Abstract
To determine the presence of a consistent osseous corridor from the lateral-posterior aspect of the anterior inferior iliac spine to the sacral wing that could be used for safe trans percutaneous screw fixation for pelvic fragility fractures of the iliac wing and fracture dislocations of the sacroiliac joint (FFP types IIIa and IIIb). Computed tomography (CT) scans were obtained from 100 patients and imported to Mimics software for 3D reconstruction. Then, a cylinder was drawn to imitate the modified LC-II screw and adjusted to a maximum radius and length to obtain the feasible region. Thirteen parameters of the osseous corridor of the modified LC-II screw were measured. Differences between sex groups were compared, and significant statistical correlations were carefully studied to determine potentially important clinical relationships. The records of patients with FFP type IIIa and IIIb fragility fractures of the pelvis were extracted from our hospital. Patients who underwent modified LC-II screw fixation, LC-II screw fixation or reconstruction plate fixation were included. Patients’ operative characteristics and complications were recorded at follow-up. Fracture reduction quality was assessed using the Matta standard. Functional outcomes were evaluated using the Majeed grading system. The mean maximum diameters of the osseous corridors of the modified LC-II screw in males and females were 12.73 and 10.83 mm, respectively. The mean maximum lengths of the osseous corridors of the modified LC-II screw in males and females were 96.37 and 93.37 mm, respectively. In the treatment of patients with FFP IIIa and FFP IIIb fractures, the group of treatment by the modified LC-II screws fixation was shown significantly shorter operative time and fewer intraoperative blood loss in comparison to that by the reconstruction plates. In the present study, all the males and females had a complete osseous corridor of the modified LC-II screw. The clinical results of the patients who were treated with modified LC-II screw fixation suggest that the novel method has a good preliminary outcome.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
In 2002, Starr et al.1 reported the use of internal fixation for iliac wing fractures via the use of an LC-II screw inserted along the anterior inferior iliac spine (AIIS) to the posterior inferior iliac spine (PIIS), which has been widely used to treat adult iliac fractures for 20 years. Recently, it has been widely used to treat FFP type IIIa pelvic fractures. However, due to the increased risk of loosening and failure of internal fixation with LC-II screws in elderly patients with osteoporosis1,2, we proposed a modified LC-II screw placement method involving sacroiliac joint fixation, resulting in 3-layer cortical fixation, which heightens fixation stability and facilitates early mobility. The entry point of the osseous corridor of the modified LC-II screw is more lateral and enters the sacroiliac joint through the iliac osseous corridor at an angle of 5°–10° to the osseous corridor of the LC-II screw. In addition, the osseous corridor of the modified LC-II screw can avoid the influence of the curvature of the iliac fossa on the osseous corridor by adjusting the distance of the entry point to the lateral side. At the same time, the path of the osseous corridor of the modified LC-II screw is shorter and does not pass through the curved bone surface of the iliac fossa, thus reducing the risk of the in–out-in phenomenon.
This study aimed to determine the presence, dimensions and limits of a ‘‘safe zone’’ osseous corridor through which a percutaneous screw can be placed from the lateral-posterior aspect of the anterior inferior iliac spine to the sacral wing in the male and female pelvis and to which the osseous corridor can be applied in clinical practice.
Materials and methods
All procedures performed in this study involving human participants were in accordance with the Third Affiliated Hospital of Southern Medical University Research/Ethics Committee approval (NO. 201704006). All personal data are published with the person’s informed consent.
Images of 50 adult male and 50 adult female patients who underwent computed tomography (CT) scans of their pelvis for unrelated medical reasons between October 2022 and April 2023 were included in the study. Investigations that revealed obvious degeneration or traumatic or osteolytic conditions were excluded. Investigations with a slice thickness greater than 2.0 mm were excluded.
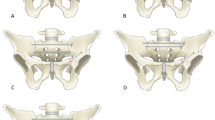
Building the osseous corridor
Mimics 19.0 (Materialise, Leuven, Belgium) software was used for multiplanar reconstruction and trajectory placement, allowing unrestricted rotation and transparency of the pelvis. Specifically, the presence and topography of an osseous corridor through the ilium from the lateral-posterior aspect of the anterior inferior iliac spine to the sacral wing, which would safely accommodate a virtual trans percutaneous screw of 7.3 mm, were determined. The osseous corridor was defined as complete osseous continuity through the ilium from the lateral-posterior aspect of the anterior inferior iliac spine to the sacral wing of at least 7.3 mm in diameter without cortical breach of the anterior, posterior, superior or inferior borders of the ilium and sacrum bodies (Fig. 1).
