Abstract
Maternal health is a global public health concern. The paucity of antenatal care (ANC) during pregnancy is directly associated with maternal mortality. This study assessed the individual and community-level determinants of quality ANC in six South-Asian countries. Data were obtained from a Demographic health survey of six South-Asian countries. This study included a sample of 180,567 (weighted) women aged 15–49 who had given birth in the preceding three years prior to the survey. The quality of ANC was determined by assessing whether a woman had received blood pressure monitoring, urine and blood sample screening, and iron supplements at any ANC visits. Frequency, percentage distribution, and inferential analysis (multilevel mixed-effects model) were conducted. The proportion of quality antenatal care utilization in South Asia was 66.9%. The multilevel analysis showed that women aged 35–49 years (AOR = 1.16; 95% CI = 1.09–1.24), higher education (AOR = 2.84; 95% CI = 2.69–2.99), middle wealth status (AOR = 1.55; 95% CI = 1.49–1.62), richest wealth status (AOR = 3.21; 95% CI = 3.04–3.39), unwanted pregnancy (AOR = 0.92; 95% CI = 0.89–0.95) and 2–4 birth order (AOR = 0.86; 95% CI = 0.83–0.89) were among the individual-level factors that were significantly associated with quality ANC utilization. In addition, rural residence (AOR = 0.77; 95% CI = 0.74–0.8), and big problem – distance to health facility (AOR = 0.63; 95% CI: 0.53–0.76) were the among community level factors there were also significantly associated with use of quality ANC. Meanwhile, women who lived in India (AOR: 22.57; 95% CI: 20.32–25.08) and Maldives (AOR: 33.33; 95% CI: 31.06–35.76) had higher odds of quality ANC than those lived in Afghanistan. Educational status, wealth status, pregnancy wantedness, sex of household head, birth order, place of residence, and distance to health facility were associated with quality ANC. Improving educational status, improving wealth status, reducing the distance to health facilities, and providing rural area-friendly interventions are important to increase the quality of ANC in South Asia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Mitigating maternal mortality and pregnancy-related morbidities remains paramount at the global health level. Globally, maternal mortality rate is far below the targets set by the Sustainable Development Goals (SDGs) target 3.1, which calls for reducing maternal mortality to less than 70 deaths per 100,000 live births1. The World Health Organisation reports that nearly 810 women die each day from maternal-related factors2. Sub-Saharan Africa and South Asia account for 85% of the global burden of maternal mortality1. Specifically, the maternal mortality rate in South Asia stands at 163 per 100,000 live births3. This is twice the acceptable threshold stipulated by SDG target 3.1. Thus, underscoring the need for pragmatic efforts to help South Asian countries attain the SDG target.
Most pregnancy complications (i.e., sepsis, eclampsia, embolism, haemorrhage, etc.) are preventable through proper healthcare utilisation throughout the continuum of pregnancy4. This means that antenatal care (ANC) services play a critical role in determining the survivorship of mothers. Quality ANC is necessary to ensure a positive birth experience. A study conducted in Ghana has found that women who did not receive quality ANC were more likely to have adverse pregnancy outcomes including anaemia, preeclampsia, and having a child with low birth weight5. Although there is no consensus on the measures for quality ANC, different studies6,7 have used different approaches to conceptualise quality ANC. For instance, a study in Nepal operationalised quality ANC by the number of visits, timing of initiation of care, and inclusion of all recommended components of care6. Another study in Nigeria also defined quality ANC as receiving all recommended and recognised components of ANC, namely: “receiving of iron supplements, intestinal parasite drugs (IPD), at least two doses of Tetanus Toxoid injections, malaria intermittent preventive treatment in pregnancy (IPTp) and health education on danger signs and complications during pregnancy, blood pressure measurement, urine tests, blood tests, health talk on prevention of mother to child transmission (PMTCT) of HIV/AIDS and HIV/AIDS counselling, testing and collection of results”7.
Quality ANC enhances maternal health and reduces the risk of anaemia, pregnancy-induced hypertension, and premature labour6,8,9. Previous studies from Bangladesh10, Nepal6, and Nigeria7 have found that quality ANC was determined by multiple individual and household factors, including urban residency, receiving skilled birth attendance, higher maternal educational attainment, autonomous decision-making, higher household economic status, early initiation of ANC, higher parity and older age.
