Abstract
The number of diabetic foot ulcer patients is substantially increasing, with the rapidly rising burden of diabetic mellitus in sub-Saharan Africa. The data on the regional prevalence of diabetic foot ulcer infecting bacteria and their antimicrobial resistance patterns is crucial for its proper management. This systematic review and meta-analysis determined the pooled prevalence of bacterial profiles and antimicrobial resistance patterns of infected diabetic foot ulcers in sub-Saharan Africa. A comprehensive search of the literature was performed on CINAHL, EMBASE, Google Scholar, PubMed, Scopus, and Web of Science databases. Critical appraisal was done using the Joanna Briggs Institute’s tool for prevalence studies. A pooled statistical meta-analysis was conducted using STATA Version 17.0. The I2 statistics and Egger’s test were used to assess the heterogeneity and publication bias. The pooled prevalence and the corresponding 95% confidence interval of bacterial profiles and their antimicrobial resistance patterns were estimated using a random effect model. Eleven studies with a total of 1174 study participants and 1701 bacteria isolates were included. The pooled prevalence of the most common bacterial isolates obtained from DFU were S. aureus (34.34%), E. coli (21.16%), and P. aeruginosa (20.98%). The highest pooled resistance pattern of S. aureus was towards Gentamicin (57.96%) and Ciprofloxacin (52.45%). E.coli and K. Pneumoniae showed more than a 50% resistance rate for the most common antibiotics tested. Both gram-positive and gram-negative bacteria were associated with diabetic foot ulcers in sub-Saharan Africa. Our findings are important for planning treatment with the appropriate antibiotics in the region. The high antimicrobial resistance prevalence rate indicates the need for context-specific effective strategies aimed at infection prevention and evidence-based alternative therapies.
Similar content being viewed by others
Introduction
Diabetic foot ulcer (DFU) is a severe chronic diabetic complication, which affected 15–25% of diabetic patients in their lifetime1. The International Diabetes Federation estimated that DFU affected 9.1 million to 26.1 million people with diabetes worldwide in 20152. The global incidence of DFU has recently increased due to the increased longevity of diabetic patients and the increased prevalence of diabetes mellitus worldwide3. In sub-Saharan Africa (SSA), the number of DFU patients is increasing substantially, with the rapid rising of diabetes prevalence in the region4,5.
DFUs can progress rapidly to infection, contributing to significant morbidity and mortality in diabetic patients6. DFUs can be infected by different aerobes and anaerobes bacteria, Gram-positive and Gram-negative bacteria7. Polymicrobial DFUs infections can occur in chronic DFUs which can be colonized by different types of aerobic bacteria, such as Staphylococcus, Streptococcus, Enterococcus, Pseudomonas species, and anaerobic pathogens7,8. The frequency of typical microorganisms isolated from DFUs differs substantially across studies carried out in various locations throughout the world9,10,11,12. The bacterial distribution in DFUs can in be influenced by different factors such as geographical features, infection duration, patient’s metadata (e.g., smoking habits), and antibiotic use7.
According to a review conducted in 2014 by Lord Jim O'Neill and his team, it was estimated that antimicrobial resistance (AMR) has the potential to result in approximately 10 million deaths annually by the year 205013. Antimicrobial resistance is a significant public health threat that has been implicated in several studies on DFUs and identified as among the key challenges to the achievement of sustainable development goals (SDG)14,15,16,17. A study from Kenya reported that the bacterial isolates from DFUs showed resistance to commonly used antibiotics such as ampicillin, amoxicillin, cefepime, ceftazidime, cefuroxime, clindamycin, erythromycin, piperacillin–tazobactam, tetracycline and trimethoprim–sulphamethoxazole15. Another study from Iran revealed that multidrug-resistant (MDR) bacteria constituted up to 48.4% of moderate-to-severe diabetic foot infections, with 37.5% of isolated Enterococcus species being vancomycin-resistant Enterococcus, 48.8% of Staphylococcus species. Being methicillin-resistant, 77.8% of isolated E. coli being ESBL and 66.7% of isolated Pseudomonas being MDR17. A recent review and meta-analysis identified ischemic ulcer, ulcer size, ulcer grade, osteomyelitis, previous antibiotic therapy and previous hospitalization as the risk factors for AMR in patients with DFU18.
