Abstract
Because of the advent of genome-editing technology, gene knockout (KO) hamsters have become attractive research models for diverse diseases in humans. This study established a new KO model of diabetes by disrupting the insulin receptor substrate-2 (Irs2) gene in the golden (Syrian) hamster. Homozygous KO animals were born alive but with delayed postnatal growth until adulthood. They showed hyperglycemia, high HbA1c, and impaired glucose tolerance. However, they normally responded to insulin stimulation, unlike Irs2 KO mice, an obese type 2 diabetes (T2D) model. Consistent with this, Irs2 KO hamsters did not increase serum insulin levels upon glucose administration and showed β-cell hypoplasia in their pancreas. Thus, our Irs2 KO hamster provide a unique T2D animal model that is distinct from the obese T2D models. This model may contribute to a better understanding of the pathophysiology of human non-obese T2D with β-cell dysfunction, the most common type of T2D in East Asian countries, including Japan.
Similar content being viewed by others
Introduction
Animal models have played major roles in the etiological analysis and the therapeutic development of human diseases. In particular, laboratory mice and rats have provided many model strains carrying spontaneous mutations or artificially modified genes1,2,3. However, because of the differences between humans and mice/rats in various metabolic systems, they cannot appropriately reproduce some human diseases, such as lipid metabolic disorders4,5,6. Although primates and domestic animals can compensate for the shortcomings of mice and rats, these non-rodent animals are not widely used because of animal ethics issues and the time/cost required to create genetically modified animals.
The golden hamster (Mesocricetus auratus) is a rodent widely used in biomedical research, including oncology, immunology, physiology, and reproductive biology7. Hamsters belong to the family Cricetidae, which is taxonomically distinct from that of mice and rats, the Muridae rodents. The last common ancestor of hamsters and mice/rats lived about 10–40 million years ago8,9, and it is possible that the different lineages acquired distinct physiological traits during this long period. Therefore, hamsters may provide a valuable experimental model that cannot be achieved with rats or mice, based on their unique physiological characteristics. For example, hamsters have unique reproductive characteristics, such as a stable 4-day estrous cycle, high responsiveness to conventional superovulation methods (> 50 oocytes per female), and the shortest gestation period (16 days) among eutherian mammals10. Like mice and rats, hamsters can be easily kept and bred in standard laboratories7.
Gene knockout (KO) technology plays a major role in the generation of model animals. In mice, generating KO lines became practical as early as the 1980s with the availability of embryonic stem cells that can be gene-targeted and contribute to the germ line11. However, for many animals, including hamsters, the inability to establish high-quality embryonic stem cells has made the generation of KO animals difficult. In 2013, genome-editing technology using the CRISPR/Cas9 system was for the first time used in mice, making it possible to create KO animals using fertilized eggs in mammals12,13. In hamsters, the first gene-edited knockout strain (Stat2 KO) was produced in 201414. The golden hamster has cardiovascular and lipid metabolism systems similar to humans, so it may provide unique and useful animal models for research on human metabolic diseases15. Based on this advantage, genome-edited KO hamsters have been generated for models of aortic atherosclerosis with the lecithin-cholesterol acyltransferase mutation16 and coronary atherosclerosis with the LDL receptor mutation17.
Although human lipid metabolism abnormalities caused by metabolic syndrome have been well reproduced in a hamster model, there is no hamster model for diabetes, the other major disease related to metabolic syndrome. Therefore, we attempted to generate a diabetic hamster model by targeting the Irs2 (insulin receptor substrate 2) gene, a causative factor of diabetes in mice and humans18,19. IRS2 is one of the insulin receptor substrates essential for mediating the signaling downstream of the insulin receptor and other receptor tyrosine kinases20. Accumulated experimental evidence indicates that IRS2 is critical for pancreatic β-cell growth, function, and development21. As expected, Irs2 KO hamsters developed congenital diabetes with typical hyperglycemia and glucose intolerance. However, unlike Irs2 KO mice, Irs2 KO hamsters showed a non-obese (lean) phenotype, insulin responsiveness, and heavy β-cell hypoplasia. These animals are expected to provide a unique animal model for human type 2 diabetes (T2D) with β-cell dysfunction, the most prevailing diabetes in East Asian countries, including Japan22,23. According to the classification of T2D, they also resemble a subtype of severe insulin-deficient diabetes (SIDD) characterized by low age onset and low BMI24.
