Abstract
An unbiased and accurate diagnosis of benign and malignant endometrial lesions is essential for the gynecologist, as each type might require distinct treatment. Radiomics is a quantitative method that could facilitate deep mining of information and quantification of the heterogeneity in images, thereby aiding clinicians in proper lesion diagnosis. The aim of this study is to develop an appropriate predictive model for the classification of benign and malignant endometrial lesions, and evaluate potential clinical applicability of the model. 139 patients with pathologically-confirmed endometrial lesions from January 2018 to July 2020 in two independent centers (center A and B) were finally analyzed. Center A was used for training set, while center B was used for test set. The lesions were manually drawn on the largest slice based on the lesion area by two radiologists. After feature extraction and feature selection, the possible associations between radiomics features and clinical parameters were assessed by Uni- and multi- variable logistic regression. The receiver operator characteristic (ROC) curve and DeLong validation were employed to evaluate the possible predictive performance of the models. Decision curve analysis (DCA) was used to evaluate the net benefit of the radiomics nomogram. A radiomics prediction model was established from the 15 selected features, and were found to be relatively high discriminative on the basis of the area under the ROC curve (AUC) for both the training and the test cohorts (AUC = 0.90 and 0.85, respectively). The radiomics nomogram also showed good performance of discrimination for both the training and test cohorts (AUC = 0.91 and 0.86, respectively), and the DeLong test shows that AUCs were significantly different between clinical parameters and nomogram. The result of DCA demonstrated the clinical usefulness of this novel nomogram method. The predictive model constructed based on MRI radiomics and clinical parameters indicated a highly diagnostic efficiency, thereby implying its potential clinical usefulness for the precise identification and prediction of endometrial lesions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Endometrial lesions are commonly occurring diseases of the female reproductive system which can cause infertility or lead to an abnormal uterine bleeding1,2. As a consequence of the ageing population and increasing obesity rate3, the incidence of endometrial cancer (EC) is rapidly rising and it has become one of the most commonly diagnosed gynaecological malignancy in the developed world4. As a result of the tremendous advantage of significantly higher resolution, magnetic resonance imaging (MRI) could illustrate the endometrial conditions clearly, as well as the form the basis of imaging option for newly diagnosed EC patients5. However, an accurate and objective assessment of abnormalities related to the endometrium could pose a range of challenges to the radiologists and gynecologists. On the one hand, the normal endometrium is a dynamic tissue, that can be predominantly influenced by the age, menopausal status, menstrual cycle and the hormonal therapy6. Moreover, it has been found that overlapping image characters and clinical features of benign and malignant lesions might be detected simultaneously1,7. The varying sizes of the endometrial lesions pose a significant challenge to accurate diagnosis; presence of large lesions can lead to an abnormal appearance of endometrium and confuse exact origin of histology while small lesions that frequently overlap with the normal tissue are often ignored8. Transvaginal ultrasound and hysteroscopy have also been found to be helpful for the diagnosis of endometrial lesions, but both are dependent on the experience of the surgeons involved8,9, leading to a relatively high subjectivity and variability. Therefore, an accurate and precise differentiation between the benign and malignant endometrial lesions is important for efficient treatment.
Radiomics, a rapidly developing science, which can effectively convert the digital images into mineable high-dimensional data and thus clearly reflect biomedical information underlying both pathophysiological conditions and tumor heterogeneity10,11. It has been widely used to monitor the progression of the various diseases because it can overcome the deficiency of image interpretation by the human visual perception and thereby result in more objective and accurate information10. Our group has previously used CT-based radiomics to develop an automated diagnosis approach for the detection of ovarian neoplasm malignancy and obtained satisfactory results12. There are several reports that have focused on the precise evaluation of preoperative assessment of EC13,14,15. However, a reliable primary differential diagnosis of endometrial lesions is also urgently needed to guide the gynecologist to select an appropriate treatment. In this study, we hypothesized that imaging biomarkers could be potentially developed non-invasively to facilitate the differentiation between the benign and malignant diseases on the basis of MRI-based radiomics data that was extracted from the primary endometrial lesions.