In a previous study involving five Southeast Asian countries11, it was revealed that Cambodia and Timor-Leste had higher proportions of women who had less than four ANC (20.3% and 36.2%, respectively) compared to Indonesia, Myanmar, and the Philippines (ranging from 8.3 to 12.2%). However, in terms of timing of first ANC, Myanmar had a higher percentage of women who initiated ANC late (at four months of gestation or more) compared to the other countries (ranging from 16.2 to 34.8%). Similarly, a study conducted in Bangladesh has shown that only 18% of mothers had received all components of quality ANC10.
Due to this heterogeneous nature of quality ANC indicators in previous studies6,7,8,9,10, there is a limitation in providing a comprehensive picture of the determinants of quality ANC in the South Asian Region. However, understanding the determinants of quality ANC at this regional level is likely to help experts and regional organizations that co-ordinate health-related activities and policies in South-Asia, such as UNICEF South Asia, to identify common challenges of quality ANC that are faced by South-Asian countries and to develop collective solutions that would benefit the South-Asian region. It is against this literature gap and relevance to policy that we conducted this study. Our findings are likely to contribute towards narrowing this gap in the literature by examining the determinants of quality ANC among South Asian countries using nationally representative data.
Methods
Study setting and design
There are five regions in Asia. Among the five regions, South Asia is the home of 1.857 billion people. The region includes eight countries (Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan and Sri Lanka). Out of these countries, we considered only those that had the Demographic and Health Survey (DHS) data. Using this as the inclusion criteria, two countries (Bhutan and Sri Lanka were excluded. Bhutan had no DHS data and Sri Lanka has no DHS data available since 1987. Therefore, the final analysis was based on data from six nations, including Afghanistan, Bangladesh, India, Maldives, Nepal, and Pakistan. The DHS surveys adopted a cross-sectional study design. Details of the survey methods have been described elsewhere12,13,14,15,16.
Data source, extraction and sampling strategy
The datasets were obtained from the DHS official database after getting approval through an application that explained the purpose of our research. Afghanistan DHS 2015, Bangladesh DHS 2017–2018, India National Family and Health Survey 2015–2016, Maldives DHS 2016–2017, Nepal DHS 2016, and Pakistan DHS 2017–2018 datasets were analysed in this study. The individual recode (IR) files were used for the analysis. DHS provides data on the nationally-representative population, health, and nutrition indicator. Using multistage stratified random sampling, women aged 15–49 were selected for face-to-face interviews. Details of sampling methods have been described elsewhere12,13,14,15,16.
Population and eligibility criteria
Women aged 15–49 who had given birth in the preceding three years of prior to the surveys in the selected countries were the study population. Pregnant women who had not received ANC visits were excluded from the study. A total of 180,567 pregnant women who received at least one ANC visit and provided complete information on quality of care were included in this study. Additionally, the analysis was limited to women’s most recent birth in order to reduce recall bias.
Quality of ANC
Potential indicators of Quality Antenatal care, according to the WHO recommendations17 on ANC for a positive pregnancy experience involves comprehensive patient assessments such as medical history taking, clinical assessment, and laboratory screenings (e.g., full blood count testing and urine culture); appropriate preventive and curative treatments (e.g., immunizations and nutritional supplementation); and patient counselling and education (e.g., on healthy behaviours and lifestyle as well as sign and symptoms of complication)18. Despite the existence of WHO ANC model which serves as international guideline, many countries have different recommendations on number, frequency and content of consultation. In fact, Lina Sofia et al. in 2018 found that among the studies on quality ANC, 72.5% studies have assessed quality of ANC based on national standards and recommendations, and the use of different country-specific indicators and standards for assessing quality ANC has resulted in limited international monitoring and comparability19.
Quality ANC related indicators which exist in the DHS data also vary across countries. Even though there are thirteen indicators in DHS data which are related to quality ANC, only three indicators are ubiquitously present for all countries18. Notably, four indicators were measured for all six countries. These included blood pressure monitoring, urine and blood samples taken, and iron supplements. In order to obtain a comparable measure of quality ANC across South-Asia, the estimate of quality ANC was limited to these four indicators. Therefore, women who reported having blood pressure measured, urine and blood sample taken for laboratory screenings, and iron supplement provided at any of the ANC visits are considered as recipient of quality ANC. In spite of providing a limited view of antenatal care quality, these four indicators are crucial for screening and avoiding of several pregnancy complications.
