Abstract
Conflicting evidence still exists regarding Vitamin B12’s involvement in coronary heart disease (CHD). There is no precedent for previous studies to include both Vitamin B12, Vitamin B6, as well as Vitamin E in the consideration of CHD associating factors. Our data derived from the National Health and Nutrition Examination Survey (NHANES), which covers the period 2003–2020. 33,640 samples were included in this cross-sectional study. We used an unadjusted covariates and three adjusted covariates. The intake percentage of Vitamins E, B6, and B12 was categorized into continuous and categorical variables using multivariate logistic regression analysis and subgroup logistic regression. To estimate these trends, we applied the percentage categories of Vitamin E, B6, and B12 intake as continuous variables. We recorded Vitamin E, B6, B12, age, race, BMI, gender, household annual income, education level, hypertension status, diabetes status, smoking status, and drinking status for included samples. Multivariate regression analysis revealed that Vitamin E and B6 were negatively associated with CHD and exerted protective effects, while Vitamin B12 had little correlation with CHD. Based on the quartiles of Vitamin E and Vitamin B6 percentage, the strongest protective effect was observed in the third quartile (Q3). Analyses of subgroups showed the effects of Vitamin B6 and Vitamin E on CHD were more noticeable in women, the participant’s BMI was in the 25–30 range, and participants who smoked. We identified the possible protective effect of Vitamin E and Vitamin B6 against CHD, especially in female, obese, and smoking populations, whereas income and education were also viewed as influencing factors that could be taken into account.
Similar content being viewed by others
Introduction
Coronary heart disease (CHD) ranks as one of the most devastating drivers of human mortality1. The CHD development can be ascribed mainly to genetic factors and poor lifestyle habits2. With regard to lifestyle habits, among the various recognized risk factors for CHD, food and eating habits have performed crucial roles which are also preventable3. An increasing number of evidence supports that a high-quality food-based diet which may be involved a more balanced intake of different Vitamins can facilitate the prevention of poor prognosis in CHD4.
As a fat-soluble antioxidant, Vitamin E comprises compounds such as tocopherols and tocotrienols. In the course of atherosclerosis in CHD, Vitamin E probably slows the progression through its ability to inhibit the oxidative modification of low-density lipoprotein cholesterol and reduce its uptake into the arterial wall5. The B Vitamins, including Vitamin B6 and Vitamin B12, have essential roles in the one-carbon metabolic pathway that is linked to homocysteine metabolism6. Previous evidences have demonstrated that the dietary ingestion of Vitamin B6 may help reduce the risk of CHD, while Vitamin B12 in the diet has also been implicated as a protective factor against CHD7.
However, some studies have also explored whether serum homocysteine, folate, and Vitamin B12 are associated with CHD in the elderly, denying the role of Vitamin B12 as a predictor of CHD mortality8. Conflicting evidence still exists regarding the relationship between Vitamin B12 and CHD. Consequently, it is imperative to undertake additional research to elucidate the precise mechanisms by which Vitamin E, B6, and B12 intake may modulate the risk of coronary heart disease. In this cross-sectional analysis, we investigated the correlation between the intake of Vitamins E, B6, and B12 and the prevalence of coronary heart disease, utilizing data extracted from the National Health and Nutrition Examination Survey (NHANES) spanning the years 2003 to 2020. Our objective was to identify the optimal dietary intake levels of these Vitamins to inform evidence-based dietary recommendations for the management of coronary heart disease in clinical practice.