Materials and methods
Study participants
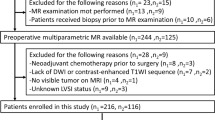
This retrospective study was performed by two independent centers jointly (center A and B). During January 2018 to July 2020, 164 consecutive histologically diagnosed endometrial lesions patients with preoperative MRI were independently collected at center A and B. These endometrial lesions encompassed benign and malignant endometrial diseases, including EC, endometrial hyperplasia, submucous myomas, endometrial polyps and endometritis. Inclusion criteria used were as follows: (1) female patients with histopathologically verified endometrial lesions, (2) patients without previous or current history of malignancy other than endometrial tumors, (3) no preoperative systemic therapy, (4) MRI performed within 30 days before the gynecological surgery. Exclusion criteria used were as follows: (1) low-quality imaging records (n = 3), (2) without surgical information (n = 12), (3) preoperative systemic therapy (n = 3), (4) malignancy other than EC (n = 2), (5) accompanied with distinct benign and malignancy lesions of endometrium (n = 5). Finally, a total of 139 patients were enrolled in this study, including 98 patients (with 46 and 52 patients with benign and malignant endometrial lesions respectively) treated in center A were assigned to the training cohort, whereas the 41 patients (with 19 and 22 patients corresponding to benign and malignant endometrial lesion respectively) treated in center B were assigned to the test cohort. An overview of the study’s workflow has been illustrated in Fig. 1.
MR imaging
The MR images were obtained by using the 3 T Trio Siemens scanner (center A) and 3 T Magnetom Skyra Siemens scanner (center B) with phased-array abdominal coils. All patients were required to breathe freely in supine position during the data acquisition. The following sequences were obtained: axial T1-weighed imaging (T1WI), axial T2-weighed imaging (T2WI), coronal and sagittal T2-weighed imaging with fat saturation (FS T2WI), and diffusion weighed imaging (DWI) with a b value of 0 and 800 s/mm2 with an apparent dispersion coefficient (ADC) map. FS T2WI images were acquired using turbo spin echo with fat saturation (repetition time (TR)/echo time (TE) = 3960/84, matrix = 512 × 512, filed of view (FOV) = 350 × 350 mm2, slice thickness = 4.0 mm, average = 1, voxel size = 0.8 × 0.8 × 4.0 mm3 for center A and TR/TE = 3200/101, matrix = 512 × 512, FOV = 207 × 207 mm2, slice thickness = 4.0 mm, average = 2, voxel size = 0.6 × 0.6 × 4.0 mm3 for center B).
Imaging segmentation
All the regions of interest (ROI) were segmented using ITK-SNAP software (version 3.8.0, www.itksnap.org) starting from the baseline DICOM image. The manual ROI segmentation was performed from the largest lesion diameter slice16 in sagittal FS T2WI sequence by a radiologist (Reader A, with 5 years’ experience in abdominal MRI) who was blinded to the histopathology data of the patients. A month later, another radiologist (Reader B, with 10 years’ experience in abdominal MRI) were randomly selected images obtained from 30 different and repeated the manual ROI drawings. The extracted features of the ROIs from two the different readers were calculated using the intra-class correlation coefficient (ICC).
Feature extraction and selection
Spatial resampling was performed before feature extraction. The original DICOM data of sagittal FS T2WI and the paired 2D ROIs were resampled by 1 × 1 × 1 voxel. Radiomics features including Histogram, Form Factor, Haralick, Gray-level co-occurrence matrix (GLCM), Gray-level zone-size matrix (GLZSM) and Gray-level Run-length matrix (GLRLM) were thereafter calculated by AK software (Artificial Intelligence Kit V 3.0.0R, GE Healthcare). GLCM and GLRLM in four different directions (0°, 45°, 90°, 135°) and three offsets1,4,7 were calculated to describe the possible spatial distribution or patterns. Finally, each ROI resulted in extraction of 396 distinct features.
There were three steps used for the preprocessing of the data. Firstly, the outliers were replaced by the median of the same features. Secondly, z-score normalization is applied to eliminate the differences in the value scale of the features. Thirdly, patients treated in center A were assigned to the training set (n = 98), and the test set consisted of patients only from center B (n = 41). Center A and B are two different institutions with different patients data and MRI scanning equipment, which is better to evaluate the generalization of the models by using them as the training and test sets respectively.