Results
Generation of Irs2 KO hamsters
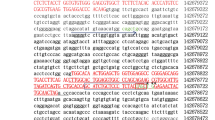
We designed seven single-guide RNAs (sgRNAs) that target the sequences of either the 5′ or 3′ side of the CDS domain (exon 1) of the hamster Irs2 gene (Fig. 1A,B). In mice and humans, the 5′ half of the Irs2 gene contains the highly conserved PH- and PTB-encoding sequences that target IRS-2 to the cell membrane and insulin receptor (IR), respectively25,26. As expected, hamster Irs2 also contains these sequences, indicating that the same functions of IRS2 may be conserved in hamsters (Fig. 1B and Supplementary Fig. S1). We injected the seven sgRNAs, together with the Cas9 protein, into the oviducts of 47 females on day 0.5 (the day after mating) and immediately applied electric pulses to the oviducts. Sixteen females became pregnant and gave birth to 101 pups on day 15.5. Of them, 12 (eight females and four males) carried mutant alleles. We mated these 12 mutant founders (F0) with wild-type (WT) hamsters to generate heterozygous KO hamsters of F1. As F0 #35 first gave birth to 25 pups, including one heterozygous KO female, we used its mutant allele to generate an Irs2 KO hamster line (Table 1). The Irs2 mutation is a 2653-bp deletion at exon 1, indicating that the mutant allele had lost the conserved domains (PH and PTB) (Fig. 1B).
Generation of Irs2 KO hamsters. (A) The exon composition of the hamster Irs2 gene. Specific gRNAs were designed to target sequences on the 5′ or 3′ side of the CDS domain (exon 1) of the hamster Irs2 gene. (B) The mutant allele of a founder F0#35 was used to establish the Irs2 KO strain. A 2653-bp deletion was identified at the first exon. The mutant allele lost three major domains of hamster Irs2 (PH, PTB, and KRLB) (see also Supplementary Fig. S1). (C) Body weight change of Irs2 KO hamsters. Homozygous (Ho) KO hamsters of both sexes had lower body weight than heterozygous (Het) KO or wild-type (WT) hamsters (*P < 0.05, Scheffe’s F multiple comparison test). There were no significant differences between homozygous KO groups and between heterozygous KO/WT groups. Each group consisted of 2–6 animals. (D) Appearance of homozygous (homo) and heterozygous (hetero) KO hamsters, which can be distinguished by size. (E) Expression levels of Irs1 and Irs2 in Irs2 KO hamsters. *P < 0.05 (vs. wild type). N.D., not detected. Error bars mean S.E.
By intercrossing heterozygous KO hamsters, we found that homozygous KO hamsters were born alive but showed retarded growth postnatally and maintained low body weight in adults in both sexes (Fig. 1C,D). However, they showed no deteriorated systemic condition until at least 14 months of age. Heterozygous KO hamsters were indistinguishable from WT hamsters in their appearance. We observed that homozygous KO hamsters of both sexes were infertile according to natural mating tests with heterozygous or WT hamsters of the opposite sex. Homozygous KO males had smaller testes than did WT or heterozygous KO littermates, although they produced mature spermatozoa, which were stored in the epididymides (Supplementary Fig. S2A). The ovaries of homozygous KO females were also small and contained fewer developing follicles, associated with many degenerating follicles (Supplementary Fig. S2B). We confirmed that at least some of the homozygous KO males mated with females and deposited spermatozoa in the females’ vagina. Some homozygous KO females maintained the regular 4-day estrous cycle and mated with males. Therefore, there may be fertilization or subsequent development failures in homozygous KO hamsters, but the exact causes of their infertility remain to be determined.
We maintained the Irs2 KO hamster line in this study by mating heterozygous siblings. The results of the mating of heterozygous parents in F1 to F7 are shown in Table 1. The proportion of homozygous KO pups was 8.2%, far less than the expected Mendelian ratio (P < 0.0001). This indicates that homozygous KO pups died before or around birth or were cannibalized by mothers before genotyping (2–3 weeks of age).
Gene expression analysis
The Irs2 gene was expressed in all tissues analyzed in heterozygous KO and WT hamsters, but no expression was observed in homozygous KO hamsters (Fig. 1E). The Irs1 gene, from the same gene family of Irs2, was expressed in all these tissues, irrespective of the genotype, but its expression level in the pancreas was significantly decreased in homozygous KO hamsters. This is likely due to the decrease of β-cell masses in homozygous KO hamsters because both Irs1 and Irs2 are expressed in pancreatic islets21 (see below; Fig. 1E). There seemed to be no compensatory mechanism of Irs1 for the Irs2 deficiency, except for the muscle that showed a significant increase of the Irs1 expression in homozygous Irs2 KO hamsters (Fig. 1E). It was reported that IRS1 and IRS2 cooperatively regulate the skeletal muscle growth and metabolism27. We confirmed that the coding sequence of the Irs1 gene is intact in the Irs2 KO hamster (Supplementary Fig. S3). The expression level of Irs1 in the kidney was also decreased in Irs2 KO hamsters, but its reason was unclear.