Materials and methods
Data source
Our data derived from the NHANES, which covers the period 2003–2020. In 1999, this research became a continuous program that continuously focuses on various health and nutritional measures to meet emerging needs, representing a cycle every 2 years. The survey surveyed a nationally representative sample of approximately 5000 people annually, more detailed information about the NHANES (https://www.cdc.gov/nchs/nhanes/) program and research procedures are available online. NHANES is a comprehensive, population-based survey conducted within the United States. Utilizing a sophisticated multi-stage sampling approach, NHANES gathers data on demographics, lifestyle factors, and various health outcomes through in-person interviews. First, we excluded the missing data of CHD, Vitamin E, Vitamin B6 and Vitamin B12 (n = 5810), and then excluded other variables, including age, race, gender, education level, annual family income, hypertension status, BMI, diabetes status, drinking status and smoking status (n = 13,642). 33,640 adult participants who met the selection criteria were included in our analysis. The flowchart of the screening process is shown in Fig. 1. All NHANES research protocols have been approved by the Research Ethics Review Committee of the National Center for Health Statistics (NCHS) as well as consented by all participants, and the data for this study can be accessed through publicly available NHANES data files.
Assessment of outcomes and exposures
The prime outcome is whether the participants have CHD. In the NHANES medical condition section (prefix MCQ), personal interview data on self-reported health conditions of children and adults is provided. Whether participants suffer from CHD is determined through participants’ self-report. This part of the questionnaire was conducted using the CAPI (Interviewer Management) system before the physical examination, The participants who answered ‘yes’ were considered to have CHD by asking ‘Have any doctors or other health professionals informed you/the sample person that SP has CHD?’.
Participants in the NHANES study were tasked with providing a detailed account of their dietary intake, including calories, nutrients, and other food components consumed within the 24 h preceding the interview. Eligible for two separate 24-h dietary recall interviews, each NHANES participant underwent the first interview on-site at the Mobile Examination Center (MEC), followed by a second interview conducted via telephone 3 to 10 days later. The comprehensive protocol and data collection methodologies are thoroughly outlined in the NHANES Dietary Interview Procedure Manual (https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/questionnaires.aspx?Cycle=2019-2020). For our study, we calculated the 24-h dietary intake of Vitamin E, B6, and B12 (mg) based on the averaged data from the two 24-h dietary recall interviews.
Assessment of covariates
We comprehensively screened 10 possible confounding factors related to CHD, namely age, gender, race, education level, BMI, annual family income, diabetes status, hypertension status, smoking status and drinking status, which were all identified as risk factors, as described in the relationship between drinking and CHD9, hypertension and CHD10, and diabetes and CHD11.The patient’s age range is between 20 and 85 years old. The range of BMI is 13.18–130.21. Race is Mexican American and other Hispanic, non Hispanic black, non Hispanic white, and other races. Gender is male and female. Education level is considered lower than high school education, higher than high school education, and higher than high school education. The annual income of households is divided into over $20,000 and under $20,000. As well as some self-reported chronic diseases: hypertension and diabetes. Participants in other variables are distinguished by yes or no.
Statistical analysis
A complex sampling weights was adopted by our research, as recommended by the Centers for Disease Control and Prevention (CDC) in the United States (weight of the first day of diet samples). We combined sample weights for 9 consecutive cycles based on the method recommended by NHANES. In the table of baseline feature, continuous variables are represented by survey weighted average (standard error), and categorical variables are represented by sample size (survey weighted percentage). To explore the relationship between Vitamin E, Vitamin B6, Vitamin B12, and CHD, we used an unadjusted model that did not adjust for covariates and three multivariable models adjusting for different covariables. Model 1 adjusted based on age, sex, education level, race, and family income. Model 2 adjusted based on age, sex, education level, race, family income, smoking status and drinking status. Model 3 was adjusted according to age, sex, education level, race, family income, BMI, drinking status, smoking status, hypertension and diabetes mellitus. Subgroup analyses were stratified by age, sex, education level, race, family income, BMI, drinking status, smoking status, hypertension and diabetes mellitus to discuss the stability of the relationship between CHD prevalence and Vitamin E, B6, and B12 intake in each stratified subgroup. Estimate these trends using the percentage categories of Vitamin E, B6, and B12 intake as a continuous variable. It was conducted leveraging R 4.2.0 (http://www.R-project.org) and EmpowerStats (http://www.empowerstats.com, X&Y Solutions, Inc.) for all analyses. When p < 0.05, all statistical analyses in this study were statistically significant.