Prior to the feature reduction, intraclass correlation coefficient (ICC) was calculated for each feature from Reader A and Reader B to remove the poorly reproducible and less robust features. Additionally, only image features with ICC > 0.75 were considered as qualified features, thereby indicating a high reproducibility and agreement14, and were reserved for subsequent calculation.
The maximum relevance minimum redundancy (mRMR) package in R software (Version 3.4.4) was employed to remove the redundant and irrelevant features preliminarily in the training dataset, and the 20 most significant features were preserved. The least absolute shrinkage and selection operator (LASSO)17 algorithm was used to effectively compress the coefficients of extracted features and cause the regression coefficients to become zero, by constructing a specific penalty function, so as to achieve an effective reduction in the additional features. In this process, the ten-fold cross-validation was then used to accurately calculate the optimal parameter λ, which was obtained at the minimum objective function value of LASSO regression model.
Model construction and assessment
The final selected features were used to construct the radiomics model, under the optimal parameter λ of LASSO algorithm. The radiomics signature was obtained for the sum of the product of the final selected features and their corresponding coefficients weighed value, which was equivalent to radiomics score (radscore).
In the training cohort, univariate logistic regression was performed to potentially screen the various clinical parameters for endometrial lesions, including age18, body mass index (BMI)19,20, status of menopause21, as well as the conditions of hypertension and diabetes22. Multivariate logistic regression and stepwise regression were utilized to choose the significant indicator, to facilitate the development of a more comprehensive and efficacious nomogram model for the differentiation of the benign and malignant endometrial diseases. Moreover, the novel nomogram model which combined clinical parameters and Radscore was established, based on the multivariate logistic regression.
Receiver operating characteristics (ROC) curve was used to evaluate the discriminatory ability of models. Patients from two centers were thereafter classified into benign- or malignant-probability groups based on the cutoff values of ROC curve, and the nomogram method could precisely indicate the probability of occurrence of endometrial malignancy. Hosmer–Lemeshow test and calibration curves were used to assess performance of the model. Finally, the decision curve analysis (DCA) was also performed to validate the feasibility of the nomogram.
Statistical analysis
The statistical analysis was conducted by using the SPSS 22.0 software and the R software. The count data between the samples was compared by χ2 test. The normality of data was verified by Kolmogorov–Smirnov test. All of the different parameters from the two datasets were compared statistically. The normally distributed data was analyzed by t test, and skewed distributed data was analyzed by Mann–Whitney U test. The predictive diagnostic efficiency of the models was also evaluated by the area under the ROC curve (AUC) and its 95% confidence interval (95% CI) to determine the specificity, sensitivity, and accuracy of the data.
Ethics approval and consent to participate
This retrospective study based on the use of anonymous data was approved by the Ethic Committee of Jiangxi Provincial People’s Hospital, and the requirement for informed consent was waived. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional (Jiangxi Provincial People’s Hospital) and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Results
Patient clinical characteristics
Overall, with regard to the indicators of age, BMI, status of menopause, prevalence of hypertension and diabetes, there were no significant differences observed between the training and test cohorts, as shown in Table 1. However, there were statistical differences in the various clinical parameters (age, menopause) between the benign and malignant endometrial diseases for the training cohort (p < 0.05), but no significant clinical parameters for the test cohort (p > 0.05).
Outcomes performance of the clinical parameters model
The prediction model consisting of the clinical parameter for classifying the benign and malignant endometrial lesions returned the following performance metrics. The AUC was 0.70 (with a 95% CI 0.60–0.80) and the specificity, sensitivity, as well as accuracy were observed to be 54.3, 80.8, 68.4% respectively in the training cohort. For the test cohort, the AUC was 0.65 (with a 95% CI 0.49–0.81) and the specificity, sensitivity, and accuracy were found to be 57.9, 72.7, 65.9% respectively (see Table 2).