Serum and blood tests
All serum biochemical and blood values were analyzed by two-way ANOVA (genotype × sex). The genotype had significant effects on glucose, urea nitrogen (UN), high-density lipoprotein cholesterol (HDL-C), triglyceride (TG), and hemoglobin A1c (HbA1c), but not in other parameters, including insulin (Table 2). Of these, glucose, UN, TG, and HbA1c had no significant interactions between two factors, indicating that the genotype affected these parameters independently of sex. Statistical analysis revealed that the glucose level was significantly higher in homozygous KO hamsters than in heterozygous KO or WT hamsters, indicating that they suffered from hyperglycemia (Fig. 2A). Consistently with this, HbA1c, which reflects the long-term glycemic status, was significantly higher in homozygous KO hamsters than in heterozygous KO or WT hamsters (Fig. 2A). The UN level was slightly but significantly higher in homozygous KO hamsters (Fig. 2A). The results of other parameters are shown in Supplementary Fig. S4.
Clinical blood parameters and glucose metabolic tests in Irs2 KO hamsters. (A) Three parameters with significant differences in genotype (homozygous KO > heterozygous KO and WT, *P < 0.05). (B) Glucose tolerance test. (C) Insulin tolerance test. (D) The serum insulin level after glucose load. Asterisks in (C) and (E) indicate significant differences between homozygous KO and heterozygous KO/WT hamsters. Scheffe’s F multiple comparison test is for the glucose tolerant test, and Student’s t-test is for the other two tests. Ho, homozygous KO (n = 3–6); Het, heterozygous KO (n = 3–5); WT, wild-type (n = 2). Error bars mean S.E.
In vivo glucose homeostasis
Upon intraperitoneal glucose administration, the increase in blood glucose levels was significantly greater and stayed higher until 120 min in homozygous KO hamsters than in heterozygous KO and WT hamsters (Fig. 2B). The same tendency was observed by oral administration of glucose. However, the significantly higher glucose level in homozygous KO hamsters was found only at 60 min (Supplementary Fig. S5). There were no significant differences in the glucose level between heterozygous KO hamsters and WT hamsters (Fig. 2B and Supplementary Fig. S5). These results indicated that glucose tolerance ability was decreased in homozygous KO hamsters but not in heterozygous KO hamsters. The insulin tolerance test revealed that homozygous and heterozygous KO hamsters reacted normally to insulin administration (Fig. 2C) and reached the same serum glucose level (Supplementary Fig. S6). We also confirmed that the insulin level in homozygous KO hamsters did not increase upon glucose treatment (Fig. 2D).
Histological observations and immunostaining
In vivo glucose homeostasis assays (above) indicated insufficient β-cell function in Irs2 KO hamsters. We then examined the population of insulin-positive β-cells in their pancreas by immunohistochemistry. The relative areas of insulin-positive cells in homozygous KO hamsters were significantly decreased and many of the islets were smaller than those of heterozygous KO hamsters (Fig. 3A–C). To determine whether the reduction in pancreatic islets in homozygous KO hamsters was resulted from increased apoptosis or decreased mitotic cells, we stained the pancreatic tissues of adult hamsters with specific antibodies. No apoptotic cells positive for cleaved Caspase-3 were detected in either homozygous or heterozygous KO islets (Fig. 3D,E). Proliferating cells positive for Ki67 were observed in both groups at a similarly low rate (Fig. 3F,G). As inflammatory markers, we also stained the pancreatic tissues for CD3 (T cell marker) and CD68 (macrophage marker). While CD3-positive cells were not detected in the islets of either homozygous or heterozygous KO hamsters, very few CD68-positive cells were observed in both groups. The islets of homozygous KO hamsters seemed to contain more CD68-positive cells than those of heterozygous KO hamsters but without any significant difference (Fig. 3H–K). Taken together, it is probable that the β-cell populations in Irs2 KO hamsters decrease before adulthood and remain small throughout life. Although the serum UN value was elevated in homozygous KO hamsters, there were no histological changes in their kidney tissue except for occasional expansion of glomerular capsules (Fig. S4).
Histological observation of β-cells in heterozygous (+/−) and homozygous (−/−) KO hamsters. (A) Insulin-positive β-cells stained with a specific antibody. (B, C) Relative insulin-positive areas of the pancreas and islet sizes. Results in (B) and (C) are from 6 and 3 animals, respectively. Bar: 100 µm. (D–K) Left column: Immunostaining for cleaved Caspase-3 (cCasp3), Ki67, CD3, and CD68, together with immunostaining for insulin. White dotted rectangles contained marker-positive cells within the insulin-positive islets. Insets were enlarged areas of the white dotted rectangles. White arrows indicate the marker-positive cells outside of islets. Right column: The areas of positive cells in islets. Bar: 100 µm. Error bars mean S.E.