Results
Participant characteristics
Participants were grouped into non-CHD (n = 32,211) and CHD (n = 1429). We recorded the following variables for included samples: Vitamin E, Vitamin B6, Vitamin B12, age, gender, household annual income, education level, race, BMI, smoking status, diabetes status, hypertension status, and drinking status. There was a significant difference in Vitamin B12 levels between the two groups, with the CHD group having a level of 4.93 (0.21) and the non-CHD group having a level of 5.24 (0.05). Except for smoking status, there were significant differences in baseline characteristics between the two groups. Participants in the CHD group were older (67.25 (0.36) vs 46.68 (0.23), P < 0.0001), had lower levels of Vitamin B6 (P = 0.001) and Vitamin E (P = 0.003) than the non-CHD group, and had a higher BMI than the non-CHD group (P < 0.0001). Participants in the CHD group were more likely to have hypertension and a history of alcohol consumption (both P < 0.0001). Additionally, noticeable differences between the two groups in terms of racial distribution and education level (both P < 0.0001) (Table 1), and their basic characteristics are shown in Table 1.
Association of Vitamin E, Vitamin B6, Vitamin B12 intake with coronary heart disease
Multivariate regression analysis revealed that Vitamin E and Vitamin B6 were negatively associated with CHD and exerted protective effects, while Vitamin B12 had little correlation with CHD.
In view of the quartiles of Vitamin E percentage, the third quartile (Q3) in all four models manifested a negative relevance between Vitamin E percentage and the suffering from CHD, indicating a protective effect. In comparison with the first quartile (Q1) of the overall, the fully adjusted model manifested a stronger protective effect against CHD in the Q3 (OR 0.66; 95% CI 0.52 to 0.83). The P value for the trend was < 0.03, with a P value of < 0.001 (Table 2). Among all the models, the strongest protective effect was observed in the third quartile (Q3), where the intake of Vitamin E was 6.45 to 9.89 mg, which maximally reduced the prevalence of CHD.
In view of the quartiles of Vitamin B6 percentage, all four models manifested a negative relevance between Vitamin B6 percentage and the suffering from CHD, indicating a protective effect. In comparison with the first quartile (Q1) of the overall, the fully adjusted model manifested a stronger protective effect against CHD in the third quartile (Q3) (OR 0.77; 95% CI 0.62 to 0.94). The P value for the trend was < 0.01 (Table 2). Among all the models, the strongest protective effect was observed in the third quartile (Q3), where the intake of Vitamin B6 was 1.703 to 2.466 mg, which maximally reduced the prevalence of CHD.
In view of the quartiles of Vitamin B12 percentage, most models manifested no statistically significant relevance between Vitamin B12 percentage and the suffering from CHD. Vitamin B12 intake was found to maybe increase the risk of coronary heart disease. In the original model (OR 1.23; 95% CI 1.02 to 1.49, P = 0.03) Vitamin B12 quartile 2 intake was statistically significant.
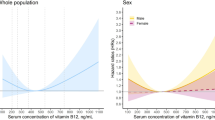
In addition, dose–response relationships between the prevalence of CHD and intake of Vitamin E, Vitamin B6, and Vitamin B12 were examined using RCS curves. We identified a nonlinear relationship between Vitamin E, Vitamin B6 and CHD (nonlinear P-value = 0.0004, nonlinear P-value = 0.0403). As Vitamin E intake increased, the OR curve for CHD decreased first, followed by a slow increase, finally to stabilize. The turning point of the OR curve was found to be 7.54 mg/day of Vitamin E intake (Fig. 2A). According to Fig. 2B, it was found that the OR curve for CHD dropped sharply at first with the increase in Vitamin B6 intake, then rose slowly and finally leveled off. The turning point of the OR curve was found to be 2.65 mg/day of Vitamin B6 intake. For Vitamin B12 there was no non-linear relationship found with CHD (non-linear P-value = 0.1322).