Construction and assessment of the radiomics signature model
Features with ICC < 0.75 were removed, leaving 271/396 features (68.4%). After selection of the various features and dimension reduction, the top 15 important features were finally selected, and these were employed for the construction of radiomics signature model (see Fig. 2). The results indicated a good prediction performance for both the training and test data with only marginal differences. It was found that the radiomics signature model exhibited a satisfactory performance with AUC values of 0.90 (with a 95% CI 0.84–0.96) and 0.85 (with a 95% CI 0.72–0.98) in the training and test cohorts, specificity values of 76.1 and 57.9%, sensitivity values of 94.2 and 95.5%, and accuracy values of 85.7 and 78.0%, respectively (see Table 2). The radscore showed a significantly better discrimination both in the training and test data, comparing with clinical parameters model, thereby indicating the high potency of radiomics signature in the differential diagnosis of endometrial diseases (Fig. 3).
The selection of the various features and dimension reduction was performed using LASSO method. (a) Ten-fold cross-validation was used to choose the optimal parameter (λ) with the minimum criteria, thus determining the number of the features. (b) Coefficients for the optimal parameter (λ). A vertical line was drawn at the selected value of log (λ) and showed the coefficients with non-zero. (c) The final selected features and corresponding coefficients.
Construction and assessment for the nomogram model
The age, menopause, hypertension were thereafter filtered as potentially clinical predictors of endometrial lesions by using a univariate logistic regression model (p < 0.1). For proper identification of benign and malignant endometrial diseases in patients, the most predictive subset of clinical parameters (age and menopause) was selected as they obtained the smallest value of Akaike information criterion (AIC) in the stepwise regression. Multivariate logistic regression finally yielded the three significant predictors including radscore, age, menopause, and lead to the construction of a more comprehensive and robust prediction model and nomogram (Fig. 4).
Radiomics nomogram showed excellent calibration potential in the prediction of properties of endometrial lesions through the calibration curves for both training and test cohorts (Fig. 4), but Hosmer–Lemeshow test indicated no statistical significance (p > 0.05). The AUCs of radiomics nomogram were 0.91 (with a 95% CI 0.86–0.97) and 0.86 (with a 95% CI 0.74–0.98) for the training and test sets respectively (Fig. 5). The specificity, sensitivity, accuracy were 91.3, 75.0, 82.7% for the training set, and 76.2%, 85.0%, 80.5% for the test set, respectively (Table 2).
(a) The ROC curve and corresponding AUC values for the nomogram, radiomics signature and the clinical parameter models for identification of the benign and malignant endometrial lesions (left: training cohort; right: test cohort). (b) The decision curve analysis was used to evaluate the clinical benefit of the models. The green, blue and red lines correspond to the clinical parameter, radiomics signature and radiomics nomogram models respectively. The black line represents an extreme situation where all indicators are positive, while the horizontal red line represents the other extreme situation where all analyzed indicators are negative.
Based on the results of DeLong test, the AUCs of the models were observed to be significantly different between the clinical indexes and nomogram in both the training and test cohorts (p < 0.05, see Table 3), which indicated a favorable prediction performance for the nomogram on both the cohorts. Moreover, according to the cut-off value of 0.566 for Youden index, the nomogram could potentially evaluate the risk score for endometrial lesions, and facilitate the categorization of patients into low- and high-risk groups. Figure 5 depicts the DCA plot of the radiomics nomogram. The outcomes indicated a more excellent risk prediction performance of the developed nomogram method as compared to the clinical parameters model.
Discussion
The major outcome of this study was the construction of the novel classification model based on radiomics, which can effectively differentiate the patients with benign and malignant endometrial lesions. Both the nomogram and radiomics models show better efficiency than clinical parameters model, implying the clinical value of preoperative and non-invasive detection of EC. Although the nomogram and radiomics models exhibit comparable AUC value, nomogram could quantify the risk probability of endometrial lesions rather than unreadable high-dimensional features.