Independent variables
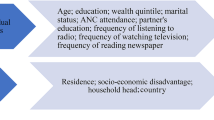
The independent variables for this study were selected based on previous studies6,20,21,22,23,24,25,26,27,28. The literature review included studies on factors influencing ANC worldwide and in selected countries. The independent variables were categorized into two categories: individual level and community level. Selected individual-level variables were age, women's education level, wealth status, problems of getting money for treatment, pregnancy wantedness, sex of household head, and birth order. " Since the fertility rate per woman in South Asian countries varies between 1.81 (Maldives) to 4.18 (Afghanistan)29, the birth order was recorded as "1," "2–4," and "≥5". Place of residence, distance to health facilities, and country were the community-level variables.
Data processing and analysis
We used the women individual level weight for each country to calculate summary statistics. Then the data was pooled from seven countries altogether. The weight of pooled data was rescaled in such a way that each country had an equal weight, ensuring that all countries were given equal importance. The weighted pooled data was used to fit multilevel mixed-effect binary logistic regression models. We chose multilevel mixed-effect model due to the hierarchical nature of the DHS data, where socio-demographic and clinical characteristics are nested under the clusters. In this study, four models were fitted. The first one, the null model, contained no covariates, the second one contained only the individual-level factors, while the third model contained only community-level variables. Finally, Model three contained all community and individual-level factors. The Akaike information criteria (AIC) and Bayesian information criteria (BIC) were used to compare the models. Frequency and percentage were carried out using SPSS, while the multilevel mixed model was performed using R.
Ethical consideration
The Ethics Committee of ORC Macro Inc., as well as the Ethics Boards of partner organisations in all the countries, such as the Ministries of Health, provided ethical approval. The DHS adheres to the rules for protecting respondents' privacy. Inner City Fund International assures that the survey conforms to the Human Subjects Protection Act of the United States Department of Health and Human Services. Respondents who participated in the DHS provided both verbal and written informed consent. However, because this was a secondary data analysis, permission was obtained to use the datasets for this study. More information about DHS data utilisation and ethical requirements may be found at http://goo.gl/ny8T6X.
Results
Socio-demographic and economic characteristics
This study comprised 180,567 ANC attendants from six countries in South Asia- Afghanistan, Bangladesh, India, Maldives, Nepal and Pakistan (Table 1). A major portion (86.3%) of the women fell in the 20–34 year age group, while almost one-tenth (9.7%) of sample were 35–49 years old. Approximately two-thirds (67.5%) of all respondents were from rural areas. Roughly one quarter (26.2%) of the respondents had no education, while 13.7%, 46.9%, and 13.2% had primary, secondary and higher education, respectively. Wealth index of the ANC attendants were evenly distributed among the following categories: poorest (18.3%), poorer (20.5%), middle (21.0%), richer (21.0%), and richest (19.2%). India had the highest contribution to the sample of this study with 84.3% of the ANC participants, while the least contribution was from the Maldives with 1.3%. The results further indicated that getting money for treatment was big problem for 28.3% of women, not a big problem for 34.0% of women, and no problem for 37.7% of women. A significant majority (88.4%) of the women were from male head family, whereas only 11.7% were from female-headed households.
Maternal characteristics and magnitude of quality of ANC
Among all study respondents, slightly more than one-third (34.7%) of them were pregnant for the first time. The results showed that 59.4% of the study women received at least 4 ANC. The results further indicated that during the ANC visits, 89.0%, 83.7%, 82.1% and 81.7% respectively of women’s blood pressure was measured, a urine sample taken, a blood sample taken and given/bought iron supplements (Table 2). Notably, only 66.6% of the women had a quality of ANC during the ANC visit.
Among the age groups, 20–34-year-old women received the most (68.2%) of quality ANC. Among the countries, women in India received the most quality ANC, while the percentage was low (14.5%) among women from Afghanistan (Fig. 1). Women with higher education received the most (85.0%) of quality ANC. Similarly, 79.9% of women from the wealthiest family received quality ANC. Figure 2 shows the variation in the percentage of quality ANC by socio-economic characteristics.