Glucose-induced insulin secretion test
Finally, we performed a glucose-induced insulin secretion test by incubating pancreatic islets (10 islets per sample) isolated from WT or homozygous KO hamsters. As expected from the reduced volume of each islet in KO hamster pancreas as described above (Fig. 3C), the amounts of secreted insulin per islet were significantly lower in the KO group, irrespective of the concentration of glucose and with/without the co-treatment of KCl (Fig. 4A). The insulin content per islet was also lower in the KO group (Fig. 4B). However, there was a possibility that this low insulin production in KO hamster islets was simply due to the small number of β-cells per islet (Fig. 4C). The insulin secretions/contents were re-evaluated per islet cell. As shown in Fig. 4D,E, insulin secretion and content were lower in the KO group. These results further confirmed the in vivo glucose homeostasis tests (above), which indicated β-cell dysfunction in Irs2 KO hamsters.
In vitro insulin secretion and content test using islets isolated from WT (gray) and Irs2 KO (blue) hamsters. (A, B) Insulin secretion and content calculated per islet (n = 10 for each measurement). (C) Cell number in each islet used for analyses. (D, E) Insulin secretion and content calculated per islet cell. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001. Average (n = 5–6) ± S.E.
Discussion
Animal models have long played an important role in understanding the etiology and clinical complications of human diabetic diseases. Historically, most diabetes models in mice and rats have been established by selective breeding of natural mutants based on their phenotypes28,29. Therefore, only a few genetically modified animals with clear diabetic phenotypes are available. Genetically modified models are advantageous in the preciseness of the causative gene involved in pathophysiology, especially when the models have a defined genetic background, i.e., inbred mice. In mice, Irs2 KO strains are such typical models that they have been generated by mixed breeding of two inbred strains, such as C57BL/6× CBA30,31. Syrian hamsters are considered genetically homogeneous because all hamsters in laboratories are descendants of two females and one male captured from their native habitat7. This study demonstrated that Irs2 KO hamsters consistently develop diabetes with typical hyperglycemia and glucose intolerance. These phenotypes will be reproducible in any laboratory given their homogeneous genetic background.
Mouse and hamster models with Irs2 deficiency share common diabetic phenotypes (hyperglycemia and glucose intolerance), but their pathophysiology seems to be largely different. Irs2 KO hamsters showed a lean phenotype throughout their lifespan, while Irs2 KO mice developed an obese phenotype due to heavy adiposity32,33. Interestingly, unlike Irs2 KO mice18, Irs2 KO hamsters normally responded to insulin treatment, indicating that they did not develop insulin resistance even under diabetic conditions. Irs2 KO hamsters lost the ability to increase serum insulin after glucose load, most likely because of the β-cell dysfunction indicated by immunohistochemistry and in vitro insulin secretion tests using isolated islets. In Irs2 KO mice, it was reported that insulin secretion ability per β-cell increased to maintain the total insulin secretion level18. In contrast, the insulin production ability of β-cells in Irs2 KO hamsters was significantly reduced (Fig. 4), indicating that these β-cells did not compensate for the decreased serum insulin level in Irs2 KO hamsters.
Human T2D can be roughly classified into two major classes (obese and non-obese types) or five subclasses based on clinical parameters and prognosis24. Irs2 KO mice have greatly contributed to understanding the pathophysiology of obese T2D, such as the underlying mechanisms of insulin resistance, the roles of Irs2 and related factors in different tissues, and the insulin signaling pathway under diabetic conditions33,34,35. Therefore, much information has been accumulated on the pathophysiology of obese T2D by this mouse model. By contrast, the pathophysiology of non-obese T2D remains poorly understood, while cases are rapidly increasing, especially in East Asian countries22,23. T2D in East Asians is characterized by β-cell dysfunction and less obesity than in Caucasians36,37,38. Thus, there may be some pathophysiological difference between the T2D of East Asians and Caucasians, which may reflect the long-term dietary difference between them; East Asians have been primarily agriculturalists since rice domestication in China about 10,000 years ago39. The phenotypes of Irs2 KO hamsters we identified resemble those of human non-obese T2D, specifically a severe insulin-deficient diabetes (SIDD) subtype regarding their non-obese feature and β-cell dysfunction tendency24. Interestingly, it is known that hamsters prefer plant diets, such as grains, while mice have more omnivorous tendencies7,40. Perhaps such differences in diet between mice and hamsters for over tens of thousands of years may have caused the differences in the β-cell robustness and the metabolic responsiveness to diabetic disorders.
A major clinical issue associated with human diabetes is that it is highly prone to various complications. Major complications include chronic kidney disease, visual impairment, nerve damage, and heart disease41. However, Irs2 KO hamsters did not show such severe complications under our standard breeding conditions. Although the serum UN level increased significantly in Irs2 KO hamsters, at the microscopic level they showed no major signs of renal pathological changes. In hamsters, the APA strain is predisposed to glomerulopathy42 and can develop persistent hyperglycemia and diabetic nephropathy after a single low dose of streptozotocin injection. Irs2 KO hamsters may also develop diabetic nephropathy if a strain prone to nephropathy can be used as the genetic background. Additionally, it would be interesting to see whether a high-fat diet may further aggravate hyperglycemia and compromise its systemic condition in Irs2 KO hamsters. As Irs2 is expressed in many tissues, conditional KO hamsters, if generated, would give more accurate information on the progress of T2D in hamsters.