Robustness of the features extracted from images is essential for the development of the radiomics. Target segmentation, feature extraction, feature selection, and classification model implementation are affected by high inter- and intra-observer variability23. We chose manual segmentation because the dataset of this study is relatively small and ICC was calculated to improve the robustness and reproducible of the features. Radiologists can flexibly delineate targets manually resulting in highly accurate segmentation and manual segmentation is more intuitive and easily implemented way of obtaining a target lesion. Nevertheless, manual segmentation is labor-intensive, time-consuming, and not always feasible for radiomics analysis requiring huge datasets. The use of automatic or semi-automatic segmentation method could overcome the problem of strongly operator-dependent. Hence, most of radiomics studies with large datasets were based on automatic or semi-automatic segmentation methods. Many semi-automatic delineation algorithms, such as region growing or thresholding, are used in the clinical environment although less precise than manual segmentation24.
The study focused on FS T2WI images for radiomics data extraction, since there were informative demonstrations in previously reported radiomics studies25,26. Moreover, ADC images possess high requirement of magnetic field uniformity and have been found to be more susceptible to artifacts, especially in the pelvic region13. Dynamic contrast material-enhanced T1WI was not considered as the conventional sequence for some benign endometrial diseases. Herein, the 15 extracted features were comprised by the different parameters of Form Factor, Haralick, GLRLM and GLCM. The Form Factor features included detailed descriptors of the three-dimensional size and shape of the lesion region27, thus indicating the role of lesion size as an important predictor of the differential diagnosis for endometrial diseases28. GLCM features could also describe the complexity and level change in the values by quantifying the distribution of co-occurrence matrix29. Entropy and inertia of GLCM can reflect both the randomness of intensity image and the clarity of image respectively. Moreover, energy of GLCM and Haralick parameters emphasized the uniformity, known as local homogeneity29. CLRLM features primarily reflected roughness and directionality of the texture30.
The radiomics analysis has already been applied against endometrial disorders and exhibited superior outcomes, especially for EC. For example, Yan et al. constructed a radiomics model, which could precisely evaluate the conditions of pelvic lymph node, thus aiding with preoperative diagnosis of lymphatic metastasis of EC31. Moreover, another study developed innovative clinical-radiomics machine learning models and attempted to identify the various molecular anomalies of EC from contrast enhanced CT images noninvasively32. The major advantage of the nomogram is that the outcomes can provide the exactly risk stratification with general MRI image. The outcomes of nomogram contain an objective and specific probability of the correct scores of EC9, even if the model can’t be the ideal level of pathology and the misclassification is inevitable. It has been found that sometimes it can be difficult for the radiologists and gynecologists to give a specific judgment for their diagnoses preoperatively. The ability to utilize objective probability is of significant benefit for the diagnosis that could make up for misjudgment on part of the clinicians. Moreover, as the nomogram can provide definite information regarding these high-risk factors from MR images before treatment, it might help to effectively screen EC patients who might require more extensive surgery with preoperative risk stratification for optimal selection, and at the same time minimizing overtreatment of low risk patients.
There are few limitations associated with this study. First, the number of patients enrolled was relatively small, especially in case of patients with benign endometrial lesions which included multi-subtypes. Moreover, there were only five common types of endometrial lesions analyzed in the study, and cases with low incidence were not included. Second, the study did not perform the volumetric analysis, because it requires considerably more time and efforts. Hence, some important features connected with intrinsic heterogeneity might have been missed for the two-dimensional method. Lacking of multi-image study is another main limitation. Theoretically, every MRI sequences can be mined for huge information. Further validation utilizing prospective studies are also needed. It might also be essential to confirm the robustness and applicability for the prediction model, by carefully avoiding intrinsic biases and overfitting33. Hence, a larger and richer dataset will be needed to significantly strengthen our model and further validate the generalization ability, so that the model can be successfully applied to several different conditions.
Conclusions
This study constructed a visualized nomogram model by combining radiomics signatures and the clinical parameters. The nomogram model exhibited an enormous clinical application value in predicting the objective probability of endometrial lesions classification non-invasive, and thus can aid the gynecologists for assessment and designing personalized treatment strategies. However, more efforts should be made to further improve applications and robustness of the model, so that it may become a real risk stratification tool for use in patients with endometrial lesions in the clinic.
