Abstract
The aim of this study was to evaluate the distance between the maxillary central incisor root and the incisive canal based on skeletal malocclusion classification and to analyze the morphology of the incisive canal using cone-beam computed tomography (CBCT). Skeletal malocclusion was categorized into Class I, II, and III using lateral cephalometric analysis. Measurements of the distance between the maxillary central incisor root and the incisive canal were taken at two levels: 2 mm (L1) and 4 mm (L2) superior to the labial cementoenamel junction of the maxillary central incisor. At L1, the distance was found to be closer in the Class II group compared to the Class I or Class III groups. Similarly, at L2, the Class II group exhibited a closer distance than the Class III group. Interestingly, females showed a closer distance compared to males at both L1 and L2. Further analysis revealed a significant gender difference in the Class I and III groups, but not in the Class II group. These findings emphasize the significance of evaluating the distance between the maxillary central incisor root and the incisive canal in patients with skeletal Class II malocclusion, regardless of gender.
Similar content being viewed by others
Introduction
The orthodontic treatment plan is determined based on various factors such as the skeletal malocclusion pattern, arch length discrepancy and the anterior–posterior position of the teeth. Skeletal malocclusion is classified into Class I, Class II, and Class III malocclusions based on the anterior–posterior position of the maxilla and mandible in relation to cranial base. Skeletal Class I malocclusion is characterized by the mandibular base being positioned vertically aligned beneath the maxillary base, with neither the maxilla nor mandible protruding excessively anteriorly or posteriorly relative to the cranial base. In the case of Class II malocclusion, the maxilla is positioned anteriorly compared to the mandible, while in Class III malocclusion, the mandible is positioned anteriorly compared to the maxilla1. Additionally, Class II malocclusion can be divided into division 1 and division 2. Cases where the maxillary incisors are inclined labially are classified as division 1, and cases where the maxillary incisors are lingually inclined are classified as division 22,3. Class II division 1 can also be classified into seven categories according to the type of mandibular retrusion4. In the case of Class II malocclusion, compensatory treatment options may include extraction of maxillary premolars and subsequent posterior retraction of the anterior maxillary teeth to compensate for jaw disharmony5. In contrast, in instances of Class III malocclusion, compensatory therapeutic strategies may entail the extraction of mandibular premolars followed by posterior retraction of the anterior mandibular dentition6. Accordingly, the treatment plan may differ based on the type of skeletal malocclusion. Therefore, it is important to classify patients according to skeletal malocclusion classification. This classification needs to be carefully considered because the relative position of the upper and lower teeth determines occlusal stability, which is related to muscular performance7.
The maxillary central incisors play an important role in pronunciation, function, and aesthetics. From an aesthetic perspective, it is important to set the position of the maxillary central incisors during orthodontic treatment. Depending on the orthodontic treatment plan, changes in the anterior and posterior position of the maxillary central incisors may be necessary. When moving the maxillary central incisors posteriorly, the structure that orthodontist should pay most attention to is the incisive canal8.
The incisive canal is a long and slender structure located posteriorly to the roots of the maxillary central incisors in the mid-palatal region of the maxilla, surrounded by thick cortical bone. The incisive canal connects the oral and nasal cavities, containing the nasopalatine nerve and arteries9. The morphology of the incisive canal is known to vary not only based on race but also on an individual basis10,11,12,13. The incisive canal can undergo remodeling as a result of posterior retraction of teeth during orthodontic treatment. However, it is known that during the process of posterior retraction, the maxillary central incisors may come too close to the incisive canal, and there is a possibility of contact or invasion of the maxillary central incisors into the incisive canal. Root resorption can occur as a reaction between the tooth and the surrounding periodontal tissues, and research has been conducted on this phenomenon14. In severe cases, it can lead to resorption of the roots of the maxillary central incisors15,16,17. Root resorption is one of the significant side effects of orthodontic treatment. Therefore, orthodontists need to assess the morphology of the incisive canal and determine the extent of posterior movement based on the distance between the incisive canal and the roots of the maxillary central incisors before initiating orthodontic treatment18,19.