Hence, there is a significant discrepancy in the prevalence of DFU-infecting bacteria and their AMR patterns across different regions of the world, regional data for sub-Saharan Africa is crucial for the proper management of DFUs. To date, no systematic review and meta-analysis have been conducted to investigate the prevalence and patterns of AMR in DFUs in the region. Therefore, we conducted a systematic review and meta-analysis of the literature to investigate the prevalence and patterns of AMR in DFUs in Sub-Saharan Africa.
Methods
Protocol registration
The International Prospective Register of Systematic Reviews (PROSPERO) has registered the study protocol for this systemic review and meta-analysis with registration code CRD4202338877519.
Search strategy and selection of studies
This systematic review was done according to Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram (Fig. 1)20. The combination of MeSH/Emtree terms and free text words were used to run for each database using Boolean operators “AND” and “OR.” CINAHL, EMBASE, PubMed, Scopus, and Web of Science databases were used to retrieve the studies (supplementary material Table 1). The reference lists of all included studies were screened to obtain additional studies and authors were contacted to receive any missing articles. Original studies conducted in SSA were included without restriction on the language and year of publication21.
PRISMA flow diagram of included studies: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. https://doi.org/10.1136/bmj.n71.
EndNote version 20.2.1. was used to remove duplicates. Two independent reviewers (FW and MTB) screened titles and abstracts, which were double-checked by a third reviewer (AAA). Potentially relevant studies were retrieved in full text and eligible studies were assessed in detail against the inclusion criteria by two reviewers (FW and MTB) and double-checked by a third reviewer (MTB). Reasons for the exclusion of studies during full text critical appraisal were recorded and reported. Discrepancies between reviewers during screening at each stage were resolved through discussion, otherwise with a third reviewer (AAA)22.
Inclusion criteria
All observational studies conducted in SSA, which reported bacterial profile and/or antimicrobial resistance patterns of infected diabetic foot ulcers and published in the English language were included.
Exclusion criteria
We excluded studies that were conducted outside SSA. Reviews, commentary, and letters to editors were also excluded. Studies that used invalid laboratory diagnostic tests and those without clear results were excluded.
Data extraction
Data were extracted onto an Excel spreadsheet. A data extraction tool was prepared that included authors, publication year, country, healthcare setup, clinical site (ward name/clinical service area), clinical condition (disease), sample size, study design, study period, clinical sample type, bacteria identification method used, antibiotics resistance test method, standard breakpoint reference used, sex of study participants, the mean age of study participants, types and the number of bacteria isolates, and antibiotics resistance pattern. Data extraction was conducted by (FWW and MTB), and cross-checked by (AAA). In addition, there were two rounds of meetings for further data cross-checking and validation.
Data quality and risk of bias assessment
(MTB and FW) assessed the methodological quality of eligible studies using the Joanna Briggs Institute's critical appraisal instrument for prevalence studies. The results of the critical appraisal were reported in narrative form and a table. A lower risk of bias (94%) was observed after the assessment (Table 1). Articles were reviewed using titles, abstracts, and full text screening23.
Data analysis
Data synthesis and statistical analyses were conducted using STATA version 17 software (STATA Corp., College Station, TX). The random-effect model of analysis was adopted as a method of meta-analysis because it reduced the heterogeneity of included studies. A meta-analysis of observational studies using the random-effect model of analysis was carried out. The heterogeneity was assessed using Cochrane chi-square (I2) statistics, while the Egger intercept was used to assess publication bias. The P value of < 0.05 for I2 statistics was used to determine the presence of heterogeneity. The findings were reported using the pooled prevalence with a 95% confidence interval (CI) and forest plot.
In line with the author's interpretation, definitions of the terms antibiotic resistance, intermediate, and susceptible were directly taken from each study. We computed the pooled prevalence of antibiotic resistance by taking absolute numbers reported by each study.
Results
Study selection
Systematic searching yielded 735 articles, from which 227 articles were removed due to duplication. Articles removed were (n = 508) during the title and (n = 429) abstract screening. Full-text screening involved 79, out of 68 were excluded. Only 11 articles that fulfilled the inclusion criteria were included in this systematic review and meta-analysis (Fig. 1).