Data availability
The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ADC:
-
Apparent dispersion coefficient
- AIC:
-
Akaike information criterion
- AUC:
-
Area under the receiver operation characteristic curve
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- DCA:
-
Decision curve analysis
- DWI:
-
Diffusion weighted imaging
- EC:
-
Endometrial cancer
- FOV:
-
Field of view
- FS-T2WI:
-
T2-weighted image with fat saturation
- GLCM:
-
Gray level co-occurrence matrix
- GLRLM:
-
Gray level run-length matrix
- GLZSM:
-
Gray level zone-size matrix
- ICC:
-
Intra-class correlation coefficient
- LASSO:
-
The least absolute shrinkage and selection operator
- MRI:
-
Magnetic resonance imaging
- mRMR:
-
Maximum relevance minimum redundancy
- ROC:
-
Receiver operation characteristic
- ROI:
-
Region of interest
- TE:
-
Echo time
- TR:
-
Repetition time
- T1WI:
-
T1-weighted image
- T2WI:
-
T2-weighted image
References
Bacon, J. L. Abnormal uterine bleeding: Current classification and clinical management. Obstet. Gynecol. Clin. North Am. 44(2), 179 (2017).
Vander Borght, M. & Wyns, C. Fertility and infertility: Definition and epidemiology. Clin. Biochem. 62, 2–10 (2018).
Bafligil, C. et al. Association between genetic polymorphisms and endometrial cancer risk: A systematic review. J. Med. Genet. 57(9), 591–600 (2020).
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2019. CA: A Cancer J. Clin. 69(1), 7–34 (2019).
Nougaret, S. et al. Endometrial cancer MRI staging: Updated guidelines of the European Society of Urogenital Radiology. Eur. Radiol. 29(2), 792–805 (2019).
Nalaboff, K. M., Pellerito, J. S. & Ben-Levi, E. Imaging the endometrium: Disease and normal variants. Radiographics 21(6), 1409–1424 (2001).
Kierans, A. S., Bennett, G. L., Haghighi, M. & Rosenkrantz, A. B. Utility of conventional and diffusion-weighted MRI features in distinguishing benign from malignant endometrial lesions. Eur. J. Radiol. 83(4), 726–732 (2014).
Bakir, B. et al. Role of diffusion weighted MRI in the differential diagnosis of endometrial cancer, polyp, hyperplasia, and physiological thickening. Clin. Imaging 41, 86–94 (2017).
Zhang, Y. et al. Deep learning model for classifying endometrial lesions. J. Transl. Med. 19(1), 10 (2021).
Gillies, R. J., Kinahan, P. E. & Hricak, H. Radiomics: Images are more than pictures, they are data. Radiology 278(2), 563–577 (2016).
Rizzo, S. et al. Radiomics: The facts and the challenges of image analysis. Eur. Radiol. Exp. 2(1), 36 (2018).
Li, S. et al. A radiomics approach for automated diagnosis of ovarian neoplasm malignancy in computed tomography. Sci. Rep. 11(1), 8730 (2021).
Stanzione, A. et al. Deep myometrial infiltration of endometrial cancer on MRI: A radiomics-powered machine learning pilot study. Acad. Radiol. 28(5), 737–744 (2021).
Fasmer, K. E. et al. Whole-volume tumor MRI radiomics for prognostic modeling in endometrial cancer. J. Magn. Reson. Imaging 53(3), 928–937 (2021).
Chen, X. et al. Deep learning for the determination of myometrial invasion depth and automatic lesion identification in endometrial cancer MR imaging: A preliminary study in a single institution. Eur. Radiol. 30(9), 4985–4994 (2020).
Ueno, Y. et al. Endometrial carcinoma: MR imaging-based texture model for preoperative risk stratification-A preliminary analysis. Radiology 284(3), 748–757 (2017).
Kato, T. & Uemura, M. Period analysis using the least absolute shrinkage and selection operator (Lasso). Publ. Astron. Soc. Japan 64(6), 122 (2012).
Castle, P. E. et al. Relationship of atypical glandular cell cytology, age, and human papillomavirus detection to cervical and endometrial cancer risks. Obstet. Gynecol. 115(2 Pt 1), 243–248 (2010).