Lateral cephalometric radiographs are commonly used to plan orthodontic treatment. These radiographs assess the evaluation of craniofacial skeletal structures using landmarks and reference planes depicted on anatomical structures. However, lateral cephalometric radiographs are two-dimensional images, and many structures appear superimposed. As a result, it is difficult to accurately evaluate the distance between the maxillary central incisor root and the incisive canal. On the other hand, cone-beam computed tomography (CBCT) provides three-dimensional volumetric images, allowing for an accurate assessment of the distance between the root of the maxillary central incisor and the incisive canal20.
When planning orthodontic treatment, it is crucial to carefully consider the distance between the maxillary central incisor root and the incisive canal. Ignoring this distance during maximum anterior retraction can lead to root resorption, making its evaluation essential for successful orthodontic outcomes. This study aims to measure the distance between the maxillary central incisor root and the incisive canal according to different skeletal malocclusion classifications and to analyze the morphology of the incisive canal using CBCT images. Through this, we aim to identify the characteristics of each skeletal malocclusion type and provide valuable information for orthodontic treatment planning. Additionally, this study examines whether there are any gender-based differences.
Materials and methods
Study subjects
This study was approved by the Institutional Review Board (IRB) at Chosun University Dental Hospital (IRB No: CUDHIRB 2205 002). It involved a total of 190 patients (85 males and 105 females) who visited Chosun University Dental Hospital for orthodontic diagnosis between 2021 and 2022. Patients in the primary and mixed dentition stages (35 individuals) were excluded, focusing exclusively on those in the permanent dentition stage. The included patients ranged in age from 14 to 52 years, with an average age of 23.2 years. Patients with conditions potentially affecting the maxilla, such as cleft lip and palate or skeletal abnormalities, were excluded from the study. Additionally, patients with incomplete or low-quality CBCT images unsuitable for analysis were excluded. Following these criteria, measurements were conducted on a total of 145 patients.
Data acquisition
The investigation was conducted using CBCT images taken for diagnostic purposes. The CBCT images were exported in Digital Imaging and Communications in Medicine (DICOM) format and imported into InVivoDental 5.55 (Anatomage, San Jose, CA, USA) for analysis.
Lateral cephalometric analysis
The patient's mid-sagittal plane was aligned through multi-planar reconstruction on the CBCT, and lateral cephalometric analysis was performed. Among the lateral cephalometric analysis methods, Steiner analysis was utilized to classify skeletal malocclusion21. In Steiner analysis, the reference plane is the sella-nasion plane (SN plane), which connects the center of the sella turcica to the most anterior point of the frontonasal suture (nasion). The relationship of the maxilla to the skull is represented by the angle SNA, which is formed by connecting the sella-nasion plane (SN plane) to the deepest point on the maxilla in the mid-sagittal plane, known as A point. The relationship of the mandible to the skull is represented by the angle SNB, formed by connecting the SN plane to the most prominent point on the mandible, known as B point. The relationship between the maxilla and mandible was evaluated using the ANB angle, the difference between SNA and SNB. ANB values between 0.5° and 3.5° were classified as Class I malocclusion, ANB values greater than this range were classified as Class II malocclusion, and values smaller than this range were classified as Class III malocclusion22. Thirty participants were selected for each malocclusion group. The average ANB values for the patients included in the study were 2.3° for Class I malocclusion, 6.2° for Class II malocclusion, and -2.8° for Class III malocclusion.