After the reconstruction of the coordinate system with the virtual osseous corridor of the modified LC-II screw, it was repeatedly confirmed that the edge of the osseous corridor did not penetrate the bone on the continuous CT images of the sagittal plane, coronal plane and horizontal planes. The diameter and length measured before the osseous corridor passed through the bone cortex were the actual maximum usable diameter and length, respectively (Fig. 2).
Specific measurements
3-Matic 13.0 (Materialise, Leuven, Belgium) software was used to obtain measurements for each simulated screw trajectory. These measurements included angles (∠α, ∠β, and ∠γ) between the osseous corridor and the coronal, sagittal, and horizontal planes of the body. Distances from the bony entry point of the osseous corridor to the anterior inferior iliac spine (AI), anterior superior iliac spine (AS), top of the acetabulum (AC), and large sciatic notch (AN) were also measured. Additional measurements included the vertical distance (Dv1) and horizontal distance (Dh1) between the skin entry point of the osseous corridor and the anterior superior iliac spine, as well as the angles (∠LPM and ∠LPM') of the osseous corridor with the pelvic median line in the anterior–posterior and inlet views (Fig. 3).
(a) Construction of the human coronal, sagittal, and horizontal planes, (b–d) measurement of the angle between the osseous corridor of the modified LC-II screw and the coronal, sagittal, and horizontal planes, (e) the relationship between the bone entry point of the osseous corridor of the modified LC-II screw and the anterior superior iliac spine, anterior inferior iliac spine, acetabular roof, and greater sciatic notch, (f–h) the relationship between the skin entry point of the osseous corridor of the modified LC-II screw and the anterior superior iliac spine, (i,j) the angle between the osseous corridor of the modified LC-II screw and the median line of the pelvis in the anterior–posterior and inlet views.
Patient screening and selection
This study was approved by our Institutional Review Board (No. 201704006). From January 2011 to January 2023, 360 patients with pelvic fractures at the Third Affiliated Hospital of Southern Medical University were selected. According to the FFP classification for pelvic fracture and considering the mechanism of injury in each patient, three experienced physicians screened FFP IIIa and IIIb fragility fractures of the pelvis by using pelvic anterior–posterior, inlet, and outlet plain, computed tomography (CT), and three-dimensional imaging.
The inclusion criteria were (1) ≥ 60 years of age; (2) pelvic pain, tenderness, hip dysfunction, or local swelling; (4) FFP type IIIa and IIIb fragility fractures of the pelvis confirmed using radiography and computed tomography (CT); (5) surgical treatment in our department; (6) modified LC-II screw fixation, LC-II screw fixation or reconstruction plate fixation; and (7) at least six months of follow-up. The exclusion criteria were (1) age < 60 years; (2) history of falling from a height or a traffic accident; (3) fractures other than FFP type IIIa and IIIb fragility fractures of the pelvis; (3) serious soft tissue injury (Morel-Lavallée); (4) serious multiple injuries; or (5) stupor.
We searched the medical records for patients with FFP type IIIa and IIIb fragility fractures of the pelvis who were surgically treated with modified LC-II screw fixation (group I), LC-II screw fixation (group II) or reconstruction plate fixation (group III).