In conclusion, we generated a T2D hamster model with a non-obese phenotype that may become a unique experimental model for human non-obese T2D with β-cell dysfunction. Further experiments, including high-fat diet treatment, detailed analysis at an early age, or tissue-specific KO, would elucidate the advantage of the Irs2 KO hamster as T2D models in the future. They would also provide important information on the mechanisms underlying the severe clinical symptoms of SARS-Co-2 infection in patients with diabetes43. Our Irs2 KO hamsters are freely available from the RIKEN BioResource Research Center (AO) on request.
Methods
Animals
Seven- to ten-week-old golden (Syrian) hamsters were purchased from Japan SLC, Inc. (Shizuoka, Japan). They were used for experiments at 15–40 weeks of age. All hamsters were kept under specific pathogen-free conditions, provided with commercial laboratory mouse food and water ad libitum, and housed under controlled lighting conditions (daily light period, 04:00–18:00 h) at a temperature of 24 °C and humidity of 50%. The care and use of animals in this study were performed according to the guidelines for using and maintaining experimental animals from the Japanese Ministry of Environment. The Institutional Animal Care and Use Committee of RIKEN Tsukuba Branch approved all animal experiments included in this study. This study is reported by ARRIVE guidelines (https://arriveguidelines.org). All the operations during i-GONAD experiments were performed on animals under ketamine anesthesia. When samples were collected from animals, they were euthanized with high concentrations of isoflurane.
Genome editing by the CRISPR/Cas9 system
The sgRNAs were designed using CRISPR (http://crispor.tefor.net) and produced using a GeneArt Precision gRNA Synthesis Kit (#A29377; Thermo Fisher Scientific). In this study, we employed an in vivo genome-editing method (improved genome editing via oviductal nucleic acid delivery, i-GONAD44,45 to avoid in vitro developmental arrest of hamster embryos highly sensitive to an in vitro milieu10. Briefly, a solution containing seven sgRNAs and the Cas9 protein (#1081059; IDT) was prepared (Fig. 1A). Approximately 3.5–4.0 μL of the solution was injected from the upper segment of the ampulla to the lower segments using a fine glass micropipette. After injection, the oviduct was pinched by a forceps-type electrode (#CUY650P5; NEPA GENE). Electroporation was performed using NEPA21 (NEPA GENE). Electroporation conditions consisted of three sequential poring pulses (40–50 V, 5-ms duration, 50-ms intervals) followed by three transfer pulses (10 V, 50-ms duration, 50-ms intervals). On day 15.5 of pregnancy, the fetuses were delivered naturally, and live pups were examined for CRISPR-Cas9-induced mutations at the target sites.
Gene expression analysis
Total RNAs from fresh tissues were purified using the RNeasy Mini Kit (#74104; Qiagen, Nordrhein-Westfalen, Germany). DNaseI treatment was performed on columns with the RNase-Free DNase Set (Qiagen). cDNAs were synthesized from purified RNA using the SuperScript IV First-Strand Synthesis System (#18091050; Thermo Fisher Scientific). RT-PCR was performed using PowerUp SYBR Green Master Mix (#A25742; Thermo Fisher Scientific) with the QuantStudio 7 system (Thermo Fisher Scientific). Ct values were normalized to those of beta-actin, and relative gene expression levels were calculated using the ΔΔCt method. Each experiment was performed in duplicate. Primer sets used are as follows: Irs1 (CTGACATTGGAGGTGGGTCC and TTTGGAATGAGGCAGGGCAT), Irs2 (GACAGCGACCAGTATGTGCT and GAGTGGTGAGGCTGGGTATG), and beta-actin (CAAGAGATGGCCACTGCCG and GTGGATGCCACAGGATTCCATA).
Serum and blood tests
Blood samples were taken from WT and homozygous and heterozygous KO hamsters by cardiac puncture. Serum was centrifuged at 5000×g for 10 min at 8 °C. Biochemical parameters were measured using an automated biochemical analyzer, BioMajesty JCA-BM6070 (JEOL Ltd.,). Serum insulin levels were measured using a Bio-Plex mouse diabetes insulin set (Bio-Rad Laboratories, Inc.) and a Bio-Plex200 system (Bio-Rad Laboratories, Inc.).
In vivo glucose homeostasis
For the glucose tolerance test, the hamsters were fasted for 20 h and peritoneally injected with 1 mg/kg glucose solution. Blood samples were taken from the tail or orbital sinus at different time points and glucose (GLUCOCARD G + meter, ARKRAY, Inc.) or insulin (described above) was measured. For the insulin tolerance test, the hamsters were fed freely and fasted during the experiment. They were peritoneally injected with 0.75 U/kg of human insulin (Eli Lilly, Japan), and blood sample collection and glucose measurement were performed as described above.