Measurement of the distance between the maxillary central incisor root and the incisive canal and analysis of the shape of the incisive canal
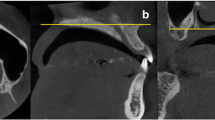
Employing the investigative approach outlined by Yu et al.19, an examination was conducted to assess the association between the root of the maxillary central incisor and the incisive canal, alongside an analysis of the morphology of the incisive canal. A mid-sagittal plane view of the incisive canal perpendicular to the Frankfort horizontal plane (FH plane) was used, passing through the anterior nasal spine (ANS), the end of the skeletal anterior nasal spine, and the posterior nasal spine (PNS), the most distal point of the hard palate. The distance between the maxillary central incisor root and the incisive canal was evaluated at two vertical references in the axial view of the maxillary anterior region (Fig. 1). The distances were assessed at 2mm above the labial cementoenamel junction (L1) and 4mm above the labial cementoenamel junction (L2) of the maxillary central incisor. The distance between the maxillary central incisor root and the incisive canal was defined as the shortest distance between the posterior border of the maxillary central incisor and the anterior border of the cortical bone of the incisive canal19.
Measurement of distance between the maxillary central incisor root and the incisive canal. (A) Sagittal view. (B) Axial view. The distance between the maxillary central incisor root and the incisive canal was defined as the shortest distance between the posterior border of the maxillary central incisor root and the anterior border of the incisive canal. L1; 2 mm above the labial cementoenamel junction of the maxillary central incisor. L2; 4 mm above the labial cementoenamel junction of the maxillary central incisor. Rt. U1; Right maxillary central incisor. Lt. U1; Left maxillary central incisor. D1; The distance between the root of the right maxillary central incisor and the incisive canal. D2; The distance between the root of the left maxillary central incisor and the incisive canal. IC; Incisive canal.
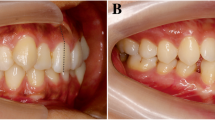
The shape of the incisive canal was classified into banana-like type, cylindrical type, funnel-like type, and hourglass-like type according to the criteria proposed by Yu et al.10,19 (Fig. 2). The classification of incisive canal shape was determined based on two-dimensional sagittal images aligned with the reference plane.
Shape of Incisive canal. (A) Banana-like type. (B) Cylindrical type. (C) Funnel-like type. (D) Hourglass-like type. According to the overall shape of the incisive canal, it was classified into four types; banana-like, cylindrical, funnel-like, and hourglass-like type based on the classification criteria presented by Yu et al.19.
Statistical analysis
The mean of the minimal distances between the incisive canal and both the right and left roots of the maxillary central incisors was computed to ascertain the closest proximity between the root of the maxillary central incisors and the incisive canal. The difference in distance between the maxillary central incisor root and the incisive canal, based on gender, was analyzed using an independent samples t-test, as it satisfied the assumption of normality. In each skeletal malocclusion group, the difference in distance between the maxillary central incisor root and incisive canal according to gender did not satisfy normality and was analyzed using the Mann–Whitney test, a non-parametric test. The difference in the distance according to skeletal malocclusion was analyzed for normality and assessed using one-way analysis of variance (ANOVA) with Tukey's post hoc analysis. The difference in distance at L1 and L2 for each skeletal malocclusion was analyzed using paired-sample T-test. For each skeletal malocclusion group, frequency analysis was performed to determine the distribution of incisive canal shapes, and cross-analysis was performed to determine the relationship between skeletal malocclusion and incisive canal shape. The data were analyzed using IBM SPSS Statistics for Windows version 27.0 (IBM, Armonk, NY, USA), applying a statistically significant difference at P < 0.05.
Informed consent
Need for Informed consent from individual participants was waived due to retrospective nature of the study by the Institutional Review Board (IRB) of Chosun University Dental Hospital.
Results
At L1, the distance between the maxillary central incisor root and the incisive canal was 1.66 ± 0.59 mm in females and 2.12 ± 0.78 mm in males. At L2, females had a mean distance of 1.85 ± 0.65 mm, while males had a mean distance of 2.41 ± 0.91 mm. The distance was closer in females compared to males at both L1 and L2, demonstrating a statistically significant difference (Table 1).