Determinants of quality ANC
The community variance 0.467 (Table 3) in the null model demonstrates that there was significant community variation in the utilization of quality of ANC. Furthermore, the intra-cluster correlation coefficient (ICC) in the null model also revealed that 12.3% of the total variability in quality ANC was attributable to variations between different communities. The community variance was reduced to 0.175 in the model-3 which was adjusted for both individual- and community-level factors. The model-3 suggested that only 3.5% of total variation in quality ANC utilisation was contributed by community-level variables. Additionally, the AIC and BIC was least for model-3 among the fitted models. Hence, the interpretation of the individual and community fixed effect results was based on model-3 as the model with smaller AIC and BIC was the best fit in terms of fixed effects. The full model (model-3) illustrated that respondents’ age group, level of education, wealth status, pregnancy wantedness, sex of household head, birth order, problems with money for treatment, place of residence, distance to health facilities and country were significantly associated with quality ANC at 5% level of significance.
Women aged 35–49 years were 16% more likely to get quality ANC than those aged between 15–19 years. As the women's education level increases, the odds of getting quality ANC also increased. Highly educated mothers were 2.84 times more likely to get quality ANC than non-educated women. Women from the richest household were 3.21 times more likely to get quality ANC than the women from the poorest households. Women who did not want the pregnancy at the time of the survey were 18% less likely to get quality ANC. Women from female-headed households were 5% less likely to get quality ANC than those from male-headed households. Pregnant women with their second to the fourth baby were 24% less likely, while women with fifth or more were 29% less likely to get quality ANC than those with one child. Women who had a big problem with money were less likely to get quality ANC compared to those who considered money as a not a big problem. Compared to women living in urban areas, those residing in rural areas had 23% lower odds of getting quality ANC (AOR: 0.77; 95% CI: 0.74–0.88). Women who faced a more significant problem (AOR: 0.63; 95% CI: 0.54–0.77) with distance to health facilities were 27% less likely to get quality ANC than those who did not have such problems. Women living in the following South Asian countries were more likely to have quality ANC, Bangladesh (AOR: 4.05; 95% CI: 3.83–4.28), India (AOR: 22.57; 95% CI: 20.32–25.08), Maldives (AOR: 33.33; 95% CI: 31.06–35.76), Nepal (AOR: 5.57; 95% CI: 5.26–5.9), and Pakistan (AOR: 3.19; 95% CI: 3.02–3.37), than women living in Afghanistan.
Discussion
Recognising the critical role of quality ANC in mitigating maternal and child health adverse effects, we examined the determinants of quality ANC in six South Asian countries. The study shows that approximately two-third women in the six countries included in this study (66.9%) received quality of ANC. This prevalence is higher than that reported in Nepal6 and Nigeria7. In Nepal, Joshi et al.6 found that only 24% of women received good quality ANC, whereas, in Nigeria, Fagbamigbe and Idemudia7 reported that less than 5% of ANC users received quality ANC services. This study's identified determinants of quality ANC explain the moderately high-quality ANC among women in the six Asian countries.
Our findings revealed that education was a significant determinant of quality ANC. Highly educated mothers were 2.84 times more likely to get quality ANC than non-educated women. Similar findings have been reported in previous related studies7,8. The significant association between maternal level of education and quality ANC can be explained from the perspective that a higher level of education often translates into empowerment for women30. As such, these women are able to make critical decisions about their healthcare, including decisions about receiving all components of quality ANC. Another plausible explanation for these findings could be that women with higher formal education better appreciate the importance of receiving quality ANC and understand the dangers of not receiving the full complement of quality ANC.
Wealth status emerged as a significant determinant of quality ANC. The regression analysis indicates a positive association between wealth status and quality ANC. This implies that women from the wealthiest household are 3.21 times more likely to get quality ANC than the women from the poorest household. The result corroborates evidence from Nepal6, Nigeria7, and Ethiopia31. A plausible explanation for this could be that women from high wealth indexed households are more likely to initiate ANC early32; hence, they are exposed to a lot of health informational messages concerning the content of ANC, the benefits of receiving quality ANC, as well as the possible maternal health complications that can arise as a result of not receiving the full pack of quality ANC. As such, women of higher wealth know what services are needed and ask for these services33. Moreover, women of higher wealth status can easily afford the direct and indirect financial costs of seeking quality ANC services compared to their lower-income counterparts. It is also possible that wealthier women are likely to reside in areas that have better resourced healthcare facilities, thereby increasing their chances of having access to higher quality healthcare service providers. This finding is further corroborated by another result from our regression analysis which showed that women who had a big problem with money were less likely to get quality ANC.