Histology and immunostaining
Hamster tissue samples with different genotypes were collected from the brain, lung, heart, kidney, liver, pancreas, and muscle (hind leg). They were fixed in 4% paraformaldehyde and embedded in paraffin. Tissue sections (4–5-µm thickness) were stained with hematoxylin and eosin. Pancreatic sections were stained with mouse anti-insulin monoclonal antibody (INS monoclonal antibody, cat no. 66198-1-Ig, 1:5000 dilution) followed by biotinylated antimouse IgG antibody (1:400 dilution). The stained biotin signals were visualized using the VECTASTAIN Elite ABC Kit (VECTOR, cat no. PK-6100) and diaminobenzidine (DAB) as a brown color. The immunostained sections were counterstained with hematoxylin. For immunofluorescence double staining, the sections were stained with mouse anti-insulin monoclonal antibody (INS monoclonal antibody, cat no. 66198-1-Ig, 1:5000 dilution) together with either rabbit anti-cleaved Caspase-3 antibody (Cell Signaling Technology, cat no. 9664, 1:1000 dilution), rabbit anti-Ki67 antibody (Abcam, cat no. ab15580, 1:200 dilution), rabbit anti-CD3 antibody (Abcam, cat no. ab16669, 1:100 dilution), or rabbit anti-CD68 antibody (Abcam, cat no. ab213363, 1:100 dilution), followed by the mixture of secondary antibodies including donkey anti-mouse IgG Alexa Fluor 555 (ThermoFisher Scientific, cat no. A-31570, 1:400 dilution) and donkey anti-rabbit IgG Alexa Fluor 488 (ThermoFisher Scientific, cat no. A-21206, 1:400 dilution). The areas of insulin-positive cells (β-cells) were traced, and ImageJ was used to calculate their proportions with the entire pancreas.
Pancreatic islet isolation
Islets of Langerhans were isolated from hamsters by collagenase digestion as previously described46. Briefly, Hank’s balanced salt solution (HBSS) supplemented with 20 mM HEPES, 5 mM NaHCO3, 1% bovine serum albumin (BSA), and 0.5 mg/ml collagenase P (Roche, Germany) was injected into the pancreas via the tied bile duct. The pancreas was dissected and digested in a water bath at 37 °C for 30 min. The digested pancreas was homogenized using a serological pipette and washed twice with Krebs–Ringer bicarbonate (KRB) buffer (129.4 mM NaCl, 5.2 mM KCl, 2.7 mM CaCl2, 1.3 mM MgSO4, 24.8 mM NaHCO3, 1.3 mM KH2PO4) containing 2.8 mM glucose. Islets were extracted from homogenate by density gradient centrifugation using histopaque 1119, histopaque 1077, and histopaque 1050 (prepared by mixing two volumes of histopaque 1077 with one volume of distilled water). After centrifugation, the islets in the inter-phase between histopaque 1050 and histopaque 1077 were transferred to a black-bottom dish. The islets were washed in ice-cold KRB buffer, handpicked, and cultured overnight in RPMI 1640 medium containing 10% fetal bovine serum, 10 mM HEPES, 5 mM NaHCO3, 1 mM sodium pyruvate, 100 U/ml penicillin, 100 mg/ml streptomycin and 11.1 mM glucose at 37 °C in humidified air containing 5% CO2.
Measurement of insulin secretion
Overnight-cultured islets were pre-incubated in Buffer A [KRB buffer containing 10 mM HEPES pH 7.4, 0.2% BSA, and 2.8 mM glucose] at 37 °C for 60 min. After preincubation, 10 size-matched islets were hand-picked into tubes with 1 mL of Buffer A containing 16.7 mM glucose and/or 30 mM KCl and incubated at 37 °C for 60 min. After incubation, each tube was centrifuged at 9000g for 1 min. The supernatant was collected for measuring insulin secretion, while the pelleted islets were lysed in 200 μl of PBS with 0.2% Triton-X100 for measuring insulin content. Insulin concentrations were measured by homogeneous time-resolved fluorescence (HTRF) assay using a Insulin High Range Assay Kit (CIS Bio International, France) and Synergy H1 (BioTek Instruments) according to the manufacturer’s instructions. The number of islet cells was measured with a hemacytometer.
Statistical analysis
Body weights at each week of age were analyzed using Scheffe’s F multiple comparison test. The proportion of β-cell areas in the pancreas and the expression levels of the expression levels of Irs1 and Irs2 genes were analyzed using an unpaired two-tailed Student t-test. The two-way ANOVA analyzed clinical blood parameters. Parameters with significant interactions between two factors (genotype and sex) were further analyzed using Tukey multiple comparisons. Other statistical analyses are indicated as appropriate. A P value less than 0.05 indicated a statistically significant difference.