The difference in the distance between the maxillary central incisor root and the incisive canal according to gender within each skeletal malocclusion group was examined (Table 2). In the skeletal Class I malocclusion group, at L1, females showed a higher mean rank (11.88) compared to males (20.23) (Mann–Whitney U = 49.000, Z = − 2.574, P = 0.009). In the skeletal Class I malocclusion group, at L2 as well, females exhibited a higher mean rank (12.12) compared to males (19.92) (Mann–Whitney U = 53.000, Z = − 2.407, P = 0.015). In the skeletal Class III malocclusion group, at L1, females showed a higher mean rank (10.64) compared to males (18.32) (Mann–Whitney U = 51.000, Z = − 2.302, P = 0.021). In the skeletal Class III malocclusion group, at L2 as well, females exhibited a higher mean rank (11.00) compared to males (18.11) (Mann–Whitney U = 55.000, Z = − 2.130, P = 0.033) (Table 2).
In the skeletal Class I malocclusion group, the average distance between the maxillary central incisor root and incisive canal at L1 was 2.07 ± 0.77 mm and at L2 was 2.29 ± 0.82 mm. In the skeletal Class II malocclusion group, the average was 1.55 ± 0.51 mm at L1 and 1.83 ± 0.75 mm at L2. In the skeletal Class III malocclusion group, the average was 2.1 ± 0.78 mm at L1 and 2.36 ± 0.89 mm at L2. The distance between the maxillary central incisor root and the incisive canal was closer at L1 than at L2 in all skeletal malocclusion groups, showing a statistically significant difference (Table 3).
There was a difference in the distance between the roots of the maxillary central incisors and the incisive canal for each skeletal malocclusion group at L1 and L2. At L1, the distance to the incisive canal was closer in the skeletal Class II malocclusion group (1.55 ± 0.51 mm) compared to the Class I malocclusion group (2.07 ± 0.77 mm) or Class III malocclusion group (2.1 ± 0.78 mm). However, there was no statistically significant difference in the distance to the incisive canal between the skeletal Class I malocclusion group or the Class III malocclusion group at L1. At L2, the distance to the incisive canal was closer in the skeletal Class II malocclusion group (1.83 ± 0.75 mm) compared to the Class III malocclusion group (2.36 ± 0.89 mm). At L2, there existed no statistically significant disparity between the skeletal Class I malocclusion group and the Class III malocclusion group, as well as between the skeletal Class I malocclusion group and the Class II malocclusion group (Table 3).
The most common shape of the incisive canal was the cylindrical type in all skeletal malocclusion groups. It accounted for 63% of the skeletal Class I malocclusion group, 77% of the Class II malocclusion group, and 70% of the Class III malocclusion group. The banana-like type was the least common in all malocclusion groups, with no cases in the Class II malocclusion group and Class III malocclusion group. A cross-analysis was conducted to determine the relationship between skeletal malocclusion and incisive canal shape, and the result was not statistically significant (Table 4).
Discussion
The distance between the maxillary central incisor root and the incisive canal was closer in females compared to males at both L1 and L2. In the Class I and III group, there was a difference between males and females in the distance, but in the Class II group, there was no difference. At L1, for cases of Class II group, the distance was closer compared to Class I (P = 0.013) or Class III (P = 0.008) group. At L2, the Class II group exhibited a closer distance than the Class III group (P = 0.039). The most common shape of the incisive canal was cylindrical, predominant in all malocclusion groups. There was no significant relationship between skeletal malocclusion type and incisive canal shape.
In this study, the distance between the maxillary central incisor root and the incisive canal was investigated for each skeletal malocclusion group. Within all skeletal malocclusion groups, the distance between the maxillary central incisor root and the incisive canal was statistically significantly different based on vertical level. The distance at L1 was closer than at L2 within all skeletal malocclusion groups. In the study results of Arnaut et al.23, who studied the difference in distance between the incisive canal and maxillary central incisor according to vertical height, the distance was closer at the oral opening of the incisive canal. A study by Matsumura et al.18 also supports that the distance from the oral opening of the incisive canal is closer than the distance from the nasal opening. However, these studies did not consider skeletal malocclusion.