The technical points of the modified LC-II screw application
For FFP type IIIa and IIIb fractures, fracture reduction is performed by pulling the affected lower limb and performing internal and external rotation of the iliac wing. When reduction is difficult, iliac crest Schanz screws can be used to assist reduction. Once C-arm fluoroscopy confirms successful reduction, an oblique incision approximately 2 cm in length is made with the anterior inferior iliac spine as the central point. Subsequently, the subcutaneous soft tissue is bluntly separated to expose the anterior inferior iliac spine along with its outer and lower bone surfaces, taking care to protect the lateral femoral cutaneous nerve. Insert the needle slightly higher than the upper edge of the acetabulum and about 2 cm lateral to the anterior inferior iliac spine, passing through the osseous corridor of the iliac bone, crossing the sacroiliac joint, and reaching the sacral wing. It is appropriate for the guide needle to have just passed through the sacroiliac joint 1 cm. The Teepee position is first visualized (Fig. 4a) during the operation, with the needle inserted diagonally inward towards the front edge of the sacroiliac joint. The guide needle is advanced within the iliac bone plate barrier by striking it with a bone hammer, crossing the fracture line and sacroiliac joint to ensure that the screws are within the iliac plate barrier. The iliac exit position (Fig. 4b) is used to monitor screw insertion depth and entry into the sacroiliac joint to prevent penetration of the greater sciatic foramen and ensure avoidance of the sacral foramen and posterior sacral canal. The lateral view of the pelvis (Fig. 4c) is utilized to confirm the safe distance and insertion depth between the screw and the greater sciatic foramen. The entrance position of the pelvic obturator hole (Fig. 4d) is observed to check the depth of screw insertion into the sacroiliac joint, ensuring that the screw does not penetrate through the anterior sacrum. The appropriate guide pin insertion path is confirmed through the mentioned fluoroscopic positions. Following depth measurement, a 7.3 mm hollow screw is inserted along the guide pin.
(a) Fluoroscopic Teepee position shows the anterior inferior iliac spine angled inward towards the front edge of the sacroiliac joint, with the needle inserted. (b) The iliac exit position is used to observe the depth of screw insertion and prevent screw penetration into the ischial hole. (c) The lateral view of the pelvis confirms the safe distance between the screw and the greater ischial foramen. (d) The obturator entrance position of the pelvis is used to observe the depth of the screw entering the sacroiliac joint.
Indicators of outcome
The primary outcomes were the Majeed score3 and the Matta score4 for evaluating fracture reduction outcomes. The secondary outcomes were operative time, intraoperative blood loss, length of hospital stay, time to weight bearing, and rates of complications (deep vein thrombosis, deep infection, superficial infection, dislocation and mortality).
Statistical analysis
The statistical analysis was performed using SPSS 25.0. Continuous data are presented as the mean ± standard deviation, while categorical data are presented as absolute numbers and percentages. All the measurements were independently analyzed by three observers with software. Independent sample t tests were used to compare the osseous corridor of the modified LC-II screw. The Shapiro‒Wilk test was used to assess the normality of the clinical trial data. The Kruskal‒Wallis H test was used to evaluate variables such as age, OR duration, and blood loss. Pearson’s chi-square test or Fisher's exact test was used to assess differences in the counts among the three groups. A p value < 0.05 was considered to indicate statistical significance. Box-plots were generated to illustrate differences in operative time and intraoperative bleeding among the three surgical methods for FFP IIIa fractures.
Ethics approval and consent to participate
This study was approved by the ethical board of the Third Affiliated Hospital of Southern Medical University (approval number 201704006). Informed consent was obtained from all included participants.
Results
The osseous corridor of the modified LC-II screws can be successfully imitated in all 3D digital images. The parameters of the osseous corridor of the modified LC-II screw are summarized in Table 1, while Table 2 compares the parameters of the osseous corridor of the modified LC-II screw on different sides. Measurements by the three independent investigators showed no significant differences (P = 0.754), with an intraclass correlation coefficient of 0.917.
Distance and angle parameters
The measurements of the distance parameters are summarized in Table 1. The maximum diameter of the osseous corridor of the modified LC-II screw was 12.73 ± 1.15 mm in men and 10.83 ± 1.11 mm in women. Women had a significantly shorter maximum length. Similarly, the mean maximum length distances for the osseous corridor in males and females were 96.37 ± 6.15 and 93.37 ± 5.77 mm, respectively. The distance of the AN was significantly shorter in women than in men (Table 1). However, there were no significant differences in the osseous corridor of the modified LC-II screw between the left and right sides of the pelvis (Table 2).
The mean angles between the osseous corridor of the modified LC-II screw and the sagittal plane in males and females were 34.94 ± 3.16° and 33.31 ± 3.6°, respectively. The mean angles between the osseous corridor of the modified LC-II screw and the horizontal plane were 35.57 ± 4.74° in men and 38.6 ± 5.52° in women. The angle of the osseous corridor to the pelvic median line in the anterior–posterior and inlet views was significantly smaller in women than in men.