(A) RCS curves describing the dose–response relationship between Vitamin E intake and coronary heart disease. (B) RCS curves describing the dose–response relationship between Vitamin B6 intake and coronary heart disease. (C) RCS curves describing the dose–response relationship between Vitamin B12 intake and coronary heart disease. The following covariates were adjusted for: age, sex, education level, race, family income, BMI, drinking status, smoking status, hypertension and diabetes mellitus.
We also conducted RCS curve analyses for the drinking as well as smoking status subgroups which revealed that the OR curve for the non-drinking population started with an increase and then decreased sharply with a turning point at 3.18 mg/day of Vitamin E intake, whereas the OR curve for the drinking population was the opposite of that of the non-drinking population, with the curve decreasing sharply and then increasing, which turned at 7.48 mg/day of Vitamin E intake (Fig. 3A). For the smoking status subgroup, we can find that the OR curve for the nonsmoking population first rises, then falls sharply, and then rises again, with a turning point at 7.54 mg/day of Vitamin E intake, while the OR curve for the drinking population is the opposite of that of the non-drinking population, with the curve first falling sharply, then rising, with a turning point at 7.48 mg/day of Vitamin E intake (Fig. 3B). For the RCS curve analysis of Vitamin B6, we found that the OR curve of the drinking population decreased and then increased, with a turning point at 2.53 mg/day of Vitamin B6 intake, while the curve of the non-drinking population showed a decreasing trend (Fig. 3C); the OR curve of the non-smoking population decreased with the increase of Vitamin B6 intake, whereas the smoking population showed the opposite trend, which increased with the increase of intake (Fig. 3D). All of the above analyses were performed under the fully adjusted model.
(A) RCS curves describing the dose–response relationship between Vitamin E intake and coronary heart disease by grouping based on drinking status. (B) RCS curves describing the dose–response relationship between Vitamin E intake and coronary heart disease by grouping based on smoking status. (C) RCS curves describing the dose–response relationship between Vitamin B6 intake and coronary heart disease by grouping based on drinking status. (D) RCS curves describing the dose–response relationship between Vitamin B6 intake and coronary heart disease by grouping based on smoking status. The following covariates were adjusted for: age, sex, education level, race, family income, BMI, drinking status, smoking status, hypertension and diabetes mellitus.
Analyses of subgroups and interactions
Figure 4 presents the results of stratified analysis based on age, gender, education level, body BMI, household annual income, race, diabetes status, hypertension status, smoking status, and drinking status. These factors significantly influence the risk of CHD, therefore we conducted stratified analysis for a more insightful understanding of the links between Vitamin E, Vitamin B6, and Vitamin B12 intake and the occurrence of CHD. The results of stratified analysis showed that in racial subgroup analysis, the intake of Vitamin B6 in Mexican Americans possessed a negative correlation with the probability of suffering from CHD (odds ratio [OR] 0.77, P = 0.002). The intake of Vitamin B6 in non Hispanic black individuals possessed a negative correlation with the probability of suffering from CHD (odds ratio [OR] 0.81, P = 0.03), while the intake of Vitamin B6 in non Hispanic white individuals possessed a negative correlation with the probability of suffering from CHD (odds ratio [OR] 0.94, P = 0.03), The intake of Vitamin B12 in Mexican Americans possessed a negative correlation with the probability of suffering from CHD (odds ratio [OR] 0.92, P = 0.01). In racial subgroup analysis, the intake of Vitamin B6 in women possessed a negative correlation with the probability of suffering from CHD (odds ratio [OR] 0.85, P < 0.0001), while the intake of Vitamin E in women possessed a negative correlation with the probability of suffering from CHD (odds ratio [OR] 0.97, P = 0.001). In BMI subgroup analysis, when the participant’s BMI was in the 25–30 range, the intake of Vitamin B6 possessed a negative correlation with the probability of suffering from CHD (odds ratio [OR] 0.03, P < 0.0001), the P-value of the