). MBL imported the testing material used in this research. Kaneko participated in the testing process; however, he did not engage in the research design and analysis. Kobashi and Tsubokura received a research grant from Pfizer Health Research Foundation for research not associated with this work. The remaining authors declare no potential conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kobashi, Y., Kawamura, T., Shimazu, Y. et al. Humoral immunity after second dose of BNT162b2 vaccine in Japanese communities: an observational cross-sectional study, Fukushima Vaccination Community Survey. Sci Rep 12, 18929 (2022). https://doi.org/10.1038/s41598-022-21797-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-21797-x
- Springer Nature Limited
This article is cited by
-
Factors impacting antibody kinetics, including fever and vaccination intervals, in SARS-CoV-2-naïve adults receiving the first four mRNA COVID-19 vaccine doses
Scientific Reports (2024)
-
Seroepidemiological assessment of SARS-CoV-2 vaccine responsiveness and associated factors in the vaccinated community of the Casablanca-Settat Region, Morocco
Scientific Reports (2024)
-
Association of systemic adverse reaction patterns with long-term dynamics of humoral and cellular immunity after coronavirus disease 2019 third vaccination
Scientific Reports (2023)