This study revealed significant sex-specific differences in the osseous canal. Men had longer osseous corridors and greater distances between the large sciatic notch and the osseous corridor entry point. Women had a smaller osseous canal diameter than men, and the osseous corridor was closer to the sagittal plane. In the pelvic inlet position, the osseous canal was closer to the median pelvis in women. These differences were statistically significant (p < 0.01).
Patients’ baseline characteristics
In this study, the osseous corridor of the modified LC-II screw fixation was used for closed reduction in 27 patients (Group I), the osseous corridor of the LC-II screw fixation was used for closed reduction in 12 patients (Group II), and reconstruction plate fixation was used for open reduction in 23 patients (Group III). Demographics, injury patterns, and anesthesia ASA grades did not significantly differ between the groups (P > 0.05). However, there was a significant difference in fracture classification among the groups (P < 0.05), as the osseous corridor of the LC-II screw fixation was available only for FFP IIIa fractures. (Table 3).
Clinical course
This study focused on the treatment of FFP IIIa fractures (Table 4). Group I included 15 patients with operation times ranging from 25–70 (39.7 ± 11.9) minutes. Group II included 12 patients with operation times ranging from 26 to 70 (45.0 ± 13.0) minutes. Group III included 14 patients with operation times ranging from 50 to 150 (88.6 ± 28.5) minutes. The osseous corridor of the modified LC-II screw fixation group or the osseous corridor of the LC-II screw fixation group had significantly shorter operation times than did the open reduction group (p < 0.01, Fig. 5). In addition, Group I had 15 patients with 20–40 (30.9 ± 7.1) ml of blood loss, Group II had 12 patients with 20–39 (29.2 ± 7.7) ml of blood loss, and Group III had 14 patients with 220–726 (448.4 ± 153.3) ml of blood loss. The blood loss in the osseous corridor of the modified LC-II screw fixation and the osseous corridor of the LC-II screw fixation groups were significantly less than the open surgery group, with statistical significance (p < 0.01, Fig. 6).
In the treatment of patients with FFP IIIb fractures, the mean operation time (p < 0.01) and intraoperative blood loss (p < 0.001) were significantly lower when the surgery involved closed reduction and fixation within the osseous corridor of the modified LC-II screw fixation (Table 5).
Follow‑up
All 62 patients were successfully followed up for an average of 22 months (range: 6–36 months). Five implant-related problems (8.0%) and six wound-healing problems (9.6%) were noted. Implant loosening or breakage did not cause a loss of reduction (Table 6).
For FFP IIIa fractures, there was no significant difference in the X-ray reduction evaluation criteria of Matta among the three groups (P > 0.05; Table 4). For FFP IIIb fractures, there was no significant difference in the X-ray reduction evaluation criteria of Matta between the two groups (P > 0.05; Table 5). There was no significant difference in the Majeed score among the patients with FFP IIIa fractures (P > 0.05; Table 4). There was no significant difference in the Majeed score (P > 0.05, Table 5) between patients with FFP IIIb fractures in either group.
Typical case
The patient was a 80-year-old woman, who fell while walking at home and suffered pain and limited range of motion in her left pelvis. She was diagnosed with Fragility Fracture of the Pelvis in the Elderly (FFP Type IIIb). No obvious surgical conscription was found in the preoperative examination and examination. Under tracheal intubation and general anesthesia, closed reduction and internal fixation of pelvic fracture were achieved. The posterior ring was fixed with 2 modified LC-II screw. The anterior ring was fixed with INFIX. The operative time was 70 min and intraoperative bleeding was 50 ml. Postoperative radiological examination showed that the modified LC-II screw crossed the sacroiliac joint and into the sacral wing (Fig. 7).
An 80-year-old woman sustained FFP IIIb. (a–c) Pelvic orthogonal, entry and exit positions suggest left iliac fracture combined with sacroiliac joint injury and left suprapubic branch fracture; (d–f) three-dimensional reconstruction of the pelvic fracture with clear fracture line visible on the iliac wing; (g–i) anterior and posterior pelvic rings fixed with modified LC-II 7screws and INFIX internal fixation; (j–l) three-dimensional reconstruction of the internal fixator shows that the modified LC-II screw is located in the bony canal across the sacroiliac joint into the sacral wing for fixation without entering the sacral foramen or spinal canal.