interaction was 0.01, and the intake of Vitamin E possessed a negative correlation with the probability of suffering from CHD (odds ratio [OR] 0.43, P < 0.0001), and the P-value of the interaction was 0.005. In the subgroup analysis of smoking status, when participants smoked, the intake of Vitamin B6 possessed a negative correlation with the probability of suffering from CHD (odds ratio [OR] 0.90, P < 0.001), and the intake of Vitamin E possessed a negative correlation with the probability of suffering from CHD (odds ratio [OR] 0.97, P < 0.001). In the subgroup analysis of household annual income, when the participant’s household annual income was less than $20,000, the intake of Vitamin E possessed a negative correlation with the probability of suffering from CHD (odds ratio [OR] 0.93, P < 0.0001), and the interaction was P < 0.001. The intake of Vitamin B12 possessed a negative correlation with the probability of suffering from CHD (odds ratio [OR] 0.94, P = 0.002); When the annual household income of participants is ≥ $20,000, the intake of Vitamin B6 possessed a negative correlation with the probability of suffering from CHD (odds ratio [OR] 0.95, P = 0.02). In the subgroup analysis of education level, when the participants had a high school education level, the intake of Vitamin B6 possessed a negative correlation with the probability of suffering from CHD (odds ratio [OR] 0.88, P = 0.02), and the intake of Vitamin E possessed a negative correlation with the probability of suffering from CHD (odds ratio [OR] 0.95, P = 0.02), with a p-value of 0.01 for the interaction; When the participant’s education level is higher than high school level, the intake of Vitamin B6 possessed a negative correlation with the probability of suffering from CHD (odds ratio [OR] 0.94, P = 0.02).
Discussion
On the basis of a large sample of 33,640 cases, our study analyzed the relationship of Vitamin E, Vitamin B6, and Vitamin B12 with CHD, proving that Vitamin E and Vitamin B6 exerted a possible protective effect against CHD, while Vitamin B12 displayed no significant correlation with CHD. Taking the dose–response relationship into account, moreover, we discovered that the prevalence of CHD was minimized when Vitamin E intake ranged from 6.45 to 9.89 mg, whereas the intake of Vitamin B6 with the strongest CHD-protective effect ranged from 1.703 to 2.466 mg. Among all models, the protective effect to CHD of Q3 was strongest from Q2 to Q4, indicating a nonlinear correlation of Vitamin E and Vitamin B6 with CHD. In particular, the conclusions regarding Vitamin B6 were consistent with a previous nonlinear dose–response meta-analysis6. The underlying mechanism regarding the intricate association between Vitamin B6 and CHD may perhaps be explained by several cardioprotective properties of Vitamin B612. Studies have shown that Vitamin B6 has anti-inflammatory13, antioxidant14, and antithrombotic effects15, acts as a vital role in DNA methylation and repair16, and contributes to the transsulfuration pathway of hcy metabolism17. These all provide some evidence to support the cardioprotective mechanism of Vitamin B6. As for the protective effect of Vitamin E against CHD, in addition to its antioxidant activity, it may be elucidated from the perspective of regulating molecular signaling18.
The results of the ethnic subgroup analysis revealed that the effects of Vitamin B6 and Vitamin E on CHD were more noticeable in women. It probably has something to do with the fact that micronutrients serve as a greater role in womankind’s particular pregnancy physiology19. It is also evident that the protective effects of Vitamin E and Vitamin B6 against CHD are significant in obese patients. A prevalence study backed up the negative relevance between serum Vitamin E levels and overweight in adolescents. In parallel, it proposed that higher serum Vitamin E levels may be associated with a lower likelihood of obesity in girls, but not in boys20. This gender distinction agrees to some extent with the results of our study. Adding to this, obesity may also differentially regulate Vitamin b6-related metabolic pathways in the body21. Smoking is a recognized risk factor for CHD. Our study found a potential interlinkage of smoking and Vitamin E and Vitamin B6 with the risk of CHD. Related studies have suggested the implication of different genotypes in this association22, but more clinical evidence is still needed to underpin this conclusion.