Consistent with the findings of previous studies conducted in Nepal6, Nigeria7, and Ghana33, our study showed that across the six Asian countries included in the study, urban residency was associated with a high likelihood of receiving quality ANC. In contrast, rural residency was associated with lower odds of receiving quality ANC. We postulate that this rural–urban disparity in determining the quality of ANC services could be due to the low presence of healthcare facilities and skilled health professionals in rural areas vis-à-vis the urban areas33. Consequently, women in rural areas have to spend much money on transportation in order to get to the nearest healthcare facility where they can receive quality ANC6. This finding is further corroborated by another result from our regression analysis which showed that women who face a more significant problem with distance to health facilities were less likely to get quality ANC.
Concerning age, our findings reveal that women aged 20–34 years were 5% more likely to receive quality ANC than adolescents (i.e., those aged 15–19 years). A related study by Muchie31 supports our result. Unlike adults, adolescents are key vulnerable populations who are stigmatised in the events of pregnancy34,35,36. These social labels and the stigma perpetuated against adolescents who get pregnant significantly reduce their willingness to receive ANC services. In situations where they are bold to seek ANC services from healthcare facilities, they are subjected to disrespectful care37. Hence, it affects their likelihood of receiving quality ANC. Also, women aged 20–34 may be aware of the various services they must receive during ANC sessions. Therefore, they can request it.
We found that women who had unwanted pregnancies were 8% less likely to get quality ANC. The reasons for the association between pregnancy intentions and quality ANC are unclear. However, one school of thought is that women who experience unwanted pregnancies are likely to terminate the pregnancy38,39. Hence, there is no room for them to seek quality ANC services. Another perspective to this finding could be that unintended pregnancies imply that women were not psychologically, socially, physically and economically ready for a child. Hence, they may not attend ANC sessions as recommended, resulting in a lower likelihood of receiving quality ANC services.
Our study revealed that women with birth orders 2–4 were 14% less likely, while women with 5 or more were 29% less likely to get quality ANC. This means that as birth order increases, the likelihood of receiving quality ANC reduces. The result aligns with the findings of Muchie31. A plausible explanation for this result could be attributed to the fact that, as women progress through birth order, they may become overly confident and forget about the importance of receiving all components of quality ANC service. It is also possible that healthcare providers downplay the necessity to conduct a comprehensive diagnostic test to women of higher birth order thereby reducing ANC quality among this cohort. Finally, we observed from the regression analysis that women from female-headed households were 5% more likely to get quality ANC than their counterparts. We are uncertain about the reasons for this association. However, we postulate that this may be due to the level of empowerment among women in female-headed households.
Policy implications
The findings of this study underscore a need to improve quality ANC at the primary healthcare level in South Asia. Practically, this can be achieved by strengthening healthcare infrastructure. Given our findings that problem with distance reduces ANC quality, it is imperative for South Asian countries to ensure that all healthcare infrastructures established to improve ANC and maternal healthcare would be brought closer to the end users (i.e., pregnant women). This includes ensuring the availability of essential equipment, supplies, and medications necessary for providing comprehensive ANC particularly in remote areas of South Asian countries. The findings that women of higher wealth status have higher odds of receiving quality ANC highlights the need to invest substantially in women's economic development. This could be achieved by implementing women empowerment programmes and interventions such as livelihood skills activities. Overall, improving the quality of antenatal care contribute has significant implications for ensuring continuity of care, promoting birth preparedness, and a reduction in maternal and neonatal mortalities in South Asian countries.
Strengths and limitations
This study used nationally representative data with a large sample size. As such, we can generalise our findings on the determinants of the quality of ANC services to all six countries included in the study. Nevertheless, some limitations must be considered when interpreting our results. First, data on quality ANC were self-reported and retrospective in nature. Hence, there is the possibility of recall bias as well as social desirability bias. The quality ANC indicators provide a limited view of quality ANC, however these indicators are also important for screening several critical pregnancy situation. Also, we are unable to establish causal inferences as the data used in our analysis was cross-sectional. Moreover, this analysis based on only demand driven quality of ANC. As a study that relies on a secondary dataset, we are unable to assess the role of other important variables such as cultural norms and stigmatisation in determining quality ANC.
Conclusions
We conclude that the determinants of quality ANC include maternal age, maternal education, place of residence, birth order, pregnancy intention, female-headed household and wealth status. Also, women who face problems with distance to healthcare facilities and money had lower odds of receiving quality ANC. Interventions targeted at improving women’s uptake of quality ANC should prioritise adolescent girls, women with no formal education, those residing in rural areas, as well as women from low wealth index households.