Discussion
Fragility fractures of the pelvis typically result from simple falls from a standing position5,6,7; therefore, fracture displacement is mild. In Chinese clinical practice, conservative treatment of elderly patients with pelvic fractures is mostly performed by strict bed rest. However, fragility fractures of the pelvis have a high long-term mortality rate, and conservative treatment can have a serious impact on patients’ functional recovery, self-care, and psychological well-being8,9. The most important factor in the management of elderly patients with pelvic ring injuries is the preservation of their mobility or the active management of the consequences of immobility10,11,12. Evidence suggests that minimally invasive techniques for internal fixation of unstable pelvic fractures in elderly individuals should be used as early as possible to support early activity, self-care, fracture healing, pain relief, and osteoporosis management13,14. The advantages of the percutaneous screw technique in minimally invasive fixation include minimal surgical trauma and reliable fixation1,15,16. The success of screw placement depends on the use of fast, safe, and accurate screw placement, which requires a thorough understanding of osseous corridor parameters. Pelvic imaging anatomical studies and cadaveric anatomical studies are the main research methods currently used. Researchers have utilized digital software to construct, analyze, and measure bony fixation osseous corridors in the pelvis and acetabulum17,18,19. Tian X et al. utilized cadaveric anatomical measurements, imaging measurements, and reconstructed pelvic 3D model measurements on 18 pelvic specimens. The results showed that the parameters of the LC-II screw tract were consistent across all three measurement methods. Therefore, the use of digital software is a feasible approach for planning, analyzing, and measuring the parameters of the osseous corridor of modified LC-II screws20. In this study, a transparent pelvic model was used to confirm the complete insertion of the osseous corridor into the bone from various angles. The osseous corridor of the modified LC-II screw was reconstructed within the bone's coronal, sagittal, and horizontal planes, providing precise and consistent confirmation of the channel's existence. The study revealed no significant differences in the maximum diameter or length of the osseous corridor of the modified LC-II screw between the left and right sides of the same sex (P > 0.05). However, significant differences were observed between males and females (P < 0.05), which may be attributed to physiological differences in pelvic structure between the sexes.
FFP III fractures have clear surgical indications due to anterior–posterior ring injury, pelvic ring instability, and a low rate of spontaneous fracture union21. Both the osseous corridor of the LC-II screw and the osseous corridor of the modified LC-II screw may experience corridor narrowing due to fracture displacement, but pelvic fragility fractures typically involve bone destruction without ligament damage, resulting in insignificant displacement7. The technical technique of modified LC-II screw fixation offers a wider range of nailing and allows for adjustment of the nailing point position to effectively reduce the impact of displacement, making this technique more versatile and adaptable to varying fracture scenarios than the traditional method of LC-II screw fixation. This study confirmed that the osseous corridor of the modified LC-II screw could be planned for all 100 pelvises tested, with a minimum osseous corridor diameter of 8.60 mm, suggesting the routine use of 7.3 mm hollow screws in all patients.
For FFP III fractures without significant displacement, Rommens21 recommended minimally invasive fixation of the anterior and posterior rings. Iliac fractures that are not significantly displaced or can be fixed through closed reduction can be treated with LC-II screw fixation. However, due to pelvic osteoporosis, there is a risk of internal fixation failure and screw withdrawal1,2. To improve stability, clinicians can consider increasing the screw diameter, injecting bone cement to improve local hardness, and optimizing the screw placement path. Nakayama et al.22 proposed a new method of locking LC-II screws with retrograde anterior column screws, which was reported to increase the stability of the fracture, and a good initial clinical effect was obtained. However, locked screws require a long learning curve due to the high accuracy and prospective requirements. Based on the characteristics of spontaneous fusion and sclerosis of the sacroiliac joint of the pelvis in elderly individuals23,24, we propose the use of the osseous corridor for modified LC-II screw fixation. In comparison, the osseous corridor of the modified LC-II screws is designed to penetrate three layers of the bone cortex in the ilium and sacrum, as well as the sclerotic sacroiliac joint, to improve screw retention and stability. The screw placement method is similar to that used for traditional LC-II screws, but the learning curve is shorter. Our preliminary clinical results indicate that this approach provides reliable fixation, early mobility, and pain relief.