A couple of interesting findings were also made in the subgroup analyses of annual household income and educational attainment. The associations of Vitamin E and Vitamin B12 intake with the development of CHD were greater when household annual income was lower, whereas it was Vitamin B6 that was more prominent when participants had higher household annual income. Vitamin B6 all showed a strong negative correlation with the occurrence of CHD when participants’ education was at the high school level and above. However, the association of Vitamin E was only demonstrated when participants’ education was at the high school level. There are fewer targeted studies on the relationship between Vitamin intake with income and education. One study has analyzed the nutritional status of older persons in home care by correlating it with the income and educational level of the caregiver. They concluded that the literacy of the caregiver was a determinant of the nutritional status of seniors, while income had no correlation with the nutritional status of seniors. Although this conclusion seems to be in slight conflict with the findings of our study, it can only be taken with a grain of salt in view of the different subjects studied23.
Naturally, limitations of the study are inevitable. First, the relationship between Vitamin B6, Vitamin E, with CHD could not be definitively established owing to the inclusion of a sample from a cross-sectional survey rather than a cohort study. Next, it was not feasible to completely exclude the effect of other possible muddled covariates, as the inclusion of covariates was on the basis of retrospective survey data. Lastly, an extended period of time was spanned by the sample included in this study, which may have been accompanied by changes in ground conditions.
Conclusion
To summarize, for a large sample of 33,640 cases, we identified the possible protective effect of Vitamin E and Vitamin B6 against CHD, especially in female, obese, and smoking populations, whereas income and education were also viewed as influencing factors that could be taken into account. It is worth emphasizing one of the strengths of this study is that we constructed the model based on the results obtained from the logistic regression analysis. Other strengths that can be mentioned include the large sample size, the continuous 18 years of investigation and the adequacy of the covariates.
Data availability
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request.
References
Heller, D. J. et al. Evaluating the impact and cost-effectiveness of statin use guidelines for primary prevention of coronary heart disease and stroke. Circulation 136(12), 1087–1098 (2017).
Kim, Y. et al. Replacing device-measured sedentary time with physical activity is associated with lower risk of coronary heart disease regardless of genetic risk. J. Intern. Med. 295, 38 (2023).
Pan, A., Lin, X., Hemler, E. & Hu, F. B. Diet and cardiovascular disease: Advances and challenges in population-based studies. Cell Metab. 27(3), 489–496 (2018).
Li, L. et al. Association between dietary intakes and plaque vulnerability measured by optical coherence tomography in patients with coronary heart disease: A mediation analysis of inflammatory factors. Front. Nutr. 9, 920892 (2022).
Pruthi, S., Allison, T. G. & Hensrud, D. D. Vitamin E supplementation in the prevention of coronary heart disease. Mayo Clin. Proc. 76(11), 1131–1136 (2001).
Jayedi, A. & Zargar, M. S. Intake of Vitamin B6, folate, and Vitamin B12 and risk of coronary heart disease: A systematic review and dose-response meta-analysis of prospective cohort studies. Crit. Rev. Food Sci. Nutr. 59(16), 2697–2707 (2019).
Ishihara, J. et al. Intake of folate, Vitamin B6 and Vitamin B12 and the risk of CHD: The Japan Public Health Center-based prospective study cohort I. J. Am. Coll. Nutr. 27(1), 127–136 (2008).