Data availability
Data was requested and obtained from concerned authorities. The data is freely available in the DHS website on request (https://dhsprogram.com/data/available-datasets.cfm).
Abbreviations
- ANC:
-
Antenatal care
- QANC:
-
Quality antenatal care
- AIC:
-
Akaike information criterion
- BIC:
-
Bayesian information criterion
References
Cha, S. The impact of the worldwide Millennium Development Goals campaign on maternal and under-five child mortality reduction: ‘Where did the worldwide campaign work most effectively?’. Glob. Health Action 10, 1267961 (2017).
Maternal mortality. World Health Organization (2019).
WHO, UNICEF, UNFPA & WBG-UK. Maternal mortality: Levels and trends 2000 to 2017 (2019).
Anik, A. I., Islam, M. R. & Rahman, M. S. Do women’s empowerment and socioeconomic status predict the adequacy of antenatal care? A cross-sectional study in five South Asian countries. BMJ Open 11, e043940 (2021).
Amponsah-Tabi, S. et al. An assessment of the quality of antenatal care and pregnancy outcomes in a tertiary hospital in Ghana. PLoS ONE 17(10), e0275933 (2022).
Joshi C, et al. Factors associated with the use and quality of antenatal care in Nepal: a population-based study using the demographic and health survey data. BMC Pregnancy Childbirth. 14, 1–1 (2014).
Fagbamigbe, A. F & Idemudia, E. S. Assessment of quality of antenatal care services in Nigeria: evidence from a population-based survey. Reprod. Health 12, 1–9 (2015).
Abaraya, M., Seid, S. & Ibro, S. Determinants of preterm birth at Jimma University Medical Center, southwest Ethiopia. Pediatr. Health Med. Ther. 9, 101–107 (2018).
Abbas, A. M., Rabeea, M., Abdel Hafiz, H. A. & Ahmed, N. H. Effects of irregular antenatal care attendance in primiparas on the perinatal outcomes: A cross sectional study. Proc. Obstet. Gynecol. 7, 1–11 (2017).
Akter Id, E. et al. Levels and determinants of quality antenatal care in Bangladesh: Evidence from the Bangladesh Demographic and Health Survey. PLoS ONE 18, e0269767 (2023).
Sebayang, S. K., Efendi, F. & Astutik, E. Women’s empowerment and the use of antenatal care services: Analysis of demographic health surveys in five Southeast Asian countries. Women Health 59(10), 1155–1171 (2019).
National Institute of Population Research and Training (NIPORT) & ICF. Bangladesh Demographic and Health Survey 2017–18. National Institute of Population Research and Training (2020).
Ministry of Health-MOH/Nepal, New ERA/Nepal & ICF. Nepal Demographic and Health Survey 2016. Ministry of Health, Nepal, New (2017).
International Institute for Population Sciences-IIPS/India & ICF. National Family Health Survey NFHS-4, 2015–16 (International Institute for Population Sciences, 2017).
National Institute of Population Studies (NIPS) [Pakistan] & ICF. Pakistan Maternal Mortality Survey 2019. National Institute of Population Studies, Pakistan (2020).
Central Statistics Organization (CSO), Ministry of Public Health (MoPH) & ICF. Afghanistan Demographic and Health Survey 2015. Central Statistics Organization, Afghanistan (2017).
World Health Organization. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience (World Health Organization, 2016).
Arsenault, C. et al. Equity in antenatal care quality: An analysis of 91 national household surveys. Lancet Glob. Health 6, e1186–e1195 (2018).
Morón-Duarte, L. S., Ramirez Varela, A., Segura, O. & Freitas Da Silveira, M. Quality assessment indicators in antenatal care worldwide: A systematic review. Int. J. Qual. Heal. Care 31, 497–505 (2019).
Raru, T. B. et al. Quality of antenatal care and associated factors among pregnant women in East Africa using Demographic and Health Surveys: A multilevel analysis. Women’s Health https://doi.org/10.1177/17455065221076731 (2022).
Okedo-Alex, I. N., Akamike, I. C., Ezeanosike, O. B. & Uneke, C. J. Determinants of antenatal care utilisation in sub-Saharan Africa: A systematic review. BMJ Open 9, e031890 (2019).
Afulani, P. A. et al. Quality of antenatal care and associated factors in a rural county in Kenya: An assessment of service provision and experience dimensions. BMC Health Serv. Res. 19, 1–16 (2019).