This study evaluated the treatment outcomes of 14 patients with FFP IIIa pelvic fractures treated with a reconstruction plate after open reduction via the lateral rectus approach (LRA). According to Matta, the percentage of excellent and good patients was 92.9%, and according to Majeed, it was 85.7%. For FFP IIIb pelvic fractures in 9 patients, the percentage of excellent and good fractures according to Matta was 66.7%, and according to Majeed, it was 77.8%. Open surgery is an option but carries risks, especially for elderly patients with cardiopulmonary insufficiency. The study included 41 elderly patients with FFP IIIa, and the operation times of the modified LC-II screw fixation group and the LC-II screw fixation group were significantly shorter than that of the open surgery group (p < 0.0001). Both modified LC-II screw fixation and LC-II screw fixation resulted in significantly less operative hemorrhage than did open surgery (p < 0.0001). Although the open surgery group had higher rates of excellent and good outcomes according to Matta, both modified LC-II screw fixation and LC-II screw fixation reduced surgical bleeding and operation time, ultimately reducing surgical risk for patients with FFP III fractures.
Because the osseous corridor of the traditional LC-II screw runs between the AIIS and the PIIS, the LC-II screw fixation group is suitable only for FFP IIIa pelvic fractures; although it is easy to place the screw in the teardrop position, there is a risk of cutting the medial cortex of the iliac bone due to the curvature of the iliac fossa (in–out-in)1. The insertion point of the osseous corridor of the modified LC-II screw is positioned laterally, and the screw enters the sacroiliac joint through the iliac diploe at a slight angle of 5°–10°, which is different from the traditional osseous corridor. By adjusting the outer deviation distance of the insertion point, the osseous corridor of the modified LC-II screw can avoid the impact of the iliac fossa radian on the screw placement channel. The insertion point of the osseous corridor of the modified LC-II screw is more lateral than the osseous corridor of the traditional LC-II screw when treating FFP IIIa fractures, which lead to a potential risk of iatrogenic fracture due to the nail entry point being close to the fracture line, theoretically. However, the distance between the entry point of the osseous corridor of the modified LC-II screw and the dorsal fracture line is actually relatively far, reducing the risk can be achieved by adjusting the position of the insertion point according to the fracture line. The insertion point of the osseous corridor of the modified LC-II screw is located near the inferior gluteal line, which offers stronger bone support, reducing the risk of iatrogenic fractures.
The osseous corridor of the modified LC-II screw is radiologically similar to that of the S2-AL (S2AI) screw, and both of these methods involve sacroiliac joint fixation25. The osseous corridor of the modified LC-II screw can be adjusted based on the pelvic morphology and fracture line, and the addition of multiple layers of cortex fixation can enhance the stability of both the fracture and the sacroiliac joint. This modification is particularly suitable for treating FFP IIIb fractures that involve the sacroiliac joint. Our team proposed the use of the osseous corridor of the modified LC-II screw, which has a wider range of indications than the osseous corridor of the traditional LC-II screw. It is theoretically more advantageous in treating elderly patients with fragile pelvic fractures.