Data availability
All data and supporting information are contained within the article.
References
Baumans, V. The UFAW Handbook on the Care and Management of Laboratory and Other Research Animals. (ed. P Trevor) 282–312 (Blackwell Science, 1999).
Koolhaas, J. M. The UFAW Handbook on the Care and Management of Laboratory and Other Research Animals (ed. P Trevor) 313–330 (Blackwell Science, 1999).
Mashimo, T. & Serikawa, T. Rat resources in biomedical research. Curr. Pharm. Biotechnol. 10, 214–220 (2009).
Thyagarajan, T., Totey, S., Danton, M. J. & Kulkarni, A. B. Genetically altered mouse models: The good, the bad, and the ugly. Crit. Rev. Oral. Biol. Med. 14, 154–174 (2003).
Seok, J. et al. Genomic responses in mouse models poorly mimic human inflammatory diseases. Proc. Natl. Acad. Sci. USA 110, 3507–3512 (2013).
Mestas, J. & Hughes, C. C. Of mice and not men: Differences between mouse and human immunology. J. Immunol. 172, 2731–2738 (2004).
Whittaker, D. The UFAW Handbook on the Care and Management of Laboratory Animals (ed. P Trevor) 356–366, (Blackwell Science, 1999).
Swanson, M. T., Oliveros, C. H. & Esselstyn, J. A. A phylogenomic rodent tree reveals the repeated evolution of masseter architectures. Proc. Biol. Sci. 286, 20190672 (2019).
Herrera-Álvarez, S. et al. How to make a rodent giant: Genomic basis and tradeoffs of gigantism in the capybara, the world’s largest rodent. Mol. Biol. Evolut. 38, 1715–1730 (2021).
Hirose, M. & Ogura, A. The golden (Syrian) hamster as a model for the study of reproductive biology: Past, present, and future. Reprod. Med. Biol. 18, 34–39 (2019).
Capecchi, M. R. The new mouse genetics: Altering the genome by gene targeting. Trends Genet. 5, 70–76 (1989).
Mashiko, D. et al. Generation of mutant mice by pronuclear injection of circular plasmid expressing Cas9 and single guided RNA. Sci. Rep. 3, 3355 (2013).
Wang, H. et al. One-step generation of mice carrying mutations in multiple genes by CRISPR/Cas-mediated genome engineering. Cell 153, 910–918 (2013).
Fan, Z. et al. Efficient gene targeting in golden Syrian hamsters by the CRISPR/Cas9 system. PLoS One 9, e109755 (2014).
Bhathena, J. et al. Diet-induced metabolic hamster model of nonalcoholic fatty liver disease. Diabetes Metab. Syndr. Obes. 4, 195–203 (2011).
Dong, Z. et al. Loss of LCAT activity in the golden Syrian hamster elicits pro-atherogenic dyslipidemia and enhanced atherosclerosis. Metabolism 83, 245–255 (2018).
Guo, X. et al. LDL receptor gene-ablated hamsters: A rodent model of familial hypercholesterolemia with dominant inheritance and diet-induced coronary atherosclerosis. EBioMedicine 27, 214–224 (2018).
Kubota, N. et al. Disruption of insulin receptor substrate 2 causes type 2 diabetes because of liver insulin resistance and lack of compensatory beta-cell hyperplasia. Diabetes 49, 1880–1889 (2000).
Bottomley, W. E. et al. IRS2 variants and syndromes of severe insulin resistance. Diabetologia 52, 1208–1211 (2009).
Haeusler, R. A., McGraw, T. E. & Accili, D. Biochemical and cellular properties of insulin receptor signalling. Nat. Rev. Mol. Cell Biol. 19, 31–44 (2018).
Taguchi, A. & White, M. F. Insulin-like signaling, nutrient homeostasis, and life span. Annu. Rev. Physiol. 70, 191–212 (2008).
Olaogun, I., Farag, M. & Hamid, P. The pathophysiology of type 2 diabetes mellitus in non-obese individuals: An overview of the current understanding. Cureus 12, e7614 (2020).
Yabe, D., Seino, Y., Fukushima, M. & Seino, S. β cell dysfunction versus insulin resistance in the pathogenesis of type 2 diabetes in East Asians. Curr. Diab. Rep. 15, 602 (2015).
Ahlqvist, E. et al. Novel subgroups of adult-onset diabetes and their association with outcomes: A data-driven cluster analysis of six variables. Lancet. Diabetes Endocrinol. 6, 361–369 (2018).
Virkamäki, A., Ueki, K. & Kahn, C. R. Protein-protein interaction in insulin signaling and the molecular mechanisms of insulin resistance. J. Clin. Invest. 103, 931–943 (1999).