Characteristics of articles included in the meta-analysis
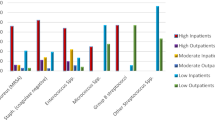
All the included studies were published between 2006 and 2022, out of which 4 were reported from Nigeria, 2 articles from Ethiopia, and 2 articles from Cameroon (Table 2). All studies collected swabs or biopsy samples from DFU patients to identify bacteria. Most of the included studies used a cross-sectional study design. The majority of the included studies utilized the disc diffusion method to perform antibiotic sensitivity tests, with Clinical & Laboratory Standards Institute (CLSI) guidelines serving as the standard breakpoint reference.
Characteristics of the study population
Both type 1 and type 2 diabetic patients were included as the study participants. A total of 1701 bacteria were isolated from 1174 diabetic patients (Table 3). Most of the studies reported the sex of their study participants, of which 674 study participants were males and 334 were females. The mean ages of the study participants range from 54 to 62.5 years.
Meta-analysis for the prevalence of bacteria isolates from DFU, sub-Saharan Africa
A total of 36 bacteria species were associated with DFU in sub-Saharan Africa (Supplementary Table 1). The most prevalent gram positive bacteria was S. aureus (Table 4), with a pooled prevalence of 34.34% [95% CI (25.73–42.85)] (Fig. 2). The most prevalent gram negative bacteria were E. coli and P. aeruginosa with a pooled prevalence of 21.16% [95% CI (14.60–28.52)] and 20.98% [95% CI (12.31–31.14)] respectively (Figs. 3 and 4).
The pooled effect size of antibiotic resistance patterns
Among S. aureus isolates, the highest pooled resistance rate was toward Gentamycin (57.96%, 95% CI [40.32–74.69]), followed by Ciprofloxacin (52.45%, 95% CI [25.42–78.85]) (Table 5). Among gram negative bacteria E.coli and K. Pneumoniae were 72.42%, 95% CI [49.54–90.82] and 62.67%, 95% CI [34.32–87.41] resistance to Amoxicillin, respectively (Table 6). These bacteria also showed a higher resistance rate for Ampicillin and Ceftriaxone. E. coli showed the lowest resistance rate against Meropenem, with 3.06%, 95% CI [15.22–43.38].
Carbapenem resistance pattern of bacterial isolates
Carbapenem-resistant bacteria are public health threats that require urgent and aggressive action. In supplementary table 2 we reported Carbapenem resistance pattern of bacterial isolates from DFU patients in sub-Saharan Africa. Some of the concerning results were reported from Congo with P. aeruginosa [10 (90.9%)] and E. coli [2 (100.0%)] resistance rates towards Imipenem32. Other alarming results were reported from Sudan and Ethiopia with K. pneumonia 7(33.3%) and 5(27.8%) resistance rate towards Meropenem, respectively29,31.
Discussion
To the best of our knowledge, this is the first comprehensive review and meta-analysis conducted in sub-Saharan Africa that assesses bacterial profile and AMR patterns of DFU cases in the region. A total of 1701 bacteria were isolated from 1174 diabetic patients with DFU; the number of isolated bacteria was found very high indicating the likelihood of poly-microbial infections. S. aureus was found to be the most prevalent isolate obtained from DFU, followed by E. coli and P. aeruginosa in descending order of frequency. A previous worldwide meta-analysis reported diverse bacteria from diabetic foot infections, and the organism most commonly identified was S. aureus with a pooled prevalence estimate of 18.0% [95% CI (13.8–22.6)]34. A comparable composition of bacteria was also reported from the meta-analysis of general wound infection, where S. aureus was the most common bacterial isolate with a pooled prevalence of 36% [95% CI (29–42)] followed by E. coli isolates with 13% [95% CI (10–16)], P. aeruginosa (9% [95% CI (6–12)]), K. pneumonia (9% (95% CI (6–11)]) and P. mirabilis (8% [95% CI (5–11)])35.
In this meta-analysis, the pooled resistance rate of S. aureus towards Gentamicin and Ciprofloxacin was identified as the highest.
Compared to a study conducted in Ethiopia on general wound infections, which reported gentamicin (13% [95% CI (8–18)]) and ciprofloxacin (12% [95% CI (8–16)]) resistance rate, our results showed considerably higher differences in resistance to those antibiotics35. This could indicate different levels of antibiotic use or other factors that contribute to the development of antibiotic resistance in these study populations. Among gram negative bacteria E.coli showed more than 50% resistance rate for all antibiotics tested except for Meropenem. K. Pneumoniae also showed more than a 50% resistance rate for towards most of the antibiotics tested.