In this study, the distance at L1, proximal to the oral aperture of the incisive canal, was closer compared to L2, exhibiting a statistically significant difference. However, what differentiates this study from other studies is that it compared and analyzed the distance between the roots of the maxillary central incisors and the incisive canal according to the skeletal malocclusion classification. In particular, the patient group with skeletal malocclusion Class II at L1 had a closer distance to the incisive canal compared to Class I (P = 0.013) or Class III (P = 0.008).
Additionally, when evaluating whether there was a difference in the distance between the maxillary central incisor root and the incisive canal according to gender, the distance was statistically significantly closer in females than in males at both L1 and L2. When divided into each skeletal malocclusion group, the distances for females in the skeletal class I malocclusion group and class III malocclusion group were significantly closer than those for males. On the other hand, in the skeletal class II malocclusion group, the distance was shorter in females than in males at both L1 and L2, but this was not statistically significant.
Class II malocclusion can be classified into Class II division 1 and Class II division 2 based on the angulation of the maxillary anterior teeth24. Class II division 1 malocclusion is characterized by the maxillary molars being positioned anteriorly to the mandibular molars. It is also typified by a labial inclination of the maxillary anterior teeth. Conversely, Class II division 2 malocclusion is characterized by a severe lingual inclination of the maxillary anterior teeth2,3. In cases of Class II division 1 malocclusion, where the maxillary anterior teeth exhibit a labial inclination, there is a higher possibility that the roots of the maxillary central incisors may be closer to the incisive canal when considering the distance from the incisive canal behind the roots of the maxillary central incisors. In skeletal Class II malocclusion, a large amount of retraction of maxillary incisors is frequently performed with the extraction of maxillary premolars as a camouflage treatment5. If the roots of the maxillary central incisors invade the incisive canal, resorption of the roots may occur15,16,17. Therefore, evaluating the distance between the maxillary central incisor root and the incisive canal is important in treatment planning for Class II malocclusion patients.
The closer measurement of the distance between the maxillary central incisor root and the incisive canal in skeletal Class II malocclusion group in our study suggests that the labioversion of the maxillary central incisors contributes to their proximity to the incisive canal. However, in this study, patients with skeletal Class II malocclusion were not further classified into Class II division 1 or Class II division 2, so additional research is needed.
After maximum anterior retraction, remodeling of the incisive canal has been reported25. Approximately one-fourth of cases showed remodeling of the Incisive canal. Remodeling group demonstrated less apical root resorption. However, since remodeling is difficult to predict, it remains important to pay attention to the distance to the incisive canal.
With the assumption that differences in the shape of the incisive canal may affect the distance between the maxillary central incisor root and the incisive canal, we conducted an investigation into the incisive canal shape for each skeletal malocclusion group. The cylindrical type accounted for most of the skeletal Class I malocclusion (63%), Class II malocclusion (77%), and Class III malocclusion (70%). The cross-analysis of skeletal malocclusion and incisive canal shape revealed no statistically significant association, indicating no correlation between skeletal malocclusion and incisive canal shape. Previous studies examining incisive canal morphology in European populations did not classify based on skeletal malocclusion, but the findings differed from our study. In that research, the funnel-like type was predominant, followed by the cylindrical, hourglass-like, and banana-like types23. In a study investigating whether the morphology of the incisive canal, located in the palate, varies according to facial profile, considering the influence of maxillary development, it was concluded that there is no difference in incisive canal morphology between different facial profiles, whether short-face or long-face profiles9.