Nagle, C. M. et al. Impact of weight change and weight cycling on risk of different subtypes of endometrial cancer. Eur. J. Cancer 49(12), 2717–2726 (2013).
Crosbie, E. J., Zwahlen, M., Kitchener, H. C., Egger, M. & Renehan, A. G. Body mass index, hormone replacement therapy, and endometrial cancer risk: A meta-analysis. Cancer Epidemiol. Biomark. Prev. 19(12), 3119–3130 (2010).
Xu, W. H. et al. Menstrual and reproductive factors and endometrial cancer risk: Results from a population-based case-control study in urban Shanghai. Int. J. Cancer 108(4), 613–619 (2004).
Wijaya, C. Diabetes mellitus and hypertension are risk factor for endometrial cancer. Indones. J. Obstet. Gynecol. https://doi.org/10.32771/inajog.v36i3.314 (2016).
van Timmeren, J. E., Cester, D., Tanadini-Lang, S., Alkadhi, H. & Baessler, B. Radiomics in medical imaging—“how-to” guide and critical reflection. Insights Imaging 11(1), 91 (2020).
Stefano, A. et al. Robustness of PET radiomics features: Impact of Co-Registration with MRI. Appl. Sci. 11(21), 10170 (2021).
Shu, Z. et al. MRI-based Radiomics nomogram to detect primary rectal cancer with synchronous liver metastases. Sci. Rep. 9(1), 3374 (2019).
Kocak, B. et al. Predicting response to somatostatin analogues in acromegaly: Machine learning-based high-dimensional quantitative texture analysis on T2-weighted MRI. Eur. Radiol. 29(6), 2731–2739 (2019).
Limkin, E. J. et al. The complexity of tumor shape, spiculatedness, correlates with tumor radiomic shape features. Sci. Rep. 9(1), 4329 (2019).
Sozzi, G. et al. Tumor size, an additional risk factor of local recurrence in low-risk endometrial cancer: A large multicentric retrospective study. Int. J. Gynecol. Cancer 28(4), 684–691 (2018).
Dhruv, B., Mittal, N. & Modi, M. Study of Haralick’s and GLCM texture analysis on 3D medical images. Int. J. Neurosci. 129(4), 350–362 (2019).
Chu, H. et al. Value of MRI radiomics based on enhanced T1WI images in prediction of meningiomas grade. Acad. Radiol. 28(5), 687–693 (2021).
Yan, B. C. et al. Radiologists with MRI-based radiomics aids to predict the pelvic lymph node metastasis in endometrial cancer: A multicenter study. Eur. Radiol. 31(1), 411–422 (2021).
Veeraraghavan, H. et al. Machine learning-based prediction of microsatellite instability and high tumor mutation burden from contrast-enhanced computed tomography in endometrial cancers. Sci. Rep. 10(1), 17769 (2020).
Ji, G. W. et al. Biliary tract cancer at CT: A radiomics-based model to predict lymph node metastasis and survival outcomes. Radiology 290(1), 90–98 (2019).
Funding
This study was supported by the Funding of Jiangxi Province Department of Science and Technology (Grants No.20202BABL206112), and the Funding of Health Commission of Jiangxi Province (Grants Nos. 20203036 and 202110004).
Author information
Authors and Affiliations
Contributions
Conception and design: B.F., J.H.Y. and J.Q.L.; Patients and clinical data collection: S.Y.L. and P.Y.L.; Image data collection: J.Q.L. and S.Y.L.; ROI delineation: J.Q.L. and B.F.; Data analysis: P.P.P. and J.Q.L.; Manuscript writing: J.Q.L., H.S.L., B.F., J.H.Y. and P.P.P.; Final approval of manuscript: All authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, J., Li, S., Lin, H. et al. Development of MRI-based radiomics predictive model for classifying endometrial lesions. Sci Rep 13, 1590 (2023). https://doi.org/10.1038/s41598-023-28819-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-28819-2
- Springer Nature Limited
This article is cited by
-
Evaluating the quality of radiomics-based studies for endometrial cancer using RQS and METRICS tools
European Radiology (2024)
-
Application of magnetic resonance imaging radiomics in endometrial cancer: a systematic review and meta-analysis
La radiologia medica (2024)