Noh, J. W. et al. Factors associated with the use of antenatal care in Sindh province, Pakistan: A population-based study. PLoS ONE 14, e0213987 (2019).
Rahman, A. et al. Trends, determinants and inequities of 4+ ANC utilisation in Bangladesh. J. Health Popul. Nutr. 36, 2 (2017).
Pervin, J. et al. Determinants of utilization of antenatal and delivery care at the community level in rural Bangladesh. PLoS ONE 16, e0257782 (2021).
Chilot, D. et al. Pooled prevalence and determinants of antenatal care visits in countries with high maternal mortality: A multi-country analysis. Front. Public Health 11, 84 (2023).
Kumar, G. et al. Utilisation, equity and determinants of full antenatal care in India: Analysis from the National Family Health Survey 4. BMC Pregnancy Childbirth 19, 327 (2019).
Stanikzai, M. H., Wafa, M. H., Wasiq, A. W. & Sayam, H. Magnitude and Determinants of Antenatal Care Utilization in Kandahar City, Afghanistan. Obstet. Gynecol. Int. 2021, 1–7 (2021).
Fertility rate, total (births per woman) - South Asia. The World Bank (2020).
Aboagye R. G. et al. Health insurance coverage and timely antenatal care attendance in sub-Saharan Africa. BMC Health Serv. Res. 22(1), 181 (2022).
Muchie, K. F. Quality of antenatal care services and completion of four or more antenatal care visits in Ethiopia: A finding based on a demographic and health survey. BMC Pregnancy Childbirth 17, 1–7 (2017).
Neupane, S. & Doku, D. T. Determinants of time of start of prenatal care and number of prenatal care visits during pregnancy among Nepalese women. J. Community Health 37, 865–873 (2012).
Afulani, P. A. Rural/urban and socioeconomic differentials in quality of antenatal care in Ghana. PLoS ONE 10, e0117996 (2015).
Huda, F. A., Chowdhuri, S., Sarker, B. K., Islam, N. & Ahmed, A. Prevalence of unintended pregnancy and needs for family planning among married adolescent girls living in urban slums of Dhaka, Bangladesh (International Centre for Diarrhoeal Disease Research, 2014).
Fahme, S. A., Sieverding, M. & Abdulrahim, S. Sexual and reproductive health of adolescent Syrian refugee girls in Lebanon: A qualitative study of healthcare provider and educator perspectives. Reprod. Health 18, 1–16 (2021).
Li, J., Imam, S. Z., Jing, Z., Wang, Y. & Zhou, C. Suicide attempt and its associated factors amongst women who were pregnant as adolescents in Bangladesh: A cross-sectional study. Reprod. Health 18, 1–9 (2021).
Pandey, P. L., Seale, H. & Razee, H. Exploring the factors impacting on access and acceptance of sexual and reproductive health services provided by adolescent-friendly health services in Nepal. PLoS ONE 14, e0220855 (2019).
Tesfaye, G., Chojenta, C., Smith, R. & Loxton, D. Predisposing, enabling and need factors associated with skilled delivery care utilization among reproductive-aged women in Kersa district, eastern Ethiopia. Reprod. Health 16, 1–11 (2019).
Ahinkorah, B. O. et al. Determinants of antenatal care and skilled birth attendance services utilization among childbearing women in Guinea: Evidence from the 2018 Guinea Demographic and Health Survey data. BMC Pregnancy Childbirth 21, 1–11 (2021).
Acknowledgements
The authors want to acknowledge the Measures DHS data archive for providing us with the datasets for further analysis.
Author information
Authors and Affiliations
Contributions
I.H., M.K.H., and B.O.A. conceptualized the study; I.H. and M.K.H. developed the methodology; I.H., B.O.A., A.S., J.O., M.K.H. validated and scrutinized the study; I.H., B.O.A., J.O., M.K.H. investigated the study; I.H., B.O.A., M.H., J.H., A.S. wrote the original draft; I.H., B.O.A., J.O., M.K.H., reviewed and edited the article. All authors have read and agreed to the current version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Methun, M.I.H., Ahinkorah, B.O., Hassan, M.M. et al. Individual and community-level determinants of quality antenatal care in six South Asian countries. Sci Rep 14, 18646 (2024). https://doi.org/10.1038/s41598-024-67206-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-67206-3
- Springer Nature Limited