As such, the shape of the incisive canal can vary depending on race and individual differences. However, because this study only investigated Koreans, there may be differences in the distance in other racial groups with different incisive canal shape. Therefore, findings from more diverse ethnic groups are needed. Additionally, there is a difference in the size of the incisive canal according to age, and some studies have reported that the size of the incisive canal is larger in older people compared to younger people9,26. The wide age range of the participants is a limitation of our study, and further research is needed to investigate differences by age.
Conclusions
This study aimed to assess the distance between the maxillary central incisor root and the incisive canal using cone-beam computed tomography (CBCT) images, categorized by skeletal malocclusion. The results revealed that in skeletal Class II malocclusion, the distance between the maxillary central incisor root and the incisive canal was significantly closer compared to other malocclusion groups. Notably, within the skeletal Class II malocclusion group, gender did not significantly influence this distance at both vertical heights, whereas females generally exhibited a closer distance compared to males in all other malocclusion groups. In this study, the shape of the incisive canal was predominantly cylindrical, and there was no significant correlation between skeletal malocclusion and the shape of the incisive canal. The results of this study highlight that the distance between the maxillary central incisor root and the incisive canal is particularly close in skeletal Class II malocclusion group. For patients with skeletal Class II malocclusion, regardless of gender, accurate assessment of this distance using CBCT images is crucial for formulating personalized orthodontic treatment plans. In conclusion, customized orthodontic strategies tailored to specific skeletal malocclusion types, guided by comprehensive CBCT evaluations, are essential for optimizing treatment effectiveness and ensuring treatment stability.
Research involving human participants and/or animals
This retrospective study was conducted with the approval of the Research Ethics Committee of Chosun University Dental Hospital (approval number, CUDHIRB-2205 002) and followed medical protocol and ethics as outlined in the Declaration of Helsinki.
Data availability
The datasets used and analysed during the current study available from the corresponding author on reasonable request.
References
Proffit, W. R., Fields, H. W., Larson, B. & Sarver, D. M. Contemporary orthodontics-e-book. (Elsevier Health Sciences, 2018).
Al-Khateeb, E. A. & Al-Khateeb, S. N. Anteroposterior and vertical components of class II division 1 and division 2 malocclusion. Angle Orthod. 79, 859–866 (2009).
Cleall, J. F. & Begole, E. A. Diagnosis and treatment of class II division 2 malocclusion. Angle Orthodontist 52(1), 38–60 (1982).
Perillo, L. et al. Class II malocclusion division 1: a new classification method by cephalometric analysis. Eur. J. Paediatr. Dent. 13, 192 (2012).
Naragond, A., Kenganal, S. & Sagarkar, R. Orthodontic camouflage treatment in an adult patient with a class ii, division 1 malocclusion–a case report. J. Clin. Diagnostic Res. JCDR 7, 395 (2013).
Ning, F. & Duan, Y. Camouflage treatment in adult skeletal Class III cases by extraction of two lower premolars. Korean J. Orthodontics 40, 349–357 (2010).
Cutroneo, G. et al. Expression of muscle-specific integrins in masseter muscle fibers during malocclusion disease. Int. J. Mol. Med. 30, 235–242 (2012).
Al-Rokhami, R. K. et al. Proximity of upper central incisors to incisive canal among subjects with maxillary dentoalveolar protrusion in various facial growth patterns: a CBCT analysis. Angle Orthodontist 92(4), 529–536 (2022).
da Costa, E. D. et al. Morphological evaluation of the nasopalatine canal in patients with different facial profiles and ages. J. Oral Maxillofac. Surg. 77, 721–729 (2019).
Etoz, M. & Sisman, Y. Evaluation of the nasopalatine canal and variations with cone-beam computed tomography. Surg. Radiologic Anatomy 36, 805–812 (2014).
Acar, B. & Kamburoğlu, K. Morphological and volumetric evaluation of the nasopalatinal canal in a Turkish population using cone-beam computed tomography. Surg. Radiol. Anatomy 37, 259–265 (2015).