Sawka-Verhelle, D. et al. Tyr624 and Tyr628 in insulin receptor substrate-2 mediate its association with the insulin receptor. J. Biol. Chem. 272, 16414–16420 (1997).
Long, Y. C., Cheng, Z., Copps, K. D. & White, M. F. Insulin receptor substrates Irs1 and Irs2 coordinate skeletal muscle growth and metabolism via the Akt and AMPK pathways. Mol. Cell. Biol. 31, 430–441 (2011).
Srinivasan, K. & Ramarao, P. Animal models in type 2 diabetes research: An overview. Indian J. Med. Res. 125, 451–472 (2007).
Leiter, E. H. The genetics of diabetes susceptibility in mice. Faseb J. 3, 2231–2241 (1989).
Goren, H. J., Kulkarni, R. N. & Kahn, C. R. Glucose homeostasis and tissue transcript content of insulin signaling intermediates in four inbred strains of mice: C57BL/6, C57BLKS/6, DBA/2, and 129X1. Endocrinology 145, 3307–3323 (2004).
Withers, D. J. et al. Disruption of IRS-2 causes type 2 diabetes in mice. Nature 391, 900–904 (1998).
Weale, R. A. Pre-retinal absorption and scotopic sensitivity. Vision Res. 15, 882 (1975).
Suzuki, R. et al. Both insulin signaling defects in the liver and obesity contribute to insulin resistance and cause diabetes in Irs2(−/−) mice. J. Biol. Chem. 279, 25039–25049 (2004).
Brady, M. J. IRS2 takes center stage in the development of type 2 diabetes. J. Clin. Invest. 114, 886–888 (2004).
Kubota, T., Kubota, N. & Kadowaki, T. Imbalanced insulin actions in obesity and type 2 diabetes: Key mouse models of insulin signaling pathway. Cell Metab. 25, 797–810 (2017).
Møller, J. B. et al. Body composition is the main determinant for the difference in type 2 diabetes pathophysiology between Japanese and Caucasians. Diabetes Care 37, 796–804 (2014).
Møller, J. B. et al. Ethnic differences in insulin sensitivity, β-cell function, and hepatic extraction between Japanese and Caucasians: A minimal model analysis. J. Clin. Endocrinol. Metab. 99, 4273–4280 (2014).
Fukushima, M., Suzuki, H. & Seino, Y. Insulin secretion capacity in the development from normal glucose tolerance to type 2 diabetes. Diabetes Res. Clin. Pract. 66(Suppl 1), S37-43 (2004).
Molina, J. et al. Molecular evidence for a single evolutionary origin of domesticated rice. Proc. Natl. Acad. Sci. USA 108, 8351–8356 (2011).
Van Hoosier, G. L. & McPherson, C. W. Laboratory Hamsters. (Academic Press, 1987).
Zheng, Y., Ley, S. H. & Hu, F. B. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol. 14, 88–98 (2018).
Doi, K. et al. Age-related non-neoplastic lesions in the heart and kidneys of Syrian hamsters of the APA strain. Lab. Anim. 21, 241–248 (1987).
Das, S. et al. Role of comorbidities like diabetes on severe acute respiratory syndrome coronavirus-2: A review. Life Sci. 258, 118202 (2020).
Gurumurthy, C. B. et al. Creation of CRISPR-based germline-genome-engineered mice without ex vivo handling of zygotes by i-GONAD. Nat. Protoc. 14, 2452–2482 (2019).
Hirose, M., Tomishima, T. & Ogura, A. Editing the genome of the golden hamster (Mesocricetus auratus). Methods Mol. Biol. (Clifton, NJ). 2637, 247–254 (2023).
Usui, R. et al. GPR40 activation initiates store-operated Ca(2+) entry and potentiates insulin secretion via the IP3R1/STIM1/Orai1 pathway in pancreatic β-cells. Sci. Rep. 9, 15562 (2019).
Acknowledgements
This study was supported by Grants-in-Aid for Scientific Research (KAKENHI) from the Japan Society for the Promotion of Science to A. Ogura (Grant numbers: JP19H05758, JP19H03151, and JP23H02403) and K. I. (Grant number: 23H04956).
Author information
Authors and Affiliations
Contributions
M.H., N.I., and A.O. designed the study. M.H., K.I., S.M., T.Tatebe, S.T., Y.D., T.Tomishima, A.Honda, M.O., A.S., R.Y., M.F., T.M., and A.O. performed the experiments. M.H., M.T., A.Hasegawa, and A.O. analyzed the data. M.H. and A.O. wrote the article. All authors have reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hirose, M., Inoue, K., Matoba, S. et al. Disruption of insulin receptor substrate 2 (IRS2) causes non-obese type 2 diabetes with β-cell dysfunction in the golden (Syrian) hamster. Sci Rep 14, 17450 (2024). https://doi.org/10.1038/s41598-024-67513-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-67513-9
- Springer Nature Limited