Safely, accurately, and expeditiously placing access screws is a paramount concern for orthopedic surgeons. This study ascertained that the skin entry point for the osseous corridor of the modified LC-II screw is situated below the anterior superior iliac spine in males (69.32 ± 12.05) mm and females (74.13 ± 16.46) mm, lateral to the anterior superior iliac spine in males (21.8 ± 10.25) mm and females (24.87 ± 14.47) mm, which guides the selection of the skin entry point for percutaneous placement of the osseous corridor of the modified LC-II screw. The study also evaluated the approach angle and coronal, sagittal, and horizontal plane angles for males (34.87 ± 5.31)° and females (33.35 ± 5.61)°, 34.94 ± 3.16 and 33.31 ± 3.6°, and 35.57 ± 4.74° and 38.75 ± 5.66°, respectively. The angle between the nail entry angle and the median pelvic line of the modified LC-II screw in the anterior–posterior view was 43.23 ± 3.87° in males and 44.49 ± 5.31° in females, and the angle between the nail entry angle and the median pelvic line in the inlet view was 35.06 ± 3° in males and 33.58 ± 2.94° in females. These parameters can provide a theoretical basis for determining the approach angle of the osseous corridor of modified LC-II screws. Because the entry parameters vary widely among individuals, we recommend individualized application, and preoperative planning is essential to reduce radiation exposure and shorten operation time. The number of fluoroscopic adjustments can also be reduced. During modified LC-II screw placement, it is critical to avoid penetrating the bone in front of the sacroiliac joint to prevent damage to important nerves and vascular structures, such as anterior iliac vessels and the lumbosacral trunk. Moreover, the depth of screw placement must be meticulously considered, and the head thread of the lag screw should be threaded only through the sacroiliac joint to prevent penetration too deep into the sacral foramen and spinal canal.
Although the osseous corridor of the modified LC-II screw and nail placement parameters have been established, several concerns remain regarding the technique's implementation. The present study solely measured imaging specimens, and further verification of access parameters via cadaveric specimens is warranted. Biomechanical analysis is also necessary to confirm the mechanical stability of the screws. Additionally, the lack of a specific fluoroscopic position is a concern, and multiple fluoroscopic positions should be utilized to confirm screw placement during clinical application. However, the risk of collateral damage resulting from screw penetration must be considered. Furthermore, the study's limited patient sample size and short follow-up period necessitate a long-term, multicenter randomized controlled clinical trial to evaluate patient prognosis.
Conclusion
All the males and females had a complete osseous corridor with the modified LC-II screw in the present study. The clinical results of the patients who were treated with modified LC-II screw fixation suggest that the novel method has a good preliminary outcome.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due the Third Affiliated Hospital of Southern Medical University, China but are available from the corresponding author on reasonable request.
References
Starr, A. J., Walter, J. C., Harris, R. W., Reinert, C. M. & Jones, A. L. Percutaneous screw fixation of fractures of the iliac wing and fracture-dislocations of the sacro-iliac joint (OTA Types 61–B22 and 61–B23, or Young-Burgess “lateral compression type II” pelvic fractures). J. Orthop. Trauma. 16(2), 116–123 (2002).
Starr, A. J., Nakatani, T., Reinert, C. M. & Cederberg, K. Superior pubic ramus fractures fixed with percutaneous screws: What predicts fixation failure?. J. Orthop. Trauma. 22(2), 81–87 (2008).
Majeed, S. A. External fixation of the injured pelvis: The functional outcome. J. Bone Joint Surg. Br. 72(4), 612–614 (1990).
Matta, J. M. & Tornetta, P. R. Internal fixation of unstable pelvic ring injuries. Clin. Orthop. Relat. Res. 329, 129–140 (1996).
Rommens, P. M. et al. Fragility fractures of the pelvis: Should they be fixed?. Acta Chir. Orthop. Traumatol. Cech. 82(2), 101–112 (2015).
Hutchings, L., Roffey, D. M. & Lefaivre, K. A. Fragility fractures of the pelvis: Current practices and future directions. Curr. Osteoporos. Rep. 20(6), 469–477 (2022).
Krappinger, D., Kammerlander, C., Hak, D. J. & Blauth, M. Low-energy osteoporotic pelvic fractures. Arch. Orthop. Trauma Surg. 130(9), 1167–1175 (2010).
Morris, R. O., Sonibare, A., Green, D. J. & Masud, T. Closed pelvic fractures: characteristics and outcomes in older patients admitted to medical and geriatric wards. Postgrad. Med. J. 76(900), 646–650 (2000).
van Dijk, W. A., Poeze, M., van Helden, S. H., Brink, P. R. & Verbruggen, J. P. Ten-year mortality among hospitalised patients with fractures of the pubic rami. Injury. 41(4), 411–414 (2010).
Morghen, S. et al. The association between patient participation and functional gain following inpatient rehabilitation. Aging Clin. Exp. Res. 29(4), 729–736 (2017).