In February 2017, the WHO released a list of pathogens based on the growing dangers posed by antibiotic resistance that includes the pathogens designated by the acronym ESKAPE (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species) which were given the highest “priority status” since they represent the great threat to humans36. Our review also showed that these ESKAPE pathogens have a significant contribution to antibiotic resistance DFU cases in sub-Saharan Africa. In the WHO European region as well as around the globe, these pathogens were responsible for hundreds of thousands of deaths associated with antibiotic resistance37,38.
Infection of DFU with Klebsiella pneumonia, Acinetobacter species or Enterobacteriaceae may require treatment with last-resort antibiotics, such as carbapenems39,40. However, in our review, those pathogens showed some level of resistance to carbapenems. Therefore, these pathogens are a great threat to diabetic patients in sub-Saharan Africa as well as they are public health threats for the general population that require urgent and aggressive action.
One limitation of this meta-analysis is that it primarily focused on aerobic bacteria isolates. It is worth noting that anaerobes often play a significant role in deep tissue infections, particularly in areas with compromised vascularization due to diabetes-related microangiopathy and subsequent low oxygen tension. Additionally, it should be mentioned that most of the included studies did not report multidrug resistance patterns. Consequently, we were unable to provide an analysis of the multidrug resistance patterns exhibited by bacteria isolates of DFU.
Conclusion
Both gram-positive and gram-negative bacteria were associated with DFU in SSA. Clinicians should be aware of bacterial resistance patterns before prescribing empirical antibiotic regimens for DFUs cases in SSA. Our findings are important for planning treatment with the appropriate antibiotics in the region. The high AMR prevalence of E.coli and K. Pneumoniae towards most of the antibiotics tested indicates the need for context-specific effective strategies aimed at practicing good hygiene and infection control measures that can help to prevent the spread of antibiotic-resistant bacteria and evidence-based alternative treatment options.
Implication for policy and practice
Antimicrobial resistance patterns of bacteria isolated from infected diabetic foot ulcers were higher in sub-Saharan Africa. There needs to be increased focus and investment in improving the management of diabetic foot ulcers in sub-Saharan Africa. This may include the development of new treatment protocols and the provision of better resources for healthcare providers, as well as increased education and awareness for diabetic patients themselves. Additionally, there may be a need for increased research on antimicrobial resistance patterns in the region in order to inform future policy decisions related to public health and infection control. Health systems in sub-Saharan Africa must implement real-time laboratory surveillance for the identification of pathogens to determine their antimicrobial resistance profile. Countries in sub-Saharan Africa must establish a common data-sharing platform that could inform evidence regarding the antimicrobial resistance profile of ESKAPE pathogens.
Data availability
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AMR:
-
Antimicrobial resistance
- AHRI:
-
The Armauer hansen research institute
- DFU:
-
Diabetic foot ulcer
- JBI:
-
The Joanna Briggs institute
- LMICs:
-
Low- and middle-income countries
- MDR:
-
Multi-drug resistance
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- PROSPERO:
-
International prospective registry of systematic reviews
- SDG:
-
Sustainable development goal
- SSA:
-
Sub-Saharan Africa
- WHO:
-
The world health organization
References
Armstrong, D. G., Boulton, A. J. & Bus, S. A. Diabetic foot ulcers and their recurrence. N. Engl. J. Med. 376, 2367–2375 (2017).
Atlas, D. International diabetes federation. In IDF Diabetes Atlas, 7th edn. Brussels, Belgium: International Diabetes Federation 33, 2 (2015).
Zhang, P. et al. Global epidemiology of diabetic foot ulceration: A systematic review and meta-analysis. Ann. Med. 49, 106–116 (2017).
Ugwu, E. et al. Burden of diabetic foot ulcer in Nigeria: Current evidence from the multicenter evaluation of diabetic foot ulcer in Nigeria. World J. Diabetes 10, 200 (2019).
Abbas, Z. G. The Diabetic Foot Worldwide: sub‐Saharan Africa. The foot in diabetes, 51–60 (2020).
Jodheea-Jutton, A., Hindocha, S. & Bhaw-Luximon, A. Health economics of diabetic foot ulcer and recent trends to accelerate treatment. Foot 52, 101909 (2022).
Sadeghpour Heravi, F., Zakrzewski, M., Vickery, K., Armstrong, D. G. & Hu, H. Bacterial diversity of diabetic foot ulcers: Current status and future prospectives. J. Clin. Med. 8, 1935 (2019).