Özçakır-Tomruk, C., Dölekoğlu, S., Özkurt-Kayahan, Z. & İlgüy, D. Evaluation of morphology of the nasopalatine canal using cone-beam computed tomography in a subgroup of Turkish adult population. Surg. Radiol. Anat. 38, 65–70 (2016).
Oyuntugs, R. et al. Evaluation of the morphology of the nasopalatine canal using cone beam computed tomography. Stomatologiia 101, 66–69 (2022).
Piancino, M. G. et al. From periodontal mechanoreceptors to chewing motor control: a systematic review. Arch. Oral Biol. 78, 109–121 (2017).
Chung, C. J., Choi, Y. J. & Kim, K.-H. Approximation and contact of the maxillary central incisor roots with the incisive canal after maximum retraction with temporary anchorage devices: report of 2 patients. Am. J. Ortho. Dentofac. Orthopedics 148, 493–502 (2015).
Pan, Y. & Chen, S. Contact of the incisive canal and upper central incisors causing root resorption after retraction with orthodontic mini-implants: a CBCT study. Angle Orthodontist 89, 200–205 (2019).
Imamura, T., Uesugi, S. & Ono, T. Unilateral maxillary central incisor root resorption after orthodontic treatment for Angle Class II, division 1 malocclusion with significant maxillary midline deviation: A possible correlation with root proximity to the incisive canal. Korean J. Orthodontics 50, 216–226 (2020).
Matsumura, T., Ishida, Y., Kawabe, A. & Ono, T. Quantitative analysis of the relationship between maxillary incisors and the incisive canal by cone-beam computed tomography in an adult Japanese population. Progr. Orthodontics 18, 1–6 (2017).
Yu, J. H. et al. Morphologic changes of the incisive canal and its proximity to maxillary incisor roots after anterior tooth movement. Am. J. Orthodontics Dentofac. Orthopedics 161(396–403), e391 (2022).
Costa, E. D. et al. Comparison of distance of upper central incisor root and incisive canal in different sagittal and vertical skeletal patterns and sex: a retrospective CBCT study. Int. Orthodontics 19, 462–470 (2021).
Steiner, C. C. Cephalometrics in clinical practice. Angle Orthodontist 29, 8–29 (1959).
Institution, B. S. British standard glossary of dental terms. (British Standards Institution, 1983).
Arnaut, A. et al. The shape of nasopalatine canal as a determining factor in therapeutic approach for orthodontic teeth movement—a CBCT study. Diagnostics 11, 2345 (2021).
Uzuner, F. D., Aslan, B. I. & Dinçer, M. Dentoskeletal morphology in adults with Class I, Class II Division 1, or Class II Division 2 malocclusion with increased overbite. Am. J. Orthodontics Dentofac. Orthopedics 156(248–256), e242 (2019).
Chung, C. J., Nguyen, T., Lee, J. H. & Kim, K. H. Incisive canal remodelling following maximum anterior retraction reduces apical root resorption. Orthodontics Craniofac. Res. 24, 59–65 (2021).
Soumya, P., Koppolu, P., Pathakota, K. R. & Chappidi, V. Maxillary incisive canal characteristics: a radiographic study using cone beam computerized tomography. Radiol. Res. Pract. 2019, 6151253 (2019).
Acknowledgements
This research was supported by research fund from Chosun University Dental Hospital, 2022.
Author information
Authors and Affiliations
Contributions
MK Jang collected data and prepared figures, wrote the main manuscript text. SR Jeong designed study, developed project and edited manuscript. MK Jih and SH Lim analyzed data and edited manuscript. SK Yu developed project, analyzed data, edited manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jang, M., Yu, SK., Lim, SH. et al. Radiologic study of the distance between the maxillary central incisor root and the incisive canal according to skeletal malocclusion classification. Sci Rep 14, 16875 (2024). https://doi.org/10.1038/s41598-024-68014-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-68014-5
- Springer Nature Limited