Liu, B. et al. Outcomes of Mobilisation of Vulnerable Elders in Ontario (MOVE ON): A multisite interrupted time series evaluation of an implementation intervention to increase patient mobilisation. Age Ageing. 47(1), 112–119 (2018).
Walsh, K., Roberts, J. & Bennett, G. Mobility in old age. Gerodontology. 16(2), 69–74 (1999).
Rommens, P. M. et al. Clinical pathways for fragility fractures of the pelvic ring: Personal experience and review of the literature. J. Orthop. Sci. 20(1), 1–11 (2015).
Wagner, D., Ossendorf, C., Gruszka, D., Hofmann, A. & Rommens, P. M. Fragility fractures of the sacrum: How to identify and when to treat surgically?. Eur. J. Trauma Emerg. Surg. 41(4), 349–362 (2015).
Cole, P. A., Dyskin, E. A. & Gilbertson, J. A. Minimally-invasive fixation for anterior pelvic ring disruptions. Injury. 46(Suppl 3), S27–S34 (2015).
Li, X. S. et al. Modified percutaneous iliosacral screw and anterior internal fixator technique for treating unstable pelvic fractures: A retrospective study. BMC Musculoskelet. Disord. 23(1), 1068 (2022).
Puchwein, P. et al. Percutaneous fixation of acetabular fractures: Computer-assisted determination of safe zones, angles and lengths for screw insertion. Arch. Orthop. Trauma Surg. 132(6), 805–811 (2012).
Chen, H., Tang, P., Yao, Y., She, F. & Wang, Y. Anatomical study of anterior column screw tunnels through virtual three-dimensional models of the pelvis. Eur. J. Orthop. Surg. Traumatol. 25(1), 105–110 (2015).
Shen, Z. et al. Morphometric characteristics of sacral-2 alar iliac screw fixation in pediatric population. Spine. 44(10), E571–E578 (2019).
Tian, X. et al. Morphometry of iliac anchorage for transiliac screws: A cadaver and CT study of the Eastern population. Surg. Radiol. Anat. 32(5), 455–462 (2010).
Rommens, P. M. & Hofmann, A. Comprehensive classification of fragility fractures of the pelvic ring: Recommendations for surgical treatment. Injury. 44(12), 1733–1744 (2013).
Nakayama, Y. et al. Interdigitating percutaneous screw fixation for Rommens type IIIa fragility fractures of the pelvis: Technical notes and preliminary clinical results. Int. Orthop. 44(11), 2431–2436 (2020).
Eno, J. J., Boone, C. R., Bellino, M. J. & Bishop, J. A. The prevalence of sacroiliac joint degeneration in asymptomatic adults. J. Bone Joint Surg. Am. 97(11), 932–936 (2015).
Ha, K. Y., Lee, J. S. & Kim, K. W. Degeneration of sacroiliac joint after instrumented lumbar or lumbosacral fusion: A prospective cohort study over five-year follow-up. Spine. 33(11), 1192–1198 (2008).
Chang, T. L., Sponseller, P. D., Kebaish, K. M. & Fishman, E. K. Low profile pelvic fixation: Anatomic parameters for sacral alar-iliac fixation versus traditional iliac fixation. Spine 34(5), 436–440 (2009).
Funding
This study was supported by National Natural Science Foundation of China (82072411), National Key Research and Development Program of China (2022YFC2504303), Guangzhou Clinical High-tech and Major Technology Projects (2024PL-GX11).
Author information
Authors and Affiliations
Contributions
Jingqi Deng and Tao Li contribute equally to this work; Jingqi Deng and Zhenhua Zhu: study implementation, data collection and organization, data analysis and interpretation, manuscript writing and revision; Jiajun Mo, Yilan Liao, and Peiyi Liu: data collection and organization; Jiacheng Li and Sheqiang Chen: data organization, data analysis and interpretation; Shicai Fan: manuscript topic selection, research design, surgical operation, manuscript review; Tao Li: research design, manuscript revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Deng, J., Zhu, Z., Li, T. et al. A new technique for percutaneous screw fixation for treating FFP IIIa and IIIb fragility fractures of the pelvis. Sci Rep 14, 17681 (2024). https://doi.org/10.1038/s41598-024-68201-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-68201-4
- Springer Nature Limited