Gopinath, B., Flood, V. M., Rochtchina, E., Thiagalingam, A. & Mitchell, P. Serum homocysteine and folate but not Vitamin B12 are predictors of CHD mortality in older adults. Eur. J. Prev. Cardiol. 19(6), 1420–1429 (2012).
Zhang, Y. et al. Association of drinking pattern with risk of coronary heart disease incidence in the middle-aged and older Chinese men: Results from the Dongfeng-Tongji cohort. PLoS ONE 12(5), e178070 (2017).
Li, M. et al. Multi-trajectories of systolic and diastolic hypertension and coronary heart disease in middle-aged and older adults. Front. Public Health 10, 1017727 (2022).
Xiao, H. et al. Disease patterns of coronary heart disease and type 2 diabetes harbored distinct and shared genetic architecture. Cardiovasc. Diabetol. 21(1), 276 (2022).
Hu, L. et al. Association of plasma Vitamin B6 with coronary heart disease in patients undergoing diagnostic coronary angiography: New insight on sex differences. Front. Cardiovasc. Med. 8, 789669 (2021).
Lotto, V., Choi, S. W. & Friso, S. Vitamin B6: A challenging link between nutrition and inflammation in CVD. Br. J. Nutr. 106(2), 183–195 (2011).
Hsu, C. C. et al. Role of Vitamin B6 status on antioxidant defenses, glutathione, and related enzyme activities in mice with homocysteine-induced oxidative stress. Food Nutr. Res. 59, 25702 (2015).
Chang, S. J., Chang, C. N. & Chen, C. W. Occupancy of glycoprotein IIb/IIIa by B-6 vitamers inhibits human platelet aggregation. J. Nutr. 132(12), 3603–3606 (2002).
Zhong, J. et al. B Vitamins attenuate the epigenetic effects of ambient fine particles in a pilot human intervention trial. Proc. Natl. Acad. Sci. U.S.A. 114(13), 3503–3508 (2017).
Humphrey, L. L., Fu, R., Rogers, K., Freeman, M. & Helfand, M. Homocysteine level and coronary heart disease incidence: A systematic review and meta-analysis. Mayo Clin. Proc. 83(11), 1203–1212 (2008).
Meydani, M. et al. Long-term Vitamin E supplementation reduces atherosclerosis and mortality in Ldlr-/- mice, but not when fed Western style diet. Atherosclerosis 233(1), 196–205 (2014).
Crawford, S. A. et al. Micronutrient gaps and supplement use in a diverse cohort of pregnant women. Nutrients 15, 14 (2023).
Zang, X. D. et al. Serum Vitamin E concentration is negatively associated with body mass index change in girls not boys during adolescence. World J. Pediatr. 17(5), 517–526 (2021).
Um, H. J., Ko, J. W., Won, S. B. & Kwon, Y. H. Effects of dietary Vitamin B6 restriction on hepatic gene expression profile of non-obese and obese mice. Nutrients 12, 12 (2020).
He, M. A. et al. Associations of polymorphism of P22 (phox) C242T, plasma levels of Vitamin E, and smoking with coronary heart disease in China. Am. Heart J. 153(4), 640–641 (2007).
Correa, B., Leandro, M. V., Pagotto, F. K. & Marques, D. O. M. Caregiver’s education level, not income, as determining factor of dietary intake and nutritional status of individuals cared for at home. J. Nutr. Health Aging 13(7), 609–614 (2009).
Author information
Authors and Affiliations
Contributions
BL contributed to the conception and design of the study. BL, MH, YM, and XS drafted the manuscript. MH, DW, and FJ collected and analyzed the data. BL and XW revised the manuscript. All authors contributed to the manuscript revision and read and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, B., Hu, M., Ma, Y. et al. Association between Vitamin E, Vitamin B6, and Vitamin B12 with coronary heart disease. Sci Rep 14, 19960 (2024). https://doi.org/10.1038/s41598-024-68413-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-68413-8
- Springer Nature Limited