Percival, S. L., Malone, M., Mayer, D., Salisbury, A. M. & Schultz, G. Role of anaerobes in polymicrobial communities and biofilms complicating diabetic foot ulcers. Int. Wound J. 15, 776–782 (2018).
Kandemir, Ö., Akbay, E., Şahin, E., Milcan, A. & Gen, R. Risk factors for infection of the diabetic foot with multi-antibiotic resistant microorganisms. J. Infect. 54, 439–445 (2007).
Sekhar, S. M., Vyas, N., Unnikrishnan, M., Rodrigues, G. & Mukhopadhyay, C. Antimicrobial susceptibility pattern in diabetic foot ulcer: A pilot study. Ann. Med. Health Sci. Res. 4, 742–745 (2014).
Jain, S. K. & Barman, R. Bacteriological profile of diabetic foot ulcer with special reference to drug-resistant strains in a tertiary care center in North-East India. Indian J. Endocrinol. Metab. 21, 688 (2017).
Zubair, M. Prevalence and interrelationships of foot ulcer, risk-factors and antibiotic resistance in foot ulcers in diabetic populations: A systematic review and meta-analysis. World J. Diabetes 11, 78 (2020).
O'Neill, J. Tackling drug-resistant infections globally: Final report and recommendations. (2016).
Jouhar, L. et al. Microbiological profile and antimicrobial resistance among diabetic foot infections in Lebanon. Int. Wound J. 17, 1764–1773 (2020).
Mutonga, D. M., Mureithi, M. W., Ngugi, N. N. & Otieno, F. C. Bacterial isolation and antibiotic susceptibility from diabetic foot ulcers in Kenya using microbiological tests and comparison with RT-PCR in detection of S. aureus and MRSA. BMC Res. Notes 12, 1–6 (2019).
Appapalam, S. T., Paul, B., Arockiasamy, S. & Panchamoorthy, R. Phytofabricated silver nanoparticles: Discovery of antibacterial targets against diabetic foot ulcer derived resistant bacterial isolates. Mater. Sci. Eng. C 117, 111256 (2020).
Najari, H. R., Karimian, T., Parsa, H., QasemiBarqi, R. & Allami, A. Bacteriology of moderate-to-severe diabetic foot infections in two tertiary hospitals of Iran. Foot 40, 54–58 (2019).
Dai, J., Jiang, C., Chen, H. & Chai, Y. Assessment of the risk factors of multidrug-resistant organism infection in adults with type 1 or type 2 diabetes and diabetic foot ulcer. Can. J. Diabetes 44, 342–349 (2020).
Akililu Alemu Ashuro, M. T. B., Getachew Tesfaye Beyene. In Prospero (2023).
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., PRISMA Group*, t. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 151, 264–269 (2009).
Duberman, J. A. & Sieving, P. C. Information resources for the clinical researcher. In Principles and Practice of Clinical Research 713–751. https://www.sciencedirect.com/science/article/abs/pii/B9780128499054000423 (Elsevier, 2018).
Waffenschmidt, S., Knelangen, M., Sieben, W., Bühn, S. & Pieper, D. Single screening versus conventional double screening for study selection in systematic reviews: A methodological systematic review. BMC Med. Res. Methodol. 19, 1–9 (2019).
Moola, S. et al. Conducting systematic reviews of association (etiology): The Joanna Briggs Institute’s approach. JBI Evidence Implement. 13, 163–169 (2015).
Yongabi, K. A., Novaković, M., Bukvički, D., Reeb, C. & Asakawa, Y. Management of diabetic bacterial foot infections with organic extracts of liverwort Marchantia debilis from Cameroon. Natural Product Commun. https://doi.org/10.1177/1934578X1601100938 (2016).
Yefou, M. D. et al. Bacterial profile of diabetic foot infections and antibiotic susceptibility in a specialized diabetes centre in Cameroon. Pan Afr. Med. J. https://doi.org/10.11604/pamj.2022.42.52.31042 (2022).
Woldeteklie, A. A., Kebede, H. B., Abdela, A. A. & Woldeamanuel, Y. Prevalence of extended-spectrum β-lactamase and carbapenemase producers of gram-negative bacteria, and methicillin-resistant Staphylococcus aureus in isolates from diabetic foot ulcer patients in Ethiopia. Infect. Drug Resist. 15, 4435–4441 (2022).
Usman, Y. et al. Phenotypic profile and antibiogram of biofilm-producing bacteria isolates from diabetic foot ulcers in Zaria, Nigeria. Nigerian Postgrad. Med. J. 28, 233 (2021).
Ogba, O. M., Nsan, E. & Eyam, E. S. Aerobic bacteria associated with diabetic foot ulcers and their susceptibility pattern. Biomed. Dermatol. 3, 1–6 (2019).
Hamid, M. H., Arbab, A. H. & Yousef, B. A. Bacteriological profile and antibiotic susceptibility of diabetic Foot infections at Ribat University hospital; a retrospective study from Sudan. J. Diabetes Metab. Disord. 19, 1397–1406 (2020).
Ako-Nai, A. et al. Characterization of bacterial isolates from diabetic foot infections in Ile-Ife, Southwestern Nigeria. Foot 16, 158–164 (2006).
Berhanu, B. Bacterial Profile and Antimicrobial Susceptibility Pattern of Isolates from Diabetic Foot Infections at Selected Public Hospitals of Addis Ababa, Ethiopia., http://etd.aau.edu.et/handle/123456789/29008 (2021).
Iyamba, J.-M.L. et al. Study of biofilm formation and antibiotic resistance pattern of bacteria isolated from diabetic foot ulcers in Hôpital de Référence Saint Joseph, Kinshasa, democratic Republic of Congo. Adv. Microbiol. 11, 283–295 (2021).
Adeyemo, A. T., Kolawole, B., Rotimi, V. O. & Aboderin, A. O. Multicentre study of the burden of multidrug-resistant bacteria in the aetiology of infected diabetic foot ulcers. Afr. J. Lab. Med. 10, 1–10 (2021).
Macdonald, K. E., Boeckh, S., Stacey, H. J. & Jones, J. D. The microbiology of diabetic foot infections: A meta-analysis. BMC Infect. Dis. 21, 1–10 (2021).
Sisay, M., Worku, T. & Edessa, D. Microbial epidemiology and antimicrobial resistance patterns of wound infection in Ethiopia: A meta-analysis of laboratory-based cross-sectional studies. BMC Pharmacol. Toxicol. 20, 1–19 (2019).
Mancuso, G., Midiri, A., Gerace, E. & Biondo, C. Bacterial antibiotic resistance: The most critical pathogens. Pathogens 10, 1310 (2021).
Murray, C. J. et al. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. The Lancet 399, 629–655 (2022).
Mestrovic, T. et al. The burden of bacterial antimicrobial resistance in the WHO European region in 2019: A cross-country systematic analysis. The Lancet Public Health 7, e897–e913 (2022).
Kadri, S. S. Key takeaways from the US CDC’s 2019 antibiotic resistance threats report for frontline providers. Crit. Care Med. 48, 939–945 (2020).
Laxminarayan, R. et al. The Lancet Infectious Diseases Commission on antimicrobial resistance: 6 years later. Lancet. Infect. Dis. 20, e51–e60 (2020).
Acknowledgements
The Joanna Briggs Institute (JBI) and the Ethiopian Evidence-Based Health Care Center (EEHCC), for providing the platform and the opportunity to attend the comprehensive systematic review training. The Armauer Hansen Research Institute (AHRI) for enabling us and creating access to the databases.
Author information
Authors and Affiliations
Contributions
F.W., M.T.B., and A.A.A. were involved in a principal role in the conception of ideas, developing methodologies, and writing the article. M.F., E.D. and S.K. were involved in the data extraction. F.W. and M.T.B. have conducted the analysis, while L.W., G.K.K., Z.E.K. and M.B. participated in the interpretation and proofreading. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wada, F.W., Mekonnen, M.F., Sawiso, E.D. et al. Bacterial profile and antimicrobial resistance patterns of infected diabetic foot ulcers in sub-Saharan Africa: a systematic review and meta-analysis. Sci Rep 13, 14655 (2023). https://doi.org/10.1038/s41598-023-41882-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-41882-z
- Springer Nature Limited
This article is cited by
-
Update on prevalence and antimicrobial resistance of Staphylococcus aureus and Pseudomonas aeruginosa isolated from diabetic foot ulcers in Africa: a systematic review and meta-analysis
Bulletin of the National Research